The Preparation of Experimental Resin-Based Dental Composites Using Different Mixing Methods for the Filler and Matrix †
Abstract
1. Introduction
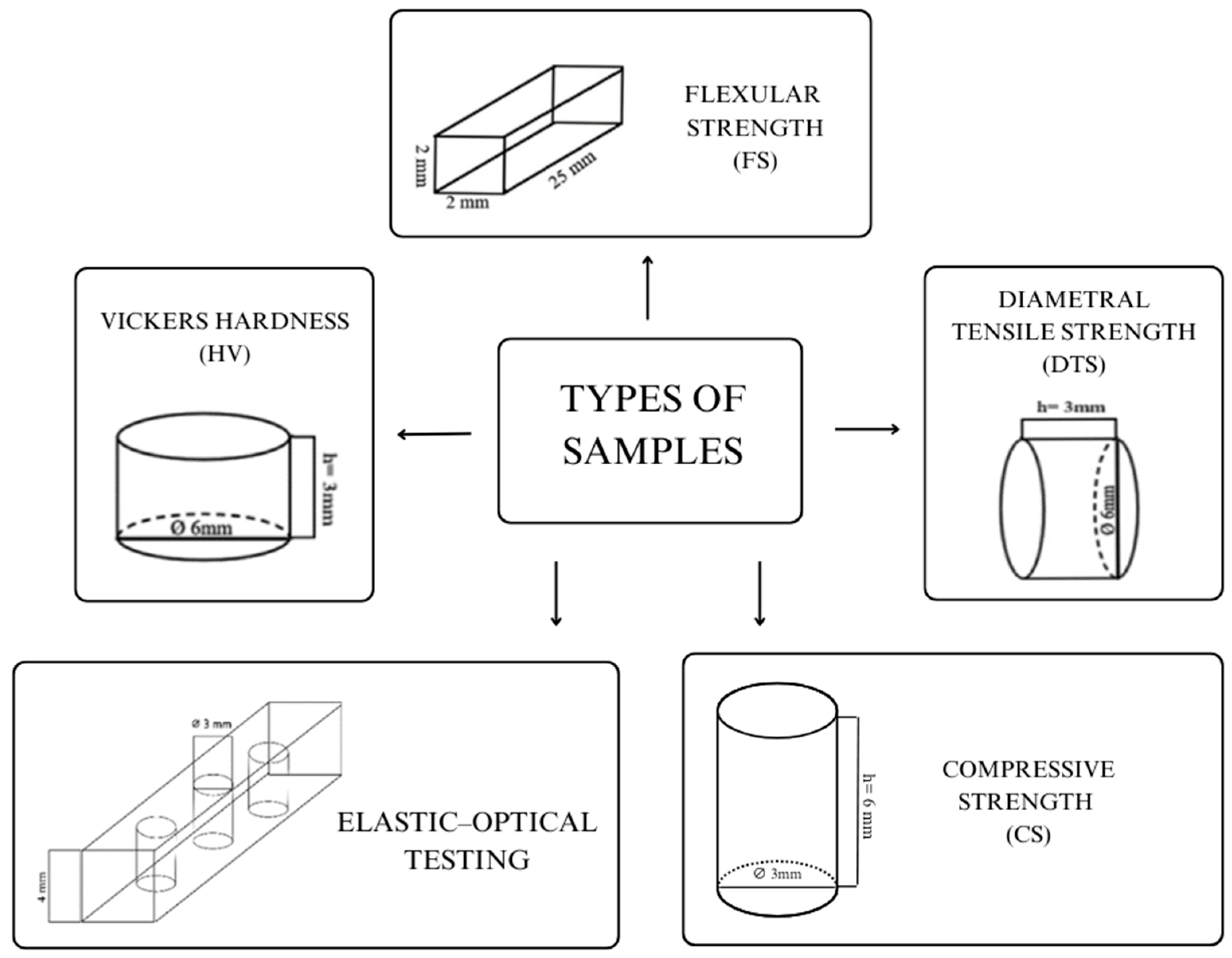
2. Materials and Methods
- F—force;
- A—lateral area of imprint A [mm2].
- L—support spacing, 20 mm [mm].
- F—load [N];
- b—width of the specimen [mm];
- h—height of the specimen [mm].
- P—compressive force [N];
- D—diameter of the specimen [mm];
- T—thickness of the specimen [mm].
- σr—radial stress;
- σθ—circumferential stress;
- ps—shrinkage stress at the periphery of the hole;
- a—inner radius of the hole in the plate;
- b—radius of the largest isochrome;
- r—radius in the ab region.
3. Results
- Hardness test
- Flexural strength
- Flexural modulus
- Diametral tensile strength
- Compressive strength
- Shrinkage stress
4. Discussion
5. Conclusions
- The method of the filler and matrix mixing affects the flexural strength and hardness of experimental composites. Mechanically prepared composites have the highest flexural strength parameters and hardness.
- The method of the filler and matrix mixing does not influence the compressive strength of the resulting composites.
- The mixing method influences contraction stress. The lowest contraction stress is observed when the composite is partially manually prepared.
- The method of the filler and matrix mixing affects the distribution and grain size of the silanized silica.
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Aminoroaya, A.; Neisiany, R.E.; Khorasani, S.N.; Panahi, P.; Das, O.; Madry, H.; Cucchiarini, M.; Ramakrishna, S. A Review of Dental Composites: Challenges, Chemistry Aspects, Filler Influences, and Future Insights. Compos. B Eng. 2021, 216, 108852. [Google Scholar] [CrossRef]
- Cadenaro, M.; Josic, U.; Maravić, T.; Mazzitelli, C.; Marchesi, G.; Mancuso, E.; Breschi, L.; Mazzoni, A. Progress in Dental Adhesive Materials. J. Dent. Res. 2023, 102, 254–262. [Google Scholar] [CrossRef]
- Ilie, N.; Hilton, T.J.; Heintze, S.D.; Hickel, R.; Watts, D.C.; Silikas, N.; Stansbury, J.W.; Cadenaro, M.; Ferracane, J.L. Academy of Dental Materials Guidance—Resin Composites: Part I—Mechanical Properties. Dent. Mater. 2017, 33, 880–894. [Google Scholar] [CrossRef] [PubMed]
- Paolone, G.; Diana, C.; Cantatore, G. 2023 State-of-the-Art in Resin-Based Composites and Future Trends. Compend. Contin. Educ. Dent. 2023, 44, 98–100. [Google Scholar] [PubMed]
- Bourbia, M.; Finer, Y. Biochemical Stability and Interactions of Dental Resin Composites and Adhesives with Host and Bacteria in the Oral Cavity: A Review. J. Can. Dent. Assoc. 2018, 84, i1. [Google Scholar]
- Liu, J.; Zhang, H.; Sun, H.; Liu, Y.; Liu, W.; Su, B.; Li, S. The Development of Filler Morphology in Dental Resin Composites: A Review. Materials 2021, 14, 5612. [Google Scholar] [CrossRef]
- Rizzante, F.A.P.; Duque, J.A.; Duarte, M.A.H.; Mondelli, R.F.L.; Mendonca, G.; Ishikiriama, S.K. Polymerization Shrinkage, Microhardness and Depth of Cure of Bulk Fill Resin Composites. Dent. Mater. J. 2019, 38, 403–410. [Google Scholar] [CrossRef]
- Ferracane, J.L. Resin Composite—State of the Art. Dent. Mater. 2011, 27, 29–38. [Google Scholar] [CrossRef]
- Hata, K.; Ikeda, H.; Nagamatsu, Y.; Masaki, C.; Hosokawa, R.; Shimizu, H. Development of Dental Poly(Methyl Methacrylate)-Based Resin for Stereolithography Additive Manufacturing. Polymers 2021, 13, 4435. [Google Scholar] [CrossRef]
- Topa-Skwarczyńska, M.; Ortyl, J. Photopolymerization Shrinkage: Strategies for Reduction, Measurement Methods and Future Insights. Polym. Chem. 2023, 14, 2145–2158. [Google Scholar] [CrossRef]
- Wang, K.; Wang, Z. Shrinkage Stress Evolution during Photopolymerization: Theory and Experiments. J. Mech. Phys. Solids 2023, 178, 105350. [Google Scholar] [CrossRef]
- Alsharif, S.; Alhareb, A.; Abudalazez, A. Components of Dental Resin Composites: A Literature Review. AlQalam J. Med. Appl. Sci. 2024, 7, 427–440. [Google Scholar] [CrossRef]
- Czech, Z.; Minciel, E. Światłoutwardzalne Kompozyty Zawierające Akrylowane Żywice Wielofunkcyjne—Skrócony Przegląd Literaturowy. Apar. Badaw. I Dydaktyczna 2015, 20, 270–275. [Google Scholar]
- Sozer, E.M.; Simacek, P.; Advani, S.G. Resin Transfer Molding (RTM) in Polymer Matrix Composites. In Manufacturing Techniques for Polymer Matrix Composites (PMCs); Elsevier: Amsterdam, The Netherlands, 2012; pp. 245–309. [Google Scholar]
- Terekhov, I.V.; Chistyakov, E.M. Binders Used for the Manufacturing of Composite Materials by Liquid Composite Molding. Polymers 2021, 14, 87. [Google Scholar] [CrossRef] [PubMed]
- Winnier, J.; Hambire, C.; Hambire, U. Effect of Nanohydroxyapatite, Zirconia and Glass Filler Particles on the Wear and Microhardness of Experimental Dental Composite Resin. Int. J. Clin. Pediatr. Dent. 2023, 16, S81–S84. [Google Scholar] [CrossRef]
- Al-Odayni, A.-B.; Alotaibi, D.H.; Saeed, W.S.; Al-Kahtani, A.; Assiri, A.; Alkhtani, F.M.; Alrahlah, A. Eugenyl-2-Hydroxypropyl Methacrylate-Incorporated Experimental Dental Composite: Degree of Polymerization and In Vitro Cytotoxicity Evaluation. Polymers 2022, 14, 277. [Google Scholar] [CrossRef]
- Pontons-Melo, J.C.; Balbinot, G.d.S.; Sauro, S.; Collares, F.M. Experimental Composite Resin with Myristyltrimethylammonium Bromide (MYTAB) and Alpha-Tricalcium Phosphate (α-TCP): Antibacterial and Remineralizing Effect. J. Funct. Biomater. 2023, 14, 303. [Google Scholar] [CrossRef]
- Loos, M. Processing of Polymer Matrix Composites Containing CNTs. In Carbon Nanotube Reinforced Composites; Elsevier: Amsterdam, The Netherlands, 2015; pp. 171–188. [Google Scholar]
- Fu, Y.-C.; Chen, C.-H.; Wang, C.-Z.; Wang, Y.-H.; Chang, J.-K.; Wang, G.-J.; Ho, M.-L.; Wang, C.-K. Preparation of Porous Bioceramics Using Reverse Thermo-Responsive Hydrogels in Combination with RhBMP-2 Carriers: In Vitro and in Vivo Evaluation. J. Mech. Behav. Biomed. Mater. 2013, 27, 64–76. [Google Scholar] [CrossRef]
- McDaniel, T.F.; Kramer, R.T.; Im, F.; Snow, D. Effects of Mixing Technique on Bubble Formation in Alginate Impression Material. Gen. Dent. 2013, 61, 35–39. [Google Scholar]
- Chambers, C.; Stewart, S.B.; Su, B.; Jenkinson, H.F.; Sandy, J.R.; Ireland, A.J. Silver Doped Titanium Dioxide Nanoparticles as Antimicrobial Additives to Dental Polymers. Dent. Mater. 2017, 33, e115–e123. [Google Scholar] [CrossRef]
- Um, J.G.; Jun, Y.-S.; Alhumade, H.; Krithivasan, H.; Lui, G.; Yu, A. Investigation of the Size Effect of Graphene Nano-Platelets (GnPs) on the Anti-Corrosion Performance of Polyurethane/GnP Composites. RSC Adv. 2018, 8, 17091–17100. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.-M.; Cai, T.; Mandaric, S.; Chopra, S.; Han, H.; Jang, S.; Il Choi, W.; Langer, R.; Farokhzad, O.C.; Karnik, R. Drug Loading Augmentation in Polymeric Nanoparticles Using a Coaxial Turbulent Jet Mixer: Yong Investigator Perspective. J. Colloid. Interface Sci. 2019, 538, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Bociong, K.; Zalega, M.; Dawicka, O.; Jasińska, A.; Żabecka, A.; Kałuża, P. Wpływ metody wytwarzania światłoutwardzalnego kompozytu do zastosowań w stomatologii na wybrane właściwości wytrzymałościowe in programme and materials of the XXII Conference of XXII Konferencji BIOMATERIAŁY I MECHANIKA W STOMATOLOGII, Wisła, Poland, 10–13 October 2024.
- ISO 4049; Dentistry—Polymer-Based Restorative Materials. ISO: Geneva, Switzerland, 2019; pp. 1–29.
- Bociong, K.; Krasowski, M.; Domarecka, M.; Sokolowski, J. Effect of the Method of Photopolymerization of Dental Composites Based on Dimethacrylate Resin on the Shrinkage Stresses and Selected Properties of the Cured Material. Polimery 2016, 61, 499–508. [Google Scholar] [CrossRef]
- Krasowski, M.; Ciesielska, S.; Śmielak, B.; Kopacz, K.; Bociong, K. Preparation of an Experimental Dental Composite with Different Bis-GMA/UDMA Proportions. Mater. Manuf. Process. 2024, 39, 1044–1051. [Google Scholar] [CrossRef]
- Ferracane, J.L. Resin-Based Composite Performance: Are There Some Things We Can’t Predict? Dent. Mater. 2013, 29, 51–58. [Google Scholar] [CrossRef]
- Ferracane, J.L. Current Trends in Dental Composites. Crit. Rev. Oral Biol. Med. 1995, 6, 302–318. [Google Scholar] [CrossRef]
- He, X.; Zhang, D.; Deng, S. Effect of Duration and Infection Control Barriers of Light Curing Unit on Hardness of Bulk Fill Composite Resin. PeerJ 2024, 12, e18021. [Google Scholar] [CrossRef]
- Ren, Z.; Chen, H.; Wang, R.; Zhu, M. Comparative Assessments of Dental Resin Composites: A Focus on Dense Microhybrid Materials. ACS Biomater. Sci. Eng. 2024, 10, 3718–3726. [Google Scholar] [CrossRef]
- Chen, F.; Sun, L.; Luo, H.; Yu, P.; Lin, J. Influence of Filler Types on Wear and Surface Hardness of Composite Resin Restorations. J. Appl. Biomater. Funct. Mater. 2023, 21, 22808000231193524. [Google Scholar] [CrossRef]
- Zalega, M.; Nowak, J.; Bociong, K. The Influence of Quaternary Ammonium Salts on Mechanical Properties of Light-Cured Resin Dental Composites. Polimery 2023, 68, 195–205. [Google Scholar] [CrossRef]
- Szczesio-Wlodarczyk, A.; Kopacz, K.; Szynkowska-Jozwik, M.I.; Sokolowski, J.; Bociong, K. An Evaluation of the Hydrolytic Stability of Selected Experimental Dental Matrices and Composites. Materials 2022, 15, 5055. [Google Scholar] [CrossRef]
- Szczesio-Wlodarczyk, A.; Barszczewska-Rybarek, I.M.; Chrószcz-Porębska, M.W.; Kopacz, K.; Sokolowski, J.; Bociong, K. Can Modification with Urethane Derivatives or the Addition of an Anti-Hydrolysis Agent Influence the Hydrolytic Stability of Resin Dental Composite? Int. J. Mol. Sci. 2023, 24, 4336. [Google Scholar] [CrossRef] [PubMed]
- Jun, S.-K.; Kim, D.-A.; Goo, H.-J.; Lee, H.-H. Investigation of the Correlation between the Different Mechanical Properties of Resin Composites. Dent. Mater. J. 2013, 32, 48–57. [Google Scholar] [CrossRef]
- Wysokińska-Miszczuk, J.; Piotrowska, K.; Paulo, M.; Madej, M. Composite Materials Used for Dental Fillings. Materials 2024, 17, 4936. [Google Scholar] [CrossRef] [PubMed]
- Bociong, K.; Szczesio, A.; Krasowski, M.; Sokolowski, J. The Influence of Filler Amount on Selected Properties of New Experimental Resin Dental Composite. Open Chem. 2018, 16, 905–911. [Google Scholar] [CrossRef]
- Shekofteh, K.; Kashi, T.J.; Behroozibakhsh, M.; Sadr, A.; Najafi, F.; Bagheri, H. Evaluation of Physical/Mechanical Properties of an Experimental Dental Composite Modified with a Zirconium-Based Metal-Organic Framework (MOF) as an Innovative Dental Filler. Dent. Mater. 2023, 39, 790–799. [Google Scholar] [CrossRef]
- Yadav, R.; Lee, H.; Lee, J.-H.; Singh, R.K.; Lee, H.-H. A Comprehensive Review: Physical, Mechanical, and Tribological Characterization of Dental Resin Composite Materials. Tribol. Int. 2023, 179, 108102. [Google Scholar] [CrossRef]
- Kundie, F.; Azhari, C.H.; Muchtar, A.; Ahmad, Z.A. Effects of Filler Size on the Mechanical Properties of Polymer-Filled Dental Composites: A Review of Recent Developments. J. Phys. Sci. 2018, 29, 141–165. [Google Scholar] [CrossRef]
- Elfakhri, F.; Alkahtani, R.; Li, C.; Khaliq, J. Influence of Filler Characteristics on the Performance of Dental Composites: A Comprehensive Review. Ceram. Int. 2022, 48, 27280–27294. [Google Scholar] [CrossRef]
- Germain, H.S.; Swartz, M.L.; Phillips, R.W.; Moore, B.K.; Roberts, T.A. Properties of Microfilled Composite Resins as Influenced by Filler Content. J. Dent. Res. 1985, 64, 155–160. [Google Scholar] [CrossRef]
- Samal, S. Effect of Shape and Size of Filler Particle on the Aggregation and Sedimentation Behavior of the Polymer Composite. Powder Technol. 2020, 366, 43–51. [Google Scholar] [CrossRef]
- Wang, R.; Habib, E.; Zhu, X.X. Evaluation of the Filler Packing Structures in Dental Resin Composites: From Theory to Practice. Dent. Mater. 2018, 34, 1014–1023. [Google Scholar] [CrossRef] [PubMed]
- Ornaghi, B.P.; Meier, M.M.; Rosa, V.; Cesar, P.F.; Lohbauer, U.; Braga, R.R. Subcritical Crack Growth and in Vitro Lifetime Prediction of Resin Composites with Different Filler Distributions. Dent. Mater. 2012, 28, 985–995. [Google Scholar] [CrossRef]
- Domarecka, M.; Szczesio-Wlodarczyk, A.; Krasowski, M.; Fronczek, M.; Gozdek, T.; Sokolowski, J.; Bociong, K. A Comparative Study of the Mechanical Properties of Selected Dental Composites with a Dual-Curing System with Light-Curing Composites. Coatings 2021, 11, 1255. [Google Scholar] [CrossRef]
- Yesudhas Jayakumari, B.; Nattanmai Swaminathan, E.; Partheeban, P. A Review on Characteristics Studies on Carbon Nanotubes-Based Cement Concrete. Constr. Build. Mater. 2023, 367, 130344. [Google Scholar] [CrossRef]
- Fu, S.-Y.; Feng, X.-Q.; Lauke, B.; Mai, Y.-W. Effects of Particle Size, Particle/Matrix Interface Adhesion and Particle Loading on Mechanical Properties of Particulate–Polymer Composites. Compos. B Eng. 2008, 39, 933–961. [Google Scholar] [CrossRef]
- Zhang, H.; Darvell, B.W. Mechanical Properties of Hydroxyapatite Whisker-Reinforced Bis-GMA-Based Resin Composites. Dent. Mater. 2012, 28, 824–830. [Google Scholar] [CrossRef]
- Kumar, N.; Shortall, A. Standardisation of mixing method for experimental resin-based composite. J. Pak. Dent. Assoc. 2011, 20, 131–134. [Google Scholar]
- Craig, R.G. (Ed.) Restorative Dental Materials; Elsevier: Amsterdam, The Netherlands, 2019; ISBN 9780323478212. [Google Scholar]
- Okulus, Z. Otrzymywanie Oraz Charakterystyka Dentystycznych Materiałów Kompozytowych. Ph.D. Thesis, Poznan University of Technology, Faculty of Chemical Technology, Poznań, Poland, 2016. [Google Scholar]
- Al-Shekhli, A.A.; Aubi, I. Al Composite Diametral Tensile Strength. World J. Dent. 2018, 9, 457–461. [Google Scholar] [CrossRef]
- Cho, G.C.; Kaneko, L.M.; Donovan, T.E.; White, S.N. Diametral and Compressive Strength of Dental Core Materials. J. Prosthet. Dent. 1999, 82, 272–276. [Google Scholar] [CrossRef]
- MIYASAKA, T. Effect of Shape and Size of Silanated Fillers on Mechanical Properties of Experimental Photo Cure Composite Resins. Dent. Mater. J. 1996, 15, 98–110,249. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zalega, M.; Bociong, K. Antibacterial Agents Used in Modifications of Dental Resin Composites: A Systematic Review. Appl. Sci. 2024, 14, 3710. [Google Scholar] [CrossRef]
- Domarecka, M.; Sokołowski, K.; Krasowski, M.; Łukomska-Szymańska, M.; Sokołowski, J. The Shrinkage Stress of Modified Flowable Dental Composites. Dent. Med. Probl. 2015, 52, 424–433. [Google Scholar] [CrossRef]
- Szczesio-Wlodarczyk, A.; Garoushi, S.; Vallittu, P.; Bociong, K.; Lassila, L. Polymerization Shrinkage Stress of Contemporary Dental Composites: Comparison of Two Measurement Methods. Dent. Mater. J. 2024, 43, 2023–2192. [Google Scholar] [CrossRef]
- Baudin, C.; Osorio, R.; Toledano, M.; de Aza, S. Work of Fracture of a Composite Resin: Fracture-toughening Mechanisms. J. Biomed. Mater. Res. A 2009, 89A, 751–758. [Google Scholar] [CrossRef]
- Sarna-Boś, K.; Skic, K.; Sobieszczański, J.; Boguta, P.; Chałas, R. Contemporary Approach to the Porosity of Dental Materials and Methods of Its Measurement. Int. J. Mol. Sci. 2021, 22, 8903. [Google Scholar] [CrossRef]
- Linden, L.-A.; Jakubiak, J. Contraction (Shrinkage) in Polymerization. Part II. Dental Resin Composites. Polimery 2001, 46, 590–595. [Google Scholar] [CrossRef][Green Version]
- Buelvas, D.D.A.; Besegato, J.F.; Vicentin, B.L.S.; Jussiani, E.I.; Hoeppner, M.G.; Andrello, A.C.; Di Mauro, E. Impact of Light-Cure Protocols on the Porosity and Shrinkage of Commercial Bulk Fill Dental Resin Composites with Different Flowability. J. Polym. Res. 2020, 27, 292. [Google Scholar] [CrossRef]
- Tyas, M.J. Correlation between Fracture Properties and Clinical Performance of Composite Resins in Class IV Cavities. Aust. Dent. J. 1990, 35, 46–49. [Google Scholar] [CrossRef]
- Heintze, S.D.; Ilie, N.; Hickel, R.; Reis, A.; Loguercio, A.; Rousson, V. Laboratory Mechanical Parameters of Composite Resins and Their Relation to Fractures and Wear in Clinical Trials—A Systematic Review. Dent. Mater. 2017, 33, e101–e114. [Google Scholar] [CrossRef]
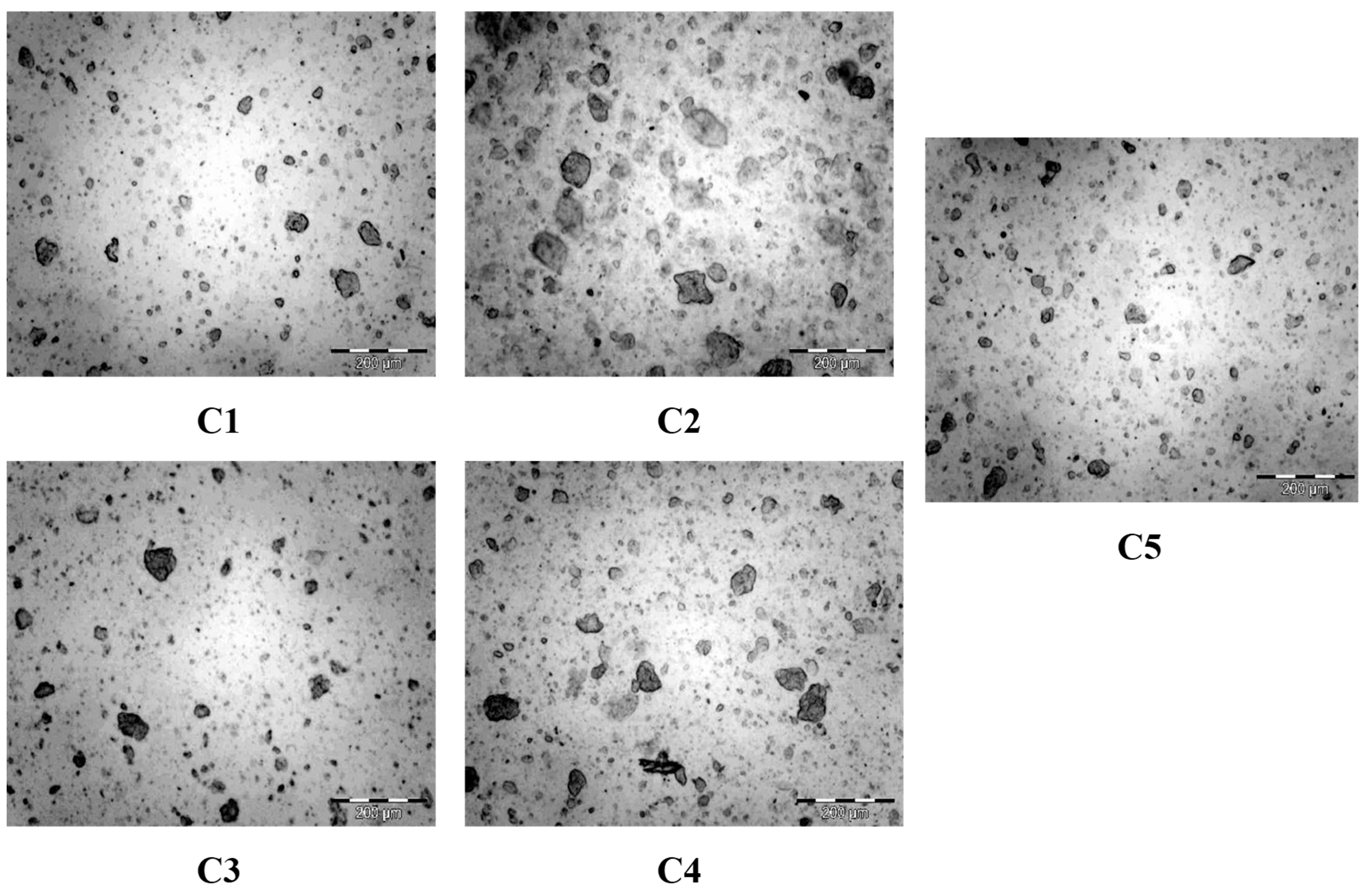
| Composite C1 | Handmade with the use of agate mortar. Small portions of silica were added every 2–5 min when it was noticed that the two components had already been properly combined and were becoming one. It took approximately 50 min to make this type of composite. |
| Composite C2 | Mixed with the use of the Hauschild SpeedMixer device (TM DAC 150 FVZ, Hauschild and Co., Hamm, Germany). Silica was progressively added to a precisely measured amount of resin. The mixing process in the device was initiated at the speed of 1500 RPM. Over approximately one hour, the speed was gradually increased until reaching a value of 3000 RPM, along with the complete filling of the measured resin with silica. |
| Composite C3 | Hybrid method. The process started with the use of a Hauschild SpeedMixer, (TM DAC 150 FVZ, Hauschild Engineering, Hamm, Germany) in which half of the silica was mixed with the resin. Then, this mixture was transferred to a mortar, where the remaining silica was further combined with the previously mixed material. Manual mixing of the material took about 30 min to achieve a complete integration of the components. |
| Composite C4 | Made with a Hauschild SpeedMixer (TM DAC 150 FVZ, Hauschild Engineering, Hamm, Germany) mixing device, with some modifications. For about an hour, silica was added to the resin in small portions, and the speed on the machine did not exceed 1500 RPM (every 7 min or so, starting at 1000 RPM, the speed was increased by 50 RPM). However, the last 1% of silica was added by hand in the mortar due to its failure to combine with the mixing machine. |
| Composite C5 | Modified hybrid method—mixed in the Hauschild SpeedMixer (TM DAC 150 FVZ, Hauschild Engineering, Hamm, Germany) device, then grated in a species mortar for 15 min. |
| HV [-] | FS [MPa] | Ef [MPa] | CS [MPa] | DTS [MPa] |
|---|---|---|---|---|
| C1 | ||||
| 31.9 ± 2.8 | 58.2 ± 8.0 * | 3156.7 ± 507.0 * | 301.2 ± 63.1 | 33.5 ± 4.5 |
| C2 | ||||
| 34.1 ± 2.3 * | 75.5 ± 10.4 * | 3738.3 ± 291.2 | 221.6 ± 50.9 | 30.2 ± 3.1 * |
| C3 | ||||
| 33.1 ± 1.8 | 65.9 ± 5.2 | 3076.7 ± 229.8 * | 195.2 ± 66.5 | 32.0 ± 3.9 |
| C4 | ||||
| 30.9 ± 1.5 * | 72.3 ± 5.6 | 3426.7 ± 394.2 | 281.2 ± 55.4 | 29.4 ± 4.1 |
| C5 | ||||
| 31.9 ± 3.1 | 58.2 ± 15.2 | 3596.7 ± 402.7 | 232.2 ± 55.6 | 27.1 ± 4.8 * |
| Type of Composite | σr [MPa] | σϴ [MPa] | σint [MPa] |
|---|---|---|---|
| C1 | 8.4 ± 0.6 | −9.8 ± 0.7 | 18.3 ± 1.3 |
| C2 | 11.4 ± 0.3 | −13.4 ± 0.6 | 24.8 ± 0.9 |
| C3 | 7.6 ± 1.1 | −9.1 ± 1.1 | 16.8 ± 2.2 |
| C4 | 9.6 ± 0.6 | −11.2 ± 0.6 | 20.8 ± 1.1 |
| C5 | 7.9 ± 1.1 | −9.5 ± 1.2 | 17.4 ± 2.3 |
| C1 | C2 | C3 | C4 | C5 | |
|---|---|---|---|---|---|
| Total number of objects | 1346 | 332 | 1753 | 391 | 1913 |
| Minimum value [μm] | 0.557 | 0.557 | 0.557 | 0.64 | 0.557 |
| Maximum value [μm] | 50.7 | 136 | 65.1 | 114 | 52.9 |
| Average value [μm] | 2.53 | 8.21 | 2.09 | 9.11 | 2.39 |
| Variability index [%] | 159 | 183 | 169 | 130 | 146 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zalega, M.; Krasowski, M.; Dawicka, O.; Jasińska, A.; Żabecka, A.; Kałuża, P.; Bociong, K. The Preparation of Experimental Resin-Based Dental Composites Using Different Mixing Methods for the Filler and Matrix. Processes 2025, 13, 1332. https://doi.org/10.3390/pr13051332
Zalega M, Krasowski M, Dawicka O, Jasińska A, Żabecka A, Kałuża P, Bociong K. The Preparation of Experimental Resin-Based Dental Composites Using Different Mixing Methods for the Filler and Matrix. Processes. 2025; 13(5):1332. https://doi.org/10.3390/pr13051332
Chicago/Turabian StyleZalega, Maja, Michał Krasowski, Olga Dawicka, Aleksandra Jasińska, Aleksandra Żabecka, Patrycja Kałuża, and Kinga Bociong. 2025. "The Preparation of Experimental Resin-Based Dental Composites Using Different Mixing Methods for the Filler and Matrix" Processes 13, no. 5: 1332. https://doi.org/10.3390/pr13051332
APA StyleZalega, M., Krasowski, M., Dawicka, O., Jasińska, A., Żabecka, A., Kałuża, P., & Bociong, K. (2025). The Preparation of Experimental Resin-Based Dental Composites Using Different Mixing Methods for the Filler and Matrix. Processes, 13(5), 1332. https://doi.org/10.3390/pr13051332








