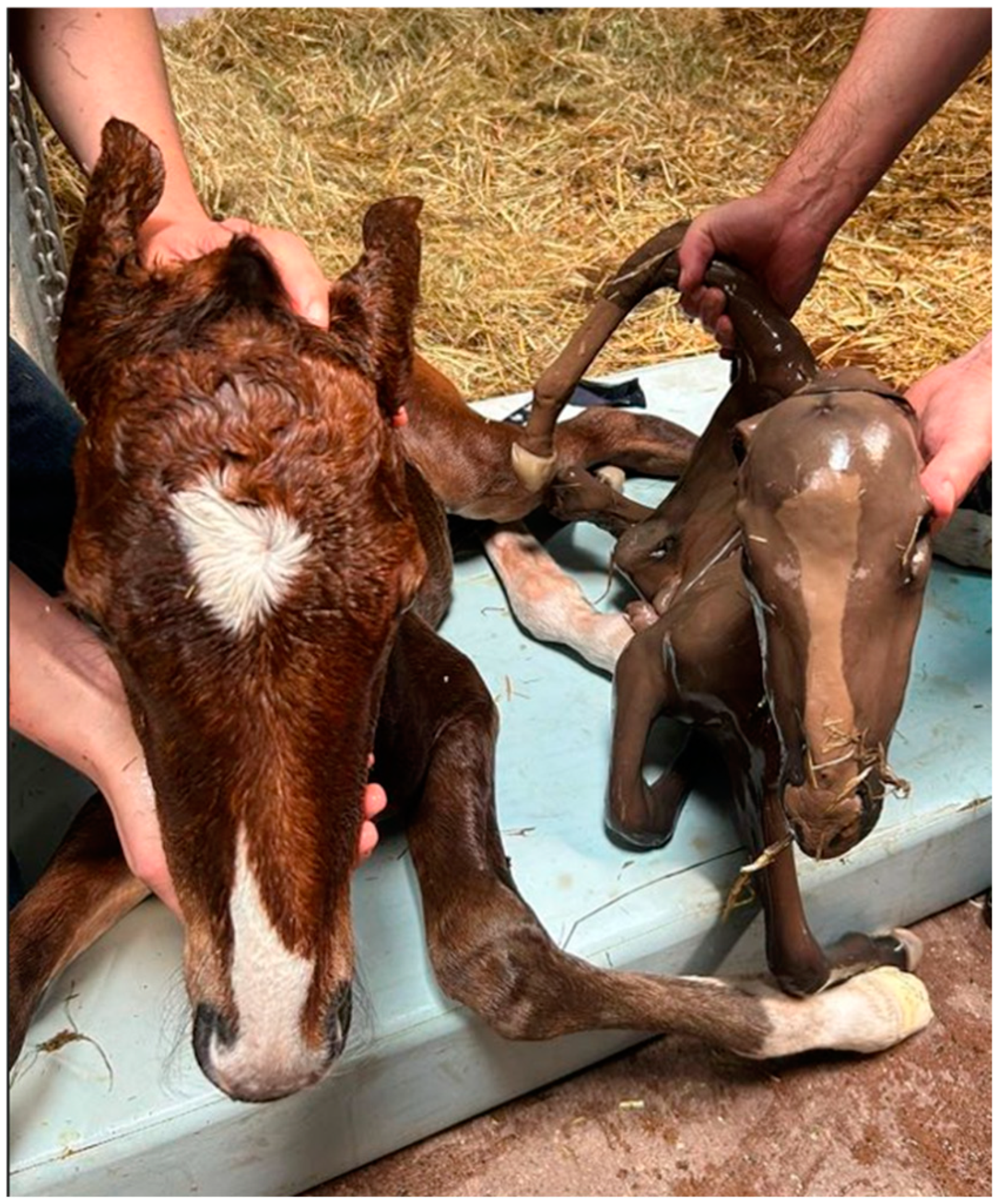
Birth of a Healthy Monozygotic Twin Foal with Hydrops and a Dead Co-Twin
Simple Summary
Abstract
1. Introduction
2. Case Description
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dijkstra, A.; Cuervo-Arango, J.; Stout, T.A.E.; Claes, A. Monozygotic Multiple Pregnancies after Transfer of Single In Vitro Produced Equine Embryos. Equine Vet. J. 2020, 52, 258–261. [Google Scholar] [CrossRef]
- Mancill, S.S.; Blodgett, G.; Arnott, R.J.; Alvarenga, M.; Love, C.C.; Hinrichs, K. Description and Genetic Analysis of Three Sets of Monozygotic Twins Resulting from Transfers of Single Embryos to Recipient Mares. J. Am. Vet. Med. Assoc. 2011, 238, 1040–1043. [Google Scholar] [CrossRef]
- Peere, S.; van Den Branden, E.; Papas, M.; Gerits, I.; Smits, K.; Govaere, J. Twin Management in the Mare: A Review. Equine Vet. J. 2024, 56, 650–659. [Google Scholar] [CrossRef]
- Peere, S.; Papas, M.; Gerits, I.; Van den Branden, E.; Smits, K.; Govaere, J. Management of Monozygotic Twins in the Mare. J. Equine Vet. Sci. 2022, 113, 103988. [Google Scholar] [CrossRef]
- Arnold, L.C.; Stout, T.A.E.; Claes, A.N.J. Ultrasound-Guided Fetal Thorax Compression to Reduce Post-Fixation Twins in the Mare. Equine Vet. J. 2024, 56, 735–741. [Google Scholar] [CrossRef] [PubMed]
- Lewi, L. What Fetal Medicine Specialists Should Know about the Monochorionic Placenta. Best Pract. Res. Clin. Obstet. Gynaecol. 2022, 84, 17–32. [Google Scholar] [CrossRef] [PubMed]
- Morris, K.R.; Mackie, F.; Garces, A.T.; Knight, M.; Kilby, M.D. The Incidence, Maternal, Fetal and Neonatal Consequences of Single Intrauterine Fetal Death in Monochorionic Twins: A Prospective Observational UKOSS Study. PLoS ONE 2020, 15, e0239477. [Google Scholar] [CrossRef] [PubMed]
- Yinon, Y.; Ashwal, E.; Weisz, B.; Chayen, B.; Schiff, E.; Lipitz, S. Selective Reduction in Complicated Monochorionic Twins: Prediction of Obstetric Outcome and Comparison of Techniques. Ultrasound Obstet. Gynecol. 2015, 46, 670–677. [Google Scholar] [CrossRef] [PubMed]
- Waelchli, R. Hydrops. In Equine Reproduction; Vaala, W.E., Dickson, V.D., Squires, E.L., McKinnon, A.O., Eds.; Wiley-Blackwell: Ames, IA, USA, 2011; Volume 2, pp. 2368–2372. [Google Scholar]
- Diel de Amorim, M.; Chenier, T.S.; Card, C.; Back, B.; McClure, J.T.; Hanna, P. Treatment of Hydropsical Conditions Using Transcervical Gradual Fetal Fluid Drainage in Mares With or Without Concurrent Abdominal Wall Disease. J. Equine Vet. Sci. 2018, 64, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Govaere, J.L.J.; De Schauwer, C.; Hoogewijs, M.K.; Chiers, K.; Lefère, L.; Catry, B.; Roels, K.; Van Heerden, M.; Broeckx, S.; De Kruif, A. Hydrallantois in the Mare-A Report of Five Cases. Reprod. Domest. Anim. 2013, 48, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Christensen, B.W.; Troedsson, M.H.T.; Murchie, T.A.; Pozor, M.A.; Vet, M.; Macpherson, M.L.; Estrada, A.H.; Carrillo, N.A.; Mackay, R.J.; Roberts, G.D.; et al. Management of Hydrops Amnion in a Mare Resulting in Birth of a Live Foal. J. Am. Vet. Med. Assoc. 2006, 228, 1228–1233. [Google Scholar] [CrossRef]
- Slovis, N.M.; Acvim, D.; Lu, K.G.; Act, D.; Wolfsdorf, K.E.; Zent, W.W. How to Manage Hydrops Allantois/Hydrops Amnion in a Mare. In Proceedings of the American Association of Equine Practitioners, Nashville, TN, USA, 11 December 2013. [Google Scholar]
- Vera, L.; Decloedt, A.; Van Steenkiste, G.; De Clercq, D.; Govaere, J.; van Loon, G. Electrocardiographic Confirmation of a Twin Pregnancy in a Mare at 8 Months of Gestation. J. Vet. Cardiol. 2018, 20, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Reef, V.B.; Vaala, W.E.; Worth, L.T.; Sertich, P.L.; Spencer, P.A. Ultrasonographic Assessment of Fetal Well-Being during Late Gestation: Development of an Equine Biophysical Profile. Equine Vet. J. 1996, 28, 200–208. [Google Scholar] [CrossRef]
- Bucca, S.; Fogarty, U.; Collins, A.; Small, V. Assessment of Feto-Placental Well-Being in the Mare from Mid-Gestation to Term: Transrectal and Transabdominal Ultrasonographic Features. Theriogenology 2005, 64, 542–557. [Google Scholar] [CrossRef]
- Allen, W.E. Two Cases of Abnormal Equine Pregnancy Associated with Excess Foetal Fluid. Equine Vet. J. 1986, 18, 220–222. [Google Scholar] [CrossRef]
- Blanchard, T.; Vamer, D.; Buonanno, A.; Palmer, V.L.; Hansen, T.; Divers, T. Hydrallantois in Two Mares. J. Equine Vet. Sci. 1987, 7, 222–225. [Google Scholar] [CrossRef]
- Williams, M.A.; Wallace, S.S.; Tyler, J.W.; McCall, C.A.; Gutierrez, A.; Spano, J.S. Biochemical Characteristics of Amniotic and Allantoic Fluid in Late Gestational Mares. Theriogenology 1993, 40, 1251–1257. [Google Scholar] [CrossRef]
- Canisso, I.F.; Ball, B.A.; Squires, E.L.; Troedsson, M.H. How to Perform Transabdominal Ultrasound-Guided Fetal Fluid Sampling in Mares. J. Equine Vet. Sci. 2014, 34, 1143–1147. [Google Scholar] [CrossRef]
- Honnas, C.M.; Spensley, M.S.; Laverty, S.; Blanchard, P.C. Hydramnios Causing Uterine Rupture in a Mare. J. Am. Vet. Med. Assoc. 1988, 193, 334–336. [Google Scholar] [PubMed]
- Canisso, I.; Ball, B.A.; Erol, E.; Squires, E.L.; Troedsson, M.H.T. Comprehensive Review Comprehensive Review on Equine Placentitis. In Proceedings of the 61st Annual Convention of the American Association of Equine Practitioners, Las Vegas, NV, USA, 5 December 2015; Volume 61, pp. 430–509. [Google Scholar]
- Renaudin, C.D.; Troedsson, M.H.; Gillis, C.L.; King, V.L.; Bodena, A. Ultrasonographic Evaluation of the Equine Placenta by Transrectal and Transabdominal Approach in the Normal Pregnant Mare. Theriogenology 1997, 47, 559–573. [Google Scholar] [CrossRef] [PubMed]
- McCue, P.M. Combined Thickness of the Uterus and Placenta. In Equine Reproductive Procedures; McCue, P., Dascanio, J., Eds.; Wiley and Sons: Hoboken, NJ, USA, 2021; pp. 277–279. [Google Scholar]
- Schmidt, A.R.; Williams, M.A.; Carleton, C.L.; Darien, B.J.; Derksen, F.J. Evaluation of Transabdominal Ultrasound-Guided Amniocentesis in the Late Gestational Mare. Equine Vet. J. 1991, 23, 261–265. [Google Scholar] [CrossRef]
- Njaa, B. Appendix A: Gestational Age Estimation Based on Fetal Measures and Phenotypic Characteristics. In Kirkbride’s Diagnosis of Abortion and Neonatal Loss in Animals; Wiley: New York, NY, USA, 2012; pp. 221–224. [Google Scholar]
- Bergin, W.C.; Gier, H.; Frey, R.A.; Marion, G.B. Developmental Horizons and Measurements Useful for Age Determination of Equine Embryos and Fetuses; American Association of Equine Practitioners: Manhattan, Kansas, 1967; pp. 179–196. [Google Scholar]
- Medica, P.; Cravana, C.; Bruschetta, G.; Ferlazzo, A.; Fazio, E. Physiological and Behavioral Patterns of Normal-Term Thoroughbred Foals. J. Vet. Behav. 2018, 26, 38–42. [Google Scholar] [CrossRef]
- Nógrádi, N.; Magdesian, K.G. Physical Examination of the Neonatal Foal. In Manual of Clinical Procedures in the Horse; Rose, M.P., Lais, R.R.C., Eds.; Wiley: Hoboken, NJ, USA, 2017; pp. 416–426. [Google Scholar]
- Robinson, K.A.; Manning, S.T. Premature Lactation and Retention of a Mummified Fetus with Live Birth of the Co-Twin in a Primiparous Morgan Mare. Can. Vet. J. 2011, 52, 423–425. [Google Scholar]
- Wilsher, S.; Allen, W.R. Factors Influencing Placental Development and Function in the Mare. Equine Vet. J. 2012, 44, 113–119. [Google Scholar] [CrossRef]
- McCue, P.M.; Sitters, S. Dystocia Management. In Equine Reproductive Procedures; McCue, P., Dascanio, J., Eds.; Wiley and Sons: Hoboken, NJ, USA, 2021; pp. 365–368. [Google Scholar]
- Wilsher, S. Love Thy Neighbour–Unless They Are Sharing Your Uterus. Equine Vet. Educ. 2022, 34, 22–25. [Google Scholar] [CrossRef]
- Buyukkaya, A.; Tekbas, G.; Buyukkaya, R. Twin Reversed Arterial Perfusion (TRAP) Sequence; Characteristic Gray-Scale and Doppler Ultrasonography Findings. Iran. J. Radiol. 2015, 12, e14979. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peere, S.; Van den Branden, E.; Broothaers, K.; Polfliet, E.; Smits, K.; Govaere, J. Birth of a Healthy Monozygotic Twin Foal with Hydrops and a Dead Co-Twin. Vet. Sci. 2024, 11, 649. https://doi.org/10.3390/vetsci11120649
Peere S, Van den Branden E, Broothaers K, Polfliet E, Smits K, Govaere J. Birth of a Healthy Monozygotic Twin Foal with Hydrops and a Dead Co-Twin. Veterinary Sciences. 2024; 11(12):649. https://doi.org/10.3390/vetsci11120649
Chicago/Turabian StylePeere, Sofie, Emma Van den Branden, Klaartje Broothaers, Ellen Polfliet, Katrien Smits, and Jan Govaere. 2024. "Birth of a Healthy Monozygotic Twin Foal with Hydrops and a Dead Co-Twin" Veterinary Sciences 11, no. 12: 649. https://doi.org/10.3390/vetsci11120649
APA StylePeere, S., Van den Branden, E., Broothaers, K., Polfliet, E., Smits, K., & Govaere, J. (2024). Birth of a Healthy Monozygotic Twin Foal with Hydrops and a Dead Co-Twin. Veterinary Sciences, 11(12), 649. https://doi.org/10.3390/vetsci11120649






