Awareness of Molar Incisor Hypomineralisation (MIH) and Hypomineralised Second Primary Molars (HSPMs) among Northern Italian Dentists: A Questionnaire Survey
Abstract
:1. Introduction
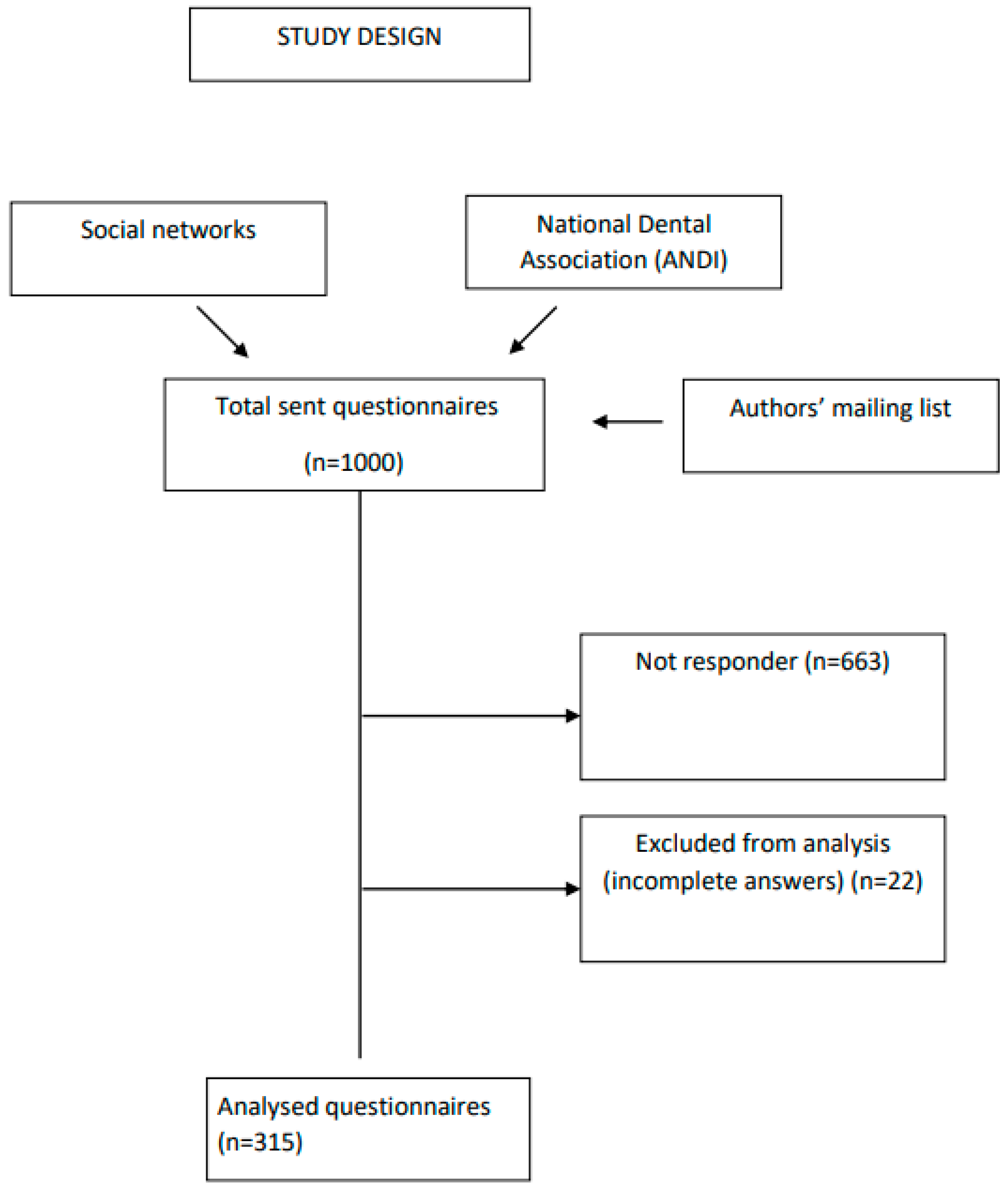
2. Materials and Methods
2.1. Questionnaire
2.2. Sample Size
2.3. Statistical Analysis
3. Results
3.1. Characteristics of Respondents
3.2. Reported Occurrence of Opacities in Caries-Free Children
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ghanim, A.; Manton, D.; Mariño, R.; Morgan, M.; Bailey, D. Prevalence of Demarcated Hypomineralisation Defects in Second Primary Molars in Iraqi Children: Prevalence of Hypomineralized Second Primary Molar. Int. J. Paediatr. Dent. 2013, 23, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Salanitri, S.; Seow, W. Developmental Enamel Defects in the Primary Dentition: Aetiology and Clinical Management. Aust. Dent. J. 2013, 58, 133–140. [Google Scholar] [CrossRef]
- Balmer, R.; Toumba, K.J.; Munyombwe, T.; Godson, J.; Duggal, M.S. The Prevalence of Incisor Hypomineralisation and Its Relationship with the Prevalence of Molar Incisor Hypomineralisation. Eur. Arch. Paediatr. Dent. 2015, 16, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Lygidakis, N.A.; Garot, E.; Somani, C.; Taylor, G.D.; Rouas, P.; Wong, F.S.L. Best Clinical Practice Guidance for Clinicians Dealing with Children Presenting with Molar-Incisor-Hypomineralisation (MIH): An Updated European Academy of Paediatric Dentistry Policy Document. Eur. Arch. Paediatr. Dent. 2022, 23, 3–21. [Google Scholar] [CrossRef]
- Lygidakis, N.A.; Wong, F.; Jälevik, B.; Vierrou, A.-M.; Alaluusua, S.; Espelid, I. Best Clinical Practice Guidance for Clinicians Dealing with Children Presenting with Molar-Incisor-Hypomineralisation (MIH). Eur. Arch. Paediatr. Dent. 2010, 11, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Weerheijm, K.L.; Duggal, M.; Mejàre, I.; Papagiannoulis, L.; Koch, G.; Martens, L.C.; Hallonsten, A.-L. Judgement Criteria for Molar Incisor Hypomineralisation (MIH) in Epidemiologic Studies: A Summary of the European Meeting on MIH Held in Athens. Eur. J. Paediatr. Dent. 2003, 4, 110–113. [Google Scholar]
- Weerheijm, K.L.; Jälevik, B.; Alaluusua, S. Molar–Incisor Hypomineralisation. Caries. Res. 2001, 35, 390–391. [Google Scholar] [CrossRef]
- Elfrink, M.E.; Schuller, A.A.; Weerheijm, K.L.; Veerkamp, J.S. Hypomineralized second primary molars: Prevalence data in Dutch 5-year-olds. Caries. Res. 2008, 42, 282–285. [Google Scholar] [CrossRef]
- Elhennawy, K.; Rajjoub, O.; Reissmann, D.R.; Doueiri, M.-S.; Hamad, R.; Sierwald, I.; Wiedemann, V.; Bekes, K.; Jost-Brinkmann, P.-G. The Association between Molar Incisor Hypomineralization and Oral Health-Related Quality of Life: A Cross-Sectional Study. Clin. Oral Investig. 2022, 26, 4071–4077. [Google Scholar] [CrossRef]
- Ghanim, A.; Silva, M.J.; Elfrink, M.E.C.; Lygidakis, N.A.; Mariño, R.J.; Weerheijm, K.L.; Manton, D.J. Molar Incisor Hypomineralisation (MIH) Training Manual for Clinical Field Surveys and Practice. Eur. Arch. Paediatr. Dent. 2017, 18, 225–242. [Google Scholar] [CrossRef]
- Farah, R.A.; Monk, B.C.; Swain, M.V.; Drummond, B.K. Protein content of molar- incisor hypomineralization enamel. J. Dent. 2010, 38, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Bussaneli, D.G.; Vieira, A.R.; Santos-Pinto, L.; Restrepo, M. Molar-Incisor Hypomineralisation: An Updated View for Aetiology 20 Years Later. Eur. Arch. Paediatr. Dent. 2022, 23, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Garot, E.; Rouas, P.; Somani, C.; Taylor, G.D.; Wong, F.; Lygidakis, N.A. An Update of the Aetiological Factors Involved in Molar Incisor Hypomineralisation (MIH): A Systematic Review and Meta-Analysis. Eur. Arch. Paediatr. Dent. 2022, 23, 23–38. [Google Scholar] [CrossRef]
- Butera, A.; Maiorani, C.; Morandini, A.; Simonini, M.; Morittu, S.; Barbieri, S.; Bruni, A.; Sinesi, A.; Ricci, M.; Trombini, J.; et al. Assessment of Genetical, Pre, Peri and Post Natal Risk Factors of Deciduous Molar Hypomineralization (DMH), Hypomineralized Second Primary Molar (HSPM) and Molar Incisor Hypomineralization (MIH): A Narrative Review. Children 2021, 8, 432. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Americano, G.C.; Jacobsen, P.E.; Soviero, V.M.; Haubek, D. A systematic review on the association between molar incisor hypomineralization and dental caries. Int. J. Paediatr. Dent. 2017, 27, 11–21. [Google Scholar] [CrossRef]
- Elfrink, M.E.; Veerkamp, J.S.; Kalsbeek, H. Caries pattern in primary molars in Dutch 5-year-old children. Eur. Arch. Paediatr. Dent. 2006, 7, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Bekes, K.; Amend, S.; Priller, J.; Zamek, C.; Stamm, T.; Krämer, N. Hypersensitivity Relief of MIH-Affected Molars Using Two Sealing Techniques: A 12-Week Follow-Up. Clin. Oral Investig. 2022, 26, 1879–1888. [Google Scholar] [CrossRef]
- Somani, C.; Taylor, G.D.; Garot, E.; Rouas, P.; Lygidakis, N.A.; Wong, F.S.L. An Update of Treatment Modalities in Children and Adolescents with Teeth Affected by Molar Incisor Hypomineralisation (MIH): A Systematic Review. Eur. Arch. Paediatr. Dent. 2022, 23, 39–64. [Google Scholar] [CrossRef]
- Garot, E.; Denis, A.; Delbos, Y.; Manton, D.; Silva, M.; Rouas, P. Are Hypomineralised Lesions on Second Primary Molars (HSPM) a Predictive Sign of Molar Incisor Hypomineralisation (MIH)? A Systematic Review and a Meta-Analysis. J. Dent. 2018, 72, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Quintero, Y.; Restrepo, M.; Rojas-Gualdrón, D.F.; Farias, A.L.; Santos-Pinto, L. Association between hypomineralization of deciduous and molar incisor hypomineralization and dental caries. Braz. Dent. J. 2022, 33, 113–119. [Google Scholar] [CrossRef]
- Elfrink, M.E.C.; Ghanim, A.; Manton, D.J.; Weerheijm, K.L. Standardised Studies on Molar Incisor Hypomineralisation (MIH) and Hypomineralised Second Primary Molars (HSPM): A Need. Eur. Arch. Paediatr. Dent. 2015, 16, 247–255. [Google Scholar] [CrossRef]
- Ghanim, A.; Elfrink, M.; Weerheijm, K.; Mariño, R.; Manton, D. A Practical Method for Use in Epidemiological Studies on Enamel Hypomineralisation. Eur. Arch. Paediatr. Dent. 2015, 16, 235–246. [Google Scholar] [CrossRef] [PubMed]
- Lopes, L.B.; Machado, V.; Mascarenhas, P.; Mendes, J.J.; Botelho, J. The Prevalence of Molar-Incisor Hypomineralization: A Systematic Review and Meta-Analysis. Sci. Rep. 2021, 11, 22405. [Google Scholar] [CrossRef] [PubMed]
- Sidhu, N.; Wang, Y.; Barrett, E.; Casas, M. Prevalence and Presentation Patterns of Enamel Hypomineralisation (MIH and HSPM) among Paediatric Hospital Dental Patients in Toronto, Canada: A Cross-Sectional Study. Eur. Arch. Paediatr. Dent. 2020, 21, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Willmott, N.S.; Bryan, R.A.E.; Duggal, M.S. Molar-Incisor-Hypomineralisation: A Literature Review. Eur. Arch. Paediatr. Dent. 2008, 9, 172–179. [Google Scholar] [CrossRef] [PubMed]
- Ghanim, A.; Morgan, M.; Mariño, R.; Manton, D.; Bailey, D. Perception of molar-incisor hypomineralisation (MIH) by Iraqi dental academics. Int. J. Paediatr. Dent. 2011, 21, 261–270. [Google Scholar] [CrossRef]
- Alanzi, A.; Faridoun, A.; Kavvadia, K.; Ghanim, A. Dentists’ perception, knowledge, and clinical management of molar-incisor-hypomineralisation in Kuwait: A cross-sectional study. BMC Oral Health 2018, 18, 34. [Google Scholar] [CrossRef]
- Wall, A.; Leith, R. A questionnaire study on perception and clinical management of molar incisor hypomineralisation (MIH) by Irish dentists. Eur. Arch. Paediatr. Dent. 2020, 21, 703–710. [Google Scholar] [CrossRef]
- Cagetti, M.G.; Salerno, C.; Bontà, G.; Bisanti, A.; Maspero, C.; Tartaglia, G.M.; Campus, G. Dental and Dental Hygiene Students’ Knowledge and Capacity to Discriminate the Developmental Defects of Enamel: A Self-Submitted Questionnaire Survey. Children 2022, 9, 1759. [Google Scholar] [CrossRef]
- Hobdell, M.; Petersen, P.E.; Clarkson, J.; Johnson, N. Global Goals for Oral Health 2020. Int. Dent. J. 2003, 53, 285–288. [Google Scholar] [CrossRef]
- Pizzo, G.; Matranga, D.; Maniscalco, L.; Buttacavoli, F.; Campus, G.; Giuliana, G. Caries Severity, Decayed First Permanent Molars and Associated Factors in 6–7 Years Old Schoolchildren Living in Palermo (Southern Italy). J. Clin. Med. 2023, 12, 4343. [Google Scholar] [CrossRef]
- Campus, G.; Cocco, F.; Strohmenger, L.; Wolf, T.G.; Balian, A.; Arghittu, A.; Cagetti, M.G. Inequalities in Caries among Pre-School Italian Children with Different Background. BMC Pediatr. 2022, 22, 443. [Google Scholar] [CrossRef]
- Naghibi Sistani, M.M.; Hataminia, Z.; Hajiahmadi, M.; Khodadadi, E. Nine Years’ Trend of Dental Caries and Severe Early Childhood Caries among 3-6-Year-Old Children in Babol, Northern Iran. Electron. Physician 2017, 9, 4683–4688. [Google Scholar] [CrossRef]
- Szöke, J.; Petersen, P.E. Changing levels of dental caries over 30 years among children in a Country of central and eastern Europe-the case of Hungary. Oral Health Prev. Dent. 2020, 18, 177–183. [Google Scholar] [CrossRef]
- Ruff, R.R.; Niederman, R. Comparative Effectiveness of School-Based Caries Prevention: A Prospective Cohort Study. BMC Oral Health 2018, 18, 53. [Google Scholar] [CrossRef]
- Campus, G.; Cocco, F.; Ottolenghi, L.; Cagetti, M.G. Comparison of ICDAS, CAST, Nyvad’s Criteria, and WHO-DMFT for Caries Detection in a Sample of Italian Schoolchildren. Int. J. Environ. Res. Public Health 2019, 16, 4120. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry. Caries-Risk Assessment and Management for Infants, Children, and Adolescents. In The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2023; pp. 301–307. [Google Scholar]
- Hummel, R.; Akveld, N.A.E.; Bruers, J.J.M.; Van Der Sanden, W.J.M.; Su, N.; Van Der Heijden, G.J.M.G. Caries Progression Rates Revisited: A Systematic Review. J. Dent. Res. 2019, 98, 746–754. [Google Scholar] [CrossRef]
- McCarra, C.; Olegário, I.C.; O’Connell, A.C.; Leith, R. Prevalence of hypomineralised second primary molars (HSPM): A systematic review and meta-analysis. Int. J. Paediatr. Dent. 2022, 32, 367–382. [Google Scholar] [CrossRef]
- Mc Carra, C.; Olegário, I.C.; O’Connell, A.C.; Leith, R. General dentists’ perceptions and clinical management of hypomineralised second primary molars (HSPM) in Ireland. Eur. Arch. Paediatr. Dent. 2023, 24, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Tarhuni, H.; Benghasheer, H.F.; Naser, Y.; Arheiam, A. Molar incisor hypomineralisation: A survey of awareness and management strategies among Libyan dentists in Benghazi. Int. J. Paediatr. Dent. 2024, 34, 554–566. [Google Scholar] [CrossRef]
- Goyal, A.; Dhareula, A.; Gauba, K.; Bhatia, S.K. Prevalence, Defect Characteristics and Distribution of Other Phenotypes in 3- to 6-Year-Old Children Affected with Hypomineralised Second Primary Molars. Eur. Arch. Paediatr. Dent. 2019, 20, 585–593. [Google Scholar] [CrossRef]
- Negre-Barber, A.; Montiel-Company, J.M.; Boronat-Catalá, M.; Catalá-Pizarro, M.; Almerich-Silla, J.M. Hypomineralized Second Primary Molars as Predictor of Molar Incisor Hypomineralization. Sci. Rep. 2016, 6, 31929. [Google Scholar] [CrossRef]
- Reyes, M.R.T.; Fatturi, A.L.; Menezes, J.V.N.B.; Fraiz, F.C.; Assunção, L.R.D.S.; Souza, J.F.D. Demarcated Opacity in Primary Teeth Increases the Prevalence of Molar Incisor Hypomineralization. Braz. Oral Res. 2019, 33, e048. [Google Scholar] [CrossRef]
- Kalkani, M.; Balmer, R.C.; Homer, R.M.; Day, P.F.; Duggal, M.S. Molar Incisor Hypomineralisation: Experience and Perceived Challenges among Dentists Specialising in Paediatric Dentistry and a Group of General Dental Practitioners in the UK. Eur. Arch. Paediatr. Dent. 2016, 17, 81–88. [Google Scholar] [CrossRef]
- Bekes, K.; Buchegger, K.; Stamm, T.; Elhennawy, K. Dental Students’ Knowledge, Attitudes and Beliefs Regarding Molar Incisor Hypomineralization (MIH): A Survey in Vienna, Austria. JMDH 2021, 14, 2881–2889. [Google Scholar] [CrossRef]
| n (%) | |
|---|---|
| Number of respondents | 315/1000 (31.50%) |
| Number of paediatric patients annually treated | |
| 0–100 | 263 (83.49) |
| 101–200 | 36 (11.43) |
| >200 | 16 (5.08) |
| Percentage of paediatric patients annually treated | |
| 1–25% | 259 (82.22) |
| 26–50% | 16 (5.08) |
| 51–75% | 13 (4.13) |
| 76–100% | 27 (8.57) |
| Percentage of children aged 6–9 among paediatric patients annually treated | |
| 0–25% | 174 (55.24) |
| 26–50% | 128 (40.63) |
| 51–75% | 8 (2.54) |
| 76–100% | 5 (1.59) |
| Percentage of caries-free children aged 6–9 | |
| None | 33 (10.48) |
| 1–25% | 226 (71.75) |
| 26–50% | 33 (10.48) |
| 51–75% | 18 (5.71) |
| 76–100% | 5 (1.59) |
| Frequency of scheduled check-up visits for children aged 6–9 | |
| yearly | 57 (18.10) |
| every six months | 151 (47.94) |
| every three months | 75 (23.81) |
| not periodically but only out of necessity | 32 (10.16) |
| N (%) | |
|---|---|
| Percentage of opacities on second primary molars | |
| None | 57 (18.10) |
| 1–25% | 187 (59.37) |
| 26–50% | 47 (14.92) |
| 51–75% | 19 (6.03) |
| 76–100% | 5 (1.59) |
| Presence of opacities on the first permanent molars, in patients with opacities on the second primary molars | |
| Yes | 188 (59.68) |
| No | 127 (40.32) |
| Percentage of opacities on the first permanent molars in patients with opacities on the second primary molars | |
| 1–25% | 82 (43.62) |
| 26–50% | 58 (30.85) |
| 51–75% | 48 (25.53) |
| 76–100% | 0 (0) |
| Presence of opacities on the first permanent molars, in patients without opacities on the second primary molars | |
| Yes | 156 (49.52) |
| No | 159 (50.48) |
| Percentage of opacities on the first permanent molars in patients without opacities on the second primary molars | |
| 1–25% | 115 (73.72) |
| 26–50% | 14 (8.97) |
| 51–75% | 27 (17.31) |
| 76–100% | 0 (0) |
| Reported Occurrence of Opacities on the First Permanent Molars, in Patients with Opacities on the Second Primary Molars | Reported Occurrence of Opacities on the First Permanent Molars, in Patients without Opacities on the Second Primary Molars | ||
|---|---|---|---|
| n (%) | n (%) | p-Value | |
| 188 (59.68) | 156 (49.52) | ||
| 1–25% | 82 (43.62) | 115 (73.72) | 0.00001 * (OR 0.28) |
| 26–50% | 58 (30.85) | 14 (8.97) | 0.00001 * (OR 4.53) |
| 51–75% | 48 (25.53) | 27 (17.31) | 0.06 (OR 1.64) |
| 76–100% | 0 (0) | 0 (0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bardellini, E.; Conti, G.; Veneri, F.; Majorana, A.; Amadori, F. Awareness of Molar Incisor Hypomineralisation (MIH) and Hypomineralised Second Primary Molars (HSPMs) among Northern Italian Dentists: A Questionnaire Survey. Dent. J. 2024, 12, 271. https://doi.org/10.3390/dj12080271
Bardellini E, Conti G, Veneri F, Majorana A, Amadori F. Awareness of Molar Incisor Hypomineralisation (MIH) and Hypomineralised Second Primary Molars (HSPMs) among Northern Italian Dentists: A Questionnaire Survey. Dentistry Journal. 2024; 12(8):271. https://doi.org/10.3390/dj12080271
Chicago/Turabian StyleBardellini, Elena, Giulio Conti, Federica Veneri, Alessandra Majorana, and Francesca Amadori. 2024. "Awareness of Molar Incisor Hypomineralisation (MIH) and Hypomineralised Second Primary Molars (HSPMs) among Northern Italian Dentists: A Questionnaire Survey" Dentistry Journal 12, no. 8: 271. https://doi.org/10.3390/dj12080271






