Abstract
In recent years, hydroxyapatite, as a ceramic material, has been a subject of growing interest due to its optimal biological properties, which are useful especially in medical and dental applications. It has been increasingly used in dentistry as a filler in composites. Nevertheless, research has shown a deterioration of their mechanical properties. The aim of this study was to investigate the influence of the content of hydroxyapatite together with fluorine and silver on the mechanical properties of a hybrid composite used in conservative dentistry. The authors compared specimens of commercial hybrid composite with specimens of experimental hybrid composite containing 2 wt% and 5 wt% of hydroxyapatite powder with fluorine and silver. The composite specimens were subjected to hardness and impact strength measurements, as well as bending, compression, and tribological wear tests. The research results indicate that the mechanical properties of composites are influenced by the type and amount of filler used. Composite containing 2 wt% of hydroxyapatite powder along with calcium fluoride and silver provided acceptable results.
1. Introduction
Dental caries is one of the most common and fastest-spreading human diseases. It affects 3.5 million people around the world [1,2]. Tooth decay is caused by the presence of cariogenic bacteria Streptococcus mutans (S. mutans) in the oral cavity [3,4], inappropriate alimentary habits and lack of oral hygiene. It results in irreversible damage to the hard tooth tissues.
The damaged tooth tissues can be restored with materials such as composites and ceramics. Light-cured composites are used for direct restoration [5]. They are composed mainly of a resin matrix (Bis-GMA TEGDMA, UDMA) and inorganic fillers (silicon oxide, colloidal silica, quartz, boron glass, aluminum oxide-lithium) [6,7,8,9]. They also contain accelerators and initiators, which promote the light-curing process. Camphorquinones (0.03–0.09%) are used to activate the visible light-induced polymerization. They initiate a free radical reaction after being exposed to light of the approximate wavelength of 470 nm [10]. The chemical composition of the organic matrix and the inorganic filler particles influence the properties of the composite. The filler particles provide dimensional stability and are also responsible for increasing the mechanical strength of the composite [11,12,13,14].
In recent years, research has been focused on the modification of dental composites in order to obtain the best possible mechanical properties and aesthetics [15,16,17]. Various calcium phosphates have been added to these materials, such as hydroxyapatite (HAp) [10,18,19,20,21], amorphous calcium phosphates (ACP) [22,23,24], tetracalcium phosphate (TTCP) [25,26] and anhydrous dicalcium phosphate (DCPA) [27,28]. The interest of the researchers in calcium phosphates can be explained by their outstanding bioactive properties, especially those of hydroxyapatite (HAp or HA). The stoichiometric ratio of calcium to phosphorus (Ca/P) is 1.67 [29]. Hydroxyapatite is the main component of human bones and teeth. The enamel is composed of 96 wt% inorganic and 4 wt% organic components (such as proteins and lipids) and water, while the mature dentin is composed of 70 wt% inorganic components, 20 wt% organic constituents and 10 wt% water [30]. Hydroxyapatite can also be synthesized [31]. Synthetic hydroxyapatite resembles the natural mineral bone component in chemical composition and crystal structure [32]. HAp is highly biocompatible and bioactive [33,34]. It is non-toxic and non-carcinogenic. It does not induce inflammation in the human body and does not irritate tissues [33,34,35]. Thanks to its excellent osteogenic properties, hydroxyapatite has a wide range of biomedical applications, such as bone scaffolds and bone fillers [36]. In dentistry, hydroxyapatite is used in implantology for implant coating and in maxillofacial surgery as a bone replacement [37]. It has recently been applied in conservative dentistry as an abrasive component of toothpaste and as a component of dental cement [38].
The current literature suggests that the use of calcium phosphates (including hydroxyapatite) in conservative dentistry is not fully satisfactory. Their addition as composite fillers deteriorates the flexural strength of resin materials [10,20,39]. This effect can be explained by low dispersion and insufficient interaction between calcium phosphate-based fillers and the resin [9,19,38]. Research also confirms the relationship between the use of different filler particle sizes and the mechanical properties of dental composites [10,20,39]. Therefore, there was a need to continue the scientific work focused on improving the mechanical properties of dental composites containing hydroxyapatite. For this purpose, the composite was modified by adding calcium fluoride and nanosilver by Mohammad Mahdi Taheri et al. [40]. Their study showed an improvement in the mechanical properties of composites based on bisphenol A-glycol dimethacrylate resin (Bis-GMA) after introducing HAp particles with calcium fluoride as filler [40]. Additionally, the addition of silver nanoparticles could potentially solve the problem of secondary caries.
The currently available research is mainly focused on dental composites based on Bis-GMA, TEGDMA, HEMA resins and resin-modified glass ionomer cement [10,41,42,43] and the use of nanohydroxyapatite [29,41]. In this study, the authors modified a dental composite based on UDMA resin, which is commonly used to restore the hard tissues of a tooth. Hydroxyapatite, calcium fluoride and nanosilver in powder form were used as fillers. Mechanical tests were carried out as an imitation of naturally occurring constant occlusal load and abrasion of human teeth.
The aim of this research was to compare selected mechanical properties, i.e., hardness, static strength (compression, bending), dynamic properties (impact strength, fracture toughness) and wear resistance of several experimental composites with a commercial filler, fluorine, nanosilver and different HAp contents. The null hypothesis is that the use of hydroxyapatite, calcium fluoride and nanosilver as fillers in dental composites does not affect their mechanical properties.
2. Materials and Methods
Two hundred fifty composite specimens were prepared. The specimens were divided into five groups depending on the additive content. The specimens were prepared using a commercial urethane dimethacrylate (UDMA)-based composite material (Gradia Direct, GC, Tokyo, Japan) (n = 50) and a hybrid composite material modified by adding 2 wt% (n = 50) and 5 wt% (n = 50) of hydroxyapatite powder with fluorine (calcium fluoride) and nanosilver. Hydroxyapatite grain size was 30 μm. Nanosilver (Sigma-Aldrich, Saint Louis, MO, USA) was added in the nanopowder form in the amount of 1 wt% (n = 50) with particle size <100 nm. Anhydrous calcium fluoride (Sigma-Aldrich, Saint Louis, MO, USA) with a purity of 99.99% was used in the amount of 0.2 wt% (n = 50). Table 1 shows a description of each group of specimens.

Table 1.
Filler size and content in composite specimens.
The experimental composite was prepared in accordance with ISO standards [44,45,46,47,48,49]. In the first phase, the filler was prepared. Hydroxyapatite was synthesized using the wet method. Subsequently, the HAp grains were dried and fractionated using a LPzE-3e laboratory shaker (MULTISERW-Morek, Brzeźnica, Poland). For this purpose, a set of three sieves was used: 0.1 mm, 0.05 mm and 0.025 mm. Hydroxyapatite powder was then enriched with additional ingredients: nanosilver and calcium fluoride. In the second phase, the filler was integrated into the composite material in a microvial with the aid of a Roti-Speed agitator (Carl Roth GmbH + Co., KG, Karlsruhe, Germany) at a speed of 5000 rpm for approx. 5 min. The process was performed in a darkened room with standard temperature and humidity conditions. To form the specimens, the material, previously stored in polypropylene syringes with a plunger, was placed in a silicone mold between two glass slides. The protection of the material’s surface from oxygen inhibition was thus ensured. Subsequently, the material was polymerized in 1 mm layers with a diode polymerization lamp (Elipar S10 with 1400 mW/cm2 real power and 450–490 nm light emission, 3M ESPE, St. Paul, MS, USA) for 20 s. Figure 1 illustrates the composition of the obtained material containing hydroxyapatite, nanosilver and fluorine fillers.
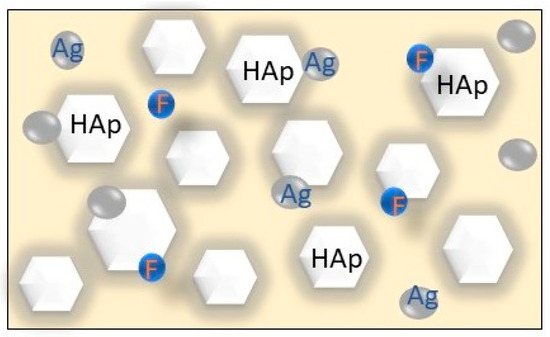
Figure 1.
Illustration of the experimental composite with HAp, Ag and F fillers.
The specimens were artificially aged by incubation in distilled water at 37 °C for 24 h to ensure complete curing. Then, mechanical tests were carried out to determine the mechanical properties of the materials. The research methods are presented in Table 2.

Table 2.
Characteristics of the implemented testing methods.
2.1. Hardness Measurements
Ten cuboid-shaped specimens from each group with dimensions of 5 mm × 10 mm × 20 mm were subjected to hardness tests. A Shore D-type hardness tester (Elcometer Inc., Warren, MI, USA) was used. Five areas on each material specimen were randomly selected for measurements.
2.2. Impact Strength Test
The impact strength tests were carried out with the aid of a HIT 5.5p ZwickRoeler hammer drill (Zwick/Roell, Ulm, Germany) with a hammer energy of 5.5 J. Ten cuboid-shaped composite specimens from each group with dimensions of 5 mm × 10 mm × 20 mm were used.
2.3. Bending Strength Test
The bending strength tests were performed on a multifunctional UMT TriboLab device (Bruker, Karlsruhe, Germany). The applied traverse shift speed was equal to 0.5 mm/min, with a maintained support spacing of 20 mm. The supports and the mandrel performing the input function had radii of 1 mm. For these tests, ten specimens from each group, in the shape of rectangular beams with the dimensions of 2 mm × 2 mm × 25 mm, were prepared.
2.4. Compression Strength Test
Ten cylindrical specimens from each group (4 mm in diameter and 6 mm in height) were subjected to compression strength tests. They were carried out on a Walter + Bai machine (Walter + Bai AG, Lohningen, Switzerland).
2.5. Tribological Wear Resistance Test
The wear resistance was tested on ten cylindrical specimens from each group. They were 2 mm high and had a diameter of 21 mm. The tests were carried out using a Tribometer device (CSM Instruments, Freiburg, Germany) with the Tribox 2.5 software and the following parameters: friction radius 6.75 mm, speed 0.05 m/s, load 1 N and friction distance 100 m. The artificial saliva environment was applied to perform the test (according to Fusayama/Meyer: 2 dm3 distilled water, 0.8 g NaCl, 0.8 g KCl, 1.59 g CaCl2·2H2O, 1.56 g NaH2PO4·2H2O, 0.01 g Na2S·9H2O, and 2 g of urea) [50] and temperature of 25 °C. The specimens were placed in a designated teflon holder with artificial saliva. The friction counterexample was a zirconium oxide ball with a diameter of 1/8 inch. The wear of the material was determined by measuring linear wear traces in the friction area based on surface roughness measurement, which was performed using a Hommel Waveline 200 profilometer (ITA, Skórzewo, Poland). The tested composite’s tribological wear was calculated as the volumetric loss of material relative to the friction area [51].
The results were statistically analyzed using IBM SPSS Statistics, version 29 (IBM Corp., Armonk, NY, USA). The Shapiro–Wilk test of normality (p < 0.05) was used to verify the normality of variables. Because of a negative outcome, non-parametric Kruskall-Wallis tests followed by multiple comparisons (with Bonferroni correction) were used to compare the type of specimens within the variables. The significance level was set at 5% (α = 0.05).
3. Results
3.1. Hardness Measurements
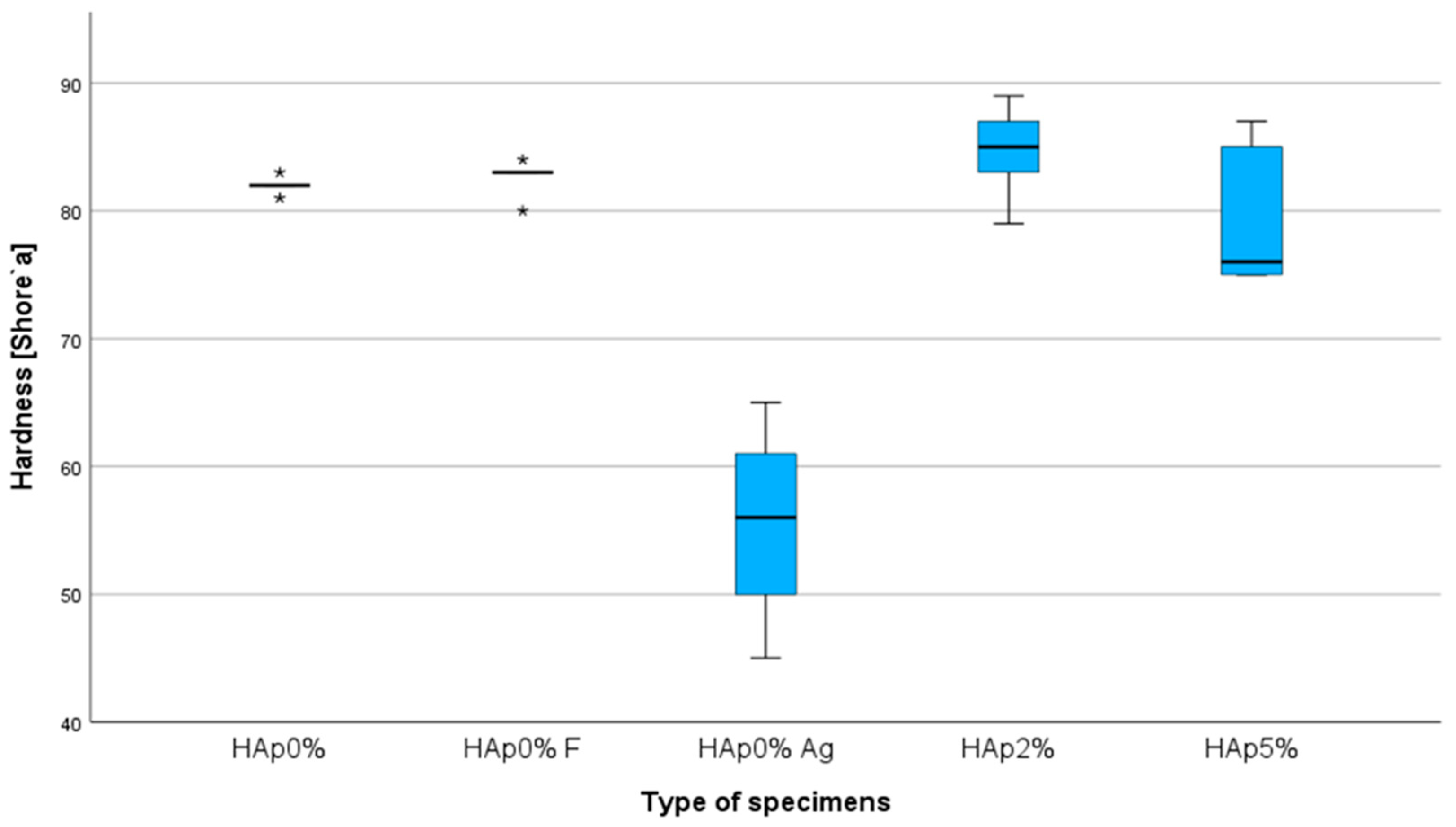
The significant value for composite materials is hardness, which determines the material’s ability to resist deformation. Conducting this test allows us to determine the mechanical properties of the obtained composites. The results of hardness measurements are presented as an average, shown in the chart below (Figure 2).
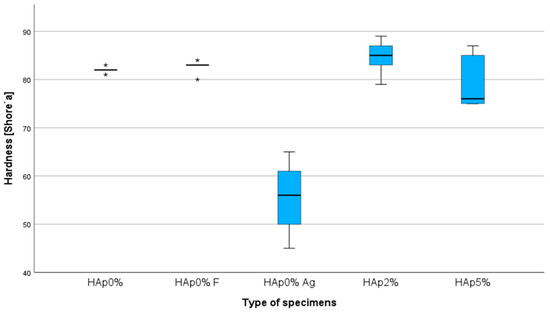
Figure 2.
Composite hardness chart (* represents outliers).
The hardness measurement conducted for composites containing fluorine and fluorine with hydroxyapatite shows that their hardness (85 ShD) increased compared to the commercial composite (82 ShD). The highest hardness values were achieved by the composite with fluorine and hydroxyapatite than by the composite with calcium fluoride alone.
The Kruskal–Wallis test indicated significant differences in the hardness [Shore] (p = 0.008). The null hypothesis of the same distribution of the groups was rejected. Differences were statistically significant (adjusted significance) in multiple comparisons between Hap 0%Ag and Hap 0%F (p = 0.044). Differences were statistically significant (adjusted significance) in multiple comparisons between Hap 0%Ag and Hap 2% (p = 0.005).
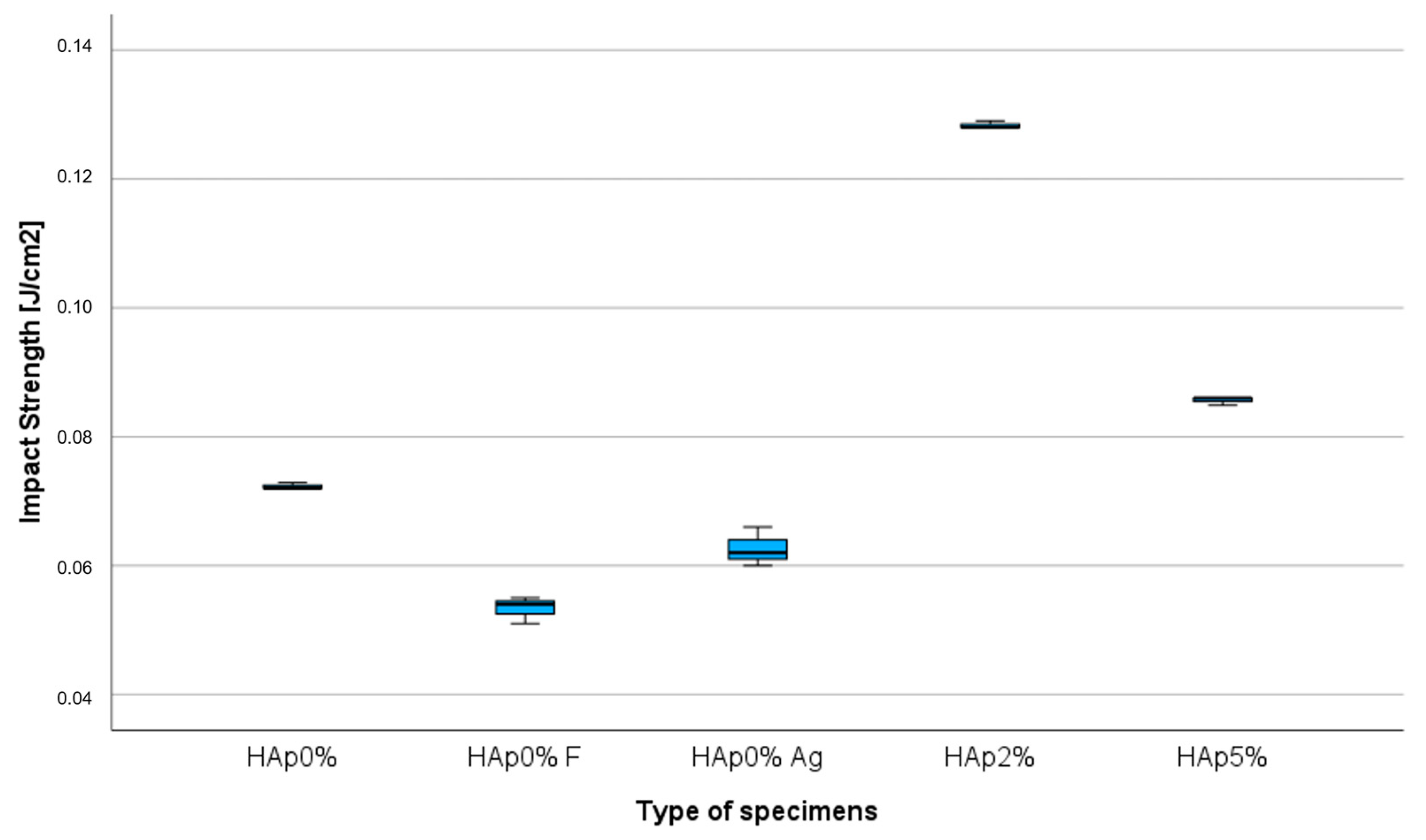
3.2. Impact Strength Test
Impact strength test results indicate the influence of the addition of hydroxyapatite, nanosilver and calcium fluoride (Figure 3).
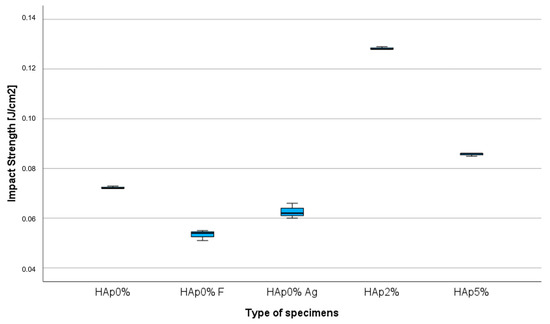
Figure 3.
Impact strength chart.
The composite containing 2 wt% hydroxyapatite with fluorine and nanosilver achieved the highest impact strength value (0.128 J/cm2) compared to the commercial composite (0.072 J/cm2).
The Kruskal–Wallis test revealed significant differences in the impact strength [J/cm2] (p = 0.009). The null hypothesis of the same distribution of the groups was rejected. Differences were statistically significant (adjusted significance) in multiple comparisons between HAp 0% and HAp 2% (p = 0.010).
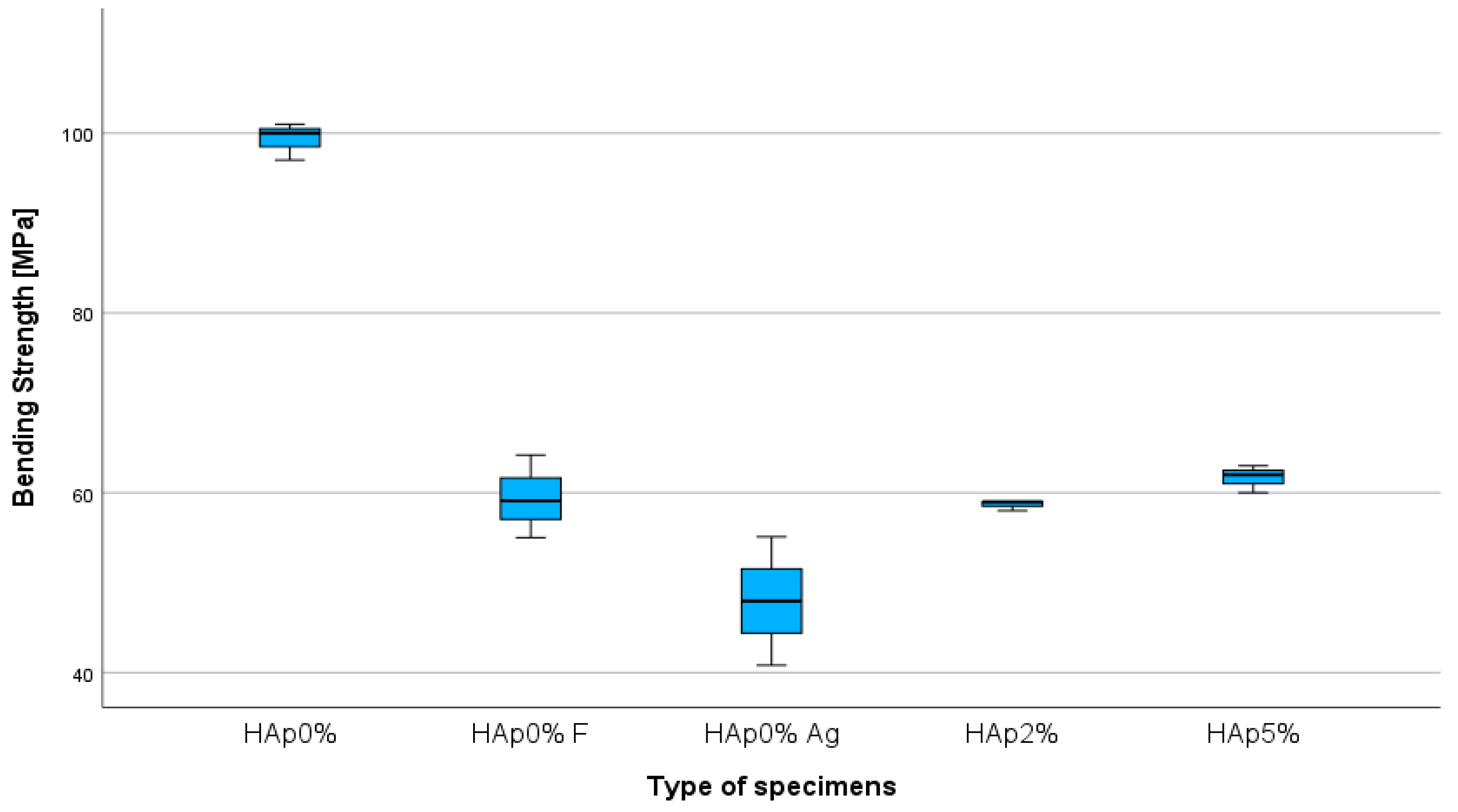
3.3. Bending Strength Test
Figure 4 shows the results of the bending strength test. It was observed that the added fillers (hydroxyapatite, nanosilver and calcium fluoride) affected the strength of the tested materials. The experimental composites showed lower values of bending strength in comparison to the commercial composite.
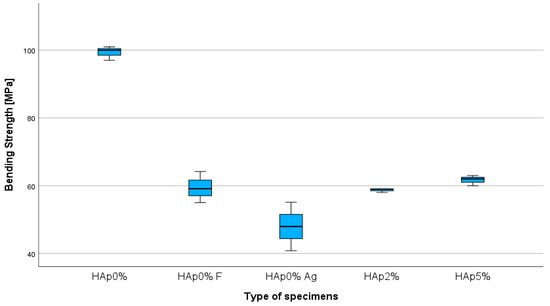
Figure 4.
Bending strength chart.
The Kruskal–Wallis test revealed significant differences in the bending strength [MPa] (p = 0.022). The null hypothesis of the same distribution of the groups was rejected. Differences were statistically significant (adjusted significance) in multiple comparisons between HAp 0% and HAp 0% Ag (p = 0.014).
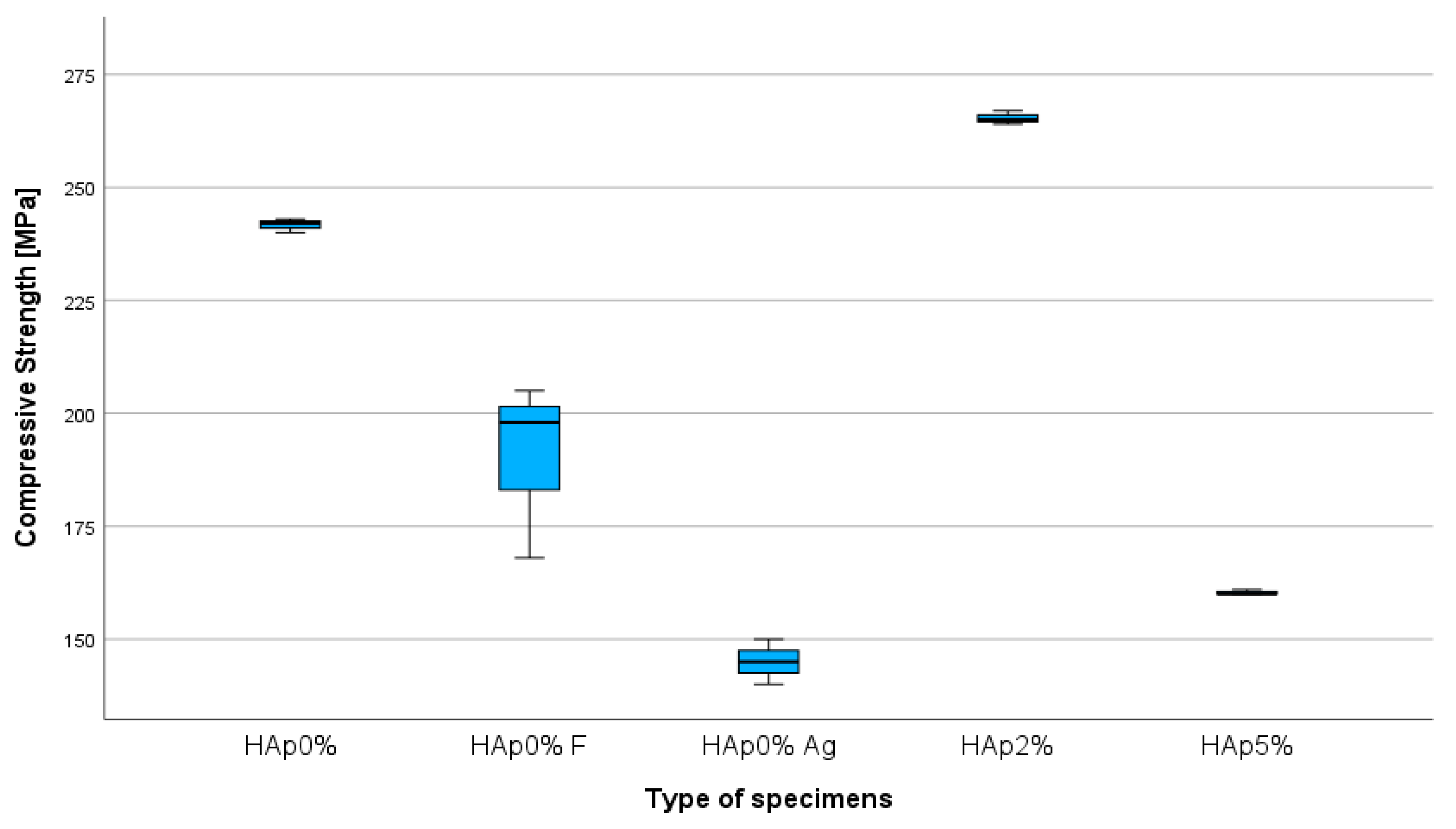
3.4. Compression Strength Test
The obtained results (Figure 5) indicate that the highest compressive strength (264 MPa) among the modified composites was achieved by the hybrid composite with 2 wt% hydroxyapatite, fluorine and nanosilver. It was higher than the compression strength of a commercial hybrid composite (242 MPa). The addition of nanosilver alone reduced the strength of the composite.
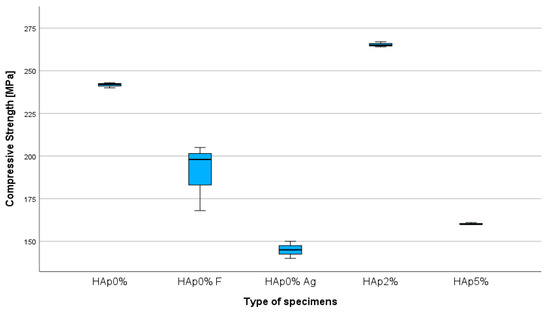
Figure 5.
Compression strength chart.
The Kruskal–Wallis test revealed significant differences in the compression strength [MPa] (p = 0.009). The null hypothesis of the same distribution of the groups was rejected. Differences were statistically significant (adjusted significance) in multiple comparisons between HAp 0% Ag and HAp 2% (p = 0.01).
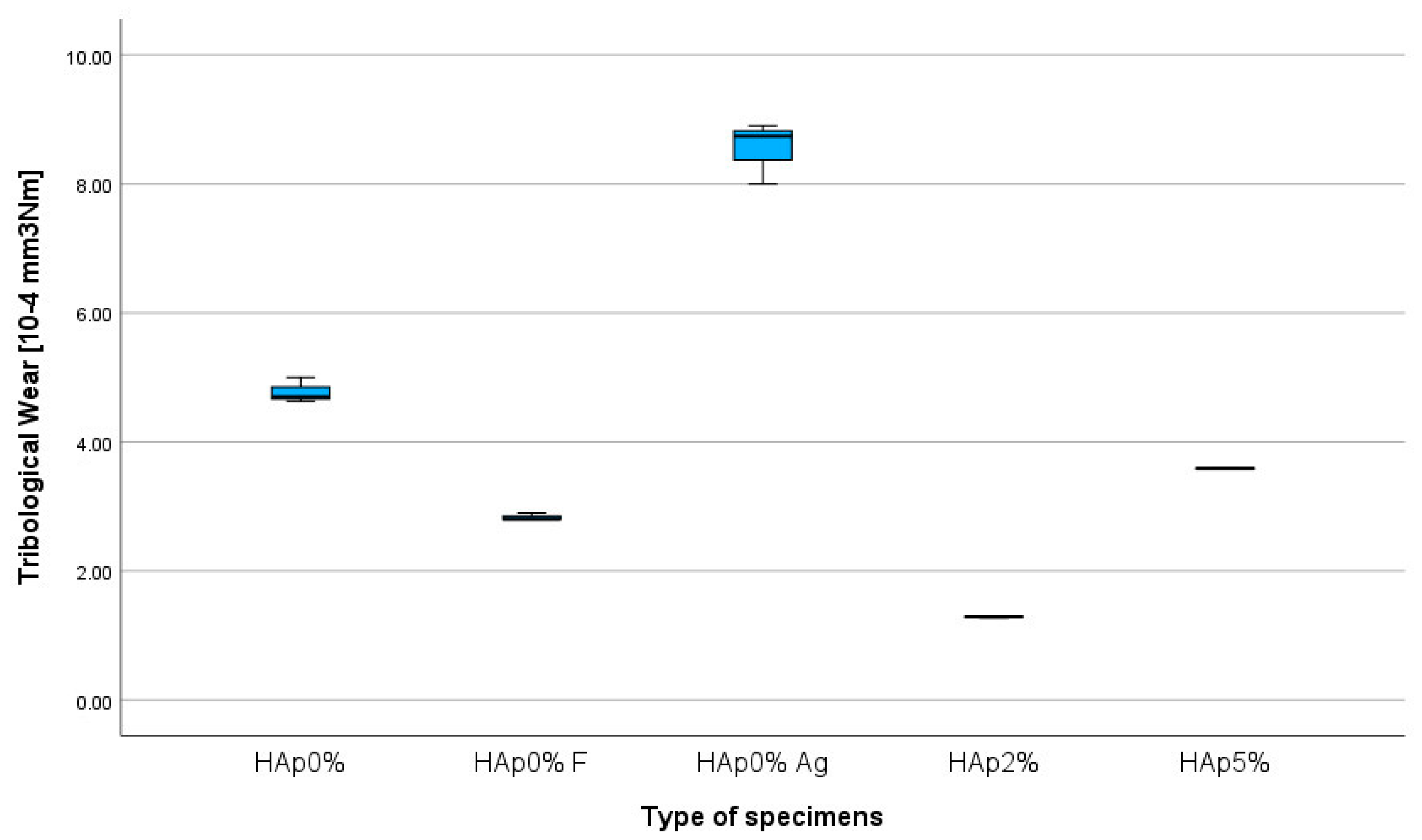
3.5. Tribological Wear Resistance Test
As mentioned in the research methodology, the tests were conducted in conditions similar to those present in the oral cavity, i.e., in artificial saliva. Figure 6 shows the wear test results for all tested composites. The results indicate the highest wear degree (8.56−4 mm3/Nm) for the composite with the addition of nanosilver. The lowest wear value (1.29−4 mm3/Nm) was recorded for the composite containing 2 wt% hydroxyapatite, calcium fluoride and nanosilver compared to the commercial composite, which has a wear degree of 4.77−4 mm3/Nm.
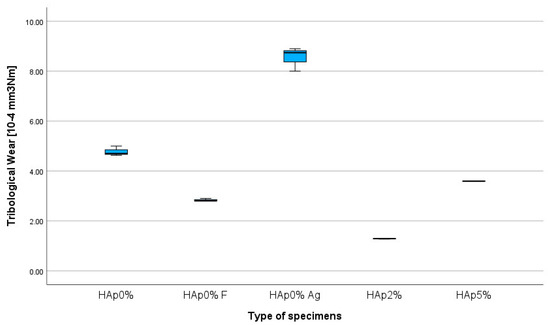
Figure 6.
Tribological wear chart.
The Kruskal–Wallis test revealed significant differences in the tribological wear [10−4 mm3/Nm] (p = 0.009). The null hypothesis of the same distribution of the groups was rejected. Differences were statistically significant (adjusted significance) in multiple comparisons between HAp 0% and HAp2% (p = 0.010).
4. Discussion
The null hypothesis of the study was rejected, as the addition of hydroxyapatite, calcium fluoride and nanosilver as fillers in dental composites affects their mechanical properties in all tested cases. The differences were statistically significant.
4.1. Hardness Measurements
Hardness is an important feature of dental materials because it determines their resistance to deformation. It is difficult to directly relate it to other mechanical properties, but it is often used in comparative research. The hardness measurement for composites containing fluorine and hydroxyapatite fillers shows that their addition improves material hardness (85 ShD). This improvement in mechanical properties is confirmed by the literature [40,52]. It can be explained by the strengthening of hydroxyapatite by fluorine ions. The ability to exchange ions is characteristic of hydroxyapatite. It reacts particularly strongly with fluorine. Fluorapatite is formed by replacing hydroxide ions with fluorine ions in HAp. Fluoroapatites are characterized by better crystallinity hardness and are much less soluble. They are more resistant to chemical and physical damage [53,54]. Thus, the highest hardness values are achieved by the composite with fluorine and hydroxyapatite filler than by the composite with calcium fluoride alone.
4.2. Impact Strength Test
It was demonstrated that the impact strength of the tested composites varies depending on their composition. The addition of nanosilver and calcium fluoride causes a decrease in the impact strength of the material proportional to an increase in the HAp content.
4.3. Bending Strength Test
Composite fillings are regularly exposed to bending forces. Therefore, a three-point bending test was performed. The ISO 4049 standard “Dentistry-polymer-based restorative materials 2009” [44] for polymer-based fillers restoring hard tissues of the tooth determines their required bending strength of 50 MPa. This value was exceeded by all tested modified composites, except the composite containing the addition of nanosilver.
4.4. Compression Strength Test
In order to restore hard tooth tissues with composites, it is necessary to analyze the forces acting on the teeth and restorations. In the oral cavity, the occlusal forces occur. They are most pronounced in the posterior section, on the molar teeth. The compression strength test showed that the hybrid composite with 2 wt% HAp, F and Ag achieved the highest strength (264 MPa) among the modified composites. This value is higher even when compared to a commercial hybrid composite. The literature indicates that the compressive strength of dentin is approximately 250–350 MPa [55,56], which is very similar to the one measured in the obtained composite material. The occlusal forces within the incisors are approximately 100–150 N [10,57]. This means that the tested material can be successfully used to restore molar teeth. Occlusal forces vary depending on the anatomical location, age, and dental restoration location. In order to properly rebuild the hard tissues of the tooth, the type of material used and the condition of the patient’s teeth should be taken into account.
4.5. Tribological Wear Resistance Test
Wear resistance is very important when it comes to dental restorations. It may determine the durability of the tooth filling. Friction and wear occur during the mastication process. They intensify when chewing hard foods. Studies described in the literature confirm that high friction values are associated with faster wear of the filling [12,58].
It was proven that the type of filler used affects the abrasive wear of dental composites. The lowest value of the wear factor (1.29−4 mm3/Nm) was recorded for the composite containing 2 wt% hydroxyapatite, calcium fluoride and nanosilver, compared to the commercial composite, which has a wear factor of 4.77−4 mm3/Nm. The literature indicates that the morphology and particle size of the added filler also significantly affect the tribological and mechanical properties of composites [7,8,59]. It should be noticed that the composite containing only nanosilver filler achieved the highest wear factor (8.56−4 mm3/Nm). The deterioration of tribological properties may be related to an incorrect polymerization process caused by the addition of silver. This suggests that its concentration and interaction with other fillers should be closely examined and enhanced to avoid compromising this critical property of dental composites.
Bearing in mind the results and limitations of this study, further research is needed to explore effective ways to enhance the properties deteriorated by the addition of the tested fillers or to present alternative fillers for dental composites. The optimization of the mixing process or filler surface treatment could also improve the compatibility and performance of proposed composites. Since it is a pilot ex vivo study, an extended in vivo study could be useful to assess the long-term functionality or color stability of the experimental materials. In addition, similar studies could be carried out, including a wider range of resin matrices, such as Bis-GMA or TEGDMA.
5. Conclusions
Based on the conducted research, it is concluded that the addition of hydroxyapatite along with calcium fluoride and nanosilver as fillers significantly affects the mechanical properties of dental composite. The best mechanical properties among all tested composites were achieved with the experimental composite containing 2 wt%. of hydroxyapatite with calcium fluoride and nanosilver. However, further research is needed to improve the tested properties of experimental composites and explore alternative solutions.
Author Contributions
Conceptualization, Z.K. and L.K.; methodology, Z.K. and L.K.; software, J.C.R.; validation K.D. and Z.K.; formal analysis, C.B.N.; investigation, K.D.; resources, Z.K. and J.C.R.; data curation, C.B.N.; writing—original draft preparation, Z.K.; writing—review and editing, K.D.; visualization, K.D.; supervision, Z.K. and L.K.; project administration, K.D. and Z.K.; funding acquisition, Z.K. and L.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- Xu, Y.; You, Y.; Yi, L.; Wu, X.; Zhao, Y.; Yu, J.; Liu, H.; Shen, Y.; Guo, J.; Huang, C. Dental plaque-inspired versatile nanosystem for caries prevention and tooth restoration. Bioact. Mater. 2023, 20, 418–433. [Google Scholar] [CrossRef] [PubMed]
- Kassebaum, N.J.; Smith, A.G.C.; Bernabé, E.; Fleming, T.D.; Reynolds, A.E.; Vos, T.; Murray, C.J.L.; Marcenes, W. Global, regional, and national prevalence, incidence, and disability-adjusted life years for oral conditions for 195 countries, 1990-2015: A systematic analysis for the global burden of diseases, injuries, and risk factors. J. Dent. Res. 2017, 96, 380–387. [Google Scholar] [CrossRef]
- Bowen, W.H.; Burne, R.A.; Wu, H.; Koo, H. Oral biofilms: Pathogens, matrix, and polymicrobial interactions in microenvironments. Trends Microbiol. 2018, 26, 229–242. [Google Scholar] [CrossRef]
- Kreth, J.; Merritt, J.; Qi, F. Bacterial and host interactions of oral streptococci. DNA Cell Biol. 2009, 28, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Paolone, G.; Scolavino, S.; Gherlone, E.; Spagnuolo, G. Direct Esthetic Composite Restorations in Anterior Teeth: Managing Symmetry Strategies. Symmetry 2021, 13, 797. [Google Scholar] [CrossRef]
- Aminoroaya, A.; Esmaeely, N.R.; Nouri, K.S.; Panahi, P.; Das, O.; Ramakrishna, S. A Review of Dental Composites: Methods of Characterizations. ACS Biomater. Sci. Eng. 2020, 13, 3713–3744. [Google Scholar] [CrossRef]
- Yadav, R.; Lee, H.; Lee, J.H.; Singh, J.K.; Lee, H.H. A comprehensive review: Physical, mechanical, and tribological characterization of dental resin composite materials. Tribol. Int. 2023, 179, 108102. [Google Scholar] [CrossRef]
- Wang, X.; Cai, Q.; Zhang, X.; Wei, Y.; Xu, M.; Yang, X.; Ma, Q.; Cheng, Y.; Deng, X. Improved performance of Bis-GMA/TEGDMA dental composites by net-like structures formed from SiO2 nanofiber fillers. Mater. Sci. Eng. 2016, 59, 464–470. [Google Scholar] [CrossRef]
- Tian, M.; Gao, Y.; Liu, Y.; Liao, Y.; Hedin, N.E.; Fong, H. Fabrication and evaluation of Bis-GMA/TEGDMA dental resins/composites containing nano fibrillar silicate. Dent. Mater. 2008, 24, 235–243. [Google Scholar] [CrossRef] [PubMed]
- De Santis, R.; Gloria, A.; Maietta, S.; Martorelli, M.; De Luca, A.; Spagnuolo, G.; Riccitiello, F.; Rengo, S. Mechanical and Thermal Properties of Dental Composites Cured with CAD/CAM Assisted Solid-State Laser. Materials 2018, 11, 504. [Google Scholar] [CrossRef]
- Rüttermann, S.; Dluzhevskaya, I.; Großsteinbeck, C.; Raab, W.H.M.; Janda, R. Impact of replacing Bis-GMA and TEGDMA by other commercially available monomers on the properties of resin-based composites. Dent. Mater. 2010, 26, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Domingo, C.; Arcís, R.W.; Osorio, E.; Osorio, R.; Fanovich, M.A.; Rodríguez-Clemente, R.; Toledano, M. Hydrolytic stability of experimental hydroxyapatite-filled dental composite materials. Dent. Mater. 2003, 19, 478–486. [Google Scholar] [CrossRef] [PubMed]
- Mirică, I.-C.; Furtos, G.; Bâldea, B.; Lucaciu, O.; Ilea, A.; Moldovan, M.; Câmpian, R.-S. Influence of Filler Loading on the Mechanical Properties of Flowable Resin Composites. Materials 2020, 13, 1477. [Google Scholar] [CrossRef] [PubMed]
- Randolph, L.D.; Palin, W.M.; Leloup, G.; Leprince, J.G. Filler characteristics of modern dental resin composites and their influence on physico-mechanical properties. Dent. Mater. 2016, 12, 1586–1599. [Google Scholar] [CrossRef] [PubMed]
- Szalewski, L.; Wójcik, D.; Bogucki, M.; Szkutnik, J.; Różyło-Kalinowska, I. The Influence of Popular Beverages on Mechanical Properties of Composite Resins. Materials 2021, 14, 3097. [Google Scholar] [CrossRef] [PubMed]
- Gornig, D.C.; Maletz, R.; Ottl, P. Influence of artificial aging: Mechanical and physicochemical properties of dental composites under static and dynamic compression. Clin. Oral Investig. 2022, 26, 1491–1504. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Sun, Y.; Xie, W.; Liu, Y.; Song, X. Development of novel dental nanocomposites reinforced with polyhedral oligomeric silsesquioxane (POSS). Dent. Mater. 2010, 26, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Santos, C.; Luklinska, Z.B.; Clarke, R.L.; Davy, K.W. Hydroxyapatite as a filler for dental composite materials: Mechanical pro-perties and in vitro bioactivity of composites. J. Mater. Sci. Mater. Med. 2001, 12, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Kula, Z.; Klimek, L.; Kopacz, K.; Śmielak, B. Evaluation of the Effect of the Addition of Hydroxyapatite on Selected Mechanical and Tribological Properties of a Flow-Type Composite. Materials 2022, 15, 9016. [Google Scholar] [CrossRef]
- Klimek, L.; Kopacz, K.; Śmielak, B.; Kula, Z. An Evaluation of the Mechanical Properties of a Hybrid Composite Containing Hydroxyapatite. Materials 2023, 16, 4548. [Google Scholar] [CrossRef]
- Nunes Jardim, R.; Araújo Rocha, A.; Malta Rossi, A.; Neves, A.A.; Barbosa Portela, M.; Tadeu Lopes, R.; Pires dos Santos, T.M.; Xing, Y.; Moreira da Silva, E. Fabrication and characterization of remineralizing dental composites containing hydroxyapatite nanoparticles. J. Mech. Behav. Biomed. Mater. 2020, 109, 103817. [Google Scholar] [CrossRef] [PubMed]
- Antonucci, J.M.; Skrtic, D. Fine-Tuning of Polymeric Resins and their Interfaces with Amorphous Calcium Phosphate. A Strategy for Designing Effective Remineralizing Dental Composites. Polymers 2010, 2, 378–392. [Google Scholar] [CrossRef]
- Skrtic, D.; Antonucci, J.M.; Liu, D.W. Ethoxylated bisphenol dimethacrylate-based amorphous calcium phosphate composites. Acta Biomater. 2006, 2, 85–94. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, J.N.R.; Schumacher, G.E.; Antonucci, J.M.; Skrtic, D. Structure-Composition-Property Relationships in Polymeric Amorphous Calcium Phosphate-Based Dental Composites. Materials 2009, 2, 1929–1954. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, F.E.Z.F.; Elsayed, M.A.; Elshiekh, M.A. In vitro–assessment of Remineralization and Microleakage of Tetra Calcium Phosphate Composite Versus Glass Ionomer Restorative Materials. Res. Sq. 2023. preprint v.1. [Google Scholar] [CrossRef]
- Elwan, R.L.; Hamzawy, E.M.A.; El-Hamid, H.K.A. Characterization, bioactivity, antibacterial and cytotoxicity of inexpensive soda-lime-silica glass/tetracalcium phosphate composites. Ceram. Int. 2024, 50, 11190–11198. [Google Scholar] [CrossRef]
- Tanaka, C.B.; Lopes, D.P.; Kikuchi, L.T.; Moreira, M.S.; Catalani, L.H.; Braga, R.R.; Kruzic, J.J.; Gonçalves, F. Development of novel dental restorative composites with dibasic calcium phosphate loaded chitosan fillers. Dent. Mater. 2020, 36, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Trinca, R.B.; Oliveira, B.A.; Vilela, H.S.; Braga, R.R. Effect of calcium orthophosphate particle size and CaP:glass ratio on optical, mechanical and physicochemical characteristics of experimental composites. Dent. Mater. 2023, 9, 770–778. [Google Scholar] [CrossRef] [PubMed]
- Balhuc, S.; Campian, R.; Labunet, A.; Negucioiu, M.; Buduru, S.; Kui, A. Dental Applications of Systems Based on Hydroxyapatite Nanoparticles—An Evidence-Based Update. Crystals 2021, 11, 674. [Google Scholar] [CrossRef]
- De Dios Teruel, J.; Alcolea, A.; Hernández, A.; Ruiz, A.J.O. Comparison of chemical composition of enamel and dentine in human, bovine, porcine and ovine teeth. Arch. Oral. Biol. 2015, 60, 768–775. [Google Scholar] [CrossRef]
- Sans, J.; Sanz, V.; Puiggalí, J.; Turon, P.; Alemán, C. Controlled Anisotropic Growth of Hydroxyapatite by Additive-Free Hydrothermal Synthesis. Cryst. Growth Des. 2020, 2, 748–756. [Google Scholar] [CrossRef]
- Kuśnieruk, S.; Wojnarowicz, J.; Chodara, A.; Chudoba, T.; Gierlotka, S.; Lojkowski, W. Influence of hydrothermal synthesis parameters on the properties of hydroxyapatite nanoparticles. Beilstein. J. Nanotechnol. 2016, 7, 1586–1601. [Google Scholar] [CrossRef] [PubMed]
- Bordea, I.; Candrea, S.; Alexescu, G.; Bran, S.; Baciut, M.; Baciut, G.; Lacaciu, O.; Dinu, C.; Todea, D. Nano-hydroxyapatite use in dentistry: A systematic review. Drug Metab. Rev. 2020, 52, 319–332. [Google Scholar] [CrossRef] [PubMed]
- Dorozhkin, S.V. Calcium orthophosphates in dentistry. Sci. Mater. Med. 2013, 24, 1335–1363. [Google Scholar] [CrossRef] [PubMed]
- Szcześ, A.; Hołysz, L.; Chibowski, E. Synthesis of hydroxyapatite for biomedical applications. Adv. Colloid Interface Sci. 2017, 249, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Ghiasi, B.; Sefidbakht, Y.; Mozaffari-Jovin, S.; Gharehcheloo, B.; Mehrarya, M.; Khodadadi, A.; Rezaei, M.; Ranaei Siadat, S.O.; Uskoković, V. Hydroxyapatite as a biomaterial–A gift that keeps on giving. Drug Dev. Ind. Pharm. 2020, 46, 1035–1062. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Zhou, Z.; Li, W.; Fan, Y.; Li, Z.; Wei, J. Hydroxyapatite based materials for bone tissue engineering: A brief and comprehensive introduction. Crystals 2021, 11, 149. [Google Scholar] [CrossRef]
- Pajor, K.; Pajchel, L.; Kolmas, J. Hydroxyapatite and Fluorapatite in Conservative Dentistry and Oral Implantology—A Review. Materials 2019, 12, 2683. [Google Scholar] [CrossRef] [PubMed]
- Arcís, R.W.; López-Macipe, A.; Toledano, M.; Osorio, E.; Rodríguez-Clemente, R.; Murtra, J.; Fanovich, M.A.; Pascual, D. Mechanical properties of visible light-cured resins reinforced with hydroxyapatite for dental restoration. Dent. Mater. 2002, 18, 49–57. [Google Scholar] [CrossRef]
- Taheri, M.M. Fluoridated hydroxyapatite nanorods as novel fillers for improving mechanical properties of dental composite: Synthesis and application. Mater. Desing 2015, 82, 119–125. [Google Scholar] [CrossRef]
- Pagano, S.; Chieruzzi, M.; Balloni, S.; Lombardo, G.; Torre, L.; Bodo, M.; Cianetti, S.; Marinucci, L. Biological, thermal and mechanical characterization of modified glass ionomer cements: The role of nanohydroxyapatite, ciprofloxacin and zinc l-carnosine. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 94, 76–85. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhang, D.; Wan, Z.; Yang, X.; Cai, Q. Dental resin composites with improved antibacterial and mineralization properties via incorporating zinc/strontium-doped hydroxyapatite as functional fillers. Biomed. Mater. 2022, 17, 045002. [Google Scholar] [CrossRef] [PubMed]
- Alatawi, R.A.S.; Elsayed, N.H.; Mohamed, W.S. Influence of hydroxyapatite nanoparticles on the properties of glass ionomer cement. J. Mater. Res. Technol. 2019, 8, 344–349. [Google Scholar] [CrossRef]
- EN ISO 4049; Dentistry–Polymer-Based Restorative Materials. ISO: Geneva, Switzerland, 2009.
- ASTM G133-05; Standard Test Method for Linearly Reciprocating Ball-on-Flat Sliding Wear. ISO: Geneva, Switzerland, 2010.
- PN-EN ISO 868; Plastics and Ebonite—Determination of Indentation Hardness by Means of a Durometer (Shore Hardness). ISO: Geneva, Switzerland, 2003.
- PN-EN ISO 604; Plastics—Determination of Compressive Properties 2002. ISO: Geneva, Switzerland, 2002.
- PN-EN ISO 179-2:2020-12; Plastics—Determination of Charpy Impact Properties. ISO: Geneva, Switzerland, 2020.
- ASTM D2240; Standard Test Method for Rubber Property—Durometer Hardness. ISO: Geneva, Switzerland, 2017.
- Banaszek, K.; Klimek, L. Ti(C, N) as Barrier. Coatings 2019, 9, 432. [Google Scholar] [CrossRef]
- Dziedzic, K.; Zubrzycka-Wróbel, J. Research on tribological properties of dental composite materials. Adv. Sci. Technol. Res. J. 2016, 10, 144–149. [Google Scholar] [CrossRef] [PubMed]
- Kutbay, I.; Yilmaz, B.; Evis, Z.; Usta, M. Effect of calcium fluoride on mechanical behavior and sinterability of nano-hydroxyapatite and titania composites. Ceram. Int. 2014, 40, 14817–14826. [Google Scholar] [CrossRef]
- Tredwin, C.H.J.; Young, A.M.; Neel, E.A.A. Hydroxyapatite, fluor-hydroxyapatite and fluorapatite produced via the sol–gel method: Dissolution behaviour and biological properties after crystallization. J. Mater. Sci. Mater. Med. 2014, 25, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Neves, C.B.; Costa, J.; Nepomuceno, L.; Madeira, A.; Portugal, J.; Bettencourt, A. Microhardness and Flexural Strength after Chemical Aging of chlorhexidine delivery systems based on acrylic resin. Rev. Port. Estomatol. Med. Dent. Cir. Maxilofac. 2019, 60, 104–110. [Google Scholar] [CrossRef]
- Zaytsev, D. Correction of some mechanical characteristics of human dentin under compression considering the shape effect. Mater. Sci. Eng. 2015, 49, 101–105. [Google Scholar] [CrossRef]
- Cappelloni, I.; Montanari, R. Mechanical characterization of human dentin: A critical review. Key Eng. Mater. 2013, 541, 75–96. [Google Scholar] [CrossRef]
- Chadda, H.; Satapathy, B.K.; Patnaik, A.; Ray, A.R. Mechanistic interpretations of fracture toughness and correlations to wear behavior of hydroxyapatite and silica/hydroxyapatite filled bis-GMA/TEGDMA micro/hybrid dental restorative composites. Compos. Part B Eng. 2017, 130, 132–146. [Google Scholar] [CrossRef]
- Priyadarsini, S.; Mukherjee, S.; Mishra, M. Nanoparticles used in dentistry: A review. J. Oral Biol. Craniofac. Res. 2018, 8, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Sajewicz, E. On evaluation of wear resistance of tooth enamel and dental materials. Wear 2006, 260, 1256–1261. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).