Abstract
Vitamin D is a lipo-soluble hormone well known for its effects on calcium homeostasis and bone metabolism. Recently, there has been growing interest in the extraskeletal effects of vitamin D. In particular, recent studies have highlighted how vitamin D plays a fundamental role in immunomodulation processes in the context of both innate and adaptive immunity, with consequent anti-inflammatory and anti-oxidant effect in different immune-mediated pathologies, such as systemic sclerosis, psoriasis, atopic dermatitis and rheumatoid arthritis; as well as in various pro-inflammatory processes affecting the airways, including chronic rhinosinusitis with (CRSwNP) or without (CRSsNP) nasal polyposis. We analyze the role of vitamin D in the genesis and progression of CRSwNP/sNP and its supplementation as a safe and valid therapeutic strategy capable of improving the clinical outcome of standard therapies.
1. Introduction
Over the years, several studies have confirmed that vitamin D is strongly involved in immunomodulation processes, with a consequent anti-inflammatory and anti-oxidant effect in different immune-mediated pathologies. In this context, it was highlighted that some diseases of the upper respiratory tract, such as chronic rhinosinusitis with (CRSwNP) or without (CRSsNP) nasal polyposis, recognize an immune-mediated pathogenetic mechanism, in which vitamin D seems to play a fundamental role in improving the clinical and therapeutic outcome. The aim of our review is to summarize and analyze the influence of vitamin D on the genesis and clinical progression of CRSwNP/sNP and the therapeutic potential of this hormone, in addition to current treatments in the management of this disease—for which we have collected a total of 26 articles from literature, matching the search criteria with the keywords vitamin D, chronic rhinosinusitis, nasal polyposis, and biologics.
2. Chronic Rhinosinusitis and Nasal Polyposis
Chronic rhinosinusitis (CRS) is a disease of the upper respiratory tract characterized by diffuse inflammation of the mucosa [1] with unknown etiologic and pathophysiologic aspects. Anatomic factors, fungal allergies, infectious causes, and immunological disorders have been identified as favoring factors [2]. CRS may be divided into two subtypes, with (CRSwNP) and without (CRSsNP) nasal polyposis [3]. The first is characterized as an end product of Th2 cell skewing, mediated by IL-4, IL-5, and IL-13. On the other hand, CRSsNP is typically considered a result of a Th1 inflammation via, with dominant production of IFN-γ [4]. More recently, it has been suggested that classification of CRS by endotype is defined by the predominate type of inflammatory infiltrate as either eosinophilic (eCRS) or non-eosinophilic (non-eCRS) [5].
3. Vitamin D3
Vitamin D3 (VD3) is a steroid hormone that enters the circulation through epidermal transfer or intestinal absorption. Once circulating, it is hydroxylated in the liver to form 25-hydroxyvitamin D3 (25-VD3), the largely inactive form of the vitamin. To be converted into its active form, 1,25-hydroxy VD3 (1,25-VD3), it needs a second hydroxylation step in the kidney [6]. The hydroxylation process of vitamin D3 in the liver occurs by the cytochrome P450 2R1 (CYP2R1) and cytochrome P450 27 (CYP27A1) enzymes. The active metabolite 1,25 (OH) 2D3 is hydroxylated in the kidney by the enzyme CYP27B1.
CYP27B1 is also expressed by other cell types, including immune cells, which are therefore capable of synthesizing 1,25 (OH) 2D3, which plays an important role in immunomodulation processes [7,8]. Due to its steroid nature, 1,25-VD3 is able to pass through the cell membrane by binding to its cytoplasmic receptor (VDR), expressed by several human cells, including lymphocytes and dendritic cells, suggesting that vitamin D may have pleiotropic effects [9]. However, 1,25 (OH) 2D3 acts primarily through vitamin D receptors (VDRs) [10]. VDR acts as a transcription factor in different varieties of tissues, including the intestine, liver, and adipose tissue [11,12]. VDR plays a key role in modulating the immune response as it is expressed in different types of immune cells, including CD4 + and CD8 + T cells, B cells, neutrophils, and antigen presenting cells (APC) [12,13,14,15]. Approximately one billion people worldwide suffer from vitamin D deficiency [16], as determined by serum 25 (OH) D concentrations below 30 ng/mL [17]. Dietary Reference Intakes (DRIs) for vitamin D are age-dependent: 400 IU of vitamin D/day for children < 1 year, 600 IU of vitamin D/day for people aged 1 to 70, and 800 IU of vitamin D/day for people > 70 years [18,19]. Several studies performed on VD3 have highlighted the fundamental role that it plays not only as a proskeletal agent, but also as an immunomodulator [20]. In recent years, moreover, there has been a focus on the role that vitamin D plays in the pathophysiology of chronic inflammatory respiratory disorders such as allergic rhinitis, chronic rhinosinusitis, and asthma [21,22]. In particular, allergic rhinitis has shown an imbalance in the Th1/Th2 ratio favoring Th2 [23,24]. Regarding this, it has been shown that vitamin D acts by suppressing the production of IL-12 and thus reducing the differentiation of type 1 (Th1) helper T cells in favor of greater proliferation of associated type 2 (Th2) T helper cell allergy. The proliferation of Th2 cells leads to an increase in interleukin 31 (IL-31) synthesis, an effector cytokine that plays an important role in the pathogenesis of atopic and allergic diseases [25,26]. Given these correlations, a significant correlation between vitamin D deficiency and inflammation in patients with chronic rhinosinusitis with and without nasal polyps is shown [27,28,29,30].
4. Immunological Correlation between VD3 and CRSwNP/CRSsNP
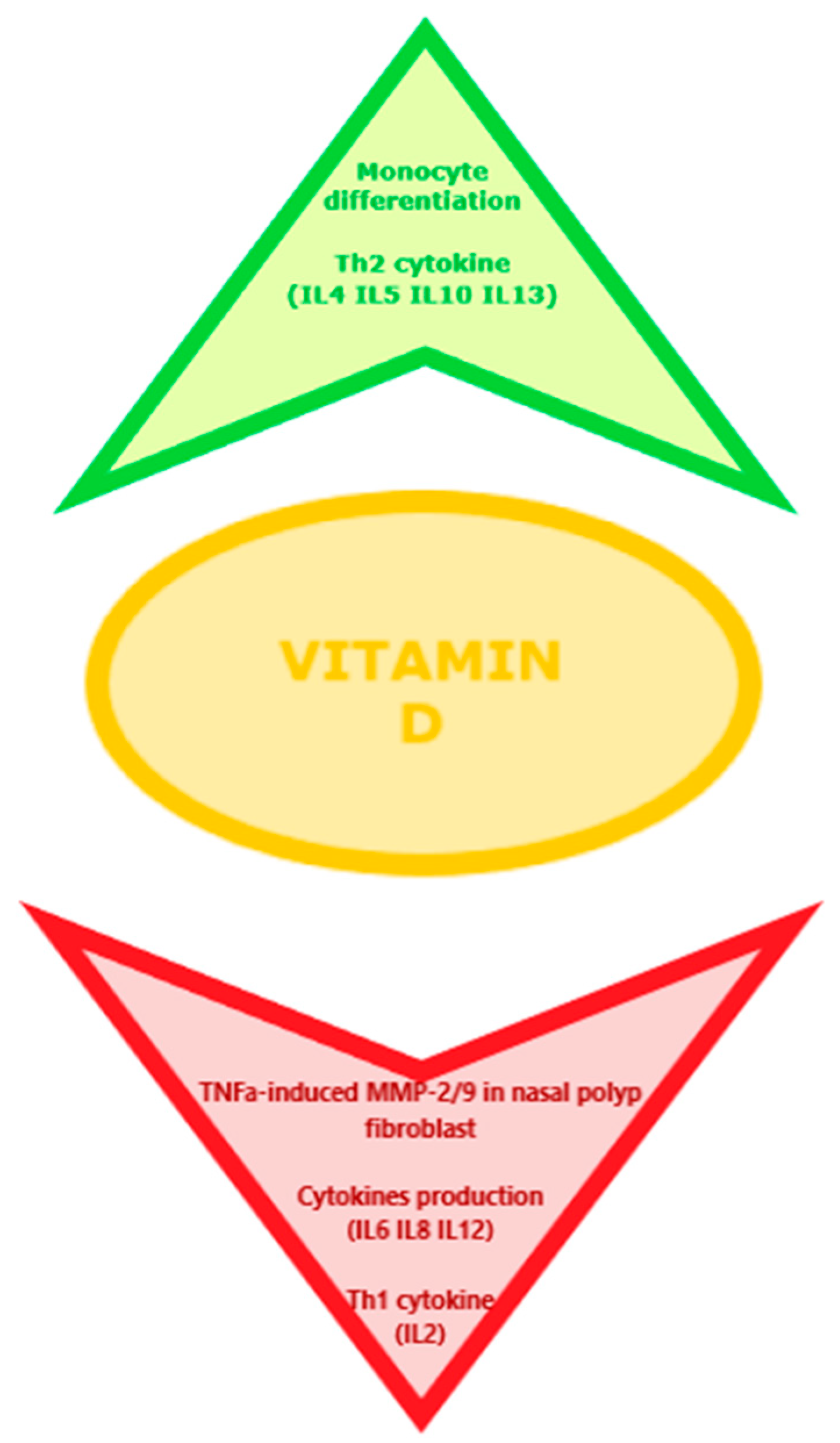
Christensen et al. [5] also reported how vitamin D is able to reduce CD4+ T-cell production of signature Th2 cytokines, such as IL-4, IL-5, and IL-13, and promotes release of IL-10, and may also modulate IL-8 expression, as 1α-hydroxylase has been shown to reduce gene expression of IL-8 in fibroblasts and keratinocyte in sinonasal tissue. According to recent studies, increased levels of IL-6 and IL-8 may participate in the pathology of primary changes as well as recurrences of chronic sinusitis and NP [31]. Furthermore, Tomaszewska et al. [32] demonstrated the presence of VDR protein expression in the sinonasal mucosa, and a statistically significant decrease in VDR nuclear staining in CRSsNP and CRSwNP patients versus controls. VDR-expressing cells believed to play a role in the pathogenesis of CRSwNP include human synonasal fibroblasts (HSNFs). These are involved in the recruitment of inflammatory cells, tissue edema, and the production and resultant of extracellular matrix (ECM) tissue remodeling [33,34]. Furthermore, vitamin D derivatives could significantly inhibit TNF-α-induced matrix metalloproteinase-2 (MMP-2) and matrix metalloproteinase-9 (MMP-9) secretion in fibroblasts involved in nasal polyp genesis [34]. Given the role that vitamin D plays in the pathogenesis of CRS and nasal polyps, low vitamin D levels could promote increased cytokine release from inflammatory cells and fibroblasts. This could be the reason for the perpetuation of chronic inflammatory sinus diseases and the degree of severity of nasal polyposis [35,36]. In fact, several studies reported a significant correlation between the serum vitamin D levels and severity of disease in patients with CRSwNP [37,38,39]. As a result, VD3 supplementation that has antiproliferative and antiinflammatory properties is suggested to be used as an adjunct therapy to decrease the incidence of inflammation and polyposis and also in reducing the recurrence of this last following endoscopic sinus surgery in patients with CRSwNP [40]. Figure 1 reports the effects of the VD on the immune pathogenesis of CRS and nasal polyposis.
Figure 1.
Effects of the VD on the immune pathogenesis of CRS and nasal polyposis.
Based on what has been discussed, vitamin D is known to act on both innate (through inhibitory effects on Toll-like receptors) and adaptive immunity (through inhibitory effects on cytokines secretion resulting in inhibition of T-cell proliferation). In addition to its cellular effects, vitamin D is capable of modulating a great variety of pro-inflammatory cytokines, thus playing a key role in the pathogenesis of many allergic disorders [41,42,43] such as asthma, atopic dermatitis, and food allergies [43,44,45,46]. Particularly in allergic diseases, vitamin D acts on the human immune system through inhibitory functions on the growth cycle of human dendritic cells and the functions of T cells, stimulating the secretion of specific cytokines such as IL-10 [47,48]. It has been widely discussed how patients diagnosed with allergic disease are characterized by below normal levels of vitamin D and how this hormonal deficiency leads to a greater severity of symptoms [49,50,51]. In fact, the metabolite of vitamin D 1,25 (OH) 2VD3 can act by inhibiting T-helper 1 (TH1) and stimulating the responses of TH2 cells. It also stimulates the differentiation of TH17 cells, resulting in upregulation of regulatory T cells (TReg) and type 1 regulatory T cells (TR1). However, 1,25 (OH) 2VD3 also inhibits the proliferation of B lymphocytes and their differentiation into antibody-secreting cells [52]. Considering these anti-inflammatory and immunomodulatory effects of vitamin D, several studies have focused on the correlation between the deficiency of this hormone and the higher prevalence of allergic diseases [53]. Some randomized studies have evaluated the role of vitamin D supplementation also in the prevention of the winter exacerbation of atopic dermatitis, demonstrating how winter supplementation of vitamin D can be useful for patients with atopic dermatitis, in terms of clinic exacerbation [54,55].
5. Results
In consideration of what has been said, we have collected a total of 26 articles corresponding to the search characteristics, and, for of each of them, we have analyzed and reported the outcomes. Of these, seven articles report how low serum vitamin D levels are common in CRS patients, particularly in the CRSwNP form, compared to control subjects. Furthermore, six of the collected works highlight how vitamin D is involved in the pathogenesis of CRS disease, as it is able to stimulate the inflammatory process mediated by T cells and the production of mediators stimulating the growth and proliferation of fibroblasts of the nasal mucosa. In six other papers, low vitamin D levels are reported to be correlated with a more severe form of CRSwNP. Finally, seven of these highlight how vitamin D supplementation could represent a valid and safe therapy able to support standard treatments, reducing the severity and relapse of the disease. In Table 1, the 26 articles collected are reported.

Table 1.
Articles collected and analyzed.
6. Discussion
On the basis of what has been reported, we have shown how vitamin D plays an important role as an immunomodulator in various pro-inflammatory processes affecting the airways and influences at different levels the different pathogenetic mechanisms involved in the genesis of CRS; in particular, lower levels of VD3 are closely associated with the form CRSwNP. In addition to the known immunomodulatory effects of vitamin D, several studies have reported that it is also endowed with important antiproliferative, anti-angiogenic, and pro-differentiative effects, mainly in some cancers such as ovarian, cervical, prostate, bladder, colorectal, gastric, leukemia, melanoma, and lung. These effects are mediated through the perturbation of several important signaling pathways mediated through genomic and non-genomic mechanisms. Specifically, vitamin D seems to be able to modulate the expression of tumor miRNAs through its action at the VDR level. Recently, an overexpression of catabolic vitamin D enzymes has been found in cancer, thus suggesting that low vitamin D levels are associated with greater tumor severity and therefore a poor prognosis [56,57,58].
Although CRS is a common disease, its treatment remains difficult in many cases, owing to varied mechanisms involved in its etiopathogenesis [59]. According to the 2016 International Consensus Statement on Allergy and Rhinology, the management of both CRS phenotypes is currently based on pharmaceutical treatment, consisting mainly of anti-inflammatory drugs like local intranasal glucocorticoids with natural high-volume saline irrigations (>200 mL) [60].
In the literature, it is reported that approximately 25–30% of patients with CRS develop nasal polyps. Histologically, nasal polyps are characterized by an infiltrate consisting predominantly of eosinophils, known as “eosinophilic CRSwNP”. This form of CRSwNP has proved to be more common in the West than in the East.
Eosinophilic infiltrate of nasal polyps has been shown to correlate with greater clinical severity of the disease and less response to conventional corticosteroid treatments. There are also studies confirming the relationship between mucosal eosinophilia and postoperative nasal recurrence.
In addition to serving as a biomarker for disease severity, it is also possible that eosinophils contribute directly to the pathogenesis of CRSwNP, resulting in a type 2 inflammation shift [61,62,63,64].
However, this current type of CRS treatment has an estimated success rate of around 50%. For some phenotypes, including nasal polyposis, comorbid asthma, aspirin-exacerbated respiratory disease (AERD), and allergic fungal rhinosinusitis (AFRS), failure of medical and surgical management is more common [65]. Low levels of VD3 are also correlated with a greater severity of CRSwNP and a worse clinical outcome of this. In consideration of the new knowledge on the pathogenetic mechanisms of this disease particularly given the involvement of Th2 and pro-inflammatory cytokines produced by them, and the high failure rate of current therapeutic protocols, new biological drugs have recently been introduced, capable of acting at the level of specific molecular targets [66,67]. In this context, vitamin D supplementation, already when levels are equal to the upper ones of the range are reached, could represent an effective and safe additional therapeutic strategy in order to slow the progression of the disease to more severe forms of CRSwNP. Should this treatment fail, the therapeutic indication remains the use of biological drugs and/or surgical treatment. Not only that, the dietary supplementation of vitamin D, even in the presence of a mild state of deficiency, would seem able to improve the clinical outcome of some allergic diseases, in particular food allergies, asthma, and atopic dermatitis. In this review, we have discussed an abundance of evidence regarding the relationship between VD3 and the different types of CRS, especially with CRSwNP. Furthermore, we have highlighted how low levels of vitamin D are correlated with a greater severity of the disease. Its integration could therefore represent a valid therapeutic strategy capable of assisting surgical and biological treatment, thus improving the clinical outcome of patients.
Author Contributions
Conceptualization, G.M. and S.G.; methodology, S.G.; software, F.P.; validation, G.M., S.G. and F.P.; formal analysis, G.M. and F.P.; investigation, S.G. and F.P.; resources, G.M., S.G. and F.P.; data curation, S.G.; writing—original draft preparation, G.M., S.G. and F.P.; writing—review and editing, G.M.; supervision, S.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The study does not report any data as a review article and not a research article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fokkens, W.J.; Lund, V.J.; Hopkins, C.; Hellings, P.W.; Kern, R.; Reitsma, S.; Toppila-Salmi, S.; Bernal-Sprekelsen, M.; Mullol, J.; Alobid, I.; et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology 2020, 58 (Suppl. 29), 1–464. [Google Scholar] [CrossRef]
- Orlandi, R.R.; Kingdom, T.T.; Smith, T.L.; Bleier, B.; DeConde, A.; Luong, A.U.; Poetker, D.M.; Soler, Z.; Welch, K.C.; Wise, S.K.; et al. International consensus statement on allergy and rhinology: Rhinosinusitis 2021. Int. Forum Allergy Rhinol. 2021, 11, 213–739. [Google Scholar] [CrossRef]
- Tomassen, P.; Vandeplas, G.; Van Zele, T.; Cardell, L.-O.; Arebro, J.; Olze, H.; Förster-Ruhrmann, U.; Kowalski, M.L.; Olszewska-Ziąber, A.; Holtappels, G.; et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J. Allergy Clin. Immunol. 2016, 137, 1449–1456.e4. [Google Scholar] [CrossRef] [Green Version]
- Wang, X.; Zhang, N.; Bo, M.; Holtappels, G.; Zheng, M.; Lou, H.; Wang, H.; Zhang, L.; Bachert, C. Diversity of TH cytokine profiles in patients with chronic rhinosinusitis: A multicenter study in Europe, Asia, and Oceania. J. Allergy Clin. Immunol. 2016, 138, 1344–1353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christensen, J.M.; Cheng, J.; Earls, P.; Gunton, J.; Sewell, W.; Sacks, R.; Harvey, R.J.R.J. Vitamin D pathway regulatory genes encoding 1α-hydroxylase and 24-hydroxylase are dysregulated in sinonasal tissue during chronic rhinosinusitis. Int. Forum Allergy Rhinol. 2016, 7, 169–176. [Google Scholar] [CrossRef]
- Sansoni, E.R.; Sautter, N.B.; Mace, J.C.; Smith, T.L.; Yawn, J.R.; Lawrence, L.A.; Schlosser, R.J.; Soler, Z.M.; Mulligan, J.K. Vitamin D3as a novel regulator of basic fibroblast growth factor in chronic rhinosinusitis with nasal polyposis. Int. Forum Allergy Rhinol. 2015, 5, 191–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saponaro, F.; Saba, A.; Zucchi, R. An Update on Vitamin D Metabolism. Int. J. Mol. Sci. 2020, 21, 6573. [Google Scholar] [CrossRef] [PubMed]
- Sassi, F.; Tamone, C.; D’Amelio, P. Vitamin D: Nutrient, Hormone, and Immunomodulator. Nutrients 2018, 10, 1656. [Google Scholar] [CrossRef] [Green Version]
- Murdaca, G.; Tonacci, A.; Negrini, S.; Greco, M.; Borro, M.; Puppo, F.; Gangemi, S. Emerging role of vitamin D in autoimmune diseases: An update on evidence and therapeutic implications. Autoimmun. Rev. 2019, 18, 102350. [Google Scholar] [CrossRef] [PubMed]
- Bakke, D.; Sun, J. Ancient Nuclear Receptor VDR with New Functions: Microbiome and Inflammation. Inflamm. Bowel Dis. 2018, 24, 1149–1154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Talsness, C.E.; Penders, J.; Jansen, E.H.J.M.; Damoiseaux, J.; Thijs, C.; Mommers, M. Influence of vitamin D on key bacterial taxa in infant microbiota in the KOALA Birth Cohort Study. PLoS ONE 2017, 12, e0188011. [Google Scholar] [CrossRef]
- Yamamoto, E.A.; Jørgensen, T.N. Relationships between Vitamin D, Gut Microbiome, and Systemic Autoimmunity. Front. Immunol. 2020, 10, 3141. [Google Scholar] [CrossRef] [PubMed]
- Ogbu, D.; Xia, E.; Sun, J. Gut instincts: Vitamin D/vitamin D receptor and microbiome in neurodevelopment disorders. Open Biol. 2020, 10, 200063. [Google Scholar] [CrossRef] [PubMed]
- Bakke, D.; Chatterjee, I.; Agrawal, A.; Dai, Y.; Sun, A.J. Regulation of Microbiota by Vitamin D Receptor: A Nuclear Weapon in Metabolic Diseases. Nucl. Recept. Res. 2018, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poole, A.; Song, Y.; Brown, H.; Hart, P.H.; Zhang, G. (Brad) Cellular and molecular mechanisms of vitamin D in food allergy. J. Cell. Mol. Med. 2018, 22, 3270–3277. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, A.; Mach, N. Role of Vitamin D in the Hygiene Hypothesis: The Interplay between Vitamin D, Vitamin D Receptors, Gut Microbiota, and Immune Response. Front. Immunol. 2016, 7, 627. [Google Scholar] [CrossRef] [Green Version]
- Jin, D.; Wu, S.; Zhang, Y.G.; Lu, R.; Xia, Y.; Dong, H.; Sun, J. Lack of Vitamin D Receptor Causes Dysbiosis and Changes the Functions of the Murine Intestinal Microbiome. Clin. Ther. 2015, 37, 996–1009. [Google Scholar] [CrossRef]
- Naderpoor, N.; Mousa, A.; Arango, L.F.G.; Barrett, H.L.; Nitert, M.D.; De Courten, B. Effect of Vitamin D Supplementation on Faecal Microbiota: A Randomised Clinical Trial. Nutrients 2019, 11, 2888. [Google Scholar] [CrossRef] [Green Version]
- Lombardi, C.; Passalacqua, G.; Italian Vitamin D Allergy Group. Vitamin D levels and allergic diseases. An italian cross-sectional multicenter survey. Eur. Ann. Allergy Clin. Immunol. 2017, 49, 75–79. [Google Scholar] [PubMed]
- Heine, R.G. Food Allergy Prevention and Treatment by Targeted Nutrition. Ann. Nutr. Metab. 2018, 72, 33–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murdaca, G.; Gerosa, A.; Paladin, F.; Petrocchi, L.; Banchero, S.; Gangemi, S. Vitamin D and Microbiota: Is There a Link with Allergies? Int. J. Mol. Sci. 2021, 22, 4288. [Google Scholar] [CrossRef] [PubMed]
- Erdag, O.; Turan, M.; Ucler, R.; Berkoz, M.; Garca, M.F.; Bozan, N.; Kıroglu, A.F.; Cankaya, H. Is Nasal Polyposis Related to Levels of Serum Vitamin D and Vitamin D Receptor Gene Expression? Med Sci. Monit. 2016, 22, 4636–4643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bozzetto, S.; Carraro, S.; Giordano, G.; Boner, A.; Baraldi, E. Asthma, allergy and respiratory infections: The vitamin D hypothesis. Allergy 2011, 67, 10–17. [Google Scholar] [CrossRef]
- Ozkara, S.; Keles, E.; Ilhan, N.; Gungor, H.; Kaygusuz, I.; Alpay, H.C. The relationship between Th1/Th2 balance and 1α,25-dihydroxyvitamin D3 in patients with nasal polyposis. Eur. Arch. Oto-Rhino-Laryngol. 2012, 269, 2519–2524. [Google Scholar] [CrossRef]
- Sikorska-Szaflik, H.; Sozańska, B. The Role of Vitamin D in Respiratory Allergies Prevention. Why the Effect Is so Difficult to Disentangle? Nutrients 2020, 12, 1801. [Google Scholar] [CrossRef]
- Bonanno, A.; Gangemi, S.; La Grutta, S.; Malizia, V.; Riccobono, L.; Colombo, P.; Cibella, F.; Profita, M. 25-Hydroxyvitamin D, IL-31, and IL-33 in Children with Allergic Disease of the Airways. Mediat. Inflamm. 2014, 2014, 520241. [Google Scholar] [CrossRef] [Green Version]
- Mirzakhani, H.; Al-Garawi, A.; Weiss, S.T.; Litonjua, A.A. Vitamin D and the development of allergic disease: How important is it? Clin. Exp. Allergy 2014, 45, 114–125. [Google Scholar] [CrossRef] [Green Version]
- Chandrakar, A.K.; Alexander, A.; Rajendiran, K.; Ramasamy, K. 25-Hydroxyl Vitamin D Deficiency in Nasal Polyposis. Mediat. Inflamm. 2014, 2014, 520241. [Google Scholar] [CrossRef]
- Mostafa, B.; Taha, M.; Hamid, T.A.; Omran, A.; Lotfi, N. Evaluation of vitamin D levels in allergic fungal sinusitis, chronic rhinosinusitis, and chronic rhinosinusitis with polyposis. Int. Forum Allergy Rhinol. 2015, 6, 185–190. [Google Scholar] [CrossRef]
- Kalińczak-Górna, P.; Radajewski, K.; Burduk, P. Relationship between the Severity of Inflammatory Changes in Chronic Sinusitis and the Level of Vitamin D before and after the FESS Procedure. J. Clin. Med. 2021, 10, 2836. [Google Scholar] [CrossRef] [PubMed]
- Konstantinidis, I.; Fotoulaki, M.; Iakovou, I.; Chatziavramidis, A.; Mpalaris, V.; Shobat, K.; Markou, K. Vitamin D3 Deficiency and its Association with Nasal Polyposis in Patients with Cystic Fibrosis and Patients with Chronic Rhinosinusitis. Am. J. Rhinol. Allergy 2017, 31, 395–400. [Google Scholar] [CrossRef]
- Rostkowska-Nadolska, B.; Sliupkas-Dyrda, E.; Potyka, J.; Kusmierz, D.; Fraczek, M.; Krecicki, T.; Kubik, P.; Zatonski, M.; Latocha, M. Vitamin D derivatives: Calcitriol and tacalcitol inhibits interleukin-6 and interleukin-8 expression in human nasal polyp fibroblast cultures. Adv. Med. Sci. 2010, 55, 86–92. [Google Scholar] [CrossRef]
- Tomaszewska, M.; Sarnowska, E.; Rusetska, N.; Kowalik, K.; Sierdzinski, J.; Siedlecki, J.A.; Badmaev, V.; Stohs, S.J.; Popko, M. Role of Vitamin D and Its Receptors in the Pathophysiology of Chronic Rhinosinusitis. J. Am. Coll. Nutr. 2019, 38, 108–118. [Google Scholar] [CrossRef]
- Carroll, W.W.; Schlosser, R.J.; O’Connell, B.P.; Soler, Z.M.; Mulligan, J.K. Vitamin D deficiency is associated with increased human sinonasal fibroblast proliferation in chronic rhinosinusitis with nasal polyps. Int. Forum Allergy Rhinol. 2016, 6, 605–610. [Google Scholar] [CrossRef]
- Mulligan, J.K.; Pasquini, W.N.; Carroll, W.W.; Williamson, T.; Reaves, N.; Patel, K.J.; Mappus, E.; Schlosser, R.J.; Atkinson, C. Dietary vitamin D3 deficiency exacerbates sinonasal inflammation and alters local 25(OH)D3 metabolism. PLoS ONE 2017, 12, e0186374. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.-F.; Tai, C.-F.; Chien, C.-Y.; Chiang, F.-Y.; Chen, J.Y.-F. Vitamin D decreases the secretion of matrix metalloproteinase-2 and matrix metalloproteinase-9 in fibroblasts derived from Taiwanese patients with chronic rhinosinusitis with nasal polyposis. Kaohsiung J. Med Sci. 2015, 31, 235–240. [Google Scholar] [CrossRef] [Green Version]
- Wang, L.-F.; Lee, C.-H.; Chien, C.-Y.; Chen, J.Y.-F.; Chiang, F.-Y.; Tai, C.-F. Serum 25-hydroxyvitamin D Levels are Lower in Chronic Rhinosinusitis with Nasal Polyposis and are Correlated with Disease Severity in Taiwanese Patients. Am. J. Rhinol. Allergy 2013, 27, e162–e165. [Google Scholar] [CrossRef]
- Zand, V.; Baradaranfar, M.; Vaziribozorg, S.; Mandegari, M.; Mansourimanesh, M.; Saeidieslami, N. Correlation of Serum Vitamin D Levels with Chronic Rhinosinusitis Disease Severity. Iran J. Otorhinolaryngol. 2020, 32, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Yang, Y.; Chen, H. Vitamin D deficiency are associated with subjective disease severity in Chinese patients with chronic rhinosinusitis with nasal polyps. Am. J. Otolaryngol. 2019, 40, 36–39. [Google Scholar] [CrossRef]
- Schlosser, R.J.; Soler, Z.M.; Schmedes, G.W.; Storck, K.; Mulligan, J.K. Impact of vitamin D deficiency upon clinical presentation in nasal polyposis. Int. Forum Allergy Rhinol. 2014, 4, 196–199. [Google Scholar] [CrossRef] [PubMed]
- Hashemian, F.; Sadegh, S.; Jahanshahi, J.; Rabiei, M.A.S.; Hashemian, F. Effects of Vitamin D Supplementation on Recurrence of Nasal Polyposis after Endoscopic Sinus Surgery. Iran J. Otorhinolaryngol. 2020, 32, 21–28. [Google Scholar] [CrossRef]
- Tian, H.-Q.; Cheng, L. The role of vitamin D in allergic rhinitis. Asia Pac. Allergy 2017, 7, 65–73. [Google Scholar] [CrossRef] [Green Version]
- Muehleisen, B.; Gallo, R.L. Vitamin D in allergic disease: Shedding light on a complex problem. J. Allergy Clin. Immunol. 2013, 131, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Bakhshaee, M.; Sharifian, M.; Esmatinia, F.; Rasoulian, B.; Mohebbi, M. Therapeutic effect of vitamin D supplementation on allergic rhinitis. Eur. Arch. Oto-Rhino-Laryngol. 2019, 276, 2797–2801. [Google Scholar] [CrossRef] [PubMed]
- Bunyavanich, S.; Rifas-Shiman, S.L.; Platts-Mills, T.A.; Workman, L.; Sordillo, J.E.; Camargo, C.A.; Gillman, M.W.; Gold, D.R.; Litonjua, A.A. Prenatal, perinatal, and childhood vitamin D exposure and their association with childhood allergic rhinitis and allergic sensitization. J. Allergy Clin. Immunol. 2016, 137, 1063–1070.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bener, A.; Ehlayel, M.S.; Bener, H.Z.; Hamid, Q. The impact of Vitamin D deficiency on asthma, allergic rhinitis and wheezing in children: An emerging public health problem. J. Fam. Community Med. 2014, 21, 154–161. [Google Scholar] [CrossRef] [Green Version]
- Wjst, M.; Hypponen, E. Vitamin D serum levels and allergic rhinitis. Allergy 2007, 62, 1085–1086. [Google Scholar] [CrossRef] [PubMed]
- Penna, G.; Adorini, L. 1α,25-Dihydroxyvitamin D3Inhibits Differentiation, Maturation, Activation, and Survival of Dendritic Cells Leading to Impaired Alloreactive T Cell Activation. J. Immunol. 2000, 164, 2405–2411. [Google Scholar] [CrossRef] [Green Version]
- Farsani, Z.S.; Behmanesh, M.; Sahraian, M.A. Interleukin-10 but not transforming growth factor-β1 gene expression is up-regulated by vitamin D treatment in multiple sclerosis patients. J. Neurol. Sci. 2015, 350, 18–23. [Google Scholar] [CrossRef]
- Sudiro, M.; Lestari, B.W.; Madiadipoera, T.; Setiabudiawan, B.; Boesoirie, T.S. Vitamin D Deficiency Is Correlated with Severity of Allergic Rhinitis. OALib 2017, 04, 1–9. [Google Scholar] [CrossRef]
- Vatankhah, V.; Lotfizadeh, M.; Iranpoor, H.; Jafari, F.; Khazraei, H. Comparison vitamin D serum levels in allergic rhinitis patients with normal population. Rev. Franç. d’Allergol. 2016, 56, 539–543. [Google Scholar] [CrossRef]
- Alnori, H.; Alassaf, F.A.; Alfahad, M.; Qazzaz, M.E.; Jasim, M.; Abed, M.N. Vitamin D and Immunoglobulin E Status in Allergic Rhinitis Patients Compared to Healthy People. J. Med. Life 2020, 13, 463–468. [Google Scholar] [CrossRef]
- Sun, J. Dietary Vitamin D, Vitamin D Receptor, and Microbiome. Curr. Opin. Clin. Nutr. Metab. Care 2018, 21, 471–474. [Google Scholar] [CrossRef]
- Willits, E.K.; Wang, Z.; Jin, J.; Patel, B.; Motosue, M.; Bhagia, A.; Almasri, J.; Erwin, P.J.; Kumar, S.; Joshi, A.Y.; et al. Vitamin D and food allergies in children: A systematic review and meta-analysis. Allergy Asthma Proc. 2017, 38, 21–28. [Google Scholar] [CrossRef]
- Camargo, C.A., Jr.; Ganmaa, D.; Sidbury, R.; Erdenedelger, K.; Radnaakhand, N.; Khandsuren, B. Randomized trial of vitamin D supplementation for winter-related atopic dermatitis in children. J. Allergy Clin. Immunol. 2014, 134, 831–835. [Google Scholar] [CrossRef] [PubMed]
- Javanbakht, M.H.; Keshavarz, S.A.; Djalali, M.; Siassi, F.; Eshraghian, M.R.; Firooz, A.; Seirafi, H.; Ehsani, A.H.; Chamari, M.; Mirshafiey, A. Randomized controlled trial using vitamins E and D supplementation in atopic dermatitis. J. Dermatol. Treat. 2010, 22, 144–150. [Google Scholar] [CrossRef]
- Deeb, K.K.; Trump, D.L.; Johnson, C.S. Vitamin D signalling pathways in cancer: Potential for anticancer therapeutics. Nat. Rev. Cancer 2007, 7, 684–700. [Google Scholar] [CrossRef]
- Zeljic, K.; Supic, G.; Magic, Z. New insights into vitamin D anticancer properties: Focus on miRNA modulation. Mol. Genet. Genom. 2017, 292, 511–524. [Google Scholar] [CrossRef] [PubMed]
- Bachert, C.; Zhang, N.; Hellings, P.W.; Bousquet, J. Endotype-driven care pathways in patients with chronic rhinosinusitis. J. Allergy Clin. Immunol. 2018, 141, 1543–1551. [Google Scholar] [CrossRef] [PubMed]
- Fujieda, S.; Imoto, Y.; Kato, Y.; Ninomiya, T.; Tokunaga, T.; Tsutsumiuchi, T.; Yoshida, K.; Kidoguchi, M.; Takabayashi, T. Eosinophilic chronic rhinosinusitis. Allergol. Int. 2019, 68, 403–412. [Google Scholar] [CrossRef]
- Lou, H.; Zhang, N.; Bachert, C.; Zhang, L. Highlights of eosinophilic chronic rhinosinusitis with nasal polyps in definition, prognosis, and advancement. Int. Forum Allergy Rhinol. 2018, 8, 1218–1225. [Google Scholar] [CrossRef] [PubMed]
- Aslan, F.; Altun, E.; Paksoy, S.; Turan, G. Could Eosinophilia predict clinical severity in nasal polyps? Multidiscip. Respir. Med. 2017, 12, 21. [Google Scholar] [CrossRef] [Green Version]
- Wang, K.; Deng, J.; Yang, M.; Chen, Y.; Chen, F.; Gao, W.-X.; Lai, Y.; Shi, J.; Sun, Y. Concordant systemic and local eosinophilia relates to poorer disease control in patients with nasal polyps. World Allergy Organ. J. 2019, 12, 100052. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bochner, B.S.; Stevens, W.W. Biology and Function of Eosinophils in Chronic Rhinosinusitis with or without Nasal Polyps. Allergy Asthma Immunol. Res. 2021, 13, 8–22. [Google Scholar] [CrossRef] [PubMed]
- Nasta, M.S.; Chatzinakis, V.A.; Georgalas, C. Updates on current evidence for biologics in chronic rhinosinusitis. Curr. Opin. Otolaryngol. Head Neck Surg. 2020, 28, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Kartush, A.G.; Schumacher, J.K.; Shah, R.; Patadia, M.O. Biologic Agents for the Treatment of Chronic Rhinosinusitis with Nasal Polyps. Am. J. Rhinol. Allergy 2018, 33, 203–211. [Google Scholar] [CrossRef]
- Brown, W.C.; Senior, B. A Critical Look at the Efficacy and Costs of Biologic Therapy for Chronic Rhinosinusitis with Nasal Polyposis. Curr. Allergy Asthma Rep. 2020, 20, 16. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).