Development and Comparison of Conventional and 3D-Printed Laboratory Models of Maxillary Defects
Abstract
:1. Introduction
- Class I: Midline resection
- Class II: Unilateral resection
- Class III: Central palate resection
- Class IV: Bilateral anteroposterior resection
- Class V: Posterior resection
- Class VI: Anterior resection
2. Materials and Methods
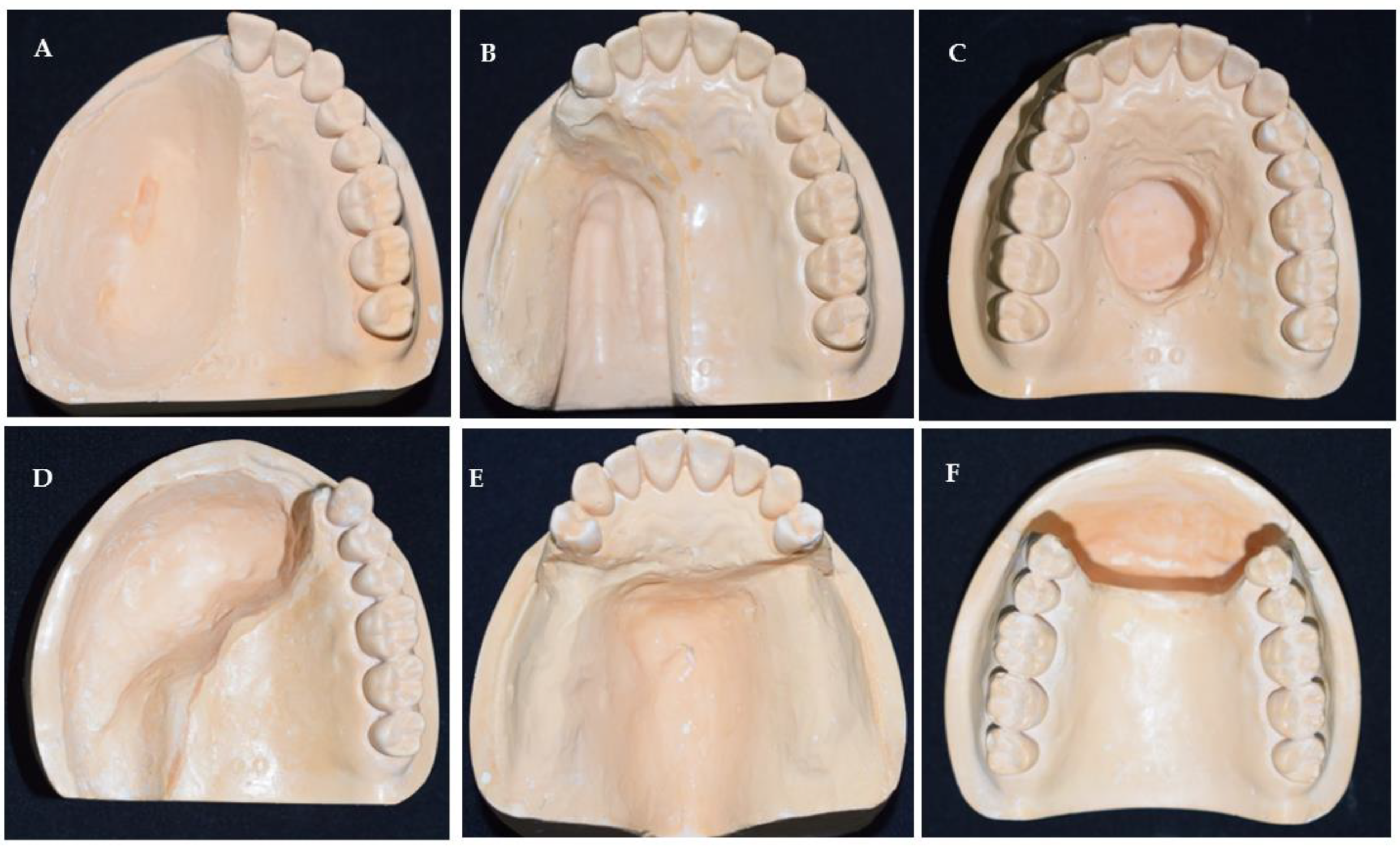
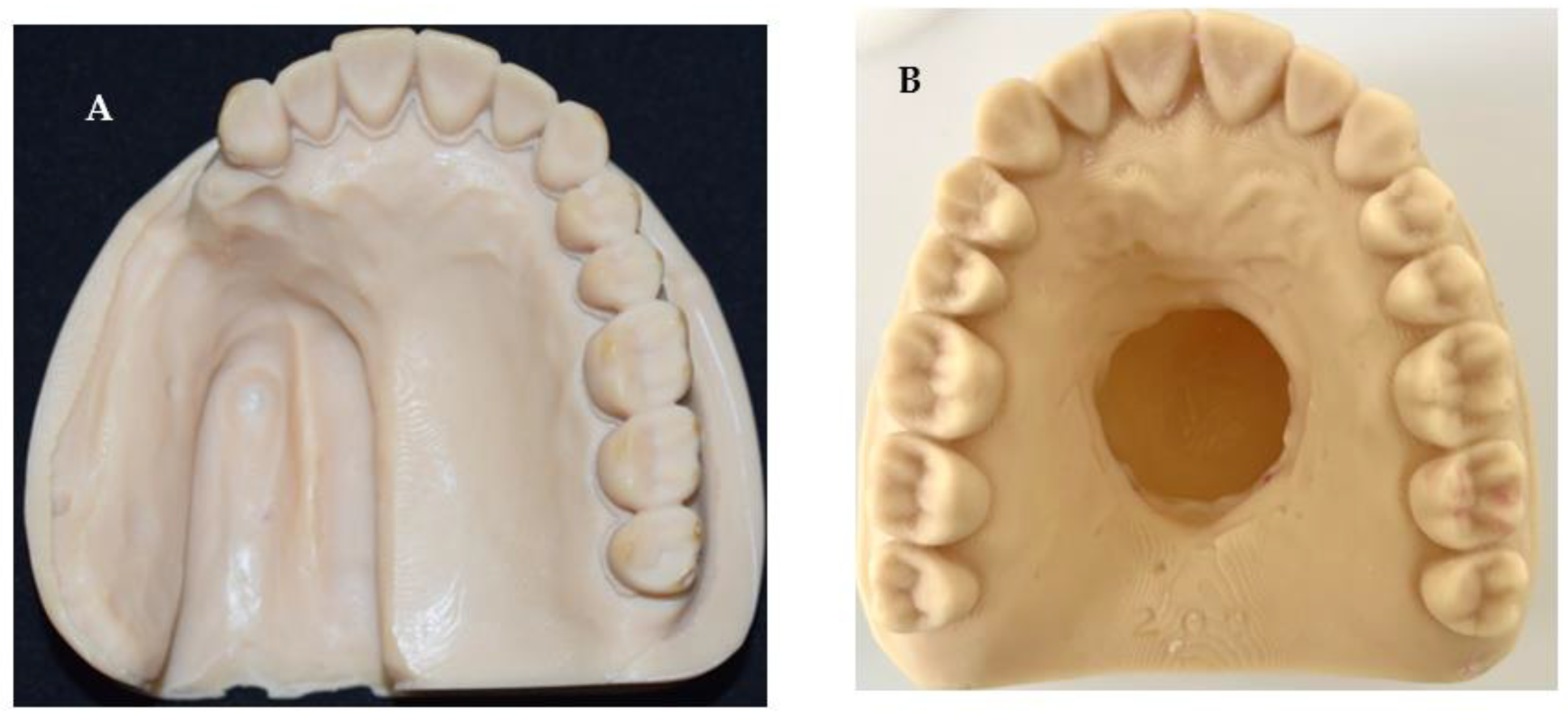
2.1. Defect Model Fabrication
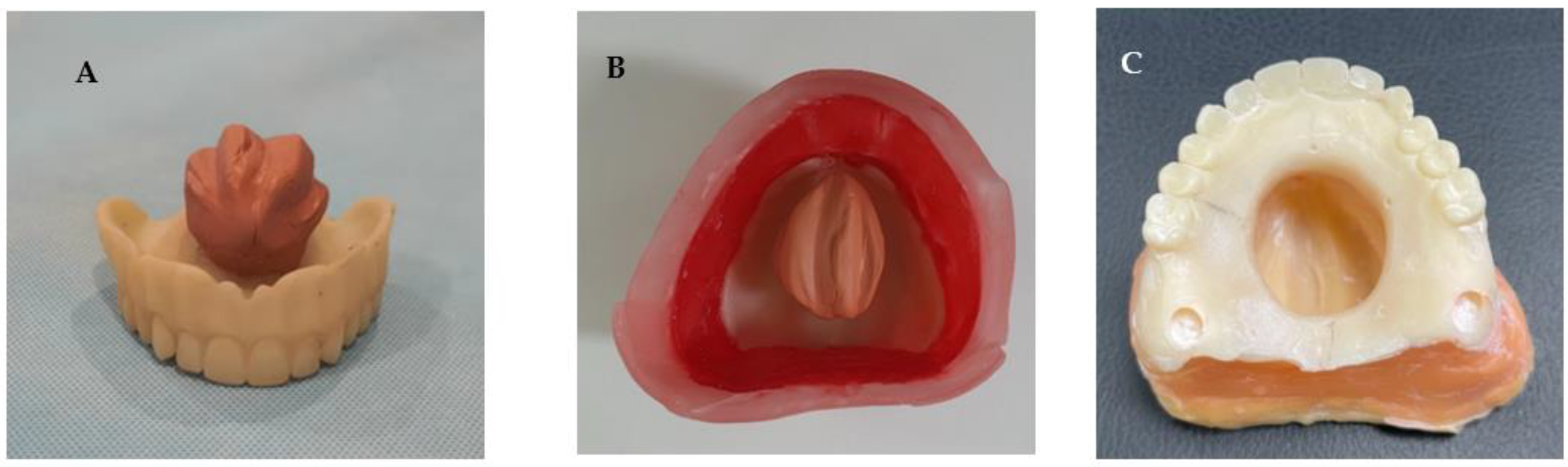
2.2. Sample Fabrication for Comparison Experiments
2.2.1. Conventional Impression Technique
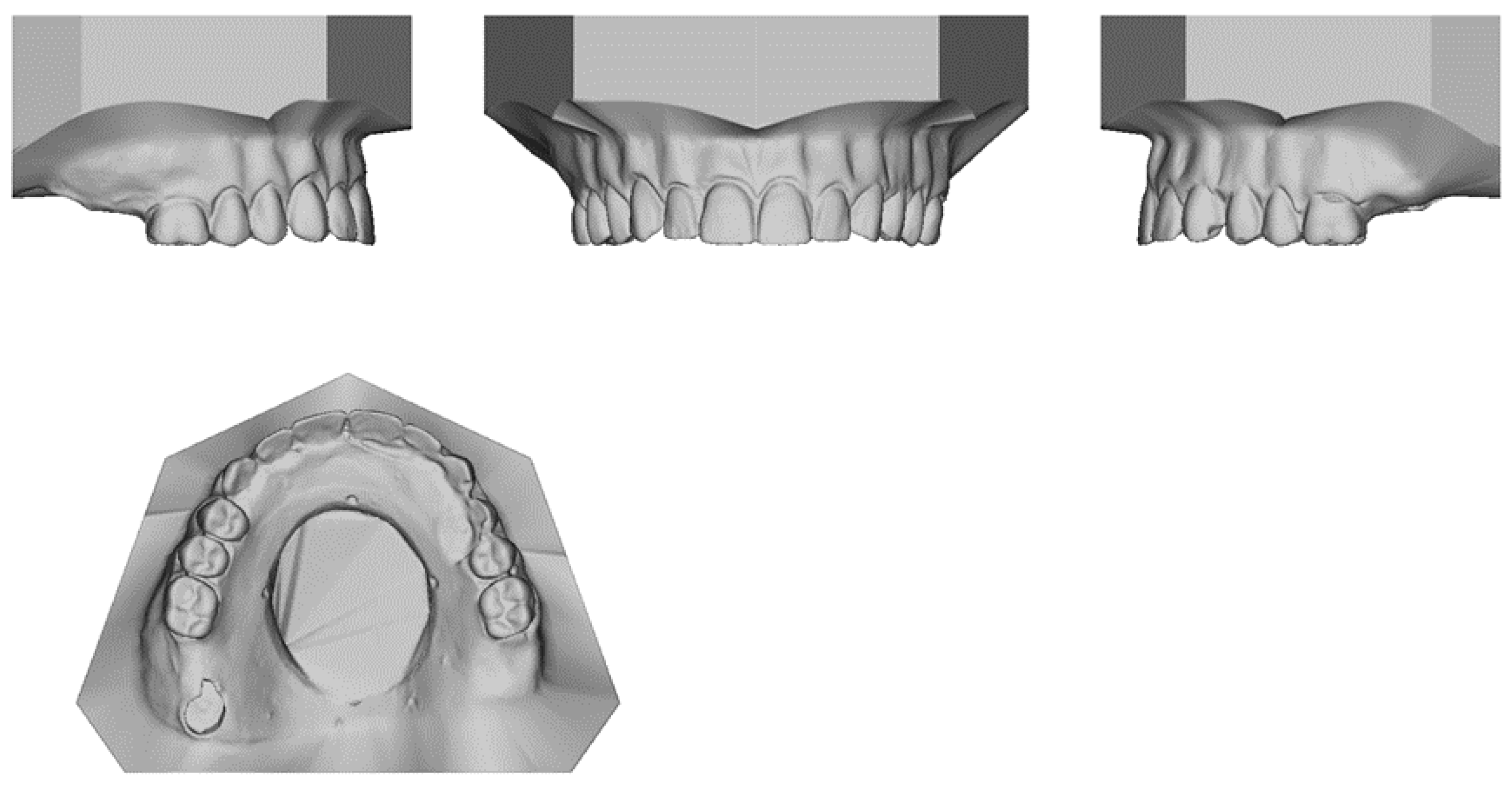
2.2.2. Digital Technique
2.3. Measurement Collection
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Oh, W.S.; Roumanas, E. Alternate technique for fabrication of a custom impression tray for definitive obturator construction. J. Prosthet. Dent. 2006, 95, 473–475. [Google Scholar] [CrossRef]
- Colvenkar, S.S. Sectional impression tray and sectional denture for a microstomia patient. J. Prosthodont. Implant Esthet. Reconstr. Dent. 2010, 19, 161–165. [Google Scholar] [CrossRef]
- Chen, C.; Ren, W.; Gao, L.; Cheng, Z.; Zhang, L.; Li, S.; Zhi, P.K.-q. Function of obturator prosthesis after maxillectomy and prosthetic obturator rehabilitation. Braz. J. Otorhinolaryngol. 2016, 82, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Kornblith, A.B.; Zlotolow, I.M.; Gooen, J.; Huryn, J.M.; Lerner, T.; Strong, E.W.; Shah, J.P.; Spiro, R.H.; Holland, J.C. Quality of life of maxillectomy patients using an obturator prosthesis. Head Neck J. Sci. Spec. Head Neck 1996, 18, 323–334. [Google Scholar] [CrossRef]
- Moharamzadeh, K. Diseases and Conditions in Dentistry: An Evidence-Based Reference; John Wiley & Sons: Hoboken, NJ, USA, 2018. [Google Scholar]
- Brown, J.S.; Shaw, R.J. Reconstruction of the maxilla and midface: Introducing a new classification. Lancet Oncol. 2010, 11, 1001–1008. [Google Scholar] [CrossRef]
- Aramany, M.A. Basic principles of obturator design for partially edentulous patients. Part II: Design principles. J. Prosthet. Dent. 1978, 40, 656–662. [Google Scholar] [CrossRef] [PubMed]
- Dalkiz, M.; Dalkiz, A.S. The effect of immediate obturator reconstruction after radical maxillary resections on speech and other functions. Dent. J. 2018, 6, 22. [Google Scholar] [CrossRef] [PubMed]
- The Glossary of Prosthodontic Terms: Ninth Edition. J. Prosthet. Dent. 2017, 117, e1–e105. [CrossRef] [PubMed]
- Ali, M.M.; Khalifa, N.; Alhajj, M.N. Quality of life and problems associated with obturators of patients with maxillectomies. Head Face Med. 2018, 14, 2. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.W.; King, G.E.; Kramer, D.C.; Rambach, S.C. Use of an interim obturator for definitive prosthesis fabrication. J. Prosthet. Dent. 1984, 51, 527–528. [Google Scholar] [CrossRef]
- Wolfaardt, J.F. Modifying a surgical obturator prosthesis into a interim obturator prosthesis. A clinical report. J. Prosthet. Dent. 1989, 62, 619–621. [Google Scholar] [CrossRef] [PubMed]
- Hegedus, T.; Kreuter, P.; Kismarczi-Antalffy, A.A.; Demeter, T.; Banyai, D.; Vegh, A.; Geczi, Z.; Hermann, P.; Payer, M.; Zsembery, A.; et al. User Experience and Sustainability of 3D Printing in Dentistry. Int. J. Env. Res. Public Health 2022, 19, 1921. [Google Scholar] [CrossRef] [PubMed]
- Tiwana, K.K.; Morton, T.; Tiwana, P.S. Aspiration and ingestion in dental practice: A 10-year institutional review. J. Am. Dent. Assoc. 2004, 135, 1287–1291. [Google Scholar] [CrossRef]
- Cameron, S.M.; Whitlock, W.L.; Tabor, M.S. Foreign body aspiration in dentistry: A review. J. Am. Dent. Assoc. 1996, 127, 1224–1229. [Google Scholar] [CrossRef] [PubMed]
- Jiao, T.; Zhu, C.; Dong, X.; Gu, X. Rehabilitation of maxillectomy defects with obturator prostheses fabricated using computer-aided design and rapid prototyping: A pilot study. Int. J. Prosthodont. 2014, 27, 480–486. [Google Scholar] [CrossRef]
- Huang, Z.; Wang, X.Z.; Hou, Y.Z. Novel method of fabricating individual trays for maxillectomy patients by computer-aided design and rapid prototyping. J. Prosthodont. 2015, 24, 115–120. [Google Scholar] [CrossRef]
- Choudhury, M.; Shanmuganathan, N.; Padmanabhan, T.; Swarup, S.; Grover, M.; Arumugam, M. Rehabilitation of Post Surgical Maxillectomy Defects Using Interim Obturators—A Case Series. Indian J. Surg. Oncol. 2014, 5, 315–320. [Google Scholar] [CrossRef]
- Chellappa, L.R.; Prabakar, J.; Indiran, M.A. Knowledge, Attitude And Practice Regarding Tooth Jewellery Among Dental Students And Dental Professionals In Chennai-A Cross Sectional Study. Int. J. Pharm. Res. 2020, 12. [Google Scholar] [CrossRef]
- Butterworth, C. The prosthodontic management of the maxillectomy patient. Br. Dent. J. 2022, 233, 744–748. [Google Scholar] [CrossRef]
- Rogers, S.N.; Adatia, A.; Hackett, S.; Boscarino, A.; Patel, A.; Lowe, D.; Butterworth, C.J. Changing trends in the microvascular reconstruction and oral rehabilitation following maxillary cancer. Eur. Arch. Otorhinolaryngol. 2022, 279, 4113–4126. [Google Scholar] [CrossRef]
- Bidra, A.S.; Jacob, R.F.; Taylor, T.D. Classification of maxillectomy defects: A systematic review and criteria necessary for a universal description. J. Prosthet. Dent. 2012, 107, 261–270. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Jamjoom, F.Z.; Le, T.; Radics, A.; Gallucci, G.O. A clinical study comparing digital scanning and conventional impression making for implant-supported prostheses: A crossover clinical trial. J. Prosthet. Dent. 2022, 128, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Marti, A.M.; Harris, B.T.; Metz, M.J.; Morton, D.; Scarfe, W.C.; Metz, C.J.; Lin, W.S. Comparison of digital scanning and polyvinyl siloxane impression techniques by dental students: Instructional efficiency and attitudes towards technology. Eur. J. Dent. Educ. 2017, 21, 200–205. [Google Scholar] [CrossRef]
- Giachetti, L.; Sarti, C.; Cinelli, F.; Russo, D.S. Accuracy of Digital Impressions in Fixed Prosthodontics: A Systematic Review of Clinical Studies. Int. J. Prosthodont. 2020, 33, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Rasaie, V.; Abduo, J.; Hashemi, S. Accuracy of Intraoral Scanners for Recording the Denture Bearing Areas: A Systematic Review. J. Prosthodont. 2021, 30, 520–539. [Google Scholar] [CrossRef]
- Costa-Palau, S.; Torrents-Nicolas, J.; Brufau-de Barberà, M.; Cabratosa-Termes, J. Use of polyetheretherketone in the fabrication of a maxillary obturator prosthesis: A clinical report. J. Prosthet. Dent. 2014, 112, 680–682. [Google Scholar] [CrossRef] [PubMed]
- Tannous, F.; Steiner, M.; Shahin, R.; Kern, M. Retentive forces and fatigue resistance of thermoplastic resin clasps. Dent. Mater. 2012, 28, 273–278. [Google Scholar] [CrossRef]
- Ye, H.; Wang, Z.; Sun, Y.; Zhou, Y. Fully digital workflow for the design and manufacture of prostheses for maxillectomy defects. J. Prosthet. Dent. 2021, 126, 257–261. [Google Scholar] [CrossRef]
- Tasopoulos, T.; Chatziemmanouil, D.; Karaiskou, G.; Kouveliotis, G.; Wang, J.; Zoidis, P. Fabrication of a 3D-printed interim obturator prosthesis: A contemporary approach. J. Prosthet. Dent. 2019, 121, 960–963. [Google Scholar] [CrossRef]




| Conventional | Digital | |
|---|---|---|
| Items | Mean (SD) | Mean (SD) |
| Time per second | 3688.6 (37.85) | 3707 (139.48) |
| AP measure (mm) | 32.03 (0.24) | 32.83(0.11) |
| Lateral measure (mm) | 25.85 (0.09) | 26.58 (0.11) |
| Conventional | Digital | ||||
|---|---|---|---|---|---|
| Case | N | Mean (SD) | CV | Mean (SD) | CV |
| C1 | 5 | 741.8 (1102.24) | 1.49 | 1119.4 (934.55) | 1.04 |
| C2 | 5 | 738.4 (1103.19) | 1.49 | 1138.6 (982.13) | 1.08 |
| C3 | 5 | 747 (1099.89) | 1.47 | 1160 (955.09) | 1.00 |
| C4 | 5 | 727 (1108.54) | 1.52 | 1134 (925.25) | 0.99 |
| C5 | 5 | 734.4 (1104.35) | 1.50 | 1089.2 (856.70) | 0.94 |
| Conventional | Digital | ||||
|---|---|---|---|---|---|
| Measurement | Standard | Mean (SD) | p-Value | Mean (SD) | p-Value |
| AP measurement | 32.55 | 32.03(0.24) | 0.008 | 32.83(0.11) | 0.005 |
| Lateral measurement | 26.54 | 25.85(0.09) | <0.001 | 26.58 (0.11) | 0.435 |
| Means | SD | 95% CI of Difference | p-Value | ||
|---|---|---|---|---|---|
| Pairs | Upper | Lower | |||
| AP-conventional-AP-digital | −0.80 | 0.22 | −0.52 | −1.08 | 0.001 |
| Lateral-conventional-Lateral-digital | −0.73 | 0.09 | −0.62 | −0.84 | <0.001 |
| Total time conventional-Total time digital | −18.60 | 127.54 | 139.76 | −176.96 | 0.761 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alanezi, A.; Aljanahi, M.; Moharamzadeh, K.; Ghoneima, A.; Tawfik, A.R.; Khamis, A.H.; Abuzayeda, M. Development and Comparison of Conventional and 3D-Printed Laboratory Models of Maxillary Defects. Dent. J. 2023, 11, 115. https://doi.org/10.3390/dj11050115
Alanezi A, Aljanahi M, Moharamzadeh K, Ghoneima A, Tawfik AR, Khamis AH, Abuzayeda M. Development and Comparison of Conventional and 3D-Printed Laboratory Models of Maxillary Defects. Dentistry Journal. 2023; 11(5):115. https://doi.org/10.3390/dj11050115
Chicago/Turabian StyleAlanezi, Ahmad, May Aljanahi, Keyvan Moharamzadeh, Ahmed Ghoneima, Abdel Rahman Tawfik, Amar Hassan Khamis, and Moosa Abuzayeda. 2023. "Development and Comparison of Conventional and 3D-Printed Laboratory Models of Maxillary Defects" Dentistry Journal 11, no. 5: 115. https://doi.org/10.3390/dj11050115
APA StyleAlanezi, A., Aljanahi, M., Moharamzadeh, K., Ghoneima, A., Tawfik, A. R., Khamis, A. H., & Abuzayeda, M. (2023). Development and Comparison of Conventional and 3D-Printed Laboratory Models of Maxillary Defects. Dentistry Journal, 11(5), 115. https://doi.org/10.3390/dj11050115








