Bilateral Iliosacral and Transsacral Screws Are Biomechanically Favorable and Reduce the Risk for Fracture Progression in Fragility Fractures of the Pelvis—A Finite Element Analysis
Abstract
1. Introduction
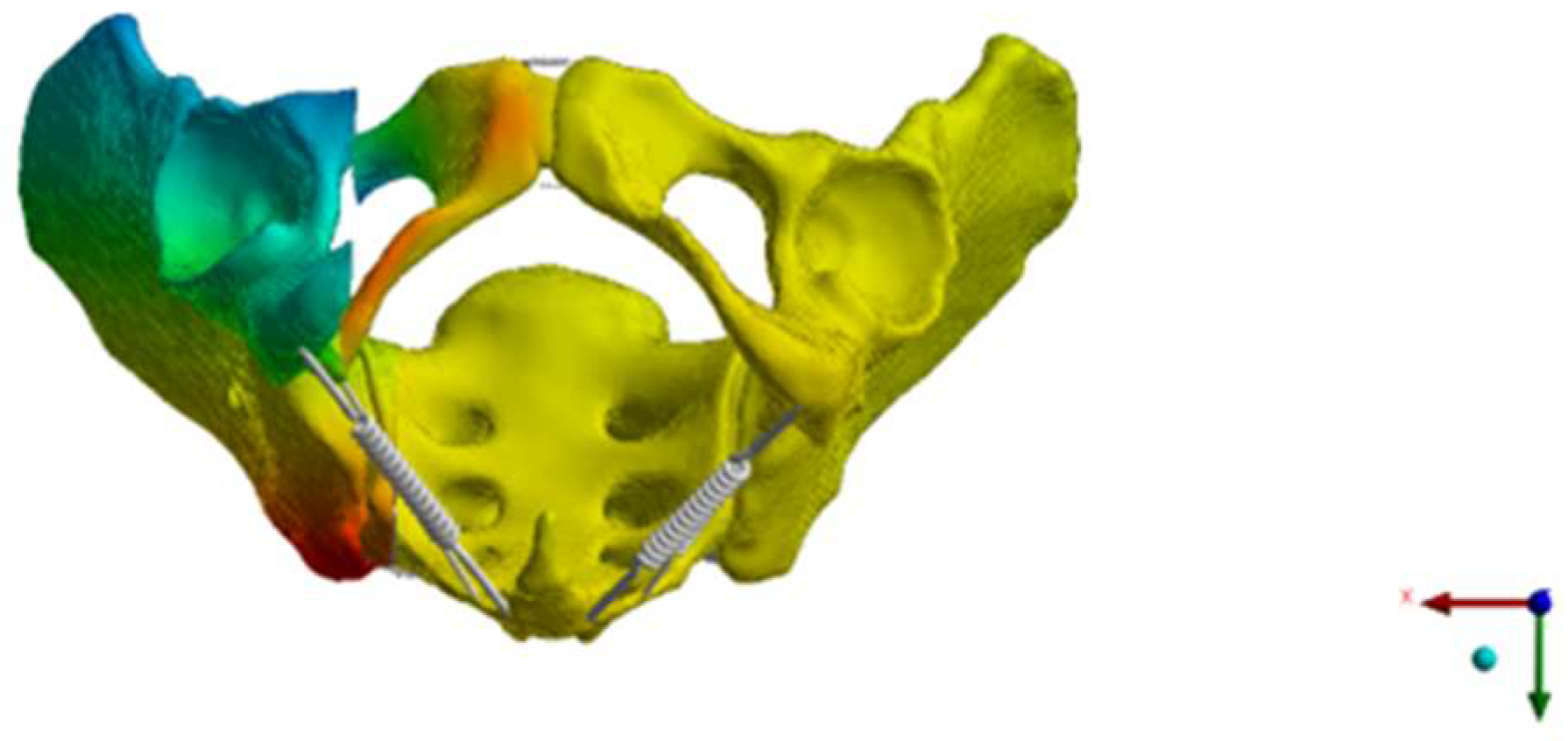
2. Materials and Methods
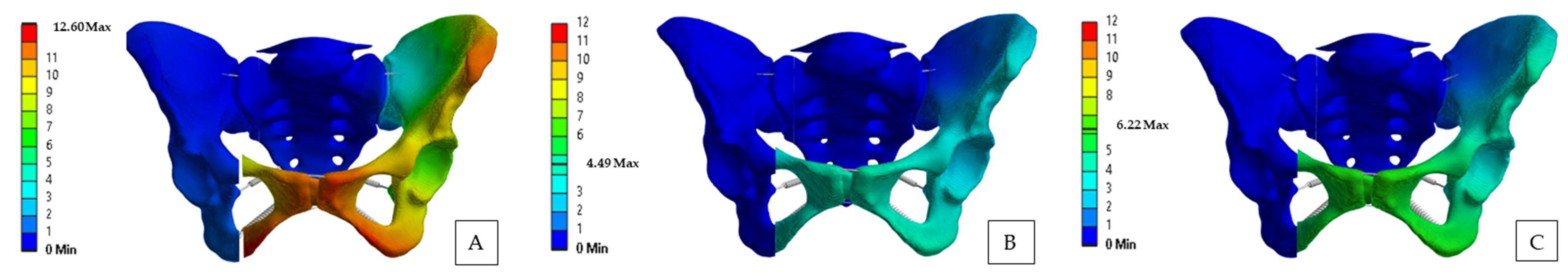
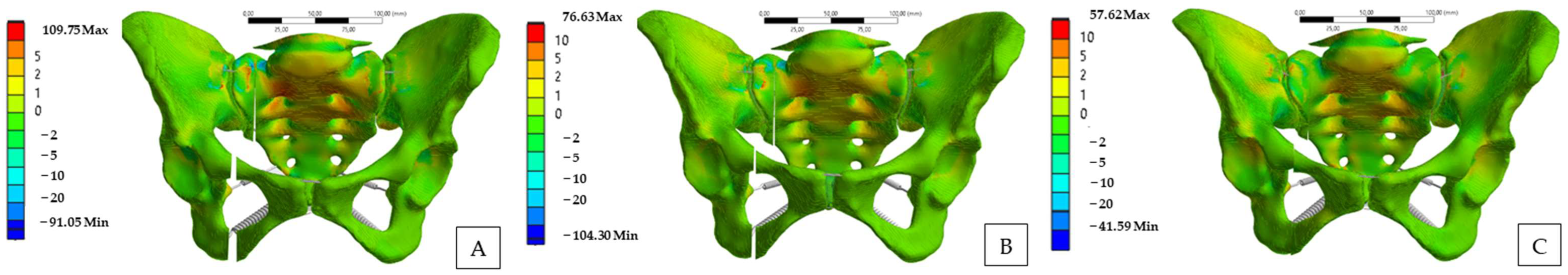
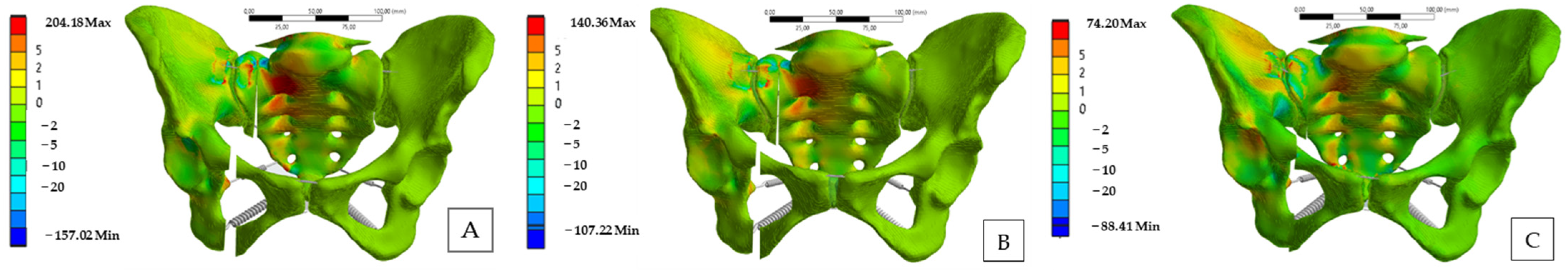
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andrich, S.; Haastert, B.; Neuhaus, E.; Neidert, K.; Arend, W.; Ohmann, C.; Grebe, J.; Vogt, A.; Jungbluth, P.; Thelen, S.; et al. Excess Mortality After Pelvic Fractures Among Older People. J. Bone Miner. Res. 2017, 32, 1789–1801. [Google Scholar] [CrossRef] [PubMed]
- Benzinger, P.; Riem, S.; Bauer, J.; Jaensch, A.; Becker, C.; Büchele, G.; Rapp, K. Risk of institutionalization following fragility fractures in older people. Osteoporos. Int. 2019, 30, 1363–1370. [Google Scholar] [CrossRef] [PubMed]
- Krappinger, D.; Struve, P.; Schmid, R.; Kroesslhuber, J.; Blauth, M. Fractures of the pubic rami: A retrospective review of 534 cases. Arch. Orthop. Trauma Surg. 2009, 129, 1685–1690. [Google Scholar] [CrossRef] [PubMed]
- Marrinan, S.; Pearce, M.S.; Jiang, X.Y.; Waters, S.; Shanshal, Y. Admission for osteoporotic pelvic fractures and predictors of length of hospital stay, mortality and loss of independence. Age Ageing 2015, 44, 258–261. [Google Scholar] [CrossRef] [PubMed]
- Schönenberg, D.; Guggenberger, R.; Frey, D.; Pape, H.-C.; Simmen, H.-P.; Osterhoff, G. CT-based evaluation of volumetric bone density in fragility fractures of the pelvis—A matched case-control analysis. Osteoporos. Int. 2018, 29, 459–465. [Google Scholar] [CrossRef]
- Lodde, M.F.; Fischer, T.M.; Riesenbeck, O.; Roßlenbroich, S.; Katthagen, J.C.; Rometsch, D.; Günes, D.; Schneider, M.; Raschke, M.J.; Liljenqvist, U. Analysis of the Spinopelvic Parameters in Patients with Fragility Fractures of the Pelvis. J. Clin. Med. 2023, 12, 4445. [Google Scholar] [CrossRef]
- Morris, R.O.; Sonibare, A.; Green, D.J.; Masud, T. Closed pelvic fractures: Characteristics and outcomes in older patients admitted to medical and geriatric wards. Postgrad. Med. J. 2000, 76, 646–650. [Google Scholar] [CrossRef]
- Nuber, S.; Ritter, B.; Fenwick, A.; Förch, S.; Wanzl, M.; Nuber, M.; Mayr, E. Midterm follow-up of elderly patients with fragility fractures of the pelvis: A prospective cohort-study comparing operative and non-operative treatment according to a therapeutic algorithm. Injury 2022, 53, 496–505. [Google Scholar] [CrossRef]
- Rommens, P.M.; Arand, C.; Hofmann, A.; Wagner, D. When and How to Operate Fragility Fractures of the Pelvis? Indian J. Orthop. 2019, 53, 128–137. [Google Scholar] [CrossRef]
- Wilson, D.G.G.; Kelly, J.; Rickman, M. Operative management of fragility fractures of the pelvis—A systematic review. BMC Musculoskelet. Disord. 2021, 22, 717. [Google Scholar] [CrossRef]
- Schuetze, K.; Eickhoff, A.; Dehner, C.; Blidon, A.; Gebhard, F.; Richter, P.H. Short-term outcome of fragility fractures of the pelvis in the elderly treated with screw osteosynthesis and external fixator. Eur. J. Trauma Emerg. Surg. 2022, 48, 2413–2420. [Google Scholar] [CrossRef] [PubMed]
- Rommens, P.M.; Hofmann, A. Comprehensive classification of fragility fractures of the pelvic ring: Recommendations for surgical treatment. Injury 2013, 44, 1733–1744. [Google Scholar] [CrossRef] [PubMed]
- Matta, J.M.; Tornetta, P. Internal fixation of unstable pelvic ring injuries. Clin. Orthop. Relat. Res. 1996, 329, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Chip, M.L.C., Jr.; Simonian, P.T.; Agnew, S.G.; Mann, F.A. Radiographic Recognition of the Sacral Alar Slope for Optimal Placement of Iliosacral Screws: A Cadaveric and Clinical Study. J. Orthop. Trauma 1996, 10, 171. [Google Scholar] [CrossRef] [PubMed]
- Choy, W.-S.; Kim, K.J.; Lee, S.K.; Park, H.J. Anterior pelvic plating and sacroiliac joint fixation in unstable pelvic ring injuries. Yonsei Med. J. 2012, 53, 422–426. [Google Scholar] [CrossRef][Green Version]
- Hartensuer, R.; Lodde, M.F.; Keller, J.; Eveslage, M.; Stolberg-Stolberg, J.; Riesenbeck, O.; Raschke, M.J. Safety, Effect and Feasibility of Percutaneous SI-Screw with and without Augmentation—A 15-Year Retrospective Analysis on over 640 Screws. J. Clin. Med. 2020, 9, 2660. [Google Scholar] [CrossRef]
- Yamamoto, N.; Someko, H.; Tsuge, T.; Nakashima, Y.; Nakao, S. Prevalence of fracture progression in fragility fractures of the pelvis: Systematic review and meta-analysis. Injury 2024, 55, 111727. [Google Scholar] [CrossRef]
- Cintean, R.; Fritzsche, C.; Zderic, I.; Gueorguiev-Rüegg, B.; Gebhard, F.; Schütze, K. Sacroiliac versus transiliac–transsacral screw osteosynthesis in osteoporotic pelvic fractures: A biomechanical comparison. Eur. J. Trauma Emerg. Surg. 2023, 49, 2553–2560. [Google Scholar] [CrossRef]
- Zderic, I.; Wagner, D.; Schopper, C.; Lodde, M.; Richards, G.; Gueorguiev, B.; Rommens, P.; Acklin, Y.P. Screw-in-screw fixation of fragility sacrum fractures provides high stability without loosening-biomechanical evaluation of a new concept. J. Orthop. Res. 2021, 39, 761–770. [Google Scholar] [CrossRef]
- Lodde, M.F.; Katthagen, J.C.; Schopper, C.O.; Zderic, I.; Richards, R.G.; Gueorguiev, B.; Raschke, M.J.; Hartensuer, R. Does Cement Augmentation of the Sacroiliac Screw Lead to Superior Biomechanical Results for Fixation of the Posterior Pelvic Ring? A Biomechanical Study. Medicina 2021, 57, 1368. [Google Scholar] [CrossRef]
- Rommens, P.M.; Arand, C.; Hopf, J.C.; Mehling, I.; Dietz, S.O.; Wagner, D. Progress of instability in fragility fractures of the pelvis: An observational study. Injury 2019, 50, 1966–1973. [Google Scholar] [CrossRef] [PubMed]
- Fada, R.; Shahgholi, M.; Azimi, R.; Babadi, N.F. Estimation of Porosity Effect on Mechanical Properties in Calcium Phosphate Cement Reinforced by Strontium Nitrate Nanoparticles: Fabrication and FEM Analysis. Arab. J. Sci. Eng. 2024, 49, 1815–1825. [Google Scholar] [CrossRef]
- Yao, F.; He, Y.; Qian, H.; Zhou, D.; Li, Q. Comparison of Biomechanical Characteristics and Pelvic Ring Stability Using Different Fixation Methods to Treat Pubic Symphysis Diastasis: A Finite Element Study. Medicine 2015, 94, e2207. [Google Scholar] [CrossRef] [PubMed]
- Shi, D.; Wang, F.; Wang, D.; Li, X.; Wang, Q. 3-D finite element analysis of the influence of synovial condition in sacroiliac joint on the load transmission in human pelvic system. Med. Eng. Phys. 2014, 36, 745–753. [Google Scholar] [CrossRef]
- Bruna-Rosso, C.; Arnoux, P.-J.; Bianco, R.-J.; Godio-Raboutet, Y.; Fradet, L.; Aubin, C.-É. Finite Element Analysis of Sacroiliac Joint Fixation under Compression Loads. Int. J. Spine Surg. 2016, 10, 16. [Google Scholar] [CrossRef]
- Zhang, L.; Peng, Y.; Du, C.; Tang, P. Biomechanical study of four kinds of percutaneous screw fixation in two types of unilateral sacroiliac joint dislocation: A finite element analysis. Injury 2014, 45, 2055–2059. [Google Scholar] [CrossRef]
- Wu, C.; Zeng, B.; Deng, J.; Qin, B.; Shen, D.; Wang, X.; Hu, H.; Huang, L.; Liu, X.; Qiu, G. Finite Element Analysis and Transiliac-Transsacral Screw Fixation for Posterior Pelvic Ring with Sacrum Dysplasia. Orthop. Surg. 2023, 15, 337–346. [Google Scholar] [CrossRef]
- Fu, S.; Zhao, Y.; Lian, W.; Zou, D.; Sun, T.; Zhao, Y.; Tan, J.; Zhang, S.; Wang, D. Comparison of the risk of breakage of two kinds of sacroiliac screws in the treatment of bilateral sacral fractures. Eur. Spine J. 2014, 23, 1558–1567. [Google Scholar] [CrossRef]
- Hu, P.; Wu, T.; Wang, H.; Qi, X.; Yao, J.; Cheng, X.; Chen, W.; Zhang, Y. Biomechanical Comparison of Three Internal Fixation Techniques for Stabilizing Posterior Pelvic Ring Disruption: A 3D Finite Element Analysis. Orthop. Surg. 2019, 11, 195–203. [Google Scholar] [CrossRef]
- Ma, Y.; Zhao, Y.; Zou, D.; Dong, S.; Sun, X.; Cheng, G.; Lian, W.; Zhao, Y.; Sun, T.; Wang, D.; et al. Breakage risk of different sacroiliac screws in unilateral sacral fractures a finite element analysis. BMC Musculoskelet. Disord. 2022, 23, 953. [Google Scholar] [CrossRef]
- Eichenseer, P.H.; Sybert, D.R.; Cotton, J.R. A finite element analysis of sacroiliac joint ligaments in response to different loading conditions. Spine 2011, 36, E1446–E1452. [Google Scholar] [CrossRef] [PubMed]
- Lipphaus, A.; Klimek, M.; Witzel, U. Comparative Finite Element Analysis of Fixation Techniques for APC II Open-Book Injuries of the Pelvis. Biomechanics 2021, 1, 321–333. [Google Scholar] [CrossRef]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.-C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef] [PubMed]
- Rubio-Pérez, I.; Díaz Lantada, A. Surgical Planning of Sacral Nerve Stimulation Procedure in Presence of Sacral Anomalies by Using Personalized Polymeric Prototypes Obtained with Additive Manufacturing Techniques. Polymers 2020, 12, 581. [Google Scholar] [CrossRef]
- Taddei, F.; Schileo, E.; Helgason, B.; Cristofolini, L.; Viceconti, M. The material mapping strategy influences the accuracy of CT-based finite element models of bones: An evaluation against experimental measurements. Med. Eng. Phys. 2007, 29, 973–979. [Google Scholar] [CrossRef]
- Taddei, F.; Pancanti, A.; Viceconti, M. An improved method for the automatic mapping of computed tomography numbers onto finite element models. Med. Eng. Phys. 2004, 26, 61–69. [Google Scholar] [CrossRef]
- Dalstra, M.; Huiskes, R.; Odgaard, A.; van Erning, L. Mechanical and textural properties of pelvic trabecular bone. J. Biomech. 1993, 26, 523–535. [Google Scholar] [CrossRef]
- Miller, J.A.; Schultz, A.B.; Andersson, G.B. Load-displacement behavior of sacroiliac joints. J. Orthop. Res. 1987, 5, 92–101. [Google Scholar] [CrossRef]
- Bergmann, G.; Deuretzbacher, G.; Heller, M.; Graichen, F.; Rohlmann, A.; Strauss, J.; Duda, G.N. Hip contact forces and gait patterns from routine activities. J. Biomech. 2001, 34, 859–871. [Google Scholar] [CrossRef]
- Denis, F.; Davis, S.; Comfort, T. Sacral Fractures. Clin. Orthop. Relat. Res. 1988, 227, 67–81. [Google Scholar] [CrossRef]
- Deddens, J.A.; Petersen, M.R. Approaches for estimating prevalence ratios. Occup. Environ. Med. 2008, 65, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Wagner, D.; Kisilak, M.; Porcheron, G.; Krämer, S.; Mehling, I.; Hofmann, A.; Rommens, P.M. Trans-sacral bar osteosynthesis provides low mortality and high mobility in patients with fragility fractures of the pelvis. Sci. Rep. 2021, 11, 14201. [Google Scholar] [CrossRef] [PubMed]
- Regenbogen, S.; Barbari, J.E.; Vetter, S.Y.; Franke, J.; Grützner, P.A.; Swartman, B. Feasibility and Safety of 3D-Navigated Trans-Sacral Bar Osteosynthesis for Fragility Fractures of the Sacrum: FIRST Clinical Experiences. J. Clin. Med. 2024, 13, 5244. [Google Scholar] [CrossRef] [PubMed]
- Kammerlander, C.; Pfeufer, D.; Lisitano, L.A.; Mehaffey, S.; Böcker, W.; Neuerburg, C. Inability of Older Adult Patients with Hip Fracture to Maintain Postoperative Weight-Bearing Restrictions. J. Bone Joint Surg. Am. 2018, 100, 936–941. [Google Scholar] [CrossRef]
- Merkle, T.P.; Hofmann, N.; Knop, C.; Da Silva, T. Can elderly individuals perform partial weight bearing on their lower limbs? A prospective cohort study using ambulatory real-time biofeedback. J. Orthop. Surg. Res. 2023, 18, 324. [Google Scholar] [CrossRef]
- Heydemann, J.; Hartline, B.; Gibson, M.E.; Ambrose, C.G.; Munz, J.W.; Galpin, M.; Achor, T.S.; Gary, J.L. Do Transsacral-transiliac Screws Across Uninjured Sacroiliac Joints Affect Pain and Functional Outcomes in Trauma Patients? Clin. Orthop. Relat. Res. 2016, 474, 1417–1421. [Google Scholar] [CrossRef]




| Shi et al. [24] | Yao et al. [23] | Eichenseer et al. [31] | |
|---|---|---|---|
| N/mm | N/mm | N/mm Defined by the Percentage Elongation | |
| ASL | 700 | 18.9 | 39–103 |
| SPSL | 400 | 21.0 | 200–525 |
| LPSL | 1.000 | 21.0 | 29–75 |
| ISL | 2.800 | 22.4 | 13–34 |
| SS | 1.400 | 12.6 | 26–68 |
| ST | 1.500 | 22.5 | 17–45 |
| SP | 500 | 12.0 | / |
| IP | 500 | 12.0 | / |
| Load Application | USI | BSI | TSI |
|---|---|---|---|
| Bipedal stance | |||
| Posterior pelvic ring | 1.84 | 1.21 | 0.69 |
| Anterior pelvic ring | 4.13 | 1.53 | −0.20 |
| Right one-legged stance | |||
| Posterior pelvic ring | 3.22 | 2.05 | 0.86 |
| Anterior pelvic ring | 5.63 | 3.31 | −1.19 |
| Left one-legged stance | |||
| Posterior pelvic ring | 0.01 | 0 | 0.05 |
| Anterior pelvic ring | 3.01 | 0.13 | 0.13 |
| Load Application | USI | BSI | TSI |
|---|---|---|---|
| Bipedal stance | |||
| S1 right side | 9.95 | 7.22 | 5.23 |
| S1 left side | 7.55 | 4.26 | 4.88 |
| S2 right side | 5.11 | 2.51 | 3.27 |
| S2 left side | 4.76 | 2.49 | 3.26 |
| Right one-legged stance | |||
| S1 right side | 19.99 | 16.23 | 9.27 |
| S1 left side | −1.37 | −0.56 | 0.28 |
| S2 right side | 8.77 | 6.77 | 4.92 |
| S2 left side | 1.33 | 0.41 | 2.08 |
| Left one-legged stance | |||
| S1 right side | −0.52 | −0.42 | 0.20 |
| S1 left side | 15.71 | 9.98 | 8.91 |
| S2 right side | 1.09 | 0.04 | 0.67 |
| S2 left side | 10.58 | 9.28 | 7.94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lodde, M.F.; Klimek, M.; Herbst, E.; Peez, C.; Riesenbeck, O.; Raschke, M.J.; Roßlenbroich, S. Bilateral Iliosacral and Transsacral Screws Are Biomechanically Favorable and Reduce the Risk for Fracture Progression in Fragility Fractures of the Pelvis—A Finite Element Analysis. Bioengineering 2025, 12, 27. https://doi.org/10.3390/bioengineering12010027
Lodde MF, Klimek M, Herbst E, Peez C, Riesenbeck O, Raschke MJ, Roßlenbroich S. Bilateral Iliosacral and Transsacral Screws Are Biomechanically Favorable and Reduce the Risk for Fracture Progression in Fragility Fractures of the Pelvis—A Finite Element Analysis. Bioengineering. 2025; 12(1):27. https://doi.org/10.3390/bioengineering12010027
Chicago/Turabian StyleLodde, Moritz F., Matthias Klimek, Elmar Herbst, Christian Peez, Oliver Riesenbeck, Michael J. Raschke, and Steffen Roßlenbroich. 2025. "Bilateral Iliosacral and Transsacral Screws Are Biomechanically Favorable and Reduce the Risk for Fracture Progression in Fragility Fractures of the Pelvis—A Finite Element Analysis" Bioengineering 12, no. 1: 27. https://doi.org/10.3390/bioengineering12010027
APA StyleLodde, M. F., Klimek, M., Herbst, E., Peez, C., Riesenbeck, O., Raschke, M. J., & Roßlenbroich, S. (2025). Bilateral Iliosacral and Transsacral Screws Are Biomechanically Favorable and Reduce the Risk for Fracture Progression in Fragility Fractures of the Pelvis—A Finite Element Analysis. Bioengineering, 12(1), 27. https://doi.org/10.3390/bioengineering12010027







