Evaluation of Load on Cervical Disc Prosthesis by Imposing Complex Motion: Multiplanar Motion and Combined Rotational–Translational Motion
Abstract
1. Introduction
- (1)
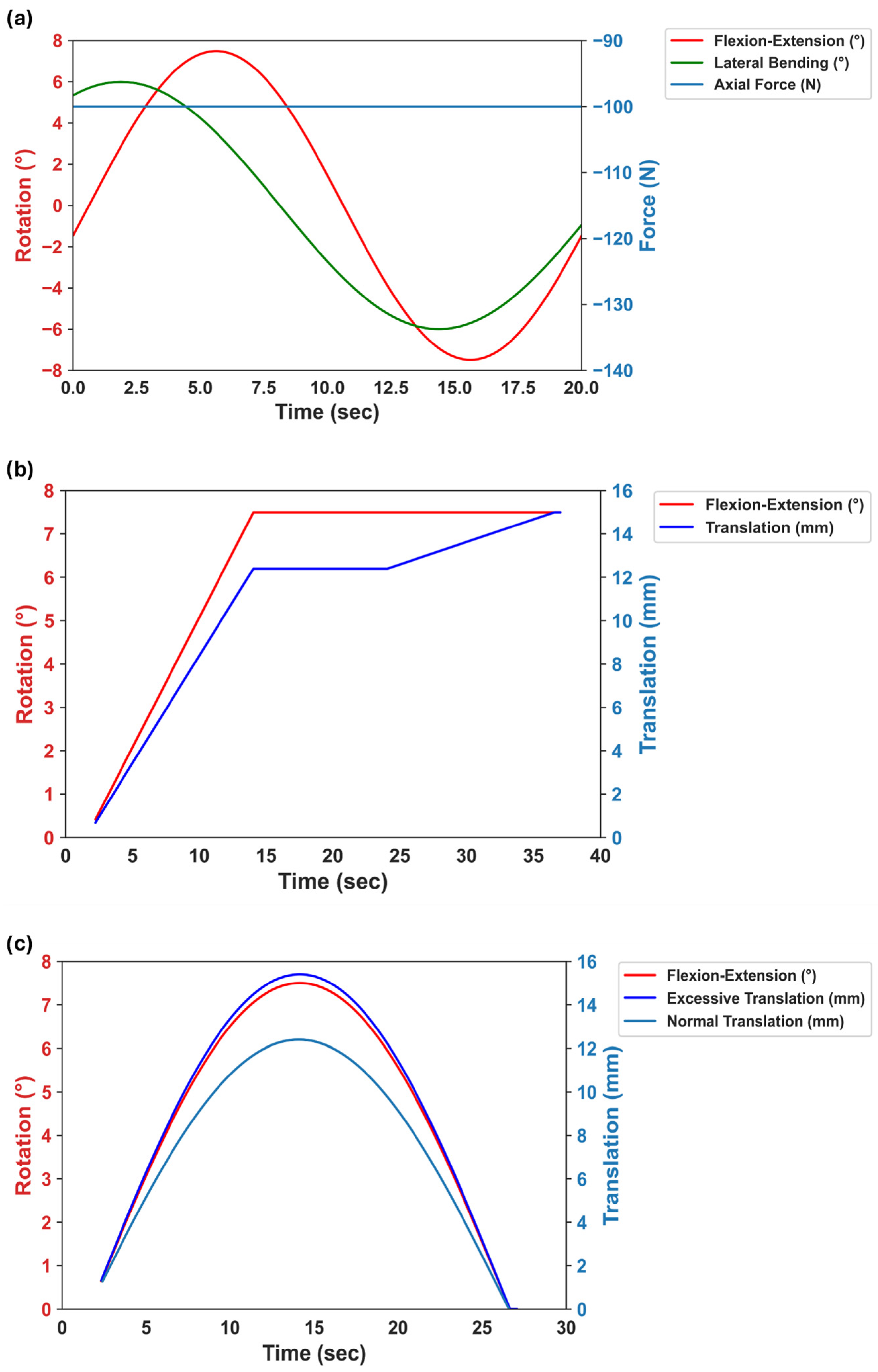
- Quantifying the forces and moments generated during the multiplanar motion (combined FE-LB). In this case, three component forces (i.e., Fx, Fy, and Fz) and three component moments (i.e., Tx, Ty, and Tz) were calculated, and the resultant values for forces and moments were then compared between the unidirectional motion test and the multiplanar motion test.
- (2)
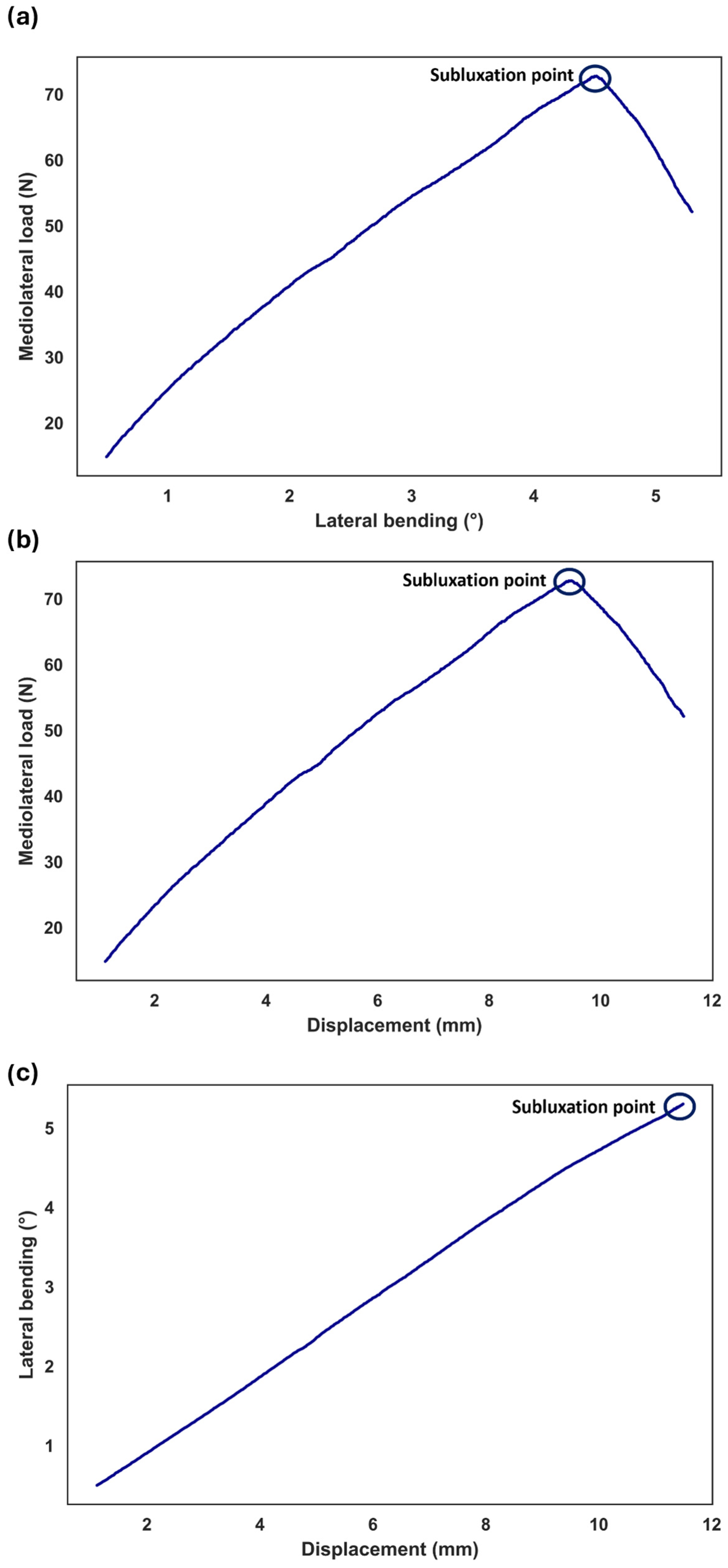
- Determining the conditions under which subluxation or dislocation occurs during combined rotational–translational movements. In this case, the lateral force, the degree of the rotation, and the translation were measured until the samples reached the subluxation point.
2. Materials and Methods
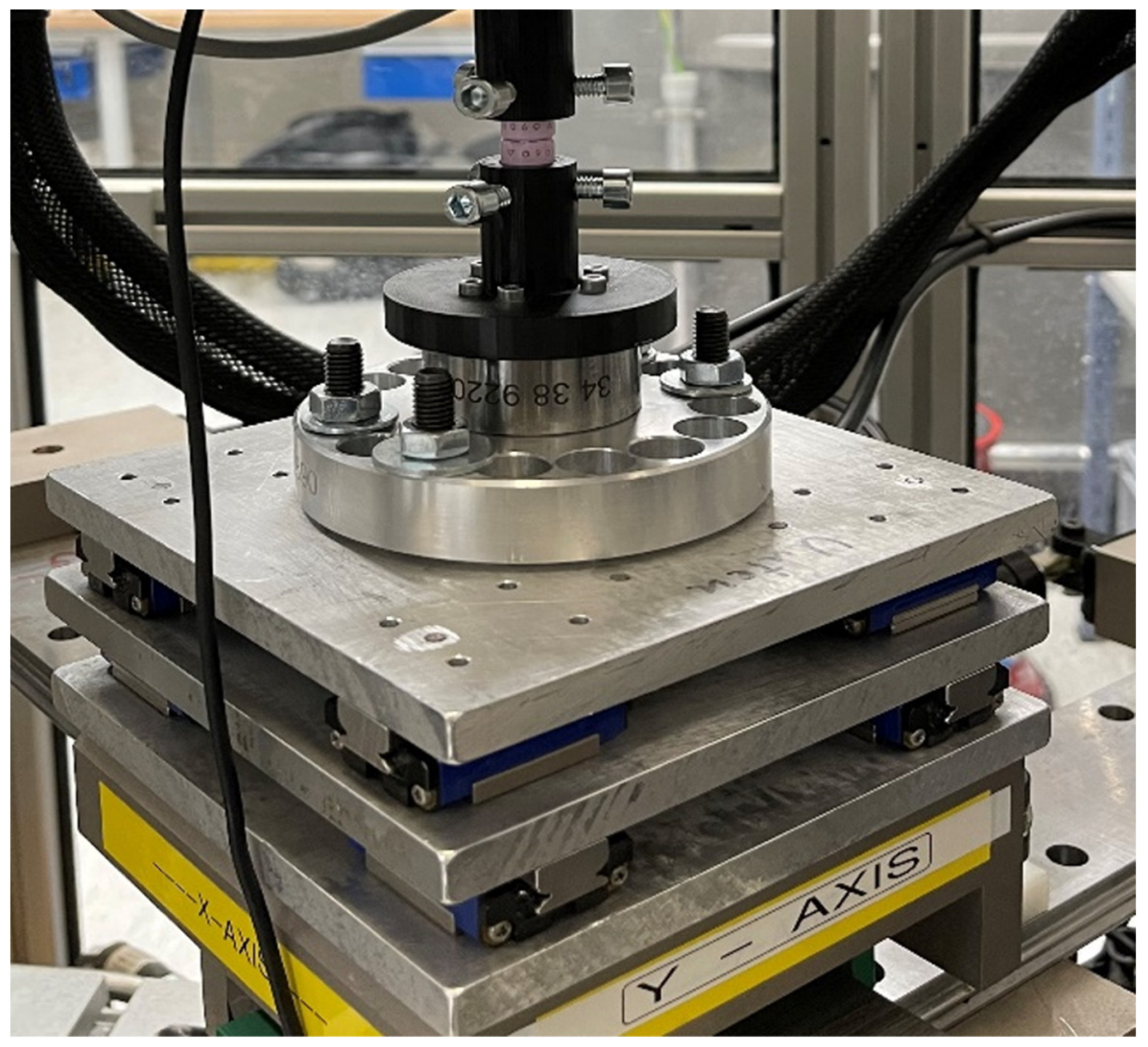
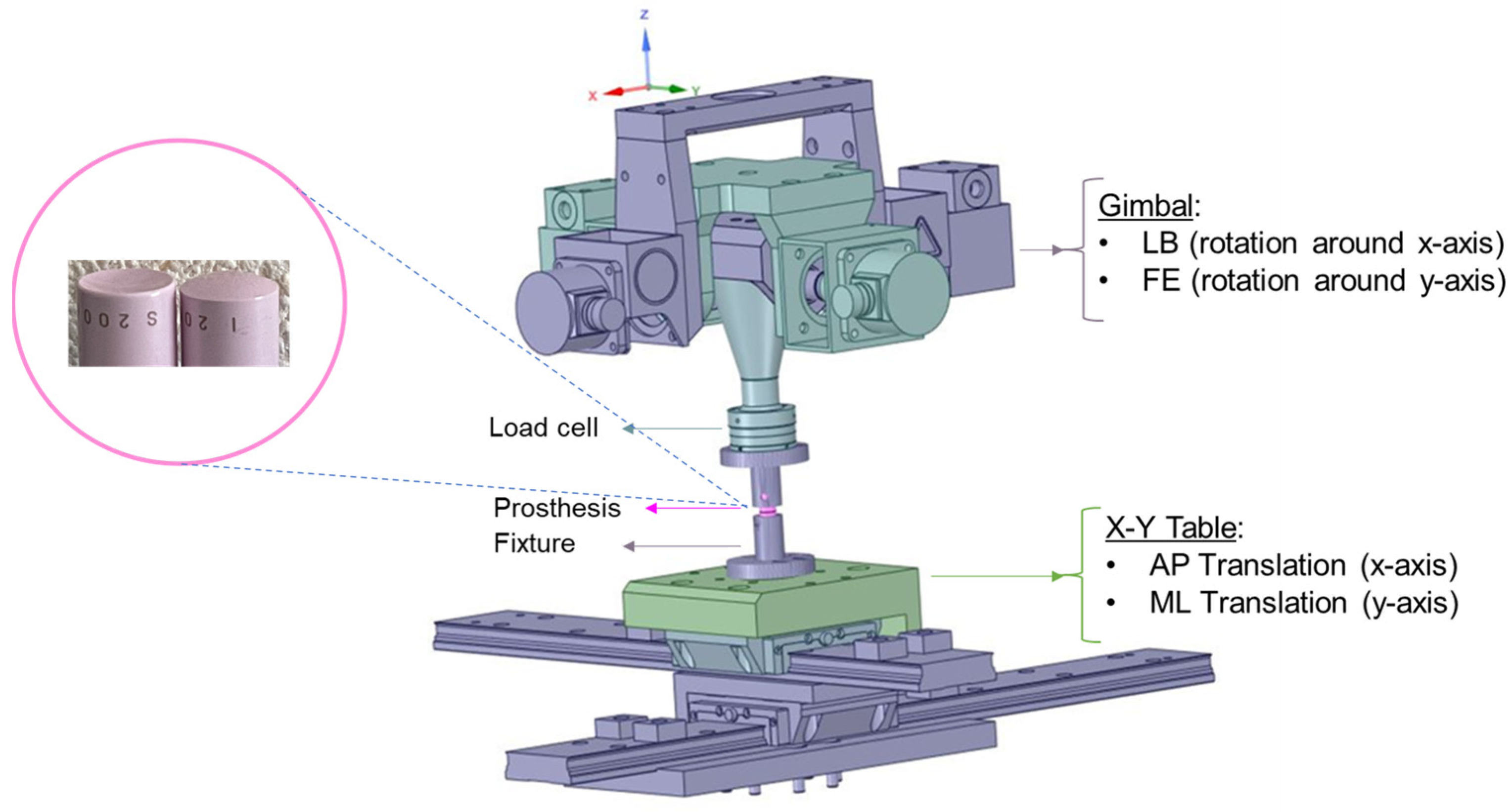
2.1. Experimental Components
2.2. Study Design
- Scenario 1: The application of an excessive translational movement (3 mm) subsequent to the complete rotation of the sample (Figure 2b). Before applying the excessive translation, the samples remained in a fully flexed condition for 10 seconds to reach the required values for rotation and axial force (i.e., the dwelling phase). During the rotation step, the applied translation was due to the offset between the testing machine’s COR and the sample’s COR (12.40 mm for FE and 9.93 mm for LB) in order to adjust the alignment.
- Scenario 2: The concurrent application of excessive translational motion (3 mm) and rotation (Figure 2c). A translational adjustment (command normal translation in Figure 2c) was made during the rotation to prevent excessive forces and moments due to the offset between the sample’s COR and the testing machine’s COR. The 3 mm of extra translation was then superimposed on the translational adjustment.

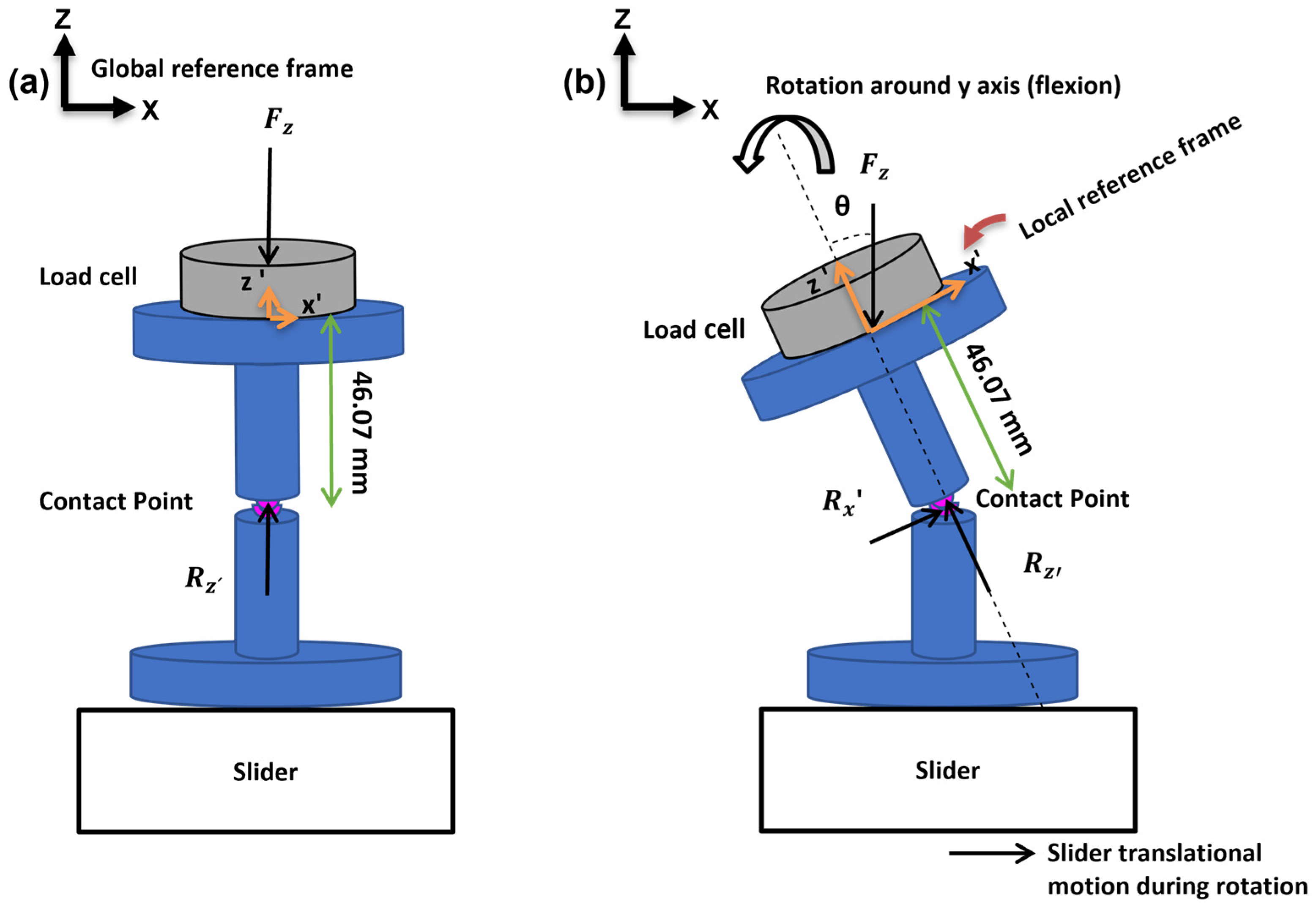
2.3. Postprocessing
2.3.1. Unidirectional and Multiplanar Motion
2.3.2. Rotational–Translational Motion
3. Results
3.1. Reaction Moments and Forces for Combined and Unidirectional Motion Tests
3.2. Shear Forces, Translations, and Degree of Rotations for Rotational–Translational Motion Tests
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Patel, V.V.; Wuthrich, Z.R.; McGilvray, K.C.; Lafleur, M.C.; Lindley, E.M.; Sun, D.; Puttlitz, C.M. Cervical facet force analysis after disc replacement versus fusion. Clin. Biomech. 2017, 44, 52–58. [Google Scholar] [CrossRef]
- Gore, D.R.; Sepic, S.B. Anterior discectomy and fusion for painful cervical disc disease. A report of 50 patients with an average follow-up of 21 years. Spine 1998, 23, 2047–2051. [Google Scholar] [CrossRef]
- Matsumoto, M.; Okada, E.; Ichihara, D.; Watanabe, K.; Chiba, K.; Toyama, Y.; Fujiwara, H.; Momoshima, S.; Nishiwaki, Y.; Iwanami, A.; et al. Anterior cervical decompression and fusion accelerates adjacent segment degeneration: Comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine 2010, 35, 36–43. [Google Scholar] [CrossRef]
- Nabhan, A.; Ahlhelm, F.; Pitzen, T.; Steudel, W.I.; Jung, J.; Shariat, K.; Steimer, O.; Bachelier, F.; Pape, D. Disc replacement using Pro-Disc C versus fusion: A prospective randomised and controlled radiographic and clinical study. Eur. Spine J. 2007, 16, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Grob, D.; Porchet, F.; Kleinstück, F.S.; Lattig, F.; Jeszenszky, D.; Luca, A.; Mutter, U.; Mannion, A.F. A comparison of outcomes of cervical disc arthroplasty and fusion in everyday clinical practice: Surgical and methodological aspects. Eur. Spine J. 2010, 19, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Baba, H.; Furusawa, N.; Imura, S.; Kawahara, N.; Tsuchiya, H.; Tomita, K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine 1993, 18, 2167–2173. [Google Scholar] [CrossRef] [PubMed]
- Hilibrand, A.S.; Carlson, G.D.; Palumbo, M.A.; Jones, P.K.; Bohlman, H.H. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J. Bone Jt. Surg. Am. 1999, 81, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Ansaripour, H.; Ferguson, S.; Flohr, M. In-vitro Biomechanics of the Cervical Spine: A Systematic Review. J. Biomech. Eng. 2022, 144, 100801. [Google Scholar] [CrossRef] [PubMed]
- Formica, M.; Divano, S.; Cavagnaro, L.; Basso, M.; Zanirato, A.; Formica, C.; Felli, L. Lumbar total disc arthroplasty: Outdated surgery or here to stay procedure? A systematic review of current literature. J. Orthop. Traumatol. 2017, 18, 197–215. [Google Scholar] [CrossRef]
- Tu, T.-H.; Wu, J.-C.; Huang, W.-C.; Guo, W.-Y.; Wu, C.-L.; Shih, Y.-H.; Cheng, H. Heterotopic ossification after cervical total disc replacement: Determination by CT and effects on clinical outcomes. J. Neurosurg. Spine 2011, 14, 457–465. [Google Scholar] [CrossRef]
- Cavanaugh, D.A.; Nunley, P.D.; Kerr, E.J., 3rd; Werner, D.J.; Jawahar, A. Delayed hyper-reactivity to metal ions after cervical disc arthroplasty: A case report and literature review. Spine 2009, 34, E262–E265. [Google Scholar] [CrossRef] [PubMed]
- Guyer, R.D.; Shellock, J.; MacLennan, B.; Hanscom, D.; Knight, R.Q.; McCombe, P.; Jacobs, J.J.; Urban, R.M.; Bradford, D.; Ohnmeiss, D.D. Early failure of metal-on-metal artificial disc prostheses associated with lymphocytic reaction: Diagnosis and treatment experience in four cases. Spine 2011, 36, E492–E497. [Google Scholar] [CrossRef]
- Amoretti, N.; Iannessi, A.; Lesbats, V.; Marcy, P.Y.; Hovorka, E.; Bronsard, N.; Fonquerne, M.E.; Hauger, O. Imaging of intervertebral disc prostheses. Diagn. Interv. Imaging 2012, 93, 10–21. [Google Scholar] [CrossRef]
- Virk, S.; Phillips, F.; Khan, S.; Qureshi, S. A cross-sectional analysis of 1347 complications for cervical disc replacements from medical device reports maintained by the United States Food and Drug Administration. Spine J. 2020, 21, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Ansaripour, H.; Haeussler, K.L.; Ferguson, S.J.; Flohr, M. Prioritizing biomaterials for spinal disc implants by a fuzzy AHP and TOPSIS decision making method. Sci. Rep. 2023, 13, 21531. [Google Scholar] [CrossRef]
- Daniels, A.H.; Paller, D.J.; Feller, R.J.; Thakur, N.A.; Biercevicz, A.M.; Palumbo, M.A.; Crisco, J.J.; Madom, I.A. Examination of cervical spine kinematics in complex, multiplanar motions after anterior cervical discectomy and fusion and total disc replacement. Int. J. Spine Surg. 2012, 6, 190–194. [Google Scholar] [CrossRef]
- Penning, L. Normal movements of the cervical spine. AJR Am. J. Roentgenol. 1978, 130, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Wilke, H.J.; Wenger, K.; Claes, L. Testing criteria for spinal implants: Recommendations for the standardization of in vitro stability testing of spinal implants. Eur. Spine J. 1998, 7, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Sherrill, J.T.; Siddicky, S.F.; Davis, W.D.; Chen, C.; Bumpass, D.B.; Mannen, E.M. Validation of a custom spine biomechanics simulator: A case for standardization. J. Biomech. 2020, 98, 109470. [Google Scholar] [CrossRef]
- Wang, T.; Ball, J.R.; Pelletier, M.H.; Walsh, W.R. Biomechanical evaluation of a biomimetic spinal construct. J. Exp. Orthop. 2014, 1, 3. [Google Scholar] [CrossRef]
- Aunoble, S.; Donkersloot, P.; le Huec, J.C. Dislocations with intervertebral disc prosthesis: Two case reports. Eur. Spine J. 2004, 13, 464–467. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-H.; Im, Y.-J.; Kim, K.-T.; Kim, Y.-H.; Park, W.-M.; Kim, K. Comparison of Cervical Spine Biomechanics after Fixed- and Mobile-Core Artificial Disc Replacement: A Finite Element Analysis. Spine 2011, 36, 700–708. Available online: https://journals.lww.com/spinejournal/Fulltext/2011/04200/Comparison_of_Cervical_Spine_Biomechanics_After.4.aspx (accessed on 20 April 2011). [CrossRef] [PubMed]
- Rousseau, M.A.; Bradford, D.S.; Bertagnoli, R.; Hu, S.S.; Lotz, J.C. Disc arthroplasty design influences intervertebral kinematics and facet forces. Spine J. 2006, 6, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Hussain, A.; Counsell, L.; Kamali, A. Clinical effects of edge loading on metal-on-metal hip resurfacings. Orthop. Proc. 2010, 92-B, 399. [Google Scholar]
- Langton, D.J.; Joyce, T.J.; Jameson, S.S.; Lord, J.; Van Orsouw, M.; Holland, J.P.; Nargol, A.V.F.; De Smet, K.A. Adverse reaction to metal debris following hip resurfacing. J. Bone Jt. Surg. Br. 2011, 93-B, 164–171. [Google Scholar] [CrossRef]
- Willert, H.-G.; Buchhorn, G.H.; Fayyazi, A.; Flury, R.; Windler, M.; Köster, G.; Lohmann, C.H. Metal-on-Metal Bearings and Hypersensitivity in Patients with Artificial Hip Joints: A Clinical and Histomorphological Study. JBJS 2005, 87, 28–36. Available online: https://journals.lww.com/jbjsjournal/fulltext/2005/01000/metal_on_metal_bearings_and_hypersensitivity_in.6.aspx (accessed on 2 January 2005). [CrossRef]
- Langton, D.J.; Jameson, S.S.; Joyce, T.J.; Hallab, N.J.; Natu, S.; Nargol, A.V.F. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement. J. Bone Jt. Surg. Br. 2010, 92-B, 38–46. [Google Scholar] [CrossRef]
- Harris, W.H. Edge Loading Has a Paradoxical Effect on Wear in Metal-on-Polyethylene Total Hip Arthroplasties. Clin. Orthop. Relat. Res. 2012, 470, 3077–3082. Available online: https://journals.lww.com/clinorthop/fulltext/2012/11000/edge_loading_has_a_paradoxical_effect_on_wear_in.17.aspx (accessed on 30 November 2012). [CrossRef]
- Jarrett, C.A.; Ranawat, A.S.; Bruzzone, M.; Blum, Y.C.; Rodriguez, J.A.; Ranawat, C.S. The Squeaking Hip: A Phenomenon of Ceramic-on-Ceramic Total Hip Arthroplasty. JBJS 2009, 91, 1344–1349. Available online: https://journals.lww.com/jbjsjournal/fulltext/2009/06000/the_squeaking_hip__a_phenomenon_of.7.aspx (accessed on 1 June 2009). [CrossRef]
- Keurentjes, J.C.; Kuipers, R.M.; Wever, D.J.; Schreurs, B.W. High Incidence of Squeaking in THAs with Alumina Ceramic-on-ceramic Bearings. Clin. Orthop. Relat. Res. 2008, 466, 1438–1443. Available online: https://journals.lww.com/clinorthop/fulltext/2008/06000/high_incidence_of_squeaking_in_thas_with_alumina.28.aspx (accessed on 26 February 2008). [CrossRef]
- Stewart, T.; Tipper, J.; Streicher, R.; Ingham, E.; Fisher, J. Long-term wear of HIPed alumina on alumina bearings for THR under microseparation conditions. J. Mater. Sci. Mater. Med. 2001, 12, 1053–1056. [Google Scholar] [CrossRef] [PubMed]
- Lusty, P.J.; Watson, A.; Tuke, M.A.; Walter, W.L.; Walter, W.K.; Zicat, B. Orientation and wear of the acetabular component in third generation alumina-on-alumina ceramic bearings. J. Bone Jt. Surg. Br. 2007, 89-B, 1158–1164. [Google Scholar] [CrossRef] [PubMed]
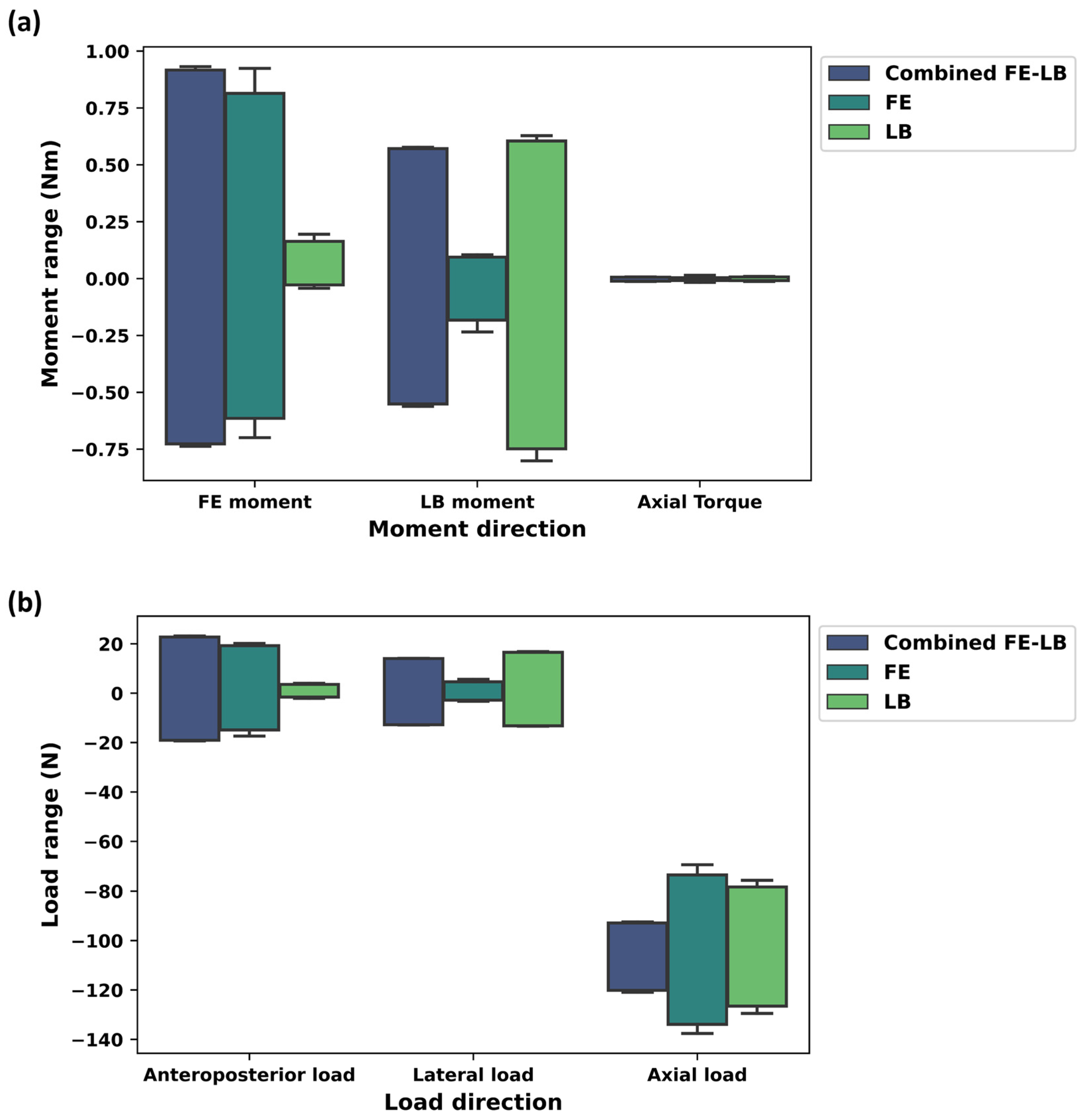


| Motion Type | Tx (Std) Nm | Ty (Std) Nm | Tz (Std) Nm | Fx (Std) N | Fy (Std) N | Fz (Std) N |
|---|---|---|---|---|---|---|
| Combined FE-LB | 0.56 (0.01) | 0.82 (0.1) | 0.01 (0.003) | 20.92 (1.84) | 13.40 (0.60) | 106.61 (13.61) |
| FE | 0.15 (0.06) | 0.74 (0.12) | 0.01 (0.01) | 17.15 (2.14) | 3.86 (1.09) | 103.38 (29.94) |
| LB | 0.67 (0.08) | 0.1 (0.07) | 0.01 (0.003) | 2.57 (1.004) | 14.87 (1.65) | 102.46 (24.33) |
| Measurement Type | Combined FE-LB (Std) | FE (Std) | LB (Std) |
|---|---|---|---|
| Resultant moment (Nm) | 1.0 (0.08) | 0.75 (0.2) | 0.68 (0.08) |
| Resultant force (N) | 109.46 (13.26) | 104.86 (29.51) | 103.57 (24.07) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ansaripour, H.; Ferguson, S.J.; Flohr, M. Evaluation of Load on Cervical Disc Prosthesis by Imposing Complex Motion: Multiplanar Motion and Combined Rotational–Translational Motion. Bioengineering 2024, 11, 857. https://doi.org/10.3390/bioengineering11080857
Ansaripour H, Ferguson SJ, Flohr M. Evaluation of Load on Cervical Disc Prosthesis by Imposing Complex Motion: Multiplanar Motion and Combined Rotational–Translational Motion. Bioengineering. 2024; 11(8):857. https://doi.org/10.3390/bioengineering11080857
Chicago/Turabian StyleAnsaripour, Hossein, Stephen J. Ferguson, and Markus Flohr. 2024. "Evaluation of Load on Cervical Disc Prosthesis by Imposing Complex Motion: Multiplanar Motion and Combined Rotational–Translational Motion" Bioengineering 11, no. 8: 857. https://doi.org/10.3390/bioengineering11080857
APA StyleAnsaripour, H., Ferguson, S. J., & Flohr, M. (2024). Evaluation of Load on Cervical Disc Prosthesis by Imposing Complex Motion: Multiplanar Motion and Combined Rotational–Translational Motion. Bioengineering, 11(8), 857. https://doi.org/10.3390/bioengineering11080857





