Abstract
This study investigated whether differences in survival rates and clinical outcomes exist in patients undergoing TKA by insurance type: National Health Insurance (NHI) vs. Medical Aid Program (MAP). This study conducted a retrospective analysis of 762 TKAs (NHI, n = 505; MAP, n = 257) with a mean follow-up of 8.4 ± 1.8 years. Patient-reported outcomes (PROMs) were evaluated using the American Knee Society’s (AKS) score at the final follow-up. The survival rate of each group was analyzed using Kaplan–Meier survival analysis. Any postoperative complications and readmissions within 90 days of discharge were recorded and compared between the groups. There were no between-group differences in pre- to postoperative improvement in AKS scores. The estimated 10-year survival rates were 98.5% in the NHI group and 96.9% in the MAP group, respectively, with no significant differences (p = 0.48). However, the length of hospital stay (LOS) was significantly longer in the MAP group than in the NHI group (13.4 days vs. 13.1 days, p = 0.03), and the transfer rate to other departments was significantly higher in the MAP group than in the NHI group (3.9% vs. 1.4%, p = 0.04). Readmission rates for orthopedic complications for 90 days were 3.0% in the NHI group and 3.5% in the MAP group, respectively (p = 0.67). Patients’ insurance type showed similar survival rates and clinical outcomes to those of primary TKA at a mean follow-up of 8.4 years, but the LOS and rate of transfer to other departments during hospitalization were influenced by insurance type.
1. Introduction
Total knee arthroplasty (TKA) is a well-established treatment to reduce pain and enhance function among individuals suffering from end-stage arthritis [1]. Although TKA utilization has increased exponentially worldwide over the last two decades, socioeconomic status (SES) has been an important factor leading to varied effects on the treatment timing, type of treatment, and patient health status, thereby contributing to persistent disparities in utilization [2,3,4,5]. Health insurance coverage, which is determined by employment status and financial resources, is an effective indicator of SES [6] and can affect the outcomes after TKA. Few studies have examined the correlation between patient insurance type and clinical outcomes after TKA [7,8]. Studies indicate that Medicaid patients undergoing TKA often experience extended lengths of stay, higher likelihoods of discharge to rehabilitation facilities, and increased readmissions within 90 days [9,10]. Additionally, the Medicaid population encounters higher risks of inpatient mortality and postoperative complications, leading to poorer postoperative outcomes [8,11,12]. However, these studies included patients who underwent TKA over a short follow-up period at multiple centers [7,8,9,10,11,12]. Moreover, there is a paucity of literature on the impact of health insurance coverage on implant survival. As such, we investigate whether differences in implant survivorship and clinical outcomes exist in patients who received TKA performed at a single institution when stratified by insurance type. We answer three questions: (1) Does health insurance type influence patient-reported outcomes (PROMs)? (2) Does health insurance type influence implant survival? And (3) Do orthopedic/medical complications differ depending on insurance type?
2. Materials and Methods
2.1. Health Insurance Coverage
The National Health Insurance (NHI) and Medical Aid Program (MAP) are the two major healthcare systems in South Korea [13]. The NHI requires individuals to pay insurance premiums for healthcare coverage. The MAP provides low-cost or free healthcare services to economically disadvantaged individuals. Both systems ensure access to healthcare but differ in terms of funding and eligibility criteria [14,15]. The NHI ensures a wide range of healthcare services, including general medical care, preventive vaccinations, dental treatments, traditional medicine, hospitalization, and surgery. Most healthcare services are covered by insurance, and patients bear some of the costs themselves. MAP provides basic medical services and various forms of social support, such as specific disease treatments, medication subsidies, and assistive devices for disabilities.
2.2. Study Design and Patients
We conducted a retrospective collection of clinical data from consecutive patients who received TKA at our institute from November 2011 to December 2018. Inclusion criteria were as follows: patients (1) with symptomatic progressed primary osteoarthritis (Kellgren–Lawrence grade ≥ III) [16] and (2) who received unilateral TKA using a cemented posterior-stabilized type. The exclusion criteria were patients with loss of complete medical records and those who were followed up for less than 5 years. Patients with significant comorbidities, including severe pulmonary disorders, coagulation abnormalities, or a history of venous thromboembolism, were excluded. To minimize bias, patients with a second knee in staged bilateral TKA, secondary osteoarthritis (OA), or stem/block fixation for primary TKA were excluded from this study. Finally, 762 knees were assigned to either the NHI group (n = 505) or the MAP group (n = 257) (Figure 1). The study protocol received approval from our institutional review board (SMC 2022-01-009).
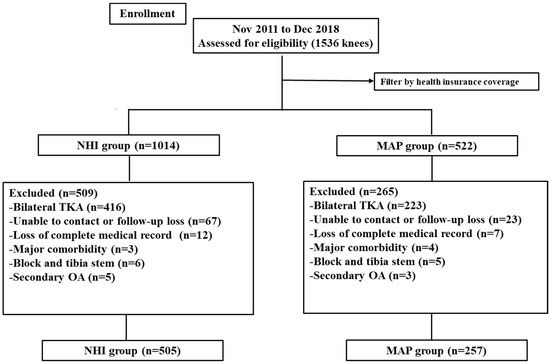
Figure 1.
Flow diagram showing the number of knees that met the study criteria. NHI, National Health Insurance; MAP, Medical Aid Program.
2.3. Surgical Methods and Postoperative Management
All surgical procedures were executed by a single surgeon (SJS) within the confines of one institution, and each patient received care in adherence to the same protocol. A pneumatic tourniquet was utilized during the operation and deflated after the surgical procedure ended. The surgical procedure was performed using the modified gap balance technique [17]. A medial parapatellar arthrotomy was used through the use of a midline incision. Following the meticulous removal of osteophytes from both the femur and tibia, an intramedullary alignment rod was employed to establish the angle for the distal femur cut, with the aim of a valgus alignment between 5° and 6°. A standard extramedullary jig was used on the proximal tibia to ensure a cut perpendicular to the tibial axis. Rotation of the femoral component was determined based on an assessment of the balanced flexion gap. Femoral size was measured using an anterior reference system to ensure procedural consistency and accuracy. A suction drain was subsequently inserted into the knee joint and unclamped upon placement. Following surgery, all patients were fitted with compressive elastic stockings for four weeks postoperatively to prevent deep vein thrombosis (DVT). Prophylactic antithrombotic treatment was not used due to potential drug-induced bleeding complications. Postoperative rehabilitation commenced on day 1, including bedside continuous passive mobilization, range of motion (ROM) exercise, calf-pump exercises, and straight leg raising. The suction drain was removed 72 h postoperatively, and patients were encouraged to ambulate based on their tolerance level.
2.4. Clinical Evaluations and Survival Rate
Clinical assessment utilized the American Knee Society (AKS) score [18]. Subsequent follow-up assessments were scheduled at the outpatient department at intervals of 6 weeks, 3 months, 6 months, and 1 year post-surgery. Clinical and radiographic evaluations were conducted at each visit. Postoperative complications and readmissions within 90 days after discharge were recorded separately for medical and orthopedic reasons and then compared between the groups. Moreover, the number of patients transferred to other departments during hospitalization for medical reasons was recorded. Occurrences of wound dehiscence, stiffness, and hemarthrosis were documented. Hemarthrosis was assessed by evaluating the patellar circumference. Acute postoperative periprosthetic joint infection (PJI) diagnosis adhered to the criteria based on the International consensus meeting in 2018 [19]. Stiffness was characterized by a flexion limitation of around 95°, hindering the patient’s ability to engage in various activities. Symptoms indicating potential pulmonary embolism, such as shortness of breath, blood-streaked sputum, or chest pain, were assessed during computed tomography (CT) for pulmonary thromboembolism (PTE) CT. Implant survival rates over a 10-year period were also evaluated. The primary endpoint was revision TKA for implant-related complications or infections. Failure attributed to infection was defined as septic failure, while failure due to other causes was defined as aseptic failure.
2.5. Statistical Analysis
The normality of variables was assessed using the Kolmogorov–Smirnov test, while comparison of continuous data utilized an independent samples t-test. Categorical data were compared using either Chi-squared or Fisher’s exact tests. Kaplan–Meier survival analysis was employed to estimate the 10-year survival rate for each group, with survival curves compared using a log-rank test. Statistical significance was defined as a two-sided p-value below 0.05. All statistical analyses were conducted using SPSS software version 23 (IBM Corp, Armonk, NY, USA), and continuous data were presented as mean ± standard deviation.
3. Results
A total of 762 patients (505 with NHI and 257 with MAP) with a mean age of 72.8 ± 6.6 years and follow-up of 8.4 ± 1.8 years were included in this study. Patient demographic characteristics are summarized in Table 1. There were no significant demographic differences between the groups, except for the length of hospital stay (LOS). The LOS was significantly longer in the MAP group than in the NHI group (13.4 days vs. 13.1 days, p = 0.03). The prosthetic components are listed in Table 2.

Table 1.
Patients’ demographic characteristics.

Table 2.
The types of prosthetic components used.
When we compared the preoperative AKS scores between the two groups, the MAP group (knee, 25.1 ± 12.1; function, 23.5 ± 11.9) had significantly lower scores than the NHI group (knee, 31.9 ± 12.5; function, 29.8 ± 11.6, p = 0.001). However, the degree of improvement in the postoperative AKS knee and function scores compared to the preoperative values was similar between the groups. The degree of improvement in the range of motion (ROM) was also no different between the groups (Table 3).

Table 3.
Clinical outcomes between the groups.
Survival rates at the 10-year follow-up were 98.5% and 96.9% for the NHI and MAP groups, respectively. The survival rates for septic failure were also calculated. In the septic failure group, the 10-year survival rates were 99.2% and 98.7% in the NHI and MAP groups, respectively. A log-rank test was performed to analyze the differences in survival curves between the groups, and no statistically significant differences were found (p = 0.48 for total failure; p = 0.79 for septic failure) (Figure 2).
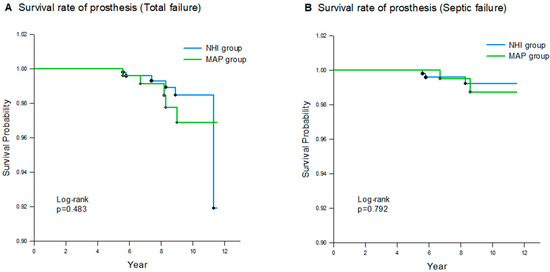
Figure 2.
Kaplan–Meier analysis of cumulative survival for all-cause failure of NHI group and MAP group: (A) failure due to all complications; (B) septic failure (due to infection).
There were no significant differences in orthopedic complications and 90-day readmission between the groups (Table 4). The 90-day readmission for orthopedic complications appeared in 24 knees: 15 in the NHI group and 9 in the MAP group (p = 0.67). Similarly, there were no significant differences in medical complications and 90-day readmission between the two groups (Table 5). The 90-day readmission for medical complications appeared in fourteen knees: seven in the NHI group and seven in the MAP group (p = 0.25). However, the rate of transfer to other departments during hospitalization was significantly higher in the MAP group than in the NHI group (3.9% vs. 1.4%, p = 0.04).

Table 4.
Comparison of orthopedic complication between the groups.

Table 5.
Comparison of medical complications between the groups.
4. Discussion
The main finding was that health insurance coverage showed similar survival rates and clinical outcomes of primary TKA at a mean follow-up of 8.4 years, while LOS and the rate of transfer to other departments during hospitalization were influenced by health insurance coverage. Considering the varied impacts of SES on patient status, it is noteworthy that the rates of prosthesis survival, improvement of patient-reported outcome measures (PROMs), and occurrences of orthopedic complications are similar among patients with different insurance types. Although further research is necessary to establish a causal relationship, these findings deserve careful consideration by arthroplasty surgeons counseling patients with MAP.
Based on the theoretical advantages of TKA, we hypothesized that comparable results, similar to those observed in individuals with NHI, could be achieved in individuals with MAP. However, Martin et al. [20] conducted a retrospective review of 293 consecutive patients who underwent total joint arthroplasty, stratifying them based on their insurance type. Medicaid coverage, similar to MAP, was a significant predictor of lower preoperative and postoperative PROMs [21]. Hinman and Bozic retrospectively reviewed 224 patients undergoing total hip arthroplasty and reported lower preoperative and postoperative Harris hip scores in Medicaid-covered patients than in non-Medicaid-covered patients [22]. These findings are thus consistent with those of previous studies. Our findings showed that postoperative AKS scores were significantly lower in the MAP group compared to the NHI group at the latest follow-up. Additionally, preoperative AKS scores were also significantly lower in the MAP group, which seems reasonable considering that MAP patients are likely less educated, engage in physically demanding situations, live alone, smoke tobacco, have poor hygiene, and have a lower baseline, as measured by PROM. Therefore, the difference in postoperative AKS scores between the two groups could be attributed to the initial difference in the preoperative AKS scores between the groups. Furthermore, there were no significant differences observed between the two groups regarding the postoperative improvement in the AKS scores compared to their preoperative values. Thus, when using PROMs to evaluate the value of care, preoperative to postoperative changes serve as more reliable indicators of surgical success than absolute values, especially in patients with MAP [23].
Although several studies have examined the relationship between socioeconomic factors and outcomes for TKA [2,3,4], few studies evaluated the influence of socioeconomic factors such as insurance payer type on TKA survival. Many studies have investigated the survivorship of primary TKA at 10 years and found survival rates of 92–98% [24,25,26]. Our study showed that the survival rates at the 10-year follow-up were 98.5% and 96.9% for the NHI and MAP groups, respectively. The higher survival rates in this study can be attributed to the fact that the literature on survivorship of primary TKA mainly comprises studies conducted from the late 2000s to the early 2010s [24,25,26], which reported comparatively lower survival rates than current studies. Moreover, surgical techniques and component designs have evolved in recent years, with a focus on improving function and outcomes after TKA [27,28]. We also confirmed that there was no statistically significant difference in the 10-year survival rates between the two groups. We believe that these results are due to the characteristics of public healthcare hospitals, where MAP patients tend to have longer hospital stays and there is an effective multidisciplinary approach within the healthcare system for the treatment of MAP patients [29].
There was no significant difference in orthopedic complications between the two groups during the midterm follow-up. Similarly, there were no differences in medical complications between the groups during hospitalization. However, the transfer rate to other departments during hospitalization was significantly higher in the MAP group. These factors contributed to the extended LOS for the MAP group. Moreover, in the case of the NHI group, additional private insurance is often purchased, and the hospitalization period may vary depending on the support of the terms and conditions of the purchased private insurance. However, for the MAP group, it may be easy to extend the hospitalization period within the support amount because the MAP group receives a fixed amount and there are many systems or assistance for receiving additional support. An extended LOS may enable a multidisciplinary team to plan a patient-tailored rehabilitation path and better allocate resources to maximize recovery [29,30]. Skura et al. [31] reported that the LOS following total joint arthroplasty was influenced by insurance type. Similarly, in this study, the LOS was affected by insurance type. The authors believe that the individuals in the MAP group, who are socially disadvantaged, undergo basic examinations before surgery but are more likely to have underlying conditions than those in the NHI group [14,15]. These patients are at higher risk of perioperative complications, leading to a higher rate of transfer to other departments [32].
Our study is not without limitations. First, this was a retrospective study with a relatively small number of patients in the MAP group. Considering that the qualifications for MAP are strict, it would be difficult to proceed with such a large number of cases prospectively. Since this study is a study on mid-term follow-up, further research may be necessary to study long-term follow-up in the future. Further, our study was conducted by a single surgeon, and we used a posterior-stabilized knee design for all patients, who adhered to the same rehabilitation protocols at a single institute. Second, several implants were used, but there was no statistical significance between implant use. Moreover, although we used different implants, all implants are widely used and proven without differences in the market. Therefore, bias in the results was likely minimal.
5. Conclusions
We should cautiously consider the fact that the patients’ insurance type showed similar survival rates and clinical outcomes to those of primary TKA at a mean follow-up of 8.4 years, but the LOS and the rate of transfer to other departments during hospitalization were influenced by the patients’ insurance type.
Author Contributions
Conceptualization, J.-S.S.; validation, J.-K.B.; investigation, S.Y.C.; writing—original draft, J.-K.B.; writing—review and editing, J.-K.B., S.-K.S., H.-G.R. and K.J.K.; visualization, S.Y.C.; supervision, S.-K.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Seoul Medical Center Institutional Review Board (SMC 2022-01-009, approval date 26 January 2022).
Informed Consent Statement
Not applicable.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors on request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Gill, G.S.; Joshi, A.B.; Mills, D.M. Total Condylar Knee Arthroplasty: 16- to 21-Year Results. Clin. Orthop. Relat. Res. 1999, 367, 210–215. [Google Scholar] [CrossRef]
- Suleiman, L.I.; Manista, G.C.; Sherman, A.E.; Adhia, A.H.; Karas, V.; Sporer, S.M.; Levine, B.R. The impact of race and socioeconomic status on total joint arthroplasty care. J. Arthroplast. 2021, 36, 2729–2733. [Google Scholar] [CrossRef] [PubMed]
- Martsolf, G.R.; Barrett, M.L.; Weiss, A.J.; Kandrack, R.; Washington, R.; Steiner, C.A.; Mehrotra, A.; SooHoo, N.F.; Coffey, R. Impact of race/ethnicity and socioeconomic status on risk-adjusted hospital readmission rates following hip and knee arthroplasty. JBJS 2016, 98, 1385–1391. [Google Scholar] [CrossRef] [PubMed]
- Barrack, R.L.; Ruh, E.L.; Chen, J.; Lombardi, A.V.; Berend, K.R.; Parvizi, J.; Della Valle, C.J.; Hamilton, W.G.; Nunley, R.M. Impact of socioeconomic factors on outcome of total knee arthroplasty. Clin. Orthop. Relat. Res. 2014, 472, 86–97. [Google Scholar] [CrossRef] [PubMed]
- Davis, E.T.; Lingard, E.A.; Schemitsch, E.H.; Waddell, J.P. Effects of socioeconomic status on patients’ outcome after total knee arthroplasty. Int. J. Qual. Health Care 2008, 20, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Penson, D.F.; Stoddard, M.L.; Pasta, D.J.; Lubeck, D.P.; Flanders, S.C.; Litwin, M.S. The association between socioeconomic status, health insurance coverage, and quality of life in men with prostate cancer. J. Clin. Epidemiol. 2001, 54, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Veltre, D.R.; Yi, P.H.; Sing, D.C.; Curry, E.J.; Endo, A.; Smith, E.L.; Li, X. Insurance status affects in-hospital complication rates after total knee arthroplasty. Orthopedics 2018, 41, e340–e347. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, B.D.; Hulst, J.B.; Moric, M.; Levine, B.R.; Sporer, S.M. The effect of payer type on clinical outcomes in total knee arthroplasty. J. Arthroplast. 2014, 29, 295–298. [Google Scholar] [CrossRef] [PubMed]
- Stone, M.L.; LaPar, D.J.; Mulloy, D.P.; Rasmussen, S.K.; Kane, B.J.; McGahren, E.D.; Rodgers, B.M. Primary payer status is significantly associated with postoperative mortality, morbidity, and hospital resource utilization in pediatric surgical patients within the United States. J. Pediatr. Surg. 2013, 48, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Inneh, I.A. The combined influence of sociodemographic, preoperative comorbid and intraoperative factors on longer length of stay after elective primary total knee arthroplasty. J. Arthroplast. 2015, 30, 1883–1886. [Google Scholar] [CrossRef] [PubMed]
- Browne, J.A.; Novicoff, W.M.; D’Apuzzo, M.R. Medicaid payer status is associated with in-hospital morbidity and resource utilization following primary total joint arthroplasty. JBJS 2014, 96, e180. [Google Scholar] [CrossRef] [PubMed]
- Courtney, P.M.; Huddleston, J.I.; Iorio, R.; Markel, D.C. Socioeconomic risk adjustment models for reimbursement are necessary in primary total joint arthroplasty. J. Arthroplast. 2017, 32, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-H.; Lee, K.-S.; Yoo, K.-B.; Park, E.-C. The differences in health care utilization between Medical Aid and health insurance: A longitudinal study using propensity score matching. PLoS ONE 2015, 10, e0119939. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.W.; Jang, J.; Choi, D.-W.; Jang, S.-I.; Park, E.-C. The effect of shifting medical coverage from National Health Insurance to Medical Aid type I and type II on health care utilization and out-of-pocket spending in South Korea. BMC Health Serv. Res. 2020, 20, 979. [Google Scholar] [CrossRef]
- Sohn, M.; Jung, M. Effects of public and private health insurance on medical service utilization in the National Health Insurance System: National panel study in the Republic of Korea. BMC Health Serv. Res. 2016, 16, 503. [Google Scholar] [CrossRef] [PubMed]
- Braun, H.J.; Gold, G.E. Diagnosis of osteoarthritis: Imaging. Bone 2012, 51, 278–288. [Google Scholar] [CrossRef] [PubMed]
- Daines, B.K.; Dennis, D.A. Gap balancing vs. measured resection technique in total knee arthroplasty. Clin. Orthop. Surg. 2014, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Liow, R.Y.; Walker, K.; Wajid, M.A.; Bedi, G.; Lennox, C.M. The reliability of the American Knee Society score. Acta Orthop. Scand. 2000, 71, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, J.; Tan, T.L.; Goswami, K.; Higuera, C.; Della Valle, C.; Chen, A.F.; Shohat, N. The 2018 definition of periprosthetic hip and knee infection: An evidence-based and validated criteria. J. Arthroplast. 2018, 33, 1309–1314.e2. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.T.; Callaghan, J.J.; Liu, S.S.; Gao, Y.; Warth, L.C.; Johnston, R.C. Disparity in total joint arthroplasty patient comorbidities, demographics, and postoperative outcomes based on insurance payer type. J. Arthroplast. 2012, 27, 1761–1765.e1. [Google Scholar] [CrossRef] [PubMed]
- D’Apuzzo, M.R.; Villa, J.M.; Alcerro, J.C.; Rossi, M.D.; Lavernia, C.J. Total joint arthroplasty: A granular analysis of outcomes in the economically disadvantaged patient. J. Arthroplast. 2016, 31, 41–44. [Google Scholar] [CrossRef] [PubMed]
- Hinman, A.; Bozic, K.J. Impact of payer type on resource utilization, outcomes and access to care in total hip arthroplasty. J. Arthroplast. 2008, 23, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Halawi, M.J.; Cote, M.P.; Savoy, L.; Williams, V.J.; Lieberman, J.R. The effect of payer type on patient-reported outcomes in total joint arthroplasty is modulated by baseline patient characteristics. J. Arthroplast. 2019, 34, 1072–1075. [Google Scholar] [CrossRef]
- Argenson, J.-N.; Boisgard, S.; Parratte, S.; Descamps, S.; Bercovy, M.; Bonnevialle, P.; Briard, J.-L.; Brilhault, J.; Chouteau, J.; Nizard, R. Survival analysis of total knee arthroplasty at a minimum 10 years’ follow-up: A multicenter French nationwide study including 846 cases. Orthop. Traumatol. Surg. Res. 2013, 99, 385–390. [Google Scholar] [CrossRef]
- Nakamura, S.; Kobayashi, M.; Ito, H.; Nakamura, K.; Ueo, T.; Nakamura, T. The Bi-Surface total knee arthroplasty: Minimum 10-year follow-up study. Knee 2010, 17, 274–278. [Google Scholar] [CrossRef] [PubMed]
- Vogt, J.-C.; Saarbach, C. LCS mobile-bearing total knee replacement. A 10-year’s follow-up study. Orthop. Traumatol. Surg. Res. 2009, 95, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Dall’Oca, C.; Ricci, M.; Vecchini, E.; Giannini, N.; Lamberti, D.; Tromponi, C.; Magnan, B. Evolution of TKA design. Acta Bio Medica Atenei Parm. 2017, 88, 17–31. [Google Scholar]
- Begum, F.A.; Kayani, B.; Magan, A.A.; Chang, J.S.; Haddad, F.S. Current concepts in total knee arthroplasty: Mechanical, kinematic, anatomical, and functional alignment. Bone Jt. Open 2021, 2, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Tornese, D.; Robustelli, A.; Ricci, G.; Rancoita, P.M.V.; Maffulli, N.; Peretti, G.M. Predictors of postoperative hospital length of stay after total knee arthroplasty. Singap. Med. J. 2024, 65, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Mathijssen, N.M.; Verburg, H.; van Leeuwen, C.C.; Molenaar, T.L.; Hannink, G. Factors influencing length of hospital stay after primary total knee arthroplasty in a fast-track setting. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2692–2696. [Google Scholar] [CrossRef]
- Skura, B.W.; Goubeaux, C.; Passias, B.J.; Schuette, H.B.; Melaragno, A.J.; Glazier, M.T.; Faherty, M.; Burgette, W. Increased length of stay following total joint arthroplasty based on insurance type. Arch. Orthop. Trauma Surg. 2023, 143, 2273–2281. [Google Scholar] [CrossRef] [PubMed]
- Bahk, J.; Kang, H.-Y.; Khang, Y.-H. Age-and cause-specific contributions to the life expectancy gap between Medical Aid recipients and National Health Insurance beneficiaries in Korea, 2008–2017. PLoS ONE 2020, 15, e0241755. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).