Methicillin-Resistant Staphylococcus aureus (MRSA) and Other Methicillin-Resistant Staphylococci and Mammaliicoccus (MRNaS) Associated with Animals and Food Products in Arab Countries: A Review
Abstract
Simple Summary
Abstract
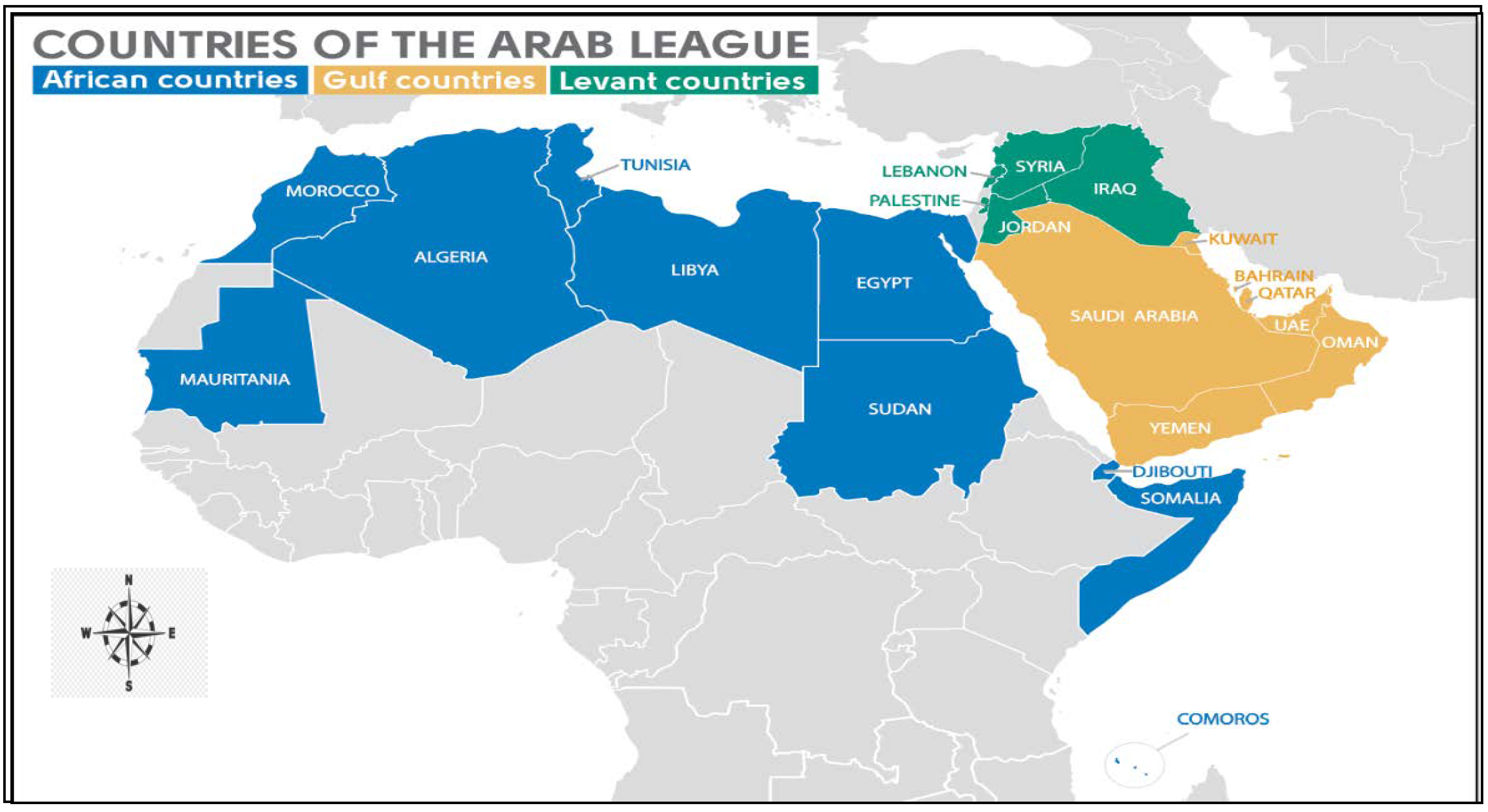
1. Introduction
2. Methicillin-Resistant Staphylococci (MRS) in Animals
2.1. MRSA
2.1.1. MRSA in Food-Producing Animals
MRSA in Cattle
MRSA in Sheep and Goat
MRSA in Poultry
MRSA in Camelids
2.1.2. MRSA in Other Animals
2.1.3. MRSA in Livestock-Derived Food Products
| Source | Year | Country | No. of Tested Samples | No. of MRSA Positive | Lineages of MRSA | Reference |
|---|---|---|---|---|---|---|
| Dairy cattle, sheep, and goat bulk tank milk | 2017 | Jordan | 208 | 54 (25.97%) | ND | [57] |
| Raw cow milk | 2018 | Tunisia | 300 | 3 (20%) | ST4114 ST4120 | [74] |
| Raw camel milk | 2019 | Saudi Arabia | 100 | 10 (50%) | ND | [114] |
| Raw cow milk and traditional dairy products | 2018 | Algeria | 270 | 11 (17,74%) | ST8 | [135] |
| Chicken meat | 2020 | Egypt | 144 | 8 (6%) | N/D | [136] |
| Raw chicken meat | 2015 | Tunisia | 164 | 2 (1.2%) | ST30 t012 ST398 t4358 | [141] |
| Retail meat (camel and chicken) | 2016 | Saudi Arabia | 100 | 6 (6%) | CC1 CC15 CC80 CC88 | [142] |
| Beef meat | 2017 | Egypt | 100 | 4 (4%) | N/D | [145] |
| Unpasteurized milk sold | 2021 | Algeria | 82 | 3 (30%) | ST80 | [146] |
MRSA on Meat and Meat Products
MRSA in Milk and Milk Products
2.2. MRNaS
3. MRS in Animals and Its Impact from a One Health Perspective
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Search Result. Available online: https://lpsn.dsmz.de/search?word=staphylococcus (accessed on 15 May 2022).
- Madhaiyan, M.; Wirth, J.S.; Saravanan, V.S. Phylogenomic analyses of the Staphylococcaceae family suggest the reclassification of five species within the genus Staphylococcus as heterotypic synonyms, the promotion of five subspecies to novel species, the taxonomic reassignment of five Staphylococcus species to Mammaliicoccus gen. nov., and the formal assignment of Nosocomiicoccus to the family Staphylococcaceae. Int. J. Syst. Evol. Microbiol. 2020, 70, 5926–5936. [Google Scholar] [CrossRef] [PubMed]
- Leroy, S.; Vermassen, A.; Talon, R. Staphylococcus: Occurrence and Properties. In 1st Encyclopedia of Food and Health; Elsevier: London, UK, 2015. [Google Scholar] [CrossRef]
- Crossley, K.B.; Jefferson, K.K.; Archer, G.L.; Fowler, V.G. Staphylococci in Human Disease, 2nd ed.; Blackwell Publishing Ltd.: Hoboken, NJ, USA, 2009; pp. 1–623. [Google Scholar]
- Bose, J.L. Genetic manipulation of staphylococci. Methods Mol. Biol. 2014, 1106, 101–111. [Google Scholar] [CrossRef]
- Becker, K.; Schaumburg, F.; Kearns, A.; Larsen, A.R.; Lindsay, J.A.; Skov, R.L.; Westh, H. Implications of identifying the recently defined members of the Staphylococcus aureus complex S. argenteus and S. schweitzeri: A position paper of members of the ESCMID Study Group for Staphylococci and Staphylococcal Diseases (ESGS). Clin. Microbiol. Infect. 2019, 25, 1064–1070. [Google Scholar] [CrossRef] [PubMed]
- Vanderhaeghen, W.; Piepers, S.; Leroy, F.; Van Coillie, E.; Haesebrouck, F.; De Vliegher, S. Identification, typing, ecology and epidemiology of coagulase negative staphylococci associated with ruminants. Vet. J. 2015, 203, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Foster, T. Staphylococcus, 4th ed.; Medical Microbiology; University of Texas Medical Branch: Galveston, TX, USA, 1996; Chapter 12. [Google Scholar]
- Zondervan, N.A.; Martins Dos Santos, V.A.P.; Suarez-Diez, M.; Saccenti, E. Correction to: Phenotype and multi-omics comparison of Staphylococcus and Streptococcus uncovers pathogenic traits and predicts zoonotic potential. BMC Genom. 2021, 22, 384. [Google Scholar] [CrossRef] [PubMed]
- Prestinaci, F.; Pezzotti, P.; Pantosti, A. Antimicrobial resistance: A global multifaceted phenomenon. Pathog. Glob. Health 2015, 109, 309–318. [Google Scholar] [CrossRef]
- Boucher, H.; Miller, L.G.; Razonable, R.R. Serious infections caused by methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 2010, 51, 183–197. [Google Scholar] [CrossRef]
- Jevons, M.P.; Coe, A.W.; Parker, M.T. Methicillin resistance in staphylococci. Lancet 1963, 1, 904–907. [Google Scholar] [CrossRef]
- Itou, T.; Katayama, Y.; Hiramatsu, K. A new mobile genetic element, staphylococcal cassette chromosome mec, encodes methicillin resistance in Staphylococcus aureus. Nihon. Saikingaku. Zasshi. 2000, 55, 483–498. (In Japanese) [Google Scholar] [CrossRef]
- Ben Chehida, F.; Gharsa, H.; Tombari, W.; Selmi, R.; Khaldi, S.; Daaloul, M.; Ben Slama, K.; Messadi, L. First Report of Antimicrobial Susceptibility and Virulence Gene Characterization Associated with Staphylococcus aureus Carriage in Healthy Camels from Tunisia. Animals 2021, 11, 2754. [Google Scholar] [CrossRef]
- Nemeghaire, S.; Vanderhaeghen, W.; Argudín, M.A.; Haesebrouck, F.; Butaye, P. Characterization of methicillin-resistant Staphylococcus sciuri isolates from industrially raised pigs, cattle and broiler chickens. J. Antimicrob. Chemother. 2014, 69, 2928–2934. [Google Scholar] [CrossRef]
- Schnitt, A.; Lienen, T.; Wichmann-Schauer, H.; Tenhagen, B.A. The occurrence of methicillin-resistant non-aureus staphylococci in samples from cows, young stock, and the environment on German dairy farms. J. Dairy Sci. 2021, 104, 4604–4614. [Google Scholar] [CrossRef]
- Vanderhaeghen, W.; Vandendriessche, S.; Crombé, F.; Nemeghaire, S.; Dispas, M.; Denis, O.; Hermans, K.; Haesebrouck, F.; Butaye, P. Characterization of methicillin-resistant non-Staphylococcus aureus staphylococci carriage isolates from different bovine populations. J. Antimicrob. Chemother. 2013, 68, 300–307. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.R.; Mattos, E.M.; Coimbra, M.V.; Ferreira-Carvalho, B.T.; Figueiredo, A.M. Isolation and molecular characterization of methicillin-resistant coagulase-negative staphylococci from nasal flora of healthy humans at three community institutions in Rio de Janeiro City. Epidemiol. Infect. 2001, 127, 57–62. [Google Scholar] [CrossRef]
- Kolappaswamy, K.; Shipley, S.T.; Tatarov, I.I.; DeTolla, L.J. Methicillin-resistant Staphylococcus non-aureus infection in an irradiated rhesus macaque (Macaca mulatta). J. Am. Assoc. Lab. Anim. Sci. 2008, 47, 64–67. [Google Scholar] [PubMed]
- Hanssen, A.M.; Ericson Sollid, J.U. SCCmec in staphylococci: Genes on the move. FEMS. Immunol. Med. Microbiol. 2006, 46, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Haag, A.F.; Fitzgerald, J.R.; Penadés, J.R. Staphylococcus aureus in Animals. Microbiol. Spectr. 2019, 7, 1–19. [Google Scholar] [CrossRef] [PubMed]
- From the Centers for Disease Control and Prevention. Four pediatric deaths from community-acquired methicillin-resistant Staphylococcus aureus—Minnesota and North Dakota, 1997–1999. JAMA 1999, 282, 1123–1125. [Google Scholar]
- Chambers, H.F. The changing epidemiology of Staphylococcus aureus? Emerg. Infect. Dis. 2001, 7, 178–182. [Google Scholar] [CrossRef]
- Simons, H.; Alcabes, P. A model for surveillance of methicillin-resistant Staphylococcus aureus. Public. Health Rep. 2008, 123, 21–29. [Google Scholar] [CrossRef]
- Bukharie, H.A. A review of community-acquired methicillin-resistant Staphylococcus aureus for primary care physicians. J. Fam. Community Med. 2010, 17, 117–120. [Google Scholar] [CrossRef] [PubMed]
- Voss, A.; Loeffen, F.; Bakker, J.; Klaassen, C.; Wulf, M. Methicillin-resistant Staphylococcus aureus in pig farming. Emerg. Infect. Dis. 2005, 11, 1965–1966. [Google Scholar] [CrossRef]
- Denis, O.; Suetens, C.; Hallin, M.; Catry, B.; Ramboer, I.; Dispas, M.; Willems, G.; Gordts, B.; Butaye, P.; Struelens, M.J. Methicillin-resistant Staphylococcus aureus ST398 in swine farm personnel, Belgium. Emerg. Infect. Dis. 2009, 15, 1098–1101. [Google Scholar] [CrossRef] [PubMed]
- Price, L.B.; Stegger, M.; Hasman, H.; Aziz, M.; Larsen, J.; Andersen, P.S.; Pearson, T.; Waters, A.E.; Foster, J.T.; Schupp, J.; et al. Staphylococcus aureus CC398: Host adaptation and emergence of methicillin resistance in livestock. mBio 2012, 3, e00305-11. [Google Scholar] [CrossRef] [PubMed]
- Butaye, P.; Argudín, M.A.; Smith, T.C. Livestock-Associated MRSA and Its Current Evolution. Curr. Clin. Micro. Rpt. 2016, 3, 19–31. [Google Scholar] [CrossRef]
- Berglund, C.; Söderquist, B. The origin of a methicillin-resistant Staphylococcus aureus isolate at a neonatal ward in Sweden-possible horizontal transfer of a staphylococcal cassette chromosome mec between methicillin-resistant Staphylococcus haemolyticus and Staphylococcus aureus. Clin. Microbiol. Infect. 2008, 14, 1048–1056. [Google Scholar] [CrossRef]
- Springer, B.; Orendi, U.; Much, P.; Höger, G.; Ruppitsch, W.; Krziwanek, K.; Metz-Gercek, S.; Mittermayer, H. Methicillin-resistant Staphylococcus aureus: A new zoonotic agent? Wien. Klin. Wochenschr. 2009, 121, 86–90. [Google Scholar] [CrossRef]
- OECD. The Middle East and North Africa: Prospects and challenges. OECDFAO Agric. Outlook 2018, 2, 67–107. [Google Scholar] [CrossRef]
- Arab Countries 2021. Available online: https://worldpopulationreview.com/country-rankings/arab-countries (accessed on 10 January 2022).
- Rizk, N.A.; Moghnieh, R.; Haddad, N.; Rebeiz, M.C.; Zeenny, R.M.; Hindy, J.R.; Orlando, G.; Kanj, S.S. Challenges to Antimicrobial Stewardship in the Countries of the Arab League: Concerns of Worsening Resistance during the COVID-19 Pandemic and Proposed Solutions. Antibiotics 2021, 10, 1320. [Google Scholar] [CrossRef]
- Dandachi, I.; Chaddad, A.; Hanna, J.; Matta, J.; Daoud, Z. Understanding the Epidemiology of Multi-Drug Resistant Gram-Negative Bacilli in the Middle East Using a One Health Approach. Front. Microbiol. 2019, 10, 1941. [Google Scholar] [CrossRef]
- WHO. Global Antimicrobial Resistance Surveillance System (GLASS) Report. 2017. Available online: http://www.who.int/glass/resources/publications/early-implementation-report/en/ (accessed on 25 January 2022).
- Ballouz, T.; Rizk, N.; Kanj, S.S. Antimicrobial Resistance in the Arab Region. In Handbook of Healthcare in the Arab World; Laher, I., Ed.; Springer: Cham, Switzerland, 2019. [Google Scholar] [CrossRef]
- Wall, B.A.; Mateus, A.L.P.; Marshall, L.; Pfeiffer, D.U.; Lubroth, J.; Ormel, H.J.; Otto, P.; Patriarchi, A. Drivers, Dynamics and Epidemiology of Antimicrobial Resistance in Animal Production; FAO: Rome, Italy, 2016. Available online: http://www.fao.org/3/a-i6209e.pdf (accessed on 14 January 2022).
- Ventola, C.L. The antibiotic resistance crisis: Part 1: Causes and threats. Pharm. Ther. 2015, 40, 277–283. [Google Scholar]
- Moghnieh, R.A.; Kanafani, Z.A.; Tabaja, H.Z.; Sharara, S.L.; Awad, L.S.; Kanj, S.S. Epidemiology of common resistant bacterial pathogens in the countries of the Arab League. Lancet Infect. Dis. 2018, 18, 379–394. [Google Scholar] [CrossRef]
- Devriese, L.A.; Van Damme, L.R.; Fameree, L. Methicillin (cloxacillin)-resistant Staphylococcus aureus strains isolated from bovine mastitis cases. Zentralbl. Veterinarmed. B 1972, 19, 598–605. [Google Scholar] [CrossRef] [PubMed]
- Devriese, L.A.; Hommez, J. Epidemiology of methicillin-resistant Staphylococcus aureus in dairy herds. Res. Vet. Sci. 1975, 19, 23–27. [Google Scholar] [CrossRef]
- Larsen, J.; Petersen, A.; Sørum, M.; Stegger, M.; van Alphen, L.; Valentiner-Branth, P.; Knudsen, L.K.; Larsen, L.S.; Feingold, B.; Price, L.B.; et al. Meticillin-resistant Staphylococcus aureus CC398 is an increasing cause of disease in people with no livestock contact in Denmark, 1999 to 2011. Euro. Surveill. 2015, 20, 10. [Google Scholar] [CrossRef]
- Ryser-Degiorgis, M.P. Wildlife health investigations: Needs, challenges and recommendations. BMC Vet. Res. 2013, 9, 223. [Google Scholar] [CrossRef]
- Vanderhaeghen, W.; Cerpentier, T.; Adriaensen, C.; Vicca, J.; Hermans, K.; Butaye, P. Methicillin-resistant Staphylococcus aureus (MRSA) ST398 associated with clinical and subclinical mastitis in Belgian cows. Vet. Microbiol. 2010, 144, 166–171. [Google Scholar] [CrossRef]
- Argudín, M.A.; Cariou, N.; Salandre, O.; Le Guennec, J.; Nemeghaire, S.; Butaye, P. Genotyping and antimicrobial resistance of Staphylococcus aureus isolates from diseased turkeys. Avian. Pathol. 2013, 42, 572–580. [Google Scholar] [CrossRef]
- Cuny, C.; Wieler, L.H.; Witte, W. Livestock-Associated MRSA: The Impact on Humans. Antibiotics 2015, 4, 521–543. [Google Scholar] [CrossRef]
- Van Cleef, B.A.; Monnet, D.L.; Voss, A.; Krziwanek, K.; Allerberger, F.; Struelens, M.; Zemlickova, H.; Skov, R.L.; Vuopio-Varkila, J.; Cuny, C.; et al. Livestock-associated methicillin-resistant Staphylococcus aureus in humans, Europe. Emerg. Infect. Dis. 2011, 17, 502–505. [Google Scholar] [CrossRef]
- Fitzgerald, J.R. Livestock-associated Staphylococcus aureus: Origin, evolution and public health threat. Trends. Microbiol. 2012, 20, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Senok, A.; Slickers, P.; Hotzel, H.; Boswihi, S.; Braun, S.D.; Gawlik, D.; Müller, E.; Nabi, A.; Nassar, R.; Nitschke, H.; et al. Characterisation of a novel SCCmec VI element harbouring fusC in an emerging Staphylococcus aureus strain from the Arabian Gulf region. PLoS ONE 2019, 14, e0223985. [Google Scholar] [CrossRef]
- EFSA, European Centre for Disease Prevention and Control. The European Union Summary Report on Antimicrobial Resistance in zoonotic and indicator bacteria from humans, animals and food in 2018/2019. EFSA J. 2021, 19, e06490. [Google Scholar] [CrossRef]
- Alzohairy, M.A. Colonization and antibiotic susceptibility pattern of methicillin resistance Staphylococcus aureus (MRSA) among farm animals in Saudi Arabia. Afr. J. Bacteriol. Res. 2011, 3, 63–68. [Google Scholar] [CrossRef]
- Bounar-Kechih, S.; Taha Hamdi, M.; Aggad, H.; Meguenni, N.; Cantekin, Z. Carriage Methicillin-Resistant Staphylococcus aureus in Poultry and Cattle in Northern Algeria. Vet. Med. Int. 2018, 2018, 4636121. [Google Scholar] [CrossRef] [PubMed]
- Algammal, A.M.; Enany, M.E.; El-Tarabili, R.M.; Ghobashy, M.O.I.; Helmy, Y.A. Prevalence, Antimicrobial Resistance Profiles, Virulence and Enterotoxins-Determinant Genes of MRSA Isolated from Subclinical Bovine Mastitis in Egypt. Pathogens 2020, 9, 362. [Google Scholar] [CrossRef]
- Klibi, A.; Jouini, A.; Gómez, P.; Slimene, K.; Ceballos, S.; Torres, C.; Maaroufi, A. Molecular Characterization and Clonal Diversity of Methicillin-Resistant and -Susceptible Staphylococcus aureus Isolates of Milk of Cows with Clinical Mastitis in Tunisia. Microb. Drug. Resist. 2018, 24, 1210–1216. [Google Scholar] [CrossRef] [PubMed]
- El-Ashker, M.; Gwida, M.; Monecke, S.; El-Gohary, F.; Ehricht, R.; Elsayed, M.; Akinduti, P.; El-Fateh, M.; Maurischat, S. Antimicrobial resistance pattern and virulence profile of S. aureus isolated from household cattle and buffalo with mastitis in Egypt. Vet. Microbiol. 2020, 240, 108535. [Google Scholar] [CrossRef]
- Obaidat, M.M.; Bani Salman, A.E.; Roess, A.A. High prevalence and antimicrobial resistance of mecA Staphylococcus aureus in dairy cattle, sheep, and goat bulk tank milk in Jordan. Trop. Anim. Health Prod. 2018, 50, 405–412. [Google Scholar] [CrossRef]
- Khudaier, B.Y.; Abbas, B.A.; Khudaier, A.M. Detection of Methicillin Resistant Staphylococcus aureus Isolated from Human and Animals in Basrah Province/Iraq. MRVSA2013 2013, 2, 12–21. [Google Scholar] [CrossRef]
- El-Ashker, M.; Gwida, M.; Tomaso, H.; Monecke, S.; Ehricht, R.; El-Gohary, F.; Hotzel, H. Staphylococci in cattle and buffaloes with mastitis in Dakahlia Governorate, Egypt. J. Dairy Sci. 2015, 98, 7450–7459. [Google Scholar] [CrossRef] [PubMed]
- Khemiri, M.; Abbassi, M.S.; Couto, N.; Mansouri, R.; Hammami, S.; Pomba, C. Genetic characterisation of Staphylococcus aureus isolated from milk and nasal samples of healthy cows in Tunisia: First report of ST97-t267-agrI-SCCmecV MRSA of bovine origin in Tunisia. J. Glob. Antimicrob. Resist. 2018, 14, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Agabou, A.; Ouchenane, Z.; Ngba Essebe, C.; Khemissi, S.; Chehboub, M.T.E.; Chehboub, I.B.; Sotto, A.; Dunyach-Remy, C.; Lavigne, J.P. Emergence of Nasal Carriage of ST80 and ST152 PVL+ Staphylococcus aureus Isolates from Livestock in Algeria. Toxins 2017, 9, 303. [Google Scholar] [CrossRef] [PubMed]
- Gharsa, H.; Ben Slama, K.; Lozano, C.; Gómez-Sanz, E.; Klibi, N.; Ben Sallem, R.; Gómez, P.; Zarazaga, M.; Boudabous, A.; Torres, C. Prevalence, antibiotic resistance, virulence traits and genetic lineages of Staphylococcus aureus in healthy sheep in Tunisia. Vet. Microbiol. 2012, 156, 367–373. [Google Scholar] [CrossRef]
- El-Deeb, W.; Fayez, M.; Elmoslemany, A.; Kandeel, M.; Zidan, K. Methicillin resistant Staphylococcus aureus among goat farms in Eastern province, Saudi Arabia: Prevalence and risk factors. Prev. Vet. Med. 2018, 156, 84–90. [Google Scholar] [CrossRef]
- Alghizzi, M.; Shami, A. The prevalence of Staphylococcus aureus and methicillin resistant Staphylococcus aureus in milk and dairy products in Riyadh, Saudi Arabia. Saudi J. Biol. Sci. 2021, 28, 7098–7104. [Google Scholar] [CrossRef]
- Benrabia, I.; Hamdi, T.M.; Shehata, A.A.; Neubauer, H.; Wareth, G. Methicillin-Resistant Staphylococcus qureus (MRSA) in Poultry Species in Algeria: Long-Term Study on Prevalence and Antimicrobial Resistance. Vet. Sci. 2020, 7, 54. [Google Scholar] [CrossRef]
- El-Adawy, H.; Ahmed, M.; Hotzel, H.; Monecke, S.; Schulz, J.; Hartung, J.; Ehricht, R.; Neubauer, H.; Hafez, H.M. Characterization of Methicillin-Resistant Staphylococcus aureus Isolated from Healthy Turkeys and Broilers Using DNA Microarrays. Front. Microbiol. 2016, 7, 2019. [Google Scholar] [CrossRef]
- Assafi, M.S.; Hado, H.A.; Abdulrahman, I.S. Detection of methicillin-resistant Staphylococcus aureus in broiler and broilers farm workers in Duhok, Iraq by using conventional and PCR techniques. Iraqi J. Vet. Sci. 2020, 34, 15–22. [Google Scholar] [CrossRef]
- Holmes, M.A.; Zadoks, R.N. Methicillin resistant S. aureus in human and bovine mastitis. J. Mammary Gland. Biol. Neoplasia 2011, 16, 373–382. [Google Scholar] [CrossRef]
- Cobirka, M.; Tancin, V.; Slama, P. Demiology and Classification of Mastitis. Animals 2020, 10, 2212. [Google Scholar] [CrossRef] [PubMed]
- Ruegg, P.L. Making Antibiotic Treatment Decisions for Clinical Mastitis. Vet. Clin. N. Am. Food Anim. Pract. 2018, 34, 413–425. [Google Scholar] [CrossRef] [PubMed]
- Juhász-Kaszanyitzky, E.; Jánosi, S.; Somogyi, P.; Dán, A.; van der Graaf-van Bloois, L.; van Duijkeren, E.; Wagenaar, J.A. MRSA transmission between cows and humans. Emerg. Infect. Dis. 2007, 13, 630–632. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H. Methicillin (Oxacillin)-resistant Staphylococcus aureus strains isolated from major food animals and their potential transmission to humans. Appl. Environ. Microbiol. 2003, 69, 6489–6494. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Moein, K.A.; Zaher, H.M. Occurrence of multidrug-resistant methicillin-resistant Staphylococcus aureus among healthy farm animals: A public health concern. Int. J. Vet. Sci. Med. 2019, 7, 55–60. [Google Scholar] [CrossRef]
- Dweba, C.C.; Zishiri, O.T.; El Zowalaty, M.E. Methicillin-resistant Staphylococcus aureus: Livestock-associated, antimicrobial, and heavy metal resistance. Infect. Drug Resist. 2018, 11, 2497–2509. [Google Scholar] [CrossRef]
- Battisti, A.; Franco, A.; Merialdi, G.; Hasman, H.; Iurescia, M.; Lorenzetti, R.; Feltrin, F.; Zini, M.; Aarestrup, F.M. Heterogeneity among methicillin-resistant Staphylococcus aureus from Italian pig finishing holdings. Vet. Microbiol. 2010, 142, 361–366. [Google Scholar] [CrossRef]
- Gómez-Sanz, E.; Torres, C.; Lozano, C.; Fernández-Pérez, R.; Aspiroz, C.; Ruiz-Larrea, F.; Zarazaga, M. Detection, molecular characterization, and clonal diversity of methicillin-resistant Staphylococcus aureus CC398 and CC97 in Spanish slaughter pigs of different age groups. Foodborne Pathog. Dis. 2010, 7, 1269–1277. [Google Scholar] [CrossRef]
- Buyukcangaz, E.; Velasco, V.; Sherwood, J.S.; Stepan, R.M.; Koslofsky, R.J.; Logue, C.M. Molecular typing of Staphylococcus aureus and methicillin-resistant S. aureus (MRSA) isolated from animals and retail meat in North Dakota, United States. Foodborne Pathog. Dis. 2013, 10, 608–617. [Google Scholar] [CrossRef]
- Earls, M.R.; Steinig, E.J.; Monecke, S.; Castruita, J.A.S.; Simbeck, A.; Schneider-Brachert, W.; Vremerǎ, T.; Dorneanu, O.S.; Loncaric, I.; Bes, M.; et al. Exploring the evolution and epidemiology of European CC1-MRSA-IV: Tracking a multidrug-resistant community-associated meticillin-resistant Staphylococcus aureus clone. Microb. Genom. 2021, 7, 000601. [Google Scholar] [CrossRef]
- Silva, V.; Sousa, T.; Gómez, P.; Sabença, C.; Vieira-Pinto, M.; Capita, R.; Alonso-Calleja, C.; Torres, C.; Capelo, J.L.; Igrejas, G.; et al. Livestock-Associated Methicillin-Resistant Staphylococcus aureus (MRSA) in Purulent Subcutaneous Lesions of Farm Rabbits. Foods 2020, 9, 439. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, G.L.; Murchan, S.; Gil-Setas, A.; Aucken, H.M. Identification and characterization of phage variants of a strain of epidemic methicillin-resistant Staphylococcus aureus (EMRSA-15). J. Clin. Microbiol. 2001, 39, 1540–1548. [Google Scholar] [CrossRef] [PubMed]
- Spoor, L.E.; McAdam, P.R.; Weinert, L.A.; Rambaut, A.; Hasman, H.; Aarestrup, F.M.; Kearns, A.M.; Larsen, A.R.; Skov, R.L.; Fitzgerald, J.R. Livestock origin for a human pandemic clone of community-associated methicillin-resistant Staphylococcus aureus. mBio 2013, 4, e00356-13. [Google Scholar] [CrossRef] [PubMed]
- Cristina, M. Building Sustainable Agriculture for Food Security in the Euro-Mediterranean Area: Challenges and Policy Options edited by Maria Cristina Paciello. In Books & Reports; Policy Center for the New South: Rabat, Morocco, 2018; Volume 3, pp. 23–26. ISBN 978-88-6812-508-0. [Google Scholar]
- Statista. MENA: Per Capita Meat Consumption by Country. 2014. Available online: https://www.statista.com/statistics/730843/mena-per-capita-meat-consumption-by-country/ (accessed on 13 April 2022).
- Ouchene-Khelifi, N.A.; Lafri, M.; Pompanon, F.; Ouhrouch, A.; Ouchene, N.; Blanquet, V.; Lenstra, J.A.; Benjelloun, B.; Da Silva, A. Genetic homogeneity of North-African goats. PLoS ONE 2018, 13, e0202196. [Google Scholar] [CrossRef] [PubMed]
- Hilali, M.; El-Mayda, E.; Rischkowsky, B. Characteristics and utilization of sheep and goat milk in the Middle East. Small Rumin. Res. 2011, 101, 92–101. [Google Scholar] [CrossRef]
- Liu, M.; Cheng, J.; Chen, Y.; Yang, L.; Raza, S.H.A.; Huang, Y.; Lei, C.; Liu, G.E.; Lan, X.; Chen, H. Distribution of DGAT1 copy number variation in Chinese goats and its associations with milk production traits. Anim. Biotechnol. 2021, 122, 1–6. [Google Scholar] [CrossRef]
- Miller, B.A.; Lu, C.D. Current status of global dairy goat production: An overview. Asian-Australas. J. Anim. Sci. 2019, 32, 1219–1232. [Google Scholar] [CrossRef]
- Rees, C.; Mullumby, J. Trends in Australian meat consumption. Agric. Commod. 2017, 7, 82–85. Available online: https://search.informit.org/doi/10.3316/informit.224110136329092 (accessed on 23 April 2022).
- Webb, E.C. Goat meat production, composition, and quality. Anim. Front. 2014, 4, 33–37. [Google Scholar] [CrossRef]
- Vasileiou, N.G.C.; Chatzopoulos, D.C.; Sarrou, S.; Fragkou, I.A.; Katsafadou, A.I.; Mavrogianni, V.S.; Petinaki, E.; Fthenakis, G.C. Role of staphylococci in mastitis in sheep. J. Dairy Res. 2019, 86, 254–266. [Google Scholar] [CrossRef]
- Alioua, M.A.; Labid, A.; Amoura, K.; Bertine, M.; Gacemi-Kirane, D.; Dekhil, M. Emergence of the European ST80 clone of community-associated methicillin-resistant Staphylococcus aureus as a cause of healthcare-associated infections in Eastern Algeria. Med. Mal. Infect. 2014, 44, 180–183. [Google Scholar] [CrossRef] [PubMed]
- Ben Slama, K.; Gharsa, H.; Klibi, N.; Jouini, A.; Lozano, C.; Gómez-Sanz, E.; Zarazaga, M.; Boudabous, A.; Torres, C. Nasal carriage of Staphylococcus aureus in healthy humans with different levels of contact with animals in Tunisia: Genetic lineages, methicillin resistance, and virulence factors. Eur. J. Clin. Microbiol. Infect. Dis. 2011, 30, 499–508. [Google Scholar] [CrossRef] [PubMed]
- Udo, E.E.; Sarkhoo, E. The dissemination of ST80-SCCmec-IV community-associated methicillin resistant Staphylococcus aureus clone in Kuwait hospitals. Ann. Clin. Microbiol. Antimicrob. 2010, 9, 31. [Google Scholar] [CrossRef]
- Dastmalchi Saei, H.; Panahi, M. Genotyping and antimicrobial resistance of Staphylococcus aureus isolates from dairy ruminants: Differences in the distribution of clonal types between cattle and small ruminants. Arch. Microbiol. 2020, 202, 115–125. [Google Scholar] [CrossRef]
- De Almeida, L.M.; de Almeida, M.Z.; de Mendonça, C.L.; Mamizuka, E.M. Novel sequence types (STs) of Staphylococcus aureus isolates causing clinical and subclinical mastitis in flocks of sheep in the northeast of Brazil. J. Dairy Res. 2011, 78, 373–378. [Google Scholar] [CrossRef] [PubMed]
- Azara, E.; Piras, M.G.; Parisi, A.; Tola, S. Antimicrobial susceptibility and genotyping of Staphylococcus aureus isolates collected between 1986 and 2015 from ovine mastitis. Vet. Microbiol. 2017, 205, 53–56. [Google Scholar] [CrossRef] [PubMed]
- Murray, S.; Pascoe, B.; Méric, G.; Mageiros, L.; Yahara, K.; Hitchings, M.D.; Friedmann, Y.; Wilkinson, T.S.; Gormley, F.J.; Mack, D.; et al. Recombination-Mediated Host Adaptation by Avian Staphylococcus aureus. Genome Biol. Evol. 2017, 9, 830–842. [Google Scholar] [CrossRef]
- Nemati, M.; Hermans, K.; Lipinska, U.; Denis, O.; Deplano, A.; Struelens, M.; Devriese, L.A.; Pasmans, F.; Haesebrouck, F. Antimicrobial resistance of old and recent Staphylococcus aureus isolates from poultry: First detection of livestock-associated methicillin-resistant strain ST398. Antimicrob. Agents Chemother. 2008, 52, 3817–3819. [Google Scholar] [CrossRef]
- Zaheer, Z.; Rahman, S.U.; Zaheer, I.; Abbas, G.; Younas, T. Methicillin-resistant Staphylococcus aureus in poultry-an emerging concern related to future epidemic. Matrix Sci. Medica 2017, 1, 15–18. [Google Scholar] [CrossRef]
- Peeters, L.E.; Argudín, M.A.; Azadikhah, S.; Butaye, P. Antimicrobial resistance and population structure of Staphylococcus aureus recovered from pigs farms. Vet. Microbiol. 2015, 180, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Crombé, F.; Argudín, M.A.; Vanderhaeghen, W.; Hermans, K.; Haesebrouck, F.; Butaye, P. Transmission Dynamics of Methicillin-Resistant Staphylococcus aureus in Pigs. Front. Microbiol. 2013, 4, 57. [Google Scholar] [CrossRef]
- Nemeghaire, S.; Roelandt, S.; Argudín, M.A.; Haesebrouck, F.; Butaye, P. Characterization of methicillin-resistant Staphylococcus aureus from healthy carrier chickens. Avian Pathol. 2013, 42, 342–346. [Google Scholar] [CrossRef] [PubMed]
- Fessler, A.T.; Kadlec, K.; Hassel, M.; Hauschild, T.; Eidam, C.; Ehricht, R.; Monecke, S.; Schwarz, S. Characterization of methicillin-resistant Staphylococcus aureus isolates from food and food products of poultry origin in Germany. Appl. Environ. Microbiol. 2011, 77, 7151–7157. [Google Scholar] [CrossRef] [PubMed]
- Khanna, T.; Friendship, R.; Dewey, C.; Weese, J.S. Methicillin resistant Staphylococcus aureus colonization in pigs and pig farmers. Vet. Microbiol. 2008, 128, 298–303. [Google Scholar] [CrossRef]
- Lowder, B.V.; Guinane, C.; Ben Zakour, N.L.; Weinert, L.A.; Conway-Morris, A.; Cartwright, R.A.; Simpson, A.J.; Rambaut, A.; Nübel, U.; Fitzgerald, J.R. Recent human-to-poultry host jump, adaptation, and pandemic spread of Staphylococcus aureus. Proc. Natl. Acad. Sci. USA 2009, 106, 19545–19550. [Google Scholar] [CrossRef]
- Zhu, S.; Zimmerman, D.; Deem, S.L. A Review of Zoonotic Pathogens of Dromedary Camels. Ecohealth 2019, 16, 356–377. [Google Scholar] [CrossRef]
- Abdallah, H.R.; Faye, B. Phenotypic classification of Saudi Arabian camel (Camelus dromedarius) by their body measurements. Emir. J. Food Agric. 2012, 24, 272–280. [Google Scholar]
- Khalaf, S. Poetics and Politics of Newly Invented Traditions in the Gulf: Camel Racing in the United Arab Emirates. Ethnology 2000, 39, 243–261. [Google Scholar] [CrossRef]
- Alhadrami, G.A.; Faye, B. Animals that produce dairy foods: Camel. In Reference Module in Food Science; Elsevier: Amsterdam, The Netherlands, 2016. [Google Scholar] [CrossRef]
- Singh, R.; Mal, G.; Kumar, D. Camel Milk: An Important Natural Adjuvant. Agric. Res. 2017, 6, 327–340. [Google Scholar] [CrossRef]
- Harrak, M.E.; Faye, B.; Bengoumi, M. Main Pathologies of Camels, Breeding of Camels, Constraints, Benefits and Perspectives. 2011. Available online: https://www.oie.int/doc/ged/D12812.PDF (accessed on 20 April 2022).
- Alagaili, A.N.; Briese, T.; Mishra, N.; Kapoor, V.; Sameroff, S.C.; Burbelo, P.D.; de Wit, E.; Munster, V.J.; Hensley, L.E.; Zalmout, I.S.; et al. Middle East respiratory syndrome coronavirus infection in dromedary camels in Saudi Arabia. mBio 2014, 5, e00884-14. [Google Scholar] [CrossRef] [PubMed]
- Babelhadj, B.; Di Bari, M.A.; Pirisinu, L.; Chiappini, B.; Gaouar, S.B.S.; Riccardi, G.; Marcon, S.; Agrimi, U.; Nonno, R.; Vaccari, G. Prion Disease in Dromedary Camels, Algeria. Emerg. Infect. Dis. 2018, 24, 1029–1036. [Google Scholar] [CrossRef] [PubMed]
- Yehia, H.M.; Al-Masoud, A.H.; Alarjani, K.M.; Alamri, M.S. Prevalence of methicillin-resistant (mecA gene) and heat-resistant Staphylococcus aureus strains in pasteurized camel milk. J. Dairy Sci. 2020, 103, 5947–5963. [Google Scholar] [CrossRef] [PubMed]
- Aljahani, A.H.; Alarjani, K.M.; Hassan, Z.K.; Elkhadragy, M.F.; Ismail, E.A.; Al-Masoud, A.H.; Yehia, H.M. Molecular detection of methicillin heat-resistant Staphylococcus aureus strains in pasteurized camel milk in Saudi Arabia. Biosci. Rep. 2020, 40, BSR20193470. [Google Scholar] [CrossRef]
- Raji, M.A.; Garaween, G.; Ehricht, R.; Monecke, S.; Shibl, A.M.; Senok, A. Genetic Characterization of Staphylococcus aureus Isolated from Retail Meat in Riyadh, Saudi Arabia. Front. Microbiol. 2016, 7, 911. [Google Scholar] [CrossRef]
- Tabaja, H.; Hindy, J.R.; Kanj, S.S. Epidemiology of Methicillin-Resistant Staphylococcus aureus in Arab Countries of the Middle East and North African (MENA) Region. Mediterr. J. Hematol. Infect. Dis. 2021, 13, e2021050. [Google Scholar] [CrossRef]
- Pletinckx, L.J.; Verhegghe, M.; Crombé, F.; Dewulf, J.; De Bleecker, Y.; Rasschaert, G.; Butaye, P.; Goddeeris, B.M.; De Man, I. Evidence of possible methicillin-resistant Staphylococcus aureus ST398 spread between pigs and other animals and people residing on the same farm. Prev. Vet. Med. 2013, 109, 293–303. [Google Scholar] [CrossRef]
- Abdullahi, I.N.; Fernández-Fernández, R.; Juárez-Fernández, G.; Martínez-Álvarez, S.; Eguizábal, P.; Zarazaga, M.; Lozano, C.; Torres, C. Wild Animals Are Reservoirs and Sentinels of Staphylococcus aureus and MRSA Clones: A Problem with “One Health” Concern. Antibiotics 2021, 10, 1556. [Google Scholar] [CrossRef]
- Van Duijkeren, E.; Wolfhagen, M.J.; Box, A.T.; Heck, M.E.; Wannet, W.J.; Fluit, A.C. Human-to-dog transmission of methicillin-resistant Staphylococcus aureus. Emerg. Infect. Dis. 2004, 10, 2235–2237. [Google Scholar] [CrossRef]
- Baptiste, K.E.; Williams, K.; Willams, N.J.; Wattret, A.; Clegg, P.D.; Dawson, S.; Corkill, J.E.; O’Neill, T.; Hart, C.A. Methicillin-resistant staphylococci in companion animals. Emerg. Infect. Dis. 2005, 11, 1942–1944. [Google Scholar] [CrossRef]
- Tarazi, Y.H.; Almajali, A.M.; Ababneh, M.M.K.; Ahmed, H.S.; Jaran, A.S. Molecular study on methicillin-resistant Staphylococcus aureus strains isolated from dogs and associated personnel in Jordan. Asian Pac. J. Trop. Biomed. 2015, 5, 902–908. [Google Scholar] [CrossRef]
- Elnageh, H.R.; Hiblu, M.A.; Abbassi, M.S.; Abouzeed, Y.M.; Ahmed, M.O. Prevalence and antimicrobial resistance of Staphylococcus species isolated from cats and dogs. Open. Vet. J. 2021, 10, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Elmoslemany, A.; Elsohaby, I.; Alorabi, M.; Alkafafy, M.; Al-Marri, T.; Aldoweriej, A.; Alaql, F.A.; Almubarak, A.; Fayez, M. Diversity and Risk Factors Associated with Multidrug and Methicillin-Resistant Staphylococci Isolated from Cats Admitted to a Veterinary Clinic in Eastern Province, Saudi Arabia. Antibiotics 2021, 10, 367. [Google Scholar] [CrossRef] [PubMed]
- Mairi, A.; Touati, A.; Pantel, A.; Yahiaoui Martinez, A.; Ahmim, M.; Sotto, A.; Dunyach-Remy, C.; Lavigne, J.-P. First Report of CC5-MRSA-IV-SCCfus “Maltese Clone” in Bat Guano. Microorganisms 2021, 9, 2264. [Google Scholar] [CrossRef]
- Da Silva, A.C.; Rodrigues, M.X.; Silva, N.C.C. Methicillin-resistant Staphylococcus aureus in food and the prevalence in Brazil: A review. Braz. J. Microbiol. 2020, 51, 347–356. [Google Scholar] [CrossRef] [PubMed]
- Kroning, I.S.; Iglesias, M.A.; Sehn, C.P.; Valente Gandra, T.K.; Mata, M.M.; da Silva, W.P. Staphylococcus aureus isolated from handmade sweets: Biofilm formation, enterotoxigenicity and antimicrobial resistance. Food Microbiol. 2016, 58, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Duan, N.; Gu, H.; Hao, L.; Ye, H.; Gong, W.; Wang, Z. A Review of the Methods for Detection of Staphylococcus aureus Enterotoxins. Toxins 2016, 8, 176. [Google Scholar] [CrossRef]
- Ono, H.K.; Omoe, K.; Imanishi, K.; Iwakabe, Y.; Hu, D.L.; Kato, H.; Saito, N.; Nakane, A.; Uchiyama, T.; Shinagawa, K. Identification and characterization of two novel staphylococcal enterotoxins, types S and T. Infect. Immun. 2008, 76, 4999–5005. [Google Scholar] [CrossRef]
- Mead, P.S.; Slutsker, L.; Dietz, V.; McCaig, L.F.; Bresee, J.S.; Shapiro, C. Food-Related Illness and Death in the United States. Emerg. Infect. Dis. 1999, 5, 607–625. [Google Scholar] [CrossRef]
- Le Loir, Y.; Baron, F.; Gautier, M. Staphylococcus aureus and food poisoning. Genet. Mol. Res. 2003, 2, 63–76. [Google Scholar]
- Kluytmans, J.A.; Wertheim, H.F. Nasal carriage of Staphylococcus aureus and prevention of nosocomial infections. Infection 2005, 33, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Argudín, M.Á.; Mendoza, M.C.; Rodicio, M.R. Food poisoning and Staphylococcus aureus enterotoxins. Toxins 2010, 2, 1751–1773. [Google Scholar] [CrossRef] [PubMed]
- Jones, T.F.; Kellum, M.E.; Porter, S.S.; Bell, M.; Schaffner, W. An outbreak of community-acquired foodborne illness caused by methicillin-resistant Staphylococcus aureus. Emerg. Infect. Dis. 2002, 8, 82–84. [Google Scholar] [CrossRef]
- Titouche, Y.; Hakem, A.; Houali, K.; Meheut, T.; Vingadassalon, N.; Ruiz-Ripa, L.; Salmi, D.; Chergui, A.; Chenouf, N.; Hennekinne, J.A.; et al. Emergence of methicillin-resistant Staphylococcus aureus (MRSA) ST8 in raw milk and traditional dairy products in the Tizi Ouzou area of Algeria. J. Dairy Sci. 2019, 102, 6876–6884. [Google Scholar] [CrossRef]
- Abolghait, S.K.; Fathi, A.G.; Youssef, F.M.; Algammal, A.M. Methicillin-resistant Staphylococcus aureus (MRSA) isolated from chicken meat and giblets often produces staphylococcal enterotoxin B (SEB) in non-refrigerated raw chicken livers. Int. J. Food Microbiol. 2020, 328, 108669. [Google Scholar] [CrossRef]
- Al-Ashmawy, M.A.; Sallam, K.I.; Abd-Elghany, S.M.; Elhadidy, M.; Tamura, T. Prevalence, Molecular Characterization, and Antimicrobial Susceptibility of Methicillin-Resistant Staphylococcus aureus Isolated from Milk and Dairy Products. Foodborne Pathog. Dis. 2016, 13, 156–162. [Google Scholar] [CrossRef]
- Kanaan, M.H.G. Antibacterial effect of ozonated water against methicillin-resistant Staphylococcus aureus contaminating chicken meat in Wasit Province, Iraq. Vet. World 2018, 11, 1445–1453. [Google Scholar] [CrossRef]
- Naas, H.T.; Edarhoby, R.A.; Garbaj, A.M.; Azwai, S.M.; Abolghait, S.K.; Gammoudi, F.T.; Moawad, A.A.; Barbieri, I.; Eldaghayes, I.M. Occurrence, characterization, and antibiogram of Staphylococcus aureus in meat, meat products, and some seafood from Libyan retail markets. Vet. World 2019, 12, 925–931. [Google Scholar] [CrossRef]
- Iyer, A.; Kumosani, T.; Azhar, E.; Barbour, E.; Harakeh, S. High incidence rate of methicillin-resistant Staphylococcus aureus (MRSA) among healthcare workers in Saudi Arabia. J. Infect. Dev. Ctries. 2014, 8, 372–378. [Google Scholar] [CrossRef]
- Chairat, S.; Gharsa, H.; Lozano, C.; Gómez-Sanz, E.; Gómez, P.; Zarazaga, M.; Boudabous, A.; Torres, C.; Ben Slama, K. Characterization of Staphylococcus aureus from Raw Meat Samples in Tunisia: Detection of Clonal Lineage ST398 from the African Continent. Foodborne Pathog. Dis. 2015, 12, 686–692. [Google Scholar] [CrossRef]
- Mahros, M.A.; Abd-Elghany, S.M.; Sallam, K.I. Multidrug-, methicillin-, and vancomycin-resistant Staphylococcus aureus isolated from ready-to-eat meat sandwiches: An ongoing food and public health concern. Int. J. Food Microbiol. 2021, 346, 109165. [Google Scholar] [CrossRef] [PubMed]
- Benjelloun Touimi, G.; Bennani, L.; Berrada, S.; Moussa, B.; Bennani, B. Prevalence and antibiotic resistance profiles of Staphylococcus sp. isolated from food, food contact surfaces and food handlers in a Moroccan hospital kitchen. Lett. Appl. Microbiol. 2020, 70, 241–251. [Google Scholar] [CrossRef] [PubMed]
- Mekhloufi, O.A.; Chieffi, D.; Hammoudi, A.; Bensefia, S.A.; Fanelli, F.; Fusco, V. Prevalence, Enterotoxigenic Potential and Antimicrobial Resistance of Staphylococcus aureus and Methicillin-Resistant Staphylococcus aureus (MRSA) Isolated from Algerian Ready to Eat Foods. Toxins 2021, 13, 835. [Google Scholar] [CrossRef] [PubMed]
- Osman, K.M.; Amer, A.M.; Badr, J.M.; Helmy, N.M.; Elhelw, R.A.; Orabi, A.; Bakry, M.; Saad, A.S. Antimicrobial Resistance, Biofilm Formation and mecA Characterization of Methicillin-Susceptible S. aureus and Non-S. aureus of Beef Meat Origin in Egypt. Front. Microbiol. 2016, 7, 222. [Google Scholar] [CrossRef]
- Osman, K.M.; Pires, Á.D.S.; Franco, O.L.; Orabi, A.; Hanafy, M.H.; Marzouk, E.; Hussien, H.; Alzaben, F.A.; Almuzaini, A.M.; Elbehiry, A. Enterotoxigenicity and Antibiotic Resistance of Coagulase-Negative Staphylococci Isolated from Raw Buffalo and Cow Milk. Microb. Drug Resist. 2020, 26, 520–530. [Google Scholar] [CrossRef]
- Quddoumi, S.S.; Bdour, S.M.; Mahasneh, A.M. Isolation and characterization of methicillin-resistant Staphylococcus aureus from livestock and poultry meat. Ann. Microbiol. 2006, 56, 155–161. [Google Scholar] [CrossRef]
- Haran, K.P.; Godden, S.M.; Boxrud, D.; Jawahir, S.; Bender, J.B.; Sreevatsan, S. Prevalence and characterization of Staphylococcus aureus, including methicillin-resistant Staphylococcus aureus, isolated from bulk tank milk from Minnesota dairy farms. J. Clin. Microbiol. 2012, 50, 688–695. [Google Scholar] [CrossRef]
- Chenouf, N.S.; Mama, O.M.; Messaï, C.R.; Ruiz-Ripa, L.; Fernández-Fernández, R.; Carvalho, I.; Zitouni, A.; Hakem, A.; Torres, C. Detection of methicillin-resistant coagulase-negative staphylococci and PVL/mecA genes in cefoxitin-susceptible Staphylococcus aureus (t044/ST80) from unpasteurized milk sold in stores in Djelfa, Algeria. J. Dairy Sci. 2021, 104, 2684–2692. [Google Scholar] [CrossRef]
- Bendahou, A.; Lebbadi, M.; Ennanei, L.; Essadqui, F.Z.; Abid, M. Characterization of Staphylococcus species isolated from raw milk and milk products (lben and jben) in North Morocco. J. Infect. Dev. Ctries. 2008, 2, 218–225. [Google Scholar] [CrossRef]
- Bendahou, A.; Abid, M.; Bouteldoun, N.; Catelejine, D.; Lebbadi, M. Enterotoxigenic coagulase positive Staphylococcus in milk and milk products, lben and jben, in northern Morocco. J. Infect. Dev. Ctries. 2009, 3, 169–176. [Google Scholar] [CrossRef]
- Herrera, F.C.; García-López, M.L.; Santos, J.A. Short communication: Characterization of methicillin-resistant Staphylococcus aureus isolated from raw milk fresh cheese in Colombia. J. Dairy Sci. 2016, 99, 7872–7876. [Google Scholar] [CrossRef] [PubMed]
- Vandendriessche, S.; Vanderhaeghen, W.; Larsen, J.; de Mendonça, R.; Hallin, M.; Butaye, P.; Hermans, K.; Haesebrouck, F.; Denis, O. High genetic diversity of methicillin-susceptible Staphylococcus aureus (MSSA) from humans and animals on livestock farms and presence of SCCmec remnant DNA in MSSA CC398. J. Antimicrob. Chemother. 2014, 69, 355–362. [Google Scholar] [CrossRef][Green Version]
- Abdulgader, S.; Shittu, A.O.; Nicol, M.P.; Kaba, M. Molecular epidemiology of Methicillin-resistant Staphylococcus aureus in Africa: A systematic review. Front. Microbiol. 2015, 6, 348. [Google Scholar] [CrossRef]
- Stefani, S.; Varaldo, P.E. Epidemiology of methicillin-resistant staphylococci in Europe. Clin. Microbiol. Infect. 2003, 9, 1179–1186. [Google Scholar] [CrossRef] [PubMed]
- Argudín, M.A.; Vanderhaeghen, W.; Vandendriessche, S.; Vandecandelaere, I.; André, F.X.; Denis, O.; Coenye, T.; Butaye, P. Antimicrobial resistance and population structure of Staphylococcus epidermidis recovered from animals and humans. Vet. Microbiol. 2015, 178, 105–113. [Google Scholar] [CrossRef]
- Van Duijkeren, E.; Catry, B.; Greko, C.; Moreno, M.A.; Pomba, M.C.; Pyörälä, S.; Ruzauskas, M.; Sanders, P.; Threlfall, E.J.; Torren-Edo, J.; et al. Review on methicillin-resistant Staphylococcus pseudintermedius. J. Antimicrob. Chemother. 2011, 66, 2705–2714. [Google Scholar] [CrossRef]
- Kim, S.G.; Giri, S.S.; Yun, S.; Kim, S.W.; Han, S.J.; Kwon, J.; Oh, W.T.; Lee, S.B.; Park, Y.H.; Park, S.C. Two Novel Bacteriophages Control Multidrug- and Methicillin-Resistant Staphylococcus pseudintermedius Biofilm. Front. Med. 2021, 8, 524059. [Google Scholar] [CrossRef]
- Bloemendaal, A.L.; Brouwer, E.C.; Fluit, A.C. Methicillin resistance transfer from Staphylocccus epidermidis to methicillin-susceptible Staphylococcus aureus in a patient during antibiotic therapy. PLoS ONE 2010, 5, e11841. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Moein, K.A.; Zaher, H.M. The Nasal Carriage of Coagulase-Negative Staphylococci Among Animals and Its Public Health Implication. Vector-Borne Zoonotic Dis. 2020, 20, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Osman, K.; Alvarez-Ordóñez, A.; Ruiz, L.; Badr, J.; ElHofy, F.; Al-Maary, K.S.; Moussa, I.M.I.; Hessain, A.M.; Orabi, A.; Saad, A.; et al. Antimicrobial resistance and virulence characterization of Staphylococcus aureus and coagulase-negative staphylococci from imported beef meat. Ann. Clin. Microbiol. Antimicrob. 2017, 16, 35. [Google Scholar] [CrossRef]
- El Zowalaty, M.E.; Järhult, J.D. From SARS to COVID-19: A previously unknown SARS-related coronavirus (SARS-CoV-2) of pandemic potential infecting humans—Call for a One Health approach. One Health 2020, 9, 100124. [Google Scholar] [CrossRef] [PubMed]
- Antimicrobial Resistance. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 1 May 2022).
- Collignon, P.J.; McEwen, S.A. One Health-Its Importance in Helping to Better Control Antimicrobial Resistance. Trop. Med. Infect. Dis. 2019, 4, 22. [Google Scholar] [CrossRef] [PubMed]
- What Is One Health? One Health Commission. Available online: https://www.onehealthcommission.org/en/why_one_health/what_is_one_health/ (accessed on 1 May 2022).
- Feil, E.J.; Cooper, J.E.; Grundmann, H.; Robinson, D.A.; Enright, M.C.; Berendt, T.; Peacock, S.J.; Smith, J.M.; Murphy, M.; Spratt, B.G.; et al. How clonal is Staphylococcus aureus? J. Bacteriol. 2003, 185, 3307–3316. [Google Scholar] [CrossRef] [PubMed]
- Weinert, L.A.; Welch, J.J.; Suchard, M.A.; Lemey, P.; Rambaut, A.; Fitzgerald, J.R. Molecular dating of human-to-bovid host jumps by Staphylococcus aureus reveals an association with the spread of domestication. Biol. Lett. 2012, 8, 829–832. [Google Scholar] [CrossRef]
| Staphylococcal Species and Subspecies | Old Taxonomic Assignments | Current Taxonomic Reassignment | Coagulase |
|---|---|---|---|
| S. aureus subsp. anaerobius 1 | S. aureus | S. aureus subsp. anaerobius later heterotrophic synonym of S. aureus subsp. aureus. | + |
| S. carnosus subsp. utilis 2 | S. carnosus | S. carnosus subsp. utilis is later heterotypic synonym of S. carnosus subsp. carnosus 2 | - |
| S. cohnii subsp. urealyticus 3 | S. cohnii | S. urealyticus sp. nov. | - |
| S. cohnii subsp. cohnii | S. cohnii | S. urealyticus sp. nov. | - |
| S. petrasii subsp. Jettensis | S. jettensis | S. petrasii subsp. jettensis is a later heterotypic synonym of S. petrasii subsp. petrasii. | - |
| S. fleurettii | S. sciuri | Mammaliicoccus fleurettii4 | - |
| S. lentus | S. sciuri | Mammaliicoccus lentus4 | - |
| S. stepanovicii | S. sciuri | Mammaliicoccus stepanovicii4 | - |
| S. sciuri | S. sciuri | Mammaliicoccus sciuri4 | - |
| S. vitulinus | S. sciuri | Mammaliicoccus vitulinus4 | - |
| S. schleiferi subsp. coagulans 5 | S. schleiferi | S. coagulans sp. nov. | - |
| S. succinus subsp. casei 6 | S. succinus | S. casei sp. nov. | - |
| S. petrasii subsp. pragensis 7 | S. petrasii | S. pragensis sp. nov. | - |
| S. petrasii subsp. croceilyticus 8 | S. petrasii | S. croceilyticus sp. nov. | - |
| Animals | Healthy/Sick | Samples | Prevalence of MRSA | Lineages of MRSA | Country | Reference |
|---|---|---|---|---|---|---|
| Cattle | Healthy | Nasal swabs | 15.5% | N/D 1 | Saudi Arabia | [52] |
| Healthy | Nasal swabs | 31% | N/D | Algeria | [53] | |
| Sick, mastitis | Milk samples | 35.7% | N/D | Egypt | [54] | |
| Sick, mastitis | Milk samples | 3.60% | ST4114-t10381, ST4120-t267 | Tunisia | [55] | |
| Sick, mastitis | Milk samples | 28.6% | CC1, CC5, CC45 | Egypt | [56] | |
| Healthy | Milk samples | 31.8% | N/D | Jordan | [57] | |
| Healthy | Nasal swabs | 40% | N/D | Iraq | [58] | |
| Sick, mastitis | Milk samples | 24.5% | CC5, CC22, CC88 | Egypt | [59] | |
| Healthy | Nasal swabs, milk samples | 3.7% | ST97-t267-agrI-SCCmecV | Tunisia | [60] | |
| Sheep/goats | Healthy | Nasal swabs | 9.3% | CC80-ST80 | Algeria | [61] |
| Healthy | Nasal swabs | 3% | CC80-ST153-t044 | Tunisia | [62] | |
| Healthy | Milk samples | 29.8% sheep/11.5% goat | N/D | Jordan | [57] | |
| Healthy | Nasal swabs | 28.9% | N/D | Saudi Arabia | [52] | |
| Healthy and Sick | Nasal swabs | 2% (goats) | N/D | Saudi Arabia | [63] | |
| Healthy | Milk samples | 17.14% | N/D | Saudi Arabia | [64] | |
| Poultry | Healthy | Nasal swabs | 30% | N/D | Algeria | [65] |
| Healthy | swabs | 27% | CC398; CC5 | Egypt | [66] | |
| Healthy | Cloacal swab | 27.3% | N/D | Iraq | [67] | |
| Healthy | Nasal swabs | Layers: 57%, broilers: 50% | N/D | Algeria | [53] | |
| Camels | Healthy | Nasal swabs | 4.4% | CC80 | Algeria | [61] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Belhout, C.; Elgroud, R.; Butaye, P. Methicillin-Resistant Staphylococcus aureus (MRSA) and Other Methicillin-Resistant Staphylococci and Mammaliicoccus (MRNaS) Associated with Animals and Food Products in Arab Countries: A Review. Vet. Sci. 2022, 9, 317. https://doi.org/10.3390/vetsci9070317
Belhout C, Elgroud R, Butaye P. Methicillin-Resistant Staphylococcus aureus (MRSA) and Other Methicillin-Resistant Staphylococci and Mammaliicoccus (MRNaS) Associated with Animals and Food Products in Arab Countries: A Review. Veterinary Sciences. 2022; 9(7):317. https://doi.org/10.3390/vetsci9070317
Chicago/Turabian StyleBelhout, Chahrazed, Rachid Elgroud, and Patrick Butaye. 2022. "Methicillin-Resistant Staphylococcus aureus (MRSA) and Other Methicillin-Resistant Staphylococci and Mammaliicoccus (MRNaS) Associated with Animals and Food Products in Arab Countries: A Review" Veterinary Sciences 9, no. 7: 317. https://doi.org/10.3390/vetsci9070317
APA StyleBelhout, C., Elgroud, R., & Butaye, P. (2022). Methicillin-Resistant Staphylococcus aureus (MRSA) and Other Methicillin-Resistant Staphylococci and Mammaliicoccus (MRNaS) Associated with Animals and Food Products in Arab Countries: A Review. Veterinary Sciences, 9(7), 317. https://doi.org/10.3390/vetsci9070317







