Translucent Zirconia in Fixed Prosthodontics—An Integrative Overview
Abstract
:1. Introduction
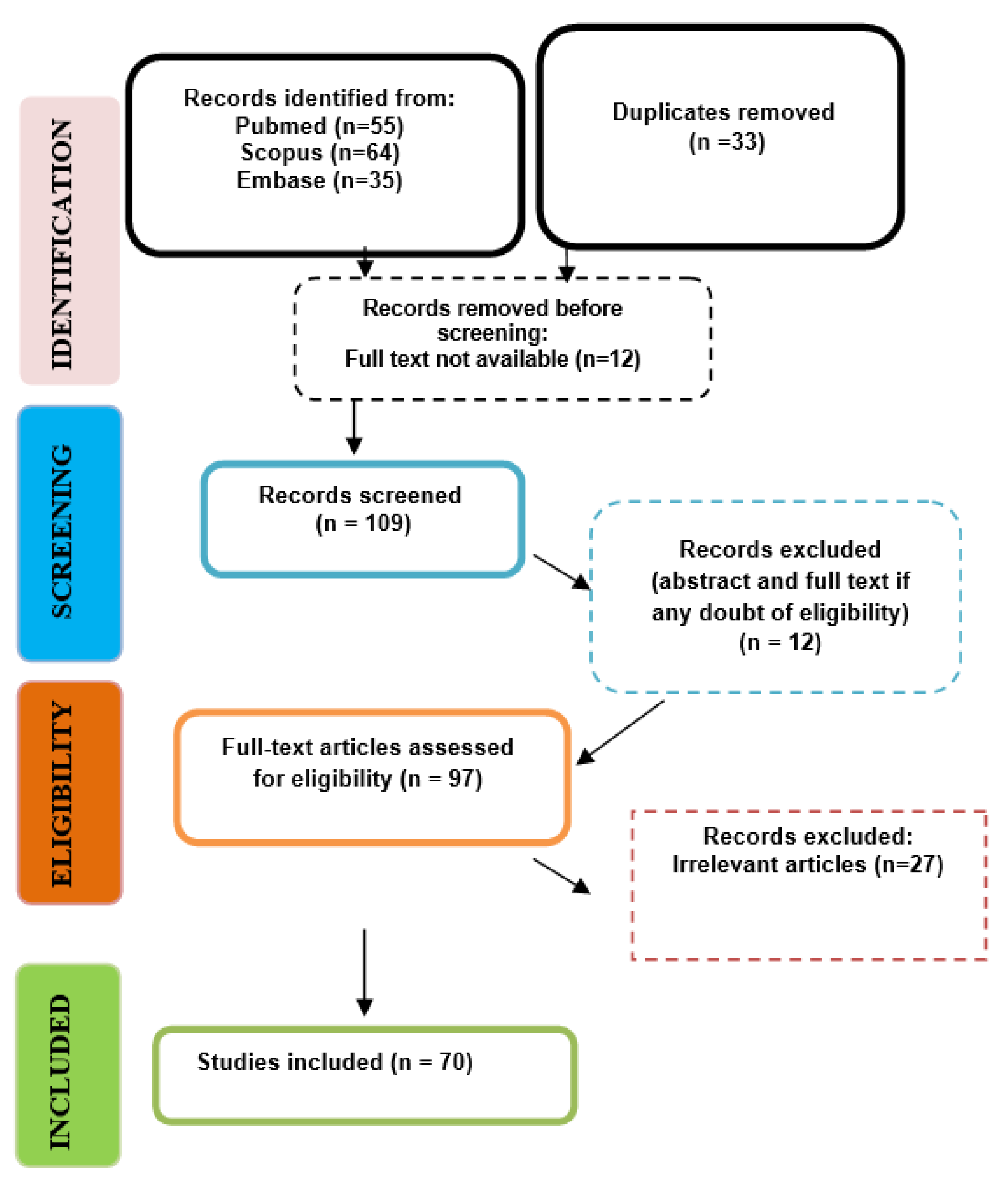
2. Materials and Methods
2.1. Information Sources and Search Strategy
2.2. Eligibility Criteria
- Randomized controlled trials, cohort studies, case reports, case–control studies—studies involving patients who have undergone fixed prosthodontic treatments using translucent zirconia.
- In vitro studies that specifically examined translucent zirconia in fixed prosthodontics; in vitro studies using human teeth or relevant analogs.
- Review articles and meta-analyses that provide comprehensive overviews or evaluations on the topic.
- Studies specifically discussing ultra-translucent/translucent or highly translucent zirconia.
- Articles focusing on different types of prosthetic restorations or which evaluated outcomes, such as mechanical strength, aesthetic outcomes, adhesion properties, clinical success rates, longevity, and wear resistance.
- Studies published in English, completed between 2008 and 2023.
- Studies involving the use of traditional or non-translucent zirconia without comparison or relevance to translucent variants
- Studies performed on animal subjects only unless they could provide essential and not otherwise available data regarding the use of translucent zirconia.
- Studies involving the use of hybrid zirconia blocks, multilayered blocks or different types of veneered translucent zirconia specimens.
- Studies that do not report any of the key outcomes of interest for the review.
- Articles published in languages other than English.
2.3. Data Extraction and Method of Analysis
2.4. Scoring Systems Used for Paper Evaluation
3. Results
3.1. Data Collection
3.2. Description of the Studies and Analysis
4. Discussion
4.1. Esthetic Properties of Translucent Zirconia
4.2. Mechanical Properties of Translucent Zirconia
4.2.1. Fracture Load, Flexural Strength and Other Mechanical Properties
4.2.2. Surface Treatments
4.2.3. Regular or Speed Sintering
4.2.4. Other Mechanical Features
4.3. Adhesion Features of Translucent Zirconia
4.4. Translucent Zirconia Used for Implant-Supported Restorations
4.5. Advancements, Applications, and Evaluations of Zirconia-Based Materials in Fixed Prosthodontics
4.6. Limitations of Our Study
5. Conclusions
- Clinical implications of the data gathered in this overview should help clinicians choose the most suitable type of high translucent zirconia for their specific case, considering esthetic and mechanical properties, but also adhesion on the specific situation to be dealt with.
- Our research emphasizes the complex nature of translucent zirconia’s aesthetic properties. While it holds promise for high translucency and color adaptability, clinicians and technicians must navigate its nuances and limitations to optimize restorative outcomes. Translucent zirconia presents complex aesthetic properties with the potential for high translucency and color adaptability.
- Future studies could benefit from a standardized approach to evaluating aesthetic properties, ensuring more consistent results and reliable guidance for clinical application.
- Despite challenges, translucent zirconia, with its evolving enhancements in esthetic and mechanical properties, stands as a versatile material in restorative and implant dentistry.
- Ongoing research and technological advancements might contribute to refining the properties of translucent zirconia, expanding its clinical applications.
- A thorough understanding of its behavior in clinical conditions, meticulous material selection, and adherence to recommended fabrication and treatment protocols are crucial for optimizing the performance and aesthetic outcomes of translucent zirconia.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| PSZ | Partially stabilized zirconia (mixture of cubic and tetragonal phase) |
| TZP | Tetragonal zirconia polycrystal (almost 100% tetragonal phase) |
| 3Y-TZP | TZP stabilized with 3-mol% yttria |
| Ce-TZP | TZP stabilized with ceria |
| ATZ | Alumina-toughened zirconia |
| ZTA | Zirconia-toughened alumina |
| NanoZR | Ce-TZP/Al2O3 nanocomposite |
| 3Y-HA | Conventional TZP stabilized with 3-mol% yttria and added with a relatively high content of alumina (0.25–0.5 wt%) |
| 3Y | High translucent TZP stabilized with 3-mol% yttria and added with a relatively low content of alumina (less than 0.05 wt%) |
| 4Y | High strength PSZ stabilized with 4-mol% yttria and added with a relatively low content of alumina (less than 0.05 wt%) |
| 5Y | High translucent PSZ stabilized with 5-mol% yttria and added with a relatively low content of alumina (less than 0.05 wt%) |
| 6Y | Super high translucent PSZ stabilized with 6-mol% yttria and added with a relatively low content of alumina (less than 0.05 wt%) |
References
- Reda, R.; Zanza, A.; Cicconetti, A.; Bhandi, S.; Guarnieri, R.; Testarelli, L.; Di Nardo, D. A Systematic Review of Cementation Techniques to Minimize Cement Excess in Cement-Retained Implant Restorations. Methods Protoc. 2022, 5, 9. [Google Scholar] [CrossRef] [PubMed]
- Wassell, R.; Nohl, F.; Steele, J.; Walls, A. Extra-Coronal Restorations: Concepts and Clinical Application, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2019; Available online: http://www.springer.com/series/15753 (accessed on 10 October 2023).
- Bartlett, D.; Ricketts, D. Advanced Operative Dentistry. In Conventional Bridges; Churchill Livingstone: London, UK, 2011; pp. 239–251. [Google Scholar] [CrossRef]
- Ispas, A.; Iosif, L.; Popa, D.; Negucioiu, M.; Constantiniuc, M.; Bacali, C.; Buduru, S. Comparative Assessment of the Functional Parameters for Metal-Ceramic and All-Ceramic Teeth Restorations in Prosthetic Dentistry—A Literature Review. Biology 2022, 11, 556. [Google Scholar] [CrossRef]
- Guess, P.; Schultheis, S.; Bonfante, E.; Coelho, P.; Ferencz, J.; Silva, N. All-ceramic systems: Laboratory and clinical performance. Dent. Clin. N. Am. 2011, 55, 333–352. [Google Scholar] [CrossRef] [PubMed]
- Monaco, C.; Rosentritt, M.; Llukacej, A.; Baldissara, P.; Scotti, R. Marginal adaptation, gap width, and fracture strength of teeth restored with different all-ceramic vs metal ceramic crown systems: An in vitro study. Eur. J. Prosthodont. Restor. Dent. 2016, 24, 130–137. [Google Scholar] [PubMed]
- Pjetursson, B.E.; Valente, N.A.; Strasding, M.; Zwahlen, M.; Liu, S.; Sailer, I. A Systematic Review of the Survival and Complication Rates of Zirconia-Ceramic and Metal-Ceramic Single Crowns. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 199–214. [Google Scholar] [CrossRef]
- Miura, S.; Yamauchi, S.; Kasahara, S.; Katsuda, Y.; Fujisawa, M.; Egusa, H. Clinical evaluation of monolithic zirconia crowns: A failure analysis of clinically obtained cases from a 3.5-year study. J. Prosthodont. Res. 2020, 65, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Kelly, J.R. Dental Ceramics for Restoration and Metal Veneering. Dent. Clin. N. Am. 2017, 61, 797–819. [Google Scholar] [CrossRef] [PubMed]
- Rosentritt, M.; Hahnel, S.; Engelhardt, F.; Behr, M.; Preis, V. In vitro performance and fracture resistance of CAD/CAM-fabricated implant supported molar crowns. Clin. Oral Investig. 2017, 21, 1213–1219. [Google Scholar] [CrossRef] [PubMed]
- Malament, K.A.; Natto, Z.S.; Thompson, V.; Rekow, D.; Eckert, S.; Weber, H.-P. Ten-Year Survival of Pressed, Acid-Etched e.Max Lithium Disilicate Monolithic and Bilayered Complete-Coverage Restorations: Performance and Outcomes as a Function of Tooth Position and Age. J. Prosthet. Dent. 2019, 121, 782–790. [Google Scholar] [CrossRef] [PubMed]
- Pahncke, E.; Hahnel, S.; Schierz, O.; Schmidt, M.B.; Schmutzler, A.; Rauch, A. Two-Year Longevity of Posterior Zirconia Multi-Unit Fixed Dental Prostheses with Monolithic Occlusal Surface. Appl. Sci. 2021, 11, 4449. [Google Scholar] [CrossRef]
- Jang, Y.-S.; Noh, H.-R.; Lee, M.-H.; Lim, M.-J.; Bae, T.-S. Effect of Lithium Disilicate Reinforced Liner Treatment on Bond and Fracture Strengths of Bilayered Zirconia All-Ceramic Crown. Materials 2018, 11, 77. [Google Scholar] [CrossRef] [PubMed]
- Saravi, B.; Vollmer, A.; Hartmann, M.; Lang, G.; Kohal, R.-J.; Boeker, M.; Patzelt, S.B.M. Clinical Performance of CAD/CAM All-Ceramic Tooth-Supported Fixed Dental Prostheses: A Systematic Review and Meta-Analysis. Materials 2021, 14, 2672. [Google Scholar] [CrossRef] [PubMed]
- Cooper, L.F.; Stanford, C.; Feine, J.; McGuire, M. Prospective assessment of CAD/CAM zirconia abutment and lithium disilicate crown restorations: 2.4 year results. J. Prosthet. Dent. 2016, 116, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Baldi, A.; Comba, A.; Michelotto Tempesta, R.; Carossa, M.; Pereira, G.K.R.; Valandro, L.F.; Paolone, G.; Vichi, A.; Goracci, C.; Scotti, N. External Marginal Gap Variation and Residual Fracture Resistance of Composite and Lithium-Silicate CAD/CAM Overlays after Cyclic Fatigue over Endodontically-Treated Molars. Polymers 2021, 13, 3002. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.R.; Benetti, P. Ceramic materials in dentistry: Historical evolution and current practice. Aust. Dent. J. 2011, 56 (Suppl. S1), 84–96. [Google Scholar] [CrossRef]
- Helvey, G. Classification of dental ceramics. Inside Dent. 2013, 13, 62–76. [Google Scholar]
- Gracis, S.; Thompson, V.P.; Ferencz, J.L.; Silva, N.R.; Bonfante, E.A. A new classification system for all-ceramic and ceramic-like restorative materials. Int. J. Prosthodont. 2015, 28, 227–235. [Google Scholar] [CrossRef] [PubMed]
- Piconi, C.; Maccauro, G. Zirconia as a ceramic biomaterial. Biomaterials 1999, 20, 1–25. [Google Scholar] [CrossRef]
- Chevalier, J. What future for zirconia as a biomaterial? Biomaterials 2006, 27, 535–543. [Google Scholar] [CrossRef]
- Ban, S. Classification and Properties of Dental Zirconia as Implant Fixtures and Superstructures. Materials 2021, 14, 4879. [Google Scholar] [CrossRef] [PubMed]
- Ban, S. Properties of zirconia for realization of all-ceramic restoration. Shika Gakuho 2007, 107, 670–684. [Google Scholar]
- Miyazaki, T.; Nakamura, T.; Matsumura, H.; Ban, S.; Kobayashi, T. Current status of zirconia restoration. J. Prosthodont. Res. 2013, 57, 236–261. [Google Scholar] [CrossRef] [PubMed]
- Chandranaik, M.B.; Thippanna, R.K. Fixed Partial Denture Failures: A Clinical Survey for Evaluation of the Factors Responsible. CODS J. Dent. 2017, 9, 41–45. [Google Scholar] [CrossRef]
- Tan, K.; Pjetursson, B.E.; Lang, N.P.; Chan, E.S.Y. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. Clin. Oral Implant. Res. 2004, 15, 654–666. [Google Scholar] [CrossRef] [PubMed]
- Dewan, H.; Haroon, T.M.; Mogla, S.; Gupta, A.; Loganathan, J.; Ahammed, A.N.; Kommuri, S. Assessment of Failure Rate of Fixed Partial Dentures: A Clinical Study. J. Pharm. Bioallied Sci. 2022, 14, S262–S263. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Zorzela, L.; Loke, Y.K.; Ioannidis, J.P.; Golder, S.; Santaguida, P.; Altman, D.G.; Moher, D.; Vohra, S.; PRISMA Harms Group. PRISMA harms checklist: Improving harms reporting in systematic reviews. BMJ 2016, 352, i157. [Google Scholar] [CrossRef] [PubMed]
- Hong, Q.N.; Pluye, P.; Fàbregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Mixed Methods Appraisal Tool (MMAT), Version 2018; Registration of Copyright (#1148552); Canadian Intellectual Property Office, Industry Canada: Gatineau, QC, Canada, 2018. [Google Scholar]
- Oermann, M.H.; Knafl, K.A. Strategies for completing a successful integrative review. Nurse Author Ed. 2021, 31, 65–68. [Google Scholar] [CrossRef]
- Alraheam, I.A.; Donovan, T.E.; Rodgers, B.; Boushell, L.; Sulaiman, T.A. Effect of masticatory simulation on the translucency of different types of dental zirconia. J. Prosthet. Dent. 2019, 122, 404–409. [Google Scholar] [CrossRef]
- Kanout, C. Evaluation of the Translucency Properties for CAD/CAM Full Ceramic Crowns Fabricated from Glass Ceramics (E.max) or High Translucency Zirconia (Lava Plus): A Clinical Study. Cureus 2023, 15, e34935. [Google Scholar] [CrossRef]
- Park, J.H.; Bang, H.J.; Choi, N.H.; Park, E.J. Translucency and masking ability of translucent zirconia; comparison with conventional zirconia and lithium disilicate. J. Adv. Prosthodont. 2022, 14, 324–333. [Google Scholar] [CrossRef]
- Cho, Y.E.; Lim, Y.J.; Han, J.S.; Yeo, I.S.L.; Yoon, H.I. Effect of yttria content on the translucency and masking ability of yttria-stabilized tetragonal zirconia polycrystal. Materials 2020, 13, 4726. [Google Scholar] [CrossRef] [PubMed]
- Mourouzis, P.; Tolidis, K. Effects of milling method and artificial ageing on optical properties of high translucent zirconia for chairside restorations. Dent. Mater. 2021, 38, 108–120. [Google Scholar] [CrossRef]
- Sasany, R.; Ergun-Kunt, G.; Yilmaz, B. Effect of mouth rinses on optical properties of CAD-CAM materials used for laminate veneers and crowns. J. Esthet. Restor. Dent. 2021, 33, 648–653. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.F.; Takahashi, H.; Iwasaki, N.; Peng, P.W. Effect of thickness of externally characterized stains on optical properties of high-translucency zirconia. Clin. Oral Investig. 2022, 27, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Dal Piva, A.M.O.; Tribst, J.P.M.; Werner, A.; Anami, L.C.; Bottino, M.A.; Kleverlaan, C.J. Three-body wear effect on different CAD/CAM ceramics staining durability: Staining durability after wear. J. Mech. Behav. Biomed. Mater. 2019, 103, 103579. [Google Scholar] [CrossRef]
- Miura, S.; Tsukada, S.; Fujita, T.; Isogai, T.; Teshigawara, D.; Saito-Murakami, K.; Asami, K.; Fujisawa, M. Effects of abutment tooth and luting agent colors on final color of high-translucent zirconia crowns. J. Prosthodont. Res. 2022, 66, 243–249. [Google Scholar] [CrossRef]
- Zhang, F.; Reveron, H.; Spies, B.C.; van Meerbeek, B.; Chevalier, J. Trade-off between fracture resistance and translucency of zirconia and lithium-disilicate glass ceramics for monolithic restorations. Acta Biomater. 2019, 91, 24–34. [Google Scholar] [CrossRef]
- Lee, W.F.; Iwasaki, N.; Peng, P.W.; Takahashi, H. Effect of toothbrushing on the optical properties and surface roughness of extrinsically stained high-translucency zirconia. Clin. Oral Investig. 2022, 26, 3041–3048. [Google Scholar] [CrossRef]
- Auzani, M.L.; Dapieve, K.S.; Zucuni, C.P.; Rocha Pereira, G.K.; Valandro, L.F. Influence of shading technique on mechanical fatigue performance and optical properties of a 4Y-TZP ceramic for monolithic restorations. J. Mech. Behav. Biomed. Mater. 2020, 102, 103457. [Google Scholar] [CrossRef]
- Fouda, A.M.; Atta, O.; Özcan, M.; Stawarczyk, B.; Glaum, R.; Bourauel, C. An investigation on fatigue, fracture resistance, and color properties of aesthetic CAD/CAM monolithic ceramics. Clin. Oral Investig. 2023, 27, 2653–2665. [Google Scholar] [CrossRef]
- da Silva, A.O.; Fiorin, L.; Faria, A.C.L.; Ribeiro, R.F.; Rodrigues, R.C.S. Translucency and mechanical behavior of partially stabilized monolithic zirconia after staining, finishing procedures and artificial aging. Sci. Rep. 2022, 12, 16094. [Google Scholar] [CrossRef] [PubMed]
- Abdulmajeed, A.; Sulaiman, T.; Abdulmajeed, A.; Bencharit, S.; Närhi, T. Fracture Load of Different Zirconia Types: A Mastication Simulation Study. J. Prosthodont. 2020, 29, 787–791. [Google Scholar] [CrossRef] [PubMed]
- Alraheam, I.A.; Donovan, T.; Boushell, L.; Cook, R.; Ritter, A.V.; Sulaiman, T.A. Fracture load of two thicknesses of different zirconia types after fatiguing and thermocycling. J. Prosthet. Dent. 2020, 123, 635–640. [Google Scholar] [CrossRef] [PubMed]
- Almansour, H.M.; Alqahtani, F. The effect of in vitro aging and fatigue on the flexural strength of monolithic high-translucency zirconia restorations. J. Contemp. Dent. Pract. 2018, 19, 867–873. [Google Scholar] [CrossRef] [PubMed]
- Elsayed, A.; Meyer, G.; Wille, S.; Kern, M. Influence of the yttrium content on the fracture strength of monolithic zirconia crowns after artificial aging. Quintessence Int. 2019, 50, 344–348. [Google Scholar] [CrossRef]
- Jerman, E.; Lümkemann, N.; Eichberger, M.; Hampe, R.; Stawarczyk, B. Impact of varying step-stress protocols on the fatigue behavior of 3Y-TZP, 4Y-TZP and 5Y-TZP ceramic. Dent. Mater. 2021, 37, 1073–1082. [Google Scholar] [CrossRef] [PubMed]
- Camposilvan, E.; Leone, R.; Gremillard, L.; Sorrentino, R.; Zarone, F.; Ferrari, M.; Chevalier, J. Aging resistance, mechanical properties and translucency of different yttria-stabilized zirconia ceramics for monolithic dental crown applications. Dent. Mater. 2018, 34, 879–890. [Google Scholar] [CrossRef]
- De Araújo-Júnior, E.N.S.; Bergamo, E.T.P.; Bastos, T.M.C.; Benalcázar Jalkh, E.B.; Lopes, A.C.O.; Monteiro, K.N.; Cesar, P.F.; Tognolo, F.C.; Migliati, R.; Tanaka, R.; et al. Ultra-translucent zirconia processing and aging effect on microstructural, optical, and mechanical properties. Dent. Mater. 2022, 38, 587–600. [Google Scholar] [CrossRef] [PubMed]
- Machry, R.V.; Dapieve, K.S.; Cadore-Rodrigues, A.C.; Werner, A.; de Jager, N.; Pereira, G.K.R.; Valandro, L.F.; Kleverlaan, C.J. Mechanical characterization of a multi-layered zirconia: Flexural strength, hardness, and fracture toughness of the different layers. J. Mech. Behav. Biomed. Mater. 2022, 135, 105455. [Google Scholar] [CrossRef]
- Yan, J.; Kaizer, M.R.; Zhang, Y. Load-bearing capacity of lithium disilicate and ultra-translucent zirconias. J. Mech. Behav. Biomed. Mater. 2018, 88, 170–175. [Google Scholar] [CrossRef]
- Dimitriadis, K.; Sfkas, A.K.; Kamnis, S.; Tsolka, P.; Agathopoulos, S. Influence of heat treatment on the microstructure and the physical and mechanical properties of dental highly translucent zirconia. J. Adv. Prosthodont. 2022, 14, 96–107. [Google Scholar] [CrossRef] [PubMed]
- Sahebi, M.; Ghodsi, S.; Berahman, P.; Amini, A.; Zeighami, S. Comparison of retention and fracture load of endo-crowns made from zirconia and zirconium lithium silicate after aging: An in vitro study. BMC Oral Health 2022, 22, 41. [Google Scholar] [CrossRef]
- Xu, Y.; Han, J.; Lin, H.; An, L. Comparative study of flexural strength test methods on CAD/CAM Y-TZP dental ceramics. Regen. Biomater. 2015, 2, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Lümkemann, N.; Stawarczyk, B. Impact of hydrothermal aging on the light transmittance and flexural strength of colored yttria-stabilized zirconia materials of different formulations. J. Prosthet. Dent. 2020, 125, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Jurado, C.A.; Sayed Ahmed, A.; Lawson, N.C.; Azpiazu-Flores, F.X.; Green, C.; Cho, S. Fracture resistance of zirconia surveyed crowns with four different occlusal rest seat designs. J. Prosthodont. 2023. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.K.; Ahn, B. Effect of Al2O3 sandblasting particle size on the surface topography and residual compressive stresses of three different dental zirconia grades. Materials 2021, 14, 610. [Google Scholar] [CrossRef] [PubMed]
- Hergeröder, C.; Wille, S.; Kern, M. Comparison of Testing Designs for Flexural Strength of 3Y-TZP and 5Y-PSZ Considering Different Surface Treatment. Materials 2022, 15, 3915. [Google Scholar] [CrossRef] [PubMed]
- Wertz, M.; Schmidt, M.B.; Hoelzig, H.; Wagner, M.; Abel, B.; Kloess, G.; Hahnel, S.; Koenig, A. Rhombohedral Phase Formation in Yttria-Stabilized Zirconia Induced by Dental Technical Tools and Its Impact on Dental Applications. Materials 2022, 15, 4471. [Google Scholar] [CrossRef] [PubMed]
- Alves, L.M.M.; Rodrigues, C.d.S.; Ramos, N.d.C.; Buizastrow, J.; Campos, T.M.B.; Bottino, M.A.; Zhang, Y.; de Melo, R.M. Silica infiltration on translucent zirconia restorations: Effects on the antagonist wear and survivability. Dent. Mater. 2022, 38, 2084–2095. [Google Scholar] [CrossRef] [PubMed]
- Yan, M.; Ding, S.J.; Lin, C.W.; Wei, C.L.; Huang, Y.W.; Yang, C.C. Aging resistance of highly translucent zirconia ceramics with rapid sintering. J. Oral Sci. 2023, 65, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Jansen, J.U.; Lümkemann, N.; Letz, I.; Pfefferle, R.; Sener, B.; Stawarczyk, B. Impact of high-speed sintering on translucency, phase content, grain sizes, and flexural strength of 3Y-TZP and 4Y-TZP zirconia materials. J. Prosthet. Dent. 2019, 122, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Jerman, E.; Wiedenmann, F.; Eichberger, M.; Reichert, A.; Stawarczyk, B. Effect of high-speed sintering on the flexural strength of hydrothermal and thermo-mechanically aged zirconia materials. Dent. Mater. 2020, 36, 1144–1150. [Google Scholar] [CrossRef] [PubMed]
- Wiedenmann, F.; Pfefferle, R.; Reichert, A.; Jerman, E.; Stawarczyk, B. Impact of high-speed sintering, layer thickness and artificial aging on the fracture load and two-body wear of zirconia crowns. Dent. Mater. 2020, 36, 846–853. [Google Scholar] [CrossRef]
- Mayinger, F.; Pfefferle, R.; Reichert, A.; Stawarczyk, B. Impact of High-Speed Sintering of Three-Unit 3Y-TZP and 4Y-TZP Fixed Dental Prostheses on Fracture Load With and Without Artificial Aging. Int. J. Prosthodont. 2021, 34, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.I.; Shin, H.J.; Kwon, Y.H.; Seol, H.J. Effect of Cooling Rate on Mechanical Properties, Translucency, Opalescence, and Light Transmission Properties of Monolithic 4Y-TZP during Glazing. Materials 2022, 15, 4357. [Google Scholar] [CrossRef]
- Kim, H.K. Effect of a rapid-cooling protocol on the optical and mechanical properties of dental monolithic zirconia containing 3-5 mol% Y2O3. Materials 2020, 13, 1923. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.K.; Han, J.S.; Yoon, H.I. Evaluation of intaglio surface trueness, wear, and fracture resistance of zirconia crown under simulated mastication: A comparative analysis between subtractive and additive manufacturing. J. Adv. Prosthodont. 2022, 14, 122–132. [Google Scholar] [CrossRef]
- de Angelis, F.; Buonvivere, M.; Sorrentino, E.; Rondoni, G.D.; D’Arcangelo, C. Wear Properties of Conventional and High-Translucent Zirconia-Based Materials. Materials 2022, 15, 7324. [Google Scholar] [CrossRef]
- Liang, S.; Yuan, F.; Chen, H.; Sun, Y. Digital evaluation of the effect of nanosilica-lithium spray coating on the internal and marginal fit of high translucent zirconia crowns. J. Dent. 2023, 132, 104503. [Google Scholar] [CrossRef]
- Schönberger, J.; Erdelt, K.J.; Bäumer, D.; Beuer, F. Marginal and internal fit of posterior three-unit fixed zirconia dental prostheses fabricated with two different CAD/CAM systems and materials. Clin. Oral Investig. 2017, 21, 2629–2635. [Google Scholar] [CrossRef] [PubMed]
- de Angelis, F.; D’Arcangelo, C.; Buonvivere, M.; Rondoni, G.D.; Vadini, M. Shear bond strength of glass ionomer and resin-based cements to different types of zirconia. J. Esthet. Restor. Dent. 2020, 32, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Ruyter, E.I.; Vajeeston, N.; Knarvang, T.; Kvam, K. A novel etching technique for surface treatment of zirconia ceramics to improve adhesion of resin-based luting cements. Acta Biomater. Odontol. Scand. 2017, 3, 36–46. [Google Scholar] [CrossRef] [PubMed]
- Franco-Tabares, S.; Stenport, V.F.; Hjalmarsson, L.; Tam, L.; Johansson, C.B. Chemical Bonding to Novel Translucent Zirconias: A Mechanical and Molecular Investigation. J. Adhes. Dent. 2019, 21, 107–116. [Google Scholar] [CrossRef]
- Grangeiro, M.; Demachkia, A.M.; Rodrigues, C.S.; Inagati, C.M.; Gonçalves, N.; Tanaka, I.v.; Rossi, N.R.; Bottino, M.A. Effect of Multiple Firings on the Microshear Bond Strength Between a Translucent Zirconia and a Resin Cement. Oper. Dent. 2023, 48, 329–336. [Google Scholar] [CrossRef]
- Kim, H.J.; Ferracane, J.L.; Park, M.J.; Choi, K.K. Effect of ethyl cellulose coating as an evaluation agent against contamination on the bond strength of zirconia restorations: An in vitro study. J. Prosthet. Dent. 2022, 127, 766.e1–766.e9. [Google Scholar] [CrossRef] [PubMed]
- Nadal, L.P.O.; Ramos, N.d.C.; Tribst, J.P.M.; Anami, L.C.; de Melo, R.M.; Bottino, M.A. Interfacial Fracture Energy Between New Translucent Zirconias and a Resin Cement. J. Adhes. Dent. 2022, 24, 147–154. [Google Scholar] [CrossRef]
- Packaeser, M.G.; Aragonez, G.C.; Soares, P.M.; Borges, A.L.S.; Pereira, G.K.R.; Valandro, L.F.; Rippe, M.P. High-versus low-viscosity resin cements: Its effect on the load-bearing capacity under fatigue of a translucent zirconia. J. Mech. Behav. Biomed. Mater. 2023, 142, 105829. [Google Scholar] [CrossRef] [PubMed]
- Mehari, K.; Parke, A.S.; Gallardo, F.F.; Vandewalle, K.S. Assessing the effects of air abrasion with aluminum oxide or glass beads to zirconia on the bond strength of cement. J. Contemp. Dent. Pract. 2020, 21, 713–717. [Google Scholar] [CrossRef] [PubMed]
- Khanlar, L.N.; Takagaki, T.; Abdou, A.; Inokoshi, M.; Ikeda, M.; Takahashi, A.; Yoshihara, K.; Nagaoka, N.; Nikaido, T.; Blatz, M.B.; et al. Effect of Air-Particle Abrasion Protocol and Primer on The Topography and Bond Strength of a High-Translucent Zirconia Ceramic. J. Prosthodont. 2022, 31, 228–238. [Google Scholar] [CrossRef]
- Ågren, M.; Kou, W.; Molin Thorén, M. Bond strength of surface-treated novel high translucent zirconia to enamel. Biomater. Investig. Dent. 2019, 6, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Dong, H.; Wu, X.; Zhao, J.; Jiang, Q. Evaluation of Er:YAG laser energy transmitted through novel dental zirconia ceramics. Dent. Mater. J. 2023, 42, 669–675. [Google Scholar] [CrossRef] [PubMed]
- Birand, C.; Kurtulmus-Yilmaz, S. Evaluation of Er,Cr:YSGG laser irradiation for debonding of zirconia hybrid abutment crowns from titanium bases. Lasers Med. Sci. 2022, 37, 2675–2685. [Google Scholar] [CrossRef] [PubMed]
- Borba, M.; Okamoto, T.K.; Zou, M.; Kaizer, M.R.; Zhang, Y. Damage sensitivity of dental zirconias to simulated occlusal contact. Dent. Mater. 2021, 37, 158–167. [Google Scholar] [CrossRef]
- Alammar, A.; Blatz, M.B. The resin bond to high-translucent zirconia—A systematic review. J. Esthet. Restor. Dent. 2022, 34, 117–135. [Google Scholar] [CrossRef] [PubMed]
- Gonzaga, D.; de França, B.; Helena, M.; Morais, S.T.; das Neves, F.D.; Barbosa, G.A.S. Influence of CAD/CAM on the fit accuracy of implant-supported zirconia and cobalt-chromium fixed dental prostheses. J. Prosthet. Dent. 2015, 113, 22–28. [Google Scholar]
- Cevik, P.; Schimmel, M.; Yilmaz, B. New generation CAD-CAM materials for implant-supported definitive frameworks fabricated by using subtractive technologies. Biomed. Res. Int. 2022, 2022, 3074182. [Google Scholar] [CrossRef] [PubMed]
- Zacher, J.; Bauer, R.; Strasser, T.; Rosentritt, M. Laboratory performance and fracture resistance of CAD/CAM implant-supported tooth-coloured anterior FDPs. J. Dent. 2020, 96, 103326. [Google Scholar] [CrossRef]
- Spitznagel, F.A.; Röhrig, S.; Langner, R.; Gierthmuehlen, P.C. Failure load and fatigue behavior of monolithic translucent zirconia, picn and rapid-layer posterior single crowns on zirconia implants. Materials 2021, 14, 1990. [Google Scholar] [CrossRef]
- Südbeck, S.; Buser, R.; Reymus, M.; Hoffmann, M.; Edelhoff, D.; Stawarczyk, B. A new implant system with directly screwed supra-constructions: Impact of restoration material and artificial aging on the bending moment. Int. J. Prosthodont. 2022. [Google Scholar] [CrossRef]
- Biadsee, A.; Özcan, M.; Masarwa, L.; Haddad, M.; Al-Haj Husain, N.; Ormianer, Z. Effect of Titanium-Base Abutment Height on Optical Properties of Monolithic Anterior Zirconia Crowns. Materials 2022, 15, 7643. [Google Scholar] [CrossRef]
- Guncu, M.B.; Aktas, G.; Turkyilmaz, I.; Gavras, J.N. Performance of high-translucent zirconia CAD/CAM fixed dental prostheses using a digital workflow: A clinical study up to 6 years. J. Dent. Sci. 2023, 18, 44–49. [Google Scholar] [CrossRef]
- Ozden, Y.E.; Guncu, M.B.; Aktas, G.; Canay, S. Effect of sintering time on the marginal and internal fit of monolithic zirconia crowns containing 3–4 mol% Y2O3. BMC Oral Health 2022, 22, 493. [Google Scholar] [CrossRef] [PubMed]
- Ghodsi, S.; Jafarian, Z. A Review on Translucent Zirconia. Eur. J. Prosthodont. Restor. Dent. 2018, 26, 62–74. [Google Scholar] [CrossRef] [PubMed]
- Arellano Moncayo, A.M.; Peñate, L.; Arregui, M.; Giner-Tarrida, L.; Cedeño, R. State of the Art of Different Zirconia Materials and Their Indications According to Evidence-Based Clinical Performance: A Narrative Review. Dent. J. 2023, 11, 18. [Google Scholar] [CrossRef] [PubMed]
- Kongkiatkamon, S.; Rokaya, D.; Kengtanyakich, S.; Peampring, C. Current classification of zirconia in dentistry: An updated review. PeerJ 2023, 11, e15669. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.B.; Rosentritt, M.; Hahnel, S.; Wertz, M.; Hoelzig, H.; Kloess, G.; Koenig, A. Fracture behavior of cantilever fixed dental prostheses fabricated from different zirconia generations. Quintessence Int. 2022, 53, 414–422. [Google Scholar] [CrossRef]
- Sachs, C.; Groesser, J.; Stadelmann, M.; Schweiger, J.; Erdelt, K.; Beuer, F. Full-arch prostheses from translucent zirconia: Accuracy of fit. Dent. Mater. 2014, 30, 817–823. [Google Scholar] [CrossRef] [PubMed]
| Concept | Keywords and MeSH Terms |
|---|---|
| Translucent zirconia | “yttria stabilized tetragonal zirconi*” [Tw] OR “yttria-stabilized zirconi*” [tw] OR “yttria stabilized zirconi*” [tw] OR “YSZ” [tw] OR “high-translucent zirconi*” [tw] OR ultratranslucent zirconi* [tw] OR “5Y-TZP” [tw] OR “6Y-PSZ” [tw] |
| Prosthetic restorations | “Denture, Partial, Fixed, Resin-Bonded” [tw] OR “Denture, Partial, Fixed” [tw] OR “Crown*” [tw] OR “Dental Veneer*” [tw] |
| Digital dentistry | “Computer-Aided Design” OR “CAD-CAM” |
| Accuracy, marginal fit, esthetic outcomes, adhesion and mechanical strength | “accuracy*” [tw] OR “marginal fit” [tw] OR “esthetic outcome*” [tw] OR “adhesion” [tw] OR “mechanical strength” [tw] |
| Database | Search Terms and Combinations |
|---|---|
| PubMed | “yttria stabilized tetragonal zirconi*” [Tw] OR “yttria-stabilized zirconi*” [tw] OR “yttria stabilized zirconi*” [tw] OR “YSZ” [tw] OR “high-translucent zirconi*” [tw] OR “ultratranslucent zirconi*” [tw] OR “5Y-TZP” [tw] OR “6Y-PSZ”[tw] “Denture, Partial, Fixed, Resin-Bonded” [tw] OR “Denture, Partial, Fixed” [tw] OR “Crown*” [tw] OR “Dental Veneer*” [tw]“accuracy*”[tw] OR “marginal fit” [tw] OR “esthetic outcome*” [tw] OR “ adhesion” [tw] OR “mechanical strength” [tw] ((“yttria stabilized tetragonal zirconi*” [Tw] OR “yttria-stabilized zirconi*” [tw] OR “yttria stabilized zirconi*” [tw] OR “YSZ” [tw] OR “high-translucent zirconi*” [tw] OR ultratranslucent zirconi*[tw] OR “5Y-TZP” [tw] OR “6Y-PSZ” [tw]) AND (“Denture, Partial, Fixed, Resin-Bonded” [tw] OR “Denture, Partial, Fixed” [tw] OR “Crown*” [tw] OR “Dental Veneer*” [tw])) AND (“accuracy*” [tw] OR “marginal fit” [tw] OR “esthetic outcome*” [tw] OR “ adhesion” [tw] OR “mechanical strength” [tw]) |
| Scopus | “yttria stabilized tetragonal zirconia” OR “yttria-stabilized zirconia” OR “yttria stabilized zirconia” OR “YSZ” OR “high-translucent zirconia” OR “ultratranslucent zirconia” OR “5Y-TZP” OR “6Y-PSZ” “Denture, Partial, Fixed, Resin-Bonded” OR “Denture, Partial, Fixed” OR “Crown*” OR “Dental Veneer*” “accuracy” OR “marginal fit” OR “esthetic outcome” OR “ adhesion” OR “mechanical strength” ((“yttria stabilized tetragonal zirconia” OR “yttria-stabilized zirconi*” OR “yttria stabilized zirconia” OR “YSZ” OR “high-translucent zirconi*” OR “ultratranslucent zirconia” OR “5Y-TZP” OR “6Y-PSZ”) AND (“Denture, Partial, Fixed, Resin-Bonded” OR “Denture, Partial, Fixed” OR “Crown*” OR “Dental Veneer*”) AND (“accuracy” OR “marginal fit” OR “esthetic outcome” OR “ adhesion” OR “mechanical strength”) |
| Embase | “yttria stabilized tetragonal zirconia” OR “yttria-stabilized zirconia” OR “yttria stabilized zirconia” OR “YSZ” OR “high-translucent zirconia” OR “ultratranslucent zirconia” OR “5Y-TZP” OR “6Y-PSZ” “Denture, Partial, Fixed, Resin-Bonded” OR “Denture, Partial, Fixed” OR “Crown*” OR “Dental Veneer*” “accuracy” OR “marginal fit” OR “esthetic outcome” OR “ adhesion” OR “mechanical strength” ((“yttria stabilized tetragonal zirconia” OR “yttria-stabilized zirconi*” OR “yttria stabilized zirconia” OR “YSZ” OR “high-translucent zirconi*” OR “ultratranslucent zirconia” OR “5Y-TZP” OR “6Y-PSZ”) AND (“Denture, Partial, Fixed, Resin-Bonded” OR “Denture, Partial, Fixed” OR “Crown*” OR “Dental Veneer*”) AND (“accuracy” OR “marginal fit” OR “esthetic outcome” OR “ adhesion” OR “mechanical strength”) |
| Criteria | Sub-Criteria | Score (Points) |
|---|---|---|
| Study design and methodology (30 points) | Clear description of study design | 5 |
| Rigorous methodology and appropriate study design for the research question | 8 | |
| Adequate sample size justification | 5 | |
| Clarity in data collection and analysis methods | 7 | |
| Appropriate statistical methods | 5 | |
| Relevance to research question (20 points) | Direct alignment with the research question or objective | 8 |
| Contribution to the overall objectives of this review | 7 | |
| Results and findings (25 points) | Clear presentation of results | 7 |
| Thorough analysis of findings | 8 | |
| Relevance of results to the study’s objectives | 5 | |
| Identification of limitations and potential biases | 5 | |
| Discussion and conclusion (15 points) | Interpretation of results in the context of the study’s objectives | 6 |
| Thorough discussion of implications | 5 | |
| Sound conclusion based on the study’s findings | 4 | |
| Quality of reporting (10 points) | Clarity and completeness in reporting study details | 4 |
| Adherence to reporting guidelines and standards | 3 | |
| Transparency in describing limitations | 3 | |
| Overall contribution to this research (10 points) | Significance of the study’s findings | 4 |
| Complementary nature to other studies included | 3 | |
| Potential impact on informing future research or clinical practice | 3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kui, A.; Manziuc, M.; Petruțiu, A.; Buduru, S.; Labuneț, A.; Negucioiu, M.; Chisnoiu, A. Translucent Zirconia in Fixed Prosthodontics—An Integrative Overview. Biomedicines 2023, 11, 3116. https://doi.org/10.3390/biomedicines11123116
Kui A, Manziuc M, Petruțiu A, Buduru S, Labuneț A, Negucioiu M, Chisnoiu A. Translucent Zirconia in Fixed Prosthodontics—An Integrative Overview. Biomedicines. 2023; 11(12):3116. https://doi.org/10.3390/biomedicines11123116
Chicago/Turabian StyleKui, Andreea, Manuela Manziuc, Adrian Petruțiu, Smaranda Buduru, Anca Labuneț, Marius Negucioiu, and Andrea Chisnoiu. 2023. "Translucent Zirconia in Fixed Prosthodontics—An Integrative Overview" Biomedicines 11, no. 12: 3116. https://doi.org/10.3390/biomedicines11123116
APA StyleKui, A., Manziuc, M., Petruțiu, A., Buduru, S., Labuneț, A., Negucioiu, M., & Chisnoiu, A. (2023). Translucent Zirconia in Fixed Prosthodontics—An Integrative Overview. Biomedicines, 11(12), 3116. https://doi.org/10.3390/biomedicines11123116














