Fracture Resistance of Provisional Crowns: A Finite Element Analysis of a Semi-Permanent Resin—A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
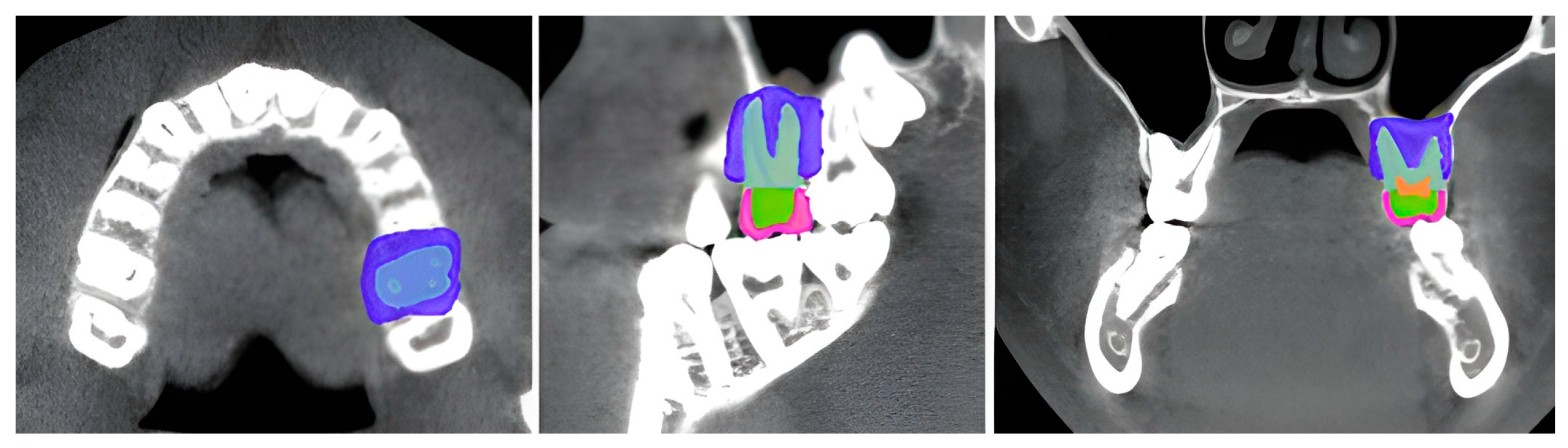
2.2.1. Model Preparation
2.2.2. Finite Element Model (FEM) Preprocessing
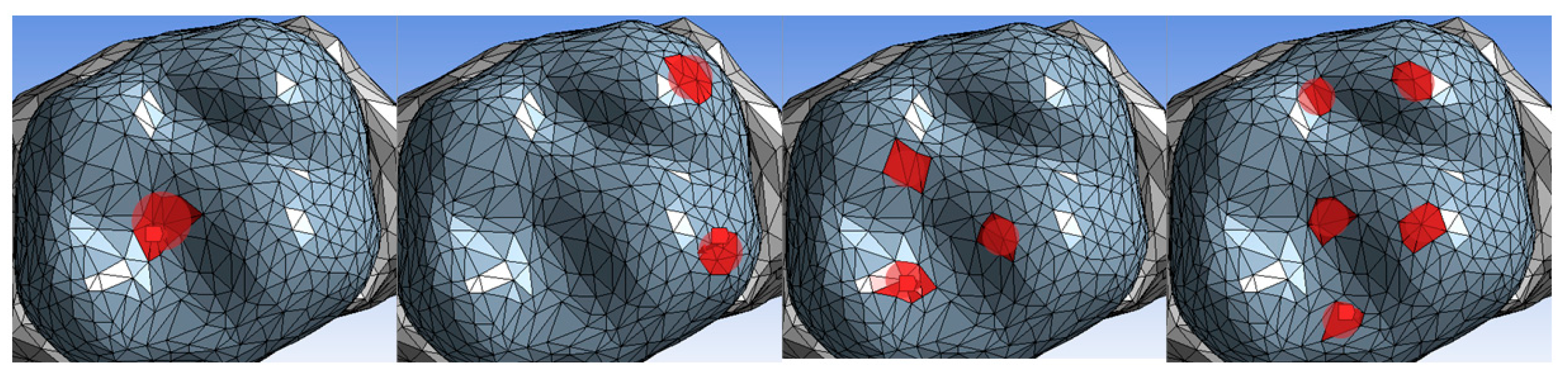
2.2.3. Stress Analysis
2.2.4. Data Analysis
3. Results
3.1. Stress Distribution
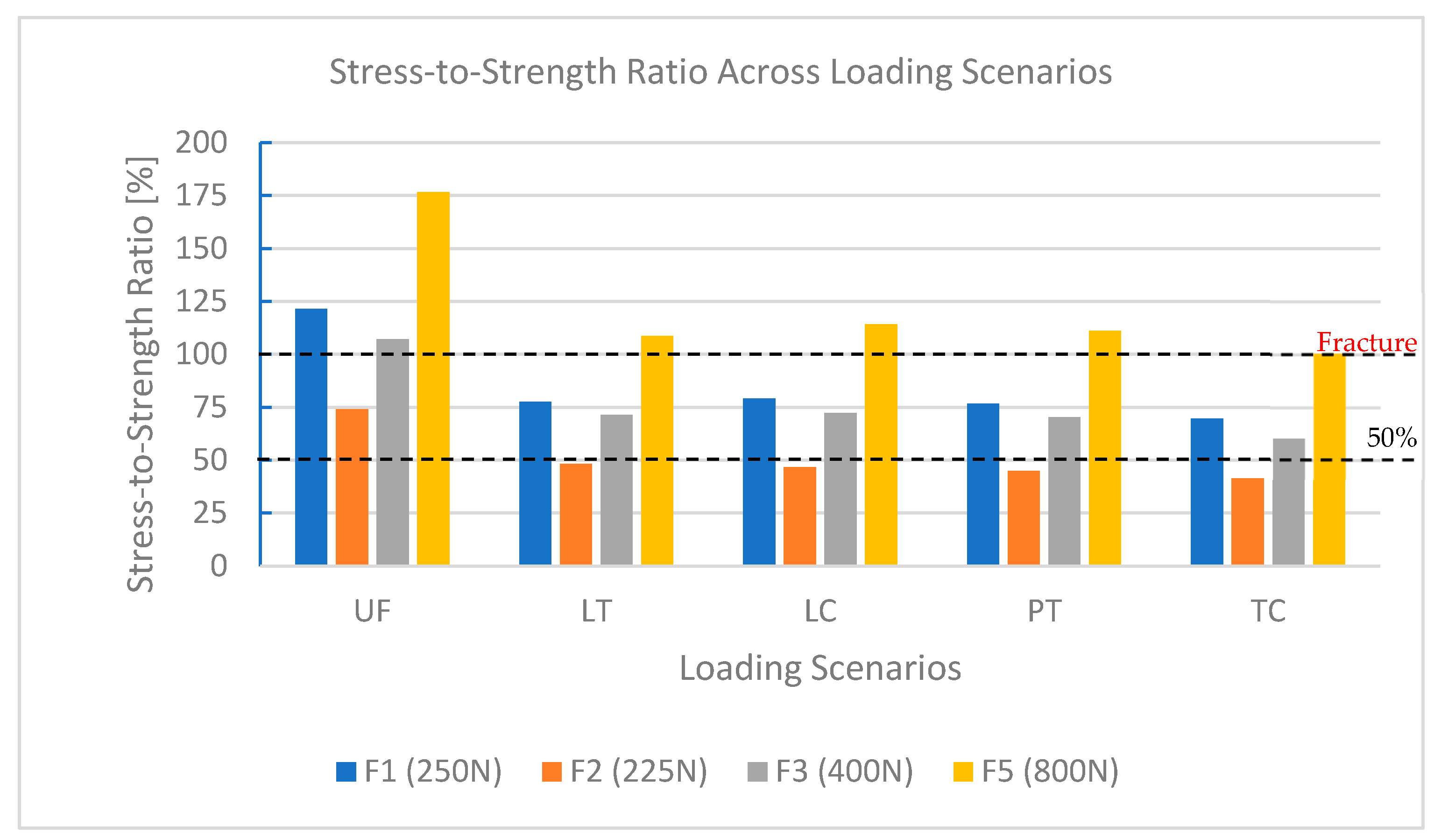
3.2. Stress-to-Strength Ratio (SSR)
3.3. Performance Under Bruxism Loads (800 N)
4. Discussion
4.1. Reliability of FEM Methodology
4.2. Interpretation of Findings
4.3. Material Performance and Clinical Implications
4.4. Material Longevity and Manufacturer Claims
4.5. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| FEA | Finite Element Analysis |
| FEM | Finite Element Method |
| PMMA | Polymethyl Methacrylate |
| CAD | Computer-Aided Design |
| CAM | Computer-Aided Manufacturing |
| NRRD | Nearly Raw Raster Data (file format for volumetric imaging) |
| SSR | Stress-to-Strength Ratio |
References
- Niem, T.; Youssef, N.; Wöstmann, B. Influence of Accelerated Ageing on the Physical Properties of CAD/CAM Restorative Materials. Clin. Oral Investig. 2019, 24, 2415–2425. [Google Scholar] [CrossRef] [PubMed]
- Abad-Coronel, C.; Carrera, E.; Mena Córdova, N.; Fajardo, J.I.; Aliaga, P. Comparative Analysis of Fracture Resistance between CAD/CAM Materials for Interim Fixed Prosthesis. Materials 2021, 14, 7791. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.B.; Rauch, A.; Haas, L.; Rosentritt, M. Influence of Provisional Cementation on the Stability of Adhesively Bonded Resin-Based Composite Crowns. Am. J. Dent. 2024, 37, 183–186. [Google Scholar]
- Zieliński, G.; Pająk, A.; Wójcicki, M. Global Prevalence of Sleep Bruxism and Awake Bruxism in Pediatric and Adult Populations: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 4259. [Google Scholar] [CrossRef] [PubMed]
- Kayumi, S.; Takayama, Y.; Yokoyama, A.; Ueda, N. Effect of Bite Force in Occlusal Adjustment of Dental Implants on the Distribution of Occlusal Pressure: Comparison among Three Bite Forces in Occlusal Adjustment. Int. J. Implant. Dent. 2015, 1, 14. [Google Scholar] [CrossRef]
- Sadek, H.M.A.; El-Banna, A. Biaxial Flexural Strength of Different Provisional Restorative Materials under Chemo-Mechanical Aging: An in Vitro Study. J. Prosthodont. 2024, 33, 149–156. [Google Scholar] [CrossRef]
- Elashkar, M.; Aboushady, Y.; Ihab, M.; El Halawani, M.T. Evaluation of the Marginal Fit and Fracture Resistance of Interim Restorations Fabricated Using Different Techniques: An in Vitro Study. BMC Oral Health 2025, 25, 354. [Google Scholar] [CrossRef]
- Sulaiman, T.A.; Suliman, A.A.; Mohamed, E.A.; Rodgers, B.; Altak, A.; Johnston, W.M. Optical Properties of Bisacryl-, Composite-, Ceramic- Resin Restorative Materials: An Aging Simulation Study. J. Esthet. Restor. Dent. 2021, 33, 913–918. [Google Scholar] [CrossRef]
- Dureja, I.; Yadav, B.; Malhotra, P.; Dabas, N.; Bhargava, A.; Pahwa, R. A Comparative Evaluation of Vertical Marginal Fit of Provisional Crowns Fabricated by Computer-Aided Design/Computer-Aided Manufacturing Technique and Direct (Intraoral Technique) and Flexural Strength of the Materials: An in Vitro Study. J. Indian Prosthodont. Soc. 2018, 18, 314–320. [Google Scholar] [CrossRef]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othman, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and Mechanical Properties of 3D-Printed Provisional Crowns and Fixed Dental Prosthesis Resins Compared to CAD/CAM Milled and Conventional Provisional Resins: A Systematic Review and Meta-Analysis. Polymers 2022, 14, 2691. [Google Scholar] [CrossRef]
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef] [PubMed]
- Saisadan, D.; Manimaran, P.; Meenapriya, P.K. In Vitro Comparative Evaluation of Mechanical Properties of Temporary Restorative Materials Used in Fixed Partial Denture. J. Pharm. Bioallied Sci. 2016, 8, S105–S109. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Guardado, W.E.; Rivera-Muñoz, E.M.; Serrano-Bello, J.; Alvarez-Perez, M.A.; Domínguez-Pérez, R.A.; Salmerón-Valdés, E.N.; Vázquez Vázquez, F.C.; Chanes-Cuevas, O.A.; Millán-Malo, B.; Peza-Ledesma, C.L.; et al. Physical and Structural Characterization of Bis-Acryl Composite Resin. Sci. Rep. 2024, 14, 8075. [Google Scholar] [CrossRef] [PubMed]
- DMG Chemisch-Pharmazeutische Fabrik GmbH. Luxacrown; DMG Chemisch-Pharmazeutische Fabrik GmbH: Hamburg, Germany, 2016. [Google Scholar]
- Schwantz, J.; Oliveira-Ogliari, A.; Meereis, C.; Leal, F.; Ogliari, F.; Moraes, R. Characterization of Bis-Acryl Composite Resins for Provisional Restorations. Braz. Dent. J. 2017, 28, 354–361. [Google Scholar] [CrossRef]
- Al-Humood, H.; Alfaraj, A.; Yang, C.-C.; Levon, J.; Chu, T.-M.G.; Lin, W.-S. Marginal Fit, Mechanical Properties, and Esthetic Outcomes of CAD/CAM Interim Fixed Dental Prostheses (FDPs): A Systematic Review. Materials 2023, 16, 1996. [Google Scholar] [CrossRef]
- Li, F.; Shao, Y.; Han, T.; Li, J.; Yan, X. Finite Element Analysis of Endodontically Treated Premolars without Ferrule Restored with One-Piece Glass Fiber Post and Core in Combination with Different Inner Shoulder Retention Form Systems. J. Mech. Behav. Biomed. Mater. 2023, 143, 105912. [Google Scholar] [CrossRef]
- Reeponmaha, T.; Angwaravong, O.; Angwarawong, T. Comparison of Fracture Strength after Thermo-Mechanical Aging between Provisional Crowns Made with CAD/CAM and Conventional Method. J. Adv. Prosthodont. 2020, 12, 218–224. [Google Scholar] [CrossRef]
- Abdullah, A.O.; Pollington, S.; Liu, Y. Comparison between Direct Chairside and Digitally Fabricated Temporary Crowns. Dent. Mater. J. 2018, 37, 957–963. [Google Scholar] [CrossRef]
- Katayama, Y.; Ohashi, K.; Iwasaki, T.; Kameyama, Y.; Wada, Y.; Miyake, K.; Tanimoto, Y.; Nihei, T. A Study on the Characteristics of Resin Composites for Provisional Restorations. Dent. Mater. J. 2022, 41, 256–265. [Google Scholar] [CrossRef]
- Shibasaki, S.; Takamizawa, T.; Suzuki, T.; Nojiri, K.; Tsujimoto, A.; Barkmeier, W.W.; Latta, M.A.; Miyazaki, M. Influence of Different Curing Modes on Polymerization Behavior and Mechanical Properties of Dual-Cured Provisional Resins. Oper. Dent. 2017, 42, 526–536. [Google Scholar] [CrossRef]
- Angwarawong, T.; Reeponmaha, T.; Angwaravong, O. Influence of Thermomechanical Aging on Marginal Gap of CAD-CAM and Conventional Interim Restorations. J. Prosthet. Dent. 2020, 124, 566.e1–566.e6. [Google Scholar] [CrossRef] [PubMed]
- Tüfekçi, B.B.; Yeşil, Z. Examination of the Effect of Aging Process on Marginal Fit and Fractute Strength of Temporary Crowns Prepared from Different Materials. Heliyon 2024, 10, e26737. [Google Scholar] [CrossRef]
- Alzahrani, S.J.; Hajjaj, M.S.; Azhari, A.A.; Ahmed, W.M.; Yeslam, H.E.; Carvalho, R.M. Mechanical Properties of Three-Dimensional Printed Provisional Resin Materials for Crown and Fixed Dental Prosthesis: A Systematic Review. Bioengineering 2023, 10, 663. [Google Scholar] [CrossRef] [PubMed]
- LourenÇo, A.L.; Jager, N.D.; Prochnow, C.; Milbrandt Dutra, D.A.; Kleverlaan, C.J. Young’s Modulus and Poisson Ratio of Composite Materials: Influence of Wet and Dry Storage. Dent. Mater. J. 2020, 39, 657–663. [Google Scholar] [CrossRef]
- Astudillo-Rubio, D.; Delgado-Gaete, A.; Bellot-Arcís, C.; Montiel-Company, J.M.; Pascual-Moscardó, A.; Almerich-Silla, J.M. Mechanical Properties of Provisional Dental Materials: A Systematic Review and Meta-Analysis. PLoS ONE 2018, 13, e0193162. [Google Scholar] [CrossRef]
- Takamizawa, T.; Barkmeier, W.W.; Tsujimoto, A.; Scheidel, D.; Erickson, R.L.; Latta, M.A.; Miyazaki, M. Mechanical Properties and Simulated Wear of Provisional Resin Materials. Oper. Dent. 2015, 40, 603–613. [Google Scholar] [CrossRef]
- DMG Chemisch-Pharmazeutische Fabrik GmbH. Luxatemp; DMG Chemisch-Pharmazeutische Fabrik GmbH: Hamburg, Germany, 2017. [Google Scholar]
- 3M ESPE. Protemp 4; 3M ESPE: Seefeld, Germany, 2011. [Google Scholar]
- Ivoclar Vivadent AG. Telio Lab Telio CAD; Ivoclar Vivadent AG: Schaan, Liechtenstein, 2010. [Google Scholar]
- Kikinis, R.; Pieper, S.; Vosburgh, K. 3D Slicer: A Platform for Subject-Specific Image Analysis, Visualization, and Clinical Support. In Intraoperative Imaging and Image-Guided Therapy; Jolesz, F.A., Ed.; Springer: New York, NY, USA, 2014; pp. 277–289. [Google Scholar]
- 3D Slicer Community 3D Slicer Sample Data: PreDentalSurgery.gipl.gz, [Online Resource]. 2024. Available online: https://github.com/Slicer/SlicerTestingData/releases/download/SHA256/4cdc3dc35519bb57daeef4e5df89c00849750e778809e94971d3876f95cc7bbd (accessed on 21 March 2025).
- Liao, C.-W.; Fuh, L.-J.; Shen, Y.-W.; Huang, H.-L.; Kuo, C.-W.; Tsai, M.-T.; Hsu, J.-T. Self-Assembled Micro-Computed Tomography for Dental Education. PLoS ONE 2018, 13, e0209698. [Google Scholar] [CrossRef]
- Dot, G.; Chaurasia, A.; Dubois, G.; Savoldelli, C.; Haghighat, S.; Azimian, S.; Taramsari, A.R.; Sivaramakrishnan, G.; Issa, J.; Dubey, A.; et al. DentalSegmentator: Robust Open Source Deep Learning-Based CT and CBCT Image Segmentation. J. Dent. 2024, 147, 105130. [Google Scholar] [CrossRef]
- Huang, L.; Nemoto, R.; Okada, D.; Shin, C.; Saleh, O.; Oishi, Y.; Takita, M.; Nozaki, K.; Komada, W.; Miura, H. Investigation of Stress Distribution within an Endodontically Treated Tooth Restored with Different Restorations. J. Dent. Sci. 2022, 17, 1115–1124. [Google Scholar] [CrossRef]
- Shetty, H.; Shetty, S.; Kakade, A.; Shetty, A.; Karobari, M.I.; Pawar, A.M.; Marya, A.; Heboyan, A.; Venugopal, A.; Nguyen, T.H.; et al. Three-Dimensional Semi-Automated Volumetric Assessment of the Pulp Space of Teeth Following Regenerative Dental Procedures. Sci. Rep. 2021, 11, 21914. [Google Scholar] [CrossRef]
- Grzebieluch, W.; Będziński, R.; Czapliński, T.; Kaczmarek, U. The Mechanical Properties of Human Dentin for 3-D Finite Element Modeling: Numerical and Analytical Evaluation. Adv. Clin. Exp. Med. 2017, 26, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Bi, S.; Shi, G. The Crucial Role of Periodontal Ligament’s Poisson’s Ratio and Tension-Compression Asymmetric Moduli on the Evaluation of Tooth Displacement and Stress State of Periodontal Ligament. J. Mech. Behav. Biomed. Mater. 2023, 148, 106217. [Google Scholar] [CrossRef]
- Martinez-Mondragon, M.; Urriolagoitia-Sosa, G.; Romero-Ángeles, B.; Maya-Anaya, D.; Martínez-Reyes, J.; Gallegos-Funes, F.J.; Urriolagoitia-Calderón, G.M. Numerical Analysis of Zirconium and Titanium Implants under the Effect of Critical Masticatory Load. Materials 2022, 15, 7843. [Google Scholar] [CrossRef]
- He, J.; Zheng, Z.; Wu, M.; Zheng, C.; Zeng, Y.; Yan, W. Influence of Restorative Material and Cement on the Stress Distribution of Endocrowns: 3D Finite Element Analysis. BMC Oral Health 2021, 21, 495. [Google Scholar] [CrossRef]
- Petrescu, S.-M.-S.; Țuculină, M.J.; Popa, D.L.; Duță, A.; Sălan, A.I.; Voinea Georgescu, R.; Diaconu, O.A.; Turcu, A.A.; Mocanu, H.; Nicola, A.G.; et al. Modeling and Simulating an Orthodontic System Using Virtual Methods. Diagnostics 2022, 12, 1296. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Alharbi, S.; Cuijpers, V.M.J.I.; Osman, R.B.; Wismeijer, D. Three-Dimensional Evaluation of Marginal and Internal Fit of 3D-Printed Interim Restorations Fabricated on Different Finish Line Designs. J. Prosthodont. Res. 2018, 62, 218–226. [Google Scholar] [CrossRef]
- Giannakopoulos, N.N.; Hellmann, D.; Schmitter, M.; Krüger, B.; Hauser, T.; Schindler, H.J. Neuromuscular Interaction of Jaw and Neck Muscles during Jaw Clenching. J. Orofac. Pain. 2013, 27, 61–71. [Google Scholar] [CrossRef]
- Pakdel, A.; Whyne, C.; Fialkov, J. Structural Biomechanics of the Craniomaxillofacial Skeleton under Maximal Masticatory Loading: Inferences and Critical Analysis Based on a Validated Computational Model. J. Plast. Reconstr. Aesthetic Surg. JPRAS 2017, 70, 842–850. [Google Scholar] [CrossRef]
- Barrientos, E.; Pelayo, F.; Tanaka, E.; Lamela-Rey, M.; Fernández-Canteli, A.; De Vicente, J. Effects of Loading Direction in Prolonged Clenching on Stress Distribution in the Temporomandibular Joint. J. Mech. Behav. Biomed. Mater. 2020, 112, 104029. [Google Scholar] [CrossRef]
- Benli, M.; Özcan, M. Short-Term Effect of Material Type and Thickness of Occlusal Splints on Maximum Bite Force and Sleep Quality in Patients with Sleep Bruxism: A Randomized Controlled Clinical Trial. Clin. Oral Investig. 2023, 27, 4313–4322. [Google Scholar] [CrossRef]
- Wang, D.; Akbari, A.; Jiang, F.; Liu, Y.; Chen, J. The Effects of Different Types of Periodontal Ligament Material Models on Stresses Computed Using Finite Element Models. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e328–e336. [Google Scholar] [CrossRef]
- Rizk, M.; Niederau, C.; Florea, A.; Kiessling, F.; Morgenroth, A.; Mottaghy, F.M.; Schneider, R.K.; Wolf, M.; Craveiro, R.B. Periodontal Ligament and Alveolar Bone Remodeling during Long Orthodontic Tooth Movement Analyzed by a Novel User-Independent 3D-Methodology. Sci. Rep. 2023, 13, 19919. [Google Scholar] [CrossRef] [PubMed]
- Wendling, M.; Mantovani, G.; Fernandes, B.; Carneiro, D.; Santos, R.; Sánchez-Ayala, A. Occlusal Loading Effect on Stress Distribution of Endodontically Treated Teeth: Finite Element Analysis Study. Eur. J. Prosthodont. Restor. Dent. 2023, 32, 102–108. [Google Scholar] [CrossRef]
- Alghazzawi, T. Relation of Crown Failure Load to Flexural Strength for Three Contemporary Dental Polymers. Polymers 2023, 15, 4312. [Google Scholar] [CrossRef]
- Ellakwa, A.; Raju, R.; Sheng, C.; Rajan, G.; Prusty, B.G. Acoustic Emission and Finite Element Study on the Influence of Cusp Angles on Zirconia Dental Crowns. Dent. Mater. 2020, 36, 1524–1535. [Google Scholar] [CrossRef]
- Reddy, M.; Rajasekar, S.; Abdelmagyd, H.E. Evaluating the Effect of Subcrestal Placement on Platform Switched Short Dental Implants and von Mises Stress in D3 Bone–A 3D FEM Study. Niger. J. Clin. Pract. 2021, 24, 660–666. [Google Scholar] [CrossRef]
- Lahoud, P.; Faghihian, H.; Richert, R.; Jacobs, R.; EzEldeen, M. Finite Element Models: A Road to in-Silico Modeling in the Age of Personalized Dentistry. J. Dent. 2024, 150, 105348. [Google Scholar] [CrossRef]
- Abad-Coronel, C.; Bravo, M.; Tello, S.; Cornejo, E.; Paredes, Y.; Paltan, C.A.; Fajardo, J.I. Fracture Resistance Comparative Analysis of Milled-Derived vs. 3D-Printed CAD/CAM Materials for Single-Unit Restorations. Polymers 2023, 15, 3773. [Google Scholar] [CrossRef] [PubMed]
- Kassis, C.; Khoury, P.; Mehanna, C.Z.; Baba, N.Z.; Bou Chebel, F.; Daou, M.; Hardan, L. Effect of Inlays, Onlays and Endocrown Cavity Design Preparation on Fracture Resistance and Fracture Mode of Endodontically Treated Teeth: An In Vitro Study. J. Prosthodont. 2021, 30, 625–631. [Google Scholar] [CrossRef]
- Corbani, K.; Hardan, L.; Eid, R.; Skienhe, H.; Alharbi, N.; Ozcan, M.; Salameh, Z. Fracture Resistance of Three-Unit Fixed Dental Prostheses Fabricated with Milled and 3D Printed Composite-Based Materials. J. Contemp. Dent. Pract. 2021, 22, 985–990. [Google Scholar]
- El Ghoul, W.A.; Özcan, M.; Ounsi, H.; Tohme, H.; Salameh, Z. Effect of Different CAD-CAM Materials on the Marginal and Internal Adaptation of Endocrown Restorations: An in Vitro Study. J. Prosthet. Dent. 2020, 123, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Juntavee, N.; Juntavee, A.; Srisontisuk, S. Flexural Strength of Various Provisional Restorative Materials for Rehabilitation After Aging. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2022, 32, 20–28. [Google Scholar] [CrossRef]
- Poggio, C.; Dagna, A.; Chiesa, M.; Colombo, M.; Scribante, A. Surface Roughness of Flowable Resin Composites Eroded by Acidic and Alcoholic Drinks. J. Conserv. Dent. 2012, 15, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Abdulmajeed, A.A.; Suliman, A.A.; Selivany, B.J.; Altitinchi, A.; Sulaiman, T.A. Wear and Color Stability of Preheated Bulk-Fill and Conventional Resin Composites. Oper. Dent. 2022, 47, 585–592. [Google Scholar] [CrossRef]
- Barua, S.L.; Poduval, T.; Rani, S.; Jain, N.; Thakur, S. Stress Distribution in Bone around an Implant-Supported Three-Unit Fixed Dental Prosthesis Using Two Different Computer-Aided Designing/Computer-Aided Milling Provisional Crown Materials: Milled Polymethylmethacrylate and Milled Polyetheretherketone—A Finite Element Analysis. Dent. Res. J. 2023, 20, 33. [Google Scholar] [CrossRef]


| Code | Material | Composition | Working Mode | Manufacturer-Claimed Lifespan |
|---|---|---|---|---|
| UF | Unifast Trad (GC, Tokyo, Japan) | PMMA-based resin (powder and liquid) | Direct | Temporary to long-term |
| LT | Luxatemp Star (DMG, Hamburg, Germany) | Bis-acryl composite (44% glass fillers) | Direct | Short-term |
| LC | Luxacrown (DMG, Hamburg, Germany) | Bis-acryl composite (46% glass fillers) | Direct | Semi-permanent (≤5 years) |
| PT | Protemp 4 (3M ESPE, Seefeld, Germany) | Nanofilled composite resin | Direct | Long-term |
| TC | Telio CAD (Ivoclar Vivadent, Liechtenstein, Schaan, Liechtenstein) | Cross-linked PMMA for CAD/CAM | Indirect | Temporary to long-term |
| Material Code | Flexural Strength (MPa) | Elastic Modulus (MPa) | Poisson’s Ratio | Density (g/cm3 at 20 °C) | References |
|---|---|---|---|---|---|
| UF | 73 | 2430 | 0.43 | 0.90 | [27] |
| LT | 119 | 3800 | 0.30 | 1.50 | [28] |
| LC | 115 | 4100 | 0.30 | 1.50 | [14] |
| PT | 113 | 3000 | 0.30 | 1.30 | [29] |
| TC | 130 | 3200 | 0.32 | 1.20 | [30] |
| Structure | Elastic Modulus (MPa) | Poisson’s Ratio | References |
|---|---|---|---|
| Dentin | 16,700 | 0.31 | [37] |
| Bone | 14,700 | 0.30 | [37] |
| Periodontal Ligament | 0.87 | 0.45 | [38] |
| Pulp | 0.0055 | 0.45 | [39] |
| Resin Cement | 16,440 | 0.26 | [40] |
| Material Code | Flexural Resistance (MPa) | Von Mises Stress (MPa) F1, 250 N | Percentage Utilization (F1, %) | Von Mises Stress (MPa) F2, 225 N | Percentage Utilization (F2, %) | Von Mises Stress (MPa) F3, 400 N | Percentage Utilization (F3, %) | Von Mises Stress (MPa) F5, 800 N | Percentage Utilization (F5, %) |
|---|---|---|---|---|---|---|---|---|---|
| UF | 73 | 88.595 | 121.36 | 53.963 | 73.92 | 78.132 | 107.03 | 128.92 | 176.60 |
| LT | 113 | 87.568 | 77.49 | 54.392 | 48.14 | 80.671 | 71.39 | 122.79 | 108.66 |
| LC | 115 | 90.906 | 79.05 | 53.633 | 46.64 | 83.066 | 72.23 | 131.39 | 114.25 |
| PT | 119 | 91.296 | 76.71 | 53.353 | 44.83 | 83.682 | 70.23 | 132.21 | 111.10 |
| TC | 130 | 90.367 | 69.51 | 53.665 | 41.28 | 78.526 | 60.40 | 130.52 | 100.40 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kamel, N.; Habre, P. Fracture Resistance of Provisional Crowns: A Finite Element Analysis of a Semi-Permanent Resin—A Pilot Study. Dent. J. 2025, 13, 137. https://doi.org/10.3390/dj13040137
Kamel N, Habre P. Fracture Resistance of Provisional Crowns: A Finite Element Analysis of a Semi-Permanent Resin—A Pilot Study. Dentistry Journal. 2025; 13(4):137. https://doi.org/10.3390/dj13040137
Chicago/Turabian StyleKamel, Nadine, and Pascale Habre. 2025. "Fracture Resistance of Provisional Crowns: A Finite Element Analysis of a Semi-Permanent Resin—A Pilot Study" Dentistry Journal 13, no. 4: 137. https://doi.org/10.3390/dj13040137
APA StyleKamel, N., & Habre, P. (2025). Fracture Resistance of Provisional Crowns: A Finite Element Analysis of a Semi-Permanent Resin—A Pilot Study. Dentistry Journal, 13(4), 137. https://doi.org/10.3390/dj13040137





