Impact of Printing Orientation on the Accuracy of Additively Fabricated Denture Base Materials: A Systematic Review
Abstract
:1. Introduction
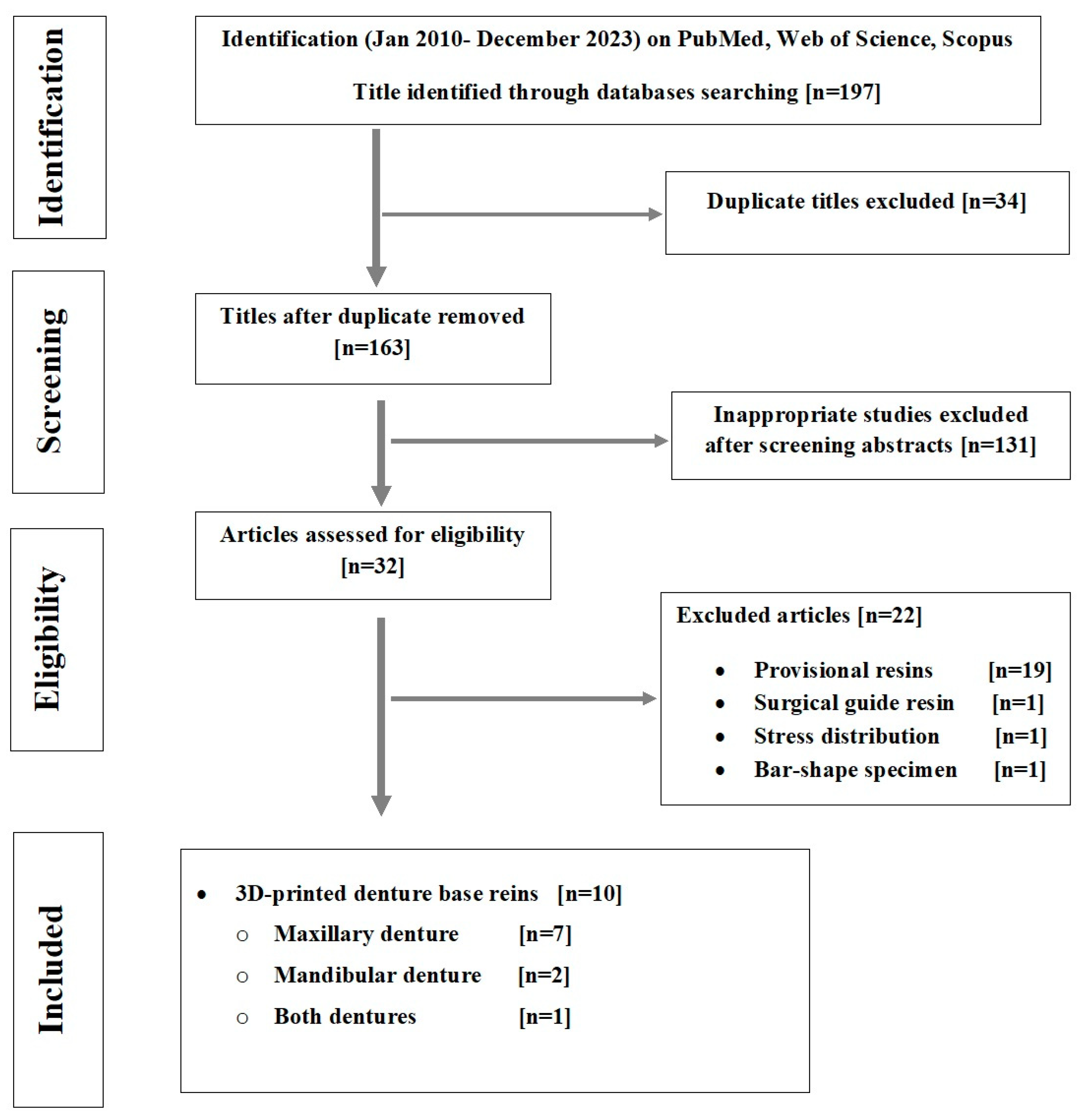
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Study Selection and Data Extraction
2.3. Quality Assessment of Included Studies
| Author/ Year/ Specimens | Printers and Technology | Specimens Configuration/ Sample Size | Orientations | Layer Thickness | Supports Position | Post-Curing Conditions | Scanners | Measurement Method/Unit | Reference Model | Software | Main Finding and Recommendations |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Jin et al., 2018 [27] | NextDent Base; NextDent Printer (Bio3D W11; NextDent) DLP | Maxillary and mandibular denture base/with tooth sockets and without teeth (n = 10) N = 40 | 90°, 100°, 135°, 150° | 100 µm | Cameo surfaces | LC 3DPrint Box; NextDent 15 min Temp. According to manufacturer instructions (no info) | Lab scanner (Identica Blue T500; Medit) used to detect 10 µm differences | Superimposed/ RMSE, PA, and NA/mm | Reference cast | Geomagic Control X; 3D Systems | No significant effect of printing angle on tissue surface adaptations |
| Hada et al. 2020 [28] | Clear resin; Formlabs Printer: Form 2; Formlabs SLA | Maxillary denture base/with tooth sockets and without teeth (n = 6) N = 18 | 0°, 45°, 90° | 100 µm | Cameo and intaglio surface | (Form Cure; Formlabs) 60 C for 10 min | Lab scanner 3D optical scanner (NeWay; Open Technologies, Rezzato, Italy) | Superimposed with a best-fit alignment RMSE (mm) | Master data | 3D analysis software (CATIA V5; Dassault Systèmes, Vélizy-Villacoublay, France). | 3D-printing accuracy is angle-dependent and 45° showed the highest accuracy |
| Yoshidomea et al. 2021 [29] | DENTCA Denture Base II Two printers SLA and one printer DLP | Maxillary denture base/without tooth sockets and without teeth (n = 5) N = 40 | 0°, 45°, 90°, 135°, 180°, 225°, 270°, 315° | 100 µm | Cameo and intaglio surface | (HiLite Power 3D, Kulzer, Hanau, Germany) 15 min Temp. NS | Lab scanner (R700, 3Shape, Copenhagen, Denmark) | Superimposed/with a best-fit alignment RMS (mm) | Master model (wax denture base scanned) | Geomagic Design X, 3D Systems, Rock Hill, CA, USA | 45° showed the highest accuracy. Support structures and built pitch affect the accuracy |
| Cameron et al., 2022 [30] | 3D+; NextDent Printer: (NextDent 5100) DLP | Maxillary denture base/with tooth sockets and without teeth (n = 10) N = 70 | 0°, 15°, 45°, 60°, 90° | 50 µm | Cameo and intaglio surface + support struts on both surfaces | 30 min (LC-3D Print Box; NextDent B.V.) 30 min Temp. MR | Lab scanner desktop laser scanner (E3; 3Shape A/S) | Superimposed/with a best-fit alignment RMSE (µm) | Reference cast | Geomagic Control X v20.0; 3D Systems Inc. | Maximum trueness found with 45, 60, and 90°. Also, the support strut affected the level of trueness |
| Charoenphol et al. 2022 [31] | Optiprint Gingiva, Dentona, Dortmund, Germany printer: Asiga Max, Asiga, DLP | Maxillary denture base/without tooth sockets and without teeth (n = 10) N = 30 | 0°, 45°, 90° | 100 µm | Cameo surface | Asiga Flush 30 min Temp. MR | Lab scanner Extra-oral scanner (E4 scanner, 3 Shape Dental System) | Surface-matching software superimposed/with a best-fit alignment RMSE (mm) | Reference cast | Geomagic Design X, 3D Systems, Rock Hill, CA, USA | The printing angle had no significant effect of the overall accuracy |
| Song et al. 2023 [32] | DENTCA base material Printer: (Pro95, SprintRay) DLP | Maxillary denture base/with tooth sockets and without teeth (n = 5) N = 70 | 0°, labial 45°, labial 90°, posterior 45°, posterior 90°, buccal 45°, buccal 90° | 50 µm; 100 µm | Cameo surface and alveolar sockets | (ProCure, Sprintray, USA) 40 min Temp. 60 °C | Laboratory scanner (Ceramill Map 600, Amann Girrbach, Austria) | Superimposed/with a best-fit alignment RMS (mm) | Reference cast by “N-Point Alignment” and “Best Fit Alignment” | Geomagic Wrap, 3D Systems, USA | Build orientation affect the accuracy and 45° and 90° showed the satisfactory accuracy |
| Lee et al. 2023 [33] | NextDent Denture 3D+ Printer: (Max UV; Asiga) DLP | Maxillary denture base/with tooth sockets and without teeth (n = 10) N = 120 | 0°, 45°, 90° | 50 µm; 100 µm | Cameo surface | (Cure M U102H; Graphy) low-viscosity 5 min high-viscosity 15min Temp. NS | Laboratory scanner (Medit T710; Medit) | Superimposed/ best-fit alignment RMS (µm) | Reference CAD data | Geomagic Control X; 3D Systems | The highest trueness was found with 45° |
| Gao et al. 2021 [34] | VisJet M3 crystal Multijet Printer: (ProJet MJP 3600 Dental MJP | Mandibular denture bases/with teeth (n = 9) N = 27 | 0°, 45°, 90° | 16 µm | Cameo surface | NS 30 min 158 °C | Lab scanner Optical surface scanner (Activity 880, Smart Optics, Bochum, Germany) | Superimposed/ best-fit alignment (RMS) (mm) | Reference STL files | Geomagic Wrap 2015 software, 3D Systems | The 45° build orientation showed higher accuracy |
| Chaiamornsup et al., 2023 [35] | (Dima Print denture base) Printer: Cara Print 4.0; Kulzer GmbH DLP | Mandibular denture bases/with tooth sockets and without teeth (n = 6) 16 DESIGN N = 96?? | 0°, 45°, 90°, 135°, 180°, 225°, 270°, 315° | 50 µm | Cameo surface + transverse bar | (HiLite Power 3D; Kulzer GmbH) 10 min Temp. NS | Laboratory scanner (D2000; 3Shape, Copenhagen, Denmark) with 5 µm accuracy | Superimposed/ best-fit alignment RMS (mm) | Original CAD | FreeForm ModelingPlus V12.0; Geomagic, NC, USA | The 270° build orientation is recommended |
| Unkovskiy et al., 2021 [36] | Denture base OP Formlabs, Printer: Form 2; Formlabs SLA | Maxillary denture base/with tooth sockets and without teeth (n = 5) | 0, 45, and 90 | NS | Cameo surface | FormCure, Formlabs, 80 °C for 60 min | Lab scanner D2000, 3Shape, Copenhagen, Denmark | Superimposed/ best-fit alignment RMSE, PA, and NA (mm) | Reference cast | Geomagic Control X, 3D systems | The 90 degree build angle may provide the best trueness. Higher precision was revealed in the DLP |
| V-print Dentbase–VOCO Printer: Solex 350 PLUS, DLP | LC-3DPrint Box, 3D Systems 30 min Temp. MR |
2.4. Quantitative Assessment of Included Studies
3. Results
3.1. Search and Selection
3.2. Risk of Bias Finding
3.3. Main Results
4. Discussion
4.1. Clinically Acceptable Value of Accuracy
4.2. Printing Technology
4.3. Denture Base Scanning, Accuracy Measurement Methods, Unit, and Evaluation Criteria in Relation to the Printing Angle
4.4. Factors Affecting Accuracy and Their Interrelationship
4.4.1. Support Structures
4.4.2. Starting Point and Separation Force Effect
4.4.3. Polymerization Shrinkage
4.4.4. Orientation and Layer Number
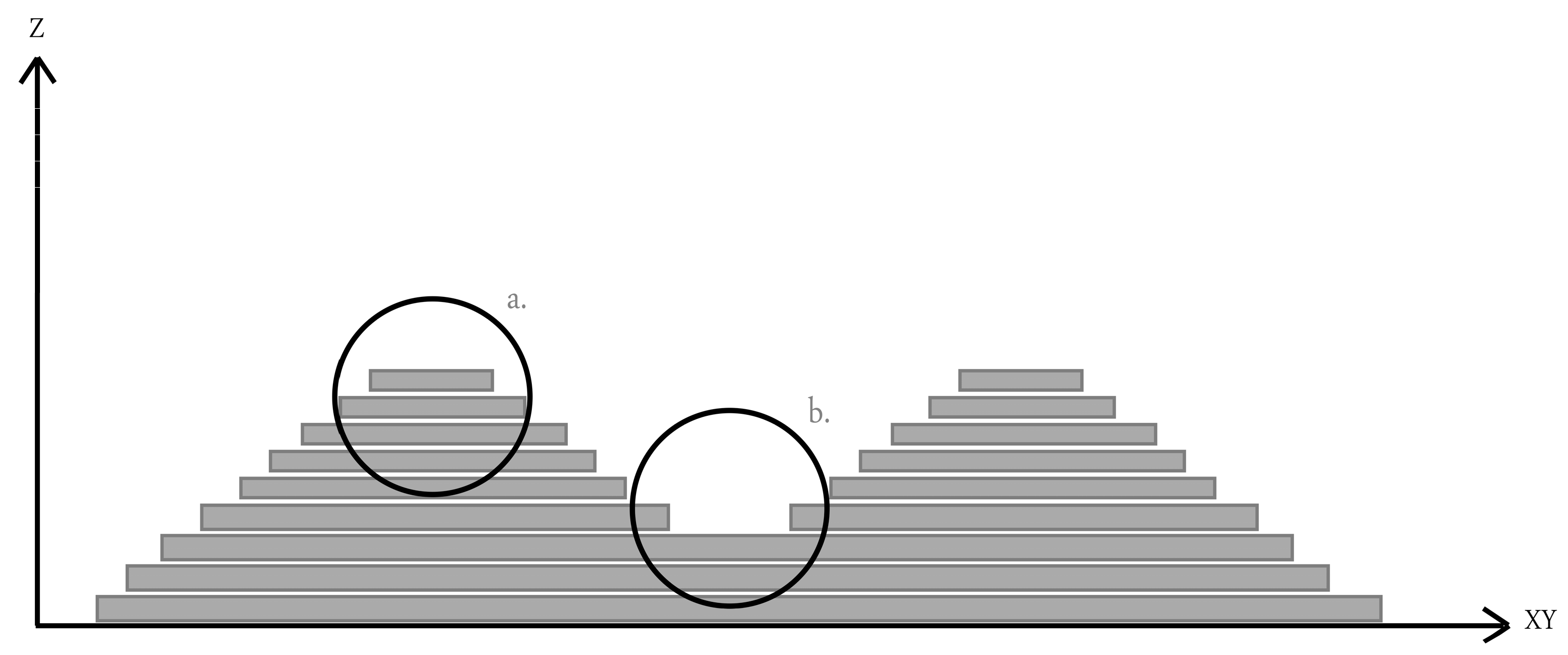
4.4.5. Staircase Effect
4.4.6. Time and Material Consumption in Relation to Angle
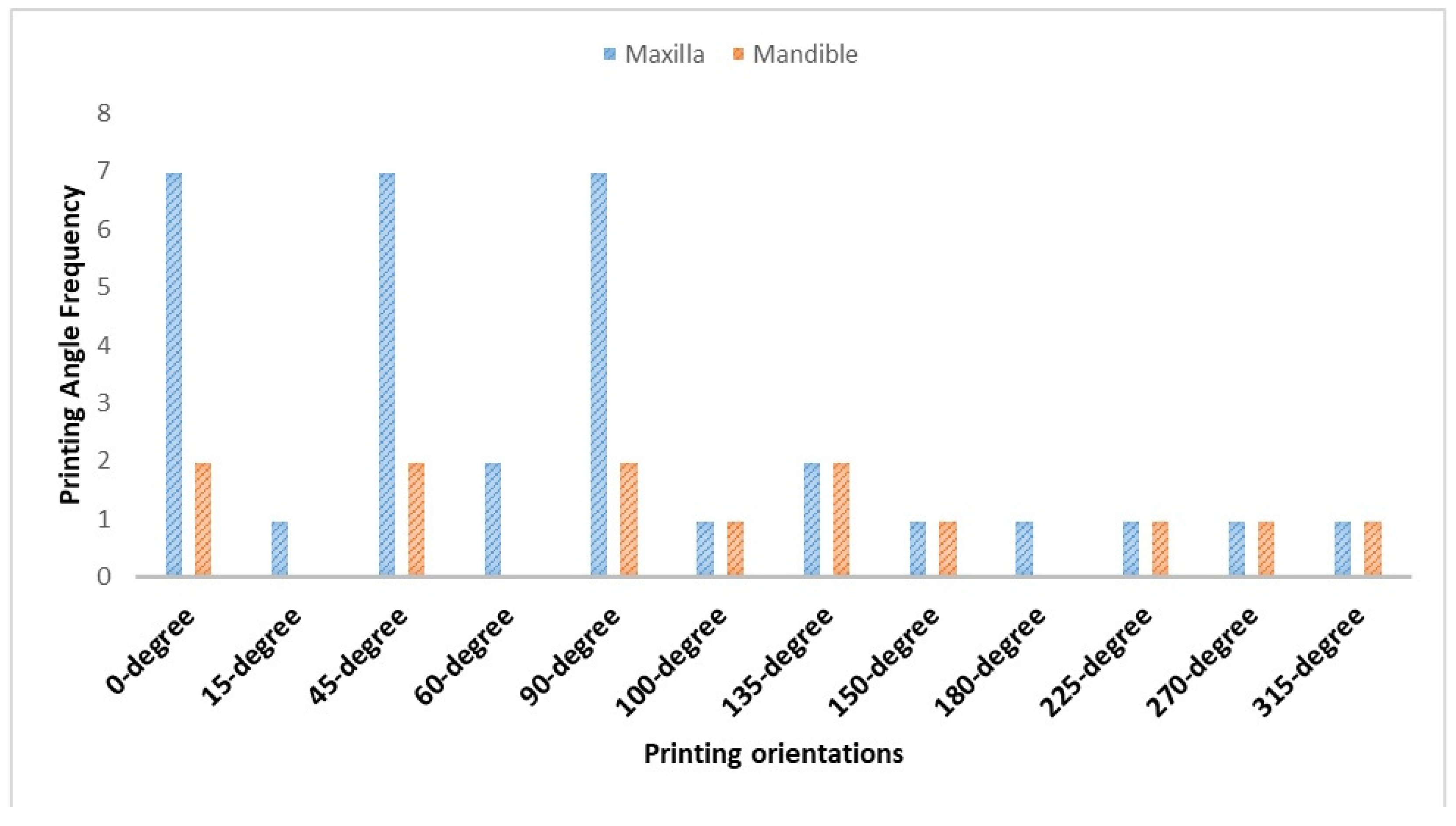
4.5. Printing Angles: Which Degree Is Better and Recommended?
4.6. Printing Angles: Which Degree Is Worst and Not Recommended?
4.7. Summary and Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Guidelines and Glossary Related to 3D Printing Technology and Printed Resins
| Terms | Definition, Description, and Explanation |
| Color map [28,30,32,33,34,35,36] | Color range indicating the clinical relevant areas. Different color interpret color mapping; light green to green (nominal deviations, acceptable deviation). Areas beyond nominal deviations are categorized as positive (+ve, yellow to red) or negative (−ve, light blue to blue) |
| +ve deviations [28,30,32,35] | The fabricated denture base data were larger than the CAD data and exceeding the allowable range limit (0.3 mm) indicating a gap between denture and mucosa affecting denture stability and durability. |
| −ve deviations [28,30,32,35] | The fabricated denture base data smaller than the CAD data and exceeded the lower limit of the allowable range (−0.3 mm) indicating an intimate contact with pressure on the mucosa which necessitate adjustment in the intaglio surface of denture base. |
| Root mean square error (RMSe) [28,30,31,32,34] | The RMSe values are overall accuracy measurement method via superimposition of two virtual files. The RMSE value, which was close to zero, meant the good adaptation of the denture base. |
| Trueness [28,30] | Closeness of measured values to the true value. The trueness value increased when the printed object and the CAD-designed object were dimensionally close |
| Precision [28,30] | Closeness of measured values during repeated measurements. The precision value increased when the printed objects were dimensionally close |
| Anisotropic Wikipedia | Anisotropy (/ˌænaɪˈsɒtrəpi, ˌænɪ-/) is the structural property of non-uniformity in different directions. An anisotropic object has properties that differ according to direction of measurement. |
| Staircase [28] | In printed surface with curvatures, the angle (θ) between two 3D printed successive layers resulted in staircase effect and expressed as the cusp height (CH). Large CH which resulted from thick printing layer/large cos (θ) negatively affect surface accuracy.
|
| overhang areas [34] | Areas of a 3D printed object are not supported by supporting structures |
References
- Lee, D.J.; Saponaro, P.C. Management of Edentulous Patients. Dent. Clin. N. Am. 2019, 63, 249–261. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.Y.; Yang, T.C.; Wang, T.M.; Lin, L.D. Effects of fabrication techniques on denture base adaptation: An in vitro study. J. Prosthet. Dent. 2020, 124, 740–747. [Google Scholar] [CrossRef]
- Deng, K.; Wang, Y.; Zhou, Y.; Sun, Y. Comparison of treatment outcomes and time efficiency between a digital complete denture and conventional complete denture: A pilot study. J. Am. Dent. Assoc. 2023, 154, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Peroz, S.; Peroz, I.; Beuer, F.; Sterzenbach, G.; von Stein-Lausnitz, M. Digital versus conventional complete dentures: A randomized, controlled, blinded study. J. Prosthet. Dent. 2022, 128, 956–963. [Google Scholar] [CrossRef]
- Srinivasan, M.; Kamnoedboon, P.; McKenna, G.; Angst, L.; Schimmel, M.; Özcan, M.; Müller, F. CAD-CAM removable complete dentures: A systematic review and meta-analysis of trueness of fit, biocompatibility, mechanical properties, surface characteristics, color stability, time-cost analysis, clinical and patient-reported outcomes. J. Dent. 2021, 113, 103777. [Google Scholar] [CrossRef]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive technology: Update on current materials and applications in dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef]
- Anadioti, E.; Musharbash, L.; Blatz, M.B.; Papavasiliou, G.; Kamposiora, P. 3D printed complete removable dental prostheses: A narrative review. BMC Oral Health 2020, 20, 343. [Google Scholar] [CrossRef]
- Jiang, C.P.; Hentihu, M.F.R.; Lee, S.Y.; Lin, R. Multiresin Additive Manufacturing Process for Printing a Complete Denture and an Analysis of Accuracy. 3D Print Addit. Manuf. 2022, 9, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Piedra-Cascón, W.; Krishnamurthy, V.R.; Att, W. Revilla-León M3D printing parameters supporting structures slicing post-processing procedures of vatpolymerization additive manufacturing technologies: A narrative review. J. Dent. 2021, 109, 103630. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M. Factors affecting flexural strength of 3D-printed resins: A systematic review. J. Prosthodont. 2023, 32, 96–110. [Google Scholar] [CrossRef]
- Derchi, G.; Marchio, V.; Cinquini, C.; Federici, M.I.; Barone, A.; Pagano, S. Evaluation of Accuracy of Different Print Angulations for 3D Printed Dental Crowns. Mater. Sci. 2024, 30, 114–120. [Google Scholar] [CrossRef]
- Al-Dulaijan, Y.A.; Alsulaimi, L.; Alotaibi, R.; Alboainain, A.; Akhtar, S.; Khan, S.Q.; Al-Ghamdi, M.; Gad, M.M. Effect of Printing Orientation and Postcuring Time on the Flexural Strength of 3D-Printed Resins. J. Prosthodont. 2023, 32, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Altarazi, A.; Haider, J.; Alhotan, A.; Silikas, N.; Devlin, H. Assessing the physical and mechanical properties of 3D printed acrylic material for denture base application. Dent. Mater. 2022, 38, 1841–1854. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Factors influencing the dimensional accuracy of 3D-printed full-coverage dental restorations using stereolithography technology. Int. J. Prosthodont. 2016, 29, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Hada, T.; Kanazawa, M.; Iwaki, M.; Arakida, T.; Minakuchi, S. Effect of printing direction on stress distortion of three-dimensional printed dentures using stereolithography technology. J. Mech. Behav. Biomed. Mater. 2020, 110, 103949. [Google Scholar] [CrossRef] [PubMed]
- You, S.M.; You, S.G.; Kang, S.Y.; Bae, S.Y.; Kim, J.H. Evaluation of the accuracy (trueness and precision) of a maxillary trial denture according to the layer thickness: An in vitro study. J. Prosthet. Dent. 2021, 125, 139–145. [Google Scholar] [CrossRef]
- Wang, C.; Shi, Y.F.; Xie, P.J.; Wu, J.H. Accuracy of digital complete dentures: A systematic review of in vitro studies. J. Prosthet. Dent. 2021, 125, 249–256. [Google Scholar] [CrossRef]
- ISO 5725-1:1998; Accuracy (Trueness and Precision) of Measurement Methods and Results–Part 1: General Principles and Definitions. International Organization of Standardization: Geneva, Switzerland, 1998. Available online: https://www.iso.org/obp/ui/#iso:std:iso:5725:-1:ed-1:v1:en (accessed on 19 January 2022).
- The Glossary of Prosthodontic Terms: Ninth Edition. J. Prosthet. Dent. 2017, 117, e1–e105. [CrossRef] [PubMed]
- Hwang, H.J.; Lee, S.J.; Park, E.J.; Yoon, H.I. Assessment of the trueness and tissue surface adaptation of CAD-CAM maxillary denture bases manufactured using digital light processing. J. Prosthet. Dent. 2019, 121, 110–117. [Google Scholar] [CrossRef]
- Unkovskiy, A.; Bui, P.H.-B.; Schille, C.; Geis-Gerstorfer, J.; Huettig, F.; Spintzyk, S. Objects build orientation, positioning, and curing influence dimensional accuracy and flexural properties of stereolithographically printed resin. Dent. Mater. 2018, 34, e324–e333. [Google Scholar] [CrossRef]
- Tsai, F.-C.; Yang, T.-C.; Wang, T.-M.; Lin, L.-D. Dimensional changes of complete dentures fabricated by milled and printed techniques: An in vitro study. J. Prosthet. Dent. 2023, 129, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Oğuz, E.İ.; Kılıçarslan, M.A.; Özcan, M.; Ocak, M.; Bilecenoğlu, B.; Orhan, K. Evaluation of denture base adaptation fabricated using conventional, subtractive, and additive technologies: A volumetric micro-computed tomography analysis. J. Prosthodont. 2021, 30, 257–263. [Google Scholar] [CrossRef]
- Rubayo, D.D.; Phasuk, K.; Vickery, J.M.; Morton, D.; Lin, W.-S. Influences of build angle on the accuracy, printing time, and material consumption of additively manufactured surgical templates. J. Prosthet. Dent. 2021, 126, 658–663. [Google Scholar] [CrossRef]
- Goodacre, B.J.; Goodacre, C.J. Additive Manufacturing for Complete Denture Fabrication: A Narrative Review. J. Prosthodont. 2022, 31, 47–51. [Google Scholar] [CrossRef]
- Faggion, C.M., Jr. Guidelines for reporting pre-clinical in vitro studies on dental materials. J. Evid. Based Dent. Pract. 2012, 12, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Jin, M.C.; Yoon, H.I.; Yeo, I.S.; Kim, S.H.; Han, J.S. The effect of build angle on the tissue surface adaptation of maxillary and mandibular complete denture bases manufactured by digital light processing. J. Prosthet. Dent. 2020, 123, 473–482. [Google Scholar] [CrossRef]
- Hada, T.; Kanazawa, M.; Iwaki, M.; Arakida, T.; Soeda, Y.; Katheng, A.; Otake, R.; Minakuchi, S. Effect of Printing Direction on the Accuracy of 3D-Printed Dentures Using Stereolithography Technology. Materials 2020, 13, 3405. [Google Scholar] [CrossRef] [PubMed]
- Yoshidome, K.; Torii, M.; Kawamura, N.; Shimpo, H.; Ohkubo, C. Trueness and fitting accuracy of maxillary 3D printed complete dentures. J. Prosthodont. Res. 2021, 65, 559–564. [Google Scholar] [CrossRef]
- Cameron, A.B.; Evans, J.L.; Abuzar, M.A.; Tadakamadla, S.K.; Love, R.M. Trueness assessment of additively manufactured maxillary complete denture bases produced at different orientations. J. Prosthet. Dent. 2024, 131, 129–135. [Google Scholar] [CrossRef]
- Charoenphol, K.; Peampring, C. An In Vitro Study of Intaglio Surface, Periphery/Palatal Seal Area, and Primary Bearing Area Adaptation of 3D-Printed Denture Base Manufactured in Various Build Angles. Int. J. Dent. 2022, 2022, 3824894. [Google Scholar] [CrossRef]
- Song, S.; Zhang, J.; Liu, M.; Li, F.; Bai, S. Effect of build orientation and layer thickness on manufacturing accuracy, printing time, and material consumption of 3D printed complete denture bases. J. Dent. 2023, 130, 104435. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.J.; Jo, Y.H.; Yilmaz, B.; Yoon, H.I. Effect of layer thickness, build angle, and viscosity on the mechanical properties and manufacturing trueness of denture base resin for digital light processing. J. Dent. 2023, 135, 104598. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Yang, Z.; Lin, W.S.; Tan, J.; Chen, L. The Effect of Build Orientation on the Dimensional Accuracy of 3D-Printed Mandibular Complete Dentures Manufactured with a Multijet 3D Printer. J. Prosthodont. 2021, 30, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Chaiamornsup, P.; Katheng, A.; Ha, R.; Tsuchida, Y.; Kanazawa, M.; Uo, M.; Minakuchi, S.; Suzuki, T.; Takahashi, H. Effects of build orientation and bar addition on accuracy of complete denture base fabricated with digital light projection: An In Vitro study. J. Prosthodont. Res. 2023, 67, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Unkovskiy, A.; Schmidt, F.; Beuer, F.; Li, P.; Spintzyk, S.; Kraemer Fernandez, P. Stereolithography vs. Direct Light Processing for Rapid Manufacturing of Complete Denture Bases: An In Vitro Accuracy Analysis. J. Clin. Med. 2021, 10, 1070. [Google Scholar] [CrossRef] [PubMed]
- Ishinabe, S. Mucosal thickness of the denture foundation under occlusal force. Nihon Hotetsu Shika Gakkai Zasshi 1991, 35, 111–124. [Google Scholar] [CrossRef]
- Deng, K.; Chen, H.; Zhao, Y.; Zhou, Y.; Wang, Y.; Sun, Y. Evaluation of adaptation of the polylactic acid pattern of maxillary complete dentures fabricated by fused deposition modelling technology: A pilot study. PLoS ONE 2018, 13, e0201777. [Google Scholar] [CrossRef] [PubMed]
- Wills, D.J.; Manderson, R.D. Biomechanical aspects of the support of partial dentures. J. Dent. 1977, 5, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Gaynor, A.T.; Meisel, N.A.; Williams, C.B.; Guest, J.K. Multiple-material topology optimization of compliant mechanisms created via PolyJet three-dimensional printing. J. Manuf. Sci. Eng. 2014, 136, 061015. [Google Scholar] [CrossRef]
- Horn, T.J.; Harrysson, O.L. Overview of current additive manufacturing technologies and selected applications. Sci. Prog. 2012, 95, 255–282. [Google Scholar] [CrossRef]
- Stansbury, J.W.; Idacavage, M.J. 3D printing with polymers: Challenges among expanding options and opportunities. Dent. Mater. 2016, 32, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Leu, M.C.; Mazumder, J.; Donmez, A. Additive manufacturing: Current state future potential gaps needs recommendations. J. Manuf. Sci. Eng. 2015, 137, 014001. [Google Scholar] [CrossRef]
- Chae, M.P.; Rozen, W.M.; McMenamin, P.G.; Findlay, M.W.; Spychal, R.T.; Hunter-Smith, D.J. Emergingapplications of bedside 3D printing in plastic surgery. FrontSurg 2015, 2, 25. [Google Scholar]
- ISO 10360-2; Geometrical Product Specifications (GPS)—Acceptance and Reverification Tests for Coordinate Measuring Machines (CMM)—Part 2: CMMs Used for Measuring Linear Dimensions. ISO: Geneva, Switzerland, 2009.
- Berger, L.; Adler, W.; Kreuzer, M.M.K.; Wichmann, M.; Matta, R.E. Comparison of Digital and Conventional Impressions Based on the 3D Fit of Crowns. Int. J. Prosthodont. 2022, 35, 801–808. [Google Scholar] [CrossRef]
- Kim, R.J.Y.; Benic, G.I.; Park, J.M. Trueness of ten intraoral scanners in determining the positions of simulated implant scan bodies. Sci. Rep. 2021, 11, 2606. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.H.; Han, S.S.; Choi, Y.J.; Woo, C.W. Linear Accuracy of Full-Arch Digital Models Using Four Different Scanning Methods: An In Vitro Study Using a Coordinate Measuring Machine. Appl. Sci. 2020, 10, 2741. [Google Scholar] [CrossRef]
- Pan, Y.; Tsoi, J.K.H.; Lam, W.Y.H.; Zhao, K.; Pow, E.H.N. The cumulative effect of error in the digital workflow for complete-arch implant-supported frameworks: An in vitro study. Clin. Oral Implants Res. 2022, 33, 886–899. [Google Scholar] [CrossRef]
- Artopoulos, A.; Juszczyk, A.S.; Rodriguez, J.M.; Clark, R.K.F.; Radford, D.R. Three-dimensional processing deformation of three denture base materials. J. Prosthet. Dent. 2013, 110, 481–487. [Google Scholar] [CrossRef]
- Alharbi, N.; Osman, R.B.; Wismeijer, D. Effects of build direction on the mechanical properties of3D- printed complete coverage interim dental restorations. J. Prosthet. Dent. 2016, 115, 760–767. [Google Scholar] [CrossRef]
- Ye, H.; Venketeswaran, A.; Das, S.; Zhou, C. Investigation of separation force for constrained-surface stereolithography process from mechanics perspective. Rapid Prototyp. J. 2017, 23, 696–710. [Google Scholar] [CrossRef]
- Osman, R.; Alharbi, N.; Wismeijer, D. Build Angle: Does it influence the accuracy of 3D-printed dental restorations using digital light-processing technology? Int. J. Prosthodont. 2017, 30, 182–188. [Google Scholar] [CrossRef] [PubMed]
- You, S.M.; You, S.G.; Lee, B.I.; Kim, J.H. Evaluation of trueness in a denture base fabricated by using CAD-CAM systems and adaptation to the socketed surface of denture base: An in vitro study. J. Prosthet. Dent. 2022, 127, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; He, H.; Xu, J.; Feinerman, A. Study of separation force in constrained surface projection stereolithography. Rapid Prototyp. J. 2017, 23, 353–361. [Google Scholar] [CrossRef]
- Mohan Pandey, P.; Venkata Reddy, N.; Dhande, S.G. Slicing procedures in layered manufacturing: A review. Rapid Prototyp. J. 2003, 9, 274–288. [Google Scholar] [CrossRef]
- Shim, J.S.; Kim, J.E.; Jeong, S.H.; Choi, Y.J.; Ryu, J.J. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J. Prosthet. Dent. 2020, 124, 468–475. [Google Scholar] [CrossRef]
- You, S.-G.; You, S.-M.; Kang, S.Y.; Bae, S.Y.; Kim, J.H. Evaluation of the adaptation of complete denture metal bases fabricated with dental CAD-CAM systems: An in vitro study. J. Prosthet. Dent. 2021, 125, 479–485. [Google Scholar] [CrossRef]
- Ortensi, L.; Sigari, G.; La Rosa, G.R.M.; Ferri, A.; Grande, F.; Pedullà, E. Digital planning of composite customized veneers using Digital Smile Design: Evaluation of its accuracy and manufacturing. Clin. Exp. Dent. Res. 2022, 8, 537–543. [Google Scholar] [CrossRef]
| Study question | What is the effect of printing orientation on the accuracy and fit of a 3D-printed denture base? |
| Search combination | “denture base” OR “acrylic resin” OR “prosthesis” OR “dental prosthesis” OR “removable dental prostheses” OR “maxillary complete denture” OR “mandibular complete denture” AND “Three-dimensional printing” OR “printing orientation” OR “building direction” OR “build orientation” OR “printing angle” OR “build angle” OR “printing parameter” OR “3D print” OR “additive manufacturing” OR “rapid prototype” OR “CAD/CAM” OR “stereolithography” OR “digital light projection” OR “3D printing” AND “accuracy” OR “dimensional change” OR “trueness ” OR “precision” OR “adaptation” OR “fit” OR “fitting accuracy“ |
| Database search | PubMed, Web of Science, Scopus |
| Author/Year | Sample Size Calculation | Sample Randomization | Control Group | Stating Clear Testing Method | Statistical Analyses Carried Out | Reliable Analytical Methods | Blinding of Evaluators | Risk of Bias |
|---|---|---|---|---|---|---|---|---|
| Jin et al., 2018 [27] | Yes | No | No | Yes | Yes | Yes | No | Medium |
| Hada et al. 2020 [28] | Yes | No | No | Yes | Yes | Yes | No | Medium |
| Yoshidomea et al. 2021 [29] | No | No | Yes | Yes | Yes | Yes | No | Medium |
| Cameron et al., 2022 [30] | Yes | No | No | Yes | Yes | Yes | No | Medium |
| Charoenphol et al. 2022 [31] | Yes | No | No | Yes | Yes | Yes | No | Medium |
| Song et al. 2023 [32] | No | No | No | Yes | Yes | Yes | No | High |
| Lee et al. 2023 [33] | No | No | Yes | Yes | Yes | Yes | No | Medium |
| Gao et al. 2021 [34] | No | No | Yes | Yes | Yes | Yes | No | Medium |
| Chaiamornsup et al., 2023 [35] | No | No | No | Yes | Yes | Yes | No | High |
| Unkovskiy et al., 2021 [36] | No | No | Yes | Yes | Yes | Yes | No | Medium |
| Study/Denture | Measurement Methods/Unit | Orientation° | Trueness Mean ± SD | Precision Mean ± SD | +Ve Deviation | −Ve Deviations | Comment on Values Presentations |
|---|---|---|---|---|---|---|---|
| Jin et al., 2018 [27] Maxillary and mandibular denture | RMSE, PA, and NA (mm) | 90 | 0.095 ± 0.008 | 0.061 ± 0.002 | −0.083 ± 0.007 | Maxillary | |
| 100 | 0.079 ± 0.003 | 0.053 ± 0.002 | −0.074 ± 0.002 | ||||
| 135 | 0.087 ± 0.007 | 0.039 ± 0.004 | −0.072 ± 0.004 | ||||
| 150 | 0.088 ± 0.006 | 0.038 ± 0.002 | −0.074 ± 0.006 | ||||
| 90 | 0.114 ± 0.005 | 0.095 ± 0.003 | −0.089 ± 0.006 | Mandibular | |||
| 100 | 0.103 ± 0.007 | 0.090 ± 0.005 | −0.073 ± 0.006 | ||||
| 135 | 0.123 ± 0.008 | 0.105 ± 0.007 | −0.082 ± 0.005 | ||||
| 150 | 0.136 ± 0.015 | 0.097 ± 0.008 | −0.102 ± 0.010 | ||||
| Hada et al. 2020 [28] Maxillary denture | RMSE/mm | 0 | 0.129 ± 0.006 | 0.072 ± 0.004 | ---- | ----- | Trueness values |
| 45 | 0.086 ± 0.004 | 0.050 ± 0.003 | ------ | ----- | |||
| 90 | 0.109 ± 0.005 | 0.069 ± 0.002 | ------- | ------- | |||
| Yoshidomea et al. 2021 [29] Maxillary denture | RMS/mm | 0 | Results present in tables as the average and with no mean values and standard deviation. | ||||
| 45 | |||||||
| 90 | |||||||
| 135 | |||||||
| 180 | |||||||
| 225 | |||||||
| 270 | |||||||
| 315 | |||||||
| Cameron et al., 2022 [30] Maxillary denture | RMS/µm | 0 | 68.1 ± 4.2 µm | 57.6 ± 3.1 µm | −55.5 ± 6.4 µm | ||
| 15 | 74.8 ± 8.3 µm | 62. ± 2 6.8 µm | −54.2 ± 4.4 µm | ||||
| 45 | 60.2 ± 3.9 µm | 44.6 ±2.2 µm | −43.3 ± 6.1 µm | ||||
| 60 | 56.2 ± 7.2 µm | 40.6 ± 7.7 µm | −42.5 ± 6.8 µm | ||||
| 90 | 58.6 ± 4.5 µm | 37.7 ±3.4 µm | −45.8 ± 4.3 µm | ||||
| Charoenphol et al. 2022 [31] Maxillary denture | RMSE/mm Overall surface area | 0 | 0.1209 ± 0.0033 | Three readings: overall, peripheral and posterior palatal seal areas, and the primary bearing area | |||
| 45 | 0.1265 ± 0.0036 | ||||||
| 90 | 0.1219 ± 0.0037 | ||||||
| Song et al. 2023 [32] Maxillary denture | RMS/mm intaglio surface | 0 | 0.095 ± 0.016 | Accuracy palate, residual ridge, borders, and intaglio surface | |||
| 45 labial | 0.076 ± 0.010 | ||||||
| 90 labial | 0.078 ± 0.012 | ||||||
| 45 posterior | 0.098 ± 0.016 | ||||||
| 90 posterior | 0.120 ± 0.008 | ||||||
| 45 buccal | 0.088 ± 0.009 | ||||||
| 90 buccal | 0.129 ± 0.011 | ||||||
| Lee et al. 2023 [33] Maxillary denture | RMS/µm | 0 | High resin viscosity–Layer thickness 50 µm | ||||
| 45 | |||||||
| 90 | |||||||
| 0 | High resin viscosity–Layer thickness 100 µm | ||||||
| 45 | |||||||
| 90 | |||||||
| 0 | Low resin viscosity–Layer thickness 50 µm | ||||||
| 45 | |||||||
| 90 | |||||||
| 0 | Low resin viscosity–Layer thickness 100 µm | ||||||
| 45 | |||||||
| 90 | |||||||
| Gao et al. 2021 [34] Mandibular denture | RMS/mm Whole denture | 0 | 0.185 ± 0.060 | Whole denture, teeth, denture extension, intaglio surface | |||
| 45 | 0.170 ± 0.043 | ||||||
| 90 | 0.183 ± 0.044 | ||||||
| RMS/mm Intaglio surface | 0 | 0.228 ± 0.010 | |||||
| 45 | 0.207 ± 0.006 | ||||||
| 90 | 0.218 ± 0.057 | ||||||
| Chaiamornsup et al., 2023 [35] Mandibular denture | RMS/mm | 0 | Results presented in a bar chart and with no mean values and standard deviation. | ||||
| 45 | |||||||
| 90 | |||||||
| 135 | |||||||
| 180 | |||||||
| 225 | |||||||
| 270 | |||||||
| 315 | |||||||
| Unkovskiy et al., 2021 [36] Maxillary denture | 0 | 0.094 ± 0.004 | 0.087 ± 0.042 | 0.082 ± 0.011 | −0.054 ± 0.006 | SLA | |
| 45 | 0.132 ± 0.016 | 0.094 ± 0.034 | 0.099 ± 0.015 | −0.089 ± 0.018 | |||
| 90 | 0.083 ± 0.009 | 0.098 ± 0.037 | 0.055 ± 0.009 | −0.045 ± 0.010 | |||
| 0 | 0.256 ± 0.031 | 0.134 ± 0.028 | 0.166 ± 0.027 | −0.187 ± 0.024 | DLP | ||
| 45 | 0.211 ± 0.031 | 0.048 ± 0.023 | 0.101 ± 0.010 | −0.097 ± 0.008 | |||
| 90 | 0.163 ± 0.030 | 0.044 ± 0.023 | 0.066 ± 0.010 | −0.065 ± 0.006 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AlGhamdi, M.A.; Gad, M.M. Impact of Printing Orientation on the Accuracy of Additively Fabricated Denture Base Materials: A Systematic Review. Dent. J. 2024, 12, 230. https://doi.org/10.3390/dj12070230
AlGhamdi MA, Gad MM. Impact of Printing Orientation on the Accuracy of Additively Fabricated Denture Base Materials: A Systematic Review. Dentistry Journal. 2024; 12(7):230. https://doi.org/10.3390/dj12070230
Chicago/Turabian StyleAlGhamdi, Maram A., and Mohammed M. Gad. 2024. "Impact of Printing Orientation on the Accuracy of Additively Fabricated Denture Base Materials: A Systematic Review" Dentistry Journal 12, no. 7: 230. https://doi.org/10.3390/dj12070230






