The Influence of Risk Factors in the Early Detection of Developmental Dysplasia of the Hip in a Country with Limited Material Resources
Abstract
:1. Introduction
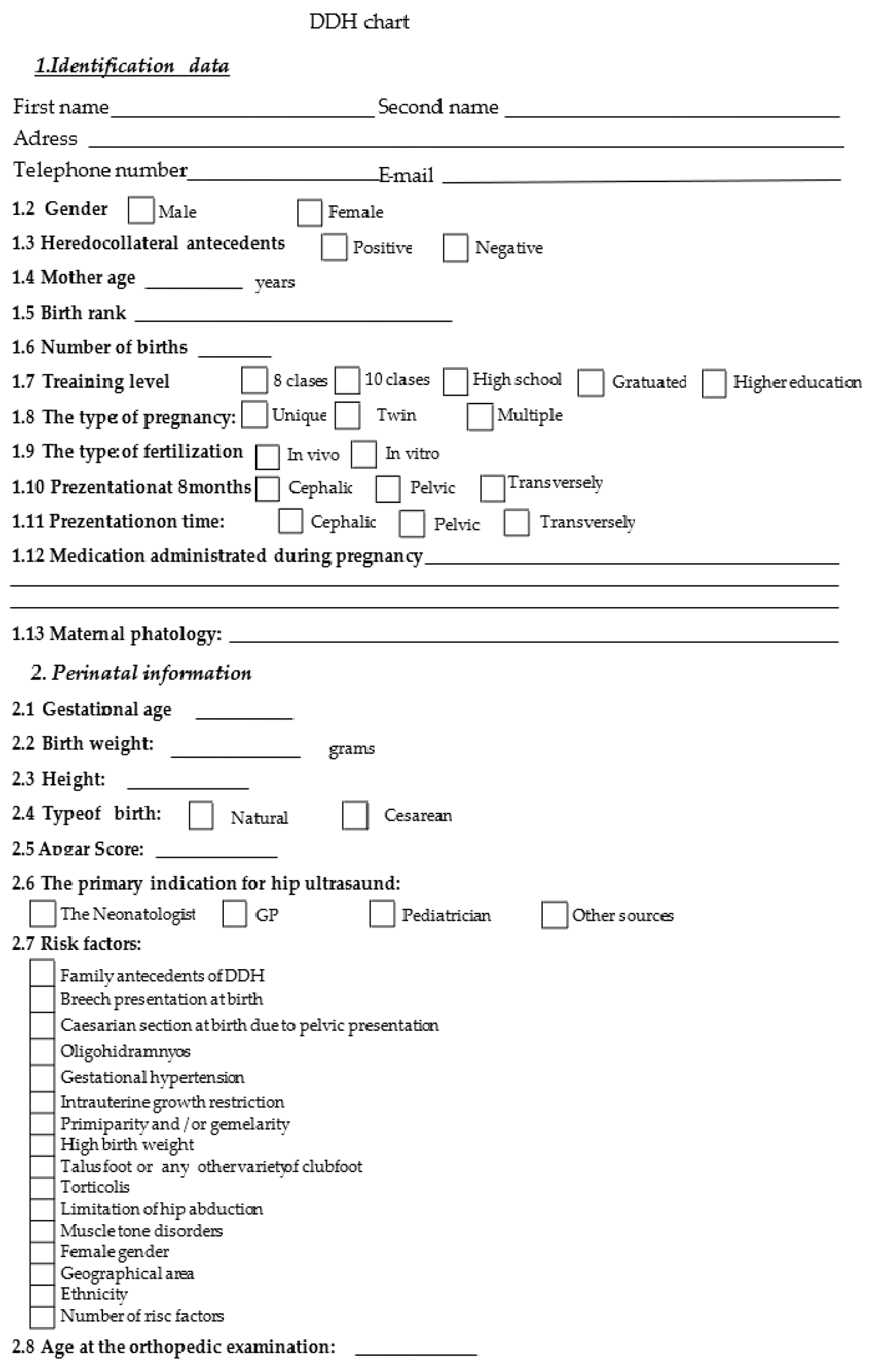
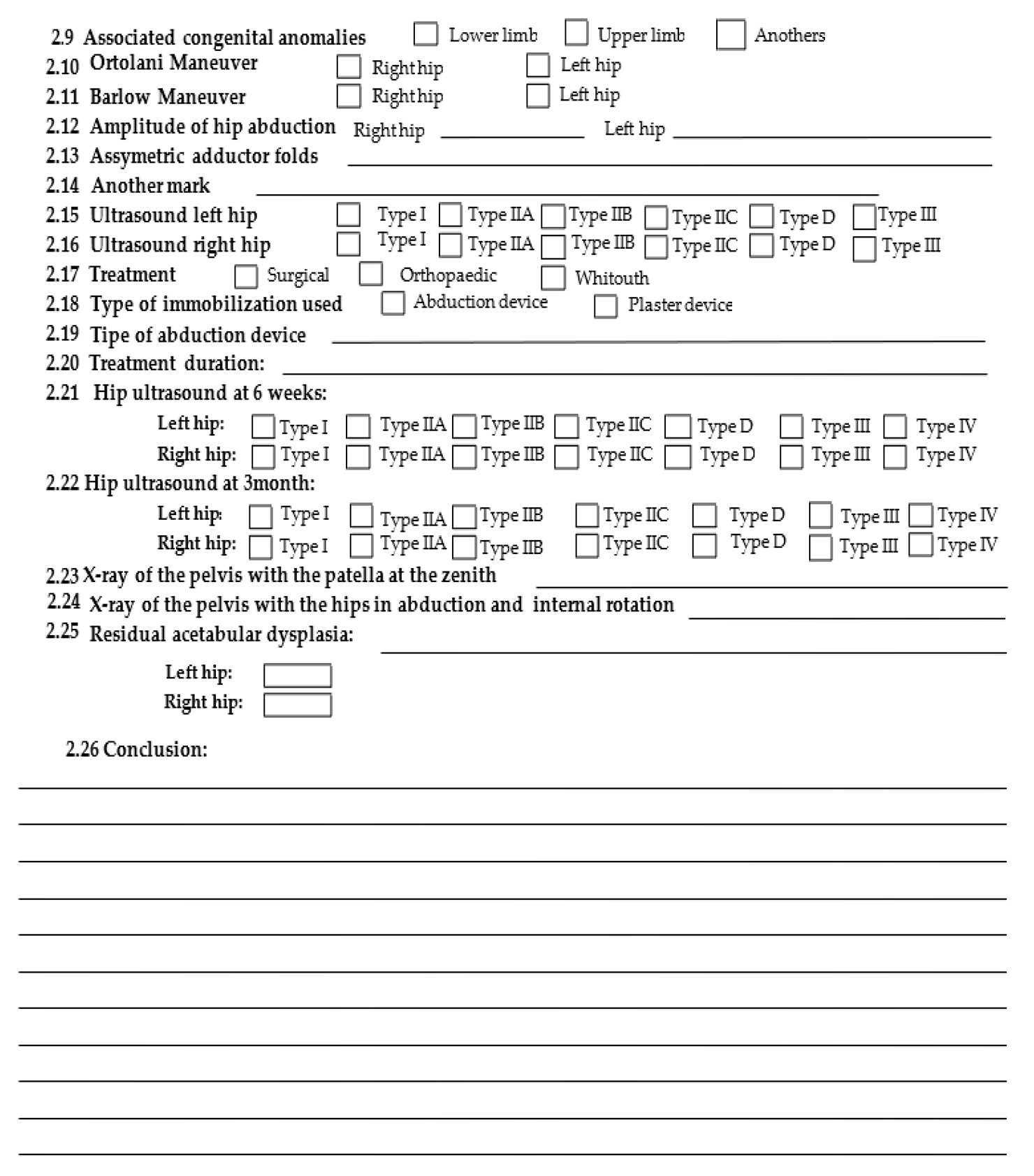
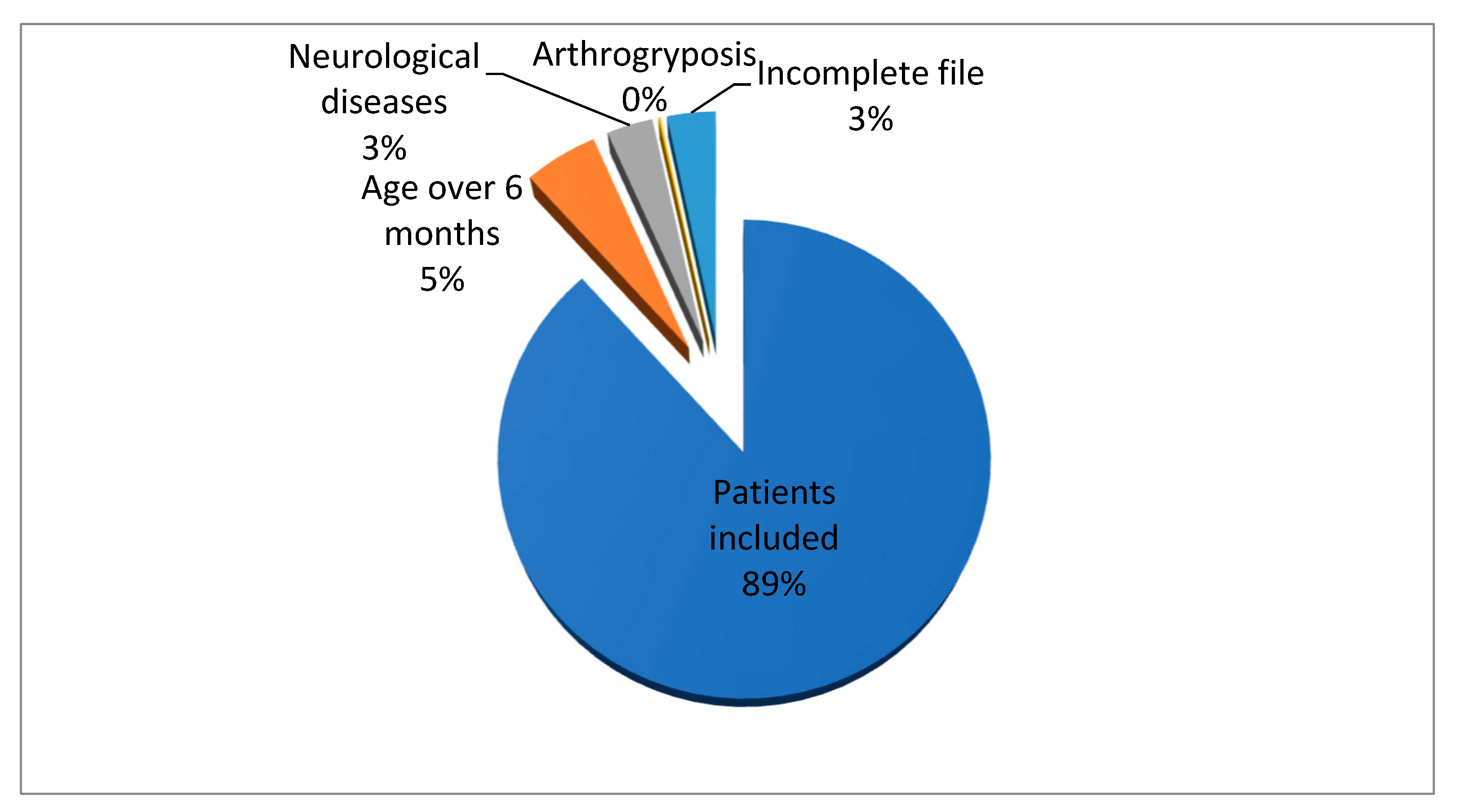
2. Materials and Methods
3. Results
4. Discussion
- 1.
- Sex—DDH represents a pathology that is more common in girls, the rate being 4/1 or 6/1 [8]. This is due to the sensitivity of the female fetus to maternal hormones (especially relaxin), which causes ligamentous laxity. It is known that the female sex is favored in the occurrence of this injury. The examined group shows a difference in the proportion of female patients diagnosed with DDH. The Chi-square test highlighted a cause–effect relationship between the female sex and the presence of DDH; the p-value is 0.00133, which is statistically significant. This statistic concludes that the female sex is associated with an increased risk of DDH and that the addressability is higher in girls. DDH etiopathogenesis and risk factors were reviewed by Harsanyi et al., who noticed that female newborns are nine times more frequently diagnosed with DDH than male newborns [11].
- 2.
- Pelvic presentation—Pelvic presentation is known to increase the risk of DDH. In a complete pelvic presentation, the thighs are flexed on the abdomen, and due to the pressure of the uterus and abdominal wall muscles, the femoral head is forced posteriorly. In addition, the permanent flexion of the thighs leads to the shortening of the iliopsoas, which is an important factor in postnatal dislocation. In the incomplete pelvic presentation, the instability of the hip increases due to the increased tension in the hamstrings due to the position of the knees in extension. Studies have shown an increased incidence in patients with pelvic presentation born vaginally (17.5%) compared to those born by cesarean section (10.3%) [9]. The statistical results of our study are consistent with the data from the literature. Hsieh, in his study [14], states that he believes that DDH is part of the complex of injuries secondary to the pelvic presentation, including torticollis and facial anomalies. This statistically proves that a patient in a pelvic presentation will have a risk of 2.337 (statistically significant) to develop DDH compared to a newborn in another type of presentation.
- 3.
- Primiparity—Due to the particulars of the primiparous pregnant woman, the first newborn has a higher incidence: lack of elasticity of the uterus, increased tonicity of the abdominal muscles, and oligohydramnios.
- 4.
- The location of the injury—DDH is more frequent on the left because the fetus is positioned with its back to the left side of the mother, and the thigh is placed on the sacrum. It is positioned in flexion and adduction, increasing the risk of dysplasia. In addition, the right hip is more exposed in the pelvic presentation [15].
- 5.
- Family history—Studies have shown that compared to dizygotic twins, monozygotic twins have a higher incidence, and positive family history for DDH increases the risk of the pathology by 10%.
- 6.
- High birth weight—A weight over 4000–4500 g increases the risk of DDH.
- 7.
- Prematurity/postmaturity—The risk of DDH seems lower in premature infants than in postmature ones, supporting the theory that DDH appears late in intrauterine life.
- 8.
- Disorders of muscle tone—The slow progression of the femoral head in the socket may result from early muscle hypertonia.
- 9.
- Congenital disorders of the foot—Studies have shown that metatarsus adductus and talus valgus foot associate in a proportion of 20% with DDH, although initially it was considered that equine varus foot was associated with DDH. In the group presented, a congenital foot disorder was represented by different entities: talus valgus foot, metatarsus adductus, and equine varus foot. Both rigid and flexible forms represent these forms. Although the number of patients with DDH and congenital foot disorders is not large, the association is statistically significant between the two pathologies is in the literature’s data. The common pathogenic substrate of the two pathologies is ligament hyperlaxity; congenital foot disorders represent its evident clinical expression, and DDH represents its hidden variant.
- 10.
- Abduction limitation—Abduction limitation represents a critical risk factor in detecting DDH. It is also a conclusive clinical sign. Still, in newborns, the limitation of abduction can be secondary to physiological muscle hypertonia. Limitation of abduction is a valuable clinical sign; it suggests, in most cases, a problem at the hip level, and unilateral limitation has increased specificity for DDH. Bilateral limitation of abduction, especially when not significant, can be erroneously interpreted by the examining physician as a deviation from normal. The statistical risk that a patient with abduction limitation will present DDH is 22.9% (CI 95% 4.51–16.19). It is a high risk from a statistical point of view.
- 11.
- Postnatal position—A still-used practice is swaddling the newborn by fixing the lower limbs in extension and adduction. However, in this position, all the conditions for developing DDH are created through maximum coxo-femoral instability and the association with ligament hyperlaxity. In 1975, according to a study in Japan, the incidence of DDH was reduced by half by avoiding swaddling the newborn with maximum knee extension and adduction.
- 12.
- Oligohydramnios—Oligohydramnios in the patients of the studied group was not present. Therefore, due to insufficient data, we consider that the analysis is statistically insignificant.
- 13.
- Twinship—Twinship is a risk factor that supports the mechanical theory of DDH occurrence. Due to the inadequate intrauterine space, twinning or multiple pregnancies were considered for a long time as an etiopathogenic factor in the occurrence of DDH, but the studies performed did not highlight a significant connection between the two elements [12,16].
- 14.
- Geographical area and ethnicity—International studies have highlighted an increased incidence of DDH in Caucasians from Eastern Europe, so we can conclude that our country is in an endemic area for DDH.
- 15.
- Torticollis—Torticollis is associated with DDH in 15% of cases.
- It must be performed by the same medical staff;
- It congests the outpatient service;
- It can delay diagnosis and treatment.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DDH | Developmental dysplasia of the hip |
| N.M.D. | Neurological motor disorders |
| H.B.W. | High birth weight |
References
- Bjorlykke, J.; Reigstad, H.; Indrekvam, K.; Lehmann, T.; Engesaer, I.; Engesaer, L.; Rosendahl, K. Selective ultrasound screening for developmental hip dysplasia: Effect on management and late detected cases. A prospective survey during 1991–2006. Pediatr. Radiol. 2014, 44, 410–424. [Google Scholar]
- Finne, P.H.; Dalen, I.; Ikonomou, N.; Ulimoen, G.; Hansen, T.W.R. Diagnosis of congenital hip dysplasia in the newborn. Acta Orthop. 2008, 79, 313–320. [Google Scholar] [CrossRef]
- Thallinger, C.; Pospischill, P.; Ganger, R.; Radler, C.; Krall, C.; Grill, F. Long-term results of a nationwide general ultrasound screening system for developmental disorders of the hip: The Austrian hip screening program. J. Child. Orthop. 2014, 8, 3–10. [Google Scholar] [CrossRef]
- Roposch, A.; Protopapa, E.; Malaga-Shaw, O.; Gelfer, Y.; Humphries, P.; Ridout, D.; Wedge, J.H. Predicting developmental dysplasia of the hip in at-risk newborns. BMC Musculoskelet. Disord. 2020, 21, 442. [Google Scholar] [CrossRef] [PubMed]
- Koşar, P.; Ergun, E.; Yiğit, H.; Gökharman, F.D.; Kosar, U. Developmental dysplasia in male infants: Risk factors, instability and ultrasound screening. Hip Int. 2011, 21, 409–414. [Google Scholar] [CrossRef]
- Chan, A.; McCaul, K.A.; Cundy, P.J.; Haan, E.A.; Byron-Scott, R. Perinatal risk factors for developmental dysplasia of the hip. Arch. Dis. Childhood Fetal Neonatal Ed. 1997, 76, F94–F100. [Google Scholar] [CrossRef] [PubMed]
- Gharedaghi, M.; Mohammadzadeh, A.; Zandi, B. Comparison of Clinical and Sonographic Prevalence of Developmental. Acta Med. Iran. 2011, 49, 25–27. [Google Scholar] [PubMed]
- Dunn, P.M. Perinatal Observations on the Etiology of Congenital Dislocation of the Hip. Clin. Orthop. Relat. Res. 1976, 119, 11–22. [Google Scholar] [CrossRef]
- Vereanu, D. Chirurgie Infantila si Ortopedie-Urgente; Medicala: Bucuresti, Romania, 1973. [Google Scholar]
- Gotia, D. Patologia Ortopedica a Soldului la Copil; Gr. T. Popa, UMF: Iasi, Romania, 2005. [Google Scholar]
- Harsanyi, S.; Zamborsky, R.; Krajciova, L.; Kokavec, M.; Danisovic, L. Developmental Dysplasia of the Hip: A Review of Etiopathogenesis, Risk Factors, and Genetic Aspects. Medicina 2020, 56, 153. [Google Scholar] [CrossRef]
- Castelein, R.M.; Sauter, A.J.M. Ultrasound screening for congenital dysplasia of the hip in newborns is valuable. J. Pediatr. Orthop. 1988, 8, 666–670. [Google Scholar] [CrossRef]
- Gulati, V.; Eseonu, K.; Sayani, J.; Ismail, N.; Uzoigwe, C.; Choudhury, M.Z.; Gulati, P.; Aqil, A.; Tibrewal, S. Developmental dysplasia of the hip in the newborn: A systematic review. World J. Orthop. 2013, 4, 32–41. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, S.M.; Huang, S.C. Treatment of developmental dysplasia of the hip after failed open reduction. J. Formos. Med. Assoc. 1998, 97, 763–769. [Google Scholar] [PubMed]
- Pakula, L.; Weinblatt, H.; Young, D. Early Detection of Developmental Dysplasia of the hip. Pediatrics 2000, 105, 896–905. [Google Scholar]
- Bergo, K.; Rosendahl, K. Parent satisfaction with early and delayed abduction splinting therapy of developmental hip dysplasia. Acta Paediatr. 2013, 102, e339–e343. [Google Scholar] [CrossRef] [PubMed]
- Czeizel, A.; Szentpétery, J.; Tusnády, G.; Vizkelety, T. Two family studies on congenital dislocation of the hip after early orthopaedic screening Hungary. J. Med. Genet. 1975, 12, 125–130. [Google Scholar] [CrossRef]
- Moličnik, A.; Janša, J.; Kocjančič, B.; Kralj-Iglič, V.; Dolinar, D. Secondary hip dysplasia increases risk for early coxarthritis after Legg-Calve-Perthes disease. A study of 255 hips. Comput. Methods Biomech. Biomed. Eng. 2019, 22, 1107–1115. [Google Scholar] [CrossRef]
- Feldman, G.J.; Parvizi, J.; Levenstien, M.; Scott, K.; Erickson, J.A.; Fortina, P.; Devoto, M.; Peters, C.L. Developmental Dysplasia of the Hip: Linkage Mapping and Whole Exome Sequencing Identify a Shared Variant in CX 3 CR 1 in All Affected Members of a Large Multigeneration Family. J. Bone Miner. Res. 2013, 28, 2540–2549. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, A.; Mortada, E.; Alqahtani, S.; Alkathri, H.; Alsayyed, R.; Abualait, T.; Alwhaibi, R. Developmental dysplasia of the hip and associated risk factors in Saudi children: A retrospective study. J. Back Musculoskelet. Rehabil. 2021, 34, 573–580. [Google Scholar] [CrossRef]
- Aronsson, D.D.; Goldberg, M.J.; Kling, T.F.; Roy, D.R. Developmental dysplasia of the hip. Pediatrics 1994, 94, 201–208. [Google Scholar] [CrossRef]
- Pollet, V.; Percy, V.; Prior, H.J. Relative Risk and Incidence for Developmental Dysplasia of the Hip. J. Pediatr. 2017, 181, 202–207. [Google Scholar] [CrossRef]
- Panagiotopoulou, N.; Bitar, K.; Hart, W.J. The association between mode of delivery and developmental dysplasia of the hip in breech infants: A systematic review of 9 cohort studies. Acta Orthop. Belg. 2012, 78, 697–702. [Google Scholar] [PubMed]
- Woodacre, T.; Ball, T.; Cox, P. Epidemiology of developmental dysplasia of the hip within the U.K.: Refining the risk factors. J. Child. Orthop. 2016, 10, 633–642. [Google Scholar]
- Rabin, D.L.; Barnett, C.R.; Arnold, W.D.; Freiberger, R.H.; Brooks, G. Untreated congenital hip disease: A study of the epidemiology, natural history, and social aspects of the disease in a Navajo population. Am. J. Public Health Nations Health 1965, 55, i3–i44. [Google Scholar] [CrossRef]
- Stevenson, D.A.; Mineau, G.; Kerber, R.A.; Viskochil, D.H.; Schaefer, C.; Roach, J.W. Familial Predisposition to Developmental Dysplasia of the Hip. J. Pediatr. Orthop. 2009, 29, 463–466. [Google Scholar] [CrossRef] [PubMed]
- Van Gijzen, A.F.M.; Rouers, E.D.M.; van Douveren, F.Q.M.P.; Dieleman, J.; Hendriks, J.G.E.; Halbertsma, F.J.J.; Bok, L.A. Developmental dysplasia of the hip in children with Down syndrome: Comparison of clinical and radiological examinations in a local cohort. Eur. J. Pediatr. 2019, 178, 559–564. [Google Scholar] [CrossRef]
- Jang, S.-A.; Cho, Y.-H.; Byun, Y.-S.; Jeong, D.-G.; Han, I.-H.; Kim, M.-G. Unusual Cause of Hip Pain: Intrusion of the Acetabular Labrum. Hip Pelvis 2015, 27, 49–52. [Google Scholar] [CrossRef]
- Kural, B.; Karapınar, E.D.; Yılmazbaş, P.; Eren, T.; Gökçay, G. Risk Factor Assessment and a Ten-Year Experience of DDH Screening in a Well-Child Population. Biomed. Res. Int. 2019, 2019, 7213681. [Google Scholar] [CrossRef]
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Age ≤ 6 months | Age ≥ 6 months |
| First presentation | Arthrogryposis |
| Complete DDH chart | Incomplete DDH chart |
| Neurological disorders |
| Risk Factors | p | Chi |
|---|---|---|
| Sex | 0.0133 | 19.31 |
| Pelvic presentation | 0.0224 | 17.85 |
| Primiparity | 0.1153 | 12.90 |
| Location of injury | 0.9925 | 1.51 |
| Family history | 0.5759 | 6.64 |
| High birth weight | 0.6394 | 6.07 |
| Prematurity/Postmaturity | 0.9434 | 2.85 |
| Disorders of muscle tone | 0.8471 | 4.11 |
| Congenital disorders of the foot | 0.0004 | 28.53 |
| Limitation of hip abduction | 0.0042 | 22.4 |
| Postnatal position | 0.9512 | 2.72 |
| Oligohydramnios | 0.9434 | 2.85 |
| Twinship | 0.1646 | 11.71 |
| Torticollis | 0.9584 | 2.57 |
| Geographical area and ethnicity | 0.9246 | 3.15 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Candussi, I.-L.; Ene, D.; Bușilă, C.; Mihailov, R.; Sârbu, I.; Lungu, C.N.; Ciongradi, C.I. The Influence of Risk Factors in the Early Detection of Developmental Dysplasia of the Hip in a Country with Limited Material Resources. Healthcare 2023, 11, 2416. https://doi.org/10.3390/healthcare11172416
Candussi I-L, Ene D, Bușilă C, Mihailov R, Sârbu I, Lungu CN, Ciongradi CI. The Influence of Risk Factors in the Early Detection of Developmental Dysplasia of the Hip in a Country with Limited Material Resources. Healthcare. 2023; 11(17):2416. https://doi.org/10.3390/healthcare11172416
Chicago/Turabian StyleCandussi, Iuliana-Laura, Daniela Ene, Camelia Bușilă, Raul Mihailov, Ioan Sârbu, Claudiu N. Lungu, and Carmen Iulia Ciongradi. 2023. "The Influence of Risk Factors in the Early Detection of Developmental Dysplasia of the Hip in a Country with Limited Material Resources" Healthcare 11, no. 17: 2416. https://doi.org/10.3390/healthcare11172416
APA StyleCandussi, I.-L., Ene, D., Bușilă, C., Mihailov, R., Sârbu, I., Lungu, C. N., & Ciongradi, C. I. (2023). The Influence of Risk Factors in the Early Detection of Developmental Dysplasia of the Hip in a Country with Limited Material Resources. Healthcare, 11(17), 2416. https://doi.org/10.3390/healthcare11172416







