Evaluating Molecular Mechanism of Viral Inhibition of Aerosolized Smart Nano-Enabled Antiviral Therapeutic (SNAT) on SARS-CoV-2-Infected Hamsters
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cells and Virus
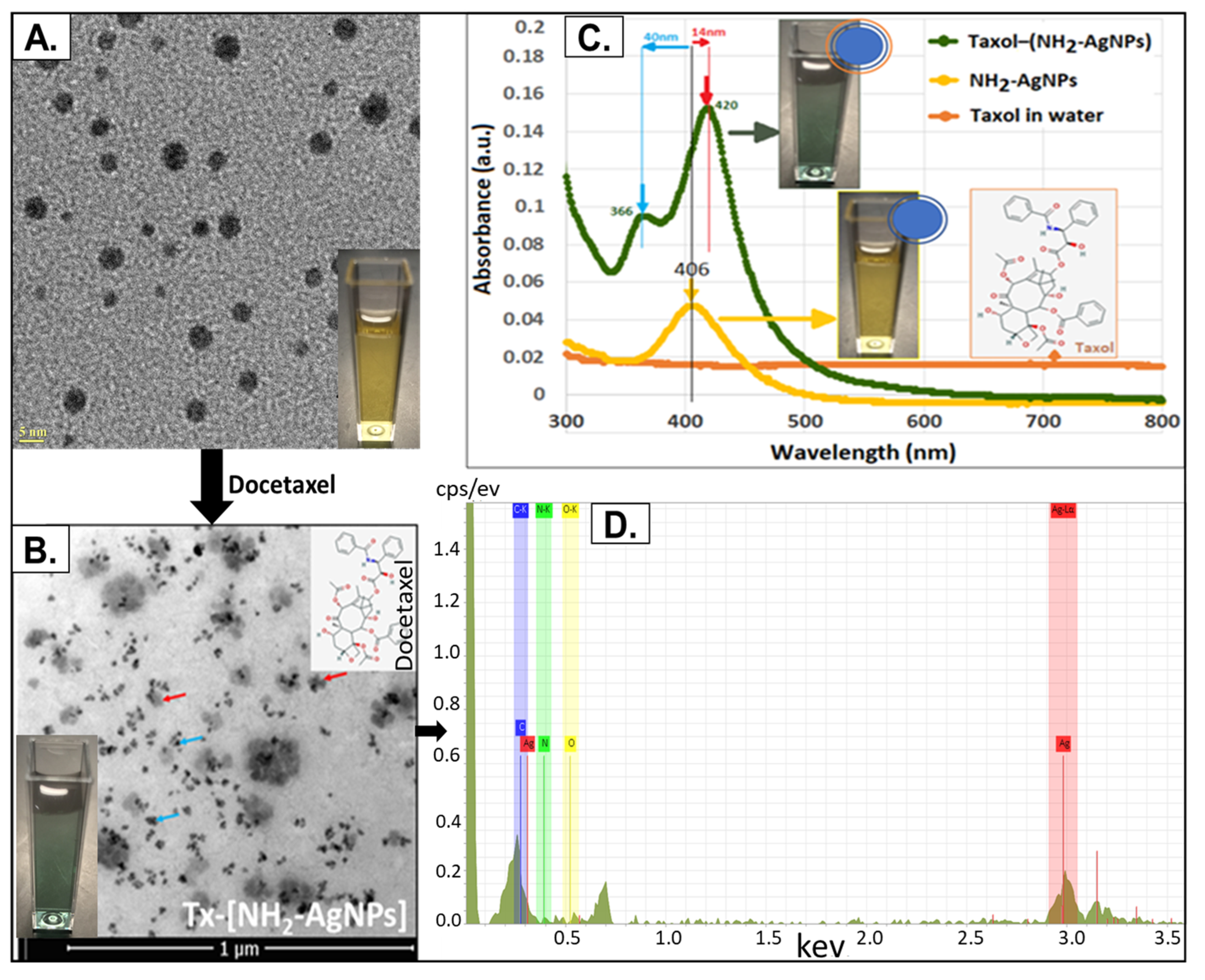
2.2. SNAT Synthesis and Characterization
2.3. Enzyme-Linked Immunosorbent Assay (ELISA)
2.4. Infection Assay Conducted Using Calu-3 Cells
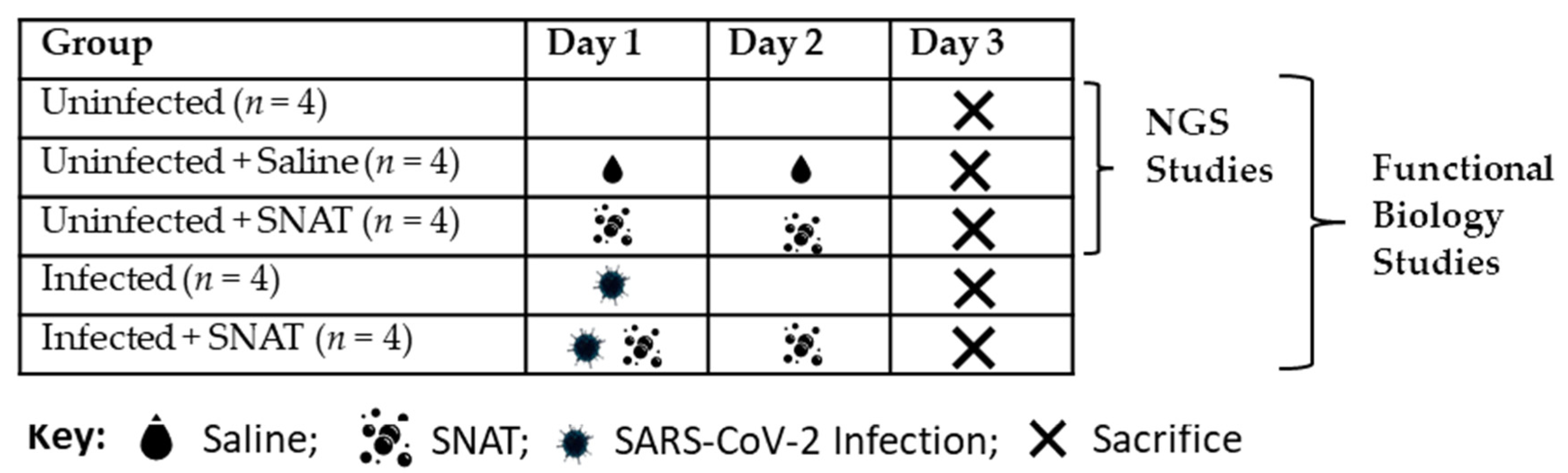
2.5. SNAT Administration and Experiment
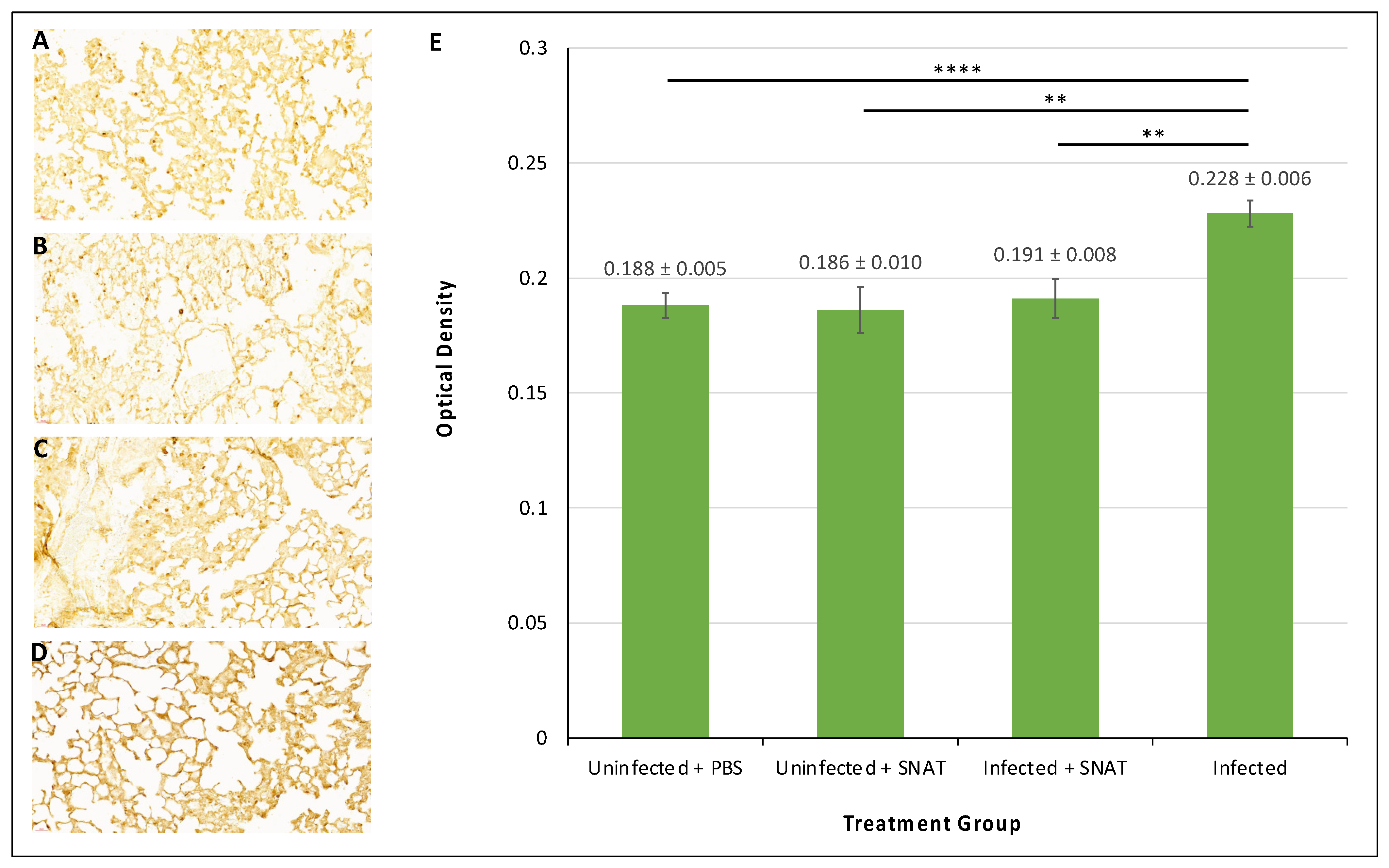
2.6. Preparation of Lung Tissues for Histology and Immunohistochemistry
2.7. RT-qPCR to Monitor Expression of Hamster IL-6
2.8. Whole Transcriptome Assay
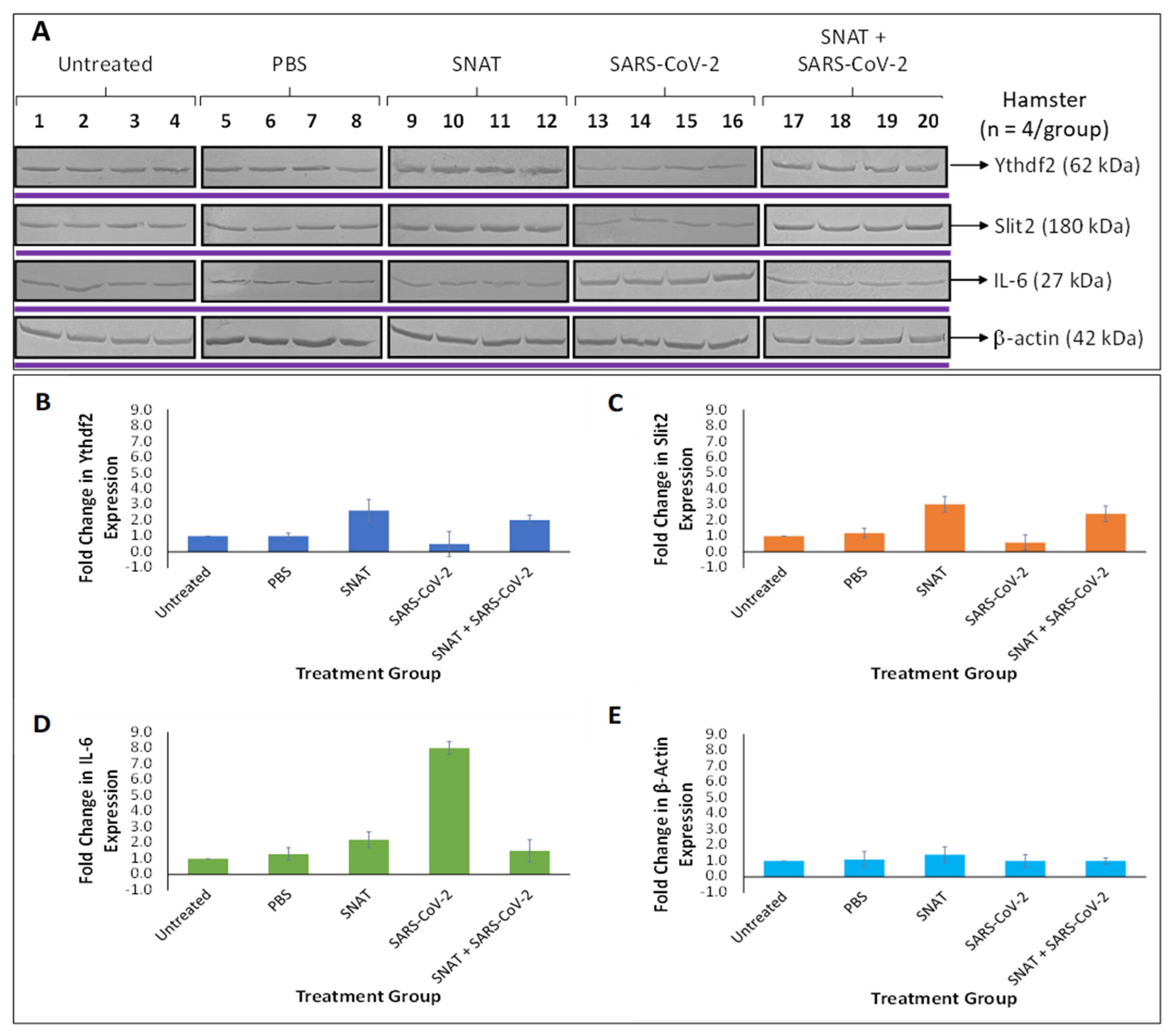
2.9. Dual-Luciferase Reporter Assay and Western Blotting
3. Results
3.1. Characterization of SNAT
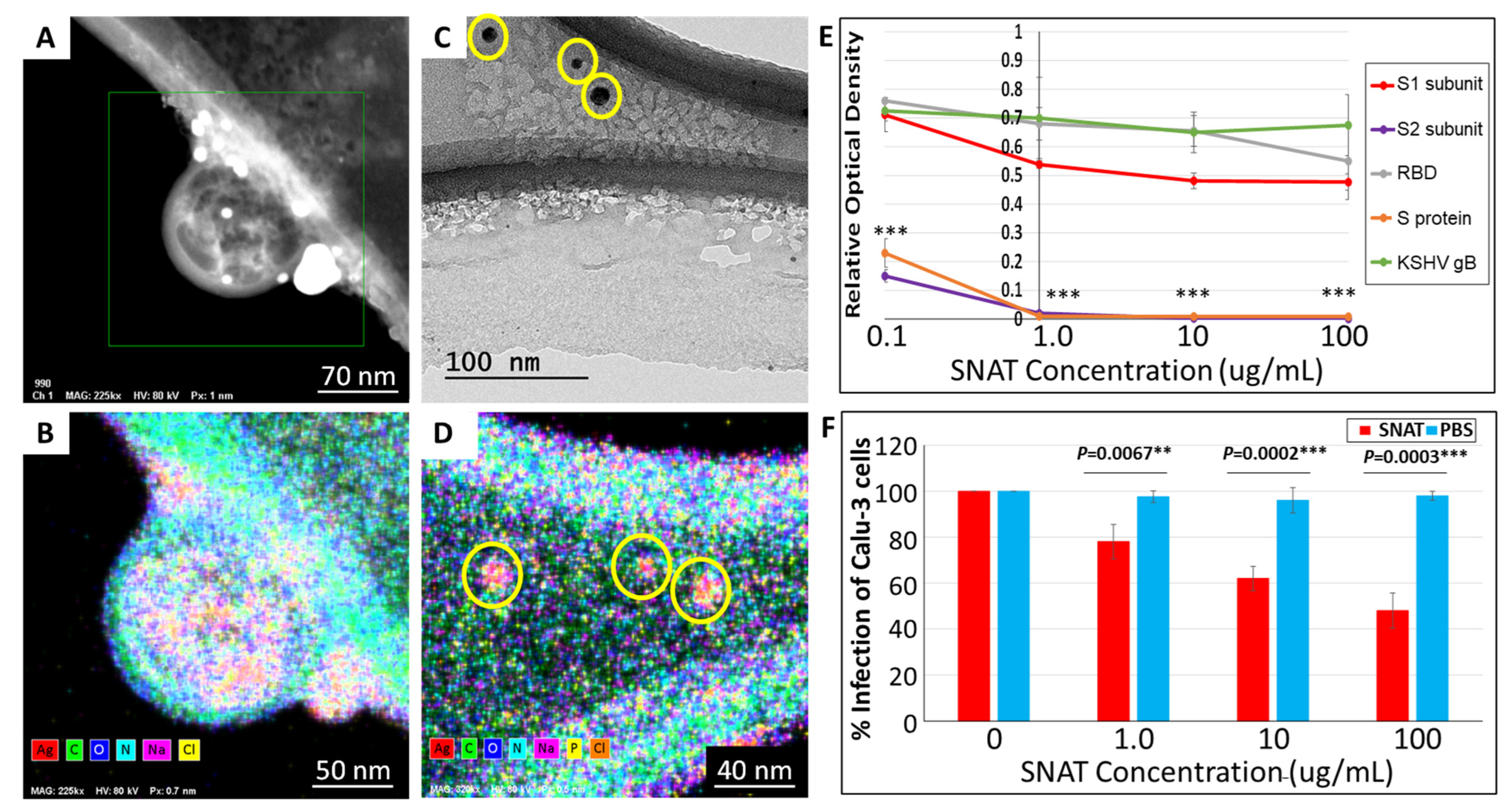
3.2. SNAT Directly Interacts with SARS-CoV-2
3.3. SNAT-Induced Differential Expression of Circulatory miRNAs in Uninfected Hamsters
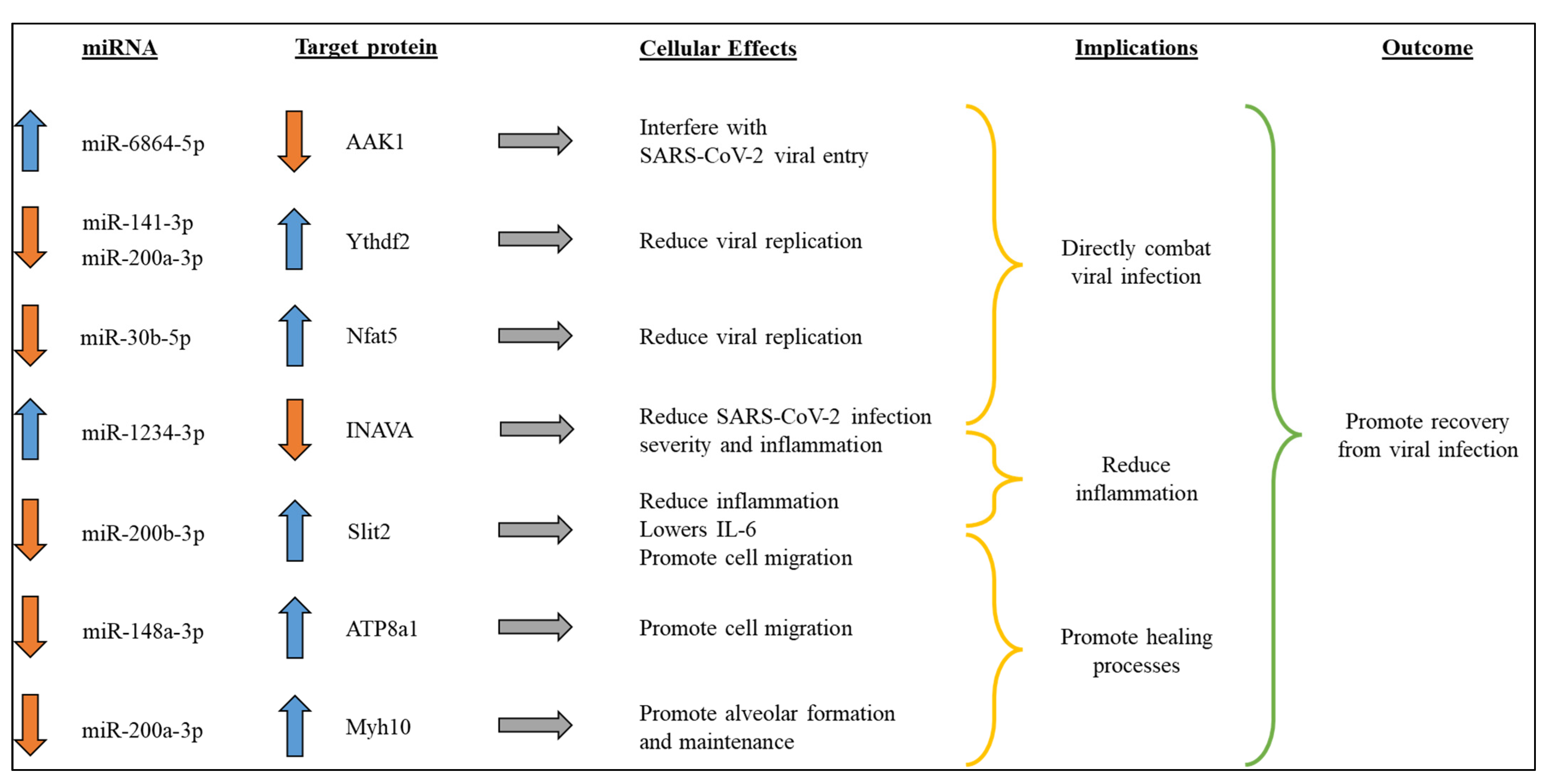
3.4. SNAT Promotes Recovery from SARS-CoV-2 Viral Infection by Altering Select Circulatory miRNAs in Hamsters
4. Discussion
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wilson, B.; Mukundan Geetha, K. Nanomedicine to deliver biological macromolecules for treating COVID-19. Vaccine 2022, 40, 3931–3941. [Google Scholar] [CrossRef]
- Kianpour, M.; Akbarian, M.; Uversky, V.N. Nanoparticles for Coronavirus Control. Nanomaterials 2022, 12, 1602. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.; Wang, S.; Zhang, Q.; Gao, W.; Zhang, L. Nanoparticle approaches against SARS-CoV-2 infection. Curr. Opin. Solid. State Mater. Sci. 2021, 25, 100964. [Google Scholar] [CrossRef]
- Guan, Q.; Zhou, X.; Yang, F.; Zhang, X.; Wang, Y.; Li, W.; Li, X. A novel strategy against hepatitis B virus: Glycyrrhetnic acid conjugated multi-component synergistic nano-drug delivery system for targeted therapy. J. Biomater. Appl. 2023, 37, 1393–1408. [Google Scholar] [CrossRef]
- Souri, M.; Kiani Shahvandi, M.; Chiani, M.; Moradi Kashkooli, F.; Farhangi, A.; Mehrabi, M.R.; Rahmim, A.; Savage, V.M.; Soltani, M. Stimuli-sensitive nano-drug delivery with programmable size changes to enhance accumulation of therapeutic agents in tumors. Drug Deliv. 2023, 30, 2186312. [Google Scholar] [CrossRef]
- Pokhrel, L.R.; Jacobs, Z.L.; Dikin, D.; Akula, S.M. Five nanometer size highly positive silver nanoparticles are bactericidal targeting cell wall and adherent fimbriae expression. Sci. Rep. 2022, 12, 6729. [Google Scholar] [CrossRef]
- Tang, Z.; Ma, Q.; Chen, X.; Chen, T.; Ying, Y.; Xi, X.; Wang, L.; Ma, C.; Shaw, C.; Zhou, M. Recent Advances and Challenges in Nanodelivery Systems for Antimicrobial Peptides (AMPs). Antibiotics 2021, 10, 990. [Google Scholar] [CrossRef] [PubMed]
- Shan, X.; Gong, X.; Li, J.; Wen, J.; Li, Y.; Zhang, Z. Current approaches of nanomedicines in the market and various stage of clinical translation. Acta Pharm. Sin. B 2022, 12, 3028–3048. [Google Scholar] [CrossRef] [PubMed]
- Thapa, R.K.; Kim, J.O. Nanomedicine-based commercial formulations: Current developments and future prospects. J. Pharm. Investig. 2023, 53, 19–33. [Google Scholar] [CrossRef]
- Farjadian, F.; Ghasemi, A.; Gohari, O.; Roointan, A.; Karimi, M.; Hamblin, M.R. Nanopharmaceuticals and nanomedicines currently on the market: Challenges and opportunities. Nanomedicine 2019, 14, 93–126. [Google Scholar] [CrossRef]
- Chakravarty, M.; Vora, A. Nanotechnology-based antiviral therapeutics. Drug Deliv. Transl. Res. 2021, 11, 748–787. [Google Scholar] [CrossRef]
- Rudramurthy, G.R.; Swamy, M.K.; Sinniah, U.R.; Ghasemzadeh, A. Nanoparticles: Alternatives Against Drug-Resistant Pathogenic Microbes. Molecules 2016, 21, 836. [Google Scholar] [CrossRef]
- Jeon, W.J.; Lee, H.K.; Na, Y.G.; Jung, M.; Han, S.C.; Hwang, J.H.; Jung, E.; Hwang, D.; Shin, J.S.; Cho, C.W. Antiviral Lipid Nanocarrier Loaded with Remdesivir Effective Against SARS-CoV-2 in vitro Model. Int. J. Nanomed. 2023, 18, 1561–1575. [Google Scholar] [CrossRef]
- Onoue, S.; Yamada, S.; Chan, H.K. Nanodrugs: Pharmacokinetics and safety. Int. J. Nanomed. 2014, 9, 1025–1037. [Google Scholar] [CrossRef]
- Reagen, S.; Zhao, J.X. Analysis of Nanomaterials on Biological and Environmental Systems and New Analytical Methods for Improved Detection. Int. J. Mol. Sci. 2022, 23, 6331. [Google Scholar] [CrossRef]
- Bonamy, C.; Pesnel, S.; Ben Haddada, M.; Gorgette, O.; Schmitt, C.; Morel, A.L.; Sauvonnet, N. Impact of Green Gold Nanoparticle Coating on Internalization, Trafficking, and Efficiency for Photothermal Therapy of Skin Cancer. ACS Omega 2023, 8, 4092–4105. [Google Scholar] [CrossRef]
- Pokhrel, L.R.; Williams, F.; Cook, P.P.; O’Rourke, D.; Murray, G.; Akula, S.M. Preclinical efficacy and safety of novel SNAT against SARS-CoV-2 using a hamster model. Drug Deliv. Transl. Res. 2022, 12, 3007–3016. [Google Scholar] [CrossRef]
- Jeremiah, S.S.; Miyakawa, K.; Morita, T.; Yamaoka, Y.; Ryo, A. Potent antiviral effect of silver nanoparticles on SARS-CoV-2. Biochem. Biophys. Res. Commun. 2020, 533, 195–200. [Google Scholar] [CrossRef]
- Atherton, E.; Hu, Y.; Brown, S.; Papiez, E.; Ling, V.; Colvin, V.L.; Borton, D.A. A 3D in vitro model of the device-tissue interface: Functional and structural symptoms of innate neuroinflammation are mitigated by antioxidant ceria nanoparticles. J. Neural Eng. 2022, 19, 036004. [Google Scholar] [CrossRef]
- Chen, M.; Kim, B.; Robertson, N.; Mondal, S.K.; Medarova, Z.; Moore, A. Co-administration of temozolomide (TMZ) and the experimental therapeutic targeting miR-10b, profoundly affects the tumorigenic phenotype of human glioblastoma cells. Front. Mol. Biosci. 2023, 10, 1179343. [Google Scholar] [CrossRef]
- Walker, L.R.; Hussein, H.A.M.; Akula, S.M. Disintegrin-like domain of glycoprotein B regulates Kaposi’s sarcoma-associated herpesvirus infection of cells. J. Gen. Virol. 2014, 95, 1770–1782. [Google Scholar] [CrossRef]
- Yang, S.J.; Wei, T.C.; Hsu, C.H.; Ho, S.N.; Lai, C.Y.; Huang, S.F.; Chen, Y.Y.; Liu, S.J.; Yu, G.Y.; Dou, H.Y. Characterization of Virus Replication, Pathogenesis, and Cytokine Responses in Syrian Hamsters Inoculated with SARS-CoV-2. J. Inflamm. Res. 2021, 14, 3781–3795. [Google Scholar] [CrossRef]
- Cheng, Y.; Zheng, D.; Zhang, D.; Guo, D.; Wang, Y.; Liu, W.; Liang, L.; Hu, J.; Luo, T. Molecular recognition of SARS-CoV-2 spike protein with three essential partners: Exploring possible immune escape mechanisms of viral mutants. J. Mol. Model. 2023, 29, 109. [Google Scholar] [CrossRef]
- Hussein, H.A.M.; Walker, L.R.; Akula, S.M. KSHV gB associated RGD interactions promote attachment of cells by inhibiting the potential migratory signals induced by the disintegrin-like domain. BMC Cancer 2016, 16, 148. [Google Scholar] [CrossRef]
- Qiu, Y.; Ye, X.; Zhang, H.M.; Hanson, P.; Zhao, G.; Tong, L.; Xie, R.; Yang, D. Cleavage of osmosensitive transcriptional factor NFAT5 by Coxsackieviral protease 2A promotes viral replication. PLoS Pathog. 2017, 13, e1006744. [Google Scholar] [CrossRef]
- Xu, J.; Cai, Y.; Ma, Z.; Jiang, B.; Liu, W.; Cheng, J.; Guo, N.; Wang, Z.; Sealy, J.E.; Song, C.; et al. The RNA helicase DDX5 promotes viral infection via regulating N6-methyladenosine levels on the DHX58 and NFkappaB transcripts to dampen antiviral innate immunity. PLoS Pathog. 2021, 17, e1009530. [Google Scholar] [CrossRef]
- Karim, M.; Saul, S.; Ghita, L.; Sahoo, M.K.; Ye, C.; Bhalla, N.; Lo, C.W.; Jin, J.; Park, J.G.; Martinez-Gualda, B.; et al. Numb-associated kinases are required for SARS-CoV-2 infection and are cellular targets for antiviral strategies. Antiviral Res. 2022, 204, 105367. [Google Scholar] [CrossRef]
- Luong, P.; Hedl, M.; Yan, J.; Zuo, T.; Fu, T.M.; Jiang, X.; Thiagarajah, J.R.; Hansen, S.H.; Lesser, C.F.; Wu, H.; et al. INAVA-ARNO complexes bridge mucosal barrier function with inflammatory signaling. eLife 2018, 7, e38539. [Google Scholar] [CrossRef]
- Ghezelbash, B.; Rostami, M.; Heidarvand, M.; Mafi, A.; Chegni, H.; Eskandari, N. Correlation of Expression of MMP-2, ACE2, and TMPRSS2 Genes with Lymphopenia for Mild and Severity of COVID-19. Iran. J. Allergy Asthma Immunol. 2023, 22, 91–98. [Google Scholar] [CrossRef]
- Xiao, K.; Zhao, F.; Xie, W.; Ding, J.; Gong, X.; OuYang, C.; Le, A.P. Mechanism of TLR4 mediated immune effect in transfusion-induced acute lung injury based on Slit2/Robo4 signaling pathway. Transfus. Apher. Sci. 2023, 62, 103500. [Google Scholar] [CrossRef]
- Ye, B.Q.; Geng, Z.H.; Ma, L.; Geng, J.G. Slit2 regulates attractive eosinophil and repulsive neutrophil chemotaxis through differential srGAP1 expression during lung inflammation. J. Immunol. 2010, 185, 6294–6305. [Google Scholar] [CrossRef]
- Kim, H.T.; Yin, W.; Jin, Y.J.; Panza, P.; Gunawan, F.; Grohmann, B.; Buettner, C.; Sokol, A.M.; Preussner, J.; Guenther, S.; et al. Myh10 deficiency leads to defective extracellular matrix remodeling and pulmonary disease. Nat. Commun. 2018, 9, 4600. [Google Scholar] [CrossRef]
- Zheng, L.; Pan, C.; Tian, W.; Liang, C.; Feng, Y.; He, W.; Yang, Z.; Wang, B.; Qiu, Q.; Li, N.; et al. Atp8a1 deletion increases the proliferative activity of hematopoietic stem cells by impairing PTEN function. Cell. Oncol. 2023, 46, 1069–1083. [Google Scholar] [CrossRef]
- Lao, N.; Barron, N. Enhancing recombinant protein and viral vector production in mammalian cells by targeting the YTHDF readers of N(6)-methyladenosine in mRNA. Biotechnol. J. 2023, 18, e2200451. [Google Scholar] [CrossRef]
- Kook, S.; Wang, P.; Meng, S.; Jetter, C.S.; Sucre, J.M.S.; Benjamin, J.T.; Gokey, J.J.; Hanby, H.A.; Jaume, A.; Goetzl, L.; et al. AP-3-dependent targeting of flippase ATP8A1 to lamellar bodies suppresses activation of YAP in alveolar epithelial type 2 cells. Proc. Natl. Acad. Sci. USA 2021, 118, e2025208118. [Google Scholar] [CrossRef]
- Kato, U.; Inadome, H.; Yamamoto, M.; Emoto, K.; Kobayashi, T.; Umeda, M. Role for phospholipid flippase complex of ATP8A1 and CDC50A proteins in cell migration. J. Biol. Chem. 2013, 288, 4922–4934. [Google Scholar] [CrossRef]
- Francis, M.E.; Goncin, U.; Kroeker, A.; Swan, C.; Ralph, R.; Lu, Y.; Etzioni, A.L.; Falzarano, D.; Gerdts, V.; Machtaler, S.; et al. SARS-CoV-2 infection in the Syrian hamster model causes inflammation as well as type I interferon dysregulation in both respiratory and non-respiratory tissues including the heart and kidney. PLoS Pathog. 2021, 17, e1009705. [Google Scholar] [CrossRef]
- Nguyen, H.T.; Zhang, S.; Wang, Q.; Anang, S.; Wang, J.; Ding, H.; Kappes, J.C.; Sodroski, J. Spike glycoprotein and host cell determinants of SARS-CoV-2 entry and cytopathic effects. J. Virol. 2021, 95, 10–1128. [Google Scholar] [CrossRef]
- Lavie, M.; Dubuisson, J.; Belouzard, S. SARS-CoV-2 Spike Furin Cleavage Site and S2’ Basic Residues Modulate the Entry Process in a Host Cell-Dependent Manner. J. Virol. 2022, 96, e0047422. [Google Scholar] [CrossRef]
- Cao, Y.; Yang, R.; Wang, W.; Jiang, S.; Yang, C.; Liu, N.; Dai, H.; Lee, I.; Meng, X.; Yuan, Z. Probing the formation, structure and free energy relationships of M protein dimers of SARS-CoV-2. Comput. Struct. Biotechnol. J. 2022, 20, 573–582. [Google Scholar] [CrossRef]
- Dolan, K.A.; Dutta, M.; Kern, D.M.; Kotecha, A.; Voth, G.A.; Brohawn, S.G. Structure of SARS-CoV-2 M protein in lipid nanodiscs. eLife 2022, 11, e81702. [Google Scholar] [CrossRef]
- Zhang, L.; Hom, N.; Ojha, A.; Lovendahl, K.N.; Mou, H.; Lee, K.K.; Choe, H. Cytoplasmic Tail Truncation Stabilizes S1-S2 Association and Enhances S Protein Incorporation into SARS-CoV-2 Pseudovirions. J. Virol. 2023, 97, e0165022. [Google Scholar] [CrossRef]
- Pawlowski, P.H. Charged amino acids may promote coronavirus SARS-CoV-2 fusion with the host cell. AIMS Biophys. 2021, 8, 111–120. [Google Scholar] [CrossRef]
- Yao, Z.; Geng, B.; Marcon, E.; Pu, S.; Tang, H.; Merluza, J.; Bello, A.; Snider, J.; Lu, P.; Wood, H.; et al. Omicron Spike Protein is Vulnerable to Reduction. J. Mol. Biol. 2023, 435, 168128. [Google Scholar] [CrossRef]
- McDonald, J.T.; Enguita, F.J.; Taylor, D.; Griffin, R.J.; Priebe, W.; Emmett, M.R.; Sajadi, M.M.; Harris, A.D.; Clement, J.; Dybas, J.M.; et al. Role of miR-2392 in driving SARS-CoV-2 infection. Cell Rep. 2021, 37, 109839. [Google Scholar] [CrossRef]
- Ahirwar, D.K.; Charan, M.; Mishra, S.; Verma, A.K.; Shilo, K.; Ramaswamy, B.; Ganju, R.K. Slit2 Inhibits Breast Cancer Metastasis by Activating M1-Like Phagocytic and Antifibrotic Macrophages. Cancer Res. 2021, 81, 5255–5267. [Google Scholar] [CrossRef]
- Uskokovic, V. Lessons from the history of inorganic nanoparticles for inhalable diagnostics and therapeutics. Adv. Colloid Interface Sci. 2023, 315, 102903. [Google Scholar] [CrossRef]
- Jonigk, D.; Werlein, C.; Acker, T.; Aepfelbacher, M.; Amann, K.U.; Baretton, G.; Barth, P.; Bohle, R.M.; Buttner, A.; Buttner, R.; et al. Organ manifestations of COVID-19: What have we learned so far (not only) from autopsies? Virchows Arch. 2022, 481, 139–159. [Google Scholar] [CrossRef]
- Albanese, A.; Tang, P.S.; Chan, W.C. The effect of nanoparticle size, shape, and surface chemistry on biological systems. Annu. Rev. Biomed. Eng. 2012, 14, 1–16. [Google Scholar] [CrossRef]
- Wieler, L.; Vittos, O.; Mukherjee, N.; Sarkar, S. Reduction in the COVID-19 pneumonia case fatality rate by silver nanoparticles: A randomized case study. Heliyon 2023, 9, e14419. [Google Scholar] [CrossRef]
- Almanza-Reyes, H.; Moreno, S.; Plascencia-Lopez, I.; Alvarado-Vera, M.; Patron-Romero, L.; Borrego, B.; Reyes-Escamilla, A.; Valencia-Manzo, D.; Brun, A.; Pestryakov, A.; et al. Evaluation of silver nanoparticles for the prevention of SARS-CoV-2 infection in health workers: In vitro and in vivo. PLoS ONE 2021, 16, e0256401. [Google Scholar] [CrossRef]
- Yoosefian, M.; Sabaghian, H. Silver nanoparticle-based drug delivery systems in the fight against COVID-19: Enhancing efficacy, reducing toxicity and improving drug bioavailability. J. Drug Target. 2024, 24, 1–13. [Google Scholar] [CrossRef]
- Ayipo, Y.O.; Badeggi, U.M.; Jimoh, A.A.; Mordi, M.N. Chapter 14—Silver nanoparticles for treatment of COVID-19 and other viral diseases. In Silver Nanoparticles for Drug Delivery; Academic Press: Cambridge, MA, USA, 2024; pp. 313–340. [Google Scholar] [CrossRef]
- Zhang, G.; Wang, X.; Wang, G.; Suo, X.; Qiu, Y.; Luo, R.H.; Liu, Y.; Li, Q.; Luo, W.; Shi, Z.; et al. Nanoparticles insert a three dimensional cavity structure of proteins for function inhibition: The Case of CeO2 and SARS-CoV-2. Nano Today 2024, 55, 102183. [Google Scholar] [CrossRef]
- Shigi, N.; Otani, K.; Komiyama, M. Gene manipulation of adenovirus vector by artificial restriction DNA cutter. In Nucleic Acids Symposium Series; Oxford University Press: Oxford, UK, 2007; Volume 51, pp. 197–198. [Google Scholar] [CrossRef]
- Shcherbakov, A.B. CeO2 nanoparticles and cerium species as antiviral agents: Critical review. Eur. J. Med. Chem. Rep. 2024, 10, 100141. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bauer, A.N.; Williams, J.F.; Pokhrel, L.R.; Garcia, S.; Majumdar, N.; Eells, J.B.; Cook, P.P.; Akula, S.M. Evaluating Molecular Mechanism of Viral Inhibition of Aerosolized Smart Nano-Enabled Antiviral Therapeutic (SNAT) on SARS-CoV-2-Infected Hamsters. Toxics 2024, 12, 495. https://doi.org/10.3390/toxics12070495
Bauer AN, Williams JF, Pokhrel LR, Garcia S, Majumdar N, Eells JB, Cook PP, Akula SM. Evaluating Molecular Mechanism of Viral Inhibition of Aerosolized Smart Nano-Enabled Antiviral Therapeutic (SNAT) on SARS-CoV-2-Infected Hamsters. Toxics. 2024; 12(7):495. https://doi.org/10.3390/toxics12070495
Chicago/Turabian StyleBauer, Anais N., John F. Williams, Lok R. Pokhrel, Selena Garcia, Niska Majumdar, Jeffrey B. Eells, Paul P. Cook, and Shaw M. Akula. 2024. "Evaluating Molecular Mechanism of Viral Inhibition of Aerosolized Smart Nano-Enabled Antiviral Therapeutic (SNAT) on SARS-CoV-2-Infected Hamsters" Toxics 12, no. 7: 495. https://doi.org/10.3390/toxics12070495






