The Flexion Relaxation Phenomenon in Patients with Radiculopathy and Low Back Pain: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Subjective Measures Using Questionnaires (LBP and LBPR Groups)
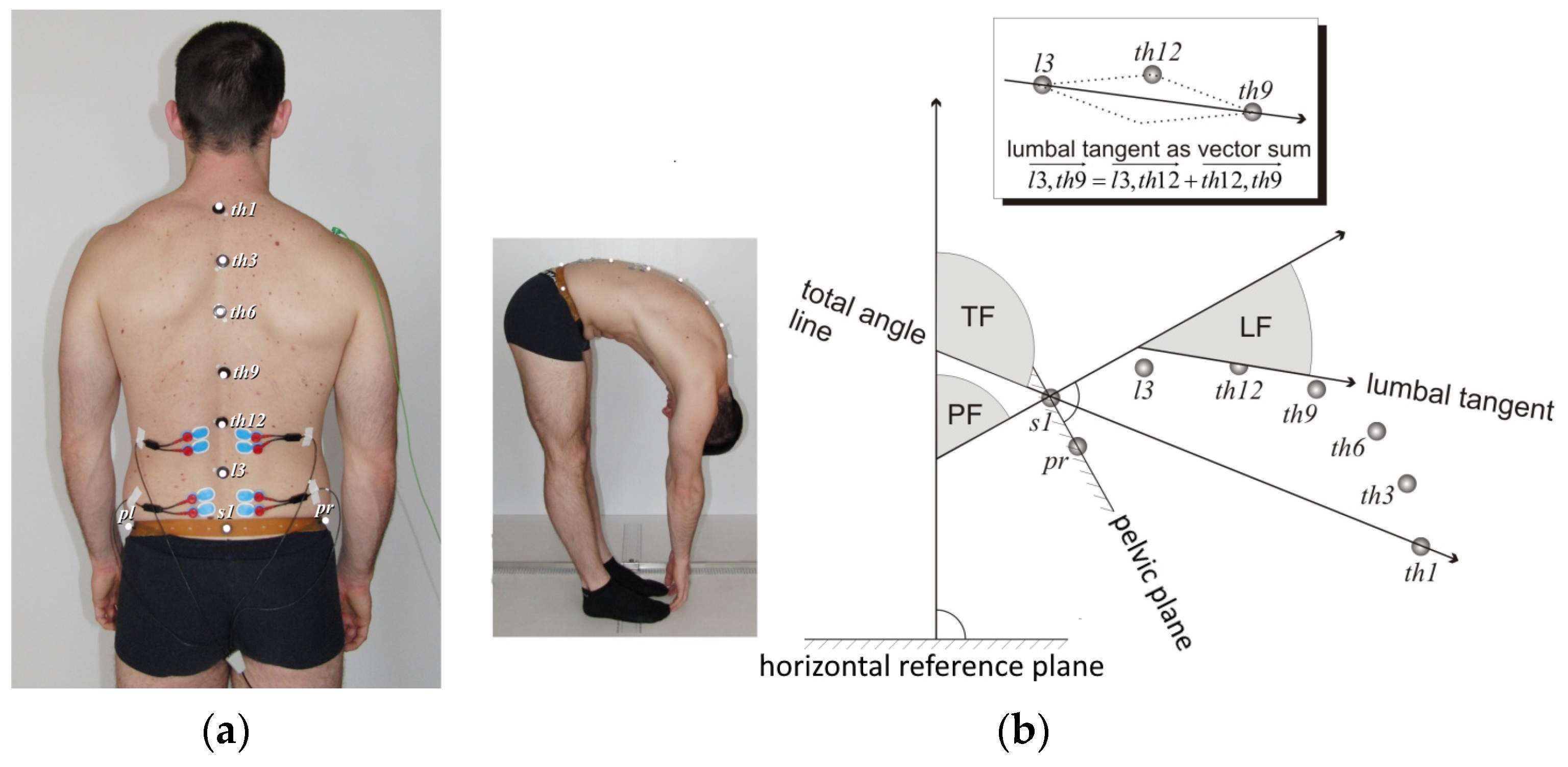
2.2.2. Flexion Relaxation Phenomenon
2.2.3. Measurements
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Valat, J.P.; Genevay, S.; Marty, M.; Rozenberg, S.; Koes, B. Sciatica. Best Pract. Res. Clin. Rheumatol. 2010, 24, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Tarulli, A.W.; Raynor, E.M. Lumbosacral radiculopathy. Neurol. Clin. 2007, 25, 387–405. [Google Scholar] [CrossRef] [PubMed]
- Deyo, R.A.; Loeser, J.D.; Bigos, S.J. Herniated lumbar intervertebral disk. Ann. Intern. Med. 1990, 112, 598–603. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, A.H. Diagnosis and management of low back pain and sciatica. Am. Fam. Physician 1995, 52, 1333–1341, 1347–1348. [Google Scholar] [PubMed]
- Atlas, S.J.; Deyo, R.A.; Keller, R.B.; Chapin, A.M.; Patrick, D.L.; Long, J.M.; Singeret, D.E. The Maine Lumbar Spine Study, Part II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine 1996, 21, 1777–1786. [Google Scholar] [CrossRef] [PubMed]
- Modic, M.T.; Obuchowski, N.A.; Ross, J.S.; Brant-Zawadzki, M.N.; Grooff, P.N.; Mazanec, D.J.; Benzel, E.C. Acute low back pain and radiculopathy: MR imaging findings and their prognostic role and effect on outcome. Radiology 2005, 237, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Suri, P.; Rainville, J.; Hunter, D.J.; Li, L.; Katz, J.N. Recurrence of radicular pain or back pain after nonsurgical treatment of symptomatic lumbar disk herniation. Arch. Phys. Med. Rehabil. 2012, 93, 690–695. [Google Scholar] [CrossRef] [PubMed]
- Paquet, N.; Malouin, F.; Richards, C. Hip-spine movement interaction and muscle activation patterns during sagittal trunk movements in low back patients. Spine 1994, 19, 596–603. [Google Scholar] [CrossRef] [PubMed]
- Haig, A.J.; Weismann, G.; Haugh, L.D.; Pope, M.; Grobler, L.J. Prospective evidence for change in paraspinal muscle activity after herniated nucleus pulposus. Spine 1993, 18, 926–930. [Google Scholar] [CrossRef]
- Alschuler, K.N.; Neblett, R.; Wiggert, E.; Haig, A.J.; Geisser, M.E. Flexion-relaxation and clinical features associated with chronic low back pain: A comparison of different methods of quantifying flexion-relaxation. Clin. J. Pain 2009, 25, 760–766. [Google Scholar] [CrossRef]
- Floyd, W.F.; Silver, P.H.S. Function of the erector spinae in flexion of the trunk. Lancet 1951, 1, 133–134. [Google Scholar] [CrossRef] [PubMed]
- Sihvonen, T.; Huttunen, M.; Makkonen, M.; Airaksinen, O. Functional changes in back muscle activity correlate with pain intensity and prediction of low back pain during pregnancy. Arch. Phys. Med. Rehabil. 1998, 79, 1210–1212. [Google Scholar] [CrossRef] [PubMed]
- Shirado, O.; Ito, T.; Kaneda, K.; Strax, T.E. Flexion-relaxation phenomenon in the back muscles: A comparative study between healthy subjects and patients with chronic low back pain. Am. J. Phys. Med. Rehabil. 1995, 74, 139–144. [Google Scholar] [CrossRef] [PubMed]
- van Dieen, J.; Selen, L.; Cholewicki, J. Trunk muscle activation in low-back pain patients, an analysis of the literature. J. Electromyogr. Kinesiol. 2003, 13, 333–351. [Google Scholar] [CrossRef] [PubMed]
- Geisser, M.E.; Haig, A.J.; Wallbom, A.S.; Wiggert, E.A. Pain-Related Fear, Lumbar Flexion, and Dynamic EMG Among Persons with Chronic Musculoskeletal Low Back Pain. Clin. J. Pain 2004, 20, 61–69. [Google Scholar] [CrossRef]
- Ambroz, C.; Scott, A.; Ambroz, A.; Talbott, E.O. Chronic low back pain assessment using surface electromyography. J. Occup. Environ. Med. 2000, 42, 660–669. [Google Scholar] [CrossRef] [PubMed]
- Sihvonen, T.; Partanen, J.; Hänninen, O.; Soimakallio, S. Electric behavior of low back muscles during lumbar pelvic rhythm in low back pain patients and healthy controls. Arch. Phys. Med. Rehabil. 1991, 72, 1080–1087. [Google Scholar] [PubMed]
- Watson, P.J.; Booker, C.K.; Main, C.J.; Chen, A.C.N. Surface electromyography in the identification of chronic low back pain patients: The development of the flexion relaxation ratio. Clin. Biomech. 1997, 3, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Neblett, R.; Brede, E.; Mayer, T.G.; Gatchel, J.R. What is the best surface EMG measure of lumbar flexion-relaxation for distinguishing chronic low back pain patients from pain-free controls? Clin. J. Pain 2013, 29, 334–340. [Google Scholar] [CrossRef]
- Owens, E.F., Jr.; Gudavalli, M.R.; Wilder, D.G. Paraspinal muscle function assessed with the flexion-relaxation ratio at baseline in a population of patients with back-related leg pain. J. Manip. Physiol. Ther. 2011, 34, 594–601. [Google Scholar] [CrossRef]
- Wong, T.K.; Lee, R.Y. Effects of low back pain on the relationship between the movements of the lumbar spine and hip. Hum. Mov. Sci. 2004, 23, 21–34. [Google Scholar] [CrossRef] [PubMed]
- Tabard-Fougère, A.; Dayer, R.; Armand, S.; Vuillerme, N. Flexion-Relaxation Phenomenon in Children and Adolescents with and without Nonspecific Chronic Low Back Pain: An. Electromyographic and Kinematic Cross-Sectional Comparative Study. Spine 2018, 43, 1322–1330. [Google Scholar] [CrossRef] [PubMed]
- Price, D.D.; McGrath, P.A.; Rafii, A.; Buckingham, B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983, 17, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Roland, M.; Fairbank, J. The Roland-Morris disability questionnaire and the Oswestry disability questionnaire. Spine 2000, 25, 3115–3124. [Google Scholar] [CrossRef] [PubMed]
- Staerkle, R.; Mannion, A.F.; Elfering, A.; Junge, A.; Semmer, N.K.; Jacobshagen, N.; Grob, D.; Dvorak, J.; Boos, N. Longitudinal validation of the fear-avoidance beliefs questionnaire (FABQ) in a Swiss-German sample of low back pain patients. Eur. Spine J. 2004, 13, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Merletti, R.; Lo Conte, L.; Avignone, E.; Guglielminotti, P. Modeling of surface myoelectric signals Part I: Model implementation. IEEE Trans. Biomed. Eng. 1999, 46, 810–820. [Google Scholar] [CrossRef] [PubMed]
- Peharec, S.; Jerkovic, R.; Bacic, P.; Azman, J.; Bobinac, D. Kinematic measurement of the lumbar spine and pelvis in the normal population. Coll. Antropol. 2007, 31, 1039–1042. [Google Scholar] [PubMed]
- Vismara, L.; Menegoni, F.; Zaina, F.; Galli, M.; Negrini, S.; Capodaglio, P. Effect of obesity and low back pain on spinal mobility: A cross sectional study in women. J. Neuroeng. Rehabil. 2010, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar] [CrossRef]
- Gouteron, A.; Tabard-Fougere, A.; Moissenet, F.; Bourredjem, A.; Rose-Dulcina, K.; Genevay, S.; Laroche, D.; Armand, S. Sensitivity and specificity of the flexion and extension relaxation ratios to identify altered paraspinal muscles’ flexion relaxation phenomenon in nonspecific chronic low back pain patients. J. Electromyogr. Kinesiol. 2023, 68, 102740. [Google Scholar] [CrossRef]
- Schinkel-Ivy, A.; Nairn, B.C.; Drake, J.D.M. Quantification of the lumbar flexion-relaxation phenomenon: Comparing outcomes of lumbar erector spinae and superficial lumbar multifidus in standing full trunk flexion and slumped sitting postures. J. Manip. Physiol. Ther. 2014, 37, 494–501. [Google Scholar] [CrossRef]
- Stevens, S.; Agten, A.; Timmermans, A.; Vandenabeele, F. Unilateral changes of the multifidus in persons with lumbar disc herniation: A systematic review and meta-analysis. Spine J. 2020, 20, 1573–1585. [Google Scholar] [CrossRef] [PubMed]
- Srhoj-Egekher, V.; Cifrek, M.; Peharec, S. Feature modeling for interpretable low back pain classification based on surface EMG. IEEE Access 2022, 10, 73702–73727. [Google Scholar] [CrossRef]
- Solomonow, M.; Hatipkarasulu, S.; Zhou, B.H.; Baratta, R.V.; Aghazadeh, F. Biomechanics and electromyography of a common idiopathic low back disorder. Spine 2003, 28, 1235–1248. [Google Scholar] [CrossRef] [PubMed]
- Solomonow, M.; Baratta, R.V.; Zhou, B.H.; Burger, E.; Zieske, A.; Gedalia, A. Muscular dysfunction elicited by creep of lumbar viscoelastic tissue. J. Electromyogr. Kinesiol. 2003, 13, 381–396. [Google Scholar] [CrossRef] [PubMed]
- Neblett, R.; Mayer, T.G.; Gatchel, R.J.; Keeley, J.; Proctor, T.; Anagnostis, C. Quantifying the lumbar flexion-relaxation phenomenon: Theory, normative data, and clinical applications. Spine 2003, 28, 1435–1446. [Google Scholar] [CrossRef] [PubMed]
- Kuslich, S.D.; Ulstrom, C.L.; Michael, C.J. The tissue origin of low back pain and sciatica: A report of pain response to tissue stimulation during operations on the lumbar spine using local anesthesia. Orthop. Clin. N. Am. 1991, 22, 181–187. [Google Scholar] [CrossRef]
- Dilley, A.; Lynn, B.; Pang, S.J. Pressure and stretch mechanosensitivity of peripheral nerve fibres following local inflammation of the nerve trunk. Pain 2005, 117, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Hall, T.; Quintner, J. Responses to mechanical stimulation of the upper limb in painful cervical radiculopathy. Aust. J. Physiother. 1996, 42, 277–285. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Butler, D.S. Adverse mechanical tension in the nervous system: A model for assessment and treatment. Aust. J. Physiother. 1989, 35, 227–238. [Google Scholar] [CrossRef]
- Smith, S.A.; Massie, J.B.; Chesnut, R.; Garfin, S.R. Straight leg raising. Anatomical effects on the spinal nerve root withou and with fusion. Spine 1993, 18, 992–999. [Google Scholar] [CrossRef]
- Gilbert, K.K.; Brismée, J.M.; Collins, D.L.; James, C.R.; Shah, R.V.; Sawyer, S.F.; Sizer, P.S., Jr. 2006 Young Investigator Award Winner: Lumbosacral nerve root displacement and strain: Part 1. A novel measurement technique during straight leg raises in unembalmed cadavers. Spine 2007, 32, 1513–1520. [Google Scholar] [CrossRef]
- Shum, G.L.; Attenborough, A.S.; Marsden, J.F.; Hough, A.D. Tibial nerve excursion during lumbar spine and hip flexion measured with diagnostic ultrasound. Ultrasound Med. Biol. 2013, 39, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, S.; Shizu, N.; Suzuki, Y.; Asai, T.; Yoshizawa, H. Changes in nerve root motion and intraradicular blood flow during an intraoperative straight-leg-raising test. Spine 2003, 28, 1427–1434. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, K.; Shima, I.; Porter, R.W. Nerve root pressure in lumbar disc herniation. Spine 1999, 24, 2003–2006. [Google Scholar] [CrossRef] [PubMed]
- Hirayama, J.; Yamagata, M.; Takahashi, K.; Moriya, H. Effect of noxious electrical stimulation of the peroneal nerve on stretch reflex activity of the hamstring muscle in rats. Spine 2005, 30, 1014–1018. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Cavanaugh, J.M.; Song, Z.; Takebayashi, T.; Kallakuri, S.; Wooley, P.H. Effects of nucleus pulposus on nerve root neural activity, mechanosensitivity, axonal morphology, and sodium channel expression. Spine 2004, 29, 17–25. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Granata, K.P.; Marras, W.S. Cost-benefit of muscle co-contraction in protecting against spinal instability. Spine 2000, 25, 1398–1404. [Google Scholar] [CrossRef] [PubMed]
- Geisser, M.E.; Ranavaya, M.; Haig, A.J.; Roth, R.S.; Zucker, R.; Ambroz, C.; Caruso, M. A meta-analytic review of surface electromyography among persons with low back pain and normal, healthy controls. J Pain 2005, 6, 711–726. [Google Scholar] [CrossRef] [PubMed]
- Marshall, P.W.; Murphy, B.A. Evaluation of functional and neuromuscular changes after exercise rehabilitation for low back pain using a Swiss ball: A pilot study. J. Manip. Physiol. Ther. 2006, 29, 550–560. [Google Scholar] [CrossRef]
- Ritvanen, T.; Zaproudina, N.; Nissen, M.; Leinonen, V.; Hänninen, O. Dynamic surface electromyographic responses in chronic low back pain treated by traditional bone setting and conventional physical therapy. J. Manip. Physiol. Ther. 2007, 30, 31–37. [Google Scholar] [CrossRef]
- Wallbom, A.S.; Geisser, M.E.; Koch, J.; Haig, A.J.; Guido, C.; Hoff, J.T. Lumbar flexion and dynamic EMG among persons with single level disk herniation pre- and postsurgery with radicular low-back pain. Am. J. Phys. Med. Rehabil. 2009, 88, 302–307. [Google Scholar] [CrossRef] [PubMed]
- McGorry, R.W.; Lin, J.H. Flexion relaxation and its relation to pain and function over the duration of a back pain episode. PLoS ONE 2012, 7, e39207. [Google Scholar] [CrossRef] [PubMed]

| CG (n = 34) | LBP (n = 75) | LBPR (n = 37) | p (ANOVA) | |
|---|---|---|---|---|
| Age mean ± SD | 31.0 ± 10.0 | 39.5 ± 11.1 | 35.7 ± 12.0 | 0.001 |
| BMI mean ± SD | 23.0 ± 3.1 | 25.3 ± 3.4 | 24.6 ± 2.5 | 0.002 |
| Gender–female | 53% | 28% | 30% | 0.030 |
| p (M-W test) | ||||
| Pain duration in months * | 8.4 (3.6–24.0) | 3.6 (1.2–7.2) | 0.011 | |
| Pain VAS now * | 3 (1–5) | 6 (2–6) | 0.001 | |
| Pain VAS average in last 4 weeks * | 5 (3–6) | 6 (4.5–7) | 0.002 | |
| RMQ questionnaire * | 5 (3–9) | 12.5 (8.5–15.5) | <0.001 | |
| ODI questionnaire * | 19 (10–30) | 35 (22–44) | <0.001 | |
| FABQPA questionnaire * | 18 (14–24) | 21 (18–24,5) | 0.043 | |
| FABQW questionnaire * | 23 (9–34.5) | 32.5 (25.5–46) | <0.001 |
| FRR L1–L2 inf/f | FRR L4–L5 inf/f | FRR L1–L2 inf/e | FRR L4–L5 inf/e | FRR L1–L2 f/e | FRR L4–L5 f/e | |
|---|---|---|---|---|---|---|
| VAS now | 0.25 (p = 0.009) | 0.30 (p = 0.001) | 0.31 (p = 0.001) | 0.32 (p = 0.001) | 0.35 (p = 0.001) | 0.29 (p = 0.002) |
| VAS average in last 4 weeks | 0.18 | 0.17 | 0.20 (p = 0.031) | 0.22 (p = 0.020) | 0.22 (p = 0.020) | 0.26 (p = 0.002) |
| I CG (n = 34) | II LBP (n = 75) | III LBPR (n = 37) | p | Cohen’s d | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| MOTION | Mean | SD | Mean | SD | Mean | SD | LBP to CG | LBPR to CG | LBP to LBPR | |
| Total flexion /° | 116.2 | 9.9 | 99.6 | 16.4 | 62.3 | 19.7 | <0.001 | −1.14 | −3.44 | −2.17 |
| Lumbar flexion /° | 63.2 | 6.5 | 51.9 | 11.7 | 32.8 | 12.2 | <0.001 | −1.10 | −3.10 | −1.66 |
| Pelvis flexion /° | 55.6 | 7.0 | 46.5 | 12.1 | 25.2 | 12.1 | <0.001 | −0.85 | −3.07 | −1.80 |
| Hamstrings flexibility right /° | 86.3 | 9.6 | 77.8 | 10.0 | 71.0 | 13.6 | <0.001 | −0.90 | −1.84 | −1.44 |
| Hamstrings flexibility left /° | 86.6 | 9.6 | 77.3 | 9.8 | 70.7 | 13.5 | <0.001 | −0.97 | −2.08 | −1.67 |
| sEMG | Mean | SD | Mean | SD | Mean | SD | p | LBP to CG | LBPR to CG | LBP to LBPR |
| FRR L1–L2 inf/f | 0.25 | 0.13 | 0.35 | 0.27 | 0.75 | 0.30 | <0.001 | 0.43 | 2.18 | 1.30 |
| FRR L4–L5 inf/f | 0.25 | 0.13 | 0.46 | 0.32 | 0.85 | 0.22 | <0.001 | 0.77 | 3.27 | 1.36 |
| FRR L1–L2 inf/e | 0.07 | 0.03 | 0.16 | 0.16 | 0.46 | 0.26 | <0.001 | 0.66 | 2.09 | 1.56 |
| FRR L4–L5 inf/e | 0.09 | 0.05 | 0.29 | 0.25 | 0.68 | 0.23 | <0.001 | 0.97 | 3.53 | 1.74 |
| FRR L1–L2 f/e | 0.32 | 0.14 | 0.41 | 0.15 | 0.59 | 0.21 | <0.001 | 0.61 | 1.53 | 1.14 |
| FRR L4–L5 f/e | 0.40 | 0.11 | 0.55 | 0.18 | 0.79 | 0.15 | <0.001 | 0.92 | 2.89 | 1.33 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peharec, M.; Peharec, S.; Srhoj-Egekher, V.; Jerković, R.; Girotto, D.; Starčević-Klasan, G. The Flexion Relaxation Phenomenon in Patients with Radiculopathy and Low Back Pain: A Cross-Sectional Study. J. Funct. Morphol. Kinesiol. 2024, 9, 77. https://doi.org/10.3390/jfmk9020077
Peharec M, Peharec S, Srhoj-Egekher V, Jerković R, Girotto D, Starčević-Klasan G. The Flexion Relaxation Phenomenon in Patients with Radiculopathy and Low Back Pain: A Cross-Sectional Study. Journal of Functional Morphology and Kinesiology. 2024; 9(2):77. https://doi.org/10.3390/jfmk9020077
Chicago/Turabian StylePeharec, Marijan, Stanislav Peharec, Vedran Srhoj-Egekher, Romana Jerković, Dean Girotto, and Gordana Starčević-Klasan. 2024. "The Flexion Relaxation Phenomenon in Patients with Radiculopathy and Low Back Pain: A Cross-Sectional Study" Journal of Functional Morphology and Kinesiology 9, no. 2: 77. https://doi.org/10.3390/jfmk9020077
APA StylePeharec, M., Peharec, S., Srhoj-Egekher, V., Jerković, R., Girotto, D., & Starčević-Klasan, G. (2024). The Flexion Relaxation Phenomenon in Patients with Radiculopathy and Low Back Pain: A Cross-Sectional Study. Journal of Functional Morphology and Kinesiology, 9(2), 77. https://doi.org/10.3390/jfmk9020077







