From the Lab to Real Life: Monitoring Cardiorespiratory Fitness during the COVID-19 Pandemic through Wearable Devices. An Exploratory Longitudinal Study on Healthy Participants
Abstract
:1. Introduction
2. Materials and Methods
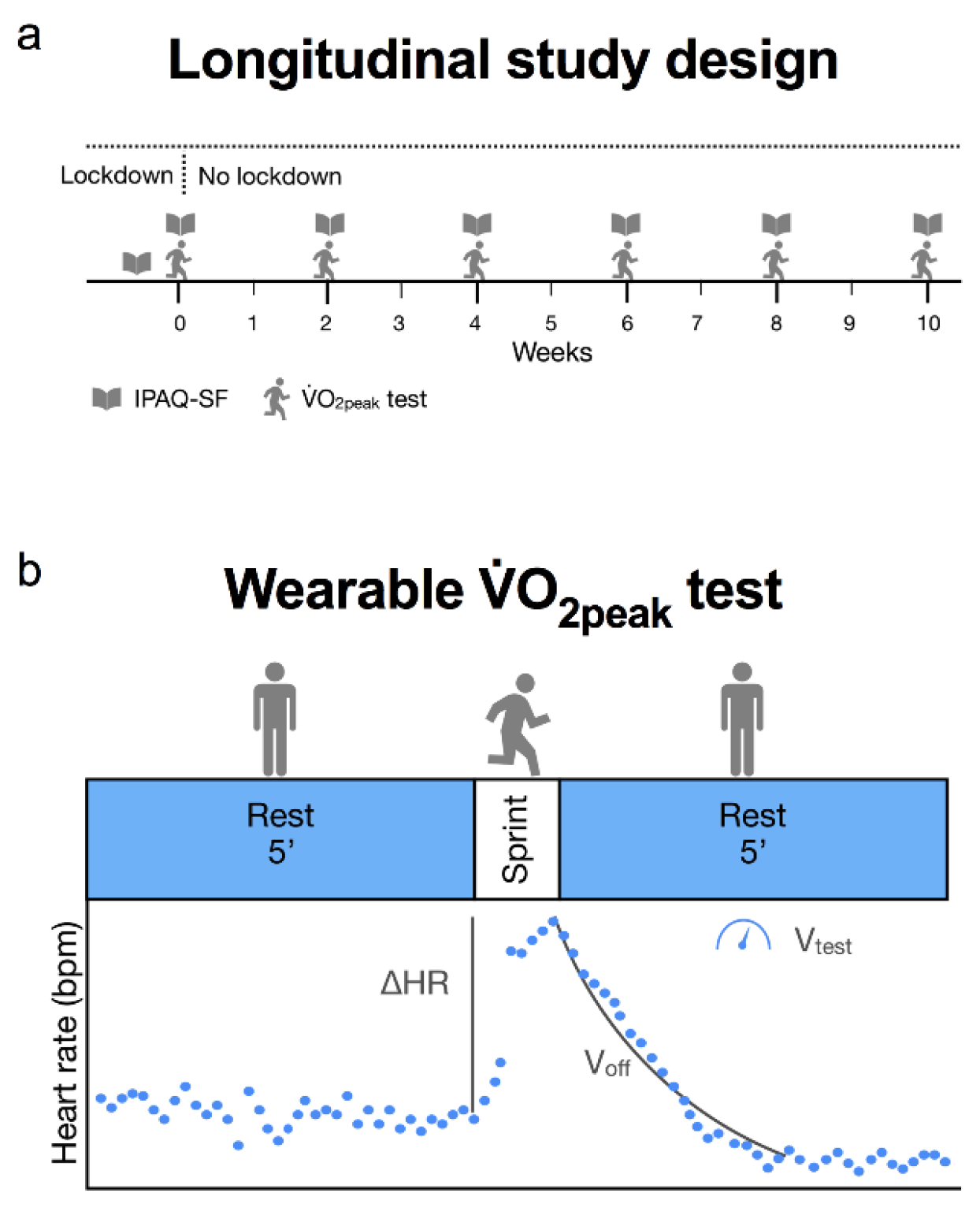
2.1. Study Design and Participants
2.2. Measurement Instruments
2.3. Statistical Analysis
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.-M. Does Physical Activity Attenuate, or Even Eliminate, the Detrimental Association of Sitting Time with Mortality? A Harmonised Meta-Analysis of Data from More than 1 Million Men and Women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef] [Green Version]
- Narici, M.; De Vito, G.; Franchi, M.; Paoli, A.; Moro, T.; Marcolin, G.; Grassi, B.; Baldassarre, G.; Zuccarelli, L.; Biolo, G.; et al. Impact of Sedentarism Due to the COVID-19 Home Confinement on Neuromuscular, Cardiovascular and Metabolic Health: Physiological and Pathophysiological Implications and Recommendations for Physical and Nutritional Countermeasures. Eur. J. Sport Sci. 2020, 21, 614–635. [Google Scholar] [CrossRef] [PubMed]
- Apple. COVID-19 Mobility Trends Reports. 2020. Available online: https://covid19.apple.com/mobility (accessed on 22 March 2022).
- Hodkinson, A.; Kontopantelis, E.; Adeniji, C.; van Marwijk, H.; McMillian, B.; Bower, P.; Panagioti, M. Interventions Using Wearable Physical Activity Trackers among Adults with Cardiometabolic Conditions: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2021, 4, e2116382. [Google Scholar] [CrossRef] [PubMed]
- Harber, M.P.; Kaminsky, L.A.; Arena, R.; Blair, S.N.; Franklin, B.A.; Myers, J.; Ross, R. Impact of Cardiorespiratory Fitness on All-Cause and Disease-Specific Mortality: Advances Since 2009. Prog. Cardiovasc. Dis. 2017, 60, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Luciano, F.; Cenacchi, V.; Vegro, V.; Pavei, G. COVID-19 Lockdown: Physical Activity, Sedentary Behaviour and Sleep in Italian Medicine Students. Eur. J. Sport Sci. 2021, 21, 1459–1468. [Google Scholar] [CrossRef] [PubMed]
- Runacres, A.; Mackintosh, K.A.; Knight, R.L.; Sheeran, L.; Thatcher, R.; Shelley, J.; McNarry, M.A. Impact of the COVID-19 Pandemic on Sedentary Time and Behaviour in Children and Adults: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 11286. [Google Scholar] [CrossRef]
- Zaccagni, L.; Toselli, S.; Barbieri, D. Physical Activity during COVID-19 Lockdown in Italy: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6416. [Google Scholar] [CrossRef]
- Booth, F.W.; Roberts, C.K.; Thyfault, J.P.; Ruegsegger, G.N.; Toedebusch, R.G. Role of Inactivity in Chronic Diseases: Evolutionary Insight and Pathophysiological Mechanisms. Physiol. Rev. 2017, 97, 1351–1402. [Google Scholar] [CrossRef]
- Ried-Larsen, M.; Aarts, H.M.; Joyner, M.J. Effects of Strict Prolonged Bed Rest on Cardiorespiratory Fitness: Systematic Review and Meta-Analysis. J. Appl. Physiol. 2017, 123, 790–799. [Google Scholar] [CrossRef]
- Saltin, B.; Blomqvist, G.; Mitchell, J.H.; Johnson, R.L.; Wildenthal, K.; Chapman, C.B. Response to Exercise after Bed Rest and after Training. Circulation 1968, 38, VII1-78. [Google Scholar]
- Tipton, M.; Wilkes, M.; Long, G.; Morgan, P.; Roiz de Sa, D.; Corbett, J.; Montgomery, H.; Mekjavic, I.; Friedl, K. Returning to the Laboratory. The Physiological Society. Available online: https://Www.Physoc.Org/Covid19/Returning-to-the-Lab (accessed on 25 March 2022).
- McDonough, D.J.; Helgeson, M.A.; Liu, W.; Gao, Z. Effects of a Remote, YouTube-Delivered Exercise Intervention on Young Adults’ Physical Activity, Sedentary Behavior, and Sleep during the COVID-19 Pandemic: Randomized Controlled Trial. J. Sport Health Sci. 2021, in press. [Google Scholar] [CrossRef] [PubMed]
- Natalucci, V.; Marini, C.F.; Flori, M.; Pietropaolo, F.; Lucertini, F.; Annibalini, G.; Vallorani, L.; Sisti, D.; Saltarelli, R.; Villarini, A.; et al. Effects of a Home-Based Lifestyle Intervention Program on Cardiometabolic Health in Breast Cancer Survivors during the COVID-19 Lockdown. J. Clin. Med. 2021, 10, 2678. [Google Scholar] [CrossRef] [PubMed]
- Storniolo, J.L.; Pavei, G.; Minetti, A.E. A “Wearable” Test for Maximum Aerobic Power: Real-Time Analysis of a 60-m Sprint Performance and Heart Rate Off-Kinetics. Front. Physiol. 2017, 8, 868. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [Green Version]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef] [Green Version]
- Hale, T.; Angrist, N.; Goldszmidt, R.; Kira, B.; Petherick, A.; Phillips, T.; Webster, S.; Cameron-Blake, E.; Hallas, L.; Majumdar, S.; et al. A Global Panel Database of Pandemic Policies (Oxford COVID-19 Government Response Tracker). Nat. Hum. Behav. 2021, 5, 529–538. [Google Scholar] [CrossRef]
- IPAQ Scoring Protocol—International Physical Activity Questionnaire. Available online: https://sites.google.com/site/theipaq/scoring-protocol (accessed on 22 March 2022).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- RStudio Team. RStudio: Integrated Development for R; RStudio, PBC: Boston, MA, USA, 2020. [Google Scholar]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting Linear Mixed-Effects Models Using Lme4. J. Stat. Soft. 2015, 67, 1–48. [Google Scholar] [CrossRef]
- Florian Hartig. DHARMa: Resid2ual Diagnostics for Hierarchical (Multi-Level/Mixed) Regression Models. R Package Version 0.4.4. 2021. Available online: http://Florianhartig.Github.Io/DHARMa (accessed on 22 March 2022).
- Wasserstein, R.L.; Lazar, N.A. The ASA Statement on P-Values: Context, Process, and Purpose. Am. Stat. 2016, 70, 129–133. [Google Scholar] [CrossRef] [Green Version]
- Knudsen, S.H.; Hansen, L.S.; Pedersen, M.; Dejgaard, T.; Hansen, J.; Hall, G.V.; Thomsen, C.; Solomon, T.P.J.; Pedersen, B.K.; Krogh-Madsen, R. Changes in Insulin Sensitivity Precede Changes in Body Composition during 14 Days of Step Reduction Combined with Overfeeding in Healthy Young Men. J. Appl. Physiol. 2012, 113, 7–15. [Google Scholar] [CrossRef] [Green Version]
- Krogh-Madsen, R.; Thyfault, J.P.; Broholm, C.; Mortensen, O.H.; Olsen, R.H.; Mounier, R.; Plomgaard, P.; van Hall, G.; Booth, F.W.; Pedersen, B.K. A 2-Wk Reduction of Ambulatory Activity Attenuates Peripheral Insulin Sensitivity. J. Appl. Physiol. 2010, 108, 1034–1040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Batacan, R.B.; Duncan, M.J.; Dalbo, V.J.; Tucker, P.S.; Fenning, A.S. Effects of High-Intensity Interval Training on Cardiometabolic Health: A Systematic Review and Meta-Analysis of Intervention Studies. Br. J. Sports Med. 2017, 51, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Bonato, M.; Turrini, F.; De Zan, V.; Meloni, A.; Plebani, M.; Brambilla, E.; Giordani, A.; Vitobello, C.; Caccia, R.; Piacentini, M.F.; et al. A Mobile Application for Exercise Intervention in People Living with HIV. Med. Sci. Sports Exerc. 2020, 52, 425–433. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luciano, F.; Cenacchi, V.; Ruggiero, L.; Pavei, G. From the Lab to Real Life: Monitoring Cardiorespiratory Fitness during the COVID-19 Pandemic through Wearable Devices. An Exploratory Longitudinal Study on Healthy Participants. Healthcare 2022, 10, 634. https://doi.org/10.3390/healthcare10040634
Luciano F, Cenacchi V, Ruggiero L, Pavei G. From the Lab to Real Life: Monitoring Cardiorespiratory Fitness during the COVID-19 Pandemic through Wearable Devices. An Exploratory Longitudinal Study on Healthy Participants. Healthcare. 2022; 10(4):634. https://doi.org/10.3390/healthcare10040634
Chicago/Turabian StyleLuciano, Francesco, Valentina Cenacchi, Luca Ruggiero, and Gaspare Pavei. 2022. "From the Lab to Real Life: Monitoring Cardiorespiratory Fitness during the COVID-19 Pandemic through Wearable Devices. An Exploratory Longitudinal Study on Healthy Participants" Healthcare 10, no. 4: 634. https://doi.org/10.3390/healthcare10040634
APA StyleLuciano, F., Cenacchi, V., Ruggiero, L., & Pavei, G. (2022). From the Lab to Real Life: Monitoring Cardiorespiratory Fitness during the COVID-19 Pandemic through Wearable Devices. An Exploratory Longitudinal Study on Healthy Participants. Healthcare, 10(4), 634. https://doi.org/10.3390/healthcare10040634





