Five Amino Acid Substitutions in the S1 Unit of Infectious Bronchitis Virus Are Critical Determinants Enhancing Its Adaptation to Vero Cells
Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Cell Culture and Virus
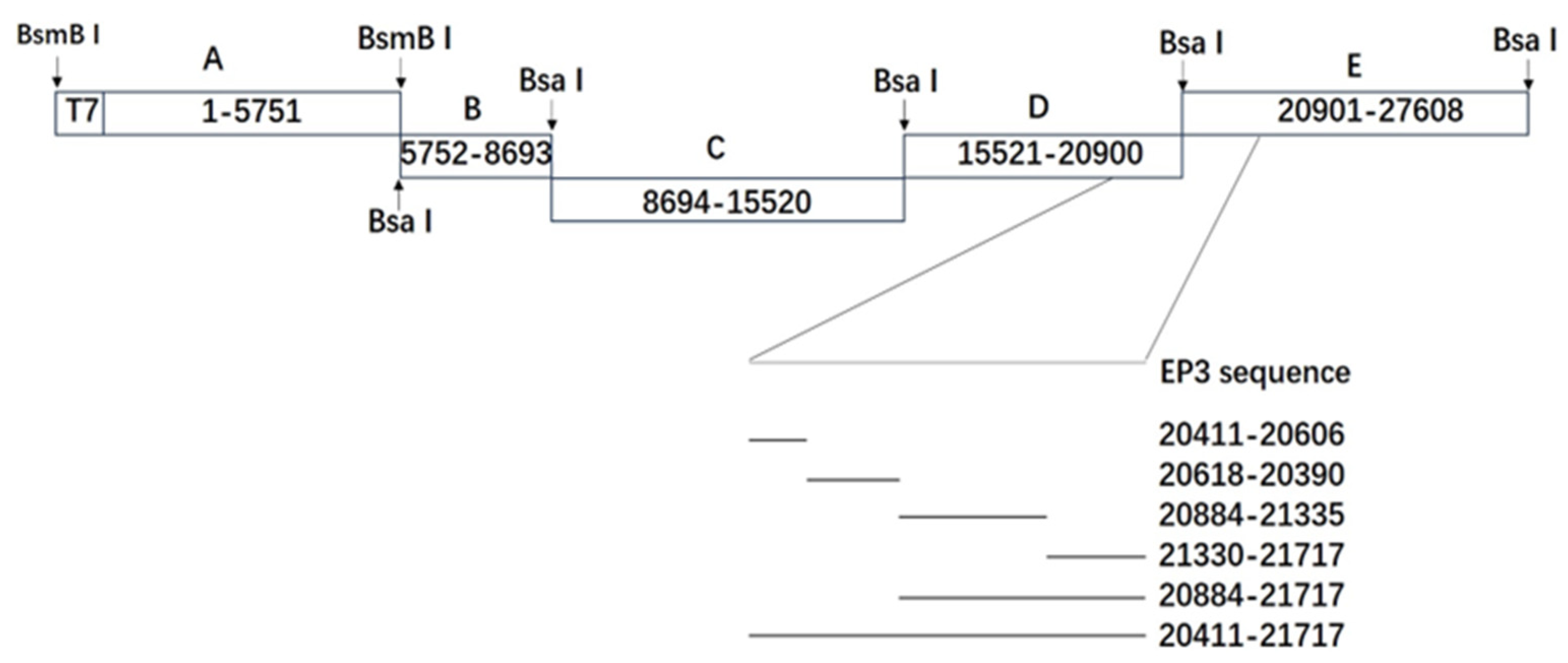
2.2. Generation of Mutant Viruses
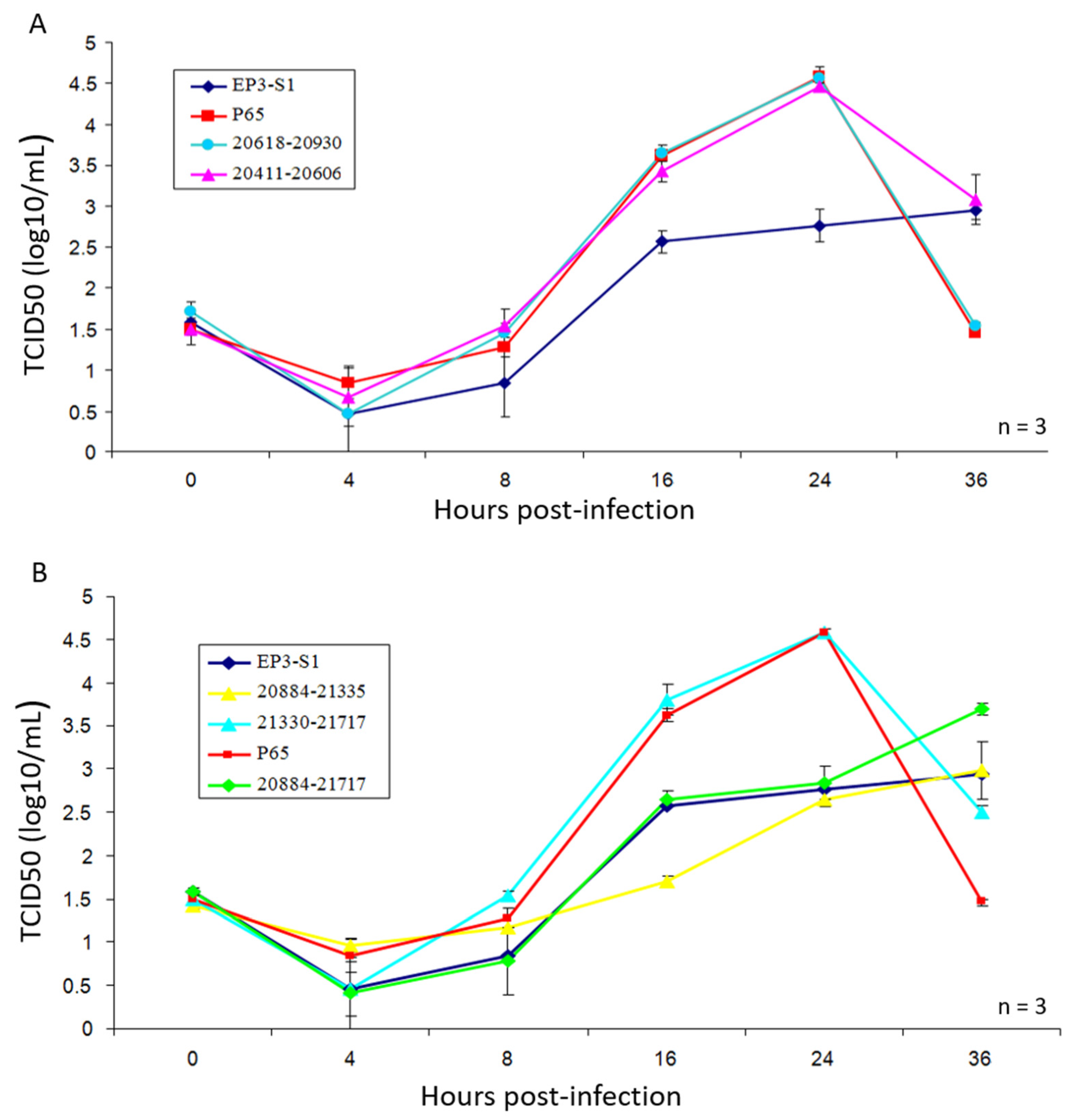
2.3. Growth Curves of Recombinant Viruses on Vero Cells
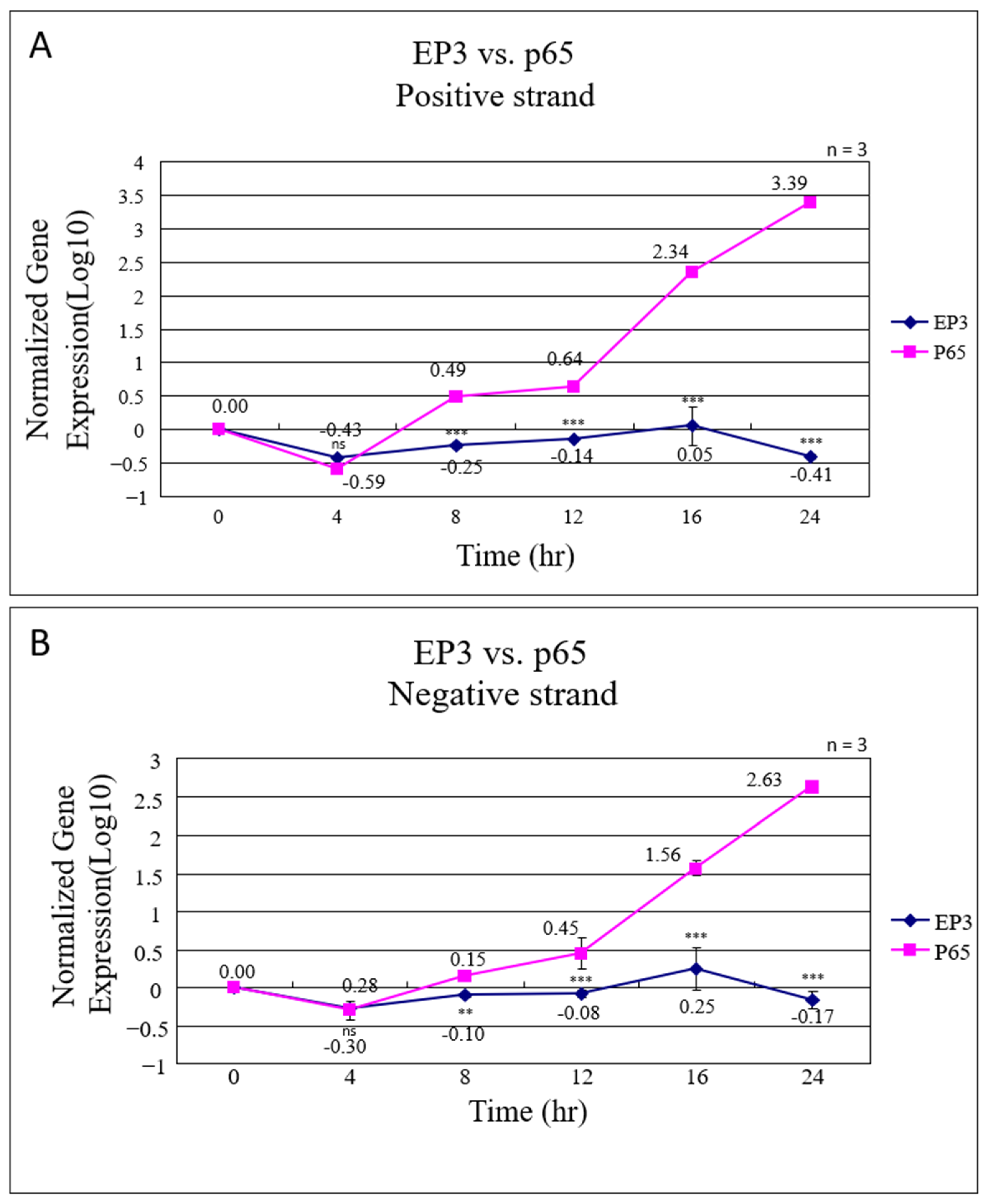
2.4. Analysis of RNA Synthesis of EP3 by Real-Time PCR
2.5. Growth Curves of Viruses
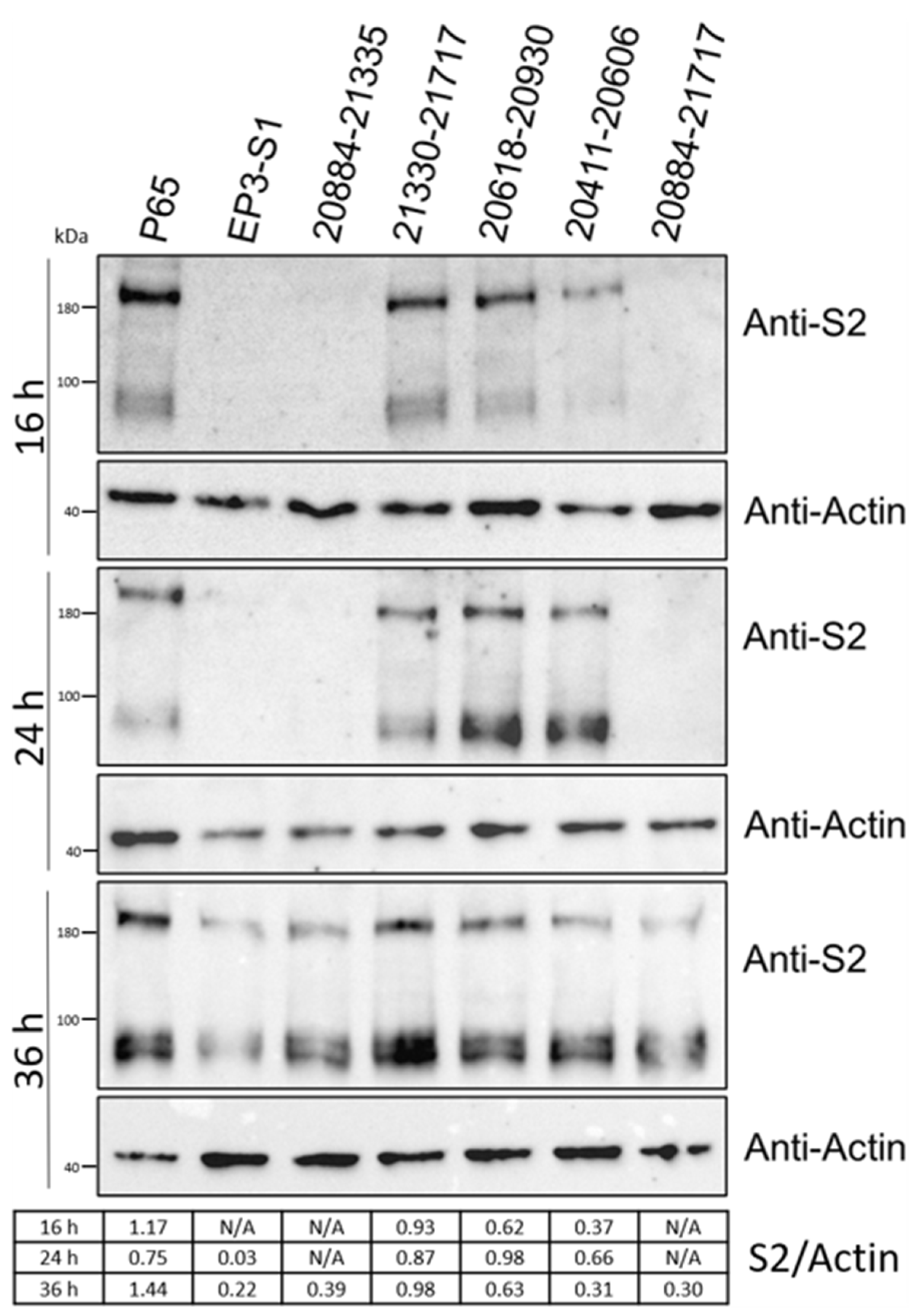
2.6. Western Blotting
3. Results
3.1. Assessment of Infectivity of IBV-EP3 and IBV-P65 in Vero Cells
3.2. Recovery of Recombinant Viruses
3.3. Growth Characteristics of Recombinant Viruses
3.4. Effects of Amino Acid Changes on Expression of IBV-S
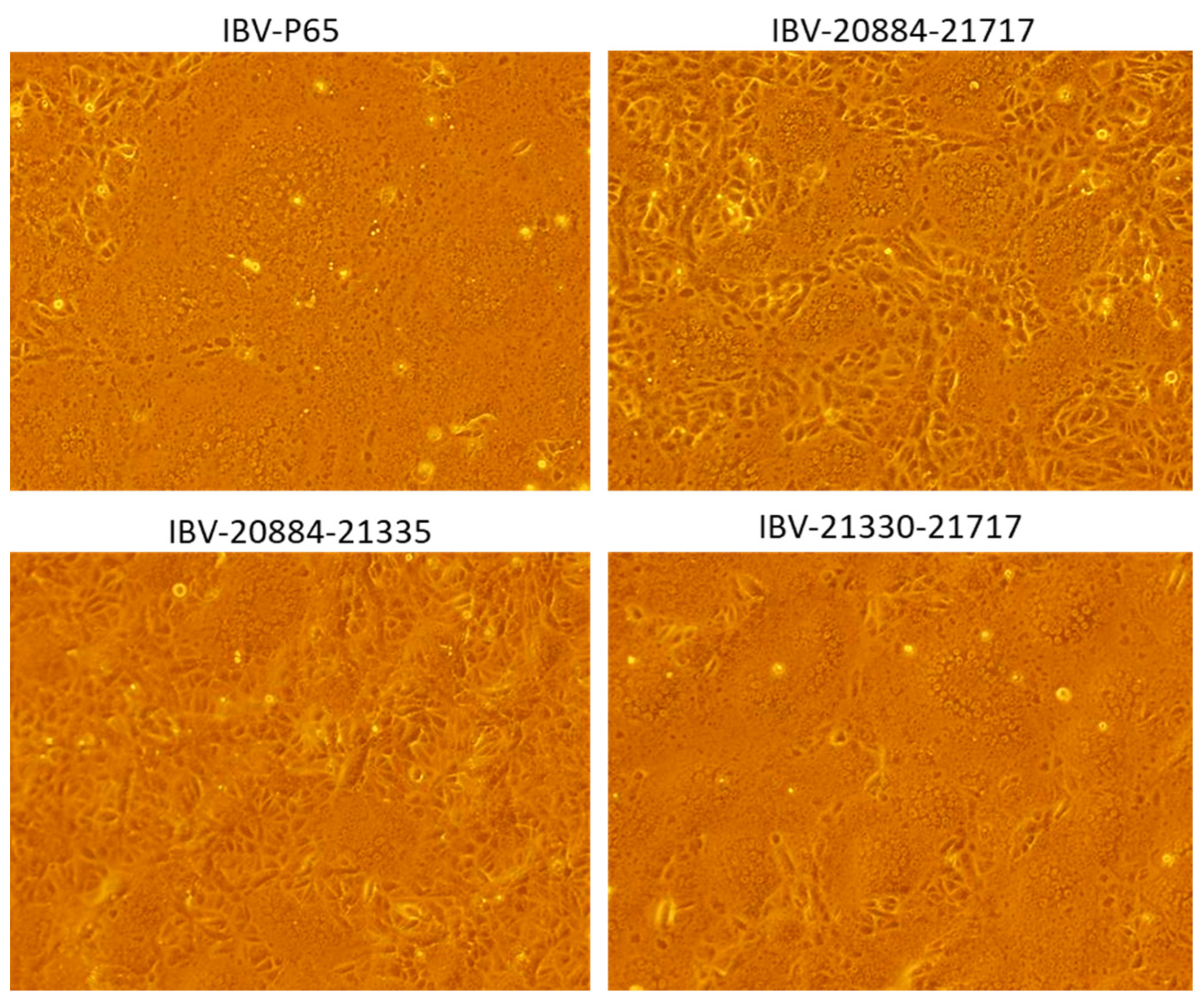
3.5. Effects of Amino Acid Changes on CPE Formation
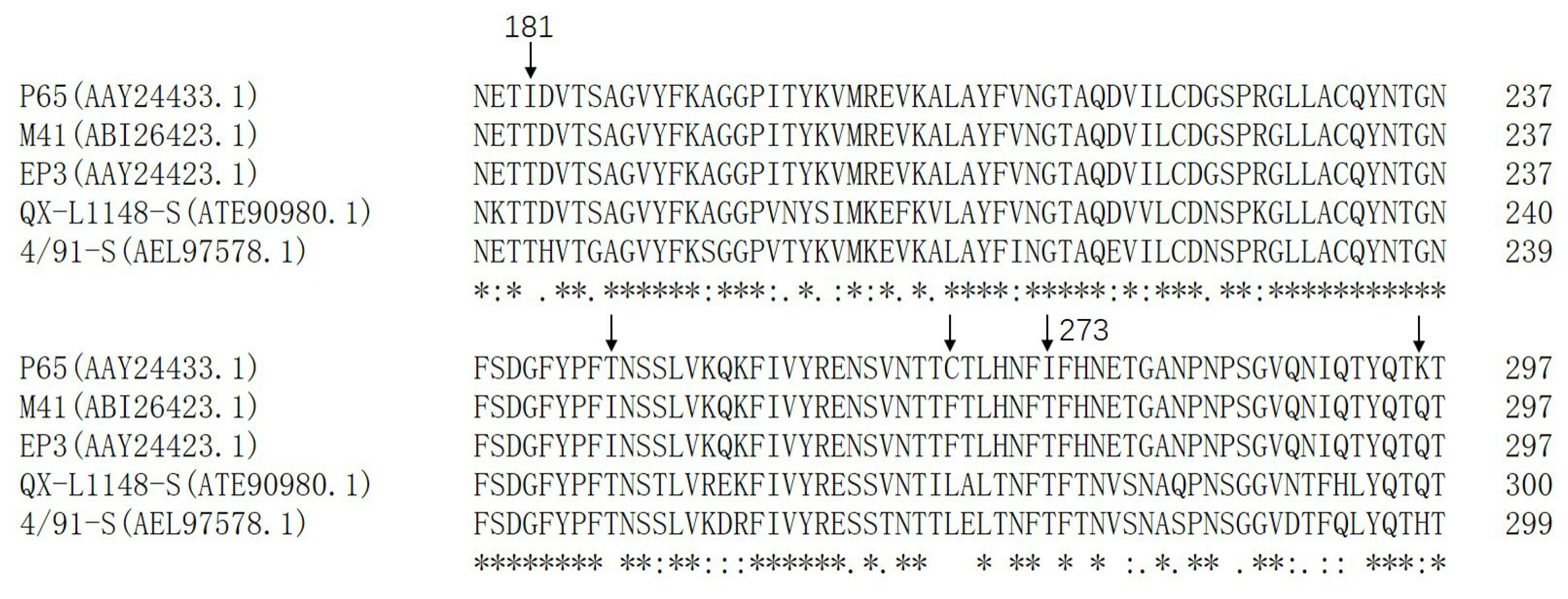
3.6. Amino Acid Sequence Alignment of Different IBV Strains
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Graham, R.L.; Donaldson, E.F.; Baric, R.S. A decade after SARS: Strategies for controlling emerging coronaviruses. Nat. Rev. Microbiol. 2013, 11, 836–848. [Google Scholar] [CrossRef] [PubMed]
- de Wilde, A.H.; Snijder, E.J.; Kikkert, M.; van Hemert, M.J. Host Factors in Coronavirus Replication. Curr. Top. Microbiol. Immunol. 2018, 419, 1–42. [Google Scholar] [CrossRef] [PubMed]
- Li, F. Structure, Function, and Evolution of Coronavirus Spike Proteins. Annu. Rev. Virol. 2016, 3, 237–261. [Google Scholar] [CrossRef] [PubMed]
- Cook, J.K.; Jackwood, M.; Jones, R.C. The long view: 40 years of infectious bronchitis research. Avian Pathol. 2012, 41, 239–250. [Google Scholar] [CrossRef]
- Jackwood, M.W. Review of infectious bronchitis virus around the world. Avian Dis. 2012, 56, 634–641. [Google Scholar] [CrossRef]
- Sjaak de Wit, J.J.; Cook, J.K.; van der Heijden, H.M. Infectious bronchitis virus variants: A review of the history, current situation and control measures. Avian Pathol. 2011, 40, 223–235. [Google Scholar] [CrossRef]
- Casais, R.; Dove, B.; Cavanagh, D.; Britton, P. Recombinant avian infectious bronchitis virus expressing a heterologous spike gene demonstrates that the spike protein is a determinant of cell tropism. J. Virol. 2003, 77, 9084–9089. [Google Scholar] [CrossRef]
- Luo, Z.; Weiss, S.R. Roles in cell-to-cell fusion of two conserved hydrophobic regions in the murine coronavirus spike protein. Virology 1998, 244, 483–494. [Google Scholar] [CrossRef]
- Belouzard, S.; Millet, J.K.; Licitra, B.N.; Whittaker, G.R. Mechanisms of coronavirus cell entry mediated by the viral spike protein. Viruses 2012, 4, 1011–1033. [Google Scholar] [CrossRef]
- Shang, J.; Zheng, Y.; Yang, Y.; Liu, C.; Geng, Q.; Luo, C.; Zhang, W.; Li, F. Cryo-EM structure of infectious bronchitis coronavirus spike protein reveals structural and functional evolution of coronavirus spike proteins. PLoS Pathog. 2018, 14, e1007009. [Google Scholar] [CrossRef]
- Madu, I.G.; Chu, V.C.; Lee, H.; Regan, A.D.; Bauman, B.E.; Whittaker, G.R. Heparan sulfate is a selective attachment factor for the avian coronavirus infectious bronchitis virus Beaudette. Avian Dis. 2007, 51, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Promkuntod, N.; Wickramasinghe, I.N.; de Vrieze, G.; Gröne, A.; Verheije, M.H. Contributions of the S2 spike ectodomain to attachment and host range of infectious bronchitis virus. Virus Res. 2013, 177, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Wickramasinghe, I.N.; van Beurden, S.J.; Weerts, E.A.; Verheije, M.H. The avian coronavirus spike protein. Virus Res. 2014, 194, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Cavanagh, D.; Casais, R.; Armesto, M.; Hodgson, T.; Izadkhasti, S.; Davies, M.; Lin, F.; Tarpey, I.; Britton, P. Manipulation of the infectious bronchitis coronavirus genome for vaccine development and analysis of the accessory proteins. Vaccine 2007, 25, 5558–5562. [Google Scholar] [CrossRef]
- Valastro, V.; Holmes, E.C.; Britton, P.; Fusaro, A.; Jackwood, M.W.; Cattoli, G.; Monne, I. S1 gene-based phylogeny of infectious bronchitis virus: An attempt to harmonize virus classification. Infect. Genet. Evol. 2016, 39, 349–364. [Google Scholar] [CrossRef]
- Dwars, R.M.; Matthijs, M.G.; Daemen, A.J.; van Eck, J.H.; Vervelde, L.; Landman, W.J. Progression of lesions in the respiratory tract of broilers after single infection with Escherichia coli compared to superinfection with E. coli after infection with infectious bronchitis virus. Vet. Immunol. Immunopathol. 2009, 127, 65–76. [Google Scholar] [CrossRef]
- Matthijs, M.G.; van Eck, J.H.; Landman, W.J.; Stegeman, J.A. Ability of Massachusetts-type infectious bronchitis virus to increase colibacillosis susceptibility in commercial broilers: A comparison between vaccine and virulent field virus. Avian Pathol. 2003, 32, 473–481. [Google Scholar] [CrossRef]
- Ignjatović, J.; Sapats, S. Avian infectious bronchitis virus. Rev. Sci. Tech. 2000, 19, 493–508. [Google Scholar] [CrossRef]
- Raj, G.D.; Jones, R.C. Infectious bronchitis virus: Immunopathogenesis of infection in the chicken. Avian Pathol. 1997, 26, 677–706. [Google Scholar] [CrossRef]
- Hodgson, T.; Casais, R.; Dove, B.; Britton, P.; Cavanagh, D. Recombinant infectious bronchitis coronavirus Beaudette with the spike protein gene of the pathogenic M41 strain remains attenuated but induces protective immunity. J. Virol. 2004, 78, 13804–13811. [Google Scholar] [CrossRef]
- Bouwman, K.M.; Parsons, L.M.; Berends, A.J.; de Vries, R.P.; Cipollo, J.F.; Verheije, M.H. Three Amino Acid Changes in Avian Coronavirus Spike Protein Allow Binding to Kidney Tissue. J. Virol. 2020, 94, e01363-19. [Google Scholar] [CrossRef] [PubMed]
- Otsuki, K.; Noro, K.; Yamamoto, H.; Tsubokura, M. Studies on avian infectious bronchitis virus (IBV). II. Propagation of IBV in several cultured cells. Arch. Virol. 1979, 60, 115–122. [Google Scholar] [CrossRef] [PubMed]
- Tay, F.P.; Huang, M.; Wang, L.; Yamada, Y.; Liu, D.X. Characterization of cellular furin content as a potential factor determining the susceptibility of cultured human and animal cells to coronavirus infectious bronchitis virus infection. Virology 2012, 433, 421–430. [Google Scholar] [CrossRef]
- Fang, S.G.; Shen, S.; Tay, F.P.; Liu, D.X. Selection of and recombination between minor variants lead to the adaptation of an avian coronavirus to primate cells. Biochem. Biophys. Res. Commun. 2005, 336, 417–423. [Google Scholar] [CrossRef]
- Fang, S.; Chen, B.; Tay, F.P.; Ng, B.S.; Liu, D.X. An arginine-to-proline mutation in a domain with undefined functions within the helicase protein (Nsp13) is lethal to the coronavirus infectious bronchitis virus in cultured cells. Virology 2007, 358, 136–147. [Google Scholar] [CrossRef] [PubMed]
- Promkuntod, N.; van Eijndhoven, R.E.; de Vrieze, G.; Gröne, A.; Verheije, M.H. Mapping of the receptor-binding domain and amino acids critical for attachment in the spike protein of avian coronavirus infectious bronchitis virus. Virology 2014, 448, 26–32. [Google Scholar] [CrossRef]
- You, R.; Liu, K.; Huang, M.; Tang, L.; Zhang, X.; Huang, Y.; Zhao, J.; Zhao, Y.; Ye, L.; Zhang, G. Identification and Comparison of the Sialic Acid-Binding Domain Characteristics of Avian Coronavirus Infectious Bronchitis Virus Spike Protein. J. Virol. 2023, 97, e0048923. [Google Scholar] [CrossRef]
- Wei, Y.Q.; Guo, H.C.; Dong, H.; Wang, H.M.; Xu, J.; Sun, D.H.; Fang, S.G.; Cai, X.P.; Liu, D.X.; Sun, S.Q. Development and characterization of a recombinant infectious bronchitis virus expressing the ectodomain region of S1 gene of H120 strain. Appl. Microbiol. Biotechnol. 2014, 98, 1727–1735. [Google Scholar] [CrossRef]
- Shan, D.; Fang, S.; Han, Z.; Ai, H.; Zhao, W.; Chen, Y.; Jiang, L.; Liu, S. Effects of hypervariable regions in spike protein on pathogenicity, tropism, and serotypes of infectious bronchitis virus. Virus Res. 2018, 250, 104–113. [Google Scholar] [CrossRef]
- Bouwman, K.M.; Habraeken, N.; Laconi, A.; Berends, A.J.; Groenewoud, L.; Alders, M.; Kemp, V.; Verheije, M.H. N-glycosylation of infectious bronchitis virus M41 spike determines receptor specificity. J. Gen. Virol. 2020, 101, 599–608. [Google Scholar] [CrossRef]
- Zheng, J.; Yamada, Y.; Fung, T.S.; Huang, M.; Chia, R.; Liu, D.X. Identification of N-linked glycosylation sites in the spike protein and their functional impact on the replication and infectivity of coronavirus infectious bronchitis virus in cell culture. Virology 2018, 513, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Parsons, L.M.; Bouwman, K.M.; Azurmendi, H.; de Vries, R.P.; Cipollo, J.F.; Verheije, M.H. Glycosylation of the viral attachment protein of avian coronavirus is essential for host cell and receptor binding. J. Biol. Chem. 2019, 294, 7797–7809. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Brunak, S. Prediction of glycosylation across the human proteome and the correlation to protein function. In Biocomputing; 2002; pp. 310–322. Available online: https://www.worldscientific.com (accessed on 20 April 2025). [PubMed]
- Bandyopadhyay, A.S.; Garon, J.; Seib, K.; Orenstein, W.A. Polio vaccination: Past, present and future. Future Microbiol. 2015, 10, 791–808. [Google Scholar] [CrossRef]
- Fooks, A.R.; Banyard, A.C.; Ertl, H.C.J. New human rabies vaccines in the pipeline. Vaccine 2019, 37 (Suppl. S1), A140–A145. [Google Scholar] [CrossRef] [PubMed]
- Ehrlich, H.J.; Berezuk, G.; Fritsch, S.; Aichinger, G.; Singer, J.; Portsmouth, D.; Hart, M.K.; El-Amin, W.; Kistner, O.; Barrett, P.N. Clinical development of a Vero cell culture-derived seasonal influenza vaccine. Vaccine 2012, 30, 4377–4386. [Google Scholar] [CrossRef]
- Xia, S.; Duan, K.; Zhang, Y.; Zhao, D.; Zhang, H.; Xie, Z.; Li, X.; Peng, C.; Zhang, Y.; Zhang, W.; et al. Effect of an Inactivated Vaccine Against SARS-CoV-2 on Safety and Immunogenicity Outcomes: Interim Analysis of 2 Randomized Clinical Trials. JAMA 2020, 324, 951–960. [Google Scholar] [CrossRef]
- Bickerton, E.; Dowgier, G.; Britton, P. Recombinant infectious bronchitis viruses expressing heterologous S1 subunits: Potential for a new generation of vaccines that replicate in Vero cells. J. Gen. Virol. 2018, 99, 1681–1685. [Google Scholar] [CrossRef] [PubMed]
- Ting, X.; Xiang, C.; Liu, D.X.; Chen, R. Establishment and Cross-Protection Efficacy of a Recombinant Avian Gammacoronavirus Infectious Bronchitis Virus Harboring a Chimeric S1 Subunit. Front. Microbiol. 2022, 13, 897560. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| Primer | Nucleotide Sequence |
|---|---|
| BsaI-20411-F | 5′-CGGGTCTCTATGTAGTGCTGTTTTGTATGA |
| BsaI-20416-R | 5′-CGGGTCTCTACATAGTGCACACAAAAGAGT |
| BsaI-21330-F | 5′-CGGTCTCGTATGGATCTTATCACCCAA |
| BsaI-21335-R | 5′-CGGTCTCCCATACATAAAATTAGACTC |
| BsaI-20618-F | 5′-CGGGTCTCCGGCACCGTCATCAGGTAT |
| BsaI-20623-R | 5′-CGGGTCTCGTGCCGTCATAGCTATAGA |
| BsaI-21712-F | 5′-CGGGTCTCACCGACTCAGCTGTTAGTTAT |
| BsaI-21717-R | 5′-CGGGTCTCGTCGGTTACATTAGTAATAAA |
| IBV-20884-F | 5′-GTTTACACCTCTAATGAGACCATAG |
| IBV-20930-R | 5′-ACACCTGCAGATGTAACATC’ |
| IBV-15511-F | 5′-GTGATTCATTGAGACCTTTTGC |
| IBV-15532-R | 5′-GCAAAAGGTCTCAATGAATCAC |
| IBV-3′ end | 5′-CggTCTCgTTTTTTTTTTTTTTTTTTTTTTTTTTTTTTgCTC |
| Plasmid | Region (nt) | Source | Primer | Note |
|---|---|---|---|---|
| pGEM-IBV-F | 15,511–20,416 | IBV-P65 | IBV-15511-F BsaI-20416-R | Construction of mutant 20,411–20,606 |
| pGEM-IBV-G | 20,618–20,930 | IBV-P65 | BsaI-20618-F IBV-20930-R | |
| pGEM-EP3-1 | 20,411–20,623 | IBV-EP3 | BsaI-20411-F BsaI-20623-R | |
| pGEM-IBV-H | 15,511–20,623 | IBV-P65 | IBV-15511-F BsaI-20623-R | Construction of mutant 20,618–20,930 |
| pGEM-EP3-2 | 20,618–20,930 | IBV-EP3 | BsaI-20618-F IBV-20930-R | |
| pGEM-IBV-I | 21,712–27,608 | IBV-P65 | BsaI-21712-F IBV-3′ end | Construction of mutant 20,884–21,717 |
| pGEM-EP3-3 | 20,884–21,717 | IBV-EP3 | IBV-20884-F BsaI-21717-R | |
| pGEM-IBV-J | 21,330–27,608 | IBV-P65 | BsaI-21330-F IBV-3′ end | Construction of mutant 20,884–21,335 |
| GEM-IBV-K | 20,884–21,335 | IBV-P65 | IBV-20884-F BsaI-21335-R | |
| pGEM-EP3-4 | 21,330–21,717 | IBV-EP3 | BsaI-21330-F BsaI-21717-R | Construction of mutant 21,330–21,717 |
| pGEM-EP3-5 | 20,411–21,717 | IBV-EP3 | BsaI-20411-F BsaI-21717-R | Construction for mutant EP3-S1 |
| Recombinant Viruses | Replaced Nucleotide Sequences (nt) | Replaced Amino Acid Sequences (aa) | Amino Acid Changes from IBV-P65 to IBV-EP3 |
|---|---|---|---|
| 20,411–20,606 | 20,411–20,606 | 17–82 | S38N, Q43H, F56S, S63P, T66I, I69T |
| 20,618–20,930 | 20,618–20,930 | 86–180 | H117Y, G118D, Q128K, R156K |
| 20,884–21,335 | 20,884–21,335 | 179–323 | I181T, T246I, C267F, I273T, K296Q |
| 21,330–21,717 | 21,330–21,717 | 321–451 | K330N, K364S, H391L, D405G |
| 20,884–21,717 | 20,884–21,717 | 179–451 | I181T, T246I, C267F, I273T, K296Q, K330N, K364S, H391L, D405G |
| EP3-S1 | 20,411–21,717 | 17–451 | S38N, Q43H, F56S, S63P, T66I, I69T, H117Y, G118D, Q128K, R156K, I181T, T246I, C267F, I273T, K296Q, K330N, K364S, H391L, D405G |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cai, Z.; Zhang, M.; Fang, S. Five Amino Acid Substitutions in the S1 Unit of Infectious Bronchitis Virus Are Critical Determinants Enhancing Its Adaptation to Vero Cells. Vet. Sci. 2025, 12, 394. https://doi.org/10.3390/vetsci12050394
Cai Z, Zhang M, Fang S. Five Amino Acid Substitutions in the S1 Unit of Infectious Bronchitis Virus Are Critical Determinants Enhancing Its Adaptation to Vero Cells. Veterinary Sciences. 2025; 12(5):394. https://doi.org/10.3390/vetsci12050394
Chicago/Turabian StyleCai, Zhichao, Mingjing Zhang, and Shouguo Fang. 2025. "Five Amino Acid Substitutions in the S1 Unit of Infectious Bronchitis Virus Are Critical Determinants Enhancing Its Adaptation to Vero Cells" Veterinary Sciences 12, no. 5: 394. https://doi.org/10.3390/vetsci12050394
APA StyleCai, Z., Zhang, M., & Fang, S. (2025). Five Amino Acid Substitutions in the S1 Unit of Infectious Bronchitis Virus Are Critical Determinants Enhancing Its Adaptation to Vero Cells. Veterinary Sciences, 12(5), 394. https://doi.org/10.3390/vetsci12050394






