Calcium Orthophosphate (CaPO4) Containing Composites for Biomedical Applications: Formulations, Properties, and Applications
Abstract
:1. Introduction
2. General Knowledge and Experience
3. Main Components of Bone Graft Biocomposites and Hybrid Biomaterials
3.1. CaPO4
3.2. Polymers
3.3. Inorganic Materials, Substances and Compounds
3.3.1. Metals
3.3.2. Glasses and Glass–Ceramics
3.3.3. Ceramics
3.3.4. Carbon
4. A Brief Information on Preparation Techniques
5. CaPO4-Based Biocomposites and Hybrid Biomaterials
- Biocomposites with polymers;
- Self-hardening biocomposites;
- Nanosized CaPO4-based formulations and nanosized biocomposites;
- Collagen-containing biocomposites;
- Biocomposites with other bio-organic compounds;
- Injectable bone substitutes (IBS);
- Biocomposites with glasses, inorganic compounds, carbon, and metals;
- Biocomposites from CaPO4 only;
- Inks for 3D printing;
- Functionally graded biocomposites;
- Biosensors.
5.1. Biocomposites with Polymers
5.1.1. History and General Part
5.1.2. Apatite-Based Formulations
5.1.3. TCP-Based Formulations
5.1.4. Biocomposites with Remaining CaPO4
5.2. Self-Hardening Biocomposites
5.3. Nanosized CaPO4-Based Formulations and Nanosized Biocomposites
5.4. Collagen-Containing Biocomposites
5.5. Biocomposites with Other Bio-Organic Compounds
5.6. Injectable Bone Substitutes (IBSs)
5.7. Biocomposites with Glasses, Inorganic Compounds, Metals, and Carbon
5.8. Biocomposites from CaPO4 Only
5.9. Inks for 3D Printing
5.10. Functionally Graded Biocomposites
5.11. Biosensors
6. Interactions among the Phases in CaPO4-Based Biocomposites
7. Ways to Create a Chemical Bonding among the Constituents of Biocomposites
8. Bioactivity and Biodegradability of CaPO4-Containing Biocomposites
9. Biomedical and Non-Biomedical Applications
10. Some Issues and Key Challenges
- When compared to traditional monolithic materials, the long-term performance of biocomposites is not well-supported by sufficient credible experimental and clinical data.
- The number of design variables that must be taken into account makes the design of hybrid and composite formulations significantly more challenging than the design of classic single-phase ones.
- Manufacturing techniques might be costly, time-consuming, dependent on cutting-edge technology, and restricted to certain reinforcing configurations. They might also call for certain cleaning and sterilizing procedures.
- There are currently no adequate guidelines for biocompatibility testing of biocomposite implants since it is unclear how the components of biocomposites interact with biological tissues.
- The fatigue behavior of biocomposites is much more complex and less predictable than conventional single-phase materials and there are not enough criteria to evaluate the fatigue performance of the biocomposites.
- Optimization of processing conditions for biocomposites.
- Enhancement of interfacial adhesion and strength similar to that of genuine bone.
- To facilitate bone formation, both surface characteristics and pore size should be optimized.
- Maintaining sufficient in vivo structure volume for osteogenesis to occur.
- Resistance to load-bearing conditions.
- Matching the bioabsorbability and biomechanical properties of the graft when creating new bone.
- Understanding the molecular processes by which cells and biocomposite matrices interact in vivo to support bone regeneration is necessary.
- Promoting angiogenesis and vascularization for healthy bone cell growth and subsequent tissue formation and remodeling.
11. Conclusions
Funding
Conflicts of Interest
Abbreviations
| A-W | apatite-wollastonite |
| BMP | bone morphogenetic protein |
| BSA | bovine serum albumin |
| CMC | carboxymethylcellulose |
| DNA | desoxynucleic acid |
| EVOHa | copolymer of ethylene and vinyl alcohol |
| IBS | injectable bone substitute |
| HDPE | high-density polyethylene |
| HPMC | hydroxypropylmethylcellulose |
| PA | polyamide |
| PAA | polyacrylic acid |
| PBT | polybutyleneterephthalate |
| PCL | poly(ε-caprolactone) |
| PDLA | poly(d-lactic acid) |
| PDLLA | poly(d,l-lactic acid) |
| PE | polyethylene |
| PEEK | polyetheretherketone |
| PEG | polyethylene glycol |
| PGA | polyglycolic acid |
| PHB | polyhydroxybutyrate |
| PHBHV | poly(hydroxybutyrate-co-hydroxyvalerate) |
| PHEMA | polyhydroxyethyl methacrylate |
| PLA | polylactic acid |
| PLGA | poly(lactic-co-glycolic) acid |
| PLGC | co-polyester lactide-co-glycolide-co-ε-caprolactone |
| PLLA | poly(l-lactic acid) |
| PMMA | polymethylmethacrylate |
| PP | polypropylene |
| PPF | poly(propylene-co-fumarate) |
| PSZ | partially stabilized zirconia |
| PTMC | poly(trimethylene carbonate) |
| PU | polyurethane |
| PVA | polyvinyl alcohol |
| PVAP | polyvinyl alcohol phosphate |
References
- Kaveh, K.; Ibrahim, R.; Bakar, M.Z.A.; Ibrahim, T.A. Bone grafting and bone graft substitutes. J. Anim. Vet. Adv. 2010, 9, 1055–1067. [Google Scholar] [CrossRef]
- Shibuya, N.; Jupiter, D.C. Bone graft substitute: Allograft and xenograft. Clin. Podiatr. Med. Surg. 2015, 32, 21–34. [Google Scholar] [CrossRef]
- Georgeanu, V.A.; Gingu, O.; Antoniac, I.V.; Manolea, H.O. Current options and future perspectives on bone graft and biomaterials substitutes for bone repair, from clinical needs to advanced biomaterials research. Appl. Sci. 2023, 13, 8471. [Google Scholar] [CrossRef]
- Li, S.; Chen, Y.; Lin, Z.; Cui, W.; Zhao, J.; Su, W. A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone-patellar tendon-bone autografts for the reconstruction of the anterior cruciate ligament. Arch. Orthop. Trauma Surg. 2012, 132, 1287–1297. [Google Scholar] [CrossRef]
- Gillman, C.E.; Jayasuriya, A.C. FDA-approved bone grafts and bone graft substitute devices in bone regeneration. Mater. Sci. Eng. C 2021, 130, 112466. [Google Scholar] [CrossRef]
- Keller, E.E.; Triplett, W.W. Iliac crest bone grafting: Review of 160 consecutive cases. J. Oral Maxillofac. Surg. 1987, 45, 11–14. [Google Scholar] [CrossRef]
- Giladi, A.M.; Rinkinen, J.R.; Higgins, J.P.; Iorio, M.L. Donor-site morbidity of vascularized bone flaps from the distal femur: A systematic review. Plast. Reconstr. Surg. 2018, 142, 363E–372E. [Google Scholar] [CrossRef]
- Boehm, K.S.; Al-Taha, M.; Morzycki, A.; Samargandi, O.A.; Al-Youha, S.; Leblanc, M.R. Donor site morbidities of iliac crest bone graft in craniofacial surgery: A systematic review. Ann. Plas. Surg. 2019, 83, 352–358. [Google Scholar] [CrossRef]
- Attia, A.K.; Mahmoud, K.; ElSweify, K.; Bariteau, J.; Labib, S.A. Donor site morbidity of calcaneal, distal tibial and proximal tibial cancellous bone autografts in foot and ankle surgery. A systematic review and meta-analysis of 2296 bone grafts. Foot Ankle Surg. 2022, 28, 680–690. [Google Scholar] [CrossRef]
- Li, Z.; Kawashita, M. Current progress in inorganic artificial biomaterials. J. Artif. Organ. 2011, 14, 163–170. [Google Scholar] [CrossRef]
- Bojar, W.; Kucharska, M.; Ciach, T.; Koperski, Ł.; Jastrzębski, Z.; Szałwiński, M. Bone regeneration potential of the new chitosan-based alloplastic biomaterial. J. Biomater. Appl. 2014, 28, 1060–1068. [Google Scholar] [CrossRef]
- Wickramasinghe, M.L.; Dias, G.J.; Premadasa, K.M.G.P. A novel classification of bone graft materials. J. Biomed. Mater. Res. B Appl. Biomater. 2022, 110, 1724–1749. [Google Scholar] [CrossRef]
- Panchbhavi, V.K. Synthetic bone grafting in foot and ankle surgery. Foot Ankle Clin. 2010, 15, 559–576. [Google Scholar] [CrossRef]
- Weiner, S.; Wagner, H.D. The material bone: Structure-mechanical function relations. Ann. Rev. Mater. Sci. 1998, 28, 271–298. [Google Scholar] [CrossRef]
- Rey, C.; Combes, C.; Drouet, C.; Glimcher, M.J. Bone mineral: Update on chemical composition and structure. Osteoporos. Int. 2009, 20, 1013–1021. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Calcium Orthophosphates: Applications in Nature, Biology and Medicine; Pan Stanford: Singapore, 2012; p. 854. [Google Scholar]
- Dorozhkin, S.V. Calcium Orthophosphate-Based Bioceramics and Biocomposites; Wiley-VCH: Weinheim, Germany, 2016; p. 405. [Google Scholar]
- Burr, D.B. The contribution of the organic matrix to bone’s material properties. Bone 2002, 31, 8–11. [Google Scholar] [CrossRef]
- Fratzl, P.; Gupta, H.S.; Paschalis, E.P.; Roschger, P. Structure and mechanical quality of the collagen-mineral nano-composite in bone. J. Mater. Chem. 2004, 14, 2115–2123. [Google Scholar] [CrossRef]
- Olszta, M.J.; Cheng, X.G.; Jee, S.S.; Kumar, B.R.; Kim, Y.Y.; Kaufman, M.J.; Douglas, E.P.; Gower, L.B. Bone structure and formation: A new perspective. Mater. Sci. Eng. R 2007, 58, 77–116. [Google Scholar] [CrossRef]
- Fonseca, H.; Moreira-Gonçalves, D.; Coriolano, H.J.A.; Duarte, J.A. Bone quality: The determinants of bone strength and fragility. Sports Med. 2014, 44, 37–53. [Google Scholar] [CrossRef]
- Murugan, R.; Ramakrishna, S. Development of nanocomposites for bone grafting. Compos. Sci. Technol. 2005, 65, 2385–2406. [Google Scholar] [CrossRef]
- Suchanek, W.; Yoshimura, M. Processing and properties of hydroxyapatite-based biomaterials for use as hard tissue replacement implants. J. Mater. Res. 1998, 13, 94–117. [Google Scholar] [CrossRef]
- Vallet-Regi, M.; Arcos, D. Nanostructured hybrid materials for bone tissue regeneration. Curr. Nanosci. 2006, 2, 179–189. [Google Scholar] [CrossRef]
- Doblaré, M.; Garcia, J.M.; Gómez, M.J. Modelling bone tissue fracture and healing: A review. Eng. Fract. Mech. 2004, 71, 1809–1840. [Google Scholar] [CrossRef]
- Vallet-Regi, M. Revisiting ceramics for medical applications. Dalton Trans. 2006, 44, 5211–5220. [Google Scholar] [CrossRef]
- Pioletti, D.P. Biomechanics in bone tissue engineering. Comput. Methods Biomech. Biomed. Eng. 2010, 13, 837–846. [Google Scholar] [CrossRef]
- Huiskes, R.; Ruimerman, R.; van Lenthe, H.G.; Janssen, J.D. Effects of mechanical forces on maintenance and adaptation of form in trabecular bone. Nature 2000, 405, 704–706. [Google Scholar] [CrossRef]
- Boccaccini, A.R.; Blaker, J.J. Bioactive composite materials for tissue engineering scaffolds. Expert Rev. Med. Dev. 2005, 2, 303–317. [Google Scholar] [CrossRef]
- Hutmacher, D.W.; Schantz, J.T.; Lam, C.X.F.; Tan, K.C.; Lim, T.C. State of the art and future directions of scaffold-based bone engineering from a biomaterials perspective. J. Tissue Eng. Regen. Med. 2007, 1, 245–260. [Google Scholar] [CrossRef]
- Guarino, V.; Causa, F.; Ambrosio, L. Bioactive scaffolds for bone and ligament tissue. Expert Rev. Med. Dev. 2007, 4, 405–418. [Google Scholar] [CrossRef]
- Yunos, D.M.; Bretcanu, O.; Boccaccini, A.R. Polymer-bioceramic composites for tissue engineering scaffolds. J. Mater. Sci. 2008, 43, 4433–4442. [Google Scholar] [CrossRef]
- Zhao, H.X. Progress of study on drug-loaded chitosan/hydroxyapatite composite in bone tissue engineering. J. Funct. Mater. 2014, 45, 13006–13012+13020. [Google Scholar]
- Hench, L.L.; Polak, J.M. Third-generation biomedical materials. Science 2002, 295, 1014–1017. [Google Scholar] [CrossRef]
- Mathijsen, A. Nieuwe Wijze van Aanwending van het Gips-Verband bij Beenbreuken; J.B. van Loghem: Haarlem, The Netherlands, 1852; p. 21. [Google Scholar]
- Dreesman, H. Über Knochenplombierung. Beitr. Klin. Chir. 1892, 9, 804–810. [Google Scholar]
- Wang, M. Developing bioactive composite materials for tissue replacement. Biomaterials 2003, 24, 2133–2151. [Google Scholar] [CrossRef]
- Available online: https://en.wikipedia.org/wiki/Composite_material (accessed on 10 May 2024).
- Gibson, R.F. A review of recent research on mechanics of multifunctional composite materials and structures. Compos. Struct. 2010, 92, 2793–2810. [Google Scholar] [CrossRef]
- Evans, S.L.; Gregson, P.J. Composite technology in load-bearing orthopaedic implants. Biomaterials 1998, 19, 1329–1342. [Google Scholar] [CrossRef]
- Wan, Y.Z.; Hong, L.; Jia, S.R.; Huang, Y.; Zhu, Y.; Wang, Y.L.; Jiang, H.J. Synthesis and characterization of hydroxyapatite-bacterial cellulose nanocomposites. Compos. Sci. Technol. 2006, 66, 1825–1832. [Google Scholar] [CrossRef]
- Oyane, A. Development of apatite-based composites by a biomimetic process for biomedical applications. J. Ceram. Soc. Jpn. 2010, 118, 77–81. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Calcium orthophosphate coatings on magnesium and its biodegradable alloys. Acta Biomater. 2014, 10, 2919–2934. [Google Scholar] [CrossRef]
- Varadavenkatesan, T.; Vinayagam, R.; Pai, S.; Kathirvel, B.; Pugazhendhi, A.; Selvaraj, R. Synthesis, biological and environmental applications of hydroxyapatite and its composites with organic and inorganic coatings. Prog. Org. Coat. 2021, 151, 106056. [Google Scholar] [CrossRef]
- Wysokowski, M.; Machałowski, T.; Idaszek, J.; Chlanda, A.; Jaroszewicz, J.; Heljak, M.; Niemczak, M.; Piasecki, A.; Gajewska, M.; Ehrlich, H.; et al. Deep eutectic solvent-assisted fabrication of bioinspired 3D carbon–calcium phosphate scaffolds for bone tissue engineering. RSC Adv. 2023, 13, 21971–21981. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. There are over 60 ways to produce biocompatible calcium orthophosphate (CaPO4) deposits on various substrates. J. Compos. Sci. 2023, 7, 273. [Google Scholar] [CrossRef]
- Zhao, J.; Guo, L.Y.; Yang, X.B.; Weng, J. Preparation of bioactive porous HA/PCL composite scaffolds. Appl. Surf. Sci. 2008, 255, 2942–2946. [Google Scholar] [CrossRef]
- Dorozhkin, S.; Ajaal, T. Strengthening of dense bioceramic samples using bioresorbable polymers—A statistical approach. J. Biomim. Biomater. Tiss. Eng. 2009, 4, 27–39. [Google Scholar] [CrossRef]
- Woo, A.S.; Jang, J.L.; Liberman, R.F.; Weinzweig, J. Creation of a vascularized composite graft with acellular dermal matrix and hydroxyapatite. Plast. Reconstr. Surg. 2010, 125, 1661–1669. [Google Scholar] [CrossRef]
- Vila, M.; Sánchez-Salcedo, S.; Cicuéndez, M.; Izquierdo-Barba, I.; Vallet-Regí, M. Novel biopolymer-coated hydroxyapatite foams for removing heavy-metals from polluted water. J. Hazard. Mater. 2011, 192, 71–77. [Google Scholar] [CrossRef]
- Furko, M.; Detsch, R.; Tolnai, I.; Tolnai, I.; Balázsi, K.; Boccaccini, A.R.; Balázsi, C. Biomimetic mineralized amorphous carbonated calcium phosphate-polycaprolactone bioadhesive composites as potential coatings on implant materials. Ceram. Int. 2023, 49 Pt B, 18565–18576. [Google Scholar] [CrossRef]
- Dong, J.; Uemura, T.; Kojima, H.; Kikuchi, M.; Tanaka, J.; Tateishi, T. Application of low-pressure system to sustain in vivo bone formation in osteoblast/porous hydroxyapatite composite. Mater. Sci. Eng. C 2001, 17, 37–43. [Google Scholar] [CrossRef]
- Mikán, J.; Villamil, M.; Montes, T.; Carretero, C.; Bernal, C.; Torres, M.L.; Zakaria, F.A. Porcine model for hybrid material of carbonated apatite and osteoprogenitor cells. Mater. Res. Innov. 2009, 13, 323–326. [Google Scholar] [CrossRef]
- Oe, K.; Miwa, M.; Nagamune, K.; Sakai, Y.; Lee, S.Y.; Niikura, T.; Iwakura, T.; Hasegawa, T.; Shibanuma, N.; Hata, Y.; et al. Nondestructive evaluation of cell numbers in bone marrow stromal cell/β-tricalcium phosphate composites using ultrasound. Tissue Eng. C 2010, 16, 347–353. [Google Scholar] [CrossRef]
- Kundu, B.; Soundrapandian, C.; Nandi, S.K.; Mukherjee, P.; Dandapat, N.; Roy, S.; Datta, B.K.; Mandal, T.K.; Basu, D.; Bhattacharya, R.N. Development of new localized drug delivery system based on ceftriaxone-sulbactam composite drug impregnated porous hydroxyapatite: A systematic approach for in vitro and in vivo animal trial. Pharm. Res. 2010, 27, 1659–1676. [Google Scholar] [CrossRef]
- Skrinda-Melne, M.; Locs, J.; Grava, A.; Dubnika, A. Calcium phosphates enhanced with liposomes—The future of bone regeneration and drug delivery. J. Liposome Res. 2024. early view. [Google Scholar] [CrossRef]
- Holzmeister, I.; Schamel, M.; Groll, J.; Gbureck, U.; Vorndran, E. Artificial inorganic biohybrids: The functional combination of microorganisms and cells with inorganic materials. Acta Biomater. 2018, 74, 17–35. [Google Scholar] [CrossRef]
- Kickelbick, G. (Ed.) Hybrid Materials. Synthesis, Characterization and Applications; Wiley-VCH Verlag: Weinheim, Germany, 2007; p. 498. [Google Scholar]
- Matthews, F.L.; Rawlings, R.D. Composite Materials: Engineering and Science; CRC Press: Boca Raton, FL, USA, 2000; p. 480. [Google Scholar]
- Xia, Z.; Riester, L.; Curtin, W.A.; Li, H.; Sheldon, B.W.; Liang, J.; Chang, B.; Xu, J.M. Direct observation of toughening mechanisms in carbon nanotube ceramic matrix composites. Acta Mater. 2004, 52, 931–944. [Google Scholar] [CrossRef]
- Tavares, M.I.B.; Ferreira, O.; Preto, M.; Miguez, E.; Soares, I.L.; da Silva, E.P. Evaluation of composites miscibility by low field NMR. Int. J. Polym. Mater. 2007, 56, 1113–1118. [Google Scholar] [CrossRef]
- Kiran, E. Polymer miscibility, phase separation, morphological modifications and polymorphic transformations in dense fluids. J. Supercrit. Fluids 2009, 47, 466–483. [Google Scholar] [CrossRef]
- Šupová, M. Problem of hydroxyapatite dispersion in polymer matrices: A review. J. Mater. Sci. Mater. Med. 2009, 20, 1201–1213. [Google Scholar] [CrossRef]
- Böstman, O.; Pihlajamäki, H. Clinical biocompatibility of biodegradable orthopaedic implants for internal fixation: A review. Biomaterials 2000, 21, 2615–2621. [Google Scholar] [CrossRef]
- Zhang, X.D.; Williams, D.F. (Eds.) Definitions of biomaterials for the twenty-first century. In Proceedings of the Consensus Conference, Chengdu, China, 11–12 June 2018; Materials Today. Elsevier: Amsterdam, The Netherlands, 2019; p. 290. [Google Scholar]
- John, M.J.; Thomas, S. Biofibres and biocomposites. Carbohydr. Polym. 2008, 71, 343–364. [Google Scholar] [CrossRef]
- Tanner, K.E. Bioactive ceramic-reinforced composites for bone augmentation. J. R. Soc. Interface 2010, 7, S541–S557. [Google Scholar] [CrossRef]
- Gravitis, Y.A.; Tééyaér, R.E.; Kallavus, U.L.; Andersons, B.A.; Ozol’-Kalnin, V.G.; Kokorevich, A.G.; Érin’sh, P.P.; Veveris, G.P. Biocomposite structure of wood cell membranes and their destruction by explosive autohydrolysis. Mech. Compos. Mater. 1987, 22, 721–725. [Google Scholar] [CrossRef]
- Bernard, S.L.; Picha, G.J. The use of coralline hydroxyapatite in a ‘biocomposite’ free flap. Plast. Reconstr. Surg. 1991, 87, 96–107. [Google Scholar] [CrossRef]
- Rao, H.; Thompson, W.A.; Katz, J.L.; Harper, R.A. Elastic constants of the composite system hydroxyapatite-dicalcium phosphate dihydrate. J. Dent. Res. 1976, 55, 708. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Calcium orthophosphates and human beings. A historical perspective from the 1770s until 1940. Biomatter 2012, 2, 53–70. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. A detailed history of calcium orthophosphates from 1770s till 1950. Mater. Sci. Eng. C 2013, 33, 3085–3110. [Google Scholar] [CrossRef]
- Hing, K.A. Bioceramic bone graft substitutes: Influence of porosity and chemistry. Int. J. Appl. Ceram. Technol. 2005, 2, 184–199. [Google Scholar] [CrossRef]
- Naqshbandi, A.R.; Sopyan, I. Development of porous calcium phosphate bioceramics for bone implant applications: A review. Rec. Pat. Mater. Sci. 2013, 6, 238–252. [Google Scholar]
- LeGeros, R.Z. Calcium Phosphates in Oral Biology and Medicine. In Monographs in Oral Science; Myers, H.M., Ed.; Karger: Basel, Switzerland, 1991; Volume 15, p. 201. [Google Scholar]
- Elliott, J.C. Structure and Chemistry of the Apatites and Other Calcium Orthophosphates, Studies in Inorganic Chemistry; Elsevier: Amsterdam, The Netherlands, 1994; Volume 18, p. 389. [Google Scholar]
- Heimann, R.B. (Ed.) Calcium Phosphate: Structure, Synthesis, Properties and Applications; Nova Science: New York, NY, USA, 2012; p. 498. [Google Scholar]
- Gshalaev, V.S.; Demirchan, A.C. (Eds.) Hydroxyapatite: Synthesis, Properties and Applications; Nova Science: New York, NY, USA, 2012; p. 477. [Google Scholar]
- Carraher, C.E., Jr. Introduction to Polymer Chemistry, 2nd ed.; CRC Press: Boca Raton, FL, USA, 2010; p. 534. [Google Scholar]
- Young, R.J.; Lovell, P.A. Introduction to Polymers, 3rd ed.; CRC Press: Boca Raton, FL, USA, 2011; p. 688. [Google Scholar]
- Thomson, R.C.; Ak, S.; Yaszemski, M.J.; Mikos, A.G. Polymer scaffold processing. In Principles of Tissue Engineering; Academic Press: New York, NY, USA, 2000; pp. 251–262. [Google Scholar]
- Khan, M.U.A.; Aslam, M.A.; Abdullah, M.F.B.; Hasan, A.; Shah, S.A.; Stojanović, G.M. Recent perspective of polymeric biomaterial in tissue engineering—A review. Mater. Today Chem. 2023, 34, 101818. [Google Scholar] [CrossRef]
- Shastri, V.P. Non-degradable biocompatible polymers in medicine: Past, present and future. Curr. Pharm. Biotechnol. 2003, 4, 331–337. [Google Scholar] [CrossRef]
- Chen, H.; Yuan, L.; Song, W.; Wu, Z.; Li, D. Biocompatible polymer materials: Role of protein-surface interactions. Prog. Polym. Sci. 2008, 33, 1059–1087. [Google Scholar] [CrossRef]
- Tanaka, M.; Sato, K.; Kitakami, E.; Kobayashi, S.; Hoshiba, T.; Fukushima, K. Design of biocompatible and biodegradable polymers based on intermediate water concept. Polym. J. 2015, 47, 114–121. [Google Scholar] [CrossRef]
- Lanza, R.P.; Hayes, J.L.; Chick, W.L. Encapsulated cell technology. Nat. Biotechnol. 1996, 14, 1107–1111. [Google Scholar] [CrossRef]
- Shukla, S.C.; Singh, A.; Pandey, A.K.; Mishra, A. Review on production and medical applications of ɛ-polylysine. Biochem. Eng. J. 2012, 65, 70–81. [Google Scholar] [CrossRef]
- Agrawal, C.M.; Ray, R.B. Biodegradable polymeric scaffolds for musculoskeletal tissue engineering. J. Biomed. Mater. Res. 2001, 55, 141–150. [Google Scholar] [CrossRef]
- Kweon, H.; Yoo, M.; Park, I.; Kim, T.; Lee, H.; Lee, S.; Oh, J.; Akaike, T.; Cho, C. A novel degradable polycaprolactone network for tissue engineering. Biomaterials 2003, 24, 801–808. [Google Scholar] [CrossRef]
- Wang, Y.C.; Zhang, P.H. Electrospun absorbable polycaprolactone (PCL) scaffolds for medical applications. Adv. Mater. Res. 2014, 906, 221–225. [Google Scholar] [CrossRef]
- Sartori, S.; Chiono, V.; Tonda-Turo, C.; Mattu, C.; Gianluca, C. Biomimetic polyurethanes in nano and regenerative medicine. J. Mater. Chem. B 2014, 2, 5128–5144. [Google Scholar] [CrossRef]
- Temenoff, J.S.; Mikos, A.G. Injectable biodegradable materials for orthopedic tissue engineering. Biomaterials 2000, 21, 2405–2412. [Google Scholar] [CrossRef]
- Behravesh, E.; Yasko, A.W.; Engel, P.S.; Mikos, A.G. Synthetic biodegradable polymers for orthopaedic applications. Clin. Orthop. Rel. Res. 1999, 367S, S118–S125. [Google Scholar] [CrossRef]
- Lewandrowski, K.U.; Gresser, J.D.; Wise, D.L.; White, R.L.; Trantolo, D.J. Osteoconductivity of an injectable and bioresorbable poly(propyleneglycol-co-fumaric acid) bone cement. Biomaterials 2000, 21, 293–298. [Google Scholar] [CrossRef]
- Lee, K.W.; Wang, S.; Fox, B.C.; Ritman, E.L.; Yaszemski, M.J.; Lu, L. Poly(propylene fumarate) bone tissue engineering scaffold fabrication using stereolithography: Effects of resin formulations and laser parameters. Biomacromolecules 2007, 8, 1077–1084. [Google Scholar] [CrossRef]
- Xu, J.; Feng, E.; Song, J. Renaissance of aliphatic polycarbonates: New techniques and biomedical applications. J. Appl. Polym. Sci. 2014, 131, 39822. [Google Scholar] [CrossRef]
- Boland, E.D.; Coleman, B.D.; Barnes, C.P.; Simpson, D.G.; Wnek, G.E.; Bowlin, G.L. Electrospinning polydioxanone for biomedical applications. Acta Biomater. 2005, 1, 115–123. [Google Scholar] [CrossRef]
- Swain, S.K.; Prusty, K. Biomedical applications of acrylic-based nanohydrogels. J. Mater. Sci. 2018, 53, 2303–2325. [Google Scholar] [CrossRef]
- Frazer, R.Q.; Byron, R.T.; Osborne, P.B.; West, K.P. PMMA: An essential material in medicine and dentistry. J. Long-Term Eff. Med. Implants 2005, 15, 629–639. [Google Scholar] [CrossRef]
- Li, Y.W.; Leong, J.C.Y.; Lu, W.W.; Luk, K.D.K.; Cheung, K.M.C.; Chiu, K.Y.; Chow, S.P. A novel injectable bioactive bone cement for spinal surgery: A developmental and preclinical study. J. Biomed. Mater. Res. 2000, 52, 164–170. [Google Scholar] [CrossRef]
- Mckellop, H.; Shen, F.; Lu, B.; Campbell, P.; Salovey, R. Development of an extremely wear resistant UHMW polyethylene for total hip replacements. J. Orthop. Res. 1999, 17, 157–167. [Google Scholar] [CrossRef]
- Kurtz, S.M.; Muratoglu, O.K.; Evans, M.; Edidin, A.A. Advances in the processing, sterilization and crosslinking of ultra-high molecular weight polyethylene for total joint arthroplasty. Biomaterials 1999, 20, 1659–1688. [Google Scholar] [CrossRef]
- Laurencin, C.T.; Ambrosio, M.A.; Borden, M.D.; Cooper, J.A., Jr. Tissue engineering: Orthopedic applications. Ann. Rev. Biomed. Eng. 1999, 1, 19–46. [Google Scholar] [CrossRef]
- Meijer, G.J.; Cune, M.S.; van Dooren, M.; de Putter, C.; van Blitterswijk, C.A. A comparative study of flexible (PolyactiveTM) versus rigid (hydroxylapatite) permucosal dental implants. I. Clinical aspects. J. Oral Rehabil. 1997, 24, 85–92. [Google Scholar] [CrossRef]
- Meijer, G.J.; Dalmeijer, R.A.; de Putter, C.; van Blitterswijk, C.A. A comparative study of flexible (PolyactiveTM) versus rigid (hydroxylapatite) permucosal dental implants. II. Histological aspects. J. Oral Rehabil. 1997, 24, 93–101. [Google Scholar] [CrossRef]
- Waris, E.; Ashammakhi, N.; Lehtimäki, M.; Tulamo, R.M.; Törmälä, P.; Kellomäki, M.; Konttinen, Y.T. Long-term bone tissue reaction to polyethylene oxide/polybutylene terephthalate copolymer (Polyactive®) in metacarpophalangeal joint reconstruction. Biomaterials 2008, 29, 2509–2515. [Google Scholar] [CrossRef]
- Svensson, A.; Nicklasson, E.; Harrah, T.; Panilaitis, B.; Kaplan, D.L.; Brittberg, M.; Gatenholm, P. Bacterial cellulose as a potential scaffold for tissue engineering of cartilage. Biomaterials 2005, 26, 419–431. [Google Scholar] [CrossRef]
- Rampinelli, G.; di Landro, L.; Fujii, T. Characterization of biomaterials based on microfibrillated cellulose with different modifications. J. Reinf. Plast. Compos. 2010, 29, 1793–1803. [Google Scholar] [CrossRef]
- Granja, P.L.; Barbosa, M.A.; Pouysége, L.; de Jéso, B.; Rouais, F.; Baquuey, C. Cellulose phosphates as biomaterials. Mineralization of chemically modified regenerated cellulose hydrogels. J. Mater. Sci. 2001, 36, 2163–2172. [Google Scholar] [CrossRef]
- Granja, P.L.; Jéso, B.D.; Bareille, R.; Rouais, F.; Baquey, C.; Barbosa, M.A. Cellulose phosphates as biomaterials. In vitro biocompatibility studies. React. Funct. Polym. 2006, 66, 728–739. [Google Scholar] [CrossRef]
- De Stefano, V.; Khan, S.; Tabada, A. Applications of PLA in modern medicine. Eng. Regen. 2020, 1, 76–87. [Google Scholar]
- Budak, K.; Sogut, O.; Sezer, U.A. A review on synthesis and biomedical applications of polyglycolic acid. J. Polym. Res. 2020, 27, 208. [Google Scholar] [CrossRef]
- Ashammakhi, N.; Rokkanen, P. Absorbable polyglycolide devices in trauma and bone surgery. Biomaterials 1997, 18, 3–9. [Google Scholar] [CrossRef]
- Boyan, B.; Lohmann, C.; Somers, A.; Neiderauer, G.; Wozney, J.; Dean, D.; Carnes, D.; Schwartz, Z. Potential of porous poly-D,L-lactide-co-glycolide particles as a carrier for recombinant human bone morphogenetic protein-2 during osteoinduction in vivo. J. Biomed. Mater. Res. 1999, 46, 51–59. [Google Scholar] [CrossRef]
- Gentile, P.; Chiono, V.; Carmagnola, I.; Hatton, P.V. An overview of poly(lactic-co-glycolic) acid (PLGA)-based biomaterials for bone tissue engineering. Int. J. Mol. Sci. 2014, 15, 3640–3659. [Google Scholar] [CrossRef]
- Kalirajan, C.; Dukle, A.; Nathanael, A.J.; Oh, T.H.; Manivasagam, G. A critical review on polymeric biomaterials for biomedical applications. Polymers 2021, 13, 3015. [Google Scholar] [CrossRef]
- Lacambra-Andreu, X.; Maazouz, A.; Lamnawar, K.; Chenal, J.M. A review on manufacturing processes of biocomposites based on poly(α-esters) and bioactive glass fillers for bone regeneration. Biomimetics 2023, 8, 81. [Google Scholar] [CrossRef]
- Ishuang, S.L.; Payne, R.G.; Yaszemski, M.J.; Aufdemorte, T.B.; Bizios, R.; Mikos, A.G. Osteoblast migration on poly(α-hydroxy esters). Biotechnol. Bioeng. 1996, 50, 443–451. [Google Scholar]
- Shikinami, Y.; Okuno, M. Bioresorbable devices made of forged composites of hydroxyapatite (HA) particles and poly-L-lactide (PLLA): Part I. Basic characteristics. Biomaterials 1999, 20, 859–877. [Google Scholar] [CrossRef]
- Khor, E.; Lim, L.Y. Implantable applications of chitin and chitosan. Biomaterials 2003, 24, 2339–2349. [Google Scholar] [CrossRef]
- Ali, A.; Ahmed, S. A review on chitosan and its nanocomposites in drug delivery. Int. J. Biol. Macromol. 2018, 109, 273–286. [Google Scholar] [CrossRef]
- Piskin, E.; Bölgen, N.; Egri, S.; Isoglu, I.A. Electrospun matrices made of poly(α-hydroxy acids) for medical use. Nanomedicine 2007, 2, 441–457. [Google Scholar] [CrossRef]
- Rezwana, K.; Chena, Q.Z.; Blakera, J.J.; Boccaccini, A.R. Biodegradable and bioactive porous polymer/inorganic composite scaffolds for bone tissue engineering. Biomaterials 2006, 27, 3413–3431. [Google Scholar] [CrossRef]
- Seal, B.L.; Otero, T.C.; Panitch, A. Polymeric biomaterials for tissue and organ regeneration. Mater. Sci. Eng. R 2001, 34, 147–230. [Google Scholar] [CrossRef]
- Mano, J.F.; Sousa, R.A.; Boesel, L.F.; Neves, N.M.; Reis, R.L. Bioinert, biodegradable and injectable polymeric matrix composites for hard tissue replacement: State of the art and recent developments. Compos. Sci. Technol. 2004, 64, 789–817. [Google Scholar] [CrossRef]
- de las Heras Alarcón, C.; Pennadam, S.; Alexander, C. Stimuli responsive polymers for biomedical applications. Chem. Soc. Rev. 2005, 34, 276–285. [Google Scholar] [CrossRef]
- Kohane, D.S.; Langer, R. Polymeric biomaterials in tissue engineering. Pediatr. Res. 2008, 63, 487–491. [Google Scholar] [CrossRef]
- Arzhakova, O.V.; Arzhakov, M.S.; Badamshina, E.R.; Bryuzgina, E.B.; Bryuzgin, E.V.; Bystrova, A.V.; Vaganov, G.V.; Vasilevskaya, V.V.; Vdovichenko, A.Y.; Gallyamov, M.O.; et al. Polymers for the future. Rus. Chem. Rev. 2022, 91, RCR5062. [Google Scholar] [CrossRef]
- Benalaya, I.; Alves, G.; Lopes, J.; Silva, L.R. A review of natural polysaccharides: Sources, characteristics, properties, food, and pharmaceutical applications. Int. J. Mol. Sci. 2024, 25, 1322. [Google Scholar] [CrossRef]
- Okada, M. Chemical syntheses of biodegradable polymers. Prog. Polym. Sci. 2002, 27, 87–133. [Google Scholar] [CrossRef]
- Jordan, J.; Jacob, K.I.; Tannenbaum, R.; Sharaf, M.A.; Jasiuk, I. Experimental trends in polymer nanocomposites—A review. Mater. Sci. Eng. A 2005, 393, 1–11. [Google Scholar] [CrossRef]
- Liu, X.; Chu, P.K.; Ding, C. Surface modification of titanium, titanium alloys and related materials for biomedical applications. Mater. Sci. Eng. R 2004, 47, 49–121. [Google Scholar] [CrossRef]
- Hanawa, T. Biofunctionalization of titanium for dental implant. Jpn. Dent. Sci. Rev. 2010, 46, 93–101. [Google Scholar] [CrossRef]
- Nasab, M.B.; Hassan, M.R.; Sahari, B.B. Metallic biomaterials of knee and hip—A review. Trends Biomater. Artif. Organ. 2010, 24, 69–82. [Google Scholar]
- Cheng, J.; Liu, B.; Wu, Y.H.; Zheng, Y.F. Comparative in vitro study on pure metals (Fe, Mn, Mg, Zn and W) as biodegradable metals. J. Mater. Sci. Technol. 2013, 29, 619–627. [Google Scholar] [CrossRef]
- Chen, Q.; Thouas, G.A. Metallic implant biomaterials. Mater. Sci. Eng. R 2015, 87, 1–57. [Google Scholar] [CrossRef]
- Ryan, G.; Pandit, A.; Apatsidis, D.P. Fabrication methods of porous metals for use in orthopaedic applications. Biomaterials 2006, 27, 2651–2670. [Google Scholar] [CrossRef]
- Levine, B. A new era in porous metals: Applications in orthopaedics. Adv. Eng. Mater. 2008, 10, 788–792. [Google Scholar] [CrossRef]
- Chen, C.; Zhang, M. Fabrication methods of porous tantalum metal implants for use as biomaterials. Adv. Mater. Res. 2012, 476–478, 2063–2066. [Google Scholar] [CrossRef]
- Ma, P.X. Biomimetic materials for tissue engineering. Adv. Drug Deliv. Rev. 2008, 60, 184–198. [Google Scholar] [CrossRef]
- Kathuria, Y.P. The potential of biocompatible metallic stents and preventing restenosis. Mater. Sci. Eng. A 2006, 417, 40–48. [Google Scholar] [CrossRef]
- Purnama, A.; Hermawan, H.; Couet, J.; Mantovani, D. Assessing the biocompatibility of degradable metallic materials: State-of-the-art and focus on the potential of genetic regulation. Acta Biomater. 2010, 6, 1800–1807. [Google Scholar] [CrossRef]
- Li, G.; Yang, H.; Zheng, Y.; Chen, X.H.; Yang, J.A.; Zhu, D.; Ruan, L.; Takashima, K. Challenges in the use of zinc and its alloys as biodegradable metals: Perspective from biomechanical compatibility. Acta Biomater. 2019, 97, 23–45. [Google Scholar] [CrossRef]
- Knowles, J.C. Phosphate based glasses for biomedical applications. J. Mater. Chem. 2003, 13, 2395–2401. [Google Scholar] [CrossRef]
- Tilocca, A. Current challenges in atomistic simulations of glasses for biomedical applications. Phys. Chem. Chem. Phys. 2014, 16, 3874–3880. [Google Scholar] [CrossRef]
- Kasuga, T. Development of phosphate glass-ceramics for biomedical applications. J. Ceram. Soc. Jpn. 2007, 115, 455–459. [Google Scholar] [CrossRef]
- Abdelghany, A.M.; El Batal, F.H.; El Batal, H.A. Zinc containing borate glasses and glass-ceramics: Search for biomedical applications. Process. Appl. Ceram. 2014, 8, 185–193. [Google Scholar] [CrossRef]
- Shearer, A.; Montazerian, M.; Mauro, J.C. Modern definition of bioactive glasses and glass-ceramics. J. Non-Cryst. Solids 2023, 608, 122228. [Google Scholar] [CrossRef]
- Hench, L.L. The story of Bioglass®. J. Mater. Sci. Mater. Med. 2006, 17, 967–978. [Google Scholar] [CrossRef]
- Jones, J.R. Review of bioactive glass: From Hench to hybrids. Acta Biomater. 2013, 9, 4457–4486. [Google Scholar] [CrossRef]
- Weizhong, Y.; Dali, Z.; Guangfu, Y. Research and development of A-W bioactive glass ceramic. J. Biomed. Eng. 2003, 20, 541–545. [Google Scholar]
- Li, G.; Zhou, D.; Xue, M.; Yang, W.; Long, Q.; Cao, B.; Feng, D. Study on the surface bioactivity of novel magnetic A-W glass ceramic in vitro. Appl. Surf. Sci. 2008, 255, 559–561. [Google Scholar] [CrossRef]
- Höland, W.; Schweiger, M.; Watzke, R.; Peschke, A.; Kappert, H. Ceramics as biomaterials for dental restoration. Expert Rev. Med. Dev. 2008, 5, 729–745. [Google Scholar] [CrossRef]
- Li, R.W.K.; Chow, T.W.; Matinlinna, J.P. Ceramic dental biomaterials and CAD/CAM technology: State of the art. J. Prosthodont. Res. 2014, 58, 208–216. [Google Scholar] [CrossRef]
- Ramesh, T.R.; Gangaiah, M.; Harish, P.V.; Krishnakumar, U.; Nandakishore, B. Zirconia ceramics as a dental biomaterial—An over view. Trends Biomater. Artif. Organs 2012, 26, 154–160. [Google Scholar]
- Wang, C.H.; Wang, M.C.; Du, J.K.; Sie, Y.Y.; Hsi, C.S.; Lee, H.E. Phase transformation and nanocrystallite growth behavior of 2 mol% yttria-partially stabilized zirconia (2Y-PSZ) powders. Ceram. Int. 2013, 39, 5165–5174. [Google Scholar] [CrossRef]
- Garvie, R.C. A personal history of the development of transformation toughened PSZ ceramics. J. Aust. Ceram. Soc. 2014, 50, 15–22. [Google Scholar]
- Benson, J. Elemental carbon as a biomaterial. J. Biomed. Mater. Res. 1972, 5, 41–47. [Google Scholar] [CrossRef]
- Olborska, A.; Swider, M.; Wolowiec, R.; Niedzielski, P.; Rylski, A.; Mitura, S. Amorphous carbon–biomaterial for implant coatings. Diam. Relat. Mater. 1994, 3, 899–901. [Google Scholar] [CrossRef]
- Saito, N.; Usui, Y.; Aoki, K.; Narita, N.; Shimizu, M.; Hara, K.; Ogiwara, N.; Nakamura, K.; Ishigaki, N.; Kato, H.; et al. Carbon nanotubes: Biomaterial applications. Chem. Soc. Rev. 2009, 38, 1897–1903. [Google Scholar] [CrossRef]
- Saito, N.; Haniu, H.; Usui, Y.; Aoki, K.; Hara, K.; Takanashi, S.; Shimizu, M.; Narita, N.; Okamoto, M.; Kobayashi, S.; et al. Safe clinical use of carbon nanotubes as innovative biomaterials. Chem. Rev. 2014, 114, 6040–6079. [Google Scholar] [CrossRef]
- Harrison, B.S.; Atala, A. Carbon nanotube applications for tissue engineering. Biomaterials 2007, 28, 344–353. [Google Scholar] [CrossRef]
- Saito, N.; Usui, Y.; Aoki, K.; Narita, N.; Shimizu, M.; Ogiwara, N.; Nakamura, K.; Ishigaki, N.; Kato, H.; Taruta, S. Carbon nanotubes for biomaterials in contact with bone. Curr. Med. Chem. 2008, 15, 523–527. [Google Scholar] [CrossRef]
- Ma, P.C.; Siddiqui, N.A.; Marom, G.; Kim, J.K. Dispersion and functionalization of carbon nanotubes for polymer-based nanocomposites: A review. Compos. Part A Appl. Sci. Manuf. 2010, 41, 1345–1367. [Google Scholar] [CrossRef]
- Kharissova, O.V.; González, C.M.O.; Kharisov, B.I. Solubilization and dispersion of carbon allotropes in water and non-aqueous solvents. Ind. Eng. Chem. Res. 2018, 57, 12624–12645. [Google Scholar] [CrossRef]
- Beuvelot, J.; Bergeret, C.; Mallet, R.; Fernandez, V.; Cousseau, J.; Baslé, M.F.; Chappard, D. In vitro calcification of chemically functionalized carbon nanotubes. Acta Biomater. 2010, 6, 4110–4117. [Google Scholar] [CrossRef]
- Vardharajula, S.; Ali, S.Z.; Tiwari, P.M.; Eroǧlu, E.; Vig, K.; Dennis, V.A.; Singh, S.R. Functionalized carbon nanotubes: Biomedical applications. Int. J. Nanomed. 2012, 7, 5361–5374. [Google Scholar]
- Partha, R.; Conyers, J.L. Biomedical applications of functionalized fullerene-based nanomaterials. Int. J. Nanomed. 2009, 4, 261–275. [Google Scholar]
- Xiao, Y.; Pang, Y.X.; Yan, Y.; Qian, P.; Zhao, H.; Manickam, S.; Wu, T.; Pang, C.H. Synthesis and functionalization of graphene materials for biomedical applications: Recent advances, challenges and perspectives. Adv. Sci. 2023, 10, 2205292. [Google Scholar] [CrossRef]
- Mathieu, L.M.; Bourban, P.E.; Manson, J.A.E. Processing of homogeneous ceramic/polymer blends for bioresorbable composites. Compos. Sci. Technol. 2006, 66, 1606–1614. [Google Scholar] [CrossRef]
- Nair, M.; Nancy, D.; Krishnan, A.G.; Anjusree, G.S.; Vadukumpully, S.; Nair, S.V. Graphene oxide nanoflakes incorporated gelatin-hydroxyapatite scaffolds enhance osteogenic differentiation of human mesenchymal stem cells. Nanotechnology 2015, 26, 161001. [Google Scholar] [CrossRef]
- Schappo, H.; Giry, K.; Salmoria, G.; Damia, C.; Hotza, D. Polymer/calcium phosphate biocomposites manufactured by selective laser sintering: An overview. Prog. Addit. Manuf. 2023, 8, 285–301. [Google Scholar] [CrossRef]
- Gao, X.; Wang, H.; Luan, S.; Zhou, G. Biofabrication of poly(aryletherketone)-hydroxyapatite composite scaffolds via low-temperature printing. Adv. Mater. Technol. 2023, 8, 2201676. [Google Scholar] [CrossRef]
- Soleymani, S.; Naghib, S.M. 3D and 4D printing hydroxyapatite-based scaffolds for bone tissue engineering and regeneration. Heliyon 2023, 9, e19363. [Google Scholar] [CrossRef]
- Pezzotti, G.; Asmus, S.M.F. Fracture behavior of hydroxyapatite/polymer interpenetrating network composites prepared by in situ polymerization process. Mater. Sci. Eng. A 2001, 316, 231–237. [Google Scholar] [CrossRef]
- Weickmann, H.; Gurr, M.; Meincke, O.; Thomann, R.; Mülhaupt, R. A versatile solvent-free “one-pot” route to polymer nanocomposites and the in situ formation of calcium phosphate/layered silicate hybrid nanoparticles. Adv. Funct. Mater. 2010, 20, 1778–1786. [Google Scholar] [CrossRef]
- Wei, G.; Gong, C.; Hu, K.; Wang, Y.; Zhang, Y. Biomimetic hydroxyapatite on graphene supports for biomedical applications: A review. Nanomaterials 2019, 9, 1435. [Google Scholar] [CrossRef]
- Boyapati, P.C.S.; Srinivas, K.; Akhil, S.; Bollikolla, H.B.; Chandu, B. A comprehensive review on novel graphene-hydroxyapatite nanocomposites for potential bioimplant applications. ChemistrySelect 2023, 8, e202204585. [Google Scholar] [CrossRef]
- Aryal, S.; Bhattarai, S.R.; Bahadur, K.C.R.; Khil, M.S.; Lee, D.R.; Kim, H.Y. Carbon nanotubes assisted biomimetic synthesis of hydroxyapatite from simulated body fluid. Mater. Sci. Eng. A 2006, 426, 202–207. [Google Scholar] [CrossRef]
- Kealley, C.; Ben-Nissan, B.; van Riessen, A.; Elcombe, M. Development of carbon nanotube reinforced hydroxyapatite bioceramics. Key Eng. Mater. 2006, 309–311, 597–602. [Google Scholar] [CrossRef]
- Kealley, C.; Elcombe, M.; van Riessen, A.; Ben-Nissan, B. Development of carbon nanotube reinforced hydroxyapatite bioceramics. Phys. B 2006, 385–386, 496–498. [Google Scholar] [CrossRef]
- Aryal, S.; Bahadur, K.C.R.; Dharmaraj, N.; Kim, K.W.; Kim, H.Y. Synthesis and characterization of hydroxyapatite using carbon nanotubes as a nano-matrix. Scr. Mater. 2006, 54, 131–135. [Google Scholar] [CrossRef]
- Kim, H.; Mondal, S.; Jang, B.; Manivasagan, P.; Moorthy, M.S.; Oh, J. Biomimetic synthesis of metal–hydroxyapatite (Au-HAp, Ag-HAp, Au-Ag-HAp): Structural analysis, spectroscopic characterization and biomedical application. Ceram. Int. 2018, 44, 20490–20500. [Google Scholar] [CrossRef]
- Rabadjieva, D.; Gergulova, R.; Ruseva, K.; Bonchev, A.; Shestakova, P.; Simeonov, M.; Vasileva, R.; Tatchev, D.; Titorenkova, R.; Vassileva, E. Polycarboxy/sulfo betaine–calcium phosphate hybrid materials with a remineralization potential. Materials 2023, 16, 6640. [Google Scholar] [CrossRef]
- Rautaray, D.; Mandal, S.; Sastry, M. Synthesis of hydroxyapatite crystals using amino acid-capped gold nanoparticles as a scaffold. Langmuir 2005, 21, 5185–5191. [Google Scholar] [CrossRef]
- Wang, X.J.; Li, Y.; Wei, J.; de Groot, K. Development of biomimetic nano-hydroxyapatite/poly(hexamethylene adipamide) composites. Biomaterials 2002, 23, 4787–4791. [Google Scholar] [CrossRef]
- Wei, J.; Li, Y. Tissue engineering scaffold material of nano-apatite crystals and polyamide composite. Eur. Polym. J. 2004, 40, 509–515. [Google Scholar]
- Memoto, R.; Nakamura, S.; Isobe, T.; Senna, M. Direct synthesis of hydroxyapatite-silk fibroin nano-composite sol via a mechano-chemical route. J. Sol Gel Sci. Technol. 2001, 21, 7–12. [Google Scholar]
- Yoshida, A.; Miyazaki, T.; Ashizuka, M.; Ishida, E. Bioactivity and mechanical properties of cellulose/carbonate hydroxyapatite composites prepared in situ through mechanochemical reaction. J. Biomater. Appl. 2006, 21, 179–194. [Google Scholar] [CrossRef]
- Fujiwara, M.; Shiokawa, K.; Morigaki, K.; Tatsu, Y.; Nakahara, Y. Calcium phosphate composite materials including inorganic powders, BSA or duplex DNA prepared by W/O/W interfacial reaction method. Mater. Sci. Eng. C 2008, 28, 280–288. [Google Scholar] [CrossRef]
- Nagata, F.; Miyajima, T.; Yokogawa, Y. A method to fabricate hydroxyapatite/poly(lactic acid) microspheres intended for biomedical application. J. Eur. Ceram. Soc. 2006, 26, 533–535. [Google Scholar] [CrossRef]
- Russias, J.; Saiz, E.; Nalla, R.K.; Tomsia, A.P. Microspheres as building blocks for hydroxyapatite/polylactide biodegradable composites. J. Mater. Sci. 2006, 41, 5127–5133. [Google Scholar] [CrossRef]
- Khan, Y.M.; Cushnie, E.K.; Kelleher, J.K.; Laurencin, C.T. In situ synthesized ceramic-polymer composites for bone tissue engineering: Bioactivity and degradation studies. J. Mater. Sci. 2007, 42, 4183–4190. [Google Scholar] [CrossRef]
- Liu, X.; Okada, M.; Maeda, H.; Fujii, S.; Furuzono, T. Hydroxyapatite/biodegradable poly(L-lactide-co-ε-caprolactone) composite microparticles as injectable scaffolds by a Pickering emulsion route. Acta Biomater. 2011, 7, 821–828. [Google Scholar] [CrossRef]
- Hu, Y.; Zou, S.; Chen, W.; Tong, Z.; Wang, C. Mineralization and drug release of hydroxyapatite/poly(L-lactic acid) nanocomposite scaffolds prepared by Pickering emulsion templating. Colloid Surface B 2014, 122, 559–565. [Google Scholar] [CrossRef]
- Kim, H.W.; Knowles, J.C.; Kim, H.E. Hydroxyapatite and gelatin composite foams processed via novel freeze-drying and crosslinking for use as temporary hard tissue scaffolds. J. Biomed. Mater. Res. A 2005, 72A, 136–145. [Google Scholar] [CrossRef]
- Mohandes, F.; Salavati-Niasari, M. Freeze-drying synthesis, characterization and in vitro bioactivity of chitosan/graphene oxide/hydroxyapatite nanocomposite. RSC Adv. 2014, 4, 25993–26001. [Google Scholar] [CrossRef]
- Sinha, A.; Das, G.; Sharma, B.K.; Roy, R.P.; Pramanick, A.K.; Nayar, S. Poly(vinyl alcohol)-hydroxyapatite biomimetic scaffold for tissue regeneration. Mater. Sci. Eng. C 2007, 27, 70–74. [Google Scholar] [CrossRef]
- Sugawara, A.; Yamane, S.; Akiyoshi, K. Nanogel-templated mineralization: Polymer-calcium phosphate hybrid nanomaterials. Macromol. Rapid Commun. 2006, 27, 441–446. [Google Scholar] [CrossRef]
- Liu, M.; Wang, Y.; Liu, X.; Wei, Q.; Bao, C.; Zhang, K. Comprehensive review on fabricating bioactive ceramic bone scaffold using vat photopolymerization. ACS Biomater. Sci. Eng. 2023, 9, 3032–3057. [Google Scholar] [CrossRef]
- Chu, C.; Zhu, J.; Yin, Z.; Wang, S. Hydroxyapatite-Ti functionally graded biomaterial fabricated by powder metallurgy. Mater. Sci. Eng. A 1999, 271, 95–100. [Google Scholar]
- Ul Haq, E.; Ahmed, F.; Rehman, F.U.; Channa, I.A.; Makhdoom, M.A.; Shahzad, J.; Shafiq, T.; Zain-ul-Abdein, M.; Shar, M.A.; Alhazaa, A. Synthesis and characterization of a titanium-based functionally graded material-structured biocomposite using powder metallurgy. ACS Omega 2023, 8, 28976–28983. [Google Scholar] [CrossRef]
- Escalera, C.H.; Figueroa, I.A.; Casas-Luna, M.; Rodríguez-Gómez, F.J.; Piña-Barba, C.; Montufar, E.B.; Čelko, L. Magnesium strengthening in 3D printed TCP scaffold composites. J. Compos. Sci. 2023, 7, 467. [Google Scholar] [CrossRef]
- Avila, J.D.; Stenberg, K.; Bose, S.; Bandyopadhyay, A. Hydroxyapatite reinforced Ti6Al4V composites for load-bearing implants. Acta Biomater. 2021, 123, 379–392. [Google Scholar] [CrossRef]
- Afrouzian, A.; Bandyopadhyay, A. 3D printed silicon nitride, alumina and hydroxyapatite ceramic reinforced Ti6Al4V composites–tailored microstructures to enhance bio-tribo-corrosion and antibacterial properties. J. Mech. Behav. Biomed. Mater. 2023, 144, 105973. [Google Scholar] [CrossRef]
- Juhasz, J.A.; Best, S.M. Bioactive ceramics: Processing, structures and properties. J. Mater. Sci. 2012, 47, 610–624. [Google Scholar] [CrossRef]
- Wang, S.F.; Zhang, J.; Luo, D.W.; Gu, F.; Tang, D.Y.; Dong, Z.L.; Tan, G.E.B.; Que, W.X.; Zhang, T.S.; Li, S.; et al. Transparent ceramics: Processing, materials and applications. Prog. Solid State Chem. 2013, 41, 20–54. [Google Scholar] [CrossRef]
- Mortensen, A.; Suresh, S. Functionally graded metals and metal-ceramic composites: Part 1 processing. Int. Mater. Rev. 1995, 40, 239–265. [Google Scholar] [CrossRef]
- Suresh, S.; Mortensen, A. Functionally graded metals and metal-ceramic composites: Part 2 thermomechanical behaviour. Int. Mater. Rev. 1997, 42, 85–116. [Google Scholar] [CrossRef]
- Travitzky, N. Processing of ceramic-metal composites. Adv. Appl. Ceram. 2012, 111, 286–300. [Google Scholar] [CrossRef]
- Dhandayuthapani, B.; Yoshida, Y.; Maekawa, T.; Kumar, D.S. Polymeric scaffolds in tissue engineering application: A review. Int. J. Polym. Sci. 2011, 2011, 290602. [Google Scholar] [CrossRef]
- Wang, W.; Zhang, B.; Li, M.; Li, J.; Zhang, C.; Han, Y.; Wang, L.; Wang, K.; Zhou, C.; Liu, L.; et al. 3D printing of PLA/n-HA composite scaffolds with customized mechanical properties and biological functions for bone tissue engineering. Compos. Part B Eng. 2021, 224, 109192. [Google Scholar] [CrossRef]
- Han, Y.; Wei, Q.; Chang, P.; Hu, K.; Okoro, O.V.; Shavandi, A.; Nie, L. Three-dimensional printing of hydroxyapatite composites for biomedical application. Crystals 2021, 11, 353. [Google Scholar] [CrossRef]
- Ojo, S.A.; Abere, D.V.; Adejo, H.O.; Robert, R.A.; Oluwasegun, K.M. Additive manufacturing of hydroxyapatite-based composites for bioengineering applications. Bioprinting 2023, 32, e00278. [Google Scholar] [CrossRef]
- Fuchs, A.; Bartolf-Kopp, M.; Böhm, H.; Straub, A.; Kübler, A.C.; Linz, C.; Gbureck, U. Composite grafts made of polycaprolactone fiber mats and oil-based calcium phosphate cement pastes for the reconstruction of cranial and maxillofacial defects. Clin. Oral Investig. 2023, 27, 3199–3209. [Google Scholar] [CrossRef]
- Baji, A.; Wong, S.C.; Srivatsan, T.S.; Njus, G.O.; Mathur, G. Processing methodologies for polycaprolactone-hydroxyapatite composites: A review. Mater. Manuf. Process. 2006, 21, 211–218. [Google Scholar] [CrossRef]
- Guan, L.; Davies, J.E. Preparation and characterization of a highly macroporous biodegradable composite tissue engineering scaffold. J. Biomed. Mater. Res. A 2004, 71A, 480–487. [Google Scholar] [CrossRef]
- Sun, F.; Zhou, H.; Lee, J. Various preparation methods of highly porous hydroxyapatite/polymer nanoscale biocomposites for bone regeneration. Acta Biomater. 2011, 7, 3813–3828. [Google Scholar] [CrossRef]
- Kumar, A.; Negi, Y.S.; Choudhary, V.; Bhardwaj, N.K. Microstructural and mechanical properties of porous biocomposite scaffolds based on polyvinyl alcohol, nano-hydroxyapatite and cellulose nanocrystals. Cellulose 2015, 21, 3409–3426. [Google Scholar] [CrossRef]
- Teng, X.R.; Ren, J.; Gu, S.Y. Preparation and characterization of porous PDLLA/HA composite foams by supercritical carbon dioxide technology. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 81B, 185–193. [Google Scholar] [CrossRef]
- Ren, J.; Zhao, P.; Ren, T.; Gu, S.; Pan, K. Poly (D,L-lactide)/nano-hydroxyapatite composite scaffolds for bone tissue engineering and biocompatibility evaluation. J. Mater. Sci. Mater. Med. 2008, 19, 1075–1082. [Google Scholar] [CrossRef]
- Yang, X.; Qi, D.; Xu, K.; Alimu, A.; Cao, L. Bio-compatible n-HAPs/polymer monolithic composites templated from CO2-in-water high internal phase emulsions. React. Funct. Polym. 2022, 181, 105417. [Google Scholar] [CrossRef]
- Ohji, T.; Fukushima, M. Macro-porous ceramics: Processing and properties. Int. Mater. Rev. 2012, 57, 115–131. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Calcium orthophosphate (CaPO4)-based bioceramics: Preparation, properties and applications. Coatings 2022, 12, 1380. [Google Scholar] [CrossRef]
- Babilotte, J.; Guduric, V.; le Nihouannen, D.; Naveau, A.; Fricain, J.C.; Catros, S. 3D printed polymer-mineral composite biomaterials for bone tissue engineering: Fabrication and characterization. J. Biomed. Mater. Res. B Appl. Biomater. 2019, 107B, 2579–2595. [Google Scholar] [CrossRef]
- Converse, G.L.; Yue, W.; Roeder, R.K. Processing and tensile properties of hydroxyapatite-whisker-reinforced polyetheretherketone. Biomaterials 2007, 28, 927–935. [Google Scholar] [CrossRef]
- Converse, G.L.; Roeder, R.K. Tensile properties of hydroxyapatite whisker reinforced polyetheretherketone. Mater. Res. Soc. Symp. Proc. 2005, 898, 44–49. [Google Scholar] [CrossRef]
- Zhang, H.; Darvell, B.W. Failure and behavior in water of hydroxyapatite whisker-reinforced bis-GMA-based resin composites. J. Mech. Behav. Biomed. Mater. 2012, 10, 39–47. [Google Scholar] [CrossRef]
- Liu, F.W.; Bao, S.; Jin, Y.; Jiang, X.Z.; Zhu, M.F. Novel bionic dental resin composite reinforced by hydroxyapatite whisker. Mater. Res. Innov. 2014, 18, S4854–S4858. [Google Scholar] [CrossRef]
- Nouri-Felekori, M.; Mesgar, A.S.M.; Mohammadi, Z. Development of composite scaffolds in the system of gelatin–calcium phosphate whiskers/fibrous spherulites for bone tissue engineering. Ceram. Int. 2015, 41, 6013–6019. [Google Scholar] [CrossRef]
- Watanabe, T.; Ban, S.; Ito, T.; Tsuruta, S.; Kawai, T.; Nakamura, H. Biocompatibility of composite membrane consisting of oriented needle-like apatite and biodegradable copolymer with soft and hard tissues in rats. Dental Mater. J. 2004, 23, 609–612. [Google Scholar] [CrossRef]
- Li, H.; Chen, Y.; Xie, Y. Photo-crosslinking polymerization to prepare polyanhydride/needle-like hydroxyapatite biodegradable nanocomposite for orthopedic application. Mater. Lett. 2003, 57, 2848–2854. [Google Scholar] [CrossRef]
- Nejati, E.; Firouzdor, V.; Eslaminejad, M.B.; Bagheri, F. Needle-like nano hydroxyapatite/poly(L-lactide acid) composite scaffold for bone tissue engineering application. Mater. Sci. Eng. C 2009, 29, 942–949. [Google Scholar] [CrossRef]
- Sun, S.P.; Wei, M.; Olson, J.R.; Shaw, M.T. A modified pultrusion process for preparing composites reinforced with continuous fibers and aligned hydroxyapatite nano needles. Polym. Compos. 2015, 36, 931–938. [Google Scholar] [CrossRef]
- Kasuga, T.; Ota, Y.; Nogami, M.; Abe, Y. Preparation and mechanical properties of polylactic acid composites containing hydroxyapatite fibers. Biomaterials 2000, 22, 19–23. [Google Scholar] [CrossRef]
- Smith, L. Ceramic-plastic material as a bone substitute. Arch. Surg. 1963, 87, 653–661. [Google Scholar] [CrossRef]
- Bonfield, W.; Grynpas, M.D.; Tully, A.E.; Bowman, J.; Abram, J. Hydroxyapatite reinforced polyethylene—A mechanically compatible implant material for bone replacement. Biomaterials 1981, 2, 185–189. [Google Scholar] [CrossRef]
- Bonfield, W.; Bowman, J.; Grynpas, M.D. Composite Material for Use in Orthopaedics. UK Patent 8032647, 9 October 1981. [Google Scholar]
- Bonfield, W. Composites for bone replacement. J. Biomed. Eng. 1988, 10, 522–526. [Google Scholar] [CrossRef]
- Guild, F.J.; Bonfield, W. Predictive character of hydroxyapatite-polyethelene HAPEXTM composite. Biomaterials 1993, 14, 985–993. [Google Scholar] [CrossRef]
- Wang, M.; Joseph, R.; Bonfield, W. Hydroxyapatite-polyethylene composites for bone substitution: Effect of ceramic particle size and morphology. Biomaterials 1998, 19, 2357–2366. [Google Scholar] [CrossRef]
- Nazhat, S.N.; Joseph, R.; Wang, M.; Smith, R.; Tanner, K.E.; Bonfield, W. Dynamic mechanical characterisation of hydroxyapatite reinforced polyethylene: Effect of particle size. J. Mater. Sci. Mater. Med. 2000, 11, 621–628. [Google Scholar] [CrossRef]
- Guild, F.J.; Bonfield, W. Predictive modelling of the mechanical properties and failure processes of hydroxyapatite-polyethylene (HAPEXTM) composite. J. Mater. Sci. Mater. Med. 1998, 9, 497–502. [Google Scholar] [CrossRef]
- Wang, M.; Ladizesky, N.H.; Tanner, K.E.; Ward, I.M.; Bonfield, W. Hydrostatically extruded HAPEXTM. J. Mater. Sci. 2000, 35, 1023–1030. [Google Scholar] [CrossRef]
- Bonner, M.; Saunders, L.S.; Ward, I.M.; Davies, G.W.; Wang, M.; Tanner, K.E.; Bonfield, W. Anisotropic mechanical properties of oriented HAPEXTM. J. Mater. Sci. 2002, 37, 325–334. [Google Scholar] [CrossRef]
- di Silvio, L.; Dalby, M.J.; Bonfield, W. Osteoblast behaviour on HA/PE composite surfaces with different HA volumes. Biomaterials 2002, 23, 101–107. [Google Scholar] [CrossRef]
- Dalby, M.J.; Kayser, M.V.; Bonfield, W.; di Silvio, L. Initial attachment of osteoblasts to an optimised HAPEXTM topography. Biomaterials 2002, 23, 681–690. [Google Scholar] [CrossRef]
- Zhang, Y.; Tanner, K.E.; Gurav, N.; di Silvio, L. In vitro osteoblastic response to 30 vol% hydroxyapatite-polyethylene composite. J. Biomed. Mater. Res. A 2007, 81A, 409–417. [Google Scholar] [CrossRef]
- Rea, S.M.; Brooks, R.A.; Schneider, A.; Best, S.M.; Bonfield, W. Osteoblast-like cell response to bioactive composites-surface-topography and composition effects. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 70B, 250–261. [Google Scholar] [CrossRef]
- Hench, L.L.; Wilson, J. Surface-active biomaterials. Science 1984, 226, 630–636. [Google Scholar] [CrossRef]
- Salernitano, E.; Migliaresi, C. Composite materials for biomedical applications: A review. J. Appl. Biomater. Biomech. 2003, 1, 3–18. [Google Scholar]
- Pandey, A.; Jan, E.; Aswath, P.B. Physical and mechanical behavior of hot rolled HDPE/HA composites. J. Mater. Sci. 2006, 41, 3369–3376. [Google Scholar] [CrossRef]
- Bonner, M.; Ward, I.M.; McGregor, W.; Tanner, K.E.; Bonfield, W. Hydroxyapatite/polypropylene composite: A novel bone substitute material. J. Mater. Sci. Lett. 2001, 20, 2049–2052. [Google Scholar] [CrossRef]
- Suppakarn, N.; Sanmaung, S.; Ruksakulpiwa, Y.; Sutapun, W. Effect of surface modification on properties of natural hydroxyapatite/polypropylene composites. Key Eng. Mater. 2008, 361–363, 511–514. [Google Scholar]
- Younesi, M.; Bahrololoom, M.E. Formulating the effects of applied temperature and pressure of hot pressing process on the mechanical properties of polypropylene-hydroxyapatite bio-composites by response surface methodology. Mater. Des. 2010, 31, 4621–4630. [Google Scholar] [CrossRef]
- Younesi, M.; Bahrololoom, M.E. Effect of polypropylene molecular weight, hydroxyapatite particle size and Ringer’s solution on creep and impact behavior of polypropylene-surface treated hydroxyapatite biocomposites. J. Compos. Mater. 2011, 45, 513–523. [Google Scholar] [CrossRef]
- Sousa, R.A.; Reis, R.L.; Cunha, A.M.; Bevis, M.J. Processing and properties of bone-analogue biodegradable and bioinert polymeric composites. Compos. Sci. Technol. 2003, 63, 389–402. [Google Scholar] [CrossRef]
- Wang, M.; Deb, S.; Bonfield, W. Chemically coupled hydroxyapatite-polyethylene composites: Processing and characterisation. Mater. Lett. 2000, 44, 119–124. [Google Scholar] [CrossRef]
- Wang, M.; Bonfield, W. Chemically coupled hydroxyapatite-polyethylene composites: Structure and properties. Biomaterials 2001, 22, 1311–1320. [Google Scholar] [CrossRef]
- Homaeigohar, S.S.; Shokrgozar, M.A.; Khavandi, A.; Sadi, A.Y. In vitro biological evaluation of β-TCP/HDPE—A novel orthopedic composite: A survey using human osteoblast and fibroblast bone cells. J. Biomed. Mater. Res. A 2008, 84A, 491–499. [Google Scholar] [CrossRef]
- Sadi, A.Y.; Homaeigohar, S.S.; Khavandi, A.R.; Javadpour, J. The effect of partially stabilized zirconia on the mechanical properties of the hydroxyapatite-polyethylene composites. J. Mater. Sci. Mater. Med. 2004, 15, 853–858. [Google Scholar] [CrossRef]
- Nath, S.; Bodhak, S.; Basu, B. HDPE-Al2O3-HAp composites for biomedical applications: Processing and characterizations. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 88B, 1–11. [Google Scholar] [CrossRef]
- Downes, R.N.; Vardy, S.; Tanner, K.E.; Bonfield, W. Hydroxyapatite-polyethylene composite in orbital surgery. Bioceramics 4. In Proceedings of the 4th International Symposium on Ceramics in Medicine, London, UK, 11–13 September 1991; pp. 239–246. [Google Scholar]
- Bonfield, W.; Tanner, E. Hydroxyapatite composite biomaterials–evolution and applications. Mater. World 1997, 5, 18–20. [Google Scholar]
- Dornhoffer, H.L. Hearing results with the dornhoffer ossicular replacement prostheses. Laryngoscope 1998, 108, 531–536. [Google Scholar] [CrossRef]
- Swain, R.E.; Wang, M.; Beale, B.; Bonfield, W. HAPEXTM for otologic applications. Biomed. Eng. Appl. Basis Commun. 1999, 11, 315–320. [Google Scholar]
- Reis, R.L.; Cunha, A.M.; Oliveira, M.J.; Campos, A.R.; Bevis, M.J. Relationship between processing and mechanical properties of injection molded high molecular mass polyethylene + hydroxyapatite composites. Mater. Res. Inn. 2001, 4, 263–272. [Google Scholar] [CrossRef]
- Sousa, R.A.; Reis, R.L.; Cunha, A.M.; Bevis, M.J. Structure development and interfacial interactions in high-density polyethylene/hydroxyapatite (HDPE/HA) composites molded with preferred orientation. J. Appl. Polym. Sci. 2002, 86, 2873–2886. [Google Scholar] [CrossRef]
- Yi, Z.; Li, Y.; Jidong, L.; Xiang, Z.; Hongbing, L.; Yuanyuan, W.; Weihu, Y. Novel bio-composite of hydroxyapatite reinforced polyamide and polyethylene: Composition and properties. Mater. Sci. Eng. A 2007, 452–453, 512–517. [Google Scholar]
- Unwin, A.P.; Ward, I.M.; Ukleja, P.; Weng, J. The role of pressure annealing in improving the stiffness of polyethylene/hydroxyapatite composites. J. Mater. Sci. 2001, 36, 3165–3177. [Google Scholar] [CrossRef]
- Fang, L.M.; Leng, Y.; Gao, P. Processing and mechanical properties of HA/UHMWPE nanocomposites. Biomaterials 2006, 27, 3701–3707. [Google Scholar] [CrossRef]
- Fang, L.M.; Gao, P.; Leng, Y. High strength and bioactive hydroxyapatite nano-particles reinforced ultrahigh molecular weight polyethylene. Compos. B 2007, 38, 345–351. [Google Scholar] [CrossRef]
- Mirsalehi, S.A.; Khavandi, A.; Mirdamadi, S.; Naimi-Jamal, M.R.; Kalantari, S.M. Nanomechanical and tribological behavior of hydroxyapatite reinforced ultrahigh molecular weight polyethylene nanocomposites for biomedical applications. J. Appl. Polym. Sci. 2015, 132, 42052. [Google Scholar] [CrossRef]
- Ramakrishna, S.; Mayer, J.; Wintermantel, E.; Leong, K.W. Biomedical applications of polymer-composite materials: A review. Compos. Sci. Technol. 2001, 61, 1189–1224. [Google Scholar] [CrossRef]
- Donners, J.J.J.M.; Nolte, R.J.M.; Sommerdijk, N.A.J.M. Dendrimer-based hydroxyapatite composites with remarkable materials properties. Adv. Mater. 2003, 15, 313–316. [Google Scholar] [CrossRef]
- Schneider, O.D.; Stepuk, A.; Mohn, D.; Luechinger, N.A.; Feldman, K.; Stark, W.J. Light-curable polymer/calcium phosphate nanocomposite glue for bone defect treatment. Acta Biomater. 2010, 6, 2704–2710. [Google Scholar] [CrossRef]
- Ignjatovic, N.L.; Plavsic, M.; Miljkovic, M.S.; Zivkovic, L.M.; Uskokovic, D.P. Microstructural characteristics of calcium hydroxyapatite/poly-L-lactide based composites. J. Microsc. 1999, 196, 243–248. [Google Scholar] [CrossRef]
- Skrtic, D.; Antonucci, J.M.; Eanes, E.D. Amorphous calcium phosphate-based bioactive polymeric composites for mineralized tissue regeneration. J. Res. Natl. Inst. Stand. Technol. 2003, 108, 167–182. [Google Scholar] [CrossRef]
- Rizzi, S.C.; Heath, D.J.; Coombes, A.G.A.; Bock, N.; Textor, M.; Downes, S. Biodegradable polymer/hydroxyapatite composites: Surface analysis and initial attachment of human osteoblasts. J. Biomed. Mater. Res. 2001, 55, 475–486. [Google Scholar] [CrossRef]
- Navarro, M.; Planell, J.A. Bioactive composites based on calcium phosphates for bone regeneration. Key Eng. Mater. 2010, 441, 203–233. [Google Scholar] [CrossRef]
- Zhang, R.Y.; Ma, P.X. Porous poly(L-lactic acid)/apatite composites created by biomimetic process. J. Biomed. Mater. Res. 1999, 45, 285–293. [Google Scholar] [CrossRef]
- Liu, Q.; de Wijn, J.R.; van Blitterswijk, C.A. Composite biomaterials with chemical bonding between hydroxyapatite filler particles and PEG/PBT copolymer matrix. J. Biomed. Mater. Res. 1998, 40, 490–497. [Google Scholar] [CrossRef]
- Cerrai, P.; Guerra, G.D.; Tricoli, M.; Krajewski, A.; Ravaglioli, A.; Martinetti, R.; Dolcini, L.; Fini, M.; Scarano, A.; Piattelli, A. Periodontal membranes from composites of hydroxyapatite and bioresorbable block copolymers. J. Mater. Sci. Mater. Med. 1999, 10, 677–682. [Google Scholar] [CrossRef]
- Roeder, R.K.; Sproul, M.M.; Turner, C.H. Hydroxyapatite whiskers provide improved mechanical properties in reinforced polymer composites. J. Biomed. Mater. Res. A 2003, 67A, 801–812. [Google Scholar] [CrossRef]
- Wagoner Johnson, A.J.; Herschler, B.A. A review of the mechanical behavior of CaP and CaP/polymer composites for applications in bone replacement and repair. Acta Biomater. 2011, 7, 16–30. [Google Scholar] [CrossRef]
- Hutmacher, D.W. Scaffolds in tissue engineering bone and cartilage. Biomaterials 2000, 21, 2529–2543. [Google Scholar] [CrossRef]
- Owji, N.; Mandakhbayar, N.; Cha, J.R.; Padalhin, A.R.; Erdogan, Z.K.; Aldaadaa, A.; Shakouri, T.; Sawadkar, P.; Frost, O.; Kim, H.W.; et al. Inclusion of calcium phosphate does not further improve in vitro and in vivo osteogenesis in a novel, highly biocompatible, mechanically stable and 3D printable polymer. Sci. Rep. 2022, 12, 16977. [Google Scholar] [CrossRef]
- Wang, M.; Yue, C.Y.; Chua, B. Production and evaluation of hydroxyapatite reinforced polysulfone for tissue replacement. J. Mater. Sci. Mater. Med. 2001, 12, 821–826. [Google Scholar] [CrossRef]
- Chlopek, J.; Rosol, P.; Morawska-Chochol, A. Durability of polymer-ceramics composite implants determined in creep tests. Compos. Sci. Technol. 2006, 66, 1615–1622. [Google Scholar] [CrossRef]
- Robinson, P.; Wilson, C.; Mecholsky, J. Processing and mechanical properties of hydroxyapatite-polysulfone laminated composites. J. Eur. Ceram. Soc. 2014, 34, 1387–1396. [Google Scholar] [CrossRef]
- Xu, F.; Li, Y.; Yao, X.; Liao, H.; Zhang, L. Preparation and in vivo investigation of artificial cornea made of nano-hydroxyapatite/poly(vinyl alcohol) hydrogel composite. J. Mater. Sci. Mater. Med. 2007, 18, 635–640. [Google Scholar]
- Xu, F.; Li, Y.; Deng, Y.; Xiong, G. Porous nano-hydroxyapatite/poly(vinyl alcohol) composite hydrogel as artificial cornea fringe: Characterization and evaluation in vitro. J. Biomater. Sci. Polym. Edn. 2008, 19, 431–439. [Google Scholar] [CrossRef]
- Poursamar, S.A.; Orang, F.; Bonakdar, S.; Savar, M.K. Preparation and characterisation of poly vinyl alcohol/hydroxyapatite nanocomposite via in situ synthesis: A potential material as bone tissue engineering scaffolds. Int. J. Nanomanuf. 2010, 5, 330–334. [Google Scholar] [CrossRef]
- Timofejeva, A.; Loca, D. Hydroxyapatite/polyvinyl alcohol composite hydrogels for bone and cartilage tissue engineering. Key Eng. Mater. 2018, 762, 54–58. [Google Scholar] [CrossRef]
- Pramanik, N.; Biswas, S.K.; Pramanik, P. Synthesis and characterization of hydroxyapatite/poly(vinyl alcohol phosphate) nanocomposite biomaterials. Int. J. Appl. Ceram. Technol. 2008, 5, 20–28. [Google Scholar] [CrossRef]
- Bigi, A.; Boanini, E.; Gazzano, M.; Rubini, K. Structural and morphological modifications of hydroxyapatite-polyaspartate composite crystals induced by heat treatment. Cryst. Res. Technol. 2005, 40, 1094–1098. [Google Scholar] [CrossRef]
- Bertoni, E.; Bigi, A.; Falini, G.; Panzavolta, S.; Roveri, N. Hydroxyapatite polyacrylic acid nanocrystals. J. Mater. Chem. 1999, 9, 779–782. [Google Scholar] [CrossRef]
- Qiu, H.J.; Yang, J.; Kodali, P.; Koh, J.; Ameer, G.A. A citric acid-based hydroxyapatite composite for orthopedic implants. Biomaterials 2006, 27, 5845–5854. [Google Scholar] [CrossRef]
- Greish, Y.E.; Brown, P.W. Chemically formed HAp-Ca poly(vinyl phosphonate) composites. Biomaterials 2001, 22, 807–816. [Google Scholar] [CrossRef]
- Greish, Y.E.; Brown, P.W. Formation and properties of hydroxyapatite-calcium poly(vinyl phosphonate) composites. J. Am. Ceram. Soc. 2002, 85, 1738–1744. [Google Scholar] [CrossRef]
- Sailaja, G.S.; Velayudhan, S.; Sunny, M.C.; Sreenivasan, K.; Varma, H.K.; Ramesh, P. Hydroxyapatite filled chitosan-polyacrylic acid polyelectrolyte complexes. J. Mater. Sci. 2003, 38, 3653–3662. [Google Scholar] [CrossRef]
- Piticescu, R.M.; Chitanu, G.C.; Albulescu, M.; Giurginca, M.; Popescu, M.L.; Łojkowski, W. Hybrid HAp-maleic anhydride copolymer nanocomposites obtained by in-situ functionalisation. Solid State Phenom. 2005, 106, 47–56. [Google Scholar] [CrossRef]
- Song, J.; Saiz, E.; Bertozzi, C.R. A new approach to mineralization of biocompatible hydrogel scaffolds: An efficient process toward 3-dimensional bonelike composites. J. Am. Chem. Soc. 2003, 125, 1236–1243. [Google Scholar] [CrossRef]
- Kutikov, A.B.; Song, J. An amphiphilic degradable polymer/hydroxyapatite composite with enhanced handling characteristics promotes osteogenic gene expression in bone marrow stromal cells. Acta Biomater. 2013, 9, 8354–8364. [Google Scholar] [CrossRef]
- Wu, S.; Wang, J.; Zou, L.; Jin, L.; Wang, Z.; Li, Y. A three-dimensional hydroxyapatite/polyacrylonitrile composite scaffold designed for bone tissue engineering. RSC Adv. 2018, 8, 1730–1736. [Google Scholar] [CrossRef]
- Borkowski, L.; Lübek, T.; Jojczuk, M.; Nogalski, A.; Belcarz, A.; Hajnos, M.; Ginalska, G. Behavior of new hydroxyapatite/glucan composite in human serum. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106B, 2653–2664. [Google Scholar] [CrossRef]
- Abu Bakar, M.S.; Cheng, M.H.W.; Tang, S.M.; Yu, S.C.; Liao, K.; Tan, C.T.; Khor, K.A.; Cheang, P. Tensile properties, tension-tension fatigue and biological response of polyetheretherketone-hydroxyapatite composites for load-bearing orthopedic implants. Biomaterials 2003, 24, 2245–2250. [Google Scholar] [CrossRef]
- Abu Bakar, M.S.; Cheang, P.; Khor, K.A. Mechanical properties of injection molded hydroxyapatite-polyetheretherketone biocomposites. Compos. Sci. Technol. 2003, 63, 421–425. [Google Scholar] [CrossRef]
- Fan, J.P.; Tsui, C.P.; Tang, C.Y. Modeling of the mechanical behavior of HA/PEEK biocomposite under quasi-static tensile load. Mater. Sci. Eng. A 2004, 382, 341–350. [Google Scholar] [CrossRef]
- Chan, K.W.; Liao, C.Z.; Wong, H.M.; Yeung, K.W.K.; Tjong, S.C. Preparation of polyetheretherketone composites with nanohydroxyapatite rods and carbon nanofibers having high strength, good biocompatibility and excellent thermal stability. RSC Adv. 2016, 6, 19417–19429. [Google Scholar] [CrossRef]
- Qi, D.; Wang, N.; Wang, S.; Liu, L.; Zhu, S.; She, P.; Yue, X. High-strength porous polyetheretherketone/hydroxyapatite composite for the treatment of bone defect. Compos. Comm. 2023, 38, 101473. [Google Scholar] [CrossRef]
- Li, S.; Li, G.; Lian, X.; Hu, J.; Li, M.; Wang, B.; Zou, Y.; Zhou, Z. Integrated porous polyetheretherketone/hydroxyapatite scaffolds: Design, manufacturing and performance evaluation. Compos. Part A—Appl. Sci. 2023, 173, 107656. [Google Scholar] [CrossRef]
- Gong, X.H.; Tang, C.Y.; Hu, H.C.; Zhou, X.P. Improved mechanical properties of HIPS/hydroxyapatite composites by surface modification of hydroxyapatite via in situ polymerization of styrene. J. Mater. Sci. Mater. Med. 2004, 15, 1141–1146. [Google Scholar] [CrossRef]
- Fu, G.; Xia, Z.; Jiang, J.; Jing, B.; Zhang, X. Fabrication and characterization of nanocomposites with high-impact polystyrene and hydroxyapatite with well-defined polystyrene via ATRP. J. Reinf. Plast. Comp. 2011, 30, 1445–1453. [Google Scholar] [CrossRef]
- Petricca, S.E.; Marra, K.G.; Kumta, P.N. Chemical synthesis of poly(lactic-co-glycolic acid)/hydroxyapatite composites for orthopaedic applications. Acta Biomater. 2006, 2, 277–286. [Google Scholar] [CrossRef]
- Zhou, H.; Lawrence, J.G.; Bhaduri, S.B. Fabrication aspects of PLA-CaP/PLGA-CaP composites for orthopedic applications: A review. Acta Biomater. 2012, 8, 1999–2016. [Google Scholar] [CrossRef]
- Hoekstra, J.W.M.; Ma, J.; Plachokova, A.S.; Bronkhorst, E.M.; Bohner, M.; Pan, J.; Meijer, G.J.; Jansen, J.A.; van den Beucken, J.J.J.P. The in vivo performance of CaP/PLGA composites with varied PLGA microsphere sizes and inorganic compositions. Acta Biomater. 2013, 9, 7518–7526. [Google Scholar] [CrossRef]
- Leung, L.H.; Naguib, H.E. Characterizing the viscoelastic behaviour of poly(lactide-co-glycolide acid)–hydroxyapatite foams. J. Cell. Plast. 2013, 49, 497–505. [Google Scholar] [CrossRef]
- Fisher, P.D.; Venugopal, G.; Milbrandt, T.A.; Hilt, J.Z.; Puleo, D.A. Hydroxyapatite-reinforced in situ forming PLGA systems for intraosseous injection. J. Biomed. Mater. Res. A 2015, 103A, 2365–2373. [Google Scholar] [CrossRef]
- Athanasiou, K.A.; Schmitz, J.P.; Agrawal, C.M. The effects of porosity on in vitro degradation of polylactic acid–polyglycolic acid implants used in repair of articular cartilage. Tissue Eng. 1998, 4, 53–63. [Google Scholar] [CrossRef]
- Verheyen, C.C.P.M.; Klein, C.P.A.T.; de Blieck-Hogervorst, J.M.A.; Wolke, J.G.C.; de Wijin, J.R.; van Blitterswijk, C.A.; de Groot, K. Evaluation of hydroxylapatite poly(L-lactide) composites: Physico-chemical properties. J. Mater. Sci. Mater. Med. 1993, 4, 58–65. [Google Scholar] [CrossRef]
- Agrawal, C.M.; Athanasiou, K.A. Technique to control pH in vicinity of biodegrading PLA-PGA implants. J. Biomed. Mater. Res. Appl. Biomater. 1997, 38, 105–114. [Google Scholar] [CrossRef]
- Li, H.; Chang, J. pH-compensation effect of bioactive inorganic fillers on the degradation of PLGA. Compos. Sci. Technol. 2005, 65, 2226–2232. [Google Scholar] [CrossRef]
- Peter, S.J.; Miller, S.T.; Zhu, G.; Yasko, A.W.; Mikos, A.G. In vivo degradation of a poly(propylene fumarate)/β-tricalcium phosphate injectable composite scaffold. J. Biomed. Mater. Res. 1998, 41, 1–7. [Google Scholar] [CrossRef]
- Ara, M.; Watanabe, M.; Imai, Y. Effect of blending calcium compounds on hydrolitic degradation of poly(D,L-lactic acid-co-glycolic acid). Biomaterials 2002, 23, 2479–2483. [Google Scholar] [CrossRef]
- Schiller, C.; Epple, M. Carbonated apatites can be used as pH-stabilizing filler for biodegradable polyesters. Biomaterials 2003, 24, 2037–2043. [Google Scholar] [CrossRef]
- Schiller, C.; Rasche, C.; Wehmöller, M.; Beckmann, F.; Eufinger, H.; Epple, M.; Weihe, S. Geometrically structured implants for cranial reconstruction made of biodegradable polyesters and calcium phosphate/calcium carbonate. Biomaterials 2004, 25, 1239–1247. [Google Scholar] [CrossRef]
- Shikinami, Y.; Okuno, M. Bioresorbable devices made of forged composites of hydroxyapatite (HA) particles and poly L-lactide (PLLA). Part II: Practical properties of miniscrews and miniplates. Biomaterials 2001, 22, 3197–3211. [Google Scholar] [CrossRef]
- Russias, J.; Saiz, E.; Nalla, R.K.; Gryn, K.; Ritchie, R.O.; Tomsia, A.P. Fabrication and mechanical properties of PLA/HA composites: A study of in vitro degradation. Mater. Sci. Eng. C 2006, 26, 1289–1295. [Google Scholar] [CrossRef]
- Akagi, H.; Iwata, M.; Ichinohe, T.; Amimoto, H.; Hayashi, Y.; Kannno, N.; Ochi, H.; Fujita, Y.; Harada, Y.; Tagawa, M.; et al. Hydroxyapatite/poly-L-lactide acid screws have better biocompatibility and femoral burr hole closure than does poly-L-lactide acid alone. J. Biomater. Appl. 2014, 28, 954–962. [Google Scholar] [CrossRef]
- Pérez-Davila, S.; Garrido-Gulías, N.; González-Rodríguez, L.; López-Álvarez, M.; Serra, J.; López-Periago, J.E.; González, P. Physicochemical properties of 3D-printed polylactic acid/hydroxyapatite scaffolds. Polymers 2023, 15, 2849. [Google Scholar] [CrossRef]
- Kim, H.W.; Lee, H.H.; Knowles, J.C. Electrospinning biomedical nanocomposite fibers of hydroxyapaite/poly(lactic acid) for bone regeneration. J. Biomed. Mater. Res. A 2006, 79A, 643–649. [Google Scholar] [CrossRef]
- Gross, K.A.; Rodríguez-Lorenzo, L.M. Biodegradable composite scaffolds with an interconnected spherical network for bone tissue engineering. Biomaterials 2004, 25, 4955–4962. [Google Scholar] [CrossRef]
- Zhang, H.; Chen, Z. Fabrication and characterization of electrospun PLGA/MWNTs/hydroxyapatite biocomposite scaffolds for bone tissue engineering. J. Bioact. Compat. Polym. 2010, 25, 241–259. [Google Scholar] [CrossRef]
- Durucan, C.; Brown, P.W. Low temperature formation of calcium-deficient hydroxyapatite-PLA/PLGA composites. J. Biomed. Mater. Res. 2000, 51, 717–725. [Google Scholar] [CrossRef]
- Durucan, C.; Brown, P.W. Calcium-deficient hydroxyapatite-PLGA composites: Mechanical and microstructural investigation. J. Biomed. Mater. Res. 2000, 51, 726–734. [Google Scholar] [CrossRef]
- Durucan, C.; Brown, P.W. Biodegradable hydroxyapatite-polymer composites. Adv. Eng. Mater. 2001, 3, 227–231. [Google Scholar] [CrossRef]
- Nazhat, S.N.; Kellomäki, M.; Törmälä, P.; Tanner, K.E.; Bonfield, W. Dynamic mechanical characterization of biodegradable composites of hydroxyapatite and polylactides. J. Biomed. Mater. Res. 2001, 58, 335–343. [Google Scholar] [CrossRef]
- Ignjatovic, N.; Suljovrujic, E.; Biudinski-Simendic, J.; Krakovsky, I.; Uskokovic, D. Evaluation of hot-presses hydroxyapatite/poly-L-lactide composite biomaterial characteristics. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 71B, 284–294. [Google Scholar] [CrossRef]
- Wang, X.; Lou, T.; Yang, J.; Yang, Z.; He, K. Preparation of PLLA/HAP/β-TCP composite scaffold for bone tissue engineering. Appl. Mech. Mater. 2014, 513–517, 143–146. [Google Scholar] [CrossRef]
- Hasegawa, S.; Tamura, J.; Neo, M.; Goto, K.; Shikinami, Y.; Saito, M.; Kita, M.; Nakamura, T. In vivo evaluation of a porous hydroxyapatite/poly-D,L-lactide composite for use as a bone substitute. J. Biomed. Mater. Res. A 2005, 75A, 567–579. [Google Scholar] [CrossRef]
- Hasegawa, S.; Neo, M.; Tamura, J.; Fujibayashi, S.; Takemoto, M.; Shikinami, Y.; Okazaki, K.; Nakamura, T. In vivo evaluation of a porous hydroxyapatite/poly-D,L-lactide composite for bone tissue engineering. J. Biomed. Mater. Res. A 2007, 81A, 930–938. [Google Scholar] [CrossRef]
- Kim, S.S.; Park, M.S.; Jeon, Q.; Choi, C.Y.; Kim, B.S. Poly(lactide-co-glycolide)/hydroxyapatite composite scaffolds for bone tissue engineering. Biomaterials 2006, 27, 1399–1409. [Google Scholar] [CrossRef]
- Mao, D.; Li, Q.; Bai, N.; Dong, H.; Li, D. Porous stable poly(lactic acid)/ethyl cellulose/hydroxyapatite composite scaffolds prepared by a combined method for bone regeneration. Carbohyd. Polym. 2018, 180, 104–111. [Google Scholar] [CrossRef]
- Carvalho, T.S.S.; Ribeiro, N.; Torres, P.M.C.; Almeida, J.C.; Belo, J.H.; Araújo, J.P.; Ramos, A.; Oliveira, M.; Olhero, S.M. Magnetic polylactic acid-calcium phosphate-based biocomposite as a potential biomaterial for tissue engineering applications. Mater. Chem. Phys. 2023, 296, 127175. [Google Scholar] [CrossRef]
- Alonso-Fernández, I.; Haugen, H.J.; López-Peña, M.; González-Cantalapiedra, A.; Muñoz, F. Use of 3D-printed polylactic acid/bioceramic composite scaffolds for bone tissue engineering in preclinical in vivo studies: A systematic review. Acta Biomater. 2023, 168, 1–21. [Google Scholar] [CrossRef]
- Reis, R.L.; Cunha, A.M. New degradable load-bearing biomaterials composed of reinforced starch based blends. J. Appl. Med. Polym. 2000, 4, 1–5. [Google Scholar]
- Sousa, R.A.; Mano, J.F.; Reis, R.L.; Cunha, A.M.; Bevis, M.J. Mechanical performance of starch based bioactive composites moulded with preferred orientation for potential medical applications. Polym. Eng. Sci. 2002, 42, 1032–1045. [Google Scholar] [CrossRef]
- Marques, A.P.; Reis, R.L. Hydroxyapatite reinforcement of different starch-based polymers affects osteoblast-like cells adhesion/spreading and proliferation. Mater. Sci. Eng. C 2005, 25, 215–229. [Google Scholar] [CrossRef]
- Reis, R.L.; Cunha, A.M.; Allan, P.S.; Bevis, M.J. Structure development and control of injection-molded hydroxylapatite-reinforced starch/EVOH composites. Adv. Polym. Technol. 1997, 16, 263–277. [Google Scholar] [CrossRef]
- Vaz, C.M.; Reis, R.L.; Cunha, A.M. Use of coupling agents to enhance the interfacial interactions in starch-EVOH/hydroxylapatite composites. Biomaterials 2002, 23, 629–635. [Google Scholar] [CrossRef]
- Leonor, I.B.; Ito, A.; Onuma, K.; Kanzaki, N.; Reis, R.L. In vitro bioactivity of starch thermoplastic/hydroxyapatite composite biomaterials: An in situ study using atomic force microscopy. Biomaterials 2003, 24, 579–585. [Google Scholar] [CrossRef]
- Vaz, C.M.; Reis, R.L.; Cunha, A.M. Degradation model of starch-EVOH+HA composites. Mater. Res. Innov. 2001, 4, 375–380. [Google Scholar] [CrossRef]
- Chen, L.J.; Wang, M. Production and evaluation of biodegradable composites based on PHB-PHV copolymer. Biomaterials 2002, 23, 2631–2639. [Google Scholar] [CrossRef]
- Ni, J.; Wang, M. In vitro evaluation of hydroxyapatite reinforced polyhydroxybutyrate composite. Mater. Sci. Eng. C 2002, 20, 101–109. [Google Scholar] [CrossRef]
- Carlo, E.C.; Borges, A.P.B.; Del Carlo, R.J.; Martinez, M.M.M.; Oliveira, P.M.; Morato, G.O.; Eleotério, R.B.; Reis, M.S. Comparison of in vivo properties of hydroxyapatite-polyhydroxybutyrate composites assessed for bone substitution. J. Craniofac. Surg. 2009, 20, 853–859. [Google Scholar] [CrossRef]
- Sadat-Shojai, M.; Khorasani, M.T.; Jamshidi, A.; Irani, S. Nano-hydroxyapatite reinforced polyhydroxybutyrate composites: A comprehensive study on the structural and in vitro biological properties. Mater. Sci. Eng. C 2013, 33, 2776–2787. [Google Scholar] [CrossRef]
- Tyubaeva, P.M.; Gasparyan, K.G.; Fedotov, A.Y.; Lobzhanidze, P.V.; Baranov, O.V.; Egorov, A.A.; Sirotinkin, V.P.; Komlev, V.S.; Olkhov, A.A. Development of nonwoven fibrous materials based on poly-3-hydroxybutyrate with a high content of α-tricalcium phosphate. Polymers 2023, 15, 3167. [Google Scholar] [CrossRef]
- Chen, D.Z.; Tang, C.Y.; Chan, K.C.; Tsui, C.P.; Yu, P.H.F.; Leung, M.C.P.; Uskokovic, P.S. Dynamic mechanical properties and in vitro bioactivity of PHBHV/HA nanocomposite. Compos. Sci. Technol. 2007, 67, 1617–1626. [Google Scholar] [CrossRef]
- Rai, B.; Noohom, W.; Kithva, P.H.; Grøndahl, L.; Trau, M. Bionanohydroxyapatite/poly(3-hydroxybutyrate-co-3-hydroxyvalerate) composites with improved particle dispersion and superior mechanical properties. Chem. Mater. 2008, 20, 2802–2808. [Google Scholar] [CrossRef]
- Wang, Y.W.; Wu, Q.; Chen, J.; Chen, G.Q. Evaluation of three-dimensional scaffolds made of blends of hydroxyapatite and poly(3-hydroxybutyrate-co-3-hydroxyhexanoate) for bone reconstruction. Biomaterials 2005, 26, 899–904. [Google Scholar] [CrossRef]
- Linhart, W.; Lehmann, W.; Siedler, M.; Peters, F.; Schilling, A.F.; Schwarz, K.; Amling, M.; Rueger, J.M.; Epple, M. Composites of amorphous calcium phosphate and poly(hydroxybutyrate) and poly(hydroxybutyrate-co-hydroxyvalerate) for bone substitution: Assessment of the biocompatibility. J. Mater. Sci. 2006, 41, 4806–4813. [Google Scholar] [CrossRef]
- Azevedo, M.; Reis, R.L.; Claase, M.; Grijpma, D.; Feijen, J. Development and properties of polycaprolactone/hydroxyapatite composite biomaterials. J. Mater. Sci. Mater. Med. 2003, 14, 103–107. [Google Scholar] [CrossRef]
- Walsh, D.; Furuzono, T.; Tanaka, J. Preparation of porous composite implant materials by in situ polymerization of porous apatite containing ε-caprolactone or methyl methacrylate. Biomaterials 2001, 22, 1205–1212. [Google Scholar] [CrossRef]
- Kim, H.W. Biomedical nanocomposites of hydroxyapatite/polycaprolactone obtained by surfactant mediation. J. Biomed. Mater. Res. A 2007, 83A, 169–177. [Google Scholar] [CrossRef]
- Chuenjitkuntaworn, B.; Inrung, W.; Damrongsri, D.; Mekaapiruk, K.; Supaphol, P.; Pavasant, P. Polycaprolactone/hydroxyapatite composite scaffolds: Preparation, characterization and in vitro and in vivo biological responses of human primary bone cells. J. Biomed. Mater. Res. A 2010, 94A, 241–251. [Google Scholar] [CrossRef]
- Kim, B.S.; Yang, S.S.; Lee, J. A polycaprolactone/cuttlefish bone-derived hydroxyapatite composite porous scaffold for bone tissue engineering. J. Biomed. Mater. Res. B Appl. Biomater. 2014, 102B, 943–951. [Google Scholar] [CrossRef]
- Hajiali, F.; Tajbakhsh, S.; Shojaei, A. Fabrication and properties of polycaprolactone composites containing calcium phosphate-based ceramics and bioactive glasses in bone tissue engineering: A review. Polym. Rev. 2017, 58, 164–207. [Google Scholar] [CrossRef]
- Huang, B.; Caetano, G.; Vyas, C.; Blaker, J.J.; Diver, C.; Bártolo, P. Polymer-ceramic composite scaffolds: The effect of hydroxyapatite and β-tri-calcium phosphate. Materials 2018, 11, 129. [Google Scholar] [CrossRef]
- Causa, F.; Netti, P.A.; Ambrosio, L.; Ciapetti, G.; Baldini, N.; Pagani, S.; Martini, D.; Giunti, A. Poly-ε-caprolactone/hydroxyapatite composites for bone regeneration: In vitro characterization and human osteoblast response. J. Biomed. Mater. Res. A 2006, 76A, 151–162. [Google Scholar] [CrossRef]
- Thomas, V.; Jagani, S.; Johnson, K.; Jose, M.V.; Dean, D.R.; Vohra, Y.K.; Nyairo, E. Electrospun bioactive nanocomposite scaffolds of polycaprolactone and nanohydroxyapatite for bone tissue engineering. J. Nanosci. Nanotechol. 2006, 6, 487–493. [Google Scholar] [CrossRef]
- Marra, K.G.; Szem, J.W.; Kumta, P.N.; DiMilla, P.A.; Weiss, L.E. In vitro analysis of biodegradable polymer blend/hydroxyapatite composites for bone tissue engineering. J. Biomed. Mater. Res. 1999, 47, 324–335. [Google Scholar] [CrossRef]
- Dunn, A.; Campbell, P.; Marra, K.G. The influence of polymer blend composition on the degradation of polymer/hydroxyapatite biomaterials. J. Mater. Sci. Mater. Med. 2001, 12, 673–677. [Google Scholar] [CrossRef]
- Calandrelli, L.; Immirzi, B.; Malinconico, M.; Volpe, M.; Oliva, A.; Ragione, F. Preparation and characterization of composites based on biodegradable polymers for in vivo application. Polymer 2000, 41, 8027–8033. [Google Scholar] [CrossRef]
- Chen, B.; Sun, K. Poly(ε-caprolactone)/hydroxyapatite composites: Effects of particle size, molecular weight distribution and irradiation on interfacial interaction and properties. Polym. Test. 2005, 24, 64–70. [Google Scholar] [CrossRef]
- Kim, H.W.; Knowles, J.C.; Kim, H.E. Hydroxyapatite/poly(ε-caprolactone) composite coatings on hydroxyapatite porous bone scaffold for drug delivery. Biomaterials 2004, 25, 1279–1287. [Google Scholar] [CrossRef]
- Ural, E.; Kesenci, K.; Fambri, L.; Migliaresi, C.; Piskin, E. Poly(D,L-lactide/ε-caprolactone)/hydroxyapatite composites. Biomaterials 2000, 21, 2147–2154. [Google Scholar] [CrossRef]
- Rodenas-Rochina, J.; Vidaurre, A.; Cortázar, I.C.; Lebourg, M. Effects of hydroxyapatite filler on long-term hydrolytic degradation of PLLA/PCL porous scaffolds. Polym. Degrad. Stabil. 2015, 119, 121–131. [Google Scholar] [CrossRef]
- Kim, H.W.; Lee, E.J.; Kim, H.E.; Salih, V.; Knowles, J.C. Effect of fluoridation of hydroxyapatite in hydroxyapatite/polycaprolactone composites on osteoblast activity. Biomaterials 2005, 26, 4395–4404. [Google Scholar] [CrossRef]
- Reyna-Urrutia, V.A.; Estevez, M.; González-González, A.M.; Rosales-Ibáñez, R. 3D scaffolds of caprolactone/chitosan/polyvinyl alcohol/hydroxyapatite stabilized by physical bonds seeded with swine dental pulp stem cell for bone tissue engineering. J. Mater. Sci. Mater. Med. 2022, 33, 81. [Google Scholar] [CrossRef]
- Gloria, A.; Russo, T.; D’Amora, U.; Zeppetelli, S.; D’Alessandro, T.; Sandri, M.; Bañobre-López, M.; Piñeiro-Redondo, Y.; Uhlarz, M.; Tampieri, A.; et al. Magnetic poly(ε-caprolactone)/iron-doped hydroxyapatite nanocomposite substrates for advanced bone tissue engineering. J. R. Soc. Interface 2013, 10, 20120833. [Google Scholar] [CrossRef]
- Shokrollahi, P.; Mirzadeh, H.; Scherman, O.A.; Huck, W.T.S. Biological and mechanical properties of novel composites based on supramolecular polycaprolactone and functionalized hydroxyapatite. J. Biomed. Mater. Res. A 2010, 95A, 209–221. [Google Scholar] [CrossRef]
- Mehmanchi, M.; Shokrollahi, P.; Atai, M.; Omidian, H.; Bagheri, R. Supramolecular polycaprolactone nanocomposite based on functionalized hydroxyapatite. J. Bioact. Compat. Polym. 2012, 27, 467–480. [Google Scholar] [CrossRef]
- Bose, S.; Razack, S.A.; Arthanari, S.; Kim, Y.; Lee, H.; Kang, H.W. Near-infrared light-responsive Cu2O@CuFeS2-hydroxyapatite-chitosan based antibacterial coating on titanium bioimplant. Prog. Org. Coat. 2023, 183, 107714. [Google Scholar] [CrossRef]
- Popkov, A.; Tverdokhlebov, S.; Muradisinov, S.; Popkov, D. First clinical case of Ilizarov femur lengthening over a bioactive and degradable intramedullary implant. Case Rep. Orthop. 2023, 2023, 7547590. [Google Scholar] [CrossRef]
- Cojocaru, F.D.; Gardikiotis, I.; Dodi, G.; Rotaru, A.; Balan, V.; Rezus, E.; Verestiuc, L. Polysaccharides-calcium phosphates composite beads as bone substitutes for fractures repair and regeneration. Polymers 2023, 15, 1509. [Google Scholar] [CrossRef]
- Klimek, L.; Kopacz, K.; Smielak, B.; Kula, Z. An evaluation of the mechanical properties of a hybrid composite containing hydroxyapatite. Materials 2023, 16, 4548. [Google Scholar] [CrossRef]
- Forysenkova, A.A.; Fadeeva, I.V.; Deyneko, D.V.; Gosteva, A.N.; Mamin, G.V.; Shurtakova, D.V.; Davydova, G.A.; Yankova, V.G.; Antoniac, I.V.; Rau, J.V. Polyvinylpyrrolidone–alginate–carbonate hydroxyapatite porous composites for dental applications. Materials 2023, 16, 4478. [Google Scholar] [CrossRef]
- Deng, C.; Wang, B.; Dongqin, X.; Zhou, S.; Duan, K.; Weng, J. Preparation and shape memory property of hydroxyapatite/poly (vinyl alcohol) composite. Polym.—Plast. Technol. Eng. 2012, 51, 1315–1318. [Google Scholar] [CrossRef]
- Kutikov, A.B.; Reyer, K.A.; Song, J. Shape-memory performance of thermoplastic amphiphilic triblock copolymer poly(D,L-lactic acid-co-ethylene glycol-co-D,L-lactic acid) (PELA)/hydroxyapatite composites. Macromol. Chem. Phys. 2014, 215, 2482–2490. [Google Scholar] [CrossRef]
- Bao, M.; Wang, X.; Yuan, H.; Lou, X.; Zhao, Q.; Zhang, Y. HAp incorporated ultrafine polymeric fibers with shape memory effect for potential use in bone screw hole healing. J. Mater. Chem. B 2016, 4, 5308–5320. [Google Scholar] [CrossRef]
- Esposti, M.D.; Chiellini, F.; Bondioli, F.; Morselli, D.; Fabbri, P. Highly porous PHB-based bioactive scaffolds for bone tissue engineering by in situ synthesis of hydroxyapatite. Mater. Sci. Eng. C 2019, 100, 286–296. [Google Scholar] [CrossRef]
- Guillaume, O.; Geven, M.A.; Varjas, V.; Gehweiler, D.; Stadelmann, V.A.; Smidt, T.; Zeiter, S.; Sprecher, C.; Bos, R.R.M.; Grijpma, D.W.; et al. Orbital floor repair using patient specific osteoinductive implant made by stereolithography. Biomaterials 2020, 233, 119721. [Google Scholar] [CrossRef]
- Sikkema, R.; Keohan, B.; Zhitomirsky, I. Alginic acid polymer-hydroxyapatite composites for bone tissue engineering. Polymers 2021, 13, 3070. [Google Scholar] [CrossRef]
- Novesar, J.; Dinda, A.; Rahmayeni; Upita, S.; Vivi, S. The effect of temperature on the synthesis and characterization of hydroxyapatite-polyethylene glycol composites by in-situ process. Hybrid Adv. 2023, 2, 100031. [Google Scholar]
- Ghasroldasht, M.M.; Mastrogiacomo, M.; Akbarian, F.; Rezaeian, A. Polyurethane and polyurethane/hydroxyapatite scaffold in a three-dimensional culture system. Cell Biol. Int. 2022, 46, 2041–2049. [Google Scholar] [CrossRef]
- Behl, M.; Razzaq, M.Y.; Lendlein, A. Multifunctional shape-memory polymers. Adv. Mater. 2010, 22, 3388–3410. [Google Scholar] [CrossRef]
- Cojocaru, F.D.; Balan, V.; Popa, M.I.; Lobiuc, A.; Antoniac, A.; Antoniac, I.V.; Verestiuc, L. Biopolymers–calcium phosphates composites with inclusions of magnetic nanoparticles for bone tissue engineering. Int. J. Biol. Macromol. 2019, 125, 612–620. [Google Scholar] [CrossRef]
- Carvalho, T.S.S.; Torres, P.M.C.; Belo, J.H.; Mano, J.; Olhero, S.M. Bioactive magnetic materials in bone tissue engineering: A review of recent findings in CaP-based particles and 3D-printed scaffolds. Adv. NanoBiomed. Res. 2023, 3, 2300035. [Google Scholar] [CrossRef]
- Ramesh, N.; Moratti, S.C.; Dias, G.J. Hydroxyapatite-polymer biocomposites for bone regeneration: A review of current trends. J. Biomed. Mater. Res. B Appl. Biomater. 2018, 106B, 2046–2057. [Google Scholar] [CrossRef]
- Ielo, I.; Calabrese, G.; de Luca, G.; Conoci, S. Recent advances in hydroxyapatite-based biocomposites for bone tissue regeneration in orthopedics. Int. J. Mol. Sci. 2022, 23, 9721. [Google Scholar] [CrossRef]
- Furko, M.; Balázsi, K.; Balázsi, C. Calcium phosphate loaded biopolymer composites—A comprehensive review on the most recent progress and promising trends. Coatings 2023, 13, 360. [Google Scholar] [CrossRef]
- Aoki, K.; Ideta, H.; Komatsu, Y.; Tanaka, A.; Kito, M.; Okamoto, M.; Takahashi, J.; Suzuki, S.; Saito, N. Bone-regeneration therapy using biodegradable scaffolds: Calcium phosphate bioceramics and biodegradable polymers. Bioengineering 2024, 11, 180. [Google Scholar] [CrossRef]
- Handschel, J.; Wiesmann, H.P.; Stratmann, U.; Kleinheinz, J.; Meyer, U.; Joos, U. TCP is hardly resorbed and not osteoconductive in a non-loading calvarial model. Biomaterials 2002, 23, 1689–1695. [Google Scholar] [CrossRef]
- Kikuchi, M.; Tanaka, J. Chemical interaction in β-tricalcium phosphate/copolymerized poly-L-lactide composites. J. Ceram. Soc. Jpn. 2000, 108, 642–645. [Google Scholar] [CrossRef]
- Haaparanta, A.M.; Haimi, S.; Ellä, V.; Hopper, N.; Miettinen, S.; Suuronen, R.; Kellomäki, M. Porous polylactide/β-tricalcium phosphate composite scaffolds for tissue engineering applications. J. Tissue Eng. Regen. Med. 2010, 4, 366–373. [Google Scholar] [CrossRef]
- Shin, D.Y.; Kang, M.H.; Kang, I.G.; Kim, H.E.; Jeong, S.H. In vitro and in vivo evaluation of polylactic acid-based composite with tricalcium phosphate microsphere for enhanced biodegradability and osseointegration. J. Biomater. Appl. 2018, 32, 1360–1370. [Google Scholar] [CrossRef]
- Kikuchi, M.; Koyama, Y.; Yamada, T.; Imamura, Y.; Okada, T.; Shirahama, N.; Akita, K.; Takakuda, K.; Tanaka, J. Development of guided bone regeneration membrane composed of β-tricalcium phosphate and poly(L-lactide-co-glycolide-co-ε-caprolactone) composites. Biomaterials 2004, 25, 5979–5986. [Google Scholar] [CrossRef]
- Chen, T.M.; Yao, C.H.; Wang, H.J.; Chou, G.H.; Lee, T.W.; Lin, F.H. Evaluation of a novel malleable, biodegradable osteoconductive composite in a rabbit cranial defect model. Mater. Chem. Phys. 1998, 55, 44–50. [Google Scholar] [CrossRef]
- Dong, G.C.; Chen, H.M.; Yao, C.H. A novel bone substitute composite composed of tricalcium phosphate, gelatin and drynaria fortunei herbal extract. J. Biomed. Mater. Res. A 2008, 84A, 167–177. [Google Scholar] [CrossRef]
- Ji, J.; Yuan, X.; Xia, Z.; Liu, P.; Chen, J. Porous β-tricalcium phosphate composite scaffold reinforced by K2HPO4 and gelatin. Key Eng. Mater. 2010, 434–435, 620–623. [Google Scholar] [CrossRef]
- Yao, C.H.; Liu, B.S.; Hsu, S.H.; Chen, Y.S.; Tsai, C.C. Biocompatibility and biodegradation of a bone composite containing tricalcium phosphate and genipin crosslinked gelatin. J. Biomed. Mater. Res. A 2004, 69A, 709–717. [Google Scholar] [CrossRef]
- Eslaminejad, M.B.; Mirzadeh, H.; Mohamadi, Y.; Nickmahzar, A. Bone differentiation of marrow-derived mesenchymal stem cells using β-tricalcium phosphate-alginate-gelatin hybrid scaffolds. J. Tissue Eng. Regen. Med. 2007, 1, 417–424. [Google Scholar] [CrossRef]
- Bigi, A.; Cantelli, I.; Panzavolta, S.; Rubini, K. α-tricalcium phosphate-gelatin composite cements. J. Appl. Biomater. Biomech. 2004, 2, 81–87. [Google Scholar]
- Yang, S.H.; Hsu, C.K.; Wang, K.C.; Hou, S.M.; Lin, F.H. Tricalcium phosphate and glutaraldehyde crosslinked gelatin incorporating bone morphogenetic protein—A viable scaffold for bone tissue engineering. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 74B, 468–475. [Google Scholar] [CrossRef]
- Muramatsu, K.; Oba, K.; Mukai, D.; Hasegawa, K.; Masuda, S.; Yoshihara, Y. Subacute systemic toxicity assessment of β-tricalcium phosphate/carboxymethyl-chitin composite implanted in rat femur. J. Mater. Sci. Mater. Med. 2007, 18, 513–522. [Google Scholar] [CrossRef]
- Panzavolta, S.; Fini, M.; Nicoletti, A.; Bracci, B.; Rubini, K.; Giardino, R.; Bigi, A. Porous composite scaffolds based on gelatin and partially hydrolyzed α-tricalcium phosphate. Acta Biomater. 2009, 5, 636–643. [Google Scholar] [CrossRef]
- Uchino, T.; Kamitakahara, M.; Otsuka, M.; Ohtsuki, C. Hydroxyapatite-forming capability and mechanical properties of organic-inorganic hybrids and α-tricalcium phosphate porous bodies. J. Ceram. Soc. Jpn. 2010, 118, 57–61. [Google Scholar] [CrossRef]
- Flauder, S.; Sajzew, R.; Müller, F.A. Mechanical properties of porous β-tricalcium phosphate composites prepared by ice-templating and poly(σ-caprolactone) impregnation. ACS Appl. Mater. Interfaces 2015, 7, 845–851. [Google Scholar] [CrossRef]
- Ramanathan, M.; Shijirbold, A.; Okui, T.; Tatsumi, H.; Kotani, T.; Shimamura, Y.; Morioka, R.; Ayasaka, K.; Kanno, T. In vivo evaluation of bone regenerative capacity of the novel nanobiomaterial: β-tricalcium phosphate polylactic acid-co-glycolide (β-TCP/PLLA/PGA) for use in maxillofacial bone defects. Nanomaterials 2024, 14, 91. [Google Scholar] [CrossRef]
- Liao, L.; Zhu, W.; Tao, C.; Li, D.; Mao, M. Cissus quadrangularis L. extract-loaded tricalcium phosphate reinforced natural polymer composite for guided bone regeneration. J. Mater. Sci. Mater. Med. 2023, 34, 33. [Google Scholar] [CrossRef]
- Ritschl, L.; Schilling, P.; Wittmer, A.; Bohner, M.; Bernstein, A.; Schmal, H.; Seidenstuecker, M. Composite material consisting of microporous beta-TCP ceramic and alginate-dialdehyde-gelatin for controlled dual release of clindamycin and bone morphogenetic protein 2. J. Mater. Sci. Mater. Med. 2023, 34, 39. [Google Scholar] [CrossRef]
- Cohen, B.; Panker, M.; Zuckerman, E.; Foox, M.; Zilberman, M. Effect of calcium phosphate-based fillers on the structure and bonding strength of novel gelatin-alginate bioadhesives. J. Biomater. Appl. 2014, 28, 1366–1375. [Google Scholar] [CrossRef]
- Bleach, N.C.; Tanner, K.E.; Kellomäki, M.; Törmälä, P. Effect of filler type on the mechanical properties of self-reinforced polylactide-calcium phosphate composites. J. Mater. Sci. Mater. Med. 2001, 12, 911–915. [Google Scholar] [CrossRef]
- Liu, L.; Xiong, Z.; Yan, Y.N.; Hu, Y.Y.; Zhang, R.J.; Wang, S.G. Porous morphology, porosity, mechanical properties of poly(α-hydroxy acid)-tricalcium phosphate composite scaffolds fabricated by low-temperature deposition. J. Biomed. Mater. Res. A 2007, 82A, 618–629. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, M.Q. Synthesis and characterization of macroporous chitosan/calcium phosphate composite scaffolds for tissue engineering. J. Biomed. Mater. Res. 2001, 55, 304–312. [Google Scholar] [CrossRef]
- Rai, B.; Teoh, S.H.; Hutmacher, D.W.; Cao, T.; Ho, K.H. Novel PCL-based honeycomb scaffolds as drug delivery systems for rhBMP-2. Biomaterials 2005, 26, 3739–3748. [Google Scholar] [CrossRef]
- Rai, B.; Teoh, S.H.; Ho, K.H.; Hutmacher, D.W.; Cao, T.; Chen, F.; Yacob, K. The effect of rhBMP-2 on canine osteoblasts seeded onto 3D bioactive polycaprolactone scaffolds. Biomaterials 2004, 25, 5499–5506. [Google Scholar] [CrossRef]
- Lei, Y.; Rai, B.; Ho, K.H.; Teoh, S.H. In vitro degradation of novel bioactive polycaprolactone—20% tricalcium phosphate composite scaffolds for bone engineering. Mater. Sci. Eng. C 2007, 27, 293–298. [Google Scholar] [CrossRef]
- Miyai, T.; Ito, A.; Tamazawa, G.; Matsuno, T.; Sogo, Y.; Nakamura, C.; Yamazaki, A.; Satoh, T. Antibiotic-loaded poly-ε-caprolactone and porous β-tricalcium phosphate composite for treating osteomyelitis. Biomaterials 2008, 29, 350–358. [Google Scholar] [CrossRef]
- Li, Y.; Wu, Z.G.; Li, X.K.; Guo, Z.; Wu, S.H.; Zhang, Y.Q.; Shi, L.; Teoh, S.H.; Liu, Y.C.; Zhang, Z.Y. A polycaprolactone-tricalcium phosphate composite scaffold as an autograft-free spinal fusion cage in a sheep model. Biomaterials 2014, 35, 5647–5659. [Google Scholar] [CrossRef]
- Takahashi, Y.; Yamamoto, M.; Tabata, Y. Enhanced osteoinduction by controlled release of bone morphogenetic protein-2 from biodegradable sponge composed of gelatin and β-tricalcium phosphate. Biomaterials 2005, 26, 4856–4865. [Google Scholar] [CrossRef]
- Ignatius, A.A.; Betz, O.; Augat, P.; Claes, L.E. In vivo investigations on composites made of resorbable ceramics and poly(lactide) used as bone graft substitutes. J. Biomed. Mater. Res. Appl. Biomater. 2001, 58, 701–709. [Google Scholar] [CrossRef]
- Miao, X.; Lim, W.K.; Huang, X.; Chen, Y. Preparation and characterization of interpenetrating phased TCP/HA/PLGA composites. Mater. Lett. 2005, 59, 4000–4005. [Google Scholar] [CrossRef]
- Ozbek, B.; Erdogan, B.; Ekren, N.; Oktar, F.N.; Akyol, S.; Ben-Nissan, B.; Sasmazel, H.T.; Kalkandelen, C.; Mergen, A.; Kuruca, S.E.; et al. Production of the novel fibrous structure of poly(ε-caprolactone)/tri-calcium phosphate/hexagonal boron nitride composites for bone tissue engineering. J. Austral. Ceram. Soc. 2018, 54, 251–260. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Multiphasic calcium orthophosphate (CaPO4) bioceramics and their biomedical applications. Ceram. Int. 2016, 42, 6529–6554. [Google Scholar] [CrossRef]
- Zhang, L.F.; Sun, R.; Xu, L.; Du, J.; Xiong, Z.C.; Chen, H.C.; Xiong, C.D. Hydrophilic poly (ethylene glycol) coating on PDLLA/BCP bone scaffold for drug delivery and cell culture. Mater. Sci. Eng. C 2008, 28, 141–149. [Google Scholar] [CrossRef]
- Ignjatovic, N.; Ninkov, P.; Ajdukovic, Z.; Konstantinovic, V.; Uskokovic, D. Biphasic calcium phosphate/poly-(D,L-lactide-co-glycolide) biocomposite as filler and blocks for reparation of bone tissue. Mater. Sci. Forum 2005, 494, 519–524. [Google Scholar] [CrossRef]
- Ignjatovic, N.; Ninkov, P.; Ajdukovic, Z.; Vasiljevic-Radovic, D.; Uskokovic, D. Biphasic calcium phosphate coated with poly-D,L-lactide-co-glycolide biomaterial as a bone substitute. J. Eur. Ceram. Soc. 2007, 27, 1589–1594. [Google Scholar] [CrossRef]
- Yang, W.; Yin, G.; Zhou, D.; Gu, J.; Li, Y. In vitro characteristics of surface-modified biphasic calcium phosphate/poly(L-Lactide) biocomposite. Adv. Eng. Mater. 2010, 12, B128–B132. [Google Scholar] [CrossRef]
- Ignjatovic, N.; Ninkov, P.; Kojic, V.; Bokurov, M.; Srdic, V.; Krnojelac, D.; Selakovic, S.; Uskokovic, D. Cytotoxicity and fibroblast properties during in vitro test of biphasic calcium phosphate/poly-D,L-lactide-co-glycolide biocomposites and different phosphate materials. Microsc. Res. Techniq. 2006, 69, 976–982. [Google Scholar] [CrossRef]
- Ajdukovic, Z.; Ignjatovic, N.; Petrovic, D.; Uskokovic, D. Substitution of osteoporotic alveolar bone by biphasic calcium phosphate/poly-D,L-lactide-co-glycolide biomaterials. J. Biomater. Appl. 2007, 21, 317–328. [Google Scholar] [CrossRef]
- Kim, H.W.; Knowles, J.C.; Kim, H.E. Effect of biphasic calcium phosphates on drug release and biological and mechanical properties of poly(ε-caprolactone) composite membranes. J. Biomed. Mater. Res. A 2004, 70A, 467–479. [Google Scholar] [CrossRef]
- Kwak, K.A.; Jyoti, M.A.; Song, H.Y. In vitro and in vivo studies of three dimensional porous composites of biphasic calcium phosphate/poly ε-caprolactone: Effect of bio-functionalization for bone tissue engineering. Appl. Surf. Sci. 2014, 301, 307–314. [Google Scholar] [CrossRef]
- van Leeuwen, A.C.; Yuan, H.; Passanisi, G.; van der Meer, J.W.; de Bruijn, J.D.; van Kooten, T.G.; Grijpma, D.W.; Bos, R.R. Poly(trimethylene carbonate) and biphasic calcium phosphate composites for orbital floor reconstruction: A feasibility study in sheep. Eur. Cell. Mater. 2014, 27, 81–96; discussion 96–97. [Google Scholar] [CrossRef]
- Hossain, M.; Jeong, J.H.; Sultana, T.; Kim, J.H.; Moon, J.E.; Im, S. A composite of polymethylmethacrylate, hydroxyapatite and β-tricalcium phosphate for bone regeneration in an osteoporotic rat model. J. Biomed. Mater. Res. B Appl. Biomater. 2023, 111, 1813–1823. [Google Scholar] [CrossRef]
- Bakhtiari, L.; Rezai, H.R.; Hosseinalipour, S.M.; Shokrgozar, M.A. Investigation of biphasic calcium phosphate/gelatin nanocomposite scaffolds as a bone tissue engineering. Ceram. Int. 2010, 36, 2421–2426. [Google Scholar] [CrossRef]
- Bakhtiari, L.; Rezai, H.R.; Hosseinalipour, S.M.; Shokrgozar, M.A. Preparation of porous Biphasic calcium phosphate-gelatin nanocomposite for bone tissue engineering. J. Nano Res. 2010, 11, 67–72. [Google Scholar] [CrossRef]
- Hassouna, A.; Elgharbawy, H.; Morsy, R. Development of porous scaffolds based on the in situ synthesis of biphasic calcium phosphate in a gelatin-polyvinyl alcohol matrix for bone tissue engineering. J. Mol. Struct. 2023, 1279, 134951. [Google Scholar] [CrossRef]
- Matsuda, A.; Ikoma, T.; Kobayashi, H.; Tanaka, J. Preparation and mechanical property of core-shell type chitosan/calcium phosphate composite fiber. Mater. Sci. Eng. C 2004, 24, 723–728. [Google Scholar] [CrossRef]
- Rattanachan, S.; Lorprayoon, C.; Boonphayak, P. Synthesis of chitosan/brushite powders for bone cement composites. J. Ceram. Soc. Jpn. 2008, 116, 36–41. [Google Scholar] [CrossRef]
- Ohsawa, H.; Ito, A.; Sogo, Y.; Yamazaki, A.; Ohno, T. Synthesis of albumin/DCP nano-composite particles. Key Eng. Mater. 2007, 330–332, 239–242. [Google Scholar] [CrossRef]
- Mohammad, F.; Arfin, T.; Al-Lohedan, H.A. Synthesis, characterization and applications of ethyl cellulose-based polymeric calcium (II) hydrogen phosphate composite. J. Electron. Mater. 2018, 47, 2954–2963. [Google Scholar] [CrossRef]
- Li, X.; Noshadi, B.; Motamedi, K.; Movahed, E.; Behfarnia, P.; Semiroumi, D.T. Bioceramic calcium phosphate-polymer scaffolds: A promising strategy for osteochondral repair and regenerative medicine. Mater. Chem. Phys. 2023, 304, 127855. [Google Scholar] [CrossRef]
- Xu, H.H.K.; Sun, L.; Weir, M.D.; Antonucci, J.M.; Takagi, S.; Chow, L.C.; Peltz, M. Nano DCPA-whisker composites with high strength and Ca and PO4 release. J. Dent. Res. 2006, 85, 722–727. [Google Scholar] [CrossRef]
- Xu, H.H.K.; Weir, M.D.; Sun, L.; Takagi, S.; Chow, L.C. Effects of calcium phosphate nanoparticles on Ca-PO4 composite. J. Dent. Res. 2007, 86, 378–383. [Google Scholar] [CrossRef]
- Xu, H.H.K.; Weir, M.D.; Sun, L. Nanocomposites with Ca and PO4 release: Effects of reinforcement, dicalcium phosphate particle size and silanization. Dent. Mater. 2007, 23, 1482–1491. [Google Scholar] [CrossRef]
- Chen, W.C.; Chang, K.C.; Wu, H.Y.; Ko, C.L.; Huang, C.L. Thermal cycling effect of dicalcium phosphate-reinforced composites on auto-mineralized dental resin. Mater. Sci. Eng. C 2014, 45, 359–368. [Google Scholar] [CrossRef]
- El-Meliegy, E.; Mabrouk, M.; Kamal, G.M.; Awad, S.M.; El-Tohamy, A.M.; El Gohary, M.I. Anticancer drug carriers using dicalcium phosphate/dextran/CMCnanocomposite scaffolds. J. Drug Deliv. Sci. Technol. 2018, 45, 315–322. [Google Scholar] [CrossRef]
- Tortet, L.; Gavarri, J.R.; Nihoul, G.; Dianoux, A.J. Proton mobilities in brushite and brushite/polymer composites. Solid State Ion. 1997, 97, 253–256. [Google Scholar] [CrossRef]
- Tortet, L.; Gavarri, J.R.; Musso, J.; Nihoul, G.; Sarychev, A.K. Percolation and modeling of proton conduction in polymer/brushite composites. J. Solid State Chem. 1998, 141, 392–403. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Synthetic amorphous calcium phosphates (ACPs): Preparation, structure, properties and biomedical applications. Biomater. Sci. 2021, 9, 7748–7798. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Dental applications of calcium orthophosphates (CaPO4). J. Dent. Res. 2019, 1, 24–54. [Google Scholar]
- Zhang, L.; Weir, M.D.; Chow, L.C.; Antonucci, J.M.; Chen, J.; Xu, H.H.K. Novel rechargeable calcium phosphate dental nanocomposite. Dent. Mater. 2016, 32, 285–293. [Google Scholar] [CrossRef]
- Zhang, L.; Weir, M.D.; Chow, L.C.; Reynolds, M.A.; Xu, H.H.K. Rechargeable calcium phosphate orthodontic cement with sustained ion release and re-release. Sci. Rep. 2016, 6, 36476. [Google Scholar] [CrossRef]
- Xie, X.J.; Xing, D.; Wang, L.; Zhou, H.; Weir, M.D.; Bai, Y.X.; Xu, H.H.K. Novel rechargeable calcium phosphate nanoparticle-containing orthodontic cement. Int. J. Oral Sci. 2018, 9, 24–32. [Google Scholar] [CrossRef]
- Liang, K.; Xiao, S.; Wu, J.; Li, J.; Weir, M.D.; Cheng, L.; Reynolds, M.A.; Zhou, X.; Xu, H.H.K. Long-term dentin remineralization by poly(amido amine) and rechargeable calcium phosphate nanocomposite after fluid challenges. Dent. Mater. 2018, 34, 607–618. [Google Scholar] [CrossRef]
- Gutierrez, M.C.; Jobbágy, M.; Ferrer, M.L.; del Monte, F. Enzymatic synthesis of amorphous calcium phosphate-chitosan nanocomposites and their processing into hierarchical structures. Chem. Mater. 2008, 20, 11–13. [Google Scholar] [CrossRef]
- Hakimimehr, D.; Liu, D.M.; Troczynski, T. In-situ preparation of poly(propylene fumarate)–hydroxyapatite composite. Biomaterials 2005, 26, 7297–7303. [Google Scholar] [CrossRef]
- Antonucci, J.M.; Regnault, W.F.; Skrtic, D. Polymerization shrinkage and stress development in amorphous calcium phosphate/urethane dimethacrylate polymeric composites. J. Compos. Mater. 2010, 44, 355–367. [Google Scholar] [CrossRef]
- Wang, K.W.; Zhu, Y.J.; Chen, F.; Cao, S.W. Calcium phosphate/block copolymer hybrid porous nanospheres: Preparation and application in drug delivery. Mater. Lett. 2010, 64, 2299–2301. [Google Scholar] [CrossRef]
- Cao, S.W.; Zhu, Y.J.; Wu, J.; Wang, K.W.; Tang, Q.L. Preparation and sustained-release property of triblock copolymer/calcium phosphate nanocomposite as nanocarrier for hydrophobic drug. Nanoscale Res. Lett. 2010, 5, 781–785. [Google Scholar] [CrossRef]
- Iwama, R.; Anada, T.; Shiwaku, Y.; Tsuchiya, K.; Takahashi, T.; Suzuki, O. Osteogenic cellular activity around onlaid octacalcium phosphate-gelatin composite onto rat calvaria. J. Biomed. Mater. Res. A 2018, 106A, 1322–1333. [Google Scholar] [CrossRef]
- Yokoi, T. The development of novel calcium phosphate-polymer composite biomaterials with macro- to nano-level controlled hierarchical structures. J. Ceram. Soc. Jpn. 2019, 127, 715–721. [Google Scholar] [CrossRef]
- Suzuki, O. Octacalcium phosphate (OCP)-based bone substitute materials. Jpn. Dent. Sci. Rev. 2013, 49, 58–71. [Google Scholar] [CrossRef]
- Derakhshani, A.; Hesaraki, S.; Nezafati, N.; Azami, M. Wound closure, angiogenesis and antibacterial behaviors of tetracalcium phosphate/hydroxyethyl cellulose/hyaluronic acid/gelatin composite dermal scaffolds. J. Biomat. Sci. Polym. Ed. 2022, 33, 605–626. [Google Scholar] [CrossRef]
- Li, D.; Guo, X.; Du, H.; Ding, W.; Li, M.; Xu, Y. Tetracalcium phosphate/polycaprolactone composite scaffold: Mechanical reinforcement, biodegradability regulation and bioactivity induction. J. Mech. Behav. Biomed. Mater. 2023, 147, 106144. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Self-setting calcium orthophosphate (CaPO4) formulations and their biomedical applications. Adv. Nano-Bio. Mater. Dev. 2019, 3, 321–421. [Google Scholar]
- Brückner, T.; Schamel, M.; Kübler, A.C.; Groll, J.; Gbureck, U. Novel bone wax based on poly(ethylene glycol)–calcium phosphate cement mixtures. Acta Biomater. 2016, 33, 252–263. [Google Scholar] [CrossRef]
- Rödel, M.; Teßmar, J.; Groll, J.; Gbureck, U. Tough and elastic α-tricalcium phosphate cement composites with degradable PEG-based cross-linker. Materials 2019, 12, 53. [Google Scholar] [CrossRef]
- Lou, C.W.; Huang, C.C.; Chen, W.C.; Hu, J.J.; Lu, C.T.; Lin, J.H. Preliminary studies in composite scaffolds of calcium phosphate bone cement with polylactide. Appl. Mech. Mater. 2012, 184–185, 1098–1101. [Google Scholar] [CrossRef]
- Zhong, M.L.; Chen, X.Q.; Fan, H.S.; Zhang, X.D. Incorporation of salmon calcitonin-loaded poly(lactide-co-glycolide) (PLGA) microspheres into calcium phosphate bone cement and the biocompatibility evaluation in vitro. J. Bioact. Compat. Polym. 2012, 27, 133–147. [Google Scholar] [CrossRef]
- Bigi, A.; Bracci, B.; Panzavolta, S. Effect of added gelatin on the properties of calcium phosphate cement. Biomaterials 2004, 25, 2893–2899. [Google Scholar] [CrossRef]
- Bigi, A.; Panzavolta, S.; Sturba, L.; Torricelli, P.; Fini, M.; Giardino, R. Normal and osteopenic bone-derived osteoblast response to a biomimetic gelatin-calcium phosphate bone cement. J. Biomed. Mater. Res. A 2006, 78A, 739–745. [Google Scholar] [CrossRef]
- Panzavolta, S.; Torricelli, P.; Sturba, L.; Bracci, B.; Giardino, R.; Bigi, A. Setting properties and in vitro bioactivity of strontium-enriched gelatin-calcium phosphate bone cements. J. Biomed. Mater. Res. A 2008, 84A, 965–972. [Google Scholar] [CrossRef]
- Maazouz, Y.; Montufar, E.B.; Guillem-Marti, J.; Fleps, I.; Öhman, C.; Persson, C.; Ginebra, M.P. Robocasting of biomimetic hydroxyapatite scaffolds using self-setting inks. J. Mater. Chem. B 2014, 2, 5378–5386. [Google Scholar] [CrossRef]
- Rammelt, S.; Neumann, M.; Hanisch, U.; Reinstorf, A.; Pompe, W.; Zwipp, H.; Biewener, A. Osteocalcin enhances bone remodeling around hydroxyapatite/collagen composites. J. Biomed. Mater. Res. A 2005, 73A, 284–294. [Google Scholar] [CrossRef]
- Park, J.H.; Lee, E.J.; Knowles, J.C.; Kim, H.W. Preparation of in situ hardening composite microcarriers: Calcium phosphate cement combined with alginate for bone regeneration. J. Biomater. Appl. 2014, 28, 1079–1084. [Google Scholar] [CrossRef]
- Wang, X.; Ma, J.; Feng, Q.; Cui, F.Z. Skeletal repair in rabbits with calcium phosphate cements incorporated phosphorylated chitin. Biomaterials 2002, 23, 4591–4600. [Google Scholar] [CrossRef]
- Xue, B.; Zhang, C.; Wang, Y.; Wang, J.; Zhang, J.; Lu, M.; Li, G.; Cao, Z.; Huang, Q. A novel controlled-release system for antibacterial enzyme lysostaphin delivery using hydroxyapatite/chitosan composite bone cement. PLoS ONE 2014, 9, e113797. [Google Scholar] [CrossRef]
- Cui, G.; Li, J.; Lei, W.; Bi, L.; Tang, P.; Liang, Y.; Tao, S.; Wang, Y. The mechanical and biological properties of an injectable calcium phosphate cement-fibrin glue composite for bone regeneration. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 92B, 377–385. [Google Scholar] [CrossRef]
- Han, F.; Shi, C.; Yang, H.; Li, B. Calcium phosphate-silk fibroin composites: Bone cement and beyond. In Developments and Applications of Calcium Phosphate Bone Cements; Liu, C., He, H., Eds.; Springer Series in Biomaterials Science and Engineering; Springer: Singapore, 2018; Volume 9, pp. 449–472. [Google Scholar]
- Cassel, J.B.; Tronco, M.C.; de Melo, B.A.; Oliveira, F.D.S.D.; dos Santos, L.A.L. α-Tricalcium phosphate cement reinforced with silk fibroin: A high strength biomimetic bone cement with chloride-substituted hydroxyapatite. J. Mech. Behav. Biomed. Mater. 2023, 143, 105936. [Google Scholar] [CrossRef]
- Liu, W.; Zhang, J.; Rethore, G.; Khairoun, K.; Pilet, P.; Tancret, F.; Bouler, J.M.; Weiss, P. A novel injectable, cohesive and toughened Si-HPMC (silanized-hydroxypropyl methylcellulose) composite calcium phosphate cement for bone substitution. Acta Biomater. 2014, 10, 3335–3345. [Google Scholar] [CrossRef]
- Mirkiani, S.; Mesgar, A.S.; Mohammadi, Z.; Matinfar, M. Synergetic reinforcement of brushite cements by monetite/apatite whisker-like fibers and carboxymethylcellulose. Materialia 2022, 21, 101329. [Google Scholar] [CrossRef]
- de Lacerda Schickert, S.; Pinto, J.C.; Jansen, J.; Leeuwenburgh, S.C.G.; van den Beucken, J.J.J.P. Tough and injectable fiber reinforced calcium phosphate cement as an alternative to polymethylmethacrylate cement for vertebral augmentation: A biomechanical study. Biomater. Sci. 2020, 8, 4239. [Google Scholar] [CrossRef]
- Luo, J.; Faivre, J.; Engqvist, H.; Persson, C. The addition of poly(vinyl alcohol) fibers to apatitic calcium phosphate cement can improve its toughness. Materials 2019, 12, 1531. [Google Scholar] [CrossRef]
- Duru, İ.; Büyük, N.İ.; Köse, G.T.; Marques, D.W.; Bruce, K.A.; Martin, J.R.; Ege, D. Incorporating the antioxidant fullerenol into calcium phosphate bone cements increases cellular osteogenesis without compromising physical cement characteristics. Adv. Eng. Mater. 2023, 25, 2300301. [Google Scholar] [CrossRef]
- Sadiasa, A.; Sarkar, S.K.; Franco, R.A.; Min, Y.K.; Lee, B.T. Bioactive glass incorporation in calcium phosphate cement-based injectable bone substitute for improved in vitro biocompatibility and in vivo bone regeneration. J. Biomater. Appl. 2014, 28, 739–756. [Google Scholar] [CrossRef]
- El-Fiqi, A.; Kim, J.H.; Kim, H.W. Highly bioactive bone cement microspheres based on α-tricalcium phosphate microparticles/mesoporous bioactive glass nanoparticles: Formulation, physico-chemical characterization and in vivo bone regeneration. Colloids Surface B 2022, 217, 112650. [Google Scholar] [CrossRef]
- Demir-Oğuz, Ö.; Boccaccini, A.R.; Loca, D. Injectable bone cements: What benefits the combination of calcium phosphates and bioactive glasses could bring? Bioact. Mater. 2023, 19, 217–236. [Google Scholar] [CrossRef]
- Richter, R.F.; Ahlfeld, T.; Gelinsky, M.; Lode, A. Composites consisting of calcium phosphate cements and mesoporous bioactive glasses as a 3D plottable drug delivery system. Acta Biomater. 2023, 156, 146–157. [Google Scholar] [CrossRef]
- Richter, R.F.; Vater, C.; Korn, M.; Ahlfeld, T.; Rauner, M.; Pradel, W.; Stadlinger, B.; Gelinsky, M.; Lode, A.; Korn, P. Treatment of critical bone defects using calcium phosphate cement and mesoporous bioactive glass providing spatiotemporal drug delivery. Bioact. Mater. 2023, 28, 402–419. [Google Scholar] [CrossRef]
- Zhou, S.; Ma, J.; Shen, Y.; Haapasalo, M.; Ruse, N.D.; Yang, Q.; Troczynski, T. In vitro studies of calcium phosphate silicate bone cements. J. Mater. Sci. Mater. Med. 2013, 24, 355–364. [Google Scholar] [CrossRef]
- Motisuke, M.; Santos, V.R.; Bazanini, N.C.; Bertran, C.A. Apatite bone cement reinforced with calcium silicate fibers. J. Mater. Sci. Mater. Med. 2014, 25, 2357–2363. [Google Scholar] [CrossRef]
- Correa, D.; Almirall, A.; Carrodeguas, R.G.; dos Santos, L.A.; de Aza, A.H.; Parra, J.; Morejon, L.; Delgado, J.A. α-Tricalcium phosphate cements modified with β-dicalcium silicate and tricalcium aluminate: Physicochemical characterization, in vitro bioactivity and cytotoxicity. J. Biomed. Mater. Res. B Appl. Biomater. 2015, 103B, 72–83. [Google Scholar] [CrossRef]
- Cho, E.; Kim, J.E.; Lee, J.; Park, S.; Lee, S.; Chung, J.H.; Kim, J.; Seonwoo, H. Development of 3D printable calcium phosphate cement scaffolds with cockle shell powders. Materials 2023, 16, 6154. [Google Scholar] [CrossRef]
- Wan, Y.; Ma, H.; Ma, Z.; Tan, L.; Miao, L. Enhanced degradability of the apatite-based calcium phosphate cement incorporated with amorphous MgZnCa alloy. ACS Biomater. Sci. Eng. 2023, 9, 6084–6093. [Google Scholar] [CrossRef]
- Perez, R.A.; Patel, K.D.; Kim, H.W. Novel magnetic nanocomposite injectables: Calcium phosphate cements impregnated with ultrafine magnetic nanoparticles for bone regeneration. RSC Adv. 2015, 5, 13411–13419. [Google Scholar] [CrossRef]
- Elahpour, N.; Rabiee, S.M.; Ebrahimzadeh, M.H.; Moradi, A. In-vitro formation and growth kinetics of apatite on a new light-cured composite calcium phosphate cement. Ceram. Int. 2018, 44, 15317–15322. [Google Scholar] [CrossRef]
- Wang, Y.; Peng, Z.; Zhang, D.; Song, D. Tough, injectable calcium phosphate cement based composite hydrogels to promote osteogenesis. Gels 2023, 9, 302. [Google Scholar] [CrossRef]
- Canal, C.; Ginebra, M.P. Fibre-reinforced calcium phosphate cements: A review. J. Mech. Behav. Biomed. Mater. 2011, 4, 1658–1671. [Google Scholar] [CrossRef]
- Hasan, M.S.; Carpenter, N.; Wei, T.L.; McNally, D.; Ahmed, I.; Boszczyk, B.M. Effects of adding resorbable phosphate glass fibres and PLA to calcium phosphate bone cements. J. Appl. Biomater. Funct. Mater. 2014, 12, 203–209. [Google Scholar] [CrossRef]
- Low, K.L.; Tan, S.H.; Zein, S.H.S.; McPhail, D.S.; Boccaccini, A.R. Optimization of the mechanical properties of calcium phosphate/multi-walled carbon nanotubes/bovine serum albumin composites using response surface methodology. Mater. Des. 2011, 32, 3312–3319. [Google Scholar] [CrossRef]
- Chew, K.K.; Low, K.L.; Zein, S.H.S.; McPhail, D.S.; Gerhardt, L.C.; Roether, J.A.; Boccaccini, A.R. Reinforcement of calcium phosphate cement with multiwalled carbon nanotubes and bovine serum albumin for injectable bone substitute applications. J. Mech. Behav. Biomed. Mater. 2011, 4, 331–339. [Google Scholar] [CrossRef]
- Ruiz, J.; Moreno, D.; Copete, H.; Vargas, F.; López, M.E. Calcium phosphate cements improved by addition of carbonated hydroxyapatite type B. Bol. Soc. Esp. Ceram. V 2023, 62, 315–328. [Google Scholar] [CrossRef]
- Zima, A.; Czechowska, J.; Szponder, T.; Ślósarczyk, A. In vivo behavior of biomicroconcretes based on α-tricalcium phosphate and hybrid hydroxyapatite/chitosan granules and sodium alginate. J. Biomed. Mater. Res. A 2020, 108A, 1243–1255. [Google Scholar] [CrossRef]
- Czechowska, J.; Cichoń, E.; Belcarz, A.; Ślósarczyk, A.; Zima, A. Effect of gold nanoparticles and silicon on the bioactivity and antibacterial properties of hydroxyapatite/chitosan/tricalcium phosphate-based biomicroconcretes. Materials 2021, 14, 3854. [Google Scholar] [CrossRef]
- Kim, S.B.; Kim, Y.J.; Yoon, T.L.; Park, S.A.; Cho, I.H.; Kim, E.J.; Kim, I.A.; Shin, J.W. The characteristics of a hydroxyapatite-chitosan-PMMA bone cement. Biomaterials 2004, 25, 5715–5723. [Google Scholar] [CrossRef]
- Vallo, C.I.; Montemartini, P.E.; Fanovich, M.A.; Lópes, J.M.P.; Cuadrado, T.R. Polymethylmethacrylate-based bone cement modified with hydroxyapatite. J. Biomed. Mater. Res. B Appl. Biomater. 1999, 48, 150–158. [Google Scholar] [CrossRef]
- Moursi, A.M.; Winnard, A.V.; Winnard, P.L.; Lannutti, J.J.; Seghi, R.R. Enhanced osteoblast response to a PMMA–HA composite. Biomaterials 2002, 23, 133–144. [Google Scholar] [CrossRef]
- Dalby, M.J.; di Silvio, L.; Harper, E.J.; Bonfield, W. Increasing hydroxyapatite incorporation into poly(methylmethacrylate) cement increases osteoblast adhesion and response. Biomaterials 2002, 23, 569–576. [Google Scholar] [CrossRef]
- Itokawa, H.; Hiraide, T.; Moriya, M.; Fujimoto, M.; Nagashima, G.; Suzuki, R.; Fujimoto, T. A 12 month in vivo study on the response of bone to a hydroxyapatite-polymethylmethacrylate cranioplasty composite. Biomaterials 2007, 28, 4922–4927. [Google Scholar] [CrossRef]
- Tham, W.L.; Chow, W.S.; Ishak, Z.A.M. Flexural and morphological properties of poly(methyl methacrylate)/hydroxyapatite composites: Effects of planetary ball mill grinding time. J. Reinf. Plastics Compos. 2010, 29, 2065–2075. [Google Scholar] [CrossRef]
- Bai, H.; Walsh, F.; Gludovatz, B.; Delattre, B.; Huang, C.; Chen, Y.; Tomsia, A.P.; Ritchie, R.O. Bioinspired hydroxyapatite/poly(methyl methacrylate) composite with a nacre-mimetic architecture by a bidirectional freezing method. Adv. Mater. 2016, 28, 50–56. [Google Scholar] [CrossRef]
- Harper, E.J.; Behiri, J.C.; Bonfield, W. Flexural and fatigue properties of a bone cement based upon polyethylmethacrylate and hydroxyapatite. J. Mater. Sci. Mater. Med. 1995, 6, 799–803. [Google Scholar] [CrossRef]
- Arnold, J.C.; Venditti, N.P. Prediction of the long-term creep behaviour of hydroxyapatite-filled polyethylmethacrylate bone cements. J. Mater. Sci. Mater. Med. 2007, 18, 1849–1858. [Google Scholar] [CrossRef]
- Ohgaki, M.; Yamashita, K. Preparation of polymethylmethacrylate-reinforced functionally graded hydroxyapatite composites. J. Am. Ceram. Soc. 2003, 86, 1440–1442. [Google Scholar] [CrossRef]
- Del Real, R.P.; Padilla, S.; Vallet-Regi, M. Gentamicin release from hydroxyapatite/poly(ethyl methacrylate)/poly(methyl methacrylate)composites. J. Biomed. Mater. Res. 2000, 52, 1–7. [Google Scholar] [CrossRef]
- Bakina, O.; Svarovskaya, N.; Ivanova, L.; Glazkova, E.; Rodkevich, N.; Evstigneev, V.; Evstigneev, M.; Mosunov, A.; Lerner, M. New PMMA-based hydroxyapatite/ZnFe2O4/ZnO composite with antibacterial performance and low toxicity. Biomimetics 2023, 8, 488. [Google Scholar] [CrossRef]
- Saito, M.; Maruoka, A.; Mori, T.; Sugano, N.; Hino, K. Experimental studies on a new bioactive bone cement: Hydroxyapatite composite resin. Biomaterials 1994, 15, 156–160. [Google Scholar] [CrossRef]
- Kawagoe, K.; Saito, M.; Shibuya, T.; Nakashima, T.; Hino, K.; Yoshikawa, H. Augmentation of cancellous screw fixation with hydroxyapatite composite resin (CAP) in vivo. J. Biomed. Mater. Res. 2000, 53, 678–684. [Google Scholar] [CrossRef]
- Turner, A.W.L.; Gillies, R.M.; Svehla, M.J.; Saito, M.; Walsh, W.R. Hydroxyapatite composite resin cement augmentation of pedicle screw fixation. Clin. Orthop. Rel. Res. 2003, 406, 253–261. [Google Scholar] [CrossRef]
- Watson, K.E.; Ten Huisen, K.S.; Brown, P.W. The formation of hydroxyapatite–calcium polyacrylate composites. J. Mater. Sci. Mater. Med. 1999, 10, 205–213. [Google Scholar] [CrossRef]
- Reed, C.S.; Ten Huisen, K.S.; Brown, P.W.; Allcock, H.R. Thermal stability and compressive strength of calcium-deficient hydroxyapatite–poly[bis(carboxylatophenoxy)phosphazene] composites. Chem. Mater. 1996, 8, 440–447. [Google Scholar] [CrossRef]
- Peter, S.J.; Kim, P.; Yasko, A.W.; Yaszemski, M.J.; Mikos, A.G. Crosslinking characteristics of an injectable poly(propylene fumarate)/β-tricalcium phosphate paste and mechanical properties of the crosslinked composite for use as a biodegradable bone cement. J. Biomed. Mater. Res. 1999, 44, 314–321. [Google Scholar] [CrossRef]
- He, S.; Yaszemski, M.J.; Yasko, A.W.; Engel, P.S.; Mikos, A.G. Injectable biodegradable polymer composites based on poly (propylene fumarate) crosslinked with poly(ethylene glycol)-dimethacrylate. Biomaterials 2000, 21, 2389–2394. [Google Scholar] [CrossRef]
- Ignjatovic, N.; Jovanovic, J.; Suljovrujic, E.; Uskokovic, D. Injectable polydimethylsiloxane/hydroxyapatite composite cement. Biomed. Mater. Eng. 2003, 13, 401–410. [Google Scholar]
- Fei, Z.; Hu, Y.; Wu, D.; Wu, H.; Lu, R.; Bai, J.; Song, H. Preparation and property of a novel bone graft composite consisting of rhBMP-2 loaded PLGA microspheres and calcium phosphate cement. J. Mater. Sci. Mater. Med. 2008, 19, 1109–1116. [Google Scholar] [CrossRef]
- Link, D.P.; van den Dolder, J.; van den Beucken, J.J.J.P.; Cuijpers, V.M.; Wolke, J.G.C.; Mikos, A.G.; Jansen, J.A. Evaluation of the biocompatibility of calcium phosphate cement/PLGA microparticle composites. J. Biomed. Mater. Res. A 2008, 87A, 760–769. [Google Scholar] [CrossRef]
- Chiang, T.Y.; Ho, C.C.; Chen, D.C.H.; Lai, M.H.; Ding, S.J. Physicochemical properties and biocompatibility of chitosan oligosaccharide/gelatin/calcium phosphate hybrid cements. Mater. Chem. Phys. 2010, 120, 282–288. [Google Scholar] [CrossRef]
- Fujishiro, Y.; Takahashi, K.; Sato, T. Preparation and compressive strength of α-tricalcium phosphate/gelatin gel composite cement. J. Biomed. Mater. Res. 2001, 54, 525–530. [Google Scholar] [CrossRef]
- Miyazaki, K.; Horibe, T.; Antonucci, J.M.; Takagi, S.; Chow, L.C. Polymeric calcium phosphate cements: Analysis of reaction products and properties. Dental Mater. 1993, 9, 41–45. [Google Scholar] [CrossRef]
- Miyazaki, K.; Horibe, T.; Antonucci, J.M.; Takagi, S.; Chow, L.C. Polymeric calcium phosphate cements: Setting reaction modifiers. Dental Mater. 1993, 9, 46–50. [Google Scholar] [CrossRef]
- Dos Santos, L.A.; de Oliveira, L.C.; Rigo, E.C.S.; Carrodeguas, R.G.; Boschi, A.O.; de Arruda, A.C.F. Influence of polymeric additives on the mechanical properties of α-tricalcium phosphate cement. Bone 1999, 25, 99S–102S. [Google Scholar] [CrossRef]
- Greish, Y.E.; Brown, P.W.; Bender, J.D.; Allcockm, H.R.; Lakshmim, S.; Laurencin, C.T. Hydroxyapatite-polyphosphazane composites prepared at low temperatures. J. Am. Ceram. Soc. 2007, 90, 2728–2734. [Google Scholar] [CrossRef]
- Greish, Y.E.; Bender, J.D.; Lakshmi, S.; Brown, P.W.; Allcock, H.R.; Laurencin, C.T. Formation of hydroxyapatite-polyphosphazene polymer composites at physiologic temperature. J. Biomed. Mater. Res. A 2006, 77A, 416–425. [Google Scholar] [CrossRef]
- Greish, Y.E.; Bender, J.D.; Lakshmi, S.; Brown, P.W.; Allcock, H.R.; Laurencin, C.T. Low temperature formation of hydroxyapatite-poly(alkyl oxybenzoate) phosphazene composites for biomedical applications. Biomaterials 2005, 26, 1–9. [Google Scholar] [CrossRef]
- Mickiewicz, R.A.; Mayes, A.M.; Knaack, D. Polymer–calcium phosphate cement composites for bone substitutes. J. Biomed. Mater. Res. 2002, 61, 581–592. [Google Scholar] [CrossRef]
- Carey, L.E.; Xu, H.H.K.; Simon, C.G.; Takagi, S.; Chow, L.C. Premixed rapid-setting calcium phosphate composites for bone repair. Biomaterials 2005, 26, 5002–5014. [Google Scholar] [CrossRef]
- Krüger, R.; Seitz, J.M.; Ewald, A.; Bach, F.W.; Groll, J. Strong and tough magnesium wire reinforced phosphate cement composites for load-bearing bone replacement. J. Mech. Behav. Biomed. Mater. 2013, 20, 36–44. [Google Scholar] [CrossRef]
- Miao, X.; Tan, L.P.; Tan, L.S.; Huang, X. Porous calcium phosphate ceramics modified with PLGA–bioactive glass. Mater. Sci. Eng. C 2007, 27, 274–279. [Google Scholar] [CrossRef]
- Lickorish, D.; Guan, L.; Davies, J.E. A three-phase, fully resorbable, polyester/calcium phosphate scaffold for bone tissue engineering: Evolution of scaffold design. Biomaterials 2007, 28, 1495–1502. [Google Scholar] [CrossRef]
- Qian, G.; Fan, P.; He, F.; Ye, J. Novel strategy to accelerate bone regeneration of calcium phosphate cement by incorporating 3D plotted poly(lactic-co-glycolic acid) network and bioactive wollastonite. Adv. Healthc. Mater. 2019, 8, 1801325. [Google Scholar] [CrossRef]
- Iwasakia, Y.; Takahataa, Y.; Fujii, S. Self-setting particle-stabilized emulsion for hard-tissue engineering. Colloid Surface B 2015, 126, 394–400. [Google Scholar] [CrossRef]
- Xu, H.H.K.; Simon, C.G. Fast setting calcium phosphate-chitosan scaffold: Mechanical properties and biocompatibility. Biomaterials 2005, 26, 1337–1348. [Google Scholar] [CrossRef]
- Zhang, L.; Li, Y.; Zhou, G.; Lu, G.Y.; Zuo, Y. Setting mechanism of nano-hydroxyapatite/chitosan bone cement. J. Inorg. Mater. 2006, 21, 1197–1202. [Google Scholar]
- Ruhe, P.Q.; Hedberg, E.L.; Padron, N.T.; Spauwen, P.H.M.; Jansen, J.A.; Mikos, A.G. Biocompatibility and degradation of poly(D,L-lactic-co-glycolic acid)/calcium phosphate cement composites. J. Biomed. Mater. Res. A 2005, 74A, 533–544. [Google Scholar] [CrossRef]
- Guo, D.G.; Sun, H.L.; Xu, K.W.; Han, Y. Long-term variations in mechanical properties and in vivo degradability of CPC/PLGA composite. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 82B, 533–544. [Google Scholar]
- Habraken, W.J.E.M.; Wolke, J.G.C.; Mikos, A.G.; Jansen, J.A. Injectable PLGA microsphere/calcium phosphate cements: Physical properties and degradation characteristics. J. Biomater. Sci. Polym. Edn. 2006, 17, 1057–1074. [Google Scholar] [CrossRef]
- Ruhe, P.Q.; Hedberg-Dirk, E.L.; Padron, N.T.; Spauwen, P.H.M.; Jansen, J.A.; Mikos, A.G. Porous poly (D,L-lactic-co-glycolic acid)/calcium phosphate cement composite for reconstruction of bone defects. Tissue Eng. 2006, 12, 789–800. [Google Scholar] [CrossRef]
- Ruhe, P.Q.; Hedberg, E.L.; Padron, N.T.; Spauwen, P.H.M.; Jansen, J.A.; Mikos, A.G. rhBMP-2 release from injectable poly (D,L-lactic-co-glycolic acid)/calcium phosphate composites. J. Bone Joint Surg. 2003, 85A (Suppl. S3), 75–81. [Google Scholar] [CrossRef]
- Plachokova, A.; Link, D.; van den Dolder, J.; van den Beucken, J.; Jansen, J.A. Bone regenerative properties of injectable PGLA–CaP composite with TGF-β1 in a rat augmentation model. J. Tissue Eng. Regen. Med. 2007, 1, 457–464. [Google Scholar] [CrossRef]
- Roy, A.; Jhunjhunwala, S.; Bayer, E.; Fedorchak, M.; Little, S.R.; Kumta, P.N. Porous calcium phosphate–poly (lactic-co-glycolic) acid composite bone cement: A viable tunable drug delivery system. Mater. Sci. Eng. C 2016, 59, 92–101. [Google Scholar] [CrossRef]
- Bian, T.; Zhao, K.; Meng, Q.; Jiao, H.; Tang, Y.; Luo, J. Fabrication and performance of calcium phosphate cement/small intestinal submucosa composite bionic bone scaffolds with different microstructures. Ceram. Int. 2018, 44, 9181–9187. [Google Scholar] [CrossRef]
- Moussi, H.; Weiss, P.; le Bideau, J.; Gautier, H.; Charbonnier, B. Injectable macromolecule-based calcium phosphate bone substitutes. Mater. Adv. 2022, 3, 6125–6141. [Google Scholar] [CrossRef]
- Liu, S.; Hu, Y.; Zhang, J.; Bao, S.; Xian, L.; Dong, X.; Zheng, W.; Li, Y.; Gao, H.; Zhou, W. Bioactive and biocompatible macroporous scaffolds with tunable performances prepared based on 3D printing of the pre-crosslinked sodium alginate/hydroxyapatite hydrogel ink. Macromol. Mater. Eng. 2019, 304, 1800698. [Google Scholar] [CrossRef]
- Zhou, Z.X.; Buchanan, F.; Mitchell, C.; Dunne, N. Printability of calcium phosphate: Calcium sulfate powders for the application of tissue engineered bone scaffolds using the 3D printing technique. Mater. Sci. Eng. C 2014, 38, 1–10. [Google Scholar] [CrossRef]
- Torrejon-Moya, A.; Apalimova, A.; González-Navarro, B.; Zaera-Le Gal, R.; Marí-Roig, A.; López-López, J. Calcium sulfate in implantology (biphasic calcium sulfate/hydroxyapatite, BCS/HA, Bond Apatite®): Review of the literature and case reports. Coatings 2022, 12, 1350. [Google Scholar] [CrossRef]
- Zhang, Y.; Xie, L.; Jiao, X.; Yue, X.; Xu, Y.; Wang, C.; Li, Y.; Yang, X.; Yang, G.; Xu, S.; et al. Preferentially biodegradable gypsum fibers endowing invisible microporous structures and enhancing osteogenic capability of calcium phosphate cements. ACS Biomater. Sci. Eng. 2024, 10, 1077–1089. [Google Scholar] [CrossRef]
- Liu, J.; Qiu, F.; Zou, Y.; Zhang, Z.; Wang, A.; Zhang, Y. Physicochemical and biological properties of composite bone cement based on octacalcium phosphate and tricalcium silicate. Ceram. Int. 2023, 49, 20315–20325. [Google Scholar] [CrossRef]
- Stepanova, K.; Lytkina, D.; Sadykov, R.; Shalygina, K.; Khojazoda, T.; Mahmadbegov, R.; Kurzina, I. Composite cement materials based on β-tricalcium phosphate, calcium sulfate and a mixture of polyvinyl alcohol and polyvinylpyrrolidone intended for osteanagenesis. Polymers 2023, 15, 210. [Google Scholar] [CrossRef]
- Gao, H.; Ji, B.; Jager, I.L.; Arzt, E.; Fratzl, P. Materials become insensitive to flaws at nanoscale: Lessons from nature. Proc. Nat. Acad. Sci. USA 2003, 100, 5597–5600. [Google Scholar] [CrossRef]
- Webster, T.J. Nanophase ceramics: The future orthopedic and dental implant material. Adv. Chem. Eng. 2001, 27, 125–166. [Google Scholar]
- Webster, T.J.; Ergun, C.; Doremus, R.H.; Siegel, R.W.; Bizios, R. Enhanced functions of osteoblasts on nanophase ceramics. Biomaterials 2000, 21, 1803–1810. [Google Scholar] [CrossRef]
- Zakaria, S.M.; Zein, S.H.S.; Othman, M.R.; Yang, F.; Jansen, J.A. Nanophase hydroxyapatite as a biomaterial in advanced hard tissue engineering: A review. Tissue Eng. B 2013, 19, 431–441. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Nanometric calcium orthophosphates (CaPO4): Preparation, properties and biomedical applications. Adv. Nano-Bio. Mater. Dev. 2019, 3, 422–513. [Google Scholar]
- Li, G.; Huang, J.; Li, Y.; Zhang, R.; Deng, B.; Zhang, J.; Aoki, H. In vitro study on influence of a discrete nano-hydroxyapatite on leukemia P388 cell behavior. Biomed. Mater. Eng. 2007, 17, 321–327. [Google Scholar]
- Mizutani, T.; Okuda, N. Bioinspired mechanical materials–development of high-toughness ceramics through complexation of calcium phosphate and organic polymers. Ceramics 2023, 6, 2117–2133. [Google Scholar] [CrossRef]
- Xu, H.H.K.; Sun, L.; Weir, M.D.; Takagi, S.; Chow, L.C.; Hockey, B. Effects of incorporating nanosized calcium phosphate particles on properties of whisker-reinforced dental composites. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 81B, 116–125. [Google Scholar] [CrossRef]
- Shu, X.; Shi, Q.; Feng, J.; Xie, X.; Chen, Y. Design and in vitro evaluation of novel γ-PGA/hydroxyapatite nanocomposites for bone tissue engineering. J. Mater. Sci. 2014, 49, 7742–7749. [Google Scholar] [CrossRef]
- Hong, Z.K.; Zhang, P.B.; He, C.L.; Qiu, X.Y.; Liu, A.X.; Chen, L.; Chen, X.; Jing, X. Nanocomposite of poly(L-lactide) and surface grafted hydroxyapatite: Mechanical properties and biocompatibility. Biomaterials 2005, 26, 6296–6304. [Google Scholar] [CrossRef]
- Kothapalli, C.R.; Shaw, M.T.; Wei, M. Biodegradable HA-PLA 3-D porous scaffolds: Effect of nano-sized filler content on scaffold properties. Acta Biomater. 2005, 1, 653–662. [Google Scholar] [CrossRef]
- Aydin, E.; Planell, J.A.; Hasirci, V. Hydroxyapatite nanorod-reinforced biodegradable poly(L-lactic acid) composites for bone plate applications. J. Mater. Sci. Mater. Med. 2011, 22, 2413–2427. [Google Scholar] [CrossRef]
- Chae, T.; Yang, H.; Ko, F.; Troczynski, T. Bio-inspired dicalcium phosphate anhydrate/poly(lactic acid) nanocomposite fibrous scaffolds for hard tissue regeneration: In situ synthesis and electrospinning. J. Biomed. Mater. Res. A 2014, 102A, 514–522. [Google Scholar] [CrossRef]
- Liu, Z.; Chen, Y.; Ding, W.; Zhang, C. Filling behavior, morphology evolution and crystallization behavior of microinjection molded poly(lactic acid)/hydroxyapatite nanocomposites. Compos. A 2015, 72, 85–95. [Google Scholar] [CrossRef]
- Nguyen, N.M.; Kakarla, A.B.; Nukala, S.G.; Kong, C.; Baji, A.; Kong, I. Evaluation of physicochemical properties of a hydroxyapatite polymer nanocomposite for use in fused filament fabrication. Polymers 2023, 15, 3980. [Google Scholar] [CrossRef]
- Hong, Z.; Zhang, P.; Liu, A.; Chen, L.; Chen, X.; Jing, X. Composites of poly(lactide-co-glycolide) and the surface modified carbonated hydroxyapatite nanoparticles. J. Biomed. Mater. Res. A 2007, 81A, 515–522. [Google Scholar] [CrossRef]
- Huang, Y.X.; Ren, J.; Chen, C.; Ren, T.B.; Zhou, X.Y. Preparation and properties of poly(lactide-co-glycolide) (PLGA)/nano-hydroxyapatite (NHA) scaffolds by thermally induced phase separation and rabbit MSCs culture on scaffolds. J. Biomater. Appl. 2008, 22, 409–432. [Google Scholar] [CrossRef]
- Xue, D.; Zheng, Q.; Zong, C.; Li, Q.; Li, H.; Qian, S.; Zhang, B.; Yu, L.; Pan, Z. Osteochondral repair using porous poly(lactide-co-glycolide)/nano-hydroxyapatite hybrid scaffolds with undifferentiated mesenchymal stem cells in a rat model. J. Biomed. Mater. Res. A 2010, 94A, 259–270. [Google Scholar] [CrossRef]
- Torabinejad, B.; Mohammadi-Rovshandeh, J.; Davachi, S.M.; Zamanian, A. Synthesis and characterization of nanocomposite scaffolds based on triblock copolymer of L-lactide, ε-caprolactone and nano-hydroxyapatite for bone tissue engineering. Mater. Sci. Eng. C 2014, 42, 199–210. [Google Scholar] [CrossRef]
- Solechan, S.; Suprihanto, A.; Widyanto, S.A.; Triyono, J.; Fitriyana, D.F.; Siregar, J.P.; Cionita, T. Characterization of PLA/PCL/nano-hydroxyapatite (nHA) biocomposites prepared via cold isostatic pressing. Polymers 2023, 15, 559. [Google Scholar] [CrossRef]
- Yazdanpanah, Z.; Sharma, N.K.; Raquin, A.; Cooper, D.M.L.; Chen, X.; Johnston, J.D. Printing tissue-engineered scaffolds made of polycaprolactone and nano-hydroxyapatite with mechanical properties appropriate for trabecular bone substitutes. BioMed. Eng. OnLine 2023, 22, 73. [Google Scholar] [CrossRef]
- Kikuchi, M.; Itoh, S.; Ichinose, S.; Shinomiya, K.; Tanaka, J. Self-organization mechanism in a bone-like hydroxyapatite/collagen nanocomposite synthesized in vitro and its biological reaction in vivo. Biomaterials 2001, 22, 1705–1711. [Google Scholar] [CrossRef]
- Kikuchi, M.; Matsumoto, H.N.; Yamada, T.; Koyama, Y.; Takakuda, K.; Tanaka, J. Glutaraldehyde cross-linked hydroxyapatite/collagen self-organized nanocomposites. Biomaterials 2004, 25, 63–69. [Google Scholar] [CrossRef]
- Lynn, A.K.; Nakamura, T.; Patel, N.; Porter, A.E.; Renouf, A.C.; Laity, P.R.; Best, S.M.; Cameron, R.E.; Shimizu, Y.; Bonfield, W. Composition-controlled nanocomposites of apatite and collagen incorporating silicon as osseopromotive agent. J. Biomed. Mater. Res. A 2005, 74A, 447–453. [Google Scholar] [CrossRef]
- Chang, M.C.; Tanaka, J. FTIR study for hydroxyapatite/collagen nanocomposite cross-linked by glutaraldehyde. Biomaterials 2002, 23, 4811–4818. [Google Scholar] [CrossRef]
- Chang, M.C.; Tanaka, J. XPS study for the microstructure development of hydroxyapatite-collagen nanocomposites cross-linked using glutaraldehyde. Biomaterials 2002, 23, 3879–3885. [Google Scholar] [CrossRef]
- Fukui, N.; Sato, T.; Kuboki, Y.; Aoki, H. Bone tissue reaction of nano-hydroxyapatite/collagen composite at the early stage of implantation. Biomed. Mater. Eng. 2008, 18, 25–33. [Google Scholar]
- Kim, T.G.; Park, S.H.; Chung, H.J.; Yang, D.Y.; Park, T.G. Microstructured scaffold coated with hydroxyapatite/collagen nanocomposite multilayer for enhanced osteogenic induction of human mesenchymal stem cells. J. Mater. Chem. 2010, 20, 8927–8933. [Google Scholar] [CrossRef]
- Chen, L.; Hu, J.; Ran, J.; Shen, X.; Tong, H. Synthesis and cytocompatibility of collagen/hydroxyapatite nanocomposite scaffold for bone tissue engineering. Polym. Compos. 2016, 37, 81–90. [Google Scholar] [CrossRef]
- Sri, A.K.; Arthi, C.; Neya, N.R.; Hikku, G.S. Nano-hydroxyapatite/collagen composite as scaffold material for bone regeneration. Biomed. Mater. 2023, 18, 032002. [Google Scholar]
- Liao, S.S.; Cui, F.Z.; Zhu, Y. Osteoblasts adherence and migration through three-dimensional porous mineralized collagen based composite: nHAC/PLA. J. Bioact. Compat. Polym. 2004, 19, 117–130. [Google Scholar] [CrossRef]
- Liao, S.S.; Cui, F.Z.; Zhang, W.; Feng, Q.L. Hierarchically biomimetic bone scaffold materials: Nano-HA/collagen/PLA composite. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 69B, 158–165. [Google Scholar] [CrossRef]
- Liao, S.S.; Cui, F.Z. In vitro and in vivo degradation of the mineralized collagen based composite scaffold: Nanohydroxyapatite/collagen/poly(L-lactide). Tissue Eng. 2004, 10, 73–80. [Google Scholar] [CrossRef]
- Liao, S.S.; Wang, W.; Uo, M.; Ohkawa, S.; Akasaka, T.; Tamura, K.; Cui, F.Z.; Watari, F. A three-layered nano-carbonated hydroxyapatite/collagen/PLGA composite membrane for guided tissue regeneration. Biomaterials 2005, 26, 7564–7571. [Google Scholar] [CrossRef]
- Liao, S.; Watari, F.; Zhu, Y.; Uo, M.; Akasaka, T.; Wang, W.; Xu, G.; Cui, F.Z. The degradation of the three layered nano-carbonated hydroxyapatite/collagen/PLGA composite membrane in vitro. Dent. Mater. 2007, 23, 1120–1128. [Google Scholar] [CrossRef]
- Degirmenbasi, N.; Kalyon, D.M.; Birinci, E. Biocomposites of nanohydroxyapatite with collagen and poly(vinyl alcohol). Colloids Surf. B 2006, 48, 42–49. [Google Scholar] [CrossRef]
- Zhang, S.M.; Cui, F.Z.; Liao, S.S.; Zhu, Y.; Han, L. Synthesis and biocompatibility of porous nanohydroxyapatite/collagen/alginate composite. J. Mater. Sci. Mater. Med. 2003, 14, 641–645. [Google Scholar] [CrossRef]
- Sotome, S.; Uemura, T.; Kikuchi, M.; Chen, J.; Itoh, S.; Tanaka, J.; Tateishi, T.; Shinomiya, K. Synthesis and in vivo evaluation of a novel hydroxyapatite/collagen-alginate as a bone filler and a drug delivery carrier of bone morphogenetic protein. Mater. Sci. Eng. C 2004, 24, 341–347. [Google Scholar] [CrossRef]
- Chang, M.C.; Ikoma, T.; Tanaka, J. Cross-linkage of hydroxyapatite/gelatin nanocomposite using EGDE. J. Mater. Sci. 2004, 39, 5547–5550. [Google Scholar] [CrossRef]
- Teng, S.; Shi, J.; Peng, B.; Chen, L. The effect of alginate addition on the structure and morphology of hydroxyapatite/gelatin nanocomposites. Compos. Sci. Technol. 2006, 66, 1532–1538. [Google Scholar] [CrossRef]
- Mobini, S.; Javadpour, J.; Hosseinalipour, M.; Ghazi-Khansari, M.; Khavandi, A.; Rezaie, H.R. Synthesis and characterisation of gelatin-nano hydroxyapatite composite scaffolds for bone tissue engineering. Adv. Appl. Ceram. 2008, 107, 4–8. [Google Scholar] [CrossRef]
- Wang, H.; Bongio, M.; Farbod, K.; Nijhuis, A.W.; van den Beucken, J.; Boerman, O.C.; van Hest, J.C.; Li, Y.; Jansen, J.A.; Leeuwenburgh, S.C.G. Development of injectable organic/inorganic colloidal composite gels made of self-assembling gelatin nanospheres and calcium phosphate nanocrystals. Acta Biomater. 2014, 10, 508–519. [Google Scholar] [CrossRef]
- Maulida, H.N.; Hikmawati, D.; Budiatin, A.S. Injectable bone substitute paste based on hydroxyapatite, gelatin and streptomycin for spinal tuberculosis. J. Spine 2015, 4, 1000266. [Google Scholar] [CrossRef]
- Hachinohe, Y.; Taira, M.; Hoshi, M.; Yoshida, D.; Hatakeyama, W.; Sawada, T.; Kondo, H. Self-prepared hyaluronic acid/alkaline gelatin composite with nano-hydroxyapatite and bone morphogenetic protein for cranial bone formation. Int. J. Mol. Sci. 2023, 24, 1104. [Google Scholar] [CrossRef]
- Lewandrowski, K.U.; Bondre, S.P.; Wise, D.L.; Trantolo, D.J. Enhanced bioactivity of a poly(propylene fumarate) bone graft substitute by augmentation with nano-hydroxyapatite. Biomed. Mater. Eng. 2003, 13, 115–124. [Google Scholar]
- Klein, T.R.; Kirillova, A.; Galla, K.; Becker, M.L. Influence of post-processing on the properties of 3D-printed poly(propylene fumarate) star polymer hydroxyapatite nanocomposites. RSC Appl. Polym. 2023, 1, 73–81. [Google Scholar] [CrossRef]
- Wei, J.; Li, Y.; Chen, W.; Zuo, Y. A study on nano-composite of hydroxyapatite and polyamide. J. Mater. Sci. 2003, 38, 3303–3306. [Google Scholar] [CrossRef]
- Wang, H.; Li, Y.; Zuo, Y.; Li, J.; Ma, S.; Cheng, L. Biocompatibility and osteogenesis of biomimetic nano-hydroxyapatite/polyamide composite scaffolds for bone tissue engineering. Biomaterials 2007, 28, 3338–3348. [Google Scholar] [CrossRef]
- Zhang, X.; Li, Y.; Zuo, Y.; Lv, G.Y.; Mu, Y.H.; Li, H. Morphology, hydrogen-bonding and crystallinity of nano-hydroxyapatite/polyamide 66 biocomposites. Compos. A 2007, 38, 843–848. [Google Scholar] [CrossRef]
- Zhang, X.; Li, Y.; Lv, G.Y.; Zuo, Y.; Mu, Y.H.; Lan, W. The study on interaction mechanism between n-HA and PA66 in n-HA/PA66 biocomposites. Funct. Mater. 2005, 36, 896–899. [Google Scholar]
- Menon, D.; Anand, K.A.; Anitha, V.C.; Nair, S. Hydroxyapatite-reinforced polyamide 6,6 nanocomposites through melt compounding. Int. J. Polym. Mater. 2010, 59, 498–509. [Google Scholar] [CrossRef]
- Hu, G.; Wang, H.; Yao, X.; Bi, D.; Zhu, G.; Tang, S.; Wei, J.; Yang, L.; Tong, P.; Xiao, L. Development of nanofluorapatite polymer-based composite for bioactive orthopedic implants and prostheses. Int. J. Nanomed. 2014, 9, 3875–3884. [Google Scholar] [CrossRef]
- Yusong, P.; Dangsheng, X.; Xiaolin, C. Mechanical properties of nanohydroxyapatite reinforced poly(vinyl alcohol) gel composites as biomaterial. J. Mater. Sci. 2007, 42, 5129–5134. [Google Scholar] [CrossRef]
- Xu, F.; Li, Y.; Wang, X.; Wei, J.; Yang, A. Preparation and characterization of nano-hydroxyapatite/poly(vinyl alcohol) hydrogel biocomposite. J. Mater. Sci. 2004, 39, 5669–5672. [Google Scholar]
- Wang, H.S.; Wang, G.X.; Pan, Q.X. Electrochemical study of the interactions of DNA with redox-active molecules based on the immobilization of dsDNA on the sol-gel derived nano porous hydroxyapatite-polyvinyl alcohol hybrid material coating. Electroanalysis 2005, 17, 1854–1860. [Google Scholar] [CrossRef]
- Bobrowska, K.; Sadowska, K.; Golec, P.; Bilewicz, R.; Stolarczyk, K.; Przesniak-Welenc, M. Bovine serum albumin–hydroxyapatite nanoflowers as potential local drug delivery system of ciprofloxacin. Int. J. Nanomed. 2023, 18, 6449–6467. [Google Scholar] [CrossRef]
- Pramanik, N.; Mohapatra, S.; Pramanik, P.; Bhargava, P. Processing and properties of nano-hydroxyapatite (n-HAp)/poly(ethylene-co-acrylic acid) (EAA) composite using a phosphonic acid coupling agent for orthopedic applications. J. Am. Ceram. Soc. 2007, 90, 369–375. [Google Scholar] [CrossRef]
- Pramanik, N.; Bhargava, P.; Alam, S.; Pramanik, P. Processing and properties of nano- and macro-hydroxyapatite/poly(ethylene-co-acrylic acid) composites. Polym. Compos. 2006, 27, 633–641. [Google Scholar] [CrossRef]
- Zhang, Y.F.; Cheng, X.R.; Chen, Y.; Shi, B.; Chen, X.H.; Xu, D.X.; Ke, J. Three-dimensional nanohydroxyapatite/chitosan scaffolds as potential tissue engineered periodontal tissue. J. Biomater. Appl. 2007, 21, 333–349. [Google Scholar] [CrossRef]
- Thein-Han, W.W.; Misra, R.D.K. Biomimetic chitosan-nanohydroxyapatite composite scaffolds for bone tissue engineering. Acta Biomater. 2009, 5, 1182–1197. [Google Scholar] [CrossRef]
- Ma, X.; Wang, Y.; Guo, H.; Wang, J. Nano-hydroxyapatite/chitosan sponge-like biocomposite for repairing of rat calvarial critical-sized bone defect. J. Bioact. Compat. Polym. 2011, 26, 335–346. [Google Scholar]
- Reves, B.T.; Jennings, J.A.; Bumgardner, J.D.; Haggard, W.O. Preparation and functional assessment of composite chitosan-nano-hydroxyapatite scaffolds for bone regeneration. J. Funct. Biomater. 2012, 3, 114–130. [Google Scholar] [CrossRef]
- Roy, P.; Sailaja, R.R.N. Chitosan-nanohydroxyapatite composites: Mechanical, thermal and bio-compatibility studies. Int. J. Biol. Macromol. 2015, 73, 170–181. [Google Scholar] [CrossRef]
- Thomas, S.P.; Alghamdi, M.N. Chitosan composites with nanohydroxyapatite prepared by wet chemical reaction along with microwave irradiation: Permeability and swelling aspects. Polym. Compos. 2018, 39, 718–729. [Google Scholar] [CrossRef]
- Chakraborty, H.; Bhowmik, N. Structure and stability analysis of biocompatible hydroxyapatite reinforced chitosan nanocomposite. Polym. Compos. 2018, 39, E573–E583. [Google Scholar] [CrossRef]
- le Grill, S.; Coppel, S.Y.; Soulie, J.; Bertrand, G.; Rey, C.; Brouille, F. Towards chitosan-amorphous calcium phosphate nanocomposite: Co-precipitation induced by spray drying. Next Mater. 2024, 4, 100095. [Google Scholar] [CrossRef]
- Lu, Y.; Zhu, A.; Wang, W.; Shi, H. New bioactive hybrid material of nano-hydroxyapatite based on N-carboxyethylchitosan for bone tissue engineering. Appl. Surf. Sci. 2010, 256, 7228–7233. [Google Scholar] [CrossRef]
- Zhou, G.; Li, Y.; Zhang, L.; Li, H.; Wang, M.; Cheng, L.; Wang, Y.; Wang, H.; Shi, P. The study of tri-phasic interactions in nano-hydroxyapatite/konjac glucomannan/chitosan composite. J. Mater. Sci. 2007, 42, 2591–2597. [Google Scholar]
- Zhou, G.; Li, Y.; Zhang, L.; Zuo, Y.; Jansen, J.A. Preparation and characterization of nano-hydroxyapatite/chitosan/konjac glucomannan composite. J. Biomed. Mater. Res. A 2007, 83A, 931–939. [Google Scholar] [CrossRef]
- Mohamed, K.R.; El-Rashidy, Z.M.; Salama, A.A. Preparation and characterization of nano hydroxyapatite/polymeric composites materials. Part I. Mater. Chem. Phys. 2011, 130, 561–568. [Google Scholar] [CrossRef]
- Singh, Y.P.; Dasgupta, S.; Bhaskar, R. Preparation, characterization and bioactivities of nano anhydrous calcium phosphate added gelatin–chitosan scaffolds for bone tissue engineering. J. Biomat. Sci. Polym. Ed. 2019, 30, 1756–1778. [Google Scholar] [CrossRef]
- Wu, M.Y.; Kao, I.F.; Fu, C.Y.; Yen, S.K. Effects of adding chitosan on drug entrapment efficiency and release duration for paclitaxel-loaded hydroxyapatite–gelatin composite microspheres. Pharmaceutics 2023, 15, 2025. [Google Scholar] [CrossRef]
- Bueno, V.B.; Bentini, R.; Catalani, L.H.; Barbosa, L.R.S.; Petri, D.F.S. Synthesis and characterization of xanthan-hydroxyapatite nanocomposites for cellular uptake. Mater. Sci. Eng. C 2014, 37, 195–230. [Google Scholar] [CrossRef]
- Huang, J.; Lin, Y.W.; Fu, X.W.; Best, S.M.; Brooks, R.A.; Rushton, N.; Bonfield, W. Development of nano-sized hydroxyapatite reinforced composites for tissue engineering scaffolds. J. Mater. Sci. Mater. Med. 2007, 18, 2151–2157. [Google Scholar] [CrossRef]
- Lee, H.J.; Choi, H.W.; Kim, K.J.; Lee, S.C. Modification of hydroxyapatite nanosurfaces for enhanced colloidal stability and improved interfacial adhesion in nanocomposites. Chem. Mater. 2006, 18, 5111–5118. [Google Scholar] [CrossRef]
- Lee, H.J.; Kim, S.E.; Choi, H.W.; Kim, C.W.; Kim, K.J.; Lee, S.C. The effect of surface-modified nano-hydroxyapatite on biocompatibility of poly(ε-caprolactone) / hydroxyapatite nanocomposites. Eur. Polym. J. 2007, 43, 1602–1608. [Google Scholar] [CrossRef]
- Hao, J.Y.; Liu, Y.; Zhou, S.; Li, Z.; Deng, X. Investigation of nanocomposites based on semi-interpenetrating network of [L-poly (ε-caprolactone)]/[net-poly (ε-caprolactone)] and hydroxyapatite nanocrystals. Biomaterials 2003, 24, 1531–1539. [Google Scholar] [CrossRef]
- Meskinfam, M.; Bertoldi, S.; Albanese, N.; Cerri, A.; Tanzi, M.C.; Imani, R.; Baheiraei, N.; Farokhi, M.; Farè, S. Polyurethane foam/nano hydroxyapatite composite as a suitable scaffold for bone tissue regeneration. Mater. Sci. Eng. C 2018, 82, 130–140. [Google Scholar] [CrossRef]
- Sultan, M. Hydroxyapatite/polyurethane composites as promising biomaterials. Chem. Pap. 2018, 72, 2375–2395. [Google Scholar] [CrossRef]
- Zhang, T.; Li, J.; Wang, Y.; Han, W.; Wei, Y.; Hu, Y.; Liang, Z.; Lian, X.; Huang, D. Hydroxyapatite/polyurethane scaffolds for bone tissue engineering. Tissue Eng. Part B-Rev. 2024, 30, 60–73. [Google Scholar] [CrossRef]
- Ghassemi, B.; Estaji, S.; Mousavi, S.R.; Nemati, M.S.; Shojaei, S.; Mostafaiyan, M.; Arjmand, M.; Khonakdar, H.A. In-depth study of mechanical properties of poly(lactic acid)/thermoplastic polyurethane/hydroxyapatite blend nanocomposites. J. Mater. Sci. 2022, 57, 7250–7264. [Google Scholar] [CrossRef]
- Revilla-López, G.; Casanovas, J.; Bertran, O.; Turon, P.; Puiggalí, J.; Alemán, C. Modeling biominerals formed by apatites and DNA. Biointerphases 2013, 8, 10. [Google Scholar] [CrossRef]
- Bertran, O.; del Valle, L.J.; Revilla-López, G.; Chaves, G.; Cardús, L.; Casas, M.T.; Casanovas, J.; Turon, P.; Puiggalí, J.; Alemán, C. Mineralization of DNA into nanoparticles of hydroxyapatite. Dalton Trans. 2014, 43, 317–327. [Google Scholar] [CrossRef]
- Grande, C.J.; Torres, F.G.; Gomez, C.M.; Bañó, M.C. Nanocomposites of bacterial cellulose/hydroxyapatite for biomedical applications. Acta Biomater. 2009, 5, 1605–1615. [Google Scholar] [CrossRef]
- Zadegan, S.; Hossainalipour, M.; Ghassai, H.; Rezaie, H.R.; Naimi-Jamal, M.R. Synthesis of cellulose-nanohydroxyapatite composite in 1-n-butyl-3-methylimidazolium chloride. Ceram. Int. 2010, 36, 2375–2381. [Google Scholar] [CrossRef]
- Fu, L.H.; Qi, C.; Liu, Y.J.; Cao, W.T.; Ma, M.G. Sonochemical synthesis of cellulose/hydroxyapatite nanocomposites and their application in protein adsorption. Sci. Rep. 2018, 8, 8292. [Google Scholar] [CrossRef]
- Salama, A. Cellulose/calcium phosphate hybrids: New materials for biomedical and environmental applications. Int. J. Biol. Macromol. 2019, 127, 606–617. [Google Scholar] [CrossRef]
- Pang, P.; Li, W.; Liu, Y. Effect of ball milling process on the microstructure of titanium-nanohydroxyapatite composite powder. Rare Metals 2007, 26, 118–123. [Google Scholar] [CrossRef]
- Li, W.; Pang, P.; Liu, Y. Microstructure and phase composition of Ti-based biocomposites with different contents of nano-hydroxyapatite. Trans. Nonferrous Met. Soc. China 2007, 17, S1148–S1151. [Google Scholar]
- Niespodziana, K.; Jurczyk, K.; Jakubowicz, J.; Jurczyk, M. Fabrication and properties of titanium-hydroxyapatite nanocomposites. Mater. Chem. Phys. 2010, 123, 160–165. [Google Scholar] [CrossRef]
- Hesaraki, S.; Ebadzadeh, T.; Ahmadzadeh-Asl, S. Nanosilicon carbide/hydroxyapatite nanocomposites: Structural, mechanical and in vitro cellular properties. J. Mater. Sci. Mater. Med. 2010, 21, 2141–2149. [Google Scholar] [CrossRef]
- Zhao, X.; Yang, J.; Xin, H.; Wang, X.; Zhang, L.; He, F.; Liu, Q.; Zhang, W. Improved dispersion of SiC whisker in nano hydroxyapatite and effect of atmospheres on sintering of the SiC whisker reinforced nano hydroxyapatite composites. Mater. Sci. Eng. C 2018, 91, 135–145. [Google Scholar] [CrossRef]
- Brook, I.; Freeman, C.; Grubb, S.; Cummins, N.; Curran, D.; Reidy, C.; Hampshire, S.; Towler, M. Biological evaluation of nano-hydroxyapatite-zirconia (HA-ZrO2) composites and strontium-hydroxyapatite (Sr-HA) for load-bearing applications. J. Biomater. Appl. 2012, 27, 291–298. [Google Scholar] [CrossRef]
- Chaudhry, A.A.; Yan, H.; Viola, G.; Reece, M.J.; Knowles, J.C.; Gong, K.; Rehman, I.; Darr, J.A. Phase stability and rapid consolidation of hydroxyapatite-zirconia nano-coprecipitates made using continuous hydrothermal flow synthesis. J. Biomater. Appl. 2012, 27, 79–90. [Google Scholar] [CrossRef]
- Gain, A.K.; Zhang, L.; Liu, W. Microstructure and material properties of porous hydroxyapatite-zirconia nanocomposites using polymethyl methacrylate powders. Mater. Des. 2015, 67, 136–144. [Google Scholar] [CrossRef]
- Cicuéndez, M.; Portolés, M.T.; Izquierdo-Barba, I.; Vallet-Regí, M. New nanocomposite system with nanocrystalline apatite embedded into mesoporous bioactive glass. Chem. Mater. 2012, 24, 1100–1106. [Google Scholar] [CrossRef]
- Govindan, R.; Girija, E.K. Drug loaded phosphate glass/hydroxyapatite nanocomposite for orthopedic applications. J. Mater. Chem. B 2014, 2, 5468–5477. [Google Scholar] [CrossRef]
- Akhavan, A.; Sheikh, N.; Khoylou, F.; Naimian, F.; Ataeivarjovi, E. Synthesis of antimicrobial silver/hydroxyapatite nanocomposite by gamma irradiation. Radiat. Phys. Chem. 2014, 98, 46–50. [Google Scholar] [CrossRef]
- Bahrami, M.; Fathi, M.H.; Ahmadian, M. The effect of nanobioceramic reinforcement on mechanical and biological properties of Co-base alloy/hydroxyapatite nanocomposite. Mater. Sci. Eng. C 2015, 48, 572–578. [Google Scholar] [CrossRef]
- Chung, H.K.; Wongso, V.; Sambudi, N.S.; Isnaeni. Biowaste-derived carbon dots/hydroxyapatite nanocomposite as drug delivery vehicle for acetaminophen. J. Sol-Gel Sci. Technol. 2020, 93, 214–223. [Google Scholar] [CrossRef]
- Irfan, A.; Jeshurun, A.; Baraneedharan, P.; Reddy, B.M. A photoluminescence study of nitrogen-doped carbon quantum dots/hydroxyapatite (NCQDs/HAp) nanocomposites. Mater. Technol. 2022, 37, 768–779. [Google Scholar] [CrossRef]
- Ofudje, E.A.; Akande, J.A.; Sodiya, E.F.; Ajayi, G.O.; Ademoyegun, A.J.; Al-Sehemi, A.G.; Kavil, Y.N.; Bakheet, A.M. Bioactivity properties of hydroxyapatite/clay nanocomposites. Sci. Rep. 2023, 13, 19896. [Google Scholar] [CrossRef]
- Šupová, M. Calcium orthophosphate-clay composites—Preparation, characterisation, and applications: A review. Minerals 2024, 14, 169. [Google Scholar] [CrossRef]
- Yan, Y.; Li, Y.; Zheng, Y.; Yi, Z.; Wei, J.; Xia, C.; Chen, Y. Synthesis and properties of a copolymer of poly(1,4-phenylene sulfide)-poly(2,4-phenylene sulfide acid) and its nano-apatite reinforced composite. Eur. Polym. J. 2003, 39, 411–416. [Google Scholar]
- Yang, K.; Wang, C.; Wei, J. A study on biocomposite of nano apatite/poly (1,4-phenylene-sulfide)-poly (2,4-phenylene sulfide acid). Compos. B 2007, 38, 306–310. [Google Scholar] [CrossRef]
- Jiang, L.; Li, Y.; Zhang, L.; Liao, J. Preparation and properties of a novel bone repair composite: Nano-hydroxyapatite/chitosan/carboxymethyl cellulose. J. Mater. Sci. Mater. Med. 2008, 19, 981–987. [Google Scholar]
- Liu, L.; Liu, J.; Wang, M.; Min, S.; Cai, Y.; Zhu, L.; Yao, J. Preparation and characterization of nano-hydroxyapatite/silk fibroin porous scaffolds. J. Biomater. Sci. Polym. Edn. 2008, 19, 325–338. [Google Scholar] [CrossRef]
- Ren, Y.J.; Sun, X.D.; Cui, F.Z.; Wei, Y.T.; Cheng, Z.J.; Kong, X.D. Preparation and characterization of antheraea pernyi silk fibroin based nanohydroxyapatite composites. J. Bioact. Compat. Polym. 2007, 22, 465–474. [Google Scholar] [CrossRef]
- Sundaraseelan, J.; Sastry, T.P. Fabrication of a biomimetic compound containing nano hydroxyapatite–demineralised bone matrix. J. Biomed. Nanotechnol. 2007, 3, 401–405. [Google Scholar] [CrossRef]
- Niu, Y.; Cao, L.; Wei, J.; Ma, Y.; Song, S.; Weng, W.; Li, H.; Liu, C.; Su, J. Development of a bioactive composite of nano fluorapatite and poly(butylene succinate) for bone tissue regeneration. J. Mater. Chem. B 2014, 2, 1174–1181. [Google Scholar] [CrossRef]
- Li, H.; Yang, L.; Dong, X.; Gu, Y.; Lv, G.; Yan, Y. Composite scaffolds of nano calcium deficient hydroxyapatite/multi-(amino acid) copolymer for bone tissue regeneration. J. Mater. Sci. Mater. Med. 2014, 25, 1257–1265. [Google Scholar] [CrossRef]
- Pourdanesh, F.; Jebali, A.; Hekmatimoghaddam, S.; Allaveisie, A. In vitro and in vivo evaluation of a new nanocomposite, containing high density polyethylene, tricalcium phosphate, hydroxyapatite and magnesium oxide nanoparticles. Mater. Sci. Eng. C 2014, 40, 382–388. [Google Scholar] [CrossRef]
- Li, Z.; Mi, W.; Wang, H.; Su, Y.; He, C. Nano-hydroxyapatite/polyacrylamide composite hydrogels with high mechanical strengths and cell adhesion properties. Colloid Surface B 2014, 123, 959–964. [Google Scholar] [CrossRef]
- Gheisari, H.; Karamian, E.; Abdellahi, M. A novel hydroxyapatite–hardystonite nanocomposite ceramic. Ceram. Int. 2015, 41, 5967–5975. [Google Scholar] [CrossRef]
- Tempesti, P.; Nicotera, G.S.; Bonini, M.; Fratini, E.; Baglioni, P. Poly(N-isopropylacrylamide)-hydroxyapatite nanocomposites as thermoresponsive filling materials on dentinal surface and tubules. J. Colloid Interf. Sci. 2018, 509, 123–131. [Google Scholar] [CrossRef]
- Demétrio, K.B.; Cioato, M.J.G.; Moreschi, A.; Oliveira, G.A.; Lorenzi, W.B.; de Oliveira, F.H.; Neto, A.V.M.; Sanches, P.R.S.; Xavier, R.G.; dos Santos, L.A.L. Polydimethylsiloxane/nano calcium phosphate composite tracheal stents: Mechanical and physiological properties. J. Biomed. Mater. Res. B Appl. Biomater. 2019, 107B, 545–553. [Google Scholar] [CrossRef]
- Afifi, M.; El-Naggar, M.E.; Muhammad, S.; Alghamdi, N.A.; Wageh, S.; Salem, S.R.; Alhashmialameer, D. Nanocomposites based on hydroxyapatite/lithium oxide and graphene oxide nanosheets for medical applications. J. Mater. Sci. 2022, 57, 11300–11316. [Google Scholar] [CrossRef]
- Zandi, M.; Mirzadeh, H.; Mayer, C.; Urch, H.; Eslaminejad, M.B.; Bagheri, F.; Mivehchi, H. Biocompatibility evaluation of nano-rod hydroxyapatite/gelatin coated with nano-HAp as a novel scaffold using mesenchymal stem cells. J. Biomed. Mater. Res. A 2010, 92A, 1244–1255. [Google Scholar] [CrossRef]
- Sun, T.S.; Guan, K.; Shi, S.S.; Zhu, B.; Zheng, Y.J.; Cui, F.Z.; Zhang, W.; Liao, S.S. Effect of nano-hydroxyapatite/collagen composite and bone morphogenetic protein-2 on lumbar intertransverse fusion in rabbits. Chin. J. Traumatol. 2004, 7, 18–24. [Google Scholar]
- Itoh, S.; Kikuehi, M.; Koyama, Y.; Takakuda, K.; Shinomiya, K.; Tanaka, J. Development of a hydroxyapatite/collagen nanocomposite as a medical device. Cell Transp. 2004, 13, 451–461. [Google Scholar] [CrossRef]
- Kester, M.; Heakal, Y.; Fox, T.; Sharma, A.; Robertson, G.P.; Morgan, T.T.; Altinoğlu, E.I.; Tabaković, A.; Parette, M.R.; Rouse, S.M.; et al. Calcium phosphate nanocomposite particles for in vitro imaging and encapsulated chemotherapeutic drug delivery to cancer cells. Nano Lett. 2008, 8, 4116–4121. [Google Scholar] [CrossRef]
- Wang, K.W.; Zhou, L.Z.; Sun, Y.; Wu, G.J.; Gu, H.C.; Duan, Y.R.; Chen, F.; Zhu, Y.J. Calcium phosphate/PLGA-mPEG hybrid porous nanospheres: A promising vector with ultrahigh gene loading and transfection efficiency. J. Mater. Chem. 2010, 20, 1161–1166. [Google Scholar] [CrossRef]
- Gelinsky, M.; Welzel, P.B.; Simon, P.; Bernhardt, A.; König, U. Porous three-dimensional scaffolds made of mineralized collagen: Preparation and properties of a biomimetic nanocomposite material for tissue engineering of bone. Chem. Eng. J. 2008, 137, 84–96. [Google Scholar] [CrossRef]
- Hu, Q.; Li, B.Q.; Wang, M.; Shen, J.C. Preparation and characterization of biodegradable chitosan/hydroxyapatite nanocomposite rods via in situ hybridization: A potential material as internal fixation of bone fracture. Biomaterials 2004, 25, 779–785. [Google Scholar] [CrossRef]
- Wei, G.; Ma, P.X. Structure and properties of nano-hydroxyapatite/polymer composite scaffolds for bone tissue engineering. Biomaterials 2004, 25, 4749–4757. [Google Scholar] [CrossRef]
- Liou, S.C.; Chen, S.Y.; Liu, D.M. Synthesis and characterization of needlelike apatitic nanocomposite with controlled aspect ratios. Biomaterials 2003, 24, 3981–3988. [Google Scholar] [CrossRef]
- Liou, S.C.; Chen, S.Y.; Liu, D.M. Manipulation of nanoneedle and nanosphere apatite/poly(acrylic acid) nanocomposites. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 73B, 117–122. [Google Scholar] [CrossRef]
- Nakayama, M.; Lim, W.Q.; Kajiyama, S.; Kumamoto, A.; Ikuhara, Y.; Kato, T.; Zhao, Y. Liquid-crystalline hydroxyapatite/polymer nanorod hybrids: Potential bioplatform for photodynamic therapy and cellular scaffolds. ACS Appl. Mater. Interfaces 2019, 11, 17759–17765. [Google Scholar] [CrossRef]
- Huang, J.; Best, S.M.; Bonfield, W.; Brooks, R.A.; Rushton, N.; Jayasinghe, S.N.; Edirisinghe, M.J. In vitro assessment of the biological response to nano-size hydroxyapatite. J. Mater. Sci. Mater. Med. 2004, 15, 441–445. [Google Scholar] [CrossRef]
- Kong, L.; Gao, Y.; Cao, W.; Gong, Y.; Zhao, N.; Zhang, X. Preparation and characterization of nano-hydroxyapatite/chitosan composite scaffolds. J. Biomed. Mater. Res. A 2005, 75A, 275–282. [Google Scholar] [CrossRef]
- Venkatesan, J.; Kim, S.K. Nano-hydroxyapatite composite biomaterials for bone tissue engineering—A review. J. Biomed. Nanotechnol. 2014, 10, 3124–3140. [Google Scholar] [CrossRef]
- Christenson, E.M.; Anseth, K.S.; van den Beucken, J.J.J.P.; Chan, C.K.; Ercan, B.; Jansen, J.A.; Laurencin, C.T.; Li, W.J.; Murugan, R.; Nair, L.S.; et al. Nanobiomaterial applications in orthopedics. J. Orthop. Res. 2007, 25, 11–22. [Google Scholar] [CrossRef]
- Ridi, F.; Meazzini, I.; Castroflorio, B.; Bonini, M.; Berti, D.; Baglioni, P. Functional calcium phosphate composites in nanomedicine. Adv. Colloid Interface Sci. 2017, 244, 281–295. [Google Scholar] [CrossRef]
- Pielichowska, K.; Blazewicz, S. Bioactive polymer/hydroxyapatite (nano)composites for bone tissue regeneration. Adv. Polym. Sci. 2010, 232, 97–207. [Google Scholar]
- Liao, J.; Li, Y.; Duan, X.; Zhu, L. Nano-hydroxyapatite/polymer composite as bone repair materials. Prog. Chem. 2015, 27, 220–228. [Google Scholar]
- Du, M.; Chen, J.; Liu, K.; Xing, H.; Song, C. Recent advances in biomedical engineering of nano-hydroxyapatite including dentistry, cancer treatment and bone repair. Compos. B 2021, 215, 108790. [Google Scholar] [CrossRef]
- Radha, G.; Manjubaashini, N.; Balakumar, S. Nano-hydroxyapatite/natural polymer composite scaffolds for bone tissue engineering: A brief review of recent trend. Vitr. Models 2023, 2, 125–151. [Google Scholar] [CrossRef]
- Liu, C. Collagen–hydroxyapatite composite scaffolds for tissue engineering. In Hydroxyapatite (HAp) for Biomedical Applications; Mucalo, M.R., Ed.; Woodhead Publishing Series in Biomaterials: Number 95; Elsevier: Cambridge, UK, 2015; pp. 211–234. [Google Scholar]
- Bedell, M.L.; Navara, A.M.; Du, Y.; Zhang, S.; Mikos, A.G. Polymeric Systems for Bioprinting. Chem. Rev. 2020, 120, 10744–10792. [Google Scholar] [CrossRef]
- Hellmich, C.; Ulm, F.J. Are mineralized tissues open crystal foams reinforced by crosslinked collagen?—Some energy arguments. J. Biomech. 2002, 35, 1199–1212. [Google Scholar] [CrossRef]
- Veiga, A.; Castro, F.; Rocha, F.; Oliveira, A.L. An update on hydroxyapatite/collagen composites: What is there left to say about these bioinspired materials? J. Biomed. Mater. Res. B Appl. Biomater. 2022, 110B, 1192–1205. [Google Scholar] [CrossRef]
- Roveri, N.; Falini, G.; Sidoti, M.C.; Tampieri, A.; Landi, E.; Sandri, M.; Parma, B. Biologically inspired growth of hydroxyapatite nanocrystals inside self-assembled collagen fibers. Mater. Sci. Eng. C 2003, 23, 441–446. [Google Scholar] [CrossRef]
- Tampieri, A.; Celotti, G.; Landi, E. From biomimetic apatites to biologically inspired composites. Anal. Bioanal. Chem. 2005, 381, 568–576. [Google Scholar] [CrossRef]
- Tampieri, A.; Celotti, G.; Landi, E.; Sandri, M.; Roveri, N.; Falini, G. Biologically inspired synthesis of bone-like composite: Self-assembled collagen fibers/hydroxyapatite nanocrystals. J. Biomed. Mater. Res. A 2003, 67A, 618–625. [Google Scholar] [CrossRef]
- Clarke, K.I.; Graves, S.E.; Wong, A.T.C.; Triffit, J.T.; Francis, M.J.O.; Czernuszka, J.T. Investigation into the formation and mechanical properties of a bioactive material based on collagen and calcium phosphate. J. Mater. Sci. Mater. Med. 1993, 4, 107–110. [Google Scholar] [CrossRef]
- Ten Huisen, K.S.; Martin, R.I.; Klimkiewicz, M.; Brown, P.W. Formation and properties of a synthetic bone composite: Hydroxyapatite-collagen. J. Biomed. Mater. Res. 1995, 29, 803–810. [Google Scholar] [CrossRef]
- Ishikawa, H.; Koshino, T.; Takeuchi, R.; Saito, T. Effects of collagen gel mixed with hydroxyapatite power on interface between newly formed bone and grafted Achilles tendon in rabbit femoral bone tunnel. Biomaterials 2001, 22, 1689–1694. [Google Scholar] [CrossRef]
- ltoh, S.; Kikuchi, M.; Takakuda, K.; Koyama, Y.; Matsumoto, H.N.; Ichinose, S.; Tanaka, J.; Kawauchi, T.; Shinomiya, K. The biocompatibility and osteoconductive activity of a novel hydroxyapatite/collagen composite biomaterial and its function as a carrier of rhBMP-2. J. Biomed. Mater. Res. 2001, 54, 445–453. [Google Scholar]
- Uskokovic, V.; Ignjatovic, N.; Petranovic, N. Synthesis and characterization of hydroxyapatite-collagen biocomposite materials. Mater. Sci. Forum 2002, 413, 269–274. [Google Scholar] [CrossRef]
- Yoon, B.H.; Kim, H.W.; Lee, S.H.; Bae, C.J.; Koh, Y.H.; Kong, Y.M.; Kim, H.E. Stability and cellular responses to fluorapatite-collagen composites. Biomaterials 2005, 26, 2957–2963. [Google Scholar] [CrossRef]
- Wahl, D.A.; Czernuszka, J.T. Collagen-hydroxyapatite composites for hard tissue repair. Eur. Cell Mater. 2006, 11, 43–56. [Google Scholar] [CrossRef]
- Teng, S.H.; Lee, E.J.; Park, C.S.; Choi, W.Y.; Shin, D.S.; Kim, H.E. Bioactive nanocomposite coatings of collagen/hydroxyapatite on titanium substrates. J. Mater. Sci. Mater. Med. 2008, 19, 2453–2461. [Google Scholar] [CrossRef]
- Song, J.H.; Kim, H.E.; Kim, H.W. Collagen-apatite nanocomposite membranes for guided bone regeneration. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 83B, 248–257. [Google Scholar] [CrossRef]
- Pek, Y.S.; Gao, S.; Arshad, M.S.M.; Leck, K.J.; Ying, J.Y. Porous collagen-apatite nanocomposite foams as bone regeneration scaffolds. Biomaterials 2008, 29, 4300–4305. [Google Scholar] [CrossRef]
- Zhao, H.; Huang, C.; Jin, H.; Cai, J. A novel route for collagen/hydroxyapatite preparation by enzymatic decomposition of urea. J. Compos. Mater. 2010, 44, 2127–2133. [Google Scholar] [CrossRef]
- Kozłowska, J.; Sionkowska, A. Effects of different crosslinking methods on the properties of collagen-calcium phosphate composite materials. Int. J. Biol. Macromol. 2015, 74, 397–403. [Google Scholar] [CrossRef]
- Banglmaier, R.F.; Sander, E.A.; VandeVord, P.J. Induction and quantification of collagen fiber alignment in a three-dimensional hydroxyapatite–collagen composite scaffold. Acta Biomater. 2015, 17, 26–35. [Google Scholar] [CrossRef]
- Banks, E.; Nakajima, S.; Shapiro, L.C.; Tilevitz, O.; Alonzo, J.R.; Chianelli, R.R. Fibrous apatite grown on modified collagen. Science 1977, 198, 1164–1166. [Google Scholar] [CrossRef]
- Hayashi, K.; Yabuki, T.; Tabuchi, K.; Fujii, T. Repair of experimental bone defect with a collagen block containing synthesized apatite. Arch. Orthop. Traum. Surg. 1982, 99, 265–269. [Google Scholar] [CrossRef]
- Mittelmeier, H.; Nizzard, M. Knochenregeneration mit industriell gefertigtem Collagen Apatit Implantat (“Collapat”). In Osteogenese und Knochenwachstum; Hackenbroch, M.H., Refior, H.J., Jäger, M.G., Eds.; Thieme: Stuttgart, Germany, 1982; pp. 194–197. [Google Scholar]
- Serre, C.M.; Papillard, M.; Chavassieux, P.; Boivin, G. In vitro induction of a calcifying matrix by biomaterials constituted of collagen and/or hydroxyapatite: An ultrastructural comparison of three types of biomaterials. Biomaterials 1993, 14, 97–106. [Google Scholar] [CrossRef]
- Scabbia, A.; Trombelli, L. A comparative study on the use of a HA/collagen/chondroitin sulphate biomaterial (Biostite®) and a bovine-derived HA xenograft (Bio-Oss®) in the treatment of deep intraosseous defects. J. Clin. Periodontol. 2004, 31, 348–355. [Google Scholar] [CrossRef]
- Yamasaki, Y.; Yoshida, Y.; Okazaki, M.; Shimazu, A.; Kubo, T.; Akagawa, Y.; Uchida, T. Action of FGMgCO3Ap-collagen composite in promoting bone formation. Biomaterials 2003, 24, 4913–4920. [Google Scholar] [CrossRef]
- Wang, X.; Grogan, S.P.; Rieser, F.; Winkelmann, V.; Maquet, V.; Berge, M.L.; Mainil-Varlet, P. Tissue engineering of biphasic cartilage constructs using various biodegradable scaffolds: An in vitro study. Biomaterials 2004, 25, 3681–3688. [Google Scholar] [CrossRef]
- Zahn, D. Multi-scale simulations of apatite–collagen composites: From molecules to materials. Front. Mater. Sci. 2017, 11, 1–12. [Google Scholar] [CrossRef]
- Chang, M.C.; Ikoma, T.; Kikuchi, M.; Tanaka, J. The cross-linkage effect of hydroxyapatite/collagen nanocomposites on a self-organization phenomenon. J. Mater. Sci. Mater. Med. 2002, 13, 993–997. [Google Scholar] [CrossRef]
- Iijima, M.; Moriwaki, Y.; Kuboki, Y. Oriented growth of octacalcium phosphate on and inside the collagenous matrix in vitro. Connect. Tissue Res. 1996, 32, 519–524. [Google Scholar]
- Ortiz, F.; Díaz-Barrios, A.; Lopez-Cabaña, Z.E.; González, G. Effect of the electric field on the biomineralization of collagen. Polymers 2023, 15, 3121. [Google Scholar] [CrossRef]
- Miyamoto, Y.; Ishikawa, K.; Takechi, M.; Toh, T.; Yuasa, T.; Nagayama, M.; Suzuki, K. Basic properties of calcium phosphate cement containing atelocollagen in its liquid or powder phases. Biomaterials 1998, 19, 707–715. [Google Scholar] [CrossRef]
- Iijima, M.; Moriwaki, Y.; Kuboki, Y. In vitro crystal growth of octacalcium phosphate on type I collagen fiber. J. Cryst. Growth 1994, 137, 553–560. [Google Scholar] [CrossRef]
- Iijima, M.; Iijima, K.; Moriwaki, Y.; Kuboki, Y. Oriented growth of octacalcium phosphate crystals on type I collagen fibrils under physiological conditions. J. Cryst. Growth 1994, 140, 91–99. [Google Scholar] [CrossRef]
- Lawson, A.C.; Czernuszka, J.T. Collagen–calcium phosphate composites. Proc. Inst. Mech. Eng. H 1998, 212, 413–425. [Google Scholar] [CrossRef]
- Kamakura, S.; Sasaki, K.; Honda, Y.; Anada, T.; Suzuki, O. Octacalcium phosphate combined with collagen orthotopically enhances bone regeneration. J. Biomed. Mater. Res. B Appl. Biomater. 2006, 79B, 210–217. [Google Scholar] [CrossRef]
- Kawai, T.; Anada, T.; Honda, Y.; Kamakura, S.; Matsui, K.; Matsui, A.; Sasaki, K.; Morimoto, S.; Echigo, S.; Suzuki, O. Synthetic octacalcium phosphate augments bone regeneration correlated with its content in collagen scaffold. Tissue Eng. A 2009, 15, 23–32. [Google Scholar] [CrossRef]
- Masuda, T.; Kawai, T.; Anada, T.; Kamakura, S.; Suzuki, O. Quality of regenerated bone enhanced by implantation of octacalcium phosphate-collagen composite. Tissue Eng. C 2010, 16, 471–478. [Google Scholar] [CrossRef]
- Kikuchi, M.; Ikoma, T.; Itoh, S.; Matsumoto, H.N.; Koyama, Y.; Takakuda, K.; Shinomiya, K.; Tanaka, J. Biomimetic synthesis of bone-like nanocomposites using the self-organization mechanism of hydroxyapatite and collagen. Compos. Sci. Technol. 2004, 64, 819–825. [Google Scholar] [CrossRef]
- Li, X.; Chang, J. Preparation of bone-like apatite-collagen nanocomposites by a biomimetic process with phosphorylated collagen. J. Biomed. Mater. Res. A 2008, 85A, 293–300. [Google Scholar] [CrossRef]
- Jee, S.S.; Thula, T.T.; Gower, L.B. Development of bone-like composites via the polymer-induced liquid-precursor (PILP) process. Part 1: Influence of polymer molecular weight. Acta Biomater. 2010, 6, 3676–3686. [Google Scholar] [CrossRef]
- Aaddouz, M.; Azzaoui, K.; Sabbahi, R.; Youssoufi, M.H.; Yahyaoui, M.I.; Asehraou, A.; El Miz, M.; Hammouti, B.; Shityakov, S.; Siaj, M.; et al. Cheminformatics-based design and synthesis of hydroxyapatite/collagen nanocomposites for biomedical applications. Polymers 2024, 16, 85. [Google Scholar] [CrossRef]
- Bu, H.; Li, G. Comparative investigation of hydroxyapatite/collagen composites prepared by CaCl2 addition at different time points in collagen self-assembly process. J. Mater. Sci. 2018, 53, 6313–6324. [Google Scholar] [CrossRef]
- Bian, T.; Zhao, K.; Meng, Q.; Tang, Y.; Jiao, H.; Luo, J. The construction and performance of multi-level hierarchical hydroxyapatite (HA)/collagen composite implant based on biomimetic bone Haversian motif. Mater. Des. 2019, 162, 60–69. [Google Scholar] [CrossRef]
- Manjushree, M.B.; Archana, R.; Deepak, P.; Nibedita, L. Fabrication and characterization of ceramic-polymer composite 3D scaffolds and demonstration of osteoinductive propensity with gingival mesenchymal stem cells. RSC Adv. 2023, 13, 26967–26982. [Google Scholar]
- Andronescu, E.; Ficai, M.; Voicu, G.; Ficai, D.; Maganu, M.; Ficai, A. Synthesis and characterization of collagen/hydroxyapatite: Magnetite composite material for bone cancer treatment. J. Mater. Sci. Mater. Med. 2010, 21, 2237–2242. [Google Scholar] [CrossRef]
- Ficai, M.; Andronescu, E.; Ficai, D.; Voicu, G.; Ficai, A. Synthesis and characterization of COLL-PVA/HA hybrid materials with stratified morphology. Colloid Surface B 2010, 81, 614–619. [Google Scholar] [CrossRef]
- Chacon, E.L.; Bertolo, M.R.V.; de Guzzi Plepis, A.M.; da Conceição Amaro Martins, V.; dos Santos, G.R.; Pinto, C.A.L.; Pelegrine, A.A.; Teixeira, M.L.; Buchaim, D.V.; Nazari, F.M.; et al. Collagen-chitosan-hydroxyapatite composite scaffolds for bone repair in ovariectomized rats. Sci. Rep. 2023, 13, 28. [Google Scholar] [CrossRef]
- Hoshi, M.; Taira, M.; Sawada, T.; Hachinohe, Y.; Hatakeyama, W.; Takafuji, K.; Tekemoto, S.; Kondo, H. Preparation of collagen/hydroxyapatite composites using the alternate immersion method and evaluation of the cranial bone-forming capability of composites complexed with acidic gelatin and b-FGF. Materials 2022, 15, 8802. [Google Scholar] [CrossRef]
- Animut, T.Y.; Ningsih, H.S.; Shih, H.H.; Wu, M.H.; Shih, S.J. Effect of calcium silicate and β-tricalcium phosphate reinforcement on the mechanical–biological properties of freeze-dried collagen composite scaffolds for bone tissue engineering applications. Ceramics 2023, 6, 548–560. [Google Scholar] [CrossRef]
- Inzana, J.A.; Olvera, D.; Fuller, S.M.; Kelly, J.P.; Graeve, O.A.; Schwarz, E.M.; Kates, S.L.; Awad, H.A. 3D printing of composite calcium phosphate and collagen scaffolds for bone regeneration. Biomaterials 2014, 35, 4026–4034. [Google Scholar] [CrossRef]
- Tamimi, F.; Kumarasami, B.; Doillon, C.; Gbureck, U.; Nihouannen, D.L.; Cabarcos, E.L.; Barralet, J.E. Brushite-collagen composites for bone regeneration. Acta Biomater. 2008, 4, 1315–1321. [Google Scholar] [CrossRef]
- Mai, R.; Reinstorf, A.; Pilling, E.; Hlawitschka, M.; Jung, R.; Gelinsky, M.; Schneider, M.; Loukota, R.; Pompe, W.; Eckelt, U.; et al. Histologic study of incorporation and resorption of a bone cement-collagen composite: An in vivo study in the minipig. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 105, e9–e14. [Google Scholar] [CrossRef]
- Moreau, J.L.; Weir, M.D.; Xu, H.H.K. Self-setting collagen-calcium phosphate bone cement: Mechanical and cellular properties. J. Biomed. Mater. Res. A 2009, 91A, 605–613. [Google Scholar] [CrossRef]
- Liu, X.; Wang, X.M.; Chen, Z.; Cui, F.Z.; Liu, H.Y.; Mao, K.; Wang, Y. Injectable bone cement based on mineralized collagen. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 94B, 72–79. [Google Scholar] [CrossRef]
- Otsuka, M.; Nakagawa, H.; Ito, A.; Higuchi, W.I. Effect of geometrical structure on drug release rate of a three-dimensionally perforated porous apatite/collagen composite cement. J. Pharm. Sci. 2010, 99, 286–292. [Google Scholar] [CrossRef]
- Cui, F.Z.; Li, Y.; Ge, J. Self-assembly of mineralized collagen composites. Mater. Sci. Eng. R 2007, 57, 1–27. [Google Scholar] [CrossRef]
- Hirota, K.; Nishihara, K.; Tanaka, H. Pressure sintering of apatite-collagen composite. Biomed. Mater. Eng. 1993, 3, 147–151. [Google Scholar] [CrossRef]
- Zahn, D.; Hochrein, O.; Kawska, A.; Brickmann, J.; Kniep, R. Towards an atomistic understanding of apatite-collagen biomaterials: Linking molecular simulation studies of complex-, crystal- and composite-formation to experimental findings. J. Mater. Sci. 2007, 42, 8966–8973. [Google Scholar] [CrossRef]
- Silva, C.C.; Pinheiro, A.G.; Figueiro, S.D.; Goes, J.C.; Sasaki, J.M.; Miranda, M.A.R.; Sombra, A.S.B. Piezoelectric properties of collagen-nanocrystalline hydroxyapatite composites. J. Mater. Sci. 2002, 37, 2061–2070. [Google Scholar] [CrossRef]
- Yunoki, S.; Ikoma, T.; Tsuchiya, A.; Monkawa, A.; Ohta, K.; Sotome, S.; Shinomiya, K.; Tanaka, J. Fabrication and mechanical and tissue ingrowth properties of unidirectionally porous hydroxyapatite/collagen composite. J. Biomed. Mater. Res. B Appl. Biomater. 2007, 80B, 166–173. [Google Scholar] [CrossRef]
- Keeney, M.; Collin, E.; Pandit, A. Multi-channelled collagen-calcium phosphate scaffolds: Their physical properties and human cell response. Tissue Eng. C 2009, 15, 265–273. [Google Scholar] [CrossRef]
- Chapman, M.W.; Bucholz, R.; Cornell, C. Treatment of acute fractures with a collagen-calcium phosphate graft material: A randomized clinical trial. J. Bone Joint Surg. 1997, 79A, 495–502. [Google Scholar] [CrossRef]
- Rodrigues, C.V.M.; Serricella, P.; Linhares, A.B.R.; Guerdes, R.M.; Borojevic, R.; Rossi, M.A.; Duarte, M.E.L.; Farina, M. Characterization of a bovine collagen-hydroxyapatite composite scaffold for bone tissue engineering. Biomaterials 2003, 24, 4987–4997. [Google Scholar] [CrossRef]
- Miura, K.I.; Anada, T.; Honda, Y.; Shiwaku, Y.; Kawai, T.; Echigo, S.; Takahashi, T.; Suzuki, O. Characterization and bioactivity of nano-submicro octacalcium phosphate/gelatin composite. Appl. Surf. Sci. 2013, 282, 138–145. [Google Scholar] [CrossRef]
- Kawai, T.; Echigo, S.; Matsui, K.; Tanuma, Y.; Takahashi, T.; Suzuki, O.; Kamakura, S. First clinical application of octacalcium phosphate collagen composite in human bone defect. Tissue Eng. A 2014, 20, 1336–1341. [Google Scholar] [CrossRef]
- Lickorish, D.; Ramshaw, J.A.M.; Werkmeister, J.A.; Glattauer, V.; Howlett, C.R. Development of a collagen-hydroxyapatite composite biomaterial via biomimetic process. J. Biomed. Mater. Res. A 2004, 68A, 19–27. [Google Scholar] [CrossRef]
- Sionkowska, A.; Kozłowska, J. Characterization of collagen/hydroxyapatite composite sponges as a potential bone substitute. Int. J. Biol. Macromol. 2010, 47, 483–487. [Google Scholar] [CrossRef]
- Hsu, F.Y.; Chueh, S.C.; Wang, J.Y. Microspheres of hydroxyapatite/reconstituted collagen as supports for osteoblast cell growth. Biomaterials 1999, 20, 1931–1936. [Google Scholar] [CrossRef]
- Wu, T.J.; Huang, H.H.; Lan, C.W.; Lin, C.H.; Hsu, F.Y.; Wang, Y.J. Studies on the microspheres comprised of reconstituted collagen and hydroxyapatite. Biomaterials 2004, 25, 651–658. [Google Scholar] [CrossRef]
- Wei, Q.; Lu, J.; Wang, Q.; Fan, H.; Zhang, X. Novel synthesis strategy for composite hydrogel of collagen/hydroxyapatite-microsphere originating from conversion of CaCO3 templates. Nanotechnology 2015, 26, 115605. [Google Scholar] [CrossRef]
- Liao, S.S.; Watari, F.; Uo, M.; Ohkawa, S.; Tamura, K.; Wang, W.; Cui, F.Z. The preparation and characteristics of a carbonated hydroxyapatite/collagen composite at room temperature. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 74B, 817–821. [Google Scholar] [CrossRef]
- Yokoyama, A.; Gelinsky, M.; Kawasaki, T.; Kohgo, T.; König, U.; Pompe, W.; Watari, F. Biomimetic porous scaffolds with high elasticity made from mineralized collagen—An animal study. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 75B, 464–472. [Google Scholar] [CrossRef]
- Zou, C.; Weng, W.; Deng, X.J.; Cheng, K.; Liu, X.; Du, P.; Shen, G.; Han, G. Preparation and characterization of porous β-tricalcium phosphate/collagen composites with an integrated structure. Biomaterials 2005, 26, 5276–5284. [Google Scholar] [CrossRef]
- Available online: https://en.wikipedia.org/wiki/Bioconjugation (accessed on 1 May 2024).
- Gotterbarm, T.; Richter, W.; Jung, M.; Berardi-Vilei, S.; Mainil-Varlet, P.; Yamashita, T.; Breusch, S.J. An in vivo study of a growth-factor enhanced, cell free, two-layered collagen-tricalcium phosphate in deep osteochondral defects. Biomaterials 2006, 27, 3387–3395. [Google Scholar] [CrossRef]
- Sobczak-Kupiec, A.; Drabczyk, A.; Florkiewicz, W.; Głąb, M.; Kudłacik-Kramarczyk, S.; Słota, D.; Tomala, A.; Tyliszczak, B. Review of the applications of biomedical compositions containing hydroxyapatite and collagen modified by bioactive components. Materials 2021, 14, 2096. [Google Scholar] [CrossRef]
- Xie, H.; Ruan, S.; Zhao, M.; Long, J.; Ma, X.; Guo, J.; Lin, X. Preparation and characterization of 3D hydroxyapatite/collagen scaffolds and its application in bone regeneration with bone morphogenetic protein-2. RSC Adv. 2023, 13, 23010–23020. [Google Scholar] [CrossRef]
- Jayaraman, M.; Subramanian, M.V. Preparation and characterization of two new composites: Collagen-brushite and collagen-octacalcium phosphate. Med. Sci. Monitor 2002, 8, BR481–BR487. [Google Scholar]
- Matsui, K.; Matsui, A.; Handa, T.; Kawai, T.; Suzuki, O.; Kamakura, S.; Echigo, S. Bone regeneration by octacalcium phosphate collagen composites in a dog alveolar cleft model. Int. J. Oral Maxillofac. Surg. 2010, 39, 1218–1225. [Google Scholar] [CrossRef]
- Iibuchi, S.; Matsui, K.; Kawai, T.; Sasaki, K.; Suzuki, O.; Kamakura, S.; Echigo, S. Octacalcium phosphate (OCP) collagen composites enhance bone healing in a dog tooth extraction socket model. Int. J. Oral Maxillofac. Surg. 2010, 39, 161–168. [Google Scholar] [CrossRef]
- Kawai, T.; Matsui, K.; Ezoe, Y.; Kajii, F.; Suzuki, O.; Takahashi, T.; Kamakura, S. Efficacy of octacalcium phosphate collagen composite for titanium dental implants in dogs. Materials 2018, 11, 229. [Google Scholar] [CrossRef]
- Ni, T.; Zhu, Y.; Hao, L.; Chen, Y.; Cheng, T. Preparation of photothermal-sensitive PDGF@ZIF-8-PDA@COL/PLGA-TCP composite scaffolds for bone defect repair. Mater. Des. 2022, 217, 110643. [Google Scholar] [CrossRef]
- Kołodziejska, B.; Kaflak, A.; Kolmas, J. Biologically inspired collagen/apatite composite biomaterials for potential use in bone tissue regeneration—A review. Materials 2020, 13, 1748. [Google Scholar] [CrossRef]
- Ikeda, H.; Yamaza, T.; Yoshinari, M.; Ohsaki, Y.; Ayukawa, Y.; Kido, M.A.; Inoue, T.; Shimono, M.; Koyano, K.; Tanaka, T. Ultrastructural and immunoelectron microscopic studies of the peri-implant epithelium-implant (Ti-6Al-4V) interface of rat maxilla. J. Periodontol. 2000, 71, 961–973. [Google Scholar] [CrossRef]
- Uchida, M.; Oyane, A.; Kim, H.M.; Kokubo, T.; Ito, A. Biomimetic coating of laminin-apatite composite on titanium metal and its excellent cell-adhesive properties. Adv. Mater. 2004, 16, 1071–1074. [Google Scholar] [CrossRef]
- Oyane, A.; Uchida, M.; Ito, A. Laminin-apatite composite coating to enhance cell adhesion to ethylene-vinyl alcohol copolymer. J. Biomed. Mater. Res. A 2005, 72A, 168–174. [Google Scholar] [CrossRef]
- Oyane, A.; Uchida, M.; Onuma, K.; Ito, A. Spontaneous growth of a laminin-apatite nano-composite in a metastable calcium phosphate solution. Biomaterials 2006, 27, 167–175. [Google Scholar] [CrossRef]
- Oyane, A.; Tsurushima, H.; Ito, A. Highly efficient gene transfer system using a laminin-DNA-apatite composite layer. J. Gene Med. 2010, 12, 194–206. [Google Scholar] [CrossRef]
- Oyane, A.; Wang, X.; Sogo, Y.; Ito, A.; Tsurushima, H. Calcium phosphate composite layers for surface-mediated gene transfer. Acta Biomater. 2012, 8, 2034–2046. [Google Scholar] [CrossRef]
- Yaylaoglu, M.B.; Korkusuz, P.; Ors, U.; Korkusuz, F.; Hasirci, V. Development of a calcium phosphate-gelatin composite as a bone substitute and its use in drug release. Biomaterials 1999, 20, 711–719. [Google Scholar] [CrossRef]
- Kim, H.W.; Knowles, J.C.; Kim, H.E. Porous scaffolds of gelatin-hydroxyapatite nanocomposites obtained by biomimetic approach: Characterization and antibiotic drug release. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 74B, 686–698. [Google Scholar] [CrossRef]
- Chang, M.C.; Douglas, W.H.; Tanaka, J. Organic-inorganic interaction and the growth mechanism of hydroxyapatite crystals in gelatin matrices between 37 and 80 °C. J. Mater. Sci. Mater. Med. 2006, 17, 387–396. [Google Scholar] [CrossRef]
- Chang, M.C.; Douglas, W.H. Cross-linkage of hydroxyapatite/gelatin nanocomposite using imide-based zero-length cross-linker. J. Mater. Sci. Mater. Med. 2007, 18, 2045–2051. [Google Scholar] [CrossRef]
- Han, Y.; Dal-Fabbro, R.; Mahmoud, A.H.; Rahimnejad, M.; Xu, J.; Castilho, M.; Dissanayaka, W.L.; Bottino, M.C. GelMA/TCP nanocomposite scaffold for vital pulp therapy. Acta Biomater. 2024, 173, 495–508. [Google Scholar] [CrossRef]
- Wise, E.R.; Maltsev, S.; Davies, M.E.; Duer, M.J.; Jaeger, C.; Loveridge, N.; Murray, R.C.; Reid, D.G. The organic-mineral interface in bone is predominantly polysaccharide. Chem. Mater. 2007, 19, 5055–5057. [Google Scholar] [CrossRef]
- Lin, H.R.; Yeh, Y.J. Porous alginate/hydroxyapatite composite scaffolds for bone tissue engineering: Preparation, characterization and in vitro studies. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 71B, 52–65. [Google Scholar] [CrossRef]
- Chae, T.; Yang, H.; Leung, V.; Ko, F.; Troczynski, T. Novel biomimetic hydroxyapatite/alginate nanocomposite fibrous scaffolds for bone tissue regeneration. J. Mater. Sci. Mater. Med. 2013, 24, 1885–1894. [Google Scholar] [CrossRef]
- Li, S.; Kan, B.; Zhao, K.; Ren, T.; Lin, B.; Wei, J.; Chen, T. Preparation of tricalcium phosphate-calcium alginate composite flat sheet membranes and their application for protein release. Polym. Compos. 2015, 36, 1899–1906. [Google Scholar] [CrossRef]
- Wulandari, W.; Islami, D.M.; Wellia, D.V.; Emriadi, E.; Sisca, V.; Jamarun, N. The effect of alginate concentration on crystallinity, morphology and thermal stability properties of hydroxyapatite/alginate composite. Polymers 2023, 15, 614. [Google Scholar] [CrossRef]
- Yamaguchi, I.; Tokuchi, K.; Fukuzaki, H.; Koyama, Y.; Takakuda, K.; Monma, H.; Tanaka, J. Preparation and microstructure analysis of chitosan/hydroxyapatite nanocomposites. J. Biomed. Mater. Res. 2001, 55, 20–27. [Google Scholar] [CrossRef]
- Tang, X.J.; Gui, L.; Lü, X.Y. Hard tissue compatibility of natural hydroxyapatite/chitosan composite. Biomed. Mater. 2008, 3, 044115. [Google Scholar] [CrossRef]
- Ge, H.; Zhao, B.; Lai, Y.; Hu, X.; Zhang, D.; Hu, K. From crabshell to chitosan-hydroxyapatite composite material via a biomorphic mineralization synthesis method. J. Mater. Sci. Mater. Med. 2010, 21, 1781–1787. [Google Scholar] [CrossRef]
- Onoki, T.; Nakahira, A.; Tago, T.; Hasegawa, Y.; Kuno, T. Novel low temperature processing techniques for apatite ceramics and chitosan polymer composite bulk materials and its mechanical properties. Appl. Surf. Sci. 2012, 262, 263–266. [Google Scholar] [CrossRef]
- Fernández, T.; Olave, G.; Valencia, C.H.; Arce, S.; Quinn, J.M.W.; Thouas, G.A.; Chen, Q.Z. Effects of calcium phosphate/chitosan composite on bone healing in rats: Calcium phosphate induces osteon formation. Tissue Eng. A 2014, 20, 1948–1960. [Google Scholar] [CrossRef]
- Boudemagh, D.; Venturini, P.; Fleutot, S.; Cleymand, F. Elaboration of hydroxyapatite nanoparticles and chitosan/hydroxyapatite composites: A present status. Polym. Bull. 2019, 76, 2621–2653. [Google Scholar] [CrossRef]
- Galotta, A.; Demir, Ö.; Marsan, O.; Sglavo, V.M.; Loca, D.; Combes, C.; Locs, J. Apatite/chitosan composites formed by cold sintering for drug delivery and bone tissue engineering applications. Nanomaterials 2024, 14, 441. [Google Scholar] [CrossRef]
- Zamora, I.; Morales, G.A.; Castro, J.I.; Rojas, L.M.R.; Valencia-Llano, C.H.; Hernandez, J.H.M.; Zapata, M.E.V.; Grande-Tovar, C.D. Chitosan (CS)/hydroxyapatite (HA)/tricalcium phosphate (β-TCP)-based composites as a potential material for pulp tissue regeneration. Polymers 2023, 15, 3213. [Google Scholar] [CrossRef]
- Ait Said, H.; Noukrati, H.; Ben Youcef, H.; Mahdi, I.; Oudadesse, H.; Barroug, A. In situ precipitated hydroxyapatite-chitosan composite loaded with ciprofloxacin: Formulation, mechanical, in vitro antibiotic uptake, release and antibacterial properties. Mater. Chem. Phys. 2023, 294, 127008. [Google Scholar] [CrossRef]
- Scalera, F.; Pereira, S.I.A.; Bucciarelli, A.; Tobaldi, D.M.; Quarta, A.; Gervaso, F.; Castro, P.M.L.; Polini, A.; Piccirillo, C. Chitosan-hydroxyapatite composites made from sustainable sources: A morphology and antibacterial study. Mater. Today Sustain. 2023, 21, 100334. [Google Scholar] [CrossRef]
- Zhou, K.; Azaman, F.A.; Cao, Z.; Fournet, M.B.; Devine, D.M. Bone tissue engineering scaffold optimisation through modification of chitosan/ceramic composition. Macromol 2023, 3, 326–342. [Google Scholar] [CrossRef]
- Predoi, D.; Iconaru, S.L.; Ciobanu, S.C.; Buton, N.; Predoi, M.V. Complex evaluation of nanocomposite-based hydroxyapatite for biomedical applications. Biomimetics 2023, 8, 528. [Google Scholar] [CrossRef]
- Wan, A.C.A.; Khor, E.; Hastings, G.W. Preparation of a chitin-apatite composite by in situ precipitation onto porous chitin scaffolds. J. Biomed. Mater. Res. 1998, 41, 541–548. [Google Scholar] [CrossRef]
- Wan, A.C.A.; Khor, E.; Hastings, G.W. Hydroxyapatite modified chitin as potential hard tissue substitute material. J. Biomed. Mater. Res. 1997, 38, 235–241. [Google Scholar] [CrossRef]
- Geçer, A.; Yldz, N.; Erol, M.; Çalml, A. Synthesis of chitin calcium phosphate composite in different growth media. Polym. Compos. 2008, 29, 84–91. [Google Scholar] [CrossRef]
- Silva, S.S.; Duarte, A.R.C.; Oliveira, J.M.; Mano, J.F.; Reis, R.L. Alternative methodology for chitin–hydroxyapatite composites using ionic liquids and supercritical fluid technology. J. Bioact. Compat. Polym. 2013, 28, 481–491. [Google Scholar] [CrossRef]
- Machałowski, T.; Kozłowski, M.; Kołodziejczak-Radzimska, A.; Jakubowicz, J.; Jesionowski, T. Chitin nanofibres as reinforcement for hydroxyapatite-based composite preparation. Prog. Chem. Appl. Chitin Its Deriv. 2022, 27, 162–174. [Google Scholar] [CrossRef]
- Wang, J.; Sun, Q.Z.; Gao, J.; Liu, D.M.; Meng, X.C.; Li, M.Q. Preparation and properties on silk fibers reinforced hydroxyapatite/chitosan composites. Adv. Mater. Res. 2010, 105–106, 557–560. [Google Scholar] [CrossRef]
- Zhang, Y.; Reddy, V.J.; Wong, S.Y.; Li, X.; Su, B.; Ramakrishna, S.; Lim, C.T. Enhanced biomineralization in osteoblasts on a novel electrospun biocomposite nanofibrous substrate of hydroxyapatite/collagen/chitosan. Tissue Eng. A 2010, 16, 1949–1960. [Google Scholar] [CrossRef]
- Dehghani, N.; Haghiralsadat, F.; Yazdian, F.; Sadeghian-Nodoushan, F.; Ghasemi, N.; Mazaheri, F.; Pourmadadi, M.; Naghib, S.M. Chitosan/silk fibroin/nitrogen-doped carbon quantum dot/α-tricalcium phosphate nanocomposite electrospinned as a scaffold for wound healing application: In vitro and in vivo studies. Int. J. Biol. Macromol. 2023, 238, 124078. [Google Scholar] [CrossRef]
- Won, J.E.; El-Fiqi, A.; Jegal, S.H.; Han, C.M.; Lee, E.J.; Knowles, J.C.; Kim, H.W. Gelatin-apatite bone mimetic co-precipitates incorporated within biopolymer matrix to improve mechanical and biological properties useful for hard tissue repair. J. Biomater. Appl. 2014, 28, 1213–1225. [Google Scholar] [CrossRef]
- Sarkar, C.; Kumari, P.; Anuvrat, K.; Sahu, S.K.; Chakraborty, J.; Garai, S. Synthesis and characterization of mechanically strong carboxymethyl cellulose–gelatin–hydroxyapatite nanocomposite for load-bearing orthopedic application. J. Mater. Sci. 2018, 53, 230–246. [Google Scholar] [CrossRef]
- Xu, Z.; Li, K.; Zhou, K.; Li, S.; Chen, H.; Zeng, J.; Hu, R. 3D printing silk fibroin/hydroxyapatite/sodium alginate composite scaffolds for bone tissue engineering. Fiber. Polym. 2023, 24, 275–283. [Google Scholar] [CrossRef]
- Sukhodub, L.; Fediv, V.; Kumeda, M.; Sukhodub, L.; Kulchynskyi, V.; Tkachuk, I.; Cherepanov, V.; Prylutskyy, Y. Electrical properties of biodegradable chitosan-calcium phosphate nerve conduits doped with inorganic nanoparticles. Colloids Surf. A 2023, 678, 132425. [Google Scholar] [CrossRef]
- Kousalya, G.N.; Gandhi, R.M.; Sundaram, S.C.; Meenakshi, S. Synthesis of nano-hydroxyapatite chitin/chitosan hybrid biocomposites for the removal of Fe(III). Carbohydr. Polym. 2010, 82, 594–599. [Google Scholar] [CrossRef]
- Sundaram, C.S.; Viswanathan, N.; Meenakshi, S. Uptake of fluoride by nano-hydroxyapatite/chitosan, a bioinorganic composite. Bioresour. Technol. 2008, 99, 8226–8230. [Google Scholar] [CrossRef]
- Sundaram, C.S.; Viswanathan, N.; Meenakshi, S. Fluoride sorption by nano-hydroxyapatite/chitin composite. J. Hazard. Mater. 2009, 172, 147–151. [Google Scholar] [CrossRef]
- Salama, A. Recent progress in preparation and applications of chitosan/calcium phosphate composite materials. Int. J. Biol. Macromol. 2021, 178, 240–252. [Google Scholar] [CrossRef]
- Ait Said, H.; Mabroum, H.; Lahcini, M.; Oudadesse, H.; Barroug, A.; Ben Youcef, H.; Noukrati, H. Manufacturing methods, properties and potential applications in bone tissue regeneration of hydroxyapatite-chitosan biocomposites: A review. Int. J. Biol. Macromol. 2023, 243, 125150. [Google Scholar] [CrossRef]
- Wen, H.B.; de Wijn, J.R.; van Blitterswijk, C.A.; de Groot, K. Incorporation of bovine serum albumin in calcium phosphate coating on titanium. J. Biomed. Mater. Res. 1999, 46, 245–252. [Google Scholar] [CrossRef]
- Liu, T.Y.; Chen, S.Y.; Liu, D.M.; Liou, S.C. On the study of BSA-loaded calcium-deficient hydroxyapatite nano-carriers for controlled drug delivery. J. Control. Release 2005, 107, 112–121. [Google Scholar] [CrossRef]
- Liu, Y.; Hunziker, E.; Randall, N.; de Groot, K.; Layrolle, P. Proteins incorporated into biomimetically prepared calcium phosphate coatings modulate their mechanical strength and dissolution rate. Biomaterials 2003, 24, 65–70. [Google Scholar] [CrossRef]
- Dorozhkin, S.V.; Dorozhkina, E.I. The influence of bovine serum albumin on the crystallization of calcium phosphates from a revised simulated body fluid. Colloid Surface A 2003, 215, 191–199. [Google Scholar] [CrossRef]
- Fu, H.H.; Hu, Y.H.; McNelis, T.; Hollinger, J.O. A calcium phosphate-based gene delivery system. J. Biomed. Mater. Res. A 2005, 74A, 40–48. [Google Scholar] [CrossRef]
- Bisht, S.; Bhakta, G.; Mitra, S.; Maitra, A. pDNA loaded calcium phosphate nanoparticles: Highly efficient non-viral vector for gene delivery. Int. J. Pharm. 2005, 288, 157–168. [Google Scholar] [CrossRef]
- Kakizawa, Y.; Miyata, K.; Furukawa, S.; Kataoka, K. Size-controlled formation of a calcium phosphate-based organic-inorganic hybrid vector for gene delivery using poly(ethylene glycol)-block-poly(aspartic acid). Adv. Mater. 2004, 16, 699–702. [Google Scholar] [CrossRef]
- Singh, R.; Saxena, A.; Mozumdar, S. Calcium phosphate—DNA nanocomposites: Morphological studies and their bile duct infusion for liver-directed gene therapy. Int. J. Appl. Ceram. Technol. 2008, 5, 1–10. [Google Scholar] [CrossRef]
- Oyane, A.; Araki, H.; Sogo, Y.; Ito, A.; Tsurushima, H. Coprecipitation of DNA and calcium phosphate using an infusion fluid mixture. Key Eng. Mater. 2013, 529–530, 465–470. [Google Scholar] [CrossRef]
- Sporysh, I.; Shynkaruk, E.; Lysko, O.; Shynkaruk, A.; Dubok, V.; Buzaneva, E.; Ritter, U.; Scharff, P. Biomimetic hydroxyapatite nanocrystals in composites with C60 and Au-DNA nanoparticles: IR-spectral study. Mater. Sci. Eng. B 2010, 169, 128–133. [Google Scholar] [CrossRef]
- Taguchi, T.; Kishida, A.; Akashi, M. Hydroxyapatite formation on/in poly(vinyl alcohol) hydrogel matrices using a novel alternate soaking process. Chem. Lett. 1998, 8, 711–712. [Google Scholar] [CrossRef]
- Tachaboonyakiat, W.; Serizawa, T.; Akashi, M. Hydroxyapatite formation on/in biodegradable chitosan hydrogels by an alternate soaking process. Polym. J. 2001, 33, 177–181. [Google Scholar] [CrossRef]
- Schnepp, Z.A.C.; Gonzalez-McQuire, R.; Mann, S. Hybrid biocomposites based on calcium phosphate mineralization of self-assembled supramolecular hydrogels. Adv. Mater. 2006, 18, 1869–1872. [Google Scholar] [CrossRef]
- Patel, M.; Patel, K.J.; Caccamese, J.F.; Coletti, D.P.; Sauk, J.J.; Fisher, J.P. Characterization of cyclic acetal hydroxyapatite nanocomposites for craniofacial tissue engineering. J. Biomed. Mater. Res. A 2010, 94A, 408–418. [Google Scholar] [CrossRef]
- Yu, H.; Song, J.; Zhang, X.; Jiang, K.; Fan, H.; Li, Y.; Zhao, Y.; Liu, S.; Hao, D.; Li, G. Hydroxyapatite-tethered peptide hydrogel promotes osteogenesis. Gels 2022, 8, 804. [Google Scholar] [CrossRef]
- Bigi, A.; Boanini, E.; Gazzano, M.; Kojdecki, M.A.; Rubini, K. Microstructural investigation of hydroxyapatite-polyelectrolyte composites. J. Mater. Chem. 2004, 14, 274–279. [Google Scholar] [CrossRef]
- Bigi, A.; Boanini, E.; Gazzano, M.; Rubini, K.; Torricelli, P. Nanocrystalline hydroxyapatite-polyaspartate composites. Biomed. Mater. Eng. 2004, 14, 573–579. [Google Scholar]
- Boanini, E.; Fini, M.; Gazzano, M.; Bigi, A. Hydroxyapatite nanocrystals modified with acidic amino acids. Eur. J. Inorg. Chem. 2006, 4821–4826. [Google Scholar] [CrossRef]
- Boanini, E.; Torricelli, P.; Gazzano, M.; Giardino, R.; Bigi, A. Nanocomposites of hydroxyapatite with aspartic acid and glutamic acid and their interaction with osteoblast-like cells. Biomaterials 2006, 27, 4428–4433. [Google Scholar] [CrossRef]
- Ikawa, N.; Kimura, T.; Oumi, Y.; Sano, T. Amino acid containing amorphous calcium phosphates and the rapid transformation into apatite. J. Mater. Chem. 2009, 19, 4906–4913. [Google Scholar] [CrossRef]
- Sánchez-Salcedo, S.; Nieto, A.; Vallet-Regi, M. Hydroxyapatite/β-tricalcium phosphate/agarose macroporous scaffolds for bone tissue engineering. Chem. Eng. J. 2005, 137, 62–71. [Google Scholar] [CrossRef]
- Román, J.; Cabañas, M.V.; Peña, J.; Doadrio, J.C.; Vallet-Regi, M. An optimized β-tricalcium phosphate and agarose scaffold fabrication technique. J. Biomed. Mater. Res. A 2008, 84A, 99–107. [Google Scholar] [CrossRef]
- Alcaide, M.; Serrano, M.C.; Pagani, R.; Sánchez-Salcedo, S.; Nieto, A.; Vallet-Regí, M.; Portolés, M.T. L929 fibroblast and SAOS-2 osteoblast response to hydroxyapatite-βTCP/ agarose biomaterial. J. Biomed. Mater. Res. A 2009, 89A, 539–549. [Google Scholar] [CrossRef]
- Abiraman, S.; Varma, H.; Umashankar, P.; John, A. Fibrin sealant as an osteoinductive protein in a mouse model. Biomaterials 2002, 23, 3023–3031. [Google Scholar] [CrossRef]
- Wittkampf, A. Fibrin sealant as sealant for hydroxyapatite granules. J. Craniomaxillofac. Surg. 1989, 17, 179–181. [Google Scholar] [CrossRef]
- Le Nihouannen, D.; Guehennec, L.L.; Rouillon, T.; Pilet, P.; Bilban, M.; Layrolle, P.; Daculsi, G. Micro-architecture of calcium phosphate granules and fibrin glue composites for bone tissue engineering. Biomaterials 2006, 27, 2716–2722. [Google Scholar] [CrossRef]
- Le Nihouannen, D.; Goyenvalle, E.; Aguado, E.; Pilet, P.; Bilban, M.; Daculsi, G.; Layrolle, P. Hybrid composites of calcium phosphate granules, fibrin glue and bone marrow for skeletal repair. J. Biomed. Mater. Res. A 2007, 81A, 399–408. [Google Scholar] [CrossRef]
- Boanini, E.; Torricelli, P.; Gazzano, M.; Giardino, R.; Bigi, A. Alendronate-hydroxyapatite nanocomposites and their interaction with osteoclasts and osteoblast-like cells. Biomaterials 2008, 29, 790–796. [Google Scholar] [CrossRef]
- Wang, L.; Nemoto, R.; Senna, M. Microstructure and chemical states of hydroxyapatite/silk fibroin nanocomposites synthesized via a wet-mechanochemical route. J. Nanopart. Res. 2002, 4, 535–540. [Google Scholar] [CrossRef]
- Wang, L.; Li, C.Z.; Senna, M. High-affinity integration of hydroxyapatite nanoparticles with chemically modified silk fibroin. J. Nanopart. Res. 2007, 9, 919–929. [Google Scholar] [CrossRef]
- Fan, C.; Li, J.; Xu, G.; He, H.; Ye, X.; Chen, Y.; Sheng, X.; Fu, J.; He, D. Facile fabrication of nano-hydroxyapatite/silk fibroin composite via a simplified coprecipitation route. J. Mater. Sci. 2010, 45, 5814–5819. [Google Scholar] [CrossRef]
- Liu, H.; Xu, G.W.; Wang, Y.F.; Zhao, H.S.; Xiong, S.; Wu, Y.; Heng, B.C.; An, C.R.; Zhu, G.H.; Xie, D.H. Composite scaffolds of nano-hydroxyapatite and silk fibroin enhance mesenchymal stem cell-based bone regeneration via the interleukin 1 alpha autocrine/paracrine signaling loop. Biomaterials 2015, 49, 103–112. [Google Scholar] [CrossRef]
- Farokhi, M.; Mottaghitalab, F.; Samani, S.; Shokrgozar, M.A.; Kundu, S.C.; Reis, R.L.; Fatahi, Y.; Kaplan, D.L. Silk fibroin/hydroxyapatite composites for bone tissue engineering. Biotechnol. Adv. 2018, 36, 68–91. [Google Scholar] [CrossRef]
- Milazzo, M.; Fitzpatrick, V.; Owens, C.E.; Carraretto, I.M.; McKinley, G.H.; Kaplan, D.L.; Buehler, M.J. 3D printability of silk/hydroxyapatite composites for microprosthetic applications. ACS Biomater. Sci. Eng. 2023, 9, 1285–1295. [Google Scholar]
- Salama, A.; Neumann, M.; Günter, C.; Taubert, A. Ionic liquid-assisted formation of cellulose/calcium phosphate hybrid materials. Beilstein J. Nanotechnol. 2014, 5, 1553–1568. [Google Scholar] [CrossRef]
- Okuda, K.; Kido, E.; Hirota, K.; Mizutani, T. Water-resistant tough composites of cellulose nanofibers and hydroxyapatite. ACS Appl. Polym. Mater. 2023, 5, 8082–8088. [Google Scholar] [CrossRef]
- Wang, L.; Li, C.Z. Preparation and physicochemical properties of a novel hydroxyapatite/chitosan-silk fibroin composite. Carbohydr. Polym. 2007, 68, 740–745. [Google Scholar] [CrossRef]
- Shahbazarab, Z.; Teimouri, A.; Chermahini, A.N.; Azadi, M. Fabrication and characterization of nanobiocomposite scaffold of zein/chitosan/nanohydroxyapatite prepared by freeze-drying method for bone tissue engineering. Int. J. Biol. Macromol. 2018, 108, 1017–1027. [Google Scholar] [CrossRef]
- Oliveira, J.M.; Costa, S.A.; Leonor, I.B.; Malafaya, P.B.; Mano, J.F.; Reis, R.L. Novel hydroxyapatite/carboxymethylchitosan composite scaffolds prepared through an innovative “autocatalytic” electroless coprecipitation route. J. Biomed. Mater. Res. A 2009, 88, 470–480. [Google Scholar] [CrossRef]
- Sogo, Y.; Ito, A.; Matsuno, T.; Oyane, A.; Tamazawa, G.; Satoh, T.; Yamazaki, A.; Uchimura, E.; Ohno, T. Fibronectin-calcium phosphate composite layer on hydroxyapatite to enhance adhesion, cell spread and osteogenic differentiation of human mesenchymal stem cells in vitro. Biomed. Mater. 2007, 2, 116–123. [Google Scholar] [CrossRef]
- Lin, J.; Fan, Y.; Hutchinson, D.J.; Malkoch, M. Soft hydroxyapatite composites based on triazine-trione systems as potential biomedical engineering frameworks. ACS Appl. Mater. Interfaces 2023, 15, 7329–7339. [Google Scholar] [CrossRef]
- Rhee, S.H.; Suetsugu, Y.; Tanaka, J. Biomimetic configurational arrays of hydroxyapatite nanocrystals on bio-organics. Biomaterials 2001, 22, 2843–2847. [Google Scholar] [CrossRef]
- Cross, K.J.; Huq, N.L.; Palamara, J.E.; Perich, J.W.; Reynolds, E.C. Physicochemical characterization of casein phosphopeptide-amorphous calcium phosphate nanocomplexes. J. Biol. Chem. 2005, 280, 15362–15369. [Google Scholar] [CrossRef]
- Dimopoulou, M.; Ritzoulis, C.; Papastergiadis, E.S.; Panayiotou, C. Composite materials based on okra hydrocolloids and hydroxyapatite. Food Hydrocoll. 2014, 42, 348–354. [Google Scholar] [CrossRef]
- Nakata, R.; Tachibana, A.; Tanabe, T. Preparation of keratin hydrogel/hydroxyapatite composite and its evaluation as a controlled drug release carrier. Mater. Sci. Eng. C 2014, 41, 59–64. [Google Scholar] [CrossRef]
- Manda, M.G.; da Silva, L.P.; Cerqueira, M.T.; Pereira, D.R.; Oliveira, M.B.; Mano, J.F.; Marques, A.P.; Oliveira, J.M.; Correlo, V.M.; Reis, R.L. Gellan gum-hydroxyapatite composite spongy-like hydrogels for bone tissue engineering. J. Biomed. Mater. Res. A 2018, 106A, 479–490. [Google Scholar] [CrossRef]
- Yu, P.; Bao, R.Y.; Shi, X.J.; Yang, W.; Yang, M.B. Self-assembled high-strength hydroxyapatite/graphene oxide/chitosan composite hydrogel for bone tissue engineering. Carbohyd. Polym. 2017, 155, 507–515. [Google Scholar] [CrossRef]
- Li, C.; Born, A.K.; Schweizer, T.; Zenobi-Wong, M.; Cerruti, M.; Mezzenga, R. Amyloid-hydroxyapatite bone biomimetic composites. Adv. Mater. 2014, 26, 3207–3212. [Google Scholar] [CrossRef]
- Kolanthai, E.; Colon, V.S.D.; Sindu, P.A.; Chandra, V.S.; Karthikeyan, K.R.; Babu, M.S.; Sundaram, S.M.; Palanichamy, M.; Kalkura, S.N. Effect of solvent; enhancing the wettability and engineering the porous structure of a calcium phosphate/agarose composite for drug delivery. RSC Adv. 2015, 5, 18301–18311. [Google Scholar] [CrossRef]
- Krukowski, S.; Lysenko, N.; Kolodziejski, W. Synthesis and characterization of nanocrystalline composites containing calcium hydroxyapatite and glycine. J.Solid State Chem. 2018, 264, 59–67. [Google Scholar] [CrossRef]
- Jung, J.Y.; Hong, Y.J.; Choi, Y.S.; Jeong, S.; Lee, W.K. A new method for the preparation of bioactive calcium phosphate films hybridized with 1α,25-dihydroxyvitamin D3. J. Mater. Sci. Mater. Med. 2010, 20, 2441–2453. [Google Scholar] [CrossRef]
- Vu, B.T.; Le, A.N.M.; Tang, T.N.; Dang, N.N.T.; Duong, T.T.; Hua, H.T.N.; Phan, T.B.; Ta, H.T.K.; Pham, V.H.; Tran, Q.N.; et al. Fabrication of novel bone substitute alginate—N,O-carboxymethyl chitosan—Aldehyde hyaluronic acid—Biphasic calcium phosphate for bone regeneration. React. Funct. Polym. 2023, 191, 105691. [Google Scholar] [CrossRef]
- Killion, J.A.; Geever, L.M.; Devine, D.M.; Higginbotham, C.L. Fabrication and in vitro biological evaluation of photopolymerisable hydroxyapatite hydrogel composites for bone regeneration. J. Biomater. Appl. 2014, 28, 1274–1283. [Google Scholar] [CrossRef]
- Pontons-Melo, J.C.; Balbinot, G.d.S.; Sauro, S.; Collares, F.M. Experimental composite resin with myristyltrimethylammonium bromide (MYTAB) and alpha-tricalcium phosphate (α-TCP): Antibacterial and remineralizing effect. J. Funct. Biomater. 2023, 14, 303. [Google Scholar] [CrossRef]
- Shchukin, D.G.; Sukhorukov, G.B.; Möhwald, H. Biomimetic fabrication of nanoengineered hydroxyapatite/polyelectrolyte composite shell. Chem. Mater. 2003, 15, 3947–3950. [Google Scholar] [CrossRef]
- Busch, S.; Dolhaine, H.; DuChesne, A.; Heinz, S.; Hochrein, O.; Laeri, F.; Podebrad, O.; Vietze, U.; Weiland, T.; Kniep, R. Biomimetic morphogenesis of fluorapatite-gelatin composites: Fractal growth, the question of intrinsic electric fields, core/shell assemblies, hollow spheres and reorganization of denatured collagen. Eur. J. Inorg. Chem. 1999, 1999, 1643–1653. [Google Scholar] [CrossRef]
- Tlatlik, H.; Simon, P.; Kawska, A.; Zahn, D.; Kniep, R. Biomimetic fluorapatite-gelatin nanocomposites: Pre-structuring of gelatin matrices by ion impregnation and its effect on form development. Angew. Chem. Int. Ed. Engl. 2006, 45, 1905–1910. [Google Scholar] [CrossRef]
- Kniep, R.; Simon, P. “Hidden” hierarchy of microfibrils within 3D-periodic fluorapatite-gelatin nanocomposites: Development of complexity and form in a biomimetic system. Angew. Chem. Int. Ed. Engl. 2008, 47, 1405–1409. [Google Scholar] [CrossRef]
- Brickmann, J.; Paparcone, R.; Kokolakis, S.; Zahn, D.; Duchstein, P.; Carrillocabrera, W.; Simon, P.; Kniep, R. Fluorapatite-gelatine nanocomposite superstructures: New insights into a biomimetic system of high complexity. ChemPhysChem 2010, 11, 1851–1853. [Google Scholar] [CrossRef]
- Vyalikh, A.; Simon, P.; Rosseeva, E.; Buder, J.; Kniep, R.; Scheler, U. Intergrowth and interfacial structure of biomimetic fluorapatite-gelatin nanocomposite: A solid-state NMR study. J. Phys. Chem. B 2014, 118, 724–730. [Google Scholar] [CrossRef]
- Gashti, M.P.; Stir, M.; Hulliger, J. Synthesis of bone-like micro-porous calcium phosphate/iota-carrageenan composites by gel diffusion. Colloid Surface B 2013, 110, 426–433. [Google Scholar] [CrossRef]
- Aguilera, S.B.; McCarthy, A.; Khalifian, S.; Lorenc, Z.P.; Goldie, K.; Chernoff, W.G. The role of calcium hydroxylapatite (Radiesse) as a regenerative aesthetic treatment: A narrative review. Aesthet. Surg. J. 2023, 43, 1063–1090. [Google Scholar] [CrossRef]
- Galadari, H.; Guida, S. A systematic review of Radiesse® (calcium hydroxylapatite): Evidence and recommendations for the body. Int. J. Dermatol. 2024, 63, 150–160. [Google Scholar] [CrossRef]
- Klesing, J.; Chernousova, S.; Kovtun, A.; Neumann, S.; Ruiz, L.; Gonzalez-Calbet, J.M.; Vallet-Regi, M.; Heumann, R.; Epple, M. An injectable paste of calcium phosphate nanorods, functionalized with nucleic acids, for cell transfection and gene silencing. J. Mater. Chem. 2010, 20, 6144–6148. [Google Scholar] [CrossRef]
- Thai, V.V.; Lee, B.T. Fabrication of calcium phosphate-calcium sulfate injectable bone substitute using hydroxy-propyl-methyl-cellulose and citric acid. J. Mater. Sci. Mater. Med. 2010, 21, 1867–1874. [Google Scholar] [CrossRef]
- Low, K.L.; Tan, S.H.; Zein, S.H.S.; Roether, J.A.; Mouriño, V.; Boccaccini, A.R. Calcium phosphate-based composites as injectable bone substitute materials. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 94B, 273–286. [Google Scholar] [CrossRef]
- D’Este, M.; Eglin, D. Hydrogels in calcium phosphate moldable and injectable bone substitutes: Sticky excipients or advanced 3-D carriers? Acta Biomater. 2013, 9, 5421–5430. [Google Scholar] [CrossRef]
- Daculsi, G.; Weiss, P.; Bouler, J.M.; Gauthier, O.; Millot, F.; Aguado, E. Biphasic calcium phosphate/hydrosoluble polymer composites: A new concept for bone and dental substitution biomaterials. Bone 1999, 25 (Suppl. S2), 59S–61S. [Google Scholar] [CrossRef]
- Turczyn, R.; Weiss, P.; Lapkowski, M.; Daculsi, G. In situ self-hardening bioactive composite for bone and dental surgery. J. Biomater. Sci. Polym. Edn. 2000, 11, 217–223. [Google Scholar] [CrossRef]
- Bennett, S.; Connolly, K.; Lee, D.R.; Jiang, Y.; Buck, D.; Hollinger, J.O.; Gruskin, E.A. Initial biocompatibility studies of a novel degradable polymeric bone substitute that hardens in situ. Bone 1996, 19, 101S–107S. [Google Scholar] [CrossRef]
- Shalygina, K.; Lytkina, D.; Sadykov, R.; Kurzina, I. Composite cryogels based on hydroxyapatite and polyvinyl alcohol and the study of physicochemical and mechanical properties. Materials 2024, 17, 403. [Google Scholar] [CrossRef]
- Bongio, M.; van den Beucken, J.J.J.P.; Nejadnik, M.R.; Birgani, Z.T.; Habibovic, P.; Kinard, L.A.; Kasper, F.K.; Mikos, A.G.; Leeuwenburgh, S.C.G.; Jansen, J.A. Subcutaneous tissue response and osteogenic performance of calcium phosphate nanoparticle-enriched hydrogels in the tibial medullary cavity of guinea pigs. Acta Biomater. 2013, 9, 5464–5474. [Google Scholar] [CrossRef]
- Chernousova, S.; Klesing, J.; Soklakova, N.; Epple, M. A genetically active nano-calcium phosphate paste for bone substitution, encoding the formation of BMP-7 and VEGF-A. RSC Adv. 2013, 3, 11155–11161. [Google Scholar] [CrossRef]
- Yu, B.; Zhang, Y.; Li, X.; Wang, Q.; Ouyang, Y.; Xia, Y.; Lin, B.; Li, S.; Fan, Y.; Chen, Y. The use of injectable chitosan/nanohydroxyapatite/collagen composites with bone marrow mesenchymal stem cells to promote ectopic bone formation in vivo. J. Nanomater. 2013, 2013, 506593. [Google Scholar] [CrossRef]
- Phewchan, P.; Laoruengthana, A.; Tiyaboonchai, W. Calcium phosphate incorporated in silk fibroin/methylcellulose based injectable hydrogel: Preparation, characterization and in vitro biological evaluation for bone defect treatment. J. Biomed. Mater. Res. B Appl. Biomater. 2023, 111, 1640–1652. [Google Scholar] [CrossRef]
- Bodakhe, S.; Verma, S.; Garkhal, K.; Samal, S.K.; Sharma, S.S.; Kumar, N. Injectable photocrosslinkable nanocomposite based on poly(glycerol sebacate) fumarate and hydroxyapatite: Development, biocompatibility and bone regeneration in a rat calvarial bone defect model. Nanomedicine 2013, 8, 1777–1795. [Google Scholar] [CrossRef]
- Fricain, J.C.; Aid, R.; Lanouar, S.; Maurel, D.B.; le Nihouannen, D.; Delmond, S.; Letourneur, D.; Vilamitjana, J.A.; Catros, S. In-vitro and in-vivo design and validation of an injectable polysaccharide-hydroxyapatite composite material for sinus floor augmentation. Dent. Mater. 2018, 34, 1024–1035. [Google Scholar] [CrossRef]
- Şahin, E. Enhanced injectability of aqueous β-tricalcium phosphate suspensions through PAA incorporation, gelling and preshearing. J. Mech. Behav. Biomed. Mater. 2023, 145, 106026. [Google Scholar] [CrossRef]
- Lin, G.; Cosimbescu, L.; Karin, N.J.; Tarasevich, B.J. Injectable and thermosensitive PLGA-g-PEG hydrogels containing hydroxyapatite: Preparation, characterization and in vitro release behavior. Biomed. Mater. 2012, 7, 024107. [Google Scholar] [CrossRef]
- Nejadnik, M.R.; Yang, X.; Bongio, M.; Alghamdi, H.S.; van den Beucken, J.J.J.P.; Huysmans, M.C.; Jansen, J.A.; Hilborn, J.; Ossipov, D.; Leeuwenburgh, S.C.G. Self-healing hybrid nanocomposites consisting of bisphosphonated hyaluronan and calcium phosphate nanoparticles. Biomaterials 2014, 35, 6918–6929. [Google Scholar] [CrossRef]
- Munarin, F.; Petrini, P.; Gentilini, R.; Pillai, R.S.; Dirè, S.; Tanzi, M.C.; Sglavo, V.M. Micro- and nano-hydroxyapatite as active reinforcement for soft biocomposites. Int. J. Biol. Macromol. 2015, 72, 199–209. [Google Scholar] [CrossRef]
- Douglas, T.E.L.; Schietse, J.; Zima, A.; Gorodzha, S.; Parakhonskiy, B.V.; Khalenkow, D.; Shkarin, R.; Ivanova, A.; Baumbach, T.; Weinhardt, V.; et al. Novel self-gelling injectable hydrogel/alpha-tricalcium phosphate composites for bone regeneration: Physiochemical and microcomputer tomographical characterization. J. Biomed. Mater. Res. A 2018, 106A, 822–828. [Google Scholar] [CrossRef]
- Daculsi, G.; Rohanizadeh, R.; Weiss, P.; Bouler, J.M. Crystal polymer interaction with new injectable bone substitute: SEM and HrTEM study. J. Biomed. Mater. Res. 2000, 50, 1–7. [Google Scholar] [CrossRef]
- Weiss, P.; Lapkowski, M.; LeGeros, R.Z.; Bouler, J.M.; Jean, A.; Daculsi, G. FTIR spectroscopic study of an organic/mineral composite for bone and dental substitute materials. J. Mater. Sci. Mater. Med. 1997, 8, 621–629. [Google Scholar] [CrossRef]
- Weiss, P.; Bohic, S.; Lapkowski, M.; Daculsi, G. Application of FTIR microspectroscopy to the study of an injectable composite for bone and dental surgery. J. Biomed. Mater. Res. 1998, 41, 167–170. [Google Scholar] [CrossRef]
- Weiss, P.; Layrolle, P.; Clergeau, L.P.; Enckel, B.; Pilet, P.; Amouriq, Y.; Daculsi, G.; Giumelli, B. The safety and efficacy of an injectable bone substitute in dental sockets demonstrated in a human clinical trial. Biomaterials 2007, 28, 3295–3305. [Google Scholar] [CrossRef]
- Fatimi, A.; Tassin, J.F.; Axelos, M.A.V.; Weiss, P. The stability mechanisms of an injectable calcium phosphate ceramic suspension. J. Mater. Sci. Mater. Med. 2010, 21, 1799–1809. [Google Scholar] [CrossRef]
- Trojani, C.; Boukhechba, F.; Scimeca, J.C.; Vandenbos, F.; Michiels, J.F.; Daculsi, G.; Boileau, P.; Weiss, P.; Carle, G.F.; Rochet, N. Ectopic bone formation using an injectable biphasic calcium phosphate/Si-HPMC hydrogel composite loaded with undifferentiated bone marrow stromal cells. Biomaterials 2006, 27, 3256–3264. [Google Scholar] [CrossRef]
- Zhang, S.M.; Lü, G. Clinical application of compound injectable bone substitutes in bone injury repair. J. Clin. Rehabil. Tissue Eng. Res. 2009, 13, 10117–10120. [Google Scholar]
- Daculsi, G.; Uzel, P.A.; Bourgeois, N.; le François, T.; Rouvillain, J.L.; Bourges, X.; Baroth, S. New injectable bone substitute using reversible thermosensitive hydrogel and BCP granules: In vivo rabbit experiments. Key Eng. Mater. 2009, 396–398, 457–460. [Google Scholar] [CrossRef]
- Iooss, P.; le Ray, A.M.; Grimandi, G.; Daculsi, G.; Merle, C. A new injectable bone substitute combining poly(ε-caprolactone) microparticles with biphasic calcium phosphate granules. Biomaterials 2001, 22, 2785–2794. [Google Scholar] [CrossRef]
- Bohner, M. Design of ceramic-based cements and putties for bone graft substitution. Eur. Cell Mater. 2010, 20, 1–12. [Google Scholar] [CrossRef]
- Evis, Z.; Ergun, C.; Doremus, R.H. Hydroxylapatite-zirconia composites: Thermal stability of phases and sinterability as related to the CaO-ZrO2 phase diagram. J. Mater. Sci. 2005, 40, 1127–1134. [Google Scholar] [CrossRef]
- Rao, R.R.; Kannan, T.S. Synthesis and sintering of hydroxyapatite-zirconia composites. Mater. Sci. Eng. C 2002, 20, 187–193. [Google Scholar]
- Mansur, C.; Pope, M.; Pascucci, M.R.; Shivkumar, S. Zirconia-calcium phosphate composites for bone replacement. Ceram. Int. 1998, 24, 77–79. [Google Scholar] [CrossRef]
- Kim, H.W.; Kim, H.E.; Salih, V.; Knowles, J.C. Dissolution control and cellular responses of calcium phosphate coatings on zirconia porous scaffold. J. Biomed. Mater. Res. A 2004, 68A, 522–530. [Google Scholar] [CrossRef]
- Milella, E.; Cosentino, F.; Licciulli, A.; Massaro, C. Preparation and characterisation of titania/hydroxyapatite composite coatings obtained by sol-gel process. Biomaterials 2001, 22, 1425–1431. [Google Scholar] [CrossRef]
- Tancred, D.C.; Carr, A.J.; McCormack, B.A. The sintering and mechanical behaviour of hydroxyapatite with bioglass additions. J. Mater. Sci. Mater. Med. 2001, 12, 81–93. [Google Scholar] [CrossRef]
- Goller, G.; Demirkiran, H.; Oktar, F.N.; Demirkesen, E. Processing and characterization of Bioglass reinforced hydroxyapatite composites. Ceram. Int. 2003, 29, 721–724. [Google Scholar] [CrossRef]
- Lopes, M.A.; Silva, R.F.; Monteiro, F.J.; Santos, J.D. Microstructural dependence of Young’s moduli of P2O5 glass reinforced hydroxyapatite for biomedical applications. Biomaterials 2000, 21, 749–754. [Google Scholar] [CrossRef]
- Amaral, S.S.; de Sousa Lima, B.S.; Avelino, S.O.M.; Spirandeli, B.R.; Campos, T.M.B.; Thim, G.P.; de Sousa Trichês, E.; do Prado, R.F.; de Vasconcellos, L.M.R. β-TCP/S53P4 scaffolds obtained by gel casting: Synthesis, properties and biomedical applications. Bioengineering 2023, 10, 597. [Google Scholar] [CrossRef]
- Ruiz-Aguilar, C. Porous phosphate-based bioactive glass/β-TCP scaffold for tooth remineralization. PLoS ONE 2023, 18, e0284885. [Google Scholar] [CrossRef]
- Juang, H.Y.; Hon, M.H. Fabrication and mechanical properties of hydroxyapatite-alumina composites. Mater. Sci. Eng. C 1994, 2, 77–81. [Google Scholar] [CrossRef]
- Li, J.; Forbreg, S.; Hermansson, L. Evaluation of the mechanical properties of hot isotatically pressed titania and titania-calcium phosphate composites. Biomaterials 1991, 12, 438–440. [Google Scholar] [CrossRef]
- Noma, T.; Shoji, N.; Wada, S.; Suzuki, T. Preparation of spherical Al2O3 particle dispersed hydroxyapatite ceramics. J. Ceram. Soc. Jpn. 1993, 101, 923–927. [Google Scholar] [CrossRef]
- Gautier, S.; Champion, E.; Bernache-Assollant, D. Toughening characterization in alumina platelet-hydroxyapatite matrix composites. J. Mater. Sci. Mater. Med. 1999, 10, 533–540. [Google Scholar] [CrossRef]
- Fang, Y.; Roy, D.M.; Cheng, J.; Roy, R.; Agrawal, D.K. Microwave sintering of hydroxyapatite-based composites. Ceram. Trans. 1993, 36, 397–407. [Google Scholar]
- Park, K.; Vasilosa, T. Microstructure and mechanical properties of silicon carbide whisker/calcium phosphate composites produced by hot pressing. Mater. Lett. 1997, 32, 229–233. [Google Scholar] [CrossRef]
- Jin, H.B.; Oktar, F.N.; Dorozhkin, S.; Agathopoulos, S. Sintering behavior and properties of reinforced hydroxyapatite/TCP biphasic bioceramics with ZnO-whiskers. J. Compos. Mater. 2011, 45, 1435–1445. [Google Scholar] [CrossRef]
- de With, G.; Corbijn, A.T. Metal fibre reinforced hydroxyapatite ceramics. J. Mater. Sci. 1989, 24, 341l–3415. [Google Scholar] [CrossRef]
- Ruys, A.J.; Simpson, S.A.; Sorrell, C.C. Thixotropic casting of fibre-reinforced ceramic matrix composites. J. Mater. Sci. Lett. 1994, 13, 1323–1325. [Google Scholar] [CrossRef]
- Miao, X.; Ruys, A.J.; Milthorpe, B.K. Hydroxyapatite-316L fibre composites prepared by vibration assisted slip casting. J. Mater. Sci. 2001, 36, 3323–3332. [Google Scholar] [CrossRef]
- Kim, H.M.; Chae, W.P.; Chang, K.W.; Chun, S.; Kim, S.; Jeong, Y.; Kang, I.K. Composite nanofiber mats consisting of hydroxyapatite and titania for biomedical applications. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 94B, 380–387. [Google Scholar] [CrossRef]
- Hirakura, S.; Kobayashi, T.; Ono, S.; Oaki, Y.; Imai, H. Fibrous nanocrystals of hydroxyapatite loaded with TiO2 nanoparticles for the capture and photocatalytic decomposition of specific proteins. Colloid Surface B 2010, 79, 131–135. [Google Scholar] [CrossRef]
- Wu, J.M.; Yeh, T.S. Sintering of hydroxylapatite-zirconia composite materials. J. Mater. Sci. 1988, 23, 3771–3777. [Google Scholar] [CrossRef]
- Li, J.; Liao, H.; Hermansson, L. Sintering of partially-stabilized zirconia and partially-stabilized zirconia-hydroxyapatite composites by hot isostatic pressing and pressureless sintering. Biomaterials 1996, 17, 1787–1790. [Google Scholar] [CrossRef]
- Takagi, M.; Mochida, M.; Uchida, N.; Saito, K.; Uematsu, K. Filter cake forming and hot isostatic pressing for TZP-dispersed hydroxyapatite composite. J. Mater. Sci. Mater. Med. 1992, 3, 199–203. [Google Scholar] [CrossRef]
- Shen, Z.; Adolfsson, E.; Nygren, M.; Gao, L.; Kawaoka, H.; Niihara, K. Dense hydroxyapatite-zirconia ceramic composites with high strength for biological applications. Adv. Mater. 2001, 13, 214–216. [Google Scholar] [CrossRef]
- Nagarajan, V.S.; Rao, K.J. Structural, mechanical and biocompatibility studies of hydroxyapatite-derived composites toughened by zirconia addition. J. Mater. Chem. 1993, 3, 43–51. [Google Scholar] [CrossRef]
- Quan, R.; Yang, D.; Wu, X.; Wang, H.; Miao, X.; Li, W. In vitro and in vivo biocompatibility of graded hydroxyapatite-zirconia composite bioceramic. J. Mater. Sci. Mater. Med. 2008, 19, 183–187. [Google Scholar] [CrossRef]
- Wang, L.L.; Wang, X.F.; Jiang, H.T.; Yu, C.L. Preparation of porous hydroxyapatite-zirconia composite scaffolds by combination of gel-casting and polymer sponge methods. Adv. Mater. Res. 2010, 105–106, 616–619. [Google Scholar] [CrossRef]
- Cao, Y.; Li, C.; Xia, Y.; Ren, K.; Zhu, S. Study on the fabrication and mechanical properties of HAp-3YSZ composites by flash sintering. Ceram. Int. 2022, 48, 16300–16305. [Google Scholar] [CrossRef]
- Koushik, T.M.; Miller, C.M.; Antunes, E. Optimisation of two-step sintering parameters to produce bioactive and dense zirconia-hydroxyapatite composite ceramics. J. Eur. Ceram. Soc. 2023, 43, 2222–2233. [Google Scholar] [CrossRef]
- Ge, M.; Xie, D.; Yang, Y.; Tian, Z. Sintering densification mechanism and mechanical properties of the 3D-printed high-melting-point-difference magnesium oxide/calcium phosphate composite bio-ceramic scaffold. J. Mech. Behav. Biomed. Mater. 2023, 144, 105978. [Google Scholar] [CrossRef]
- Li, J.; Fartash, B.; Hermansson, L. Hydroxyapatite-alumina composites and bone-bonding. Biomaterials 1995, 16, 417–422. [Google Scholar] [CrossRef]
- Jun, Y.K.; Kim, W.H.; Kweon, O.K.; Hong, S.H. The fabrication and biochemical evaluation of alumina reinforced calcium phosphate porous implants. Biomaterials 2003, 24, 3731–3739. [Google Scholar] [CrossRef]
- Epure, L.M.; Dimitrievska, S.; Merhi, Y.; Yahia, L.H. The effect of varying Al2O3 percentage in hydroxyapatite/Al2O3 composite materials: Morphological, chemical and cytotoxic evaluation. J. Biomed. Mater. Res. A 2007, 83A, 1009–1023. [Google Scholar] [CrossRef]
- Youness, R.A.; Saleh, H.A.; Taha, M.A. Microstructure and elastic properties of hydroxyapatite/alumina nanocomposites prepared by mechanical alloying technique for biomedical applications. Biointerface Res. Appl. Chem. 2023, 13, 395. [Google Scholar]
- Shaly, A.A.; Priya, G.H.; Mahendiran, M.; Linet, J.M. A behavioural study of hydrothermally derived novel alumina/magnesia/hydroxyapatite (Al2O3/MgO/HA) bioceramic nanocomposite. J. Mech. Behav. Biomed. Mater. 2022, 133, 105313. [Google Scholar]
- Lu, Y.P.; Li, M.S.; Li, S.T.; Wang, Z.G.; Zhu, R.F. Plasma-sprayed hydroxyapatite + titania composite bond coat for hydroxyapatite coating on titanium substrate. Biomaterials 2004, 25, 4393–4403. [Google Scholar] [CrossRef]
- Pushpakanth, S.; Srinivasan, B.; Sreedhar, B.; Sastry, T.P. An in situ approach to prepare nanorods of titania-hydroxyapatite (TiO2-HAp) nanocomposite by microwave hydrothermal technique. Mater. Chem. Phys. 2008, 107, 492–498. [Google Scholar] [CrossRef]
- Nath, S.; Tripathi, R.; Basu, B. Understanding phase stability, microstructure development and biocompatibility in calcium phosphate-titania composites, synthesized from hydroxyapatite and titanium powder mix. Mater. Sci. Eng. C 2009, 29, 97–107. [Google Scholar] [CrossRef]
- Swapna, Y.V.; Mathew, C.T.; Thomas, J.K. Resistive coupled microwave sintering of hydroxyapatite/titania nano-biocomposite and tailoring its mechanical properties. J. Mech. Behav. Biomed. Mater. 2023, 141, 105772. [Google Scholar] [CrossRef]
- Sakka, S.; Bouaziz, J.; Ben Ayed, F. Sintering and mechanical properties of the alumina-tricalcium phosphate-titania composites. Mater. Sci. Eng. C 2014, 40, 92–101. [Google Scholar] [CrossRef]
- Yang, Z.P.; Gong, X.Y.; Zhang, C.J. Recyclable Fe3O4/hydroxyapatite composite nanoparticles for photocatalytic applications. Chem. Eng. J. 2010, 165, 117–121. [Google Scholar] [CrossRef]
- Liu, Y.; Zhong, H.; Li, L.; Zhang, C. Temperature dependence of magnetic property and photocatalytic activity of Fe3O4/hydroxyapatite nanoparticles. Mater. Res. Bull. 2010, 45, 2036–2039. [Google Scholar] [CrossRef]
- Ignatovich, Z.; Novik, K.; Abakshonok, A.; Koroleva, E.; Beklemisheva, A.; Panina, L.; Kaniukov, E.; Anisovich, M.; Shumskaya, A. One-step synthesis of magnetic nanocomposite with embedded biologically active substance. Molecules 2021, 26, 937. [Google Scholar] [CrossRef]
- Biedrzycka, A.; Skwarek, E.; Hanna, U.M. Hydroxyapatite with magnetic core: Synthesis methods, properties, adsorption and medical applications. Adv. Colloid Interface Sci. 2021, 291, 102401. [Google Scholar] [CrossRef]
- Lee, B.T.; Lee, C.W.; Gain, A.K.; Song, H.Y. Microstructures and material properties of fibrous Ap/Al2O3-ZrO2 composites fabricated by multi-pass extrusion process. J. Eur. Ceram. Soc. 2007, 27, 157–163. [Google Scholar] [CrossRef]
- Oktar, F.N.; Agathopoulos, S.; Ozyegin, L.S.; Gunduz, O.; Demirkol, N.; Bozkurt, Y.; Salman, S. Mechanical properties of bovine hydroxyapatite (BHA) composites doped with SiO2, MgO, Al2O3 and ZrO2. J. Mater. Sci. Mater. Med. 2007, 18, 2137–2143. [Google Scholar] [CrossRef]
- Gunduz, O.; Erkan, E.M.; Daglilar, S.; Salman, S.; Agathopoulos, S.; Oktar, F.N. Composites of bovine hydroxyapatite (BHA) and ZnO. J. Mater. Sci. 2008, 43, 2536–2540. [Google Scholar] [CrossRef]
- Dong, L.; Zhu, Z.; Qiu, Y.; Zhao, J. Removal of lead from aqueous solution by hydroxyapatite/manganese dioxide composite. Front. Environ. Sci. Eng. 2016, 10, 28–36. [Google Scholar] [CrossRef]
- Pandey, A.; Midha, S.; Sharma, R.K.; Maurya, R.; Nigam, V.K.; Ghosh, S.; Balani, K. Antioxidant and antibacterial hydroxyapatite-based biocomposite for orthopedic applications. Mater. Sci. Eng. C 2018, 88, 13–24. [Google Scholar] [CrossRef]
- Mostafa, S.I.; Ismail, M.S.; Mohammed, H.A.; Osman, M.F.; Elwassefy, N.A. Magnetic hydroxyapatite bisphosphonate-based composites: A bone-targeting nanosystem. Emergent Mater. 2023, 6, 1273–1284. [Google Scholar] [CrossRef]
- Lopes, M.A.; Monterio, F.J.; Santos, J.D. Glass-reinforced hydroxyapatite composites: Fracture toughness and hardness dependence on microstructural characteristics. Biomaterials 1999, 20, 2085–2090. [Google Scholar] [CrossRef]
- Ragel, C.V.; Vallet-Regi, M.; Rodríguez-Lorenzo, L.M. Preparation and in vitro bioactivity of hydroxyapatite/sol-gel glass biphasic material. Biomaterials 2002, 23, 1865–1872. [Google Scholar] [CrossRef]
- Li, X.W.; Yasuda, H.Y.; Umakoshi, Y. Bioactive ceramic composites sintered from hydroxyapatite and silica at 1200 °C: Preparation, microstructures and in vitro bone-like layer growth. J. Mater. Sci. Mater. Med. 2006, 17, 573–581. [Google Scholar] [CrossRef]
- Padilla, S.; Sánchez-Salcedo, S.; Vallet-Regi, M. Bioactive and biocompatible pieces of HA/sol-gel glass mixtures obtained by the gel-casting method. J. Biomed. Mater. Res. A 2005, 75A, 63–72. [Google Scholar] [CrossRef]
- Padilla, S.; Román, J.; Sánchez-Salcedo, S.; Vallet-Regi, M. Hydroxyapatite/SiO2-CaO-P2O5 glass materials: In vitro bioactivity and biocompatibility. Acta Biomater. 2006, 2, 331–342. [Google Scholar] [CrossRef]
- Sych, E.E.; Pinchuk, N.D.; Ivanchenko, L.A. Effect of sintering temperature on the properties of biogenic hydroxyapatite-glass composites. Powder Metall. Metal Ceram. 2010, 49, 153–158. [Google Scholar] [CrossRef]
- Marovic, D.; Tarle, Z.; Hiller, K.A.; Müller, R.; Rosentritt, M.; Skrtic, D.; Schmalz, G. Reinforcement of experimental composite materials based on amorphous calcium phosphate with inert fillers. Dent. Mater. 2014, 30, 1052–1060. [Google Scholar] [CrossRef]
- Bellucci, D.; Sola, A.; Lusvarghi, L.; Cannillo, V. Hydroxyapatite-tricalcium phosphate-bioactive glass ternary composites. Ceram. Int. 2014, 40, 3805–3808. [Google Scholar] [CrossRef]
- Bellucci, D.; Sola, A.; Anesi, A.; Salvatori, R.; Chiarini, L.; Cannillo, V. Bioactive glass/hydroxyapatite composites: Mechanical properties and biological evaluation. Mater. Sci. Eng. C 2015, 51, 196–205. [Google Scholar] [CrossRef]
- Yazdanpanah, Z.; Bahrololoom, M.E.; Hashemi, B. Evaluating morphology and mechanical properties of glass-reinforced natural hydroxyapatite composites. J. Mech. Behav. Biomed. Mater. 2015, 41, 36–42. [Google Scholar] [CrossRef]
- Seyedmajidi, M.; Haghanifar, S.; Hajian-Tilaki, K.; Seyedmajidi, S. Histopathological, histomorphometrical and radiological evaluations of hydroxyapatite/bioactive glass and fluorapatite/bioactive glass nanocomposite foams as cell scaffolds in rat tibia: An in vivo study. Biomed. Mater. 2018, 13, 025015. [Google Scholar] [CrossRef]
- Esposti, L.D.; Zheng, K.; Piancastelli, A.; Ionescu, A.C.; Adamiano, A.; Boccaccini, A.R.; Iafisco, M. Composite materials of amorphous calcium phosphate and bioactive glass nanoparticles for preventive dentistry. Ceram. Int. 2024, 50, 593–602. [Google Scholar] [CrossRef]
- Makornpan, C.; Monmaturapoj, N.; Prahsarn, C.; Klinsukhon, W.; Chokevivat, W. Hydroxyapatite/titanium dioxide/bioactive glass composites with anti-microbial performance under multiple illumination conditions. J. Mater. Sci. 2023, 58, 17751–17764. [Google Scholar] [CrossRef]
- Nishio, K.; Neo, M.; Akiyama, H.; Okada, Y.; Kokubo, T.; Nakamura, T. Effects of apatite and wollastonite containing glass-ceramic powder and two types of alumina powder in composites on osteoblastic differentiation of bone marrow cells. J. Biomed. Mater. Res. 2001, 55, 164–176. [Google Scholar] [CrossRef]
- Encinas-Romero, M.A.; Aguayo-Salinas, S.; Valenzuela-García, J.L.; Payán, S.R.; Castillón-Barraza, F.F. Mechanical and bioactive behavior of hydroxyapatite-wollastonite sintered composites. Int. J. Appl. Ceram. Technol. 2010, 7, 164–177. [Google Scholar] [CrossRef]
- Ha, N.R.; Yang, Z.X.; Hwang, K.H.; Kim, T.S.; Lee, J.K. Improvement of the stability of hydroxyapatite through glass ceramic reinforcement. J. Nanosci. Nanotechnol. 2010, 10, 3459–3462. [Google Scholar] [CrossRef]
- Nath, S.; Biswas, K.; Wang, K.; Bordia, R.K.; Basu, B. Sintering, phase stability and properties of calcium phosphate-mullite composites. J. Am. Ceram. Soc. 2010, 93, 1639–1649. [Google Scholar] [CrossRef]
- Nath, S.; Ummethala, R.; Basu, B. Fretting wear behavior of calcium phosphate-mullite composites in dry and albumin-containing simulated body fluid conditions. J. Mater. Sci. Mater. Med. 2010, 21, 1151–1161. [Google Scholar] [CrossRef]
- Nath, S.; Dubey, A.K.; Basu, B. Mechanical properties of novel calcium phosphate-mullite biocomposites. J. Biomater. Appl. 2012, 27, 67–78. [Google Scholar] [CrossRef]
- Nath, S.; Kalmodia, S.; Basu, B. In vitro biocompatibility of novel biphasic calcium phosphate-mullite composites. J. Biomater. Appl. 2013, 27, 497–509. [Google Scholar] [CrossRef]
- Obada, D.O.; Osseni, S.A.; Sina, H.; Salami, K.A.; Oyedeji, A.N.; Dodoo-Arhin, D.; Bansod, N.D.; Csaki, S.; Atta, A.Y.; Fasanya, O.O.; et al. Fabrication of novel kaolin-reinforced hydroxyapatite scaffolds with robust compressive strengths for bone regeneration. Appl. Clay Sci. 2021, 215, 106298. [Google Scholar] [CrossRef]
- de Andrade, R.; Paim, T.C.; Bertaco, I.; Naasani, L.S.; Buchner, S.; Kovářík, T.; Hájek, J.; Wink, M.R. Hierarchically porous bioceramics based on geopolymer-hydroxyapatite composite as a novel biomaterial: Structure, mechanical properties and biocompatibility evaluation. Appl. Mater. Today 2023, 33, 101875. [Google Scholar] [CrossRef]
- Tseng, W.J.; Kao, W.H. Preparation of electrically conductive calcium phosphate composite foams by particle-stabilized emulsion route. Ceramics 2018, 1, 319–328. [Google Scholar] [CrossRef]
- Chaki, T.K.; Wang, P.E. Densification and strengthening of silver-reinforced hydroxyapatite-matrix composite prepared by sintering. J. Mater. Sci. Mater. Med. 1994, 5, 533–542. [Google Scholar] [CrossRef]
- Zhang, X.; Gubbels, G.H.M.; Terpstra, R.A.; Metselaar, R. Toughening of calcium hydroxyapatite with silver particles. J. Mater. Sci. 1997, 32, 235–243. [Google Scholar] [CrossRef]
- Chu, C.; Lin, P.; Dong, Y.; Xue, X.; Zhu, J.; Yin, Z. Fabrication and characterization of hydroxyapatite reinforced with 20 vol. % Ti particles for use as hard tissue replacement. J. Mater. Sci. Mater. Med. 2002, 13, 985–992. [Google Scholar] [CrossRef]
- Ning, C.Q.; Zhou, Y. In vitro bioactivity of a biocomposite fabricated from HA and Ti powders by powder metallurgy method. Biomaterials 2002, 23, 2909–2915. [Google Scholar] [CrossRef]
- Chu, C.; Xue, X.; Zhu, J.; Yin, Z. Mechanical and biological properties of hydroxyapatite reinforced with 40 vol. % titanium particles for use as hard tissue replacement. J. Mater. Sci. Mater. Med. 2004, 15, 665–670. [Google Scholar] [CrossRef]
- Karanjai, M.; Kumarb, M.B.V.; Sundaresan, R.; Basu, B.; Mohan, R.T.R.; Kashyap, B.P. Fretting wear study on Ti-Ca-P biocomposite in dry and simulated body fluid. Mater. Sci. Eng. A 2008, 475, 299–307. [Google Scholar] [CrossRef]
- Chu, C.; Xue, X.; Zhu, J.; Yin, Z. Fabrication and characterization of titanium-matrix composite with 20 vol. % hydroxyapatite for use as heavy load-bearing hard tissue replacement. J. Mater. Sci. Mater. Med. 2006, 17, 245–251. [Google Scholar] [CrossRef]
- Miranda, M.; Fernández, A.; Díaz, M.; Esteban-Tejeda, L.; López-Esteban, S.; Malpartida, F.; Torrecillas, R.; Moya, J.S. Silver-hydroxyapatite nanocomposites as bactericidal and fungicidal materials. Int. J. Mater. Res. 2010, 101, 122–127. [Google Scholar] [CrossRef]
- Khanra, A.K.; Jung, H.C.; Hong, K.S.; Shin, K.S. Comparative property study on extruded Mg–HAP and ZM61–HAP composites. Mater. Sci. Eng. A 2010, 527, 6283–6288. [Google Scholar] [CrossRef]
- Gu, X.N.; Wang, X.; Li, N.; Li, L.; Zheng, Y.F.; Miao, X. Microstructure and characteristics of the metal-ceramic composite (MgCa-HA/TCP) fabricated by liquid metal infiltration. J. Biomed. Mater. Res. B Appl. Biomater. 2011, 99, 127–134. [Google Scholar] [CrossRef]
- Liu, D.; Zuo, Y.; Meng, W.; Chen, M.; Fan, Z. Fabrication of biodegradable nano-sized β-TCP/Mg composite by a novel melt shearing technology. Mater. Sci. Eng. C 2012, 32, 1253–1258. [Google Scholar] [CrossRef]
- Kumar, A.; Biswas, K.; Basu, B. On the toughness enhancement in hydroxyapatite-based composites. Acta Mater. 2013, 61, 5198–5215. [Google Scholar] [CrossRef]
- Wang, X.; Dong, L.H.; Li, J.T.; Ma, X.L.; Zheng, Y.F. Microstructure, mechanical property and corrosion behavior of interpenetrating (HA+β-TCP)/MgCa composite fabricated by suction casting. Mater. Sci. Eng. C 2013, 33, 4266–4273. [Google Scholar] [CrossRef]
- Chang, Q.; Ru, H.Q.; Chen, D.L.; Zhang, C.P.; Yang, J.L.; Hu, S.L. Interfacial reactions in Ti–Fe particles reinforced hydroxyapatite matrix composites. Mater. Lett. 2014, 128, 245–247. [Google Scholar] [CrossRef]
- Sunil, B.R.; Kumar, T.S.S.; Chakkingal, U.; Nandakumar, V.; Doble, M. Friction stir processing of magnesium-nanohydroxyapatite composites with controlled in vitro degradation behavior. Mater. Sci. Eng. C 2014, 39, 315–324. [Google Scholar] [CrossRef]
- Buyong, S.A.; Jamaludin, S.B.; Malek, R.A. Effect of beta tricalcium phosphate (β-TCP) on properties of Mg-Zn composites. Key Eng. Mater. 2014, 594–595, 203–206. [Google Scholar] [CrossRef]
- Arifin, A.; Sulong, A.B.; Muhamad, N.; Syarif, J.; Ramli, M.I. Material processing of hydroxyapatite and titanium alloy (HA/Ti) composite as implant materials using powder metallurgy: A review. Mater. Des. 2014, 55, 165–175. [Google Scholar] [CrossRef]
- Ma, X.L.; Dong, L.H.; Wang, X. Microstructure, mechanical property and corrosion behavior of co-continuous β-TCP/MgCa composite manufactured by suction casting. Mater. Des. 2014, 56, 305–312. [Google Scholar] [CrossRef]
- Sunil, B.R.; Kumar, T.S.S.; Chakkingal, U.; Nandakumar, V.; Doble, M. Nano-hydroxyapatite reinforced AZ31 magnesium alloy by friction stir processing: A solid state processing for biodegradable metal matrix composites. J. Mater. Sci. Mater. Med. 2014, 25, 975–988. [Google Scholar] [CrossRef]
- Wakily, H.; Dabbagh, A.; Abdullah, H.; Abdul Halim, N.F.; Abu Kasim, N.H. Improved thermal and mechanical properties in hydroxyapatite–titanium composites by incorporating silica-coated titanium. Mater. Lett. 2015, 143, 322–325. [Google Scholar] [CrossRef]
- Kuśnierczyk, K.; Basista, M. Recent advances in research on magnesium alloys and magnesium-calcium phosphate composites as biodegradable implant materials. J. Biomater. Appl. 2017, 31, 878–900. [Google Scholar] [CrossRef]
- Montufar, E.B.; Casas-Luna, M.; Horynová, M.; Tkachenko, S.; Fohlerová, Z.; Diaz-de-la-Torre, S.; Dvořák, K.; Čelko, L.; Kaiser, J. High strength, biodegradable and cytocompatible alpha tricalcium phosphate-iron composites for temporal reduction of bone fractures. Acta Biomater. 2018, 70, 293–303. [Google Scholar] [CrossRef]
- Yang, H.; Qu, X.; Lin, W.; Wang, C.; Zhu, D.; Dai, K.; Zheng, Y. In vitro and in vivo studies on zinc-hydroxyapatite composites as novel biodegradable metal matrix composite for orthopedic applications. Acta Biomater. 2018, 71, 200–214. [Google Scholar] [CrossRef]
- Castañeda-Vía, J.; Landauro, C.V.; Quispe-Marcatoma, J.; Champi, A.; Montalvo, F.; Delgado, L.; Tay, L.Y.; Moya, M.J.; Guillén, R.; Rumiche, F.; et al. Improvement of mechanical properties of hydroxyapatite composites reinforced with i-Al64Cu23Fe13 quasicrystal. J. Compos. Mater. 2020, 55, 1209. [Google Scholar] [CrossRef]
- Peng, Q.; Bin, X.; Xuxin, H.Y.; Wang, Y.H.; Peng, Z.W.; Tang, Z.G. Facile fabrication of boronized Ti6Al4V/HA composites for loadbearing applications. J. Alloys Compd. 2020, 825, 153102. [Google Scholar] [CrossRef]
- Verma, V.; Saha, J.; Gautam, A.; Pal, K. Investigation on microstructure, mechanical, biocorrosion and biocompatibility behavior of nano-sized TiO2@Al2O3 reinforced Mg-HAp composites. J. Alloys Compd. 2022, 910, 164866. [Google Scholar] [CrossRef]
- Vidal, C.; Alves, P.; Alves, M.M.; Carmezim, M.J.; Fernandes, M.H.; Grenho, L.; Inácio, P.L.; Ferreira, F.B.; Santos, T.G.; Santos, C. Fabrication of a biodegradable and cytocompatible magnesium/nanohydroxyapatite/fluorapatite composite by upward friction stir processing for biomedical applications. J. Mech. Behav. Biomed. Mater. 2022, 129, 105137. [Google Scholar] [CrossRef]
- Venkatesh, V.S.S.; Kalapala, P.; Deoghare, A.B. Characterization of microwave sintered aluminium composite reinforced with hydroxyapatite extracted from Rihu fish scales. Arch. Metall. Mater. 2023, 68, 617–624. [Google Scholar] [CrossRef]
- Jayasathyakawin, S.; Ravichandran, M.; Ismail, S.O.; Srinivasan, D. Effects of hydroxyapatite addition on the microstructure and mechanical properties of sintered magnesium matrix composites. Mater. Today Comm. 2023, 35, 105582. [Google Scholar] [CrossRef]
- Chatterjee, T.; Maji, M.; Paul, S.; Ghosh, M.; Pradhan, S.K.; Meikap, A.K. Microstructural, electrical and mechanical characterizations of green-synthesized biocompatible calcium phosphate nanocomposites with morphological hierarchy. Mater. Chem. Phys. 2023, 296, 127245. [Google Scholar] [CrossRef]
- Aggarwal, D.; Kumar, V.; Sharma, S. Effect of rare earth oxide microparticles on mechanical, corrosion, antibacterial and hemolytic behavior of Mg-hydroxyapatite composite for orthopedic applications—A preliminary in-vitro study. J. Biomed. Mater. Res. B Appl. Biomater. 2023, 111, 1232–1246. [Google Scholar] [CrossRef]
- Chebodaeva, V.V.; Luginin, N.A.; Rezvanova, A.E.; Svarovskaya, N.V.; Suliz, K.V.; Ivanova, L.Y.; Khimich, M.A.; Toropkov, N.E.; Glukhov, I.A.; Miller, A.A.; et al. Formation of bioresorbable Fe-Cu-hydroxyapatite composite by 3D printing. Coatings 2023, 13, 803. [Google Scholar] [CrossRef]
- Yao, R.; Wang, H.; Shan, R.; Liu, L.; Zhao, Y.; Sun, Y.; Yao, X.; Huang, D.; Hang, R. Biodegradable porous Zn-1Mg-3βTCP scaffold for bone defect repair: In vitro and in vivo evaluation. J. Mater. Sci. Technol. 2023, 162, 189–202. [Google Scholar] [CrossRef]
- Papynov, E.K.; Shichalin, O.O.; Belov, A.A.; Buravlev, I.Y.; Mayorov, V.Y.; Fedorets, A.N.; Buravleva, A.A.; Lembikov, A.O.; Gritsuk, D.V.; Kapustina, O.V.; et al. CaSiO3-HAp metal-reinforced biocomposite ceramics for bone tissue engineering. J. Funct. Biomater. 2023, 14, 259. [Google Scholar] [CrossRef]
- Yao, R.; Zhao, Y.; Han, S.; Shan, R.; Liu, L.; Sun, Y.; Yao, X.; Wang, X.; Hang, R. Microstructure, mechanical properties, in vitro degradation behavior and in vivo osteogenic activities of Zn-1Mg-β-TCP composites for bone defect repair. Mater. Des. 2023, 225, 111494. [Google Scholar] [CrossRef]
- Jia, Q.; Liang, S.; Wang, Q. Effect of HA content on microstructure and properties of Ti-27Nb-17Ta-8Zr/HA composite. Materials 2023, 16, 5095. [Google Scholar] [CrossRef]
- Damien, C.J.; Parsons, J.R.; Benedict, J.J.; Weisman, D.S. Investigation of a hydroxyapatite and calcium sulfate composite supplemented with an osteoinductive factor. J. Biomed. Mater. Res. 1990, 24, 639–654. [Google Scholar] [CrossRef]
- Rauschmann, M.A.; Wichelhaus, T.A.; Stirnal, V.; Dingeldein, E.; Zichner, L.; Schnettler, R.; Alt, V. Nanocrystalline hydroxyapatite and calcium sulphate as biodegradable composite carrier material for local delivery of antibiotics in bone infections. Biomaterials 2005, 26, 2677–2684. [Google Scholar] [CrossRef]
- Urban, R.M.; Turner, T.M.; Hall, D.J.; Inoue, N.; Gitelis, S. Increased bone formation using calcium sulfate-calcium phosphate composite graft. Clin. Orthop. Relat. Res. 2007, 459, 110–117. [Google Scholar] [CrossRef]
- Rauschmann, M.A.; Vogl, T.; Verheyden, A.; Pflugmacher, R.; Werba, T.; Schmidt, S.; Hierholzer, J. Bioceramic vertebral augmentation with a calcium sulphate/hydroxyapatite composite (CeramentTM SpineSupport) in vertebral compression fractures due to osteoporosis. Eur. Spine J. 2010, 19, 887–892. [Google Scholar] [CrossRef]
- Nilsson, M.; Zheng, M.H.; Tägil, M. The composite of hydroxyapatite and calcium sulphate: A review of preclinical evaluation and clinical applications. Expert Rev. Med. Dev. 2013, 10, 675–684. [Google Scholar] [CrossRef]
- Du, M.K.; Kuang, Z.D.; Ji, H.R.; Mao, K.Y. Enhanced degradation and osteogenesis of β-tricalcium phosphate/calcium sulfate composite bioceramics: The effects of phase ratio. J. Biomater. Tissue Eng. 2014, 4, 389–398. [Google Scholar] [CrossRef]
- Kumar, G.S.; Girija, E.K.; Thamizhavel, A.; Yokogawa, Y.; Kalkura, S.N. Synthesis and characterization of bioactive hydroxyapatite-calcite nanocomposite for biomedical applications. J. Colloid Interf. Sci. 2010, 349, 56–62. [Google Scholar] [CrossRef]
- Smirnov, V.V.; Goldberg, M.A.; Shvorneva, L.I.; Fadeeva, I.V.; Shibaeva, T.V.; Barinov, S.M. Synthesis of composite biomaterials in the hydroxyapatite-calcite system. Dokl. Chem. 2010, 432, 151–154. [Google Scholar] [CrossRef]
- Polley, C.; Distler, T.; Detsch, R.; Lund, H.; Springer, A.; Boccaccini, A.R.; Seitz, H. 3D printing of piezoelectric barium titanate-hydroxyapatite scaffolds with interconnected porosity for bone tissue engineering. Materials 2020, 13, 1773. [Google Scholar] [CrossRef]
- Jiao, H.; Li, Z.; Zhou, X.; Zhao, K.; Tang, Y. Study on preparation and properties of tetragonal BaTiO3/HA porous scaffolds. Mater. Sci. Eng. B 2023, 296, 116703. [Google Scholar] [CrossRef]
- Swain, S.; Bhaskar, R.; Narayanan, K.B.; Gupta, M.K.; Sharma, S.; Dasgupta, S.; Han, S.S.; Kumar, P. Physicochemical, mechanical, dielectric and biological properties of sintered hydroxyapatite/barium titanate nanocomposites for bone regeneration. Biomed. Mater. 2023, 18, 025016. [Google Scholar] [CrossRef]
- Watanabe, Y.; Ikoma, T.; Suetsugu, Y.; Yamada, H.; Tamura, K.; Komatsu, Y.; Tanaka, J.; Moriyoshi, Y. The densification of zeolite/apatite composites using a pulse electric current sintering method: A long-term assurance material for the disposal of radioactive waste. J. Eur. Ceram. Soc. 2006, 26, 481–486. [Google Scholar] [CrossRef]
- Lahiri, D.; Singh, V.; Benaduce, A.P.; Seal, S.; Kos, L.; Agarwal, A. Boron nitride nanotube reinforced hydroxyapatite composite: Mechanical and tribological performance and in-vitro biocompatibility to osteoblasts. J. Mech. Behav. Biomed. Mater. 2011, 4, 44–56. [Google Scholar] [CrossRef]
- Aguirre, T.G.; Cramer, C.L.; Torres, V.P.; Hammann, T.J.; Holland, T.B.; Ma, K. Effects of the addition of boron nitride nanoplate on the fracture toughness, flexural strength and Weibull distribution of hydroxyapatite composites prepared by spark plasma sintering. J. Mech. Behav. Biomed. Mater. 2019, 93, 105–117. [Google Scholar] [CrossRef]
- Nathanael, A.J.; Yuvakkumar, R.; Hong, S.I.; Oh, T.H. Novel zirconium nitride and hydroxyapatite nanocomposite coating: Detailed analysis and functional properties. ACS Appl. Mater. Interfaces 2014, 6, 9850–9857. [Google Scholar] [CrossRef]
- Liu, Y.; Huang, J.; Li, H. Synthesis of hydroxyapatite-reduced graphite oxide nanocomposites for biomedical applications: Oriented nucleation and epitaxial growth of hydroxyapatite. J. Mater. Chem. B 2013, 1, 1826–1834. [Google Scholar] [CrossRef]
- Zhao, X.; Chen, X.; Gui, Z.; Zheng, J.; Yang, P.; Liu, A.; Wei, S.; Yang, Z. Carbon fiber reinforced hydroxyapatite composites with excellent mechanical properties and biological activities prepared by spark plasma sintering. Ceram. Int. 2020, 46, 27446–27456. [Google Scholar] [CrossRef]
- Najafinezhad, A.; Abdellahi, M.; Saber-Samandari, S.; Ghayour, H.; Khandan, A. Hydroxyapatite-M-type strontium hexaferrite: A new composite for hyperthermia applications. J. Alloys Compd. 2018, 734, 290–300. [Google Scholar] [CrossRef]
- Agathopoulos, S.; Tulyaganov, D.U.; Marques, P.A.A.P.; Ferro, M.C.; Fernandes, M.H.V.; Correia, R.N. The fluorapatite-anorthite system in biomedicine. Biomaterials 2003, 24, 1317–1331. [Google Scholar] [CrossRef]
- Khor, K.A.; Gu, Y.W.; Pan, D.; Cheang, P. Microstructure and mechanical properties of plasma sprayed HA/YSZ/Ti-6Al-4V composite coatings. Biomaterials 2004, 25, 4009–4017. [Google Scholar] [CrossRef]
- Jodati, H.; Evis, Z.; Tezcaner, A.; Alshemary, A.Z.; Motameni, A. 3D porous bioceramic based boron-doped hydroxyapatite/baghdadite composite scaffolds for bone tissue engineering. J. Mech. Behav. Biomed. Mater. 2023, 140, 105722. [Google Scholar] [CrossRef]
- Mondal, S.; Manivasagan, P.; Bharathiraja, S.; Moorthy, M.S.; Kim, H.H.; Seo, H.; Lee, K.D.; Oh, J. Magnetic hydroxyapatite: A promising multifunctional platform for nanomedicine application. Int. J. Nanomed. 2017, 12, 8389–8410. [Google Scholar] [CrossRef]
- Mondal, S.; Manivasagan, P.; Bharathiraja, S.; Moorthy, M.S.; Nguyen, V.T.; Kim, H.H.; Nam, S.Y.; Lee, K.D.; Oh, J. Hydroxyapatite coated iron oxide nanoparticles: A promising nanomaterial for magnetic hyperthermia cancer treatment. Nanomaterials 2017, 7, 426. [Google Scholar] [CrossRef]
- Adamiano, A.; Wu, V.M.; Carella, F.; Lamura, G.; Canepa, F.; Tampieri, A.; Iafisco, M.; Uskoković, V. Magnetic calcium phosphates nanocomposites for the intracellular hyperthermia of cancers of bone and brain. Nanomedicine 2019, 14, 1267–1289. [Google Scholar] [CrossRef]
- Das, A.; Pamu, D. A comprehensive review on electrical properties of hydroxyapatite based ceramic composites. Mater. Sci. Eng. C 2019, 101, 539–563. [Google Scholar] [CrossRef]
- Kalmodia, S.; Goenka, S.; Laha, T.; Lahiri, D.; Basu, B.; Balani, K. Microstructure, mechanical properties and in vitro biocompatibility of spark plasma sintered hydroxyapatite-aluminum oxide-carbon nanotube composite. Mater. Sci. Eng. C 2010, 30, 1162–1169. [Google Scholar] [CrossRef]
- Al-Harbi, N.; Hussein, M.A.; Al-Hadeethi, Y.; Umar, A. Cellulose acetate-hydroxyapatite-bioglass-zirconia nanocomposite particles as potential biomaterial: Synthesis, characterization and biological properties for bone application. Eng. Sci. 2022, 17, 70–82. [Google Scholar] [CrossRef]
- El-Mehalawy, N.; Sayed, M.; El-Anwar, E.A.A.; Soliman, A.A.F.; Naga, S.M. Preparation and characterization of bioceramic composites based on anorthite and β-TCP from dolomitic phosphate and kaolin rocks. Mater. Chem. Phys. 2024, 312, 128625. [Google Scholar] [CrossRef]
- Best, S.M.; Porter, A.E.; Thian, E.S.; Huang, J. Bioceramics: Past, present and for the future. J. Eur. Ceram. Soc. 2008, 28, 1319–1327. [Google Scholar] [CrossRef]
- de Aza, P.N.; Guitián, F.; de Aza, S. Bioeutectic: A new ceramic material for human bone replacement. Biomaterials 1997, 18, 1285–1291. [Google Scholar] [CrossRef]
- Huang, X.; Jiang, D.; Tan, S. Apatite formation on the surface of wollastonite/tricalcium phosphate composite immersed in simulated body fluid. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 69B, 70–72. [Google Scholar] [CrossRef]
- Zhang, F.; Chang, J.; Lin, K.; Lu, J. Preparation, mechanical properties and in vitro degradability of wollastonite/tricalcium phosphate macroporous scaffolds from nanocomposite powders. J. Mater. Sci. Mater. Med. 2008, 19, 167–173. [Google Scholar] [CrossRef]
- Baudín, C.; Pena, P. Review: Tailored microstructures in the system tricalcium phosphate-wollastonite-diopside for bone regeneration scaffolds. Open Ceram. 2023, 16, 100483. [Google Scholar] [CrossRef]
- Sugiura, Y.; Ono, F.; Nohara, M.; Takechi, A.; Kutara, K.; Kanda, T.; Saito, Y.; Yamada, E.; Oowada, K.; Endo, T.; et al. Inorganic silica hybrid octacalcium phosphate bone substitute: Harmonics to acceleration in biological metabolism and its curing process. Materialia 2023, 28, 101771. [Google Scholar] [CrossRef]
- Zhao, S.; Zhou, Z.; Wu, J.; Wang, S.; Guo, X.; Zhang, Q. Preparation and characterization of a novel hydroxyapatite-wollastonite/silk fibroin composite. J. Compos. Mater. 2012, 46, 1571–1581. [Google Scholar] [CrossRef]
- Greish, Y.E.; Brown, P.W. Characterization of wollastonite-reinforced HAp-Ca polycarboxylate composites. J. Biomed. Mater. Res. 2001, 55, 618–628, Erratum in J. Biomed. Mater. Res. 2001, 56, 459. [Google Scholar] [CrossRef]
- Greish, Y.E.; Brown, P.W. Characterization of bioactive glass-reinforced HAP-polymer composites. J. Biomed. Mater. Res. 2000, 52, 687–694. [Google Scholar] [CrossRef]
- Ren, Y.; Kong, W.; Liu, Y.; Yang, X.; Xu, X.; Qiang, L.; Mi, X.; Zhang, C.; Niu, H.; Wang, C.; et al. Photocurable 3D-printed PMBG/TCP scaffold coordinated with PTH (1-34) bidirectionally regulates bone homeostasis to accelerate bone regeneration. Adv. Healthc. Mater. 2023, 12, 2300292. [Google Scholar] [CrossRef]
- Radev, L.; Hristov, V.; Samuneva, B.; Ivanova, D. Organic/inorganic bioactive materials. Part II: In vitro bioactivity of collagen-calcium phosphate silicate/wollastonite hybrids. Cent. Eur. J. Chem. 2009, 7, 711–720. [Google Scholar] [CrossRef]
- Radev, L.; Hristov, V.; Fernandes, M.H.V.; Salvado, I.M.M. Organic/inorganic bioactive materials part IV: In vitro assessment of bioactivity of gelatin-calcium phosphate silicate/wollastonite hybrids. Cent. Eur. J. Chem. 2010, 8, 278–284. [Google Scholar] [CrossRef]
- Kangasniemi, I.; de Groot, K.; Wolke, J.; Andersson, O.; Luklinska, Z.; Becht, J.G.M.; Lakkisto, M.; Yli-Urpo, A. The stability of hydroxyapatite in an optimized bioactive glass matrix at sintering temperatures. J. Mater. Sci. Mater. Med. 1991, 2, 133–137. [Google Scholar] [CrossRef]
- Kangasniemi, I.M.O.; de Groot, K.; Becht, J.G.M.; Yli-Urpo, A. Preparation of dense hydroxylapatite or rhenanite containing bioactive glass composites. J. Biomed. Mater. Res. 1992, 26, 663–674. [Google Scholar] [CrossRef]
- Maruno, S.; Ban, S.; Wang, Y.F.; Iwata, H.; Itoh, H. Properties of functionally gradient composite consisting of hydroxyapatite containing glass coated titanium and characters for bioactive implant. J. Ceram. Soc. Jpn. 1992, 100, 362–367. [Google Scholar] [CrossRef]
- Bellucci, D.; Sola, A.; Cannillo, V. Hydroxyapatite and tricalcium phosphate composites with bioactive glass as second phase: State of the art and current applications. J. Biomed. Mater. Res. A 2016, 104A, 1030–1056. [Google Scholar] [CrossRef]
- Karadjian, M.; Essers, C.; Tsitlakidis, S.; Reible, B.; Moghaddam, A.; Boccaccini, A.R.; Westhauser, F. Biological properties of calcium phosphate bioactive glass composite bone substitutes: Current experimental evidence. Int. J. Mol. Sci. 2019, 20, 305. [Google Scholar] [CrossRef]
- Angioni, D.; Orrù, R.; Cao, G.; Garroni, S.; Bellucci, D.; Cannillo, V. Bioactivity enhancement by a ball milling treatment in novel bioactive glass-hydroxyapatite composites produced by spark plasma sintering. J. Eur. Ceram. Soc. 2023, 43, 1220–1229. [Google Scholar] [CrossRef]
- Angioni, D.; Orrù, R.; Cao, G.; Garroni, S.; Bellucci, D.; Cannillo, V. Recent advances on innovative bioactive glass-hydroxyapatite composites for bone tissue applications: Processing, mechanical properties and biological performance. J. Eur. Ceram. Soc. 2023, 43, 7688–7696. [Google Scholar] [CrossRef]
- Piccirillo, C.; Moreira, I.S.; Novais, R.M.; Fernandes, A.J.S.; Pullar, R.C.; Castro, P.M.L. Biphasic apatite-carbon materials derived from pyrolysed fish bones for effective adsorption of persistent pollutants and heavy metals. J. Environ. Chem. Eng. 2015, 5, 4884–4894. [Google Scholar] [CrossRef]
- Piccirillo, C. Preparation, characterisation and applications of bone char, a food waste-derived sustainable material: A review. J. Environ. Manag. 2023, 339, 117896. [Google Scholar] [CrossRef]
- White, A.A.; Best, S.M.; Kinloch, I.A. Hydroxyapatite-carbon nanotube composites for biomedical applications: A review. Int. J. Appl. Ceram. Technol. 2007, 4, 1–13. [Google Scholar] [CrossRef]
- Kharisov, B.I.; Kharissova, O.V.; González, L.T.; Méndez, Y.P.; Uflyand, I.E.; de la Fuente, I.G. Hydroxyapatite composites with carbon allotropes: Preparation, properties and applications. Particuology 2024, 88, 239–265. [Google Scholar] [CrossRef]
- Zhao, L.P.; Gao, L. Novel in situ synthesis of MWNT-hydroxyapatite composites. Carbon 2004, 42, 423–460. [Google Scholar] [CrossRef]
- Wei, Q.; Yang, X.P.; Chen, G.Q.; Tang, J.T.; Deng, X.L. The ultrasonic assisted synthesis of nano-hydroxyapatite and MWNT/hydroxyapatite composites. New Carbon Mater. 2005, 20, 164–170. [Google Scholar]
- Bai, Y.; Neupane, M.P.; Park, I.S.; Lee, M.H.; Bae, T.S.; Watari, F.; Uo, M. Electrophoretic deposition of carbon nanotubes-hydroxyapatite nanocomposites on titanium substrate. Mater. Sci. Eng. C 2010, 30, 1043–1049. [Google Scholar] [CrossRef]
- Shin, U.S.; Yoon, I.K.; Lee, G.S.; Jang, W.C.; Knowles, J.C.; Kim, H.W. Carbon nanotubes in nanocomposites and hybrids with hydroxyapatite for bone replacements. J. Tissue Eng. 2011, 2011, 674287. [Google Scholar] [CrossRef]
- Lahiri, D.; Ghosh, S.; Agarwal, A. Carbon nanotube reinforced hydroxyapatite composite for orthopedic application: A review. Mater. Sci. Eng. C 2012, 32, 1727–1758. [Google Scholar] [CrossRef]
- Kobayashi, S.; Kawai, W. Development of carbon nanofiber reinforced hydroxyapatite with enhanced mechanical properties. Compos. A 2007, 38, 114–123. [Google Scholar] [CrossRef]
- Gunawan, G.; Sopyan, I.; Nurfaezah, S.; ‘Ammar, M. Development of triphasic calcium phosphate–carbon nanotubes (HA/TCP-CNT) composite: A preliminary study. Key Eng. Mater. 2013, 531–532, 258–261. [Google Scholar] [CrossRef]
- Balani, K.; Anderson, R.; Laha, T.; Andara, M.; Tercero, J.; Crumpler, E.; Agarwal, A. Plasma-sprayed carbon nanotube reinforced hydroxyapatite coatings and their interaction with human osteoblasts in vitro. Biomaterials 2007, 28, 618–624. [Google Scholar] [CrossRef]
- Chen, Y.; Gan, C.H.; Zhang, T.H.; Yu, G.; Bai, P.; Kaplan, A. Laser-surface-alloyed carbon nanotubes reinforced hydroxyapatite composite coatings. Appl. Phys. Lett. 2005, 86, 251905. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, T.H.; Gan, C.H.; Yu, G. Wear studies of hydroxyapatite composite coating reinforced by carbon nanotubes. Carbon 2007, 45, 998–1004. [Google Scholar] [CrossRef]
- Chen, Y.; Zhang, Y.Q.; Zhang, T.H.; Gan, C.H.; Zheng, C.Y.; Yu, G. Carbon nanotube reinforced hydroxyapatite composite coatings produced through laser surface alloying. Carbon 2006, 44, 37–45. [Google Scholar] [CrossRef]
- Xu, J.L.; Khor, K.A.; Sui, J.J.; Chen, W.N. Preparation and characterization of a novel hydroxyapatite/carbon nanotubes composite and its interaction with osteoblast-like cells. Mater. Sci. Eng. C 2009, 29, 44–49. [Google Scholar] [CrossRef]
- Mukherjee, S.; Kundu, B.; Sen, S.; Chanda, A. Improved properties of hydroxyapatite-carbon nanotube biocomposite: Mechanical, in vitro bioactivity and biological studies. Ceram. Int. 2014, 40, 5635–5643. [Google Scholar] [CrossRef]
- Hooshmand, T.; Abrishamchian, A.; Najafi, F.; Mohammadi, M.; Najafi, H.; Tahriri, M. Development of sol-gel-derived multi-wall carbon nanotube/hydroxyapatite nanocomposite powders for bone substitution. J. Compos. Mater. 2014, 48, 483–489. [Google Scholar] [CrossRef]
- Lee, H.H.; Shin, U.S.; Won, J.E.; Kim, H.W. Preparation of hydroxyapatite-carbon nanotube composite nanopowders. Mater. Lett. 2010, 65, 208–211. [Google Scholar] [CrossRef]
- White, A.A.; Kinloch, I.A.; Windle, A.H.; Best, S.M. Optimization of the sintering atmosphere for high-density hydroxyapatite-carbon nanotube composites. J. R. Soc. Interface 2010, 7 (Suppl. S5), S529–S539. [Google Scholar] [CrossRef]
- Siqueira, I.A.W.B.; Oliveira, C.A.G.S.; Zanin, H.; Grinet, M.A.V.M.; Granato, A.E.C.; Porcionatto, M.A.; Marciano, F.R.; Lobo, A.O. Bioactivity behaviour of nano-hydroxyapatite/freestanding aligned carbon nanotube oxide composite. J. Mater. Sci. Mater. Med. 2015, 26, 1–10. [Google Scholar] [CrossRef]
- Figueroa-Rosales, E.X.; Martínez-Juárez, J.; García-Díaz, E.; Hernández-Cruz, D.; Sabinas-Hernández, S.A.; Robles-Águila, M.J. Photoluminescent properties of hydroxyapatite and hydroxyapatite/multi-walled carbon nanotube composites. Crystals 2021, 11, 832. [Google Scholar] [CrossRef]
- Ding, Y.; Liu, J.; Jin, X.; Lu, H.; Shen, G.; Yu, R. Poly-L-lysine/hydroxyapatite/carbon nanotube hybrid nanocomposite applied for piezoelectric immunoassay of carbohydrate antigen 19-9. Analyst 2008, 133, 184–190. [Google Scholar] [CrossRef]
- Liu, L.; Zhang, Y.; Ma, S.; Zhu, S.; Wu, S.; Wei, B.; Yang, G. Preparation and characterization of high-strength and high-modulus multi-walled carbon nanotube/hydroxyapatite/carbon fiber/polyetheretherketone composites. Appl. Sci. 2024, 14, 1723. [Google Scholar] [CrossRef]
- Slosarcyk, A.; Klisch, M.; Blazewicz, M.; Piekarczyk, J.; Stobierski, L.; Rapacz-Kmita, A. Hot pressed hydroxyapatite-carbon fibre composites. J. Eur. Ceram. Soc. 2000, 20, 1397–1402. [Google Scholar] [CrossRef]
- Dorner-Reisel, A.; Berroth, K.; Neubauer, R.; Nestler, K.; Marx, G.; Scislo, M.; Müller, E.; Slosarcyk, A. Unreinforced and carbon fibre reinforced hydroxyapatite: Resistance against microabrasion. J. Eur. Ceram. Soc. 2004, 24, 2131–2139. [Google Scholar] [CrossRef]
- Fu, T.; Zhao, J.L.; Wei, J.H.; Han, Y.; Xu, K.W. Preparation of carbon fiber fabric reinforced hydroxyapatite/epoxy composite by RTM processing. J. Mater. Sci. 2004, 39, 1411–1413. [Google Scholar] [CrossRef]
- Pecheva, E.; Pramatarova, L.; Hikov, T.; Fingarova, D.; Tanaka, Y.; Sakamoto, H.; Doi, H.; Tsutsumi, Y.; Hanawa, T. Apatite-nanodiamond composite as a functional coating of stainless steel. Surf. Interf. Anal. 2010, 42, 475–480. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, B.; Gong, Y.; Zhou, P.; Li, H. Mechanical properties of nanodiamond-reinforced hydroxyapatite composite coatings deposited by suspension plasma spraying. Appl. Surf. Sci. 2018, 439, 60–65. [Google Scholar] [CrossRef]
- Azhari, A.; Toyserkani, E.; Villain, C. Additive manufacturing of graphene-hydroxyapatite nanocomposite structures. Int. J. Appl. Ceram. Technol. 2015, 12, 8–17. [Google Scholar] [CrossRef]
- Basirun, W.J.; Nasiri-Tabrizi, B.; Baradaran, S. Overview of hydroxyapatite–graphene nanoplatelets composite as bone graft substitute: Mechanical behavior and in-vitro biofunctionality. Crit. Rev. Solid State Mater. Sci. 2018, 43, 177–212. [Google Scholar] [CrossRef]
- Djordjevic, A.; Ignjatovic, N.; Seke, M.; Jovic, D.; Uskokovic, D.; Rakocevic, Z. Synthesis and characterization of hydroxyapatite/fullerenol nanocomposites. J. Nanosci. Nanotechnol. 2015, 15, 1538–1542. [Google Scholar] [CrossRef]
- Gao, Q.; Zhang, L.; Chen, Y.; Nie, H.; Zhang, B.; Li, H. Interfacial design and construction of carbon fiber composites by strongly bound hydroxyapatite nanobelt-carbon nanotubes for biological applications. ACS Appl. Bio Mater. 2023, 6, 874–882. [Google Scholar] [CrossRef]
- Egorov, A.; Smirnov, V.; Shvorneva, L.; Kutsev, S.; Barinov, S. High-temperature hydroxyapatite-titanium interaction. Inorg. Mater. 2010, 46, 168–171. [Google Scholar] [CrossRef]
- You, C.; Bi, Y.; Chen, M.F.; Sun, Y.; Liu, D.B. Effect of the addition of nano-β-TCP on the microstructure of Mg-Zn-Zr alloy. Adv. Mater. Res. 2012, 535–537, 259–263. [Google Scholar] [CrossRef]
- Monma, H. Tricalcium phosphate ceramics complexed with hydroxyapatite. J. Ceram. Soc. Jpn. 1987, 96, 60–64. [Google Scholar] [CrossRef]
- Farzadi, A.; Solati-Hashjin, M.; Bakhshi, F.; Aminian, A. Synthesis and characterization of hydroxyapatite/β-tricalcium phosphate nanocomposites using microwave irradiation. Ceram. Int. 2011, 37, 65–71. [Google Scholar] [CrossRef]
- Angioni, D.; Orrù, R.; Cao, G.; Garroni, S.; Ricci, P.C.; Manukyan, K.V. Combustion synthesis and spark plasma sintering of apatite-tricalcium phosphate nanocomposites. Ceram. Int. 2023, 49, 26825–26833. [Google Scholar] [CrossRef]
- Zerankeshi, M.M.; Mofakhami, S.; Salahinejad, E. 3D porous HA/TCP composite scaffolds for bone tissue engineering. Ceram. Int. 2022, 48, 22647–22663. [Google Scholar] [CrossRef]
- Wu, C.C.; Huang, S.T.; Tseng, T.W.; Rao, Q.L.; Lin, H.C. FT-IR and XRD investigations on sintered fluoridated hydroxyapatite composites. J. Mol. Struct. 2010, 979, 72–76. [Google Scholar] [CrossRef]
- Suchanek, W.; Yashima, M.; Kakihana, M.; Yoshimura, M. Processing and mechanical properties of hydroxyapatite reinforced with hydroxyapatite whiskers. Biomaterials 1996, 17, 1715–1723. [Google Scholar] [CrossRef]
- Suchanek, W.; Yashima, M.; Kakihana, M.; Yoshimura, M. Hydroxyapatite/hydroxyapatite-whisker composites without sintering additives: Mechanical properties and microstructural evolution. J. Am. Ceram. Soc. 1997, 80, 2805–2813. [Google Scholar] [CrossRef]
- Kaito, T.; Mukai, Y.; Nishikawa, M.; Ando, W.; Yoshikawa, H.; Myoui, A. Dual hydroxyapatite composite with porous and solid parts: Experimental study using canine lumbar interbody fusion model. J. Biomed. Mater. Res. B Appl. Biomater. 2006, 78B, 378–384. [Google Scholar] [CrossRef]
- Farrokhi-Rad, M. Electrophoretic deposition of hydroxyapatite fiber reinforced hydroxyapatite matrix nanocomposite coatings. Surf. Coat. Technol. 2017, 329, 155–162. [Google Scholar] [CrossRef]
- Ma, C.; Zeng, Q.; Yu, L.; Yu, S.; Song, J.; Ma, Y.; Dong, X. Preparation and characterization of 3D printed hydroxyapatite-whisker-strengthened hydroxyapatite scaffold coated with biphasic calcium phosphate. Chin. J. Mech. Eng. Addit. Manuf. Front. 2023, 2, 100097. [Google Scholar] [CrossRef]
- Ramay, H.R.; Zhang, M. Biphasic calcium phosphate nanocomposite porous scaffolds for load-bearing bone tissue engineering. Biomaterials 2004, 21, 5171–5180. [Google Scholar] [CrossRef]
- Kobayashi, S.; Murakoshi, T. Characterization of mechanical properties and bioactivity of hydroxyapatite/β-tricalcium phosphate composites. Adv. Compos. Mater. 2014, 23, 163–177. [Google Scholar] [CrossRef]
- Sasaki, K.; Ninomiya, Y.; Takechi, M.; Tsuru, K.; Ishikawa, K.; Shigeishi, H.; Ohta, K.; Aikawa, T. Physical properties and antimicrobial release ability of gentamicin-loaded apatite cement/α-TCP composites: An in vitro study. Materials 2023, 16, 995. [Google Scholar] [CrossRef]
- Wang, Z.; Li, Q.; Ren, S.; Zhang, H.; Chen, J.; Li, A.; Chen, Y. Composite monetite/amorphous calcium phosphate bone cement promotes bone regeneration. Ceram. Int. 2023, 49, 7888–7904. [Google Scholar] [CrossRef]
- Matsumoto, K.; Tsuru, K.; Kawachi, G.; Maruta, M.; Matsuya, S.; Takahashi, I.; Ishikawa, K. Reinforcement of carbonate apatite bone substitutes with carbonate apatite by Ca salt introduction. J. Ceram. Soc. Jpn. 2010, 118, 521–524. [Google Scholar] [CrossRef]
- Available online: https://en.wikipedia.org/wiki/3D_printing (accessed on 1 May 2024).
- Yan, M.; Awad, H.A. Optimizing rheological properties for printability: Low-temperature extrusion 3D printing of hydroxyapatite-polycaprolactone mixture inks for bone tissue engineering. Front. Mater. 2023, 10, 1239692. [Google Scholar] [CrossRef]
- Zhang, B.; Nguyen, A.K.; Narayan, R.J.; Huang, J. Direct ink writing of vancomycin-loaded polycaprolactone/polyethylene oxide/ hydroxyapatite 3D scaffolds. J. Am. Ceram. Soc. 2022, 105, 1821–1840. [Google Scholar] [CrossRef]
- Jahangir, S.; Vecstaudza, J.; Augurio, A.; Canciani, E.; Stipniece, L.; Locs, J.; Alini, M.; Serra, T. Cell-laden 3D printed GelMA/HAp and THA hydrogel bioinks: Development of osteochondral tissue-like bioinks. Materials 2023, 16, 7214. [Google Scholar] [CrossRef]
- Wu, X.; Chen, K.; Zhang, D.; Xu, L.; Yang, X. Study on the technology and properties of 3D bioprinting SF/GT/n-HA composite scaffolds. Mater. Lett. 2019, 238, 89–92. [Google Scholar] [CrossRef]
- Adhikari, J.; Perwez, M.S.; Das, A.; Saha, P. Development of hydroxyapatite reinforced alginate–chitosan based printable biomaterial-ink. Nano-Struct. Nano-Objects 2021, 25, 100630. [Google Scholar] [CrossRef]
- Rajabi, M.; Cabral, J.D.; Saunderson, S.; Gould, M.; Ali, M.A. Development and optimisation of hydroxyapatite-polyethylene glycol diacrylate hydrogel inks for 3D printing of bone tissue engineered scaffolds. Biomed. Mater. 2023, 18, 065009. [Google Scholar] [CrossRef]
- Tajvar, S.; Hadjizadeh, A.; Samandar, S.S. Development of bioinspired biphasic calcium phosphate inks for manufacturing bone scaffolds by robocasting. 3D Print. Addit. Manuf. 2024. early view. [Google Scholar] [CrossRef]
- Tolmacheva, N.; Bhattacharyya, A.; Noh, I. Calcium phosphate biomaterials for 3D bioprinting in bone tissue engineering. Biomimetics 2024, 9, 95. [Google Scholar] [CrossRef]
- Werner, J.; Linner-Krcmar, B.; Friess, W.; Greil, P. Mechanical properties and in vitro cell compatibility of hydroxyapatite ceramics with graded pore structure. Biomaterials 2002, 23, 4285–4294. [Google Scholar] [CrossRef]
- Hsu, Y.H.; Turner, I.G.; Miles, A.W. Fabrication of porous bioceramics with porosity gradients similar to the bimodal structure of cortical and cancellous bone. J. Mater. Sci. Mater. Med. 2007, 18, 2251–2256. [Google Scholar] [CrossRef]
- Macchetta, A.; Turner, I.G.; Bowen, C.R. Fabrication of HA/TCP scaffolds with a graded and porous structure using a camphene-based freeze-casting method. Acta Biomater. 2009, 5, 1319–1327. [Google Scholar] [CrossRef]
- Watari, F.; Yokoyama, A.; Saso, F.; Uo, M.; Kawasaki, T. Fabrication and properties of functionally graded dental implant. Compos. B 1997, 28B, 5–11. [Google Scholar] [CrossRef]
- Watari, F.; Yokoyama, A.; Omori, M.; Hirai, T.; Kondo, H.; Uo, M.; Kawasaki, T. Biocompatibility of materials and development to functionally graded implant for bio-medical application. Compos. Sci. Technol. 2004, 64, 893–908. [Google Scholar] [CrossRef]
- Chu, C.; Zhu, J.; Yin, Z.; Lin, P. Structure optimization and properties of hydroxyapatite-Ti symmetrical functionally graded biomaterial. Mater. Sci. Eng. A 2001, 316, 205–210. [Google Scholar] [CrossRef]
- Chu, C.; Zhu, J.; Yin, Z.; Lin, P. Optimal design and fabrication of hydroxyapatite-Ti asymmetrical functionally graded biomaterial. Mater. Sci. Eng. A 2003, 348, 244–250. [Google Scholar] [CrossRef]
- Bai, X.; More, K.; Rouleau, C.M.; Rabiei, A. Functionally graded hydroxyapatite coatings doped with antibacterial components. Acta Biomater. 2010, 6, 2264–2273. [Google Scholar] [CrossRef]
- Inagaki, M.; Yokogawa, Y.; Kameyama, T. Effects of plasma gas composition on bond strength of hydroxyapatite/titanium composite coatings prepared by rf-plasma spraying. J. Eur. Ceram. Soc. 2006, 26, 495–499. [Google Scholar] [CrossRef]
- Pei, X.; Wang, J.; Wan, Q.; Kang, L.; Xiao, M.; Bao, H. Functionally graded carbon nanotubes/hydroxyapatite composite coating by laser cladding. Surf. Coat. Technol. 2011, 205, 4380–4387. [Google Scholar] [CrossRef]
- Boanini, E.; Torricelli, P.; Sima, F.; Axente, E.; Fini, M.; Mihailescu, I.N.; Bigi, A. Strontium and zoledronate hydroxyapatites graded composite coatings for bone prostheses. J. Colloid Interf. Sci. 2015, 448, 1–7. [Google Scholar] [CrossRef]
- Liu, C.; Han, Z.; Czernuszka, J.T. Gradient collagen/nanohydroxyapatite composite scaffold: Development and characterization. Acta Biomater. 2009, 5, 661–669. [Google Scholar] [CrossRef]
- Jamuna-Thevi, K.; Saarani, N.N.; Kadir, M.R.A.; Hermawan, H. Triple-layered PLGA/nanoapatite/lauric acid graded composite membrane for periodontal guided bone regeneration. Mater. Sci. Eng. C 2014, 43, 253–263. [Google Scholar] [CrossRef]
- Erisken, C.; Kalyon, D.M.; Wang, H. Functionally graded electrospun polycaprolactone and β-tricalcium phosphate nanocomposites for tissue engineering applications. Biomaterials 2008, 29, 4065–4073. [Google Scholar] [CrossRef]
- Nindhia, T.G.T.; Koyoshi, Y.; Kaneko, A.; Sawada, H.; Ohta, M.; Hirai, S.; Uo, M. Hydroxyapatite-silk functionally graded material by pulse electric current sintering. Trends Biomater. Artif. Organs 2008, 22, 25–29. [Google Scholar]
- Ban, S.; Hasegawa, J.; Maruno, S. Fabrication and properties of functionally gradient bioactive composites comprising hydroxyapatite containing glass coated titanium. Mater. Sci. Forum 1999, 308–311, 350–355. [Google Scholar] [CrossRef]
- Stojanovic, D.; Jokic, B.; Veljovic, D.; Petrovic, R.; Uskokovic, P.S.; Janackovic, D. Bioactive glass-apatite composite coating for titanium implant synthesized by electrophoretic deposition. J. Eur. Ceram. Soc. 2007, 27, 1595–1599. [Google Scholar] [CrossRef]
- Wong, L.H.; Tio, B.; Miao, X. Functionally graded tricalcium phosphate/fluoroapatite composites. Mater. Sci. Eng. C 2002, 20, 111–115. [Google Scholar] [CrossRef]
- Afzal, M.A.F.; Kesarwani, P.; Reddy, K.M.; Kalmodia, S.; Basu, B.; Balani, K. Functionally graded hydroxyapatite-alumina-zirconia biocomposite: Synergy of toughness and biocompatibility Mater. Sci. Eng. C 2012, 32, 1164–1173. [Google Scholar] [CrossRef]
- Kuffner, B.H.B.; Capellato, P.; Ribeiro, L.M.S.; Sachs, D.; Silva, G. Production and characterization of a 316L stainless steel/β-TCP biocomposite using the functionally graded materials (FGMs) technique for dental and orthopedic applications. Metals 2021, 11, 1923. [Google Scholar] [CrossRef]
- Okazaki, M.; Miake, Y.; Tohda, H.; Yanagisawa, T.; Matsumoto, T.; Takahashi, J. Functionally graded fluoridated apatites. Biomaterials 1999, 20, 1421–1426. [Google Scholar] [CrossRef]
- Okazaki, M.; Takahashi, J. Synthesis of functionally graded CO3 apatite as surface biodegradable crystals. Biomaterials 1999, 20, 1073–1078. [Google Scholar] [CrossRef]
- Peltola, T.; Patsi, M.; Rahiala, H.; Kangasniemi, I.; Yli-Urpo, A. Calcium phosphate induction by sol-gel-derived titania coatings on titanium substrates in vitro. J. Biomed. Mater. Res. 1998, 41, 504–510. [Google Scholar] [CrossRef]
- Heilmann, F.; Standard, O.C.; Müller, F.A.; Hoffman, M. Development of graded hydroxyapatite/CaCO3 composite structures for bone ingrowth. J. Mater. Sci. Mater. Med. 2007, 18, 1817–1824. [Google Scholar] [CrossRef]
- Katti, K.S. Biomaterials in total joint replacement. Colloid Surface B 2004, 39, 133–142. [Google Scholar] [CrossRef]
- Cavalcanti, A.; Shirinzadeh, B.; Zhang, M.; Kretly, L.C. Nanorobot hardware architecture for medical defense. Sensors 2008, 8, 2932–2958. [Google Scholar] [CrossRef]
- Zhang, H.; Xu, J.J.; Chen, H.Y. Electrochemically deposited 2D nanowalls of calcium phosphate-PDDA on a glassy carbon electrode and their applications in biosensing. J. Phys. Chem. C 2007, 111, 16564–16570. [Google Scholar] [CrossRef]
- Ding, Y.; Liu, J.; Wang, H.; Shen, G.; Yu, R. A piezoelectric immunosensor for the detection of α-fetoprotein using an interface of gold/hydroxyapatite hybrid nanomaterial. Biomaterials 2007, 28, 2147–2154. [Google Scholar] [CrossRef]
- López, M.S.P.; Tamimi, F.; López-Cabarcos, E.; López-Ruiz, B. Highly sensitive amperometric biosensor based on a biocompatible calcium phosphate cement. Biosens. Bioelectron. 2009, 24, 2574–2579. [Google Scholar] [CrossRef]
- Wang, B.; Zhang, J.J.; Pan, Z.Y.; Tao, X.Q.; Wang, H.S. A novel hydrogen peroxide sensor based on the direct electron transfer of horseradish peroxidase immobilized on silica-hydroxyapatite hybrid film. Biosens. Bioelectron. 2009, 24, 1141–1145. [Google Scholar] [CrossRef]
- Lu, L.; Zhang, L.; Zhang, X.; Huan, S.; Shen, G.; Yu, R. A novel tyrosinase biosensor based on hydroxyapatite-chitosan nanocomposite for the detection of phenolic compounds. Anal. Chim. Acta 2010, 665, 146–151. [Google Scholar] [CrossRef]
- Huixia, L.; Yong, L.; Lanlan, L.; Yanni, T.; Qing, Z.; Kun, L. Development of ammonia sensors by using conductive polymer/hydroxyapatite composite materials. Mater. Sci. Eng. C 2016, 59, 438–444. [Google Scholar] [CrossRef]
- Ajab, H.; Dennis, J.O.; Abdullah, M.A. Synthesis and characterization of cellulose and hydroxyapatite-carbon electrode composite for trace plumbum ions detection and its validation in blood serum. Int. J. Biol. Macromol. 2018, 113, 376–385. [Google Scholar] [CrossRef]
- Mirzajani, R.; Karimi, S. Preparation of γ-Fe2O3/hydroxyapatite/Cu (II) magnetic nanocomposite and its application for electrochemical detection of metformin in urine and pharmaceutical samples. Sens. Actuat. B-Chem. 2018, 270, 405–416. [Google Scholar] [CrossRef]
- Anitta, S.; Sekar, C. HAP-TiO2 nanocomposites based electrochemical sensor for selective and simultaneous detection of para-aminohippuric acid and uric acid. Microchem. J. 2022, 181, 107704. [Google Scholar] [CrossRef]
- Pompapathi, K.; Anantharaju, K.S.; Surendra, B.S.; Meena, S.; Uma, B.; Chowdhury, A.P.; Murthy, H.C.A. Synergistic effect of a Bi2Zr2O7 and hydroxyapatite composite: Organic pollutant remediation, antibacterial and electrochemical sensing applications. RSC Adv. 2023, 13, 28198–28210. [Google Scholar] [CrossRef]
- Hartati, Y.W.; Devi, M.J.; Irkham, N.; Zulqaidah, S.; Noviyanti, A.R.; Rochani, S.; Topkaya, S.N.; Einaga, Y. Electrochemical investigation of hydroxyapatite–lanthanum strontium cobalt ferrite composites (HA–LSCF) for SARS-CoV-2 aptasensors. RSC Adv. 2023, 13, 20209–20216. [Google Scholar]
- Wypych, G. Handbook of Fillers, 3rd ed.; ChemTec Publishing: New York, NY, USA, 2009; p. 800. [Google Scholar]
- Almora-Barrios, N.; de Leeuw, N.H. A density functional theory study of the interaction of collagen peptides with hydroxyapatite surfaces. Langmuir 2010, 26, 14535–14542. [Google Scholar] [CrossRef]
- Zhang, H.P.; Lu, X.; Leng, Y.; Fang, L.; Qu, S.; Feng, B.; Weng, J.; Wang, J. Molecular dynamics simulations on the interaction between polymers and hydroxyapatite with and without coupling agents. Acta Biomater. 2009, 5, 1169–1181. [Google Scholar] [CrossRef]
- Wei, Q.; Wang, Y.; Chai, W.; Zhang, Y.; Chen, X. Molecular dynamics simulation and experimental study of the bonding properties of polymer binders in 3D powder printed hydroxyapatite bioceramic bone scaffolds. Ceram. Int. 2017, 43, 13702–13709. [Google Scholar] [CrossRef]
- Rhee, S.H.; Lee, J.D.; Tanaka, J. Nucleation of hydroxyapatite crystal through chemical interaction with collagen. J. Am. Ceram. Soc. 2000, 83, 2890–2892. [Google Scholar] [CrossRef]
- Lin, X.; Li, X.; Fan, H.; Wen, X.; Lu, J.; Zhang, X. In situ synthesis of bone-like apatite/collagen nano-composite at low temperature. Mater. Lett. 2004, 58, 3569–3572. [Google Scholar] [CrossRef]
- Zhang, W.; Liao, S.S.; Cui, F.Z. Hierarchical self-assembly of nanofibrils in mineralized collagen. Chem. Mater. 2003, 15, 3221–3226. [Google Scholar] [CrossRef]
- Liu, Q.; de Wijn, J.R.; van Blitterswijk, C.A. Covalent bonding of PMMA, PBMA and poly(HEMA) to hydroxyapatite particles. J. Biomed. Mater. Res. 1998, 40, 257–263. [Google Scholar] [CrossRef]
- Li, J.; Chen, Y.P.; Yin, Y.; Yao, F.; Yao, K. Modulation of nano-hydroxyapatite size via formation on chitosan-gelatin network film in situ. Biomaterials 2007, 28, 781–790. [Google Scholar] [CrossRef]
- Zhou, S.; Zheng, X.; Yu, X.; Wang, J.; Weng, J.; Li, X.; Feng, B.; Yin, M. Hydrogen bonding interaction of poly(D,L-lactide)/hydroxyapatite nanocomposites. Chem. Mater. 2007, 19, 247–253. [Google Scholar] [CrossRef]
- Ficai, A.; Andronescu, E.; Ghitulica, C.; Voicu, G.; Trandafir, V.; Manzu, D.; Ficai, M.; Pall, S. Collagen/hydroxyapatite interactions in composite biomaterials. Mater. Plast. 2009, 46, 11–15. [Google Scholar]
- Li, J.; Dou, Y.; Yang, J.; Yin, Y.; Zhang, H.; Yao, F.; Wang, H.; Yao, K. Surface characterization and biocompatibility of micro- and nano-hydroxyapatite/chitosan-gelatin network films. Mater. Sci. Eng. C 2009, 29, 1207–1215. [Google Scholar] [CrossRef]
- Danilchenko, S.N.; Kalinkevich, O.V.; Kuznetsov, V.N.; Kalinkevich, A.N.; Kalinichenko, T.G.; Poddubny, I.N.; Starikov, V.V.; Sklyar, A.M.; Sukhodub, L.F. Thermal transformations of the mineral component of composite biomaterials based on chitosan and apatite. Cryst. Res. Technol. 2010, 45, 685–691. [Google Scholar] [CrossRef]
- Popescu, L.M.; Rusti, C.F.; Piticescu, R.M.; Buruiana, T.; Valero, T.; Kintzios, S. Synthesis and characterization of acid polyurethane–hydroxyapatite composites for biomedical applications. J. Compos. Mater. 2013, 47, 603–612. [Google Scholar] [CrossRef]
- Ryabenkova, Y.; Jadav, N.; Conte, M.; Hippler, M.F.; Reeves-McLaren, N.; Coates, P.D.; Twigg, P.; Paradkar, A. Mechanism of hydrogen-bonded complex formation between ibuprofen and nanocrystalline hydroxyapatite. Langmuir 2017, 33, 2965–2976. [Google Scholar] [CrossRef]
- Sanchez, A.G.; Prokhorov, E.; Luna-Barcenas, G.; Mora-García, A.G.; Kovalenko, Y.; Rivera-Muñoz, E.M.; Raucci, M.G.; Buonocore, G. Chitosan-hydroxyapatite nanocomposites: Effect of interfacial layer on mechanical and dielectric properties. Mater. Chem. Phys. 2018, 217, 151–159. [Google Scholar] [CrossRef]
- Zarif, M.E.; Bita, B.; Yehia-Alexe, S.A.; Negut, I.; Groza, A. Spectral analysis of strontium-doped calcium phosphate/chitosan composite films. Polymers 2023, 15, 4245. [Google Scholar] [CrossRef]
- Boanini, E.; Gazzano, M.; Rubini, K.; Bigi, A. Composite nanocrystals provide new insight on alendronate interaction with hydroxyapatite structure. Adv. Mater. 2007, 19, 2499–2502. [Google Scholar] [CrossRef]
- Nastasović, A.B.; Ignjatović, N.L.; Uskoković, D.P.; Marković, D.D.; Ekmeščić, B.M.; Maksin, D.D.; Onjia, A.E. Determination of thermodynamic interactions of poly(L-lactide) and biphasic calcium phosphate/poly(L-lactide) composite by inverse gas chromatography at infinite dilution. J. Mater. Sci. 2014, 49, 5076–5086. [Google Scholar] [CrossRef]
- Tsuchiya, K.; Yoshioka, T.; Ikoma, T.; Tanaka, J. Chemical interaction between hydroxyapatite and organic molecules in biomaterials. Ceram. Trans. 2010, 210, 531–535. [Google Scholar]
- Dorozhkin, S.V. Is there a chemical interaction between calcium phosphates and hydroxypropylmethylcellulose (HPMC) in organic/inorganic composites? J. Biomed. Mater. Res. 2001, 54, 247–255. [Google Scholar] [CrossRef]
- Aminzare, M.; Eskandari, A.; Baroonian, M.H.; Berenov, A.; Hesabi, Z.R.; Taheri, M.; Sadrnezhaad, S.K. Hydroxyapatite nanocomposites: Synthesis, sintering and mechanical properties. Ceram. Int. 2013, 39, 2197–2206. [Google Scholar] [CrossRef]
- Shuai, C.; Yu, L.; Feng, P.; Gao, C.; Peng, S. Interfacial reinforcement in bioceramic/biopolymer composite bone scaffold: The role of coupling agent. Colloid Surface B 2020, 193, 111083. [Google Scholar] [CrossRef]
- Kickelbick, G. Concepts for the incorporation of inorganic building blocks into organic polymers on a nanoscale. Prog. Polym. Sci. 2003, 28, 83–114. [Google Scholar] [CrossRef]
- Uskokovic, P.S.; Tang, C.Y.; Tsui, C.P.; Ignjatovic, N.; Uskokovic, D.P. Micromechanical properties of a hydroxyapatite/poly-L-lactide biocomposite using nanoindentation and modulus mapping. J. Eur. Ceram. Soc. 2007, 27, 1559–1564. [Google Scholar] [CrossRef]
- Todo, M.; Kagawa, T. Improvement of fracture energy of HA/PLLA biocomposite material due to press processing. J. Mater. Sci. 2008, 43, 799–801. [Google Scholar] [CrossRef]
- Shuai, C.; Yu, L.; Feng, P.; Peng, S.; Pan, H.; Bai, X. Construction of a stereocomplex between poly(D-lactide) grafted hydroxyapatite and poly(L-lactide): Toward a bioactive composite scaffold with enhanced interfacial bonding. J. Mater. Chem. B 2022, 10, 214–223. [Google Scholar] [CrossRef]
- Grossman, R.F. Coupling agents. In Polymer Modifiers and Additives; Lutz, J.T., Jr., Grossman, R.F., Eds.; CRC Press: Boca Raton, FL, USA, 2000; pp. 95–106. [Google Scholar]
- Liu, Q.; de Wijn, J.R.; van Blitterswijk, C.A. Nanoapatite/polymer composites: Mechanical and physicochemical characteristics. Biomaterials 1997, 18, 1263–1270. [Google Scholar] [CrossRef]
- Yang, W.F.; Long, L.; Wang, R.; Chen, D.; Duan, S.; Xu, F.J. Surface-modified hydroxyapatite nanoparticle-reinforced polylactides for three-dimensional printed bone tissue engineering scaffolds. J. Biomed. Nanotechnol. 2018, 14, 294–303. [Google Scholar] [CrossRef]
- Pramanik, N.; Mohapatra, S.; Bhargava, P.; Pramanik, P. Chemical synthesis and characterization of hydroxyapatite (HAp)–poly(ethylene co vinyl alcohol) (EVA) nanocomposite using a phosphonic acid coupling agent for orthopedic applications. Mater. Sci. Eng. C 2009, 29, 228–236. [Google Scholar] [CrossRef]
- Cui, Y.; Liu, Y.; Cui, Y.; Jing, X.; Zhang, P.; Chen, X. The nanocomposite scaffold of poly(lactide-co-glycolide) and hydroxyapatite surface-grafted with L-lactic acid oligomer for bone repair. Acta Biomater. 2009, 5, 2680–2692. [Google Scholar] [CrossRef]
- Zhang, P.; Hong, Z.; Yu, T.; Chen, X.; Jing, X. In vivo mineralization and osteogenesis of nanocomposite scaffold of poly(lactide-co-glycolide) and hydroxyapatite surface-grafted with poly(L-lactide). Biomaterials 2009, 30, 58–70. [Google Scholar] [CrossRef]
- Chang, M.C.; Ikoma, T.; Kikuchi, M.; Tanaka, J. Preparation of a porous hydroxyapatite/collagen nanocomposite using glutataldehyde as a crosslinkage agent. J. Mater. Sci. Lett. 2001, 20, 1199–1201. [Google Scholar] [CrossRef]
- Sousa, R.A.; Reis, R.L.; Cunha, A.M.; Bevis, M.J. Coupling of HDPE/hydroxyapatite composites by silane-based methodologies. J. Mater. Sci. Mater. Med. 2003, 14, 475–487. [Google Scholar] [CrossRef]
- Dupraz, A.M.P.; de Wijn, J.R.; van der Meer, S.A.T.; Goedemoed, J.H. Biocompatibility screening of silane-treated hydroxyapatite powders for use as filler in resorbable composites. J. Mater. Sci. Mater. Med. 1996, 7, 731–738. [Google Scholar] [CrossRef]
- Dupraz, A.M.P.; de Wijn, J.R.; van der Meer, S.A.T.; de Groot, K. Characterization of silane-treated hydroxyapatite powders reinforced for use as filler in biodegradable composites. J. Biomed. Mater. Res. 1996, 30, 231–238. [Google Scholar] [CrossRef]
- Liao, J.G.; Wang, X.J.; Zuo, Y.; Zhang, L.; Wen, J.Q.; Li, Y. Surface modification of nano-hydroxyapatite with silane agent. J. Inorg. Mater. 2008, 23, 145–149. [Google Scholar] [CrossRef]
- Rakmae, S.; Ruksakulpiwat, Y.; Sutapun, W.; Suppakarn, N. Effect of silane coupling agent treated bovine bone based carbonated hydroxyapatite on in vitro degradation behavior and bioactivity of PLA composites. Mater. Sci. Eng. C 2012, 32, 1428–1436. [Google Scholar] [CrossRef]
- Marcomini, A.L.; Rego, B.T.; Bretas, R.E.S. Improvement of the short- and long-term mechanical properties of injection-molded poly(etheretherketone) and hydroxyapatite nanocomposites. J. Appl. Polym. Sci. 2017, 134, 44476. [Google Scholar] [CrossRef]
- Misra, D.N. Adsorption of zirconyl salts and their acids on hydroxyapatite: Use of salts as coupling agents to dental polymer composites. J. Dent. Res. 1985, 12, 1405–1408. [Google Scholar] [CrossRef]
- Carmen, A.; Rosestela, P.; Arquimedes, K.; Gema, G.; Nohemy, D.; Yanixia, S.; Luís, B.J. Characterization of HDPE/HA composites treated with titanate and zirconate coupling agents. Macromol. Symp. 2007, 247, 190–198. [Google Scholar] [CrossRef]
- Chow, W.S.; Tham, W.L.; Ishak, Z.A.M. Improvement of microstructure and properties of poly(methyl methacrylate)/hydroxyapatite composites treated with zirconate coupling agent. J. Thermoplast. Compos. Mater. 2012, 25, 165–180. [Google Scholar] [CrossRef]
- Tham, W.L.; Chow, W.S.; Ishak, Z.A.M. Effects of titanate coupling agent on the mechanical, thermal and morphological properties of poly(methyl methacrylate)/hydroxyapatite denture base composites. J. Compos. Mater. 2011, 45, 2335–2345. [Google Scholar] [CrossRef]
- Shen, D.; Fang, L.; Chen, X.; Tang, Y. Structure and properties of polyacrylic acid modified hydroxyapatite/liquid crystal polymer composite. J. Reinfor. Plast. Comp. 2011, 30, 1155–1163. [Google Scholar] [CrossRef]
- Qu, R.; Song, X.; Wang, Y.; Zhao, Y.; Fu, X. Hydroxyapatite cross-linked in situ polyvinyl alcohol hydrogel for bionic calcified cartilage layer. Colloid Surface B 2023, 230, 113510. [Google Scholar] [CrossRef]
- Liu, Q.; de Wijn, J.R.; van Blitterswijk, C.A. A study on the grafting reaction of isocyanates with hydroxyapatite particles. J. Biomed. Mater. Res. 1998, 40, 358–364. [Google Scholar] [CrossRef]
- Tanaka, H.; Yasukawa, A.; Kandori, K.; Ishikawa, T. Surface modification of calcium hydroxyapatite with hexyl and decyl phosphates. Colloid Surface A 1997, 125, 53–62. [Google Scholar] [CrossRef]
- Borum-Nicholas, L.; Wilson, O.C., Jr. Surface modification of hydroxyapatite. Part I. Dodecyl alcohol. Biomaterials 2003, 24, 3671–3679. [Google Scholar] [CrossRef]
- Borum, L.; Wilson, O.C., Jr. Surface modification of hydroxyapatite. Part II. Silica. Biomaterials 2003, 24, 3681–3688. [Google Scholar] [CrossRef]
- Li, Y.; Weng, W. Surface modification of hydroxyapatite by stearic acid: Characterization and in vitro behaviors. J. Mater. Sci. Mater. Med. 2008, 19, 19–25. [Google Scholar] [CrossRef]
- Lee, S.C.; Choi, H.W.; Lee, H.J.; Kim, K.J.; Chang, J.H.; Kim, S.Y.; Choi, J.; Oh, K.S.; Jeong, Y.K. In-situ synthesis of reactive hydroxyapatite nano-crystals for a novel approach of surface grafting polymerization. J. Mater. Chem. 2007, 17, 174–180. [Google Scholar] [CrossRef]
- Sánchez-Salcedo, S.; Colilla, M.; Izquierdo-Barba, I.; Vallet-Regi, M. Design and preparation of biocompatible zwitterionic hydroxyapatite. J. Mater. Chem. B 2013, 1, 1595–1606. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Functionalized calcium orthophosphates (CaPO4) and their biomedical applications. J. Mater. Chem. B 2019, 7, 7471–7489. [Google Scholar] [CrossRef]
- Kennedy, B.M.; de Barra, E.; Hampshire, S.; Kelleher, M.C. Investigation of oleic acid as a dispersant for hydroxyapatite powders for use in ceramic filled photo-curable resins for stereolithography. J. Eur. Ceram. Soc. 2023, 43, 7146–7166. [Google Scholar] [CrossRef]
- Heidari, B.S.; Lopez, E.M.; Chen, P.; Ruan, R.; Vahabli, E.; Davachi, S.M.; Granero-Moltó, F.; De-Juan-Pardo, E.M.; Zheng, M.; Doyle, B. Silane-modified hydroxyapatite nanoparticles incorporated into polydioxanone/poly(lactide-co-caprolactone) creates a novel toughened nanocomposite with improved material properties and in vivo inflammatory responses. Mater. Today Bio 2023, 22, 100778. [Google Scholar]
- Morita, S.; Furuya, K.; Ishihara, K.; Nakabayashi, N. Performance of adhesive bone cement containing hydroxyapatite particles. Biomaterials 1998, 19, 1601–1606. [Google Scholar] [CrossRef]
- Shinzato, S.; Nakamura, T.; Tamura, J.; Kokubo, T.; Kitamura, Y. Bioactive bone cement: Effects of phosphoric ester monomer on mechanical properties and osteoconductivity. J. Biomed. Mater. Res. 2001, 56, 571–577. [Google Scholar] [CrossRef]
- Omori, M.; Okubo, A.; Otsubo, M.; Hashida, T.; Tohji, K. Consolidation of multi-walled carbon nanotube and hydroxyapatite coating by the spark plasma system (SPS). Key Eng. Mater. 2004, 254–256, 395–398. [Google Scholar] [CrossRef]
- Zhao, B.; Hu, H.; Mandal, S.K.; Haddon, R.C. A bone mimic based on the self-assembly of hydroxyapatite on chemically functionalized single-walled carbon nanotubes. Chem. Mater. 2005, 17, 3235–3241. [Google Scholar] [CrossRef]
- Zhang, H.; Zhou, L.; Zhang, W. Control of scaffold degradation in tissue engineering: A review. Tissue Eng. B Rev. 2014, 20, 492–502. [Google Scholar] [CrossRef]
- Wu, H.; Wei, X.; Liu, Y.; Dong, H.; Tang, Z.; Wang, N.; Bao, S.; Wu, Z.; Shi, L.; Zheng, X.; et al. Dynamic degradation patterns of porous polycaprolactone/β-tricalcium phosphate composites orchestrate macrophage responses and immunoregulatory bone regeneration. Bioact. Mater. 2023, 21, 595–611. [Google Scholar] [CrossRef]
- Ehrenfried, L.M.; Patel, M.H.; Cameron, R.E. The effect of tri-calcium phosphate (TCP) addition on the degradation of polylactide-co-glycolide (PLGA). J. Mater. Sci. Mater. Med. 2008, 19, 459–466. [Google Scholar] [CrossRef]
- Ehrenfried, L.M.; Farrar, D.; Cameron, R.E. Degradation properties of co-continuous calcium-phosphate-polyester composites. Biomacromolecules 2009, 10, 1976–1985. [Google Scholar] [CrossRef]
- Pan, J.; Han, X.; Niu, W.; Cameron, R.E. A model for biodegradation of composite materials made of polyesters and tricalcium phosphates. Biomaterials 2011, 32, 2248–2255. [Google Scholar] [CrossRef]
- Barrett, C.E.; Cameron, R.E. X-ray microtomographic analysis of α-tricalcium phosphate-poly(lactic-co-glycolic) acid nanocomposite degradation. Polymer 2014, 55, 4041–4049. [Google Scholar] [CrossRef]
- Ahlfeld, T.; Lode, A.; Placht, A.M.; Fecht, T.; Wolfram, T.; Grom, S.; Hoess, A.; Vater, C.; Bräuer, C.; Heinemann, S.; et al. A comparative analysis of 3D printed scaffolds consisting of poly(lactic-co-glycolic) acid and different bioactive mineral fillers: Aspects of degradation and cytocompatibility. Biomater. Sci. 2023, 11, 5590–5604. [Google Scholar] [CrossRef]
- Heidemann, W.; Jeschkeit, S.; Ruffieux, K.; Fischer, J.H.; Wagner, M.; Krüger, G.; Wintermantel, E.; Gerlach, K.L. Degradation of poly(D,L)lactide implants with or without addition of calciumphosphates in vivo. Biomaterials 2001, 22, 2371–2381. [Google Scholar] [CrossRef]
- Adamus, A.; Jozwiakowska, J.; Wach, R.A.; Suarez-Sandoval, D.; Ruffieux, K.; Rosiak, J.M. In vitro degradation of β-tricalcium phosphate reinforced poly(L-lactic acid). Mater. Sci. Forum 2012, 714, 283–290. [Google Scholar] [CrossRef]
- Ahola, N.; Veiranto, M.; Rich, J.; Efimov, A.; Hannula, M.; Seppälä, J.; Kellomäki, M. Hydrolytic degradation of composites of poly(L-lactide-co-ε-caprolactone) 70/30 and β-tricalcium phosphate. J. Biomater. Appl. 2013, 28, 529–543. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Inorganic chemistry of the dissolution phenomenon: The dissolution mechanism of calcium apatites at the atomic (ionic) level. Comments Inorg. Chem. 1999, 20, 285–299. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Dissolution mechanism of calcium apatites in acids: A review of literature. World J. Methodol. 2012, 2, 1–17. [Google Scholar] [CrossRef]
- Davison, N.L.; Barrère-de Groot, F.; Grijpma, D.W. Degradation of biomaterials. In Tissue Engineering, 2nd ed.; Van Blitterswijk, C.A., de Boer, J., Eds.; Academic Press: Cambridge, MA, USA, 2014; Chapter 6; pp. 177–215. [Google Scholar]
- Tajvar, S.; Hadjizadeh, A.; Samandari, S.S. Scaffold degradation in bone tissue engineering: An overview. Int. Biodeter. Biodegr. 2023, 180, 105599. [Google Scholar] [CrossRef]
- Furukawa, T.; Matsusue, Y.; Yasunaga, T.; Shikinami, Y.; Okuno, M.; Nakamura, T. Biodegradation behavior of ultra-high strength hydroxyapatite/poly(L-lactide) composite rods for internal fixation of bone fractures. Biomaterials 2000, 21, 889–898. [Google Scholar] [CrossRef]
- Furukawa, T.; Matsusue, Y.; Yasunaga, T.; Nakagawa, Y.; Okada, Y.; Shikinami, Y.; Okuno, M.; Nakamura, T. Histomorphometric study on high-strength hydroxyapatite/poly(L-lactide) composite rods for internal fixation of bone fractures. J. Biomed. Mater. Res. 2000, 50, 410–419. [Google Scholar] [CrossRef]
- Yasunaga, T.; Matsusue, Y.; Furukawa, T.; Shikinami, Y.; Okuno, M.; Nakamura, T. Bonding behaviour of ultrahigh strength unsintered hydroxyapatite particles/poly(L-lactide) composites to surface of tibial cortex in rabbits. J. Biomed. Mater. Res. 1999, 47, 412–419. [Google Scholar] [CrossRef]
- Habraken, W.J.E.M.; Liao, H.B.; Zhang, Z.; Wolke, J.G.C.; Grijpma, D.W.; Mikos, A.G.; Feijen, J.; Jansen, J.A. In vivo degradation of calcium phosphate cement incorporated into biodegradable microspheres. Acta Biomater. 2010, 6, 2200–2211. [Google Scholar] [CrossRef]
- Ngiam, M.; Liao, S.; Patil, A.J.; Cheng, Z.; Chan, C.K.; Ramakrishna, S. The fabrication of nano-hydroxyapatite on PLGA and PLGA/collagen nanofibrous composite scaffolds and their effects in osteoblastic behavior for bone tissue engineering. Bone 2009, 45, 4–16. [Google Scholar]
- Hasegawa, S.; Ishii, S.; Tamura, J.; Furukawa, T.; Neo, M.; Matsusue, Y.; Shikinami, Y.; Okuno, M.; Nakamura, T. A 5–7 year in vivo study of high-strength hydroxyapatite/poly(L-lactide) composite rods for the internal fixation of bone fractures. Biomaterials 2006, 27, 1327–1332. [Google Scholar]
- Alambiaga-Caravaca, A.M.; López-Castellano, A.; Chou, Y.F.; Luzi, A.; Núñez, J.M.; Banerjee, A.; Sancho, M.d.M.J.; Sauro, S. Release kinetics of monomers from dental composites containing fluoride-doped calcium phosphates. Pharmaceutics 2023, 15, 1948. [Google Scholar] [CrossRef]
- Moreno-Gomez, I. A Phenomenological Mathematical Modelling Framework for the Degradation of Bioresorbable Composites; Springer Theses; Springer: Cham, Switzerland, 2019; p. 368. [Google Scholar]
- Dalfino, S.; Savadori, P.; Piazzoni, M.; Connelly, S.T.; Giannì, A.B.; del Fabbro, M.; Tartaglia, G.M.; Moroni, L. Regeneration of critical-sized mandibular defects using 3D-printed composite scaffolds: A quantitative evaluation of new bone formation in in vivo studies. Adv. Healthc. Mater. 2023, 12, 2300128. [Google Scholar] [CrossRef]
- Niu, Y.; Chen, L.; Wu, T. Recent advances in bioengineering bone revascularization based on composite materials comprising hydroxyapatite. Int. J. Mol. Sci. 2023, 24, 12492. [Google Scholar] [CrossRef]
- Mo, X.; Zhang, D.; Liu, K.; Zhao, X.; Li, X.; Wang, W. Nano-hydroxyapatite composite scaffolds loaded with bioactive factors and drugs for bone tissue engineering. Int. J. Mol. Sci. 2023, 24, 1291. [Google Scholar] [CrossRef]
- Sivakumar, P.M.; Yetisgin, A.A.; Demir, E.; Sahin, S.B.; Cetinel, S. Polysaccharide-bioceramic composites for bone tissue engineering: A review. Int. J. Biol. Macromol. 2023, 250, 126237. [Google Scholar] [CrossRef]
- Osakue, A.S.; Martina, M.; Luvuyo, T. Calcium phosphate bonded wood and fiber composite panels: Production and optimization of panel properties. Holzforschung 2017, 71, 725–732. [Google Scholar] [CrossRef]
- Chen, F.F.; Zhu, Y.J.; Xiong, Z.C.; Dong, L.Y.; Chen, F.; Lu, B.Q.; Yang, R.L. Hydroxyapatite nanowire-based all-weather flexible electrically conductive paper with superhydrophobic and flame-retardant properties. ACS Appl. Mater. Interfaces 2017, 9, 39534–39548. [Google Scholar] [CrossRef]
- Guo, W.; Wang, X.; Zhang, P.; Liu, J.; Song, L.; Hu, Y. Nano-fibrillated cellulose-hydroxyapatite based composite foams with excellent fire resistance. Carbohyd. Polym. 2018, 195, 71–78. [Google Scholar] [CrossRef]
- Zhang, Z.; Wang, X.; Wang, H.; Zhao, J. Removal of Pb(II) from aqueous solution using hydroxyapatite/calcium silicate hydrate (HAP/C-S-H) composite adsorbent prepared by a phosphate recovery process. Chem. Eng. J. 2018, 344, 53–61. [Google Scholar] [CrossRef]
- Wang, Y.; Liang, D.; Liu, F.; Zhang, W.; Di, X.; Wang, C. A polyethylene glycol/hydroxyapatite composite phase change material for thermal energy storage. Appl. Therm. Eng. 2017, 113, 1475–1482. [Google Scholar] [CrossRef]
- Ion, R.M.; Nyokong, T.; Nwahara, N.; Suica-Bunghez, I.R.; Iancu, L.; Teodorescu, S.; Dulama, I.D.; Stirbescu, R.M.; Gheboianu, A.; Grigorescu, R.M. Wood preservation with gold hydroxyapatite system. Herit. Sci. 2018, 6, 37. [Google Scholar] [CrossRef]
- Chen, F.; Zhang, J.; Li, N.; Zhang, C.; Ji, B.; Hu, L.; Zhao, T.; Wang, Z.; Zhang, S. Heat insulating, fire retardant and flexible inorganic nanocomposite paper. Mater. Des. 2018, 144, 281–289. [Google Scholar] [CrossRef]
- Yang, R.L.; Zhu, Y.J.; Chen, F.F.; Qin, D.D.; Xiong, Z.C. Recyclable, fire-resistant, superhydrophobic and magnetic paper based on ultralong hydroxyapatite nanowires for continuous oil/water separation and oil collection. ACS Sustain. Chem. Eng. 2018, 6, 10140–10150. [Google Scholar] [CrossRef]
- Fischer, D.; Parks, S.C.; Mannhart, J. Bio-inspired synthetic ivory as a sustainable material for piano keys. Sustainability 2019, 11, 6538. [Google Scholar] [CrossRef]
- Saroja, A.P.V.K.; Kumar, A.R.; Moharana, B.C.; Kamaraj, M.; Ramaprabhu, S. Design of porous calcium phosphate based gel polymer electrolyte for quasi-solid state sodium ion battery. J. Electroanal. Chem. 2020, 859, 113864. [Google Scholar] [CrossRef]
- Lv, J.; Chen, Z.; Li, X. Calcium phosphate paints for full-daytime subambient radiative cooling. ACS Appl. Energy Mater. 2022, 5, 4117–4124. [Google Scholar] [CrossRef]
- Niranjana, L.S.; Mathankumar, M.; Karthikkumar, D.; Ranjithkumar, R.; Chandar, S.B.; Wong, L.S.; Djearamane, S. Characterization of calcium phosphate chitosan nanocomposite as plant growth promoter. J. Exp. Biol. Agr. Sci. 2022, 10, 567–574. [Google Scholar] [CrossRef]
- Waghmare, P.G.; Narwade, V.N.; Naik, K.B.; Kutte, V.D.; Bogle, K.A.; Mahabole, M.P. CuO/HAp composites: Excellent dielectric materials. Mater. Today Proc. 2023, 72, 2681–2686. [Google Scholar] [CrossRef]
- Guo, W.; Chen, Y.; Cui, L.; Xu, N.; Wang, M.; Sun, Y.; Yan, Y. Nano-hydroxyapatite/carbon nanotube: An excellent anode modifying material for improving the power output and diclofenac sodium removal of microbial fuel cells. Bioelectrochemistry 2023, 154, 108523. [Google Scholar] [CrossRef]
- Zhou, W.; Zhou, X.; Song, W.; Wang, C.; Zhang, H.; Huang, X. Removal of benzohydroxamic acid from aqueous solutions using multi-walled carbon nanotubes/iron-doped hydroxyapatite composites: Synthesis, adsorption performance and characteristics. J. Environ. Chem. Eng. 2023, 11, 111259. [Google Scholar] [CrossRef]
- Luu, T.T.; Huynh, N.D.; Kim, H.; Lin, Z.H.; Choi, D. Highly stretchable hydroxyapatite bionanocomposite for high-performance triboelectric nanogenerators. Nanoscale 2023, 15, 14205–14214. [Google Scholar] [CrossRef]
- Bongio, M.; van den Beucken, J.J.J.P.; Leeuwenburgh, S.C.G.; Jansen, J.A. Development of bone substitute materials: From ‘biocompatible’ to ‘instructive’. J. Mater. Chem. 2010, 20, 8747–8759. [Google Scholar] [CrossRef]
- George, S.M.; Nayak, C.; Singh, I.; Balani, K. Multifunctional hydroxyapatite composites for orthopedic applications: A review. ACS Biomater. Sci. Eng. 2022, 8, 3162–3186. [Google Scholar] [CrossRef]
- Meyers, M.A.; Lin, A.Y.M.; Seki, Y.; Chen, P.Y.; Kad, B.K.; Bodde, S. Structural biological composites: An overview. JOM 2006, 58, 36–43. [Google Scholar] [CrossRef]
- Polo-Corrales, L.; Latorre-Esteves, M.; Ramirez-Vick, J.E. Scaffold design for bone regeneration. J. Nanosci. Nanotechnol. 2014, 14, 15–56. [Google Scholar] [CrossRef]
- Kumar, A.; Kargozar, S.; Baino, F.; Han, S.S. Additive manufacturing methods for producing hydroxyapatite and hydroxyapatite-based composite scaffolds: A review. Front. Mater. 2019, 6, 313. [Google Scholar] [CrossRef]
- Jagadeeshanayaka, N.; Awasthi, S.; Jambagi, S.C.; Srivastava, C. Bioactive surface modifications through thermally sprayed hydroxyapatite composite coatings: A review of selective reinforcements. Biomater. Sci. 2022, 10, 2484–2523. [Google Scholar] [CrossRef]
- Fattah-Alhosseini, A.; Chaharmahali, R.; Alizad, S.; Kaseem, M. Corrosion behavior of composite coatings containing hydroxyapatite particles on Mg alloys by plasma electrolytic oxidation: A review. J. Magnes. Alloy 2023, 11, 2999–3011. [Google Scholar] [CrossRef]
- Liu, F.; Wang, Y.; Cao, J.; Chen, J.; Luo, T.; Zhou, C.; Tang, Y.; Xie, H. A simple method for fabricating polymer/ceramic functionally graded material scaffold. Ceram. Int. 2024, 50, 14497–14512. [Google Scholar] [CrossRef]
- Joo, S.; Gwon, Y.; Kim, S.; Park, S.; Kim, J.; Hong, S. Piezoelectrically and topographically engineered scaffolds for accelerating bone regeneration. ACS Appl. Mater. Interfaces 2024, 16, 1999–2011. [Google Scholar] [CrossRef]
- Mouriño, V.; Cattalini, J.P.; Roether, J.A.; Dubey, P.; Roy, I.; Boccaccini, A.R. Composite polymer-bioceramic scaffolds with drug delivery capability for bone tissue engineering. Expert Opin. Drug Deliv. 2013, 10, 1353–1365. [Google Scholar] [CrossRef]
- Shi, J.; Dai, W.; Gupta, A.; Zhang, B.; Wu, Z.; Zhang, Y.; Pan, L.; Wang, L. Frontiers of hydroxyapatite composites in bionic bone tissue engineering. Materials 2022, 15, 8475. [Google Scholar] [CrossRef]

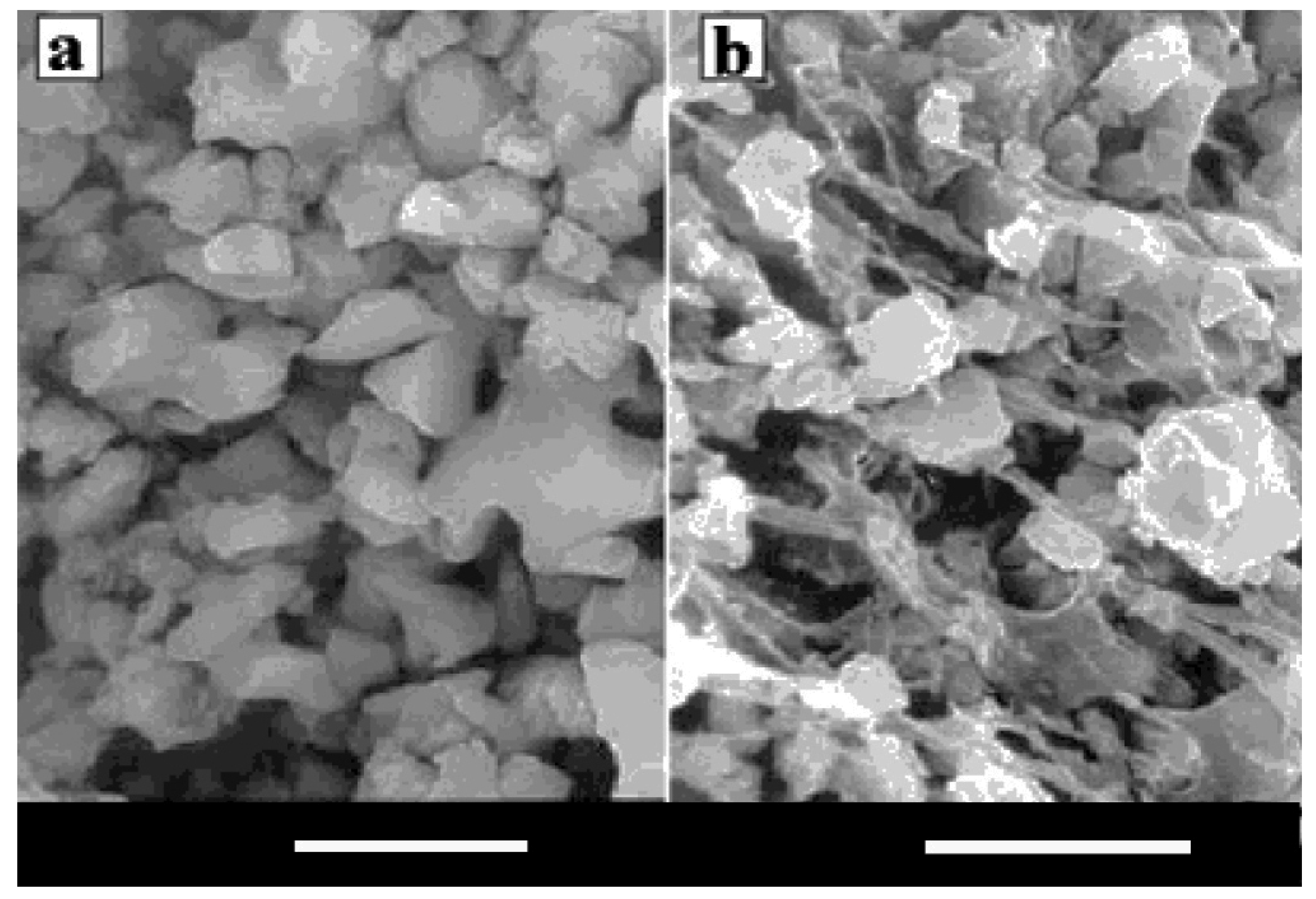













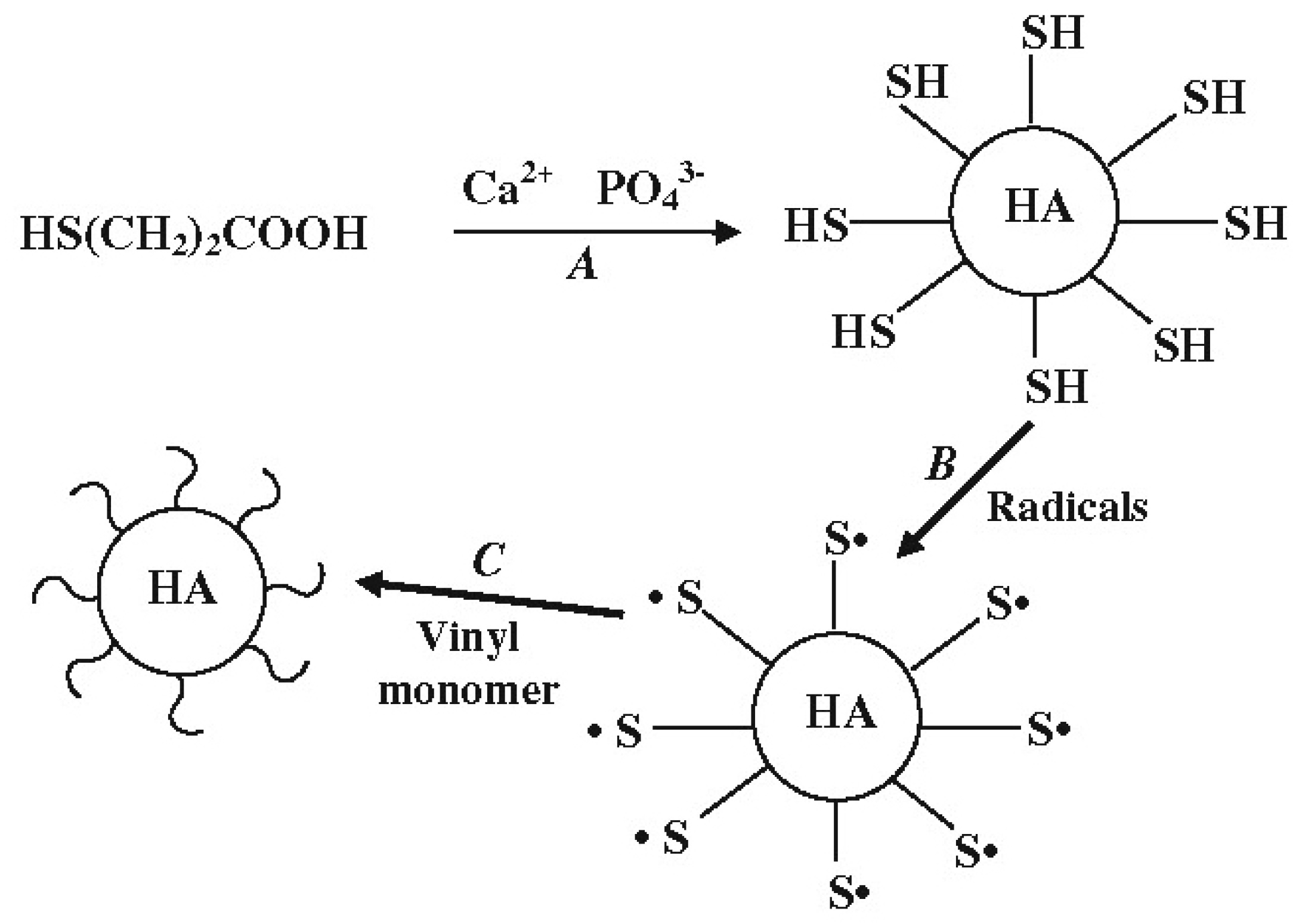
| Inorganic Phases | wt% | Bioorganic Phases | wt% |
|---|---|---|---|
| CaPO4 (biological apatite) | ~60 | collagen type I | ~20 |
| water | ~9 | non-collagenous proteins: osteocalcin, osteonectin, osteopontin, thrombospondin, morphogenetic proteins, sialoprotein, serum proteins | ~3 |
| carbonates | ~4 | other traces: polysaccharides, lipids, cytokines | balance |
| citrates | ~0.9 | primary bone cells: osteoblasts, osteocytes, osteoclasts | balance |
| sodium | ~0.7 | ||
| magnesium | ~0.5 | ||
| other traces: Cl−, F−, K+ Sr2+, Pb2+, Zn2+, Cu2+, Fe2+ | balance |
| Inorganic | Bioorganic |
|---|---|
| hardness, brittleness | elasticity, plasticity |
| high density | low density |
| thermal stability | permeability |
| hydrophilicity | hydrophobicity |
| high refractive index | selective complexation |
| mixed valence slate (red-ox) | chemical reactivity |
| strength | bioactivity |
| Ca/P Molar Ratio | Compound | Formula | Solubility at 25 °C, −log(Ks) | Solubility at 25 °C, g/L | pH Stability Range in Aqueous Solutions at 25 °C |
|---|---|---|---|---|---|
| 0.5 | Monocalcium phosphate monohydrate (MCPM) | Ca(H2PO4)2·H2O | 1.14 | ~18 | 0.0–2.0 |
| 0.5 | Monocalcium phosphate anhydrous (MCPA or MCP) | Ca(H2PO4)2 | 1.14 | ~17 | [c] |
| 1.0 | Dicalcium phosphate dihydrate (DCPD), mineral brushite | CaHPO4·2H2O | 6.59 | ~0.088 | 2.0–6.0 |
| 1.0 | Dicalcium phosphate anhydrous (DCPA or DCP), mineral monetite | CaHPO4 | 6.90 | ~0.048 | [c] |
| 1.33 | Octacalcium phosphate (OCP) | Ca8(HPO4)2(PO4)4·5H2O | 96.6 | ~0.0081 | 5.5–7.0 |
| 1.5 | α-Tricalcium phosphate (α-TCP) | α-Ca3(PO4)2 | 25.5 | ~0.0025 | [a] |
| 1.5 | β-Tricalcium phosphate (β-TCP) | β-Ca3(PO4)2 | 28.9 | ~0.0005 | [a] |
| 1.2–2.2 | Amorphous calcium phosphates (ACP) | CaxHy(PO4)z·nH2O, n = 3–4.5; 15–20% H2O | [b] | [b] | ~5–12 [d] |
| 1.5–1.67 | Calcium-deficient hydroxyapatite (CDHA or Ca-def HA) [e] | Ca10−x(HPO4)x(PO4)6−x(OH)2−x (0 < x < 1) | ~85 | ~0.0094 | 6.5–9.5 |
| 1.67 | Hydroxyapatite (HA, HAp or OHAp) | Ca10(PO4)6(OH)2 | 116.8 | ~0.0003 | 9.5–12 |
| 1.67 | Fluorapatite (FA or FAp) | Ca10(PO4)6F2 | 120.0 | ~0.0002 | 7–12 |
| 1.67 | Oxyapatite (OA, OAp or OXA) [f], mineral voelckerite | Ca10(PO4)6O | ~69 | ~0.087 | [a] |
| 2.0 | Tetracalcium phosphate (TTCP or TetCP), mineral hilgenstockite | Ca4(PO4)2O | 38–44 | ~0.0007 | [a] |
| Calcium Orthophosphate | Trade Name and Producer (When Available) |
|---|---|
| HA embedded or suspended in a gel | Bio-Gel HT hydroxyapatite (Bio-Rad, Hercules, CA, USA) |
| Coaptite (Boston Scientific, Marlborough, MA, USA) | |
| Facetem (Daewoong, Seoul, Republic of Korea) | |
| NanoBone (Artoss, Rostock, Germany) | |
| Nanogel (Teknimed, L’Union, France) | |
| Radiesse (Merz Aesthetics, Frankfurt, Germany) | |
| Renú Calcium Hydroxylapatite Implant (Cytophil, East Troy, WI, USA) | |
| HA/collagen, CDHA/collagen and/or carbonate apatite/collagen | AUGMATRIX (Wright Medical Technology, Memphis, TN, USA) |
| Bioimplant (Connectbiopharm, Vienna, Austria) | |
| Bio-Oss Collagen (Geitslich, Wolhusen, Switzerland) | |
| Boneject (Koken, Tokyo, Japan) | |
| COL.HAP-91 (JHS Biomateriais, Sabará, Brazil) | |
| Collagraft (Zimmer and Collagen Corporation, Miami, FL, USA) | |
| CollaOss (SK Bioland, Cheonan, Korea) | |
| CollapAn (Intermedapatite, Moscow, Russia) | |
| COLLAPAT (Symatese, Vourles, France) | |
| DualPor collagen (OssGen, Seoul, Republic of Korea) | |
| G-Graft (Surgiwear, Uttar Pradesh, India) | |
| HAPCOL (Polystom, Moscow, Russia) | |
| Healos (DePuy Spine, Raynham, MA, USA) | |
| LitAr (LitAr, Moscow, Russia) | |
| nanOss Bioactive (Pioneer Surgical Technology, Marquette, MI, USA) | |
| Ossbone Collagen (SK Bioland, Cheonan, Korea) | |
| OssFill (Sewon Cellontech, Seoul, Republic of Korea) | |
| OssiMend (Collagen Matrix, Oakland, NJ, USA) | |
| OSSIX Bone (Dentsply Sirona, Charlotte, NC, USA) | |
| Osteomatrix (Connectbiopharm, Russia) | |
| OsteoTape (Impladent, Queens, NY, USA) | |
| ReFit (HOYA Technosurgical, Tochigi, Japan) | |
| RegenOss (JRI Orthopaedics, Sheffield, UK) | |
| RegenerOss Synthetic (Zimmer Dental, Carlsbad, CA, USA) | |
| SmartBone (IBI, Mezzovico, Switzerland) | |
| Straumann XenoFlex (Straumann, Basel, Switzerland) | |
| SwissBone (IBI, Mezzovico, Switzerland) | |
| HA/sodium alginate | Bialgin (Biomed, Moscow, Russia) |
| rhBMP-2 + HA carrier | NOVOSIS (CGBIO, Seoul, Republic of Korea) |
| HA/poly-l-lactic acid | Biosteon (Biocomposites, Keele, UK) |
| Fisiograft HA pasta (Ghimas, Casalecchio di Reno, Italy) | |
| ReOss (ReOss, Filderstadt, Germany) | |
| OSTEOTRANS MX (Teijin Medical Technologies, Osaka, Japan) | |
| SuperFIXSORB30 (Takiron, Osaka, Japan) | |
| HA/hyaluronic acid | HArmonyCa (Allergan Aesthetics, an AbbVie Company, Dublin, UK) |
| HA/polyethylene | HAPEX (Gyrus, Memphis, TN, USA) |
| HA/glucan polysaccharide | FlexiOss (Medical Inventi, Lublin, Poland) |
| HA/CaSO4 | BioWrist Bone Void Filler (Skeletal Kinetics, Cupertino, CA, USA) |
| Bond Apatite (Augma Biomaterials, Spotswood, NJ, USA) | |
| Hapset (LifeCore, Chaska, MN, USA) | |
| PerOssal (aap Implantate, Berlin, Germany) | |
| HA/CaSO4 powders suspended in a liquid | CERAMENT (BONESUPPORT, Lund, Sweden) |
| HA/glass | Bonelike (unknwn producer) |
| bovine bone (unsintered) | Unilab Surgibone (Unilab, Hillside, NJ, USA) |
| bovine bone (unsintered) + polymer | Alpha-Bio’s Graft (Alpha-Bio Tec, Petah Tikva, Israel) |
| C-Graft Putty (unknwn producer) | |
| human bone allograft | ALLOPURE (Wright Medical Technology, Memphis, TN, USA) |
| AlloOss (ACE Surgical Supply, Brockton, MA, USA) | |
| Allosorb (Curasan, Frankfurt, Germany) | |
| CancellOss (Impladent, Queens, NY, USA) | |
| CurOss (Impladent, Queens, NY, USA) | |
| J Bone Block (Impladent, Queens, NY, USA) | |
| Maxgraft (botiss, Berlin, Germany) | |
| Mega-Oss (Megagen Implant, Daegu, Korea) | |
| NonDemin (Impladent, Queens, NY, USA) | |
| Osnatal (aap Implantate, Berlin, Germany) | |
| OsteoDemin (Impladent, Queens, NY, USA) | |
| Osteopure (O.S.T Laboratories, Saint-Beauzire, France) | |
| OsteoWrap (Curasan, Frankfurt, Germany) | |
| OVIS ALLO (DENTIS, Seoul, Republic of Korea) | |
| PentOS OI (Citagenix, Laval, QC, Canada) | |
| Puros (Zimmer Biomet, Stamford, CT, USA) | |
| RAPTOS (Citagenix, Laval, QC, Canada) | |
| Straumann AlloGraft (Straumann, Basel, Switzerland) | |
| TenFUSE (Wright Medical Technology, Memphis, TN, USA) | |
| β-TCP/CaSO4 | Fortoss vital (Biocomposites, Keele, UK) |
| Genex (Biocomposites, Keele, UK) | |
| β-TCP/poly-lactic acid | Bilok (Biocomposites, Keele, UK) |
| Duosorb (SBM, Lourdes, France) | |
| Matryx Interference Screws (Conmed, Largo, FL, USA) | |
| β-TCP/poly-lactic-co-glycolic acid | Evolvemer TCP30PLGA (Arctic Biomaterials, Tampere, Finland) |
| β-TCP/polymer | AttraX putty (NuVasive, San Diego, CA, USA) |
| ExcelOs-inject (CGBIO, Seoul, Republic of Korea) | |
| Therigraft (Therics, Akron, OH, USA) | |
| β-TCP/bone marrow aspirate | Induce (Skeletal Kinetics, Cupertino, CA, USA) |
| β-TCP/collagen | Integra Mozaik (Integra Orthobiologics, Carlsbad, CA, USA) |
| β-TCP/growth-factor | GEM 21S (Lynch Biologics, Franklin, TN, USA) |
| β-TCP/rhPDGF-BB solution | AUGMENT Bone Graft (Wright Medical Group, Memphis, TN, USA) |
| BCP (HA + β-TCP)/collagen | Allograft (Zimmer, Warsaw, IN, USA) |
| BestAid (Maxigen Biotech, Taipei, Taiwan) | |
| collacone max (botiss, Berlin, Germany) | |
| Collagraft (Zimmer, Warsaw, IN, USA) | |
| Cross.Bone Matrix (Biotech Dental, Salon-de-Provence, France) | |
| FormaGraft (Maxigen Biotech, Taipei, Taiwan) | |
| Indost (Polystom, Moscow, Russia) | |
| MasterGraft (Medtronic Sofamor Danek, Memphis, TN, USA) | |
| MATRI BONE (Biom’Up, Saint-Pries, France) | |
| Osteon III collagen (GENOSS, Suwon, Korea) | |
| SynergOss (Nobil Bio Ricerche, Portacomaro, Italy) | |
| without trade name (MedicalGroup, Lyon, France) | |
| BCP (HA + β-TCP)/hydrogel | 4MATRIX+ (MIS Implants, Misgav, Israel) |
| Eclipse (Citagenix, QC, Laval, Canada) | |
| BCP (HA + β-TCP)/polymer | In’Oss (Biomatlante, Vigneux-de-Bretagne, France) |
| Hydros (Biomatlante, Vigneux-de-Bretagne, France) | |
| Octane HyperPEEK (Octane, Toronto, ON, Canada) | |
| Osteocaf (Texas Innovative Medical Devices, Fort Worth, TX, USA) | |
| Osteotwin (Biomatlante, Vigneux-de-Bretagne, France) | |
| BCP (HA + β-TCP)/chitosan | k-IBS (Bioceramed, Lisboa, Portugal) |
| BCP (HA + β-TCP)/fibrin | TricOS (Baxter BioScience, Maurepas, France) |
| BCP (HA + β-TCP)/silicon | FlexHA (Xomed, Jacksonville, FL, USA) |
| BCP (HA + β-TCP)/bioglass | SIGNAFUSE (Bioventus, Durham, NC, USA) |
| bioglass + α-TCP + β-TCP + HA + polymers | OsteoFlo NanoPutty (SurGenTec, FL, USA) |
| FA + BCP (HA + β-TCP) | FtAP (Polystom, Moscow, Russia) |
| DCPA + MgHPO4·3H2O + SiO2 + carboxymethyl cellulose | Novogro (OsteoNovus, Toledo, OH, USA) |
| DCPD/collagen | CopiOs Bone Void Filler (Zimmer, Warsaw, IN, USA) |
| DCPD + β-TCP/CaSO4 | PRO-DENSE (Wright Medical Group, Memphis, TN, USA) |
| DCPD + β-TCP/CaSO4 + collagen | PRO-STIM (Wright Medical Group, Memphis, TN, USA) |
| OCP/fibrin | FibroFor (BioNova, Moscow, Russia) |
| OCP/collagen | Bonarc (Toyobo, Tokyo, Japan) |
| undisclosed CaPO4 + biologics | i-FACTOR (Cerapedics, Broomfield, CO, USA) |
| 3D-printed Ti mesh embedded in MCPM + β-TCP + Ca pyrophosphate | OssDsign (OssDsign AB, Uppsala, Sweden) |
| Producer | Product Name | Composition | Form |
|---|---|---|---|
| Allergan Aesthetics | HArmonyCa™ | HA, hyaluronic acid, 0.3% lidocaine | pre-mixed |
| ApaTech (Borehamwood, UK) | Actifuse™ | HA, polymer and aqueous solution | pre-mixed |
| Actifuse™ Shape Actifuse™ ABX | Si-substituted CaPO4 and a polymer | pre-mixed | |
| Baxter (Deerfield, IL, USA) | TricOs Τ TricOs | BCP (60% HA, 40% β-TCP) granules and Tissucol (fibrin glue) | to be mixed |
| Berkeley Advanced Biomaterials (Berkeley, CA, USA) | Bi-Ostetic Putty | not disclosed | not disclosed |
| BioForm (San Diego, CA, USA) | Calcium hydroxylapatite implant | HA powder embedded in a mixture of glycerine, water and CMC | pre-mixed |
| Biomatlante (Vigneux-de-Bretagne, France) | In’Oss™ | BCP granules (60% HA, 40% β-TCP; 0.08–0.2 mm) and 2% HPMC | pre-mixed |
| MBCP Gel® | BCP granules (60% HA, 40% β-TCP; 0.08–0.2 mm) and 2% HPMC | pre-mixed | |
| Hydr’Os | BCP granules (60% HA, 40% β-TCP; micro- and nanosized particles) and saline solution | pre-mixed | |
| Bioceramed (PT) | k-IBS® | BCP granules (75% HA, 25% β-TCP; 0.125–0.355 mm) and chitosan dissolved in PEG | pre-mixed |
| n-IBS® | Aqueous suspension of HA powders | pre-mixed | |
| Degradable solutions (Shanghai, China) | Easy graft™ | β-TCP or BCP granules (0.45–l.0 mm) coated with 10 μm PLGA, N-methyl-2-pyrrolydone | to be mixed |
| Dentsply (USA) | Pepgen P-15® flow | HA (0.25–0.42 mm), P-15 peptide and aqueous Na hyaluronate solution | to be mixed |
| DePuy Spine (USA) | Healos® Fx | HA (20–30%) and collagen | to be mixed |
| Fluidinova (Maia, Portugal) | nanoXIM TCP | β-TCP (5 or 15%) and water | pre-mixed |
| nanoXIM HA | HA (5, 15, 30 or 40%) and water | pre-mixed | |
| Integra LifeSciences (Princeton, NJ, USA) | Mozaik Osteoconductive Scaffold | β-TCP (80%) and type 1 collagen (20%) | to be mixed |
| Mathys Ltd. (Bettlach, Switzerland) | Ceros® Putty/cyclOS® Putty | β-TCP granules (0.125–0.71 mm; 94%) and recombinant Na hyaluronate powder (6%) | to be mixed |
| Medtronic (USA) | Mastergraft® | BCP (85% HA, 15% β-TCP) and bovine collagen | to be mixed |
| Merz Aesthetics (GER) | RADIESSE® | HA particles suspended in a gel | pre-mixed |
| NuVasive (USA) | AttraX® putty | β-TCP and alkylene oxide copolymer | pre-mixed |
| Osartis/AAΡ (Münster, Germany) | Ostim® | Nanocrystalline HA (35%) and water (65%) | pre-mixed |
| Smith & Nephew (Memphis, TN, USA) | JAXTCP | β-TCP granules and an aqueous solution of 1.75% CMC and 10% glycerol | to be mixed |
| Stryker (Portage, MI, USA) | Calstrux™ | β-TCP granules and CMC | to be mixed |
| Teknimed (FR) | Nanogel | HA (100–200 nm) (30%) and water (70%) | pre-mixed |
| Therics (USA) | Therigraft™ Putty | β-TCP granules and polymer | pre-mixed |
| Zimmer (USA) | Collagraft | BCP granules (65% HA, 35% β-TCP; 0.5–1.0 mm), bovine collagen and bone marrow aspirate | to be mixed |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dorozhkin, S.V. Calcium Orthophosphate (CaPO4) Containing Composites for Biomedical Applications: Formulations, Properties, and Applications. J. Compos. Sci. 2024, 8, 218. https://doi.org/10.3390/jcs8060218
Dorozhkin SV. Calcium Orthophosphate (CaPO4) Containing Composites for Biomedical Applications: Formulations, Properties, and Applications. Journal of Composites Science. 2024; 8(6):218. https://doi.org/10.3390/jcs8060218
Chicago/Turabian StyleDorozhkin, Sergey V. 2024. "Calcium Orthophosphate (CaPO4) Containing Composites for Biomedical Applications: Formulations, Properties, and Applications" Journal of Composites Science 8, no. 6: 218. https://doi.org/10.3390/jcs8060218
APA StyleDorozhkin, S. V. (2024). Calcium Orthophosphate (CaPO4) Containing Composites for Biomedical Applications: Formulations, Properties, and Applications. Journal of Composites Science, 8(6), 218. https://doi.org/10.3390/jcs8060218







