Abstract
Background: The purpose of this review is to determine the association between the risk of preterm birth and low birth weight in newborns and periodontal disease in pregnant women. Methods: A bibliographic search was carried out until November 2021 in the following biomedical databases: PubMed/Medline, Cochrane Library, Scopus, EMBASE, Web of Science, Scielo, LILACS and Google Scholar. Studies reporting the association between the risk of preterm birth and low birth weight in newborns with periodontal disease in pregnant women, which were systematic reviews, in English and without time limits were included. AMSTAR-2 was used to assess the risk of the included studies, and the GRADEPro GDT tool was used to assess the quality of the evidence and the strength of the recommendation of the results. Results: The preliminary search yielded a total of 161 articles, discarding those that did not meet the selection criteria, leaving only 15 articles. Seven articles were entered into a meta-analysis, and it was found that there is an association between the risk of preterm birth and low birth weight in newborns with periodontal disease in pregnant women. Conclusions: There is an association between the risk of preterm birth and low birth weight in newborns with periodontal disease in pregnant women.
1. Introduction
Periodontal disease (PD) is caused by bacteria affecting the supporting structures of the tooth, causing inflammatory processes and the destruction of the periodontium, which can lead to tooth loss [1,2]. This disease is initiated and propagated by an interaction between an altered oral microflora and the host’s vulnerable immune system [3,4]. Gingivitis is the beginning of the disease and is generally due to the accumulation of dental biofilm due to poor oral hygiene. It is characterized by localized inflammation of the gum, which appears red and sometimes bleeding. If gingival disease is not treated, there is a risk that it will progress to chronic periodontitis [5].
This progression of bacterial infection leads to the severe destruction of the periodontium, causing tooth loss, which compromises chewing, aesthetics, self-confidence and quality of life [6]; it also contributes to systemic inflammation, with bacterial substances and inflammatory mediators capable of initiating and promoting systemic diseases [2,7]. The prevalence of PD has been reported to range from 20% to 50% worldwide [8]. There is evidence that PD is associated with heart disease, diabetes mellitus, chronic obstructive pulmonary disease, rheumatoid arthritis and adverse pregnancy outcomes [9].
The prevalence of PD is approximately 40% in pregnant mothers [10]. During pregnancy, due to hormonal factors (high levels of estrogen and progesterone), 50 to 70% of women develop gingivitis, being more vulnerable to PD than their nonpregnant peers [11].
Approximately 15 million premature babies are born each year in the world; these children, in addition, are usually born weighing less than 2500 g [12]. Premature babies or premature birth (PB) with low birth weight (LBW) are one of the leading causes of infant morbidity and mortality. Some risk factors that influence these adverse pregnancy outcomes are multiparity, low socioeconomic status, mother’s age, race, history of PB, maternal infectious processes and alcohol and drug abuse [13,14]. Although more than 60% of PBs occur in Africa and South Asia, preterm birth is a global problem [15].
PBs are a primary public health problem in both developed and developing countries. Despite improvements in obstetric care, preterm birth rates have not decreased in the last ten years [16,17,18].
Some studies have related the presence of PD during pregnancy with PB and/or LBW [19,20,21,22,23,24,25], and the evidence refers to an association of PD with adverse effects in pregnancy. Two pathogenic mechanisms are mentioned to explain the effect of PD on adverse pregnancy outcomes. Firstly, the periodontopathogenic bacteria that are found in the bacterial plaque of the gingiva due to a translocation phenomenon directly affect the fetus by bacteremia [15,26].
Likewise, the inflammatory mediators secreted in the subgingival inflammation zone (IL-1, L-6, IL-8, TNF-alpha, prostaglandin E2) come from the fetoplacental unit and produce an inflammatory reaction [27]. Mothers with PD have a high possibility of giving birth to a baby with LBW, prematurely or both in comparison with a pregnant woman with a healthy periodontium; therefore, they may have seven times the risk of having a PB or LBW baby [22,28]. Therefore, the early detection of PDs in pregnant women will help to prioritize the development of preventive and therapeutic interventions to decrease the occurrence of PBs and LBW newborns [29,30].
Given the relevance of this topic for public health, it is important that, through the analysis of systematic reviews with or without meta-analysis, results are produced that allow for more consistent conclusions to be reached. The main objective of this systematic review is to critically appraise the literature on the association between the risk of PB and LBW in newborns with PD in pregnant women.
2. Materials and Methods
2.1. Protocol and Registration
This systematic review followed a protocol defined by the authors according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [31]. This protocol has the registration number CRD42021290027 of the International Prospective Registry of Systematic Reviews (PROSPERO).
To prepare and structure this review, the focused question was formulated using the PICO format (population, intervention, outcomes and results) as detailed below:
- Population: pregnant women with PB and LBW;
- Intervention: pregnant women with PD;
- Comparison: pregnant woman without PD;
- Outcomes: association between PD and PB (<37 weeks) and LBW (<2500 gm) of the newborn.
2.2. Focused Question (PICO)
Is there an association between the risk of PB and LBW with PD in pregnant women?
2.3. Search and Selection of Studies
For the present systematic review, 8 electronic databases were reviewed (PubMed/Medline, Cochrane Library, Scopus, EMBASE, Web of Science, Scielo, LILACS and Google Scholar) until November 2021, combining keywords and subject titles according to the thesaurus of each database: “periodontal disease”, “periodontitis”, “gingivitis”, “preterm birth”, “low birth weight”, “perinatal outcomes”, “premature labor” and “adverse pregnancy outcomes”. The search strategies of each of the databases are presented in Table 1.

Table 1.
Search strategies for each database.
The electronic search was independent in the different databases and was carried out by 4 authors (H.A., T.P., L.C. and F.C.). The final decision for inclusion in the study required that articles be systematic reviews with or without meta-analysis, written in English, without time limits and reporting the association between the risk of PB and LBW with PD in pregnant women. Articles that were prospective studies and unpublished studies were excluded.
2.4. Data Extraction
For the extraction of data from the eligible studies, a predefined format was used that included the author(s), year of publication, type of study, type of studies included, number of studies included in the qualitative analysis, number of studies included in quantitative analysis, type of periodontal disease, main results, OR/RR and conclusions. Information was extracted independently by three investigators (V.M., S.C. and E.M.) and any disagreement was resolved by consulting the opinion of a fourth investigator.
2.5. Risk of Bias (RoB) Assessment
The RoB of the included studies was independently assessed by two calibrated authors (V.M. and T.P.) (k = 0.98) using AMSTAR-2, which is a critical appraisal tool for systematic reviews of health research studies [32], and all disagreements were resolved by discussion with a fourth reviewer (H.V.). According to this tool, a systematic review is evaluated in 16 domains with simple answer options: “yes” when the result is positive; “no” when the standard was not met or there is insufficient information to answer; and “if partial” in cases where there was partial adherence to the standard. They are then classified into four confidence levels: high, moderate, low and critically low.
2.6. Analysis of Results
Extracted data were analyzed in RevMan 5.3 (Cochrane Group, Londres, UK) by OR measurement in a fixed effects model with a 95% confidence interval. Additionally, a GRADE analysis was performed using the guideline development tool (GRADEPro GDT) (McMaster University and Evidence Prime Inc., Canada).
3. Results
3.1. Selection of Studies
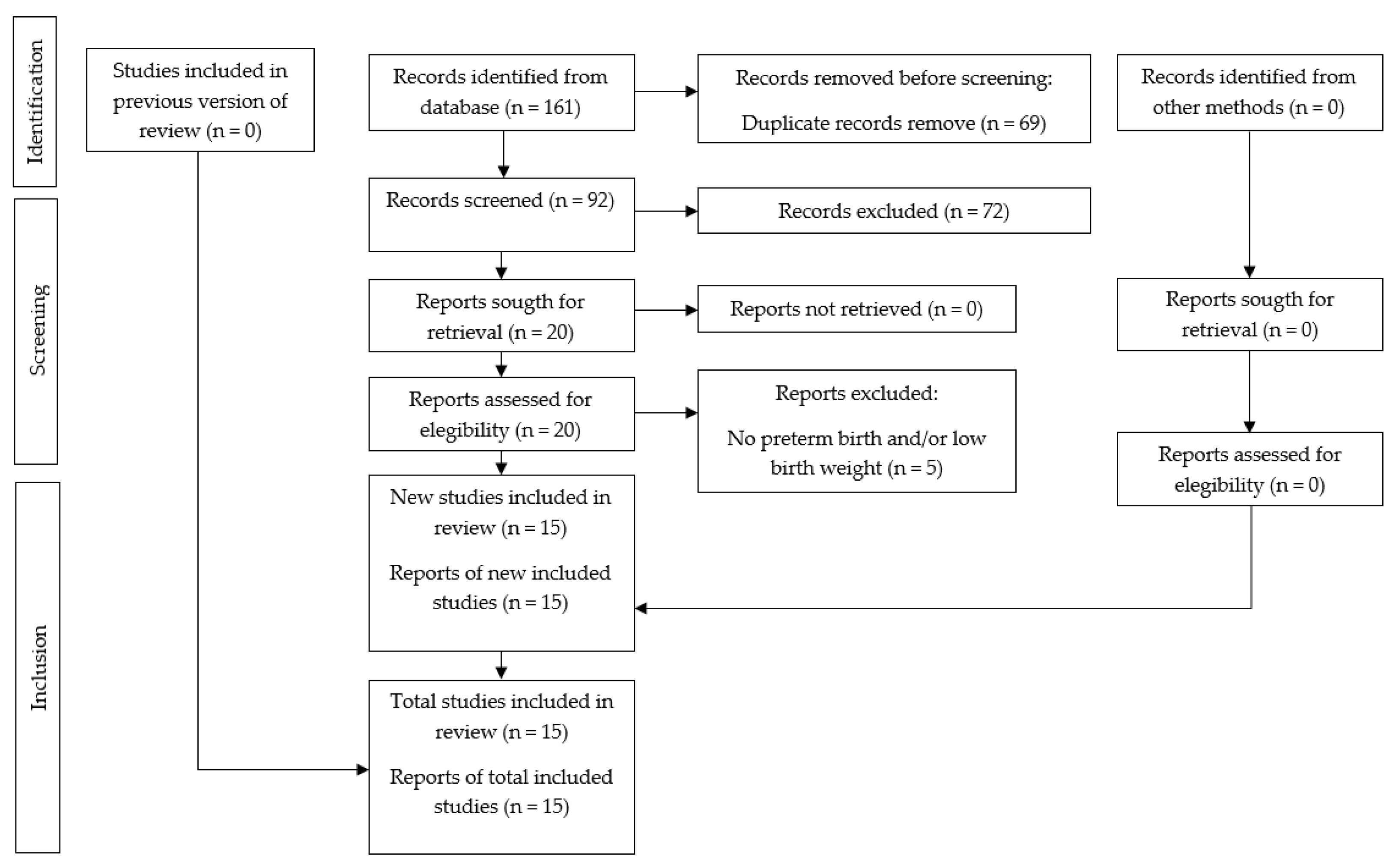
The strategy used was orientated through electronic and manual search with a total of 161 articles and 69 duplicates (Figure 1). After the selection of titles and abstracts, we chose 20 full-text articles. Then, five studies were excluded, resulting in 15 systematic reviews meeting the eligibility criteria for qualitative synthesis and seven for the quantitative analysis (meta-analysis). The reasons for the exclusion of the studies are found in Table 2.
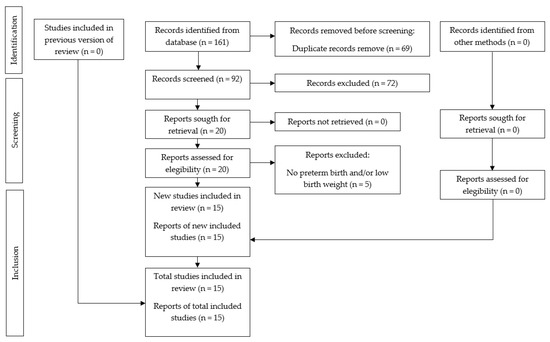
Figure 1.
PRISMA flowchart showing the process of inclusion and exclusion of studies in the systematic review.

Table 2.
Reason for exclusion of included studies.
3.2. Characteristics of the Included Studies
Overall, 15 systematic reviews were included [19,20,21,22,23,24,25,38,39,40,41,42,43,44,45], of which nine [19,20,23,38,39,40,41,42,45] had meta-analyses. The following is a list of the countries where the research was conducted: Brazil [25,38], Spain [19], Colombia [20], Indonesia [21], Ethiopia [22], Italy [23,39,45], United Kingdom [40], United States [24,41] and Jordan [42] (Table 3).

Table 3.
Characteristics of the included studies.
All the systematic reviews included studies of various types [19,20,21,22,23,24,25,38,39,40,41,42,43,44,45], such as case–control, cohort, cross-sectional and clinical trials. The number of studies included for qualitative and quantitative analysis ranged from five to thirty-six and from four to twenty-two, respectively. All the studies [19,20,21,22,23,24,25,38,39,40,41,42,43,44,45] evaluated PD, and four studies [21,22,38,44] had LBW as the main outcome, one study [20] PB, six studies [19,24,25,41,43,45] PB and LBW, one study [40] PB and PB with LBW and three studies [23,39,42] PB, LBW and PB with LBW (Table 3).
The composition of the studies with meta-analyses was [19,20,23,38,39,40,41,42,45] two studies [41,45] performed the meta-analysis based solely on clinical trials, five studies [20,23,38,40,42] took the odds ratio as a measure of association and three studies [19,39,40] took the relative risk as a measure of association. Only three studies [25,44,45] concluded that it was not possible to determine the association between PD with PB and LBW (Table 3).
3.3. Risk of Bias in the Analysis of the Studies
Eight studies [19,20,22,23,38,39,40,41] had a high overall confidence, five [21,24,25,43,44] had a moderate overall confidence and two [42,45] had a low overall confidence (Table 4).

Table 4.
Risk of bias in the analysis of the included studies.
3.4. Synthesis of the Results
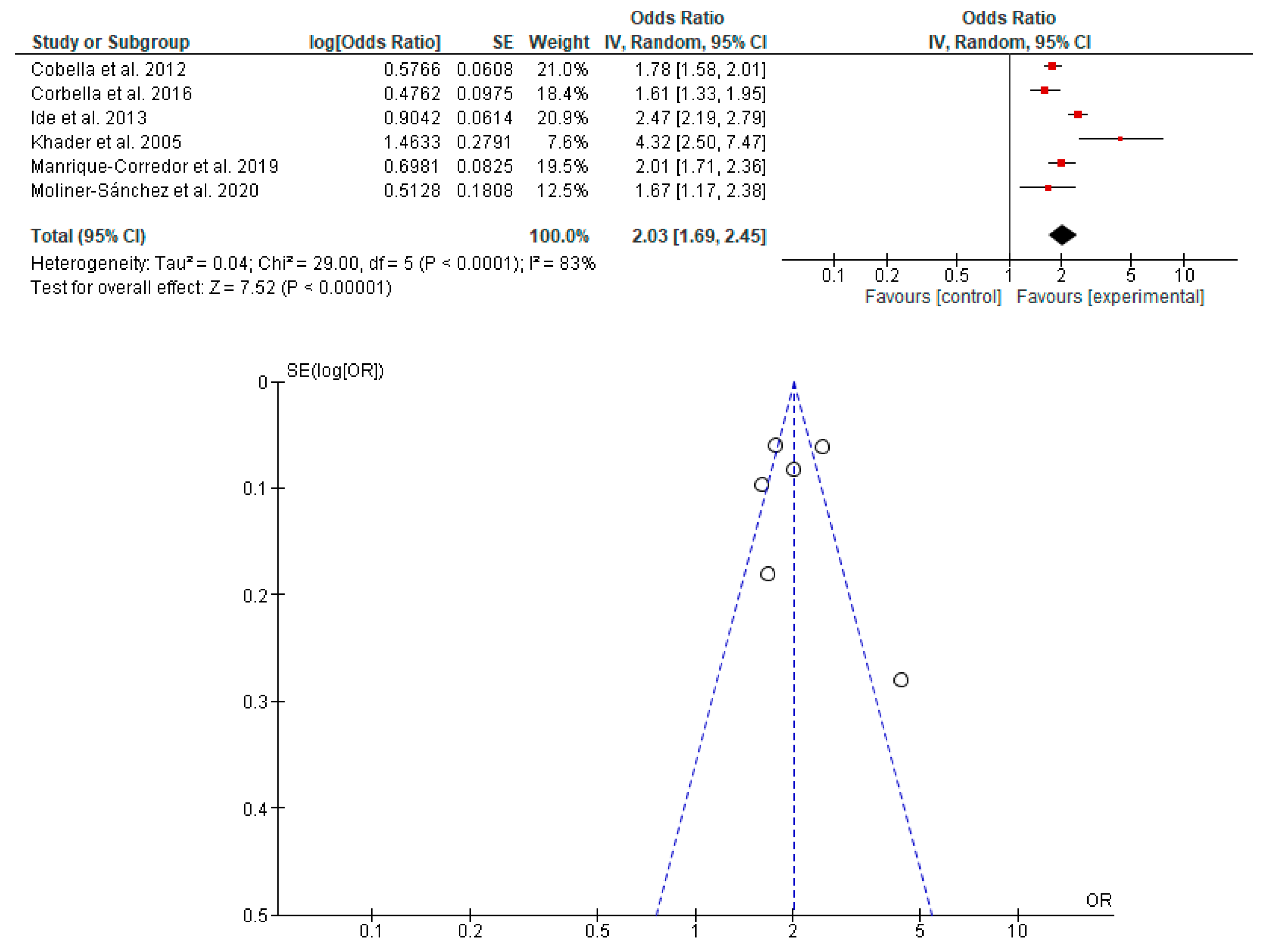
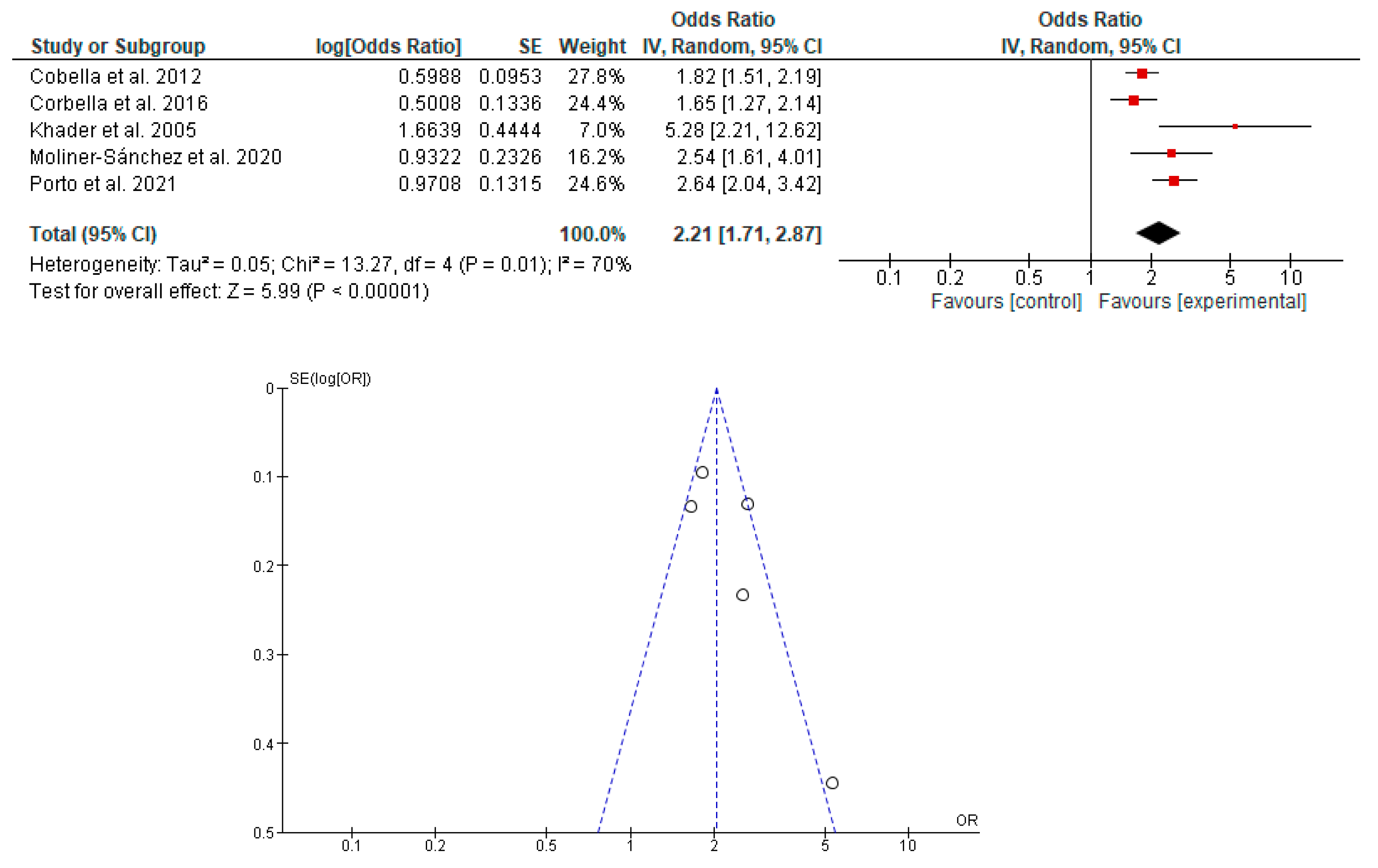
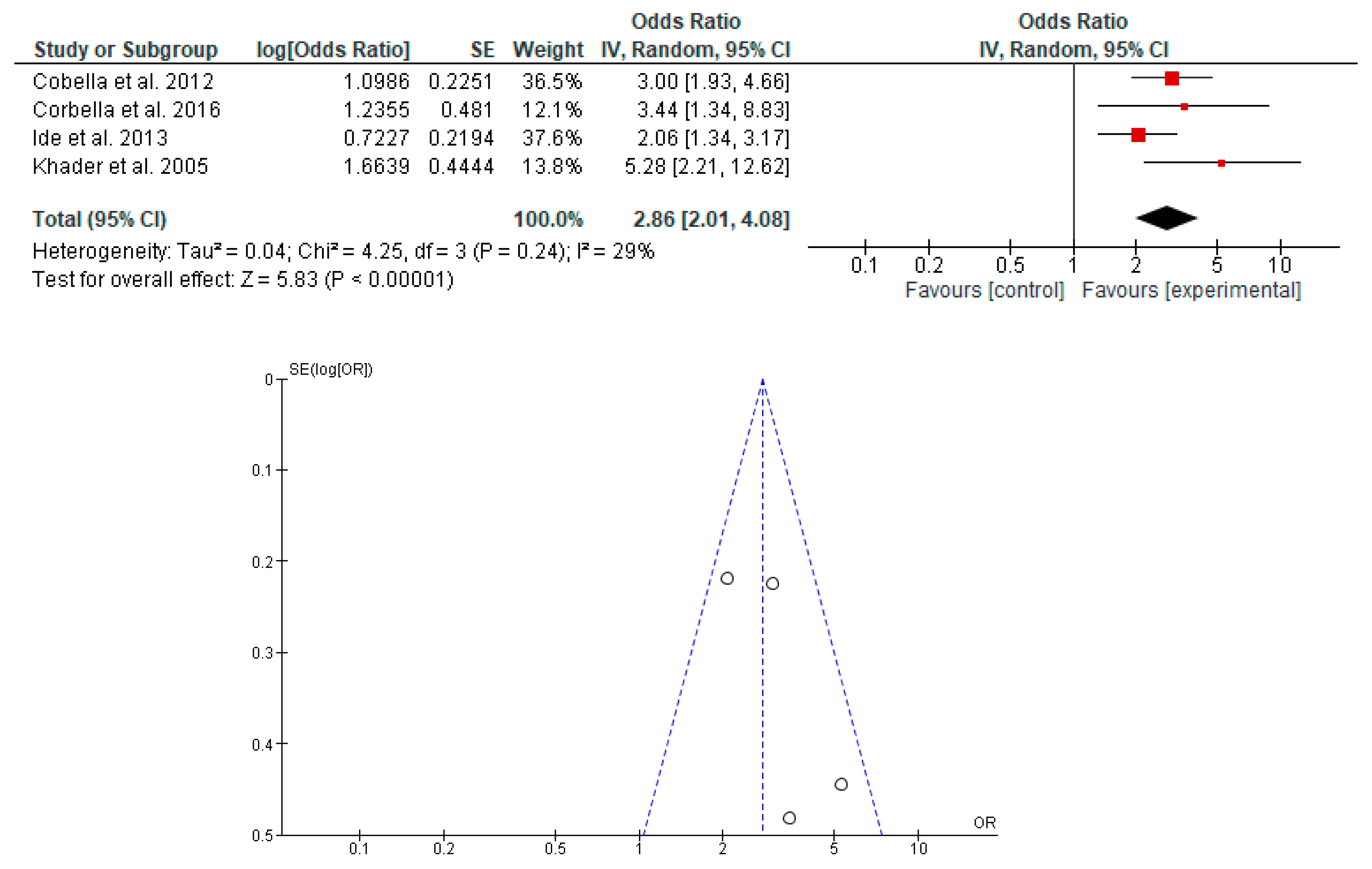
The association between the risk of PB and LBW in newborns with PD in pregnant women was determined in seven studies [19,20,23,38,39,40,42]. It was shown that PD in pregnant women is associated with the risk of PB, LBW and PB with LBW in newborns (Figure 2, Figure 3 and Figure 4).
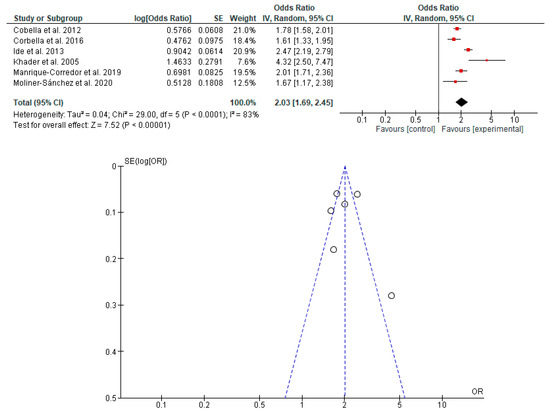
Figure 2.
Forest plot and funnel plot of the association between the risk of PB in newborns with PD in pregnant women.
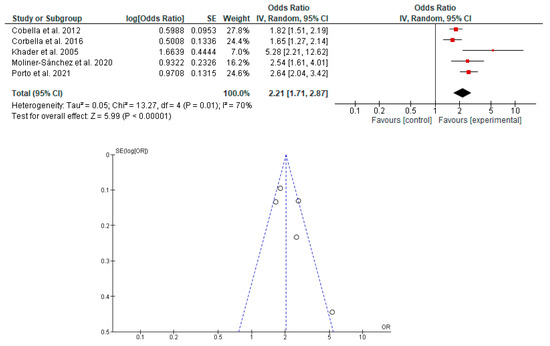
Figure 3.
Forest plot and funnel plot of the association between the risk of LBW in newborns with PD in pregnant women.
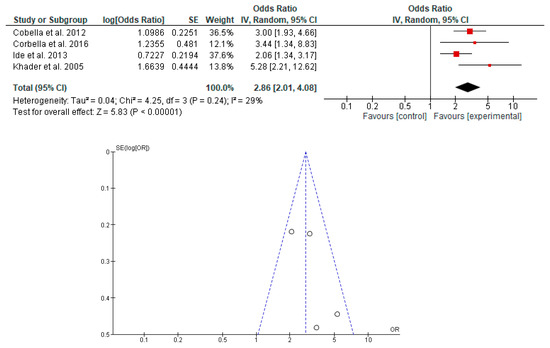
Figure 4.
Forest plot and funnel plot of the association between the risk of PB with LBW in newborns with PD in pregnant women.
3.5. GRADE Analysis
When evaluating the included studies, it was observed that there is low and moderate certainty in the association of PD in pregnant women with PB and LBW in newborns (Table 5).

Table 5.
GRADE analysis.
4. Discussion
Diagnoses, treatments and clinical decisions in dentistry must be based on the best available scientific evidence, which comes from systematic reviews.
One of the objectives is to analyze whether these systematic reviews had an optimal design and execution process. For this, the AMSTAR tool was developed, which was introduced for the first time in 2007 [32,46,47]. To increase the applicability of the AMSTAR tool, a group of experts made reviews and created the AMSTAR-2 tool [32,47], which was used in the present review.
The main problem found was that one of the studies [42] did not use an exhaustive literature search strategy, and another study [45] did not present the list of excluded studies. Several protocols, such as those found in Cochrane systematic reviews, recommend that authors provide lists of included and excluded articles, allowing the reader to easily judge the quality of the selected articles.
Additionally, some studies [21,24,25,43,44] did not meet certain points for high overall confidence; for example, they did not perform duplicate study selection and data extraction. These are important issues that authors of systematic reviews should pay attention to in the future.
In the present study, it was observed that there is an association between the risk of PB and LBW in newborns with PD in pregnant women. This may be due to inflammatory processes occurring at the placenta–fetus junction or elevated systemic inflammation in pregnant women or due to the translocation of periodontopathogenic bacteria to the uteroplacental circulation [48].
The World Health Organization (WHO) established, as one of its goals, the reduction in the incidence of PB and LBW of newborns given the great impact that these problems have on children’s morbidity and mortality indicators. In this sense, the efforts that health teams must make to reduce the incidence of PB and LBW of newborns not only aim to reduce maternal–fetal consequences but also the costs of hospitalization, use of units of intensive care, care and prevention in long-term health [49,50,51], as well as the implementation of preventive care protocols during the gestation period to reduce bacterial plaque rates from first care to subsequent visits [52]. Therefore, the authors emphasize the association found in this review so that the necessary public health measures can be taken.
However, this review has some limitations, such as the use of the AMSTAR-2 tool, which only considers the general confidence of the systematic reviews and their elements but does not describe this confidence in the studies included in each systematic review. In addition, the studies included in the systematic reviews that were able to determine the association between PD in pregnant women with PB and LBW had different study designs.
However, it has several important strengths, such as the fact that the present review cannot be compared with other previous studies since an umbrella review has not been previously carried out using the AMSTAR-2 tool. An exhaustive search of the scientific literature was carried out in the main bibliometric search engines, and a result was obtained based on systematic reviews with meta-analyses with high general confidence.
5. Conclusions
The systematic reviews included in the present study showed, in general, high confidence. In addition, there is an association between the risk of PB and LBW in newborns born and mothers with PD. A pregnant woman with PD is two to three times more likely to have a PB and a LBW.
Author Contributions
Conceptualization, T.P.-C. and H.I.A.-V.; methodology, T.P.-C. and H.I.A.-V.; software, L.C.-A.; validation, F.C.-O., V.M.-C. and S.C.-A.; formal analysis, E.M.-P.; investigation, S.P.; resources, T.P.-C.; data curation, H.V.-R.; writing—original draft preparation, T.P.-C. and H.I.A.-V.; writing—review and editing, L.C.-A.; visualization, P.C.-M.; supervision, H.I.A.-V.; project administration, T.P.-C.; funding acquisition, D.H.-A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Thomas, J.G.; Nakaishi, L.A. Managing the Complexity of a Dynamic Biofilm. J. Am. Dent. Assoc. 2006, 137, S10–S15. [Google Scholar] [CrossRef] [PubMed]
- Kinane, D.F.; Stathopoulou, P.G.; Papapanou, P.N. Periodontal Diseases. Nat. Rev. Dis. Prim. 2017, 3, 17038. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, E.M.; Reis, C.; Manzanares-Céspedes, M.C. Chronic Periodontitis, Inflammatory Cytokines, and Interrelationship with Other Chronic Diseases. Postgrad. Med. 2018, 130, 98–104. [Google Scholar] [CrossRef] [PubMed]
- Van Dyke, T.E.; Bartold, P.M.; Reynolds, E.C. The Nexus Between Periodontal Inflammation and Dysbiosis. Front. Immunol. 2020, 11, 511. [Google Scholar] [CrossRef]
- Kurgan, S.; Kantarci, A. Molecular Basis for Immunohistochemical and Inflammatory Changes during Progression of Gingivitis to Periodontitis. Periodontology 2000 2018, 76, 51–67. [Google Scholar] [CrossRef]
- Reynolds, I.; Duane, B. Periodontal Disease Has an Impact on Patients’ Quality of Life. Evid.-Based Dent. 2018, 19, 14–15. [Google Scholar] [CrossRef]
- Kane, S.F. The Effects of Oral Health on Systemic Health. Gen. Dent. 2017, 65, 30–34. [Google Scholar]
- Nazir, M.; Al-Ansari, A.; Al-Khalifa, K.; Alhareky, M.; Gaffar, B.; Almas, K. Global Prevalence of Periodontal Disease and Lack of Its Surveillance. Sci. World J. 2020, 2020, 2146160. [Google Scholar] [CrossRef]
- Nazir, M.A. Prevalence of Periodontal Disease, Its Association with Systemic Diseases and Prevention. Int. J. Health Sci. 2017, 1, 72–80. [Google Scholar] [CrossRef]
- Salih, Y.; Nasr, A.M.; Ahmed, A.B.A.; Sharif, M.E.; Adam, I. Prevalence of and Risk Factors for Periodontal Disease among Pregnant Women in an Antenatal Care Clinic in Khartoum, Sudan. BMC Res. Notes 2020, 13, 147. [Google Scholar] [CrossRef]
- Tettamanti, L.; Lauritano, D.; Nardone, M.; Gargari, M.; Silvestre-Rangil, J.; Gavoglio, P.; Tagliabue, A. Pregnancy and Periodontal Disease: Does Exist a Two-Way Relationship? ORAL Implantol. 2017, 10, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Andonova, I.; Iliev, V.; Živković, N.; Sušič, E.; Bego, I.; Kotevska, V. Can Oral Anaerobic Bacteria Cause Adverse Pregnancy Outcomes? Pril. (Makedon. Akad. Nauk. Umetnostite. Oddel. Med. Nauk.) 2015, 36, 137–143. [Google Scholar] [CrossRef]
- Zi, M.Y.H.; Longo, P.L.; Bueno-Silva, B.; Mayer, M.P.A. Mechanisms Involved in the Association between Periodontitis and Complications in Pregnancy. Front. Public Health 2015, 2, 290. [Google Scholar] [CrossRef]
- Romero, R.; Dey, S.K.; Fisher, S.J. Preterm Labor: One Syndrome, Many Causes. Science 2014, 345, 760–765. [Google Scholar] [CrossRef]
- Madianos, P.N.; Bobetsis, Y.A.; Offenbacher, S. Adverse Pregnancy Outcomes (APOs) and Periodontal Disease: Pathogenic Mechanisms. J. Clin. Periodontol. 2013, 40, 170–181. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhou, J.; Ma, Y.; Liu, L.; Xia, Q.; Fan, D.; Ai, W. Mode of Delivery and Preterm Birth in Subsequent Births: A Systematic Review and Meta-Analysis. PLoS ONE 2019, 14, e0213784. [Google Scholar] [CrossRef] [PubMed]
- Muchie, K.F.; Lakew, A.M.; Teshome, D.F.; Yenit, M.K.; Sisay, M.M.; Mekonnen, F.A.; Habitu, Y.A. Epidemiology of Preterm Birth in Ethiopia: Systematic Review and Meta-Analysis. BMC Pregnancy Childbirth 2020, 20, 574. [Google Scholar] [CrossRef]
- Chawanpaiboon, S.; Vogel, J.P.; Moller, A.-B.; Lumbiganon, P.; Petzold, M.; Hogan, D.; Landoulsi, S.; Jampathong, N.; Kongwattanakul, K.; Laopaiboon, M.; et al. Global, Regional, and National Estimates of Levels of Preterm Birth in 2014: A Systematic Review and Modelling Analysis. Lancet Glob. Health 2019, 7, e37–e46. [Google Scholar] [CrossRef]
- Moliner-Sánchez, C.A.; Iranzo-Cortés, J.E.; Almerich-Silla, J.M.; Bellot-Arcís, C.; Ortolá-Siscar, J.C.; Montiel-Company, J.M.; Almerich-Torres, T. Effect of per Capita Income on the Relationship between Periodontal Disease during Pregnancy and the Risk of Preterm Birth and Low Birth Weight Newborn. Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 8015. [Google Scholar] [CrossRef]
- Manrique-Corredor, E.; Orozco-Beltran, D.; Lopez-Pineda, A.; Quesada, J.; Gil-Guillen, V.; Carratala-Munuera, C. Maternal Periodontitis and Preterm Birth: Systematic Review and Meta-Analysis. Community Dent. Oral Epidemiol. 2019, 47, 243–251. [Google Scholar] [CrossRef]
- Syafar, I.F.; Tahir, H.; Oktawati, S. The Correlations between Periodontal Disease in the Woman with Pregnancy and Low Birth Weight Infant: A Systematic Review. Makassar Dent. J. 2019, 8, 178–184. [Google Scholar] [CrossRef]
- Teshome, A.; Yitayeh, A. Relationship between Periodontal Disease and Preterm Low Birth Weight: Systematic Review. Pan Afr. Med. J. 2016, 24, 215. [Google Scholar] [CrossRef]
- Corbella, S.; Taschieri, S.; Francetti, L.; De Siena, F.; Del Fabbro, M. Periodontal Disease as a Risk Factor for Adverse Pregnancy Outcomes: A Systematic Review and Meta-Analysis of Case-Control Studies. Odontology 2012, 100, 232–240. [Google Scholar] [CrossRef]
- Xiong, X.; Buekens, P.; Fraser, W.D.; Beck, J.; Offenbacher, S. Periodontal Disease and Adverse Pregnancy Outcomes: A Systematic Review. BJOG Int. J. Obstet. Gynaecol. 2006, 113, 135–143. [Google Scholar] [CrossRef]
- Vettore, M.V.; Lamarca, G.d.A.; Leão, A.T.T.; Thomaz, F.B.; Sheiham, A.; Leal, M.d.C. Periodontal Infection and Adverse Pregnancy Outcomes: A Systematic Review of Epidemiological Studies. Cad. Saude Publica 2006, 22, 2041–2053. [Google Scholar] [CrossRef]
- Komine-Aizawa, S.; Aizawa, S.; Hayakawa, S. Periodontal Diseases and Adverse Pregnancy Outcomes. J. Obstet. Gynaecol. Res. 2019, 45, 5–12. [Google Scholar] [CrossRef]
- Falcao, A.; Bullón, P. A Review of the Influence of Periodontal Treatment in Systemic Diseases. Periodontology 2000 2019, 79, 117–128. [Google Scholar] [CrossRef]
- Offenbacher, S.; Katz, V.; Fertik, G.; Collins, J.; Boyd, D.; Maynor, G.; McKaig, R.; Beck, J. Periodontal Infection as a Possible Risk Factor for Preterm Low Birth Weight. J. Periodontol. 1996, 67, 1103–1113. [Google Scholar] [CrossRef] [PubMed]
- Daalderop, L.A.; Wieland, B.V.; Tomsin, K.; Reyes, L.; Kramer, B.W.; Vanterpool, S.F.; Been, J.V. Periodontal Disease and Pregnancy Outcomes: Overview of Systematic Reviews. JDR Clin. Transl. Res. 2018, 3, 10–27. [Google Scholar] [CrossRef] [PubMed]
- Pockpa, Z.A.D.; Soueidan, A.; Koffi-Coulibaly, N.T.; Limam, A.; Badran, Z.; Struillou, X. Periodontal Diseases and Adverse Pregnancy Outcomes: Review of Two Decades of Clinical Research. Oral Health Prev. Dent. 2021, 19, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A Critical Appraisal Tool for Systematic Reviews That Include Randomised or Non-Randomised Studies of Healthcare Interventions, or Both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Bashir, S.; Menon, I.; Gupta, R.; Sharma, A.; Arora, V.; Varshney, S. Dental Considerations in Pregnancy—A Systematic Review. J. Pharm. Res. Int. 2021, 33, 82–100. [Google Scholar] [CrossRef]
- Gharehghani, M.; Bayani, A.; Bayat, A.; Hemmat, M.; Karimy, M.; Ahounbar, E.; Armoon, B.; Fakhri, Y.; Schroth, R. Poor Oral Health-Related Quality of Life among Pregnant Women: A Systematic Review and Meta-Analysis. Int. J. Dent. Hyg. 2021, 19, 39–49. [Google Scholar] [CrossRef]
- Konopka, T.; Zakrzewska, A. Periodontitis and Risk for Preeclampsia—A Systematic Review. Ginekol. Pol. 2020, 91, 158–164. [Google Scholar] [CrossRef]
- Abariga, S.; Whitcomb, B. Periodontitis and Gestational Diabetes Mellitus: A Systematic Review and Meta-Analysis of Observational Studies. BMC Pregnancy Childbirth 2016, 16, 344. [Google Scholar] [CrossRef]
- Kunnen, A.; van Doormaal, J.; Abbas, F.; Aarnoudse, J.; van Pampus, M.; Faas, M. Periodontal Disease and Pre-Eclampsia: A Systematic Review. J. Clin. Periodontol. 2010, 37, 1075–1087. [Google Scholar] [CrossRef]
- Porto, E.; Gomes, I.; Batista, J.; Lyrio, A.; Souza, E.; Figueiredo, A.; Pereira, M.; da Cruz, S. Maternal periodontitis and low birth weight: Systematic review and meta-analysis. Cienc. Saude Coletiva 2021, 26, 5383–5392. [Google Scholar] [CrossRef]
- Corbella, S.; Taschieri, S.; Del Fabbro, M.; Francetti, L.; Weinstein, R.; Ferrazzi, E. Adverse Pregnancy Outcomes and Periodontitis: A Systematic Review and Meta-Analysis Exploring Potential Association. Quintessence Int. 2016, 47, 193–204. [Google Scholar] [CrossRef]
- Ide, M.; Papapanou, P.N. Epidemiology of Association between Maternal Periodontal Disease and Adverse Pregnancy Outcomes-Systematic Review. J. Clin. Periodontol. 2013, 40, S181–S194. [Google Scholar] [CrossRef]
- Xiong, X.; Buekens, P.; Vastardis, S.; Yu, S.M. Periodontal Disease and Pregnancy Outcomes: State-of-the-Science. Obstet. Gynecol. Surv. 2007, 62, 605–615. [Google Scholar] [CrossRef] [PubMed]
- Khader, Y.S.; Ta’ani, Q. Periodontal Diseases and the Risk of Preterm Birth and Low Birth Weight: A Meta-Analysis. J. Periodontol. 2005, 76, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Scannapieco, F.A.; Bush, R.B.; Paju, S. Periodontal Disease as a Risk Factor for Adverse Pregnancy Outcomes. A Systematic Review. Ann. Periodontol. 2003, 8, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Madianos, P.N.; Bobetsis, G.A.; Kinane, D.F. Is Periodontitis Associated with an Increased Risk of Coronary Heart Disease and Preterm and/or Low Birth Weight Births? J. Clin. Periodontol. 2002, 29, 22–36. [Google Scholar] [CrossRef]
- Corbella, S.; Del Fabbro, M.; Taschieri, S.; Francetti, L. Periodontal Disease and Adverse Pregnancy Outcomes: A Systematic Review. Ital. Oral Surg. 2012, 11, 132–146. [Google Scholar] [CrossRef]
- Natto, Z.S.; Hameedaldain, A. Methodological Quality Assessment of Meta-Analyses and Systematic Reviews of the Relationship Between Periodontal and Systemic Diseases. J. Evid. Based Dent. Pract. 2019, 19, 131–139. [Google Scholar] [CrossRef]
- Chugh, A.; Patnana, A.K.; Kumar, P.; Chugh, V.K.; Khera, D.; Singh, S. Critical Analysis of Methodological Quality of Systematic Reviews and Meta-Analysis of Antibiotics in Third Molar Surgeries Using AMSTAR 2. J. Oral Biol. Craniofacial Res. 2020, 10, 441–449. [Google Scholar] [CrossRef]
- Radochova, V.; Stepan, M.; Kacerovska Musilova, I.; Slezak, R.; Vescicik, P.; Menon, R.; Jacobsson, B.; Kacerovsky, M. Association between Periodontal Disease and Preterm Prelabour Rupture of Membranes. J. Clin. Periodontol. 2019, 46, 189–196. [Google Scholar] [CrossRef]
- Luna, M.C.; Cubides Munevar, A.M.; Ruiz Melo, C.F.; Alonso, S.V.; Pinzón, E.M.; Gullozo, L.; Luna, M.C.; Cubides Munevar, A.M.; Ruiz Melo, C.F.; Alonso, S.V.; et al. Asociación Entre Bajo Peso al Nacer y Parto Pretermino En Gestantes Con Signos de Enfermedad Periodontal Atendidas En Una Institución Del Nivel Primario de Salud Del Valle Del Cauca-Colombia. Rev. Chil. Obstet. Ginecol. 2019, 84, 103–111. [Google Scholar] [CrossRef]
- World Health Organization. Global Nutrition Targets 2025: Low Birth Weight Policy Brief. Available online: https://www.who.int/publications-detail-redirect/WHO-NMH-NHD-14.5 (accessed on 3 January 2022).
- World Health Organization. Nacimientos Prematuros. Available online: https://www.who.int/es/news-room/fact-sheets/detail/preterm-birth (accessed on 3 January 2022).
- Maspero, C.; Fama, A.; Giannini, L.; Galbiati, G.; Batia, S.; Farronato, M. Preventive Hygiene Protocol of University of Milan for Women during Pregnancy: A Qualitative and Quantitative Bacterial Plaque Analysis Prospective Original Study. Saudi Dent. J. 2020, 32, 29–35. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).