Mechanical Properties of Five Esthetic Ceramic Materials Used for Monolithic Restorations: A Comparative In Vitro Study
Abstract
:1. Introduction
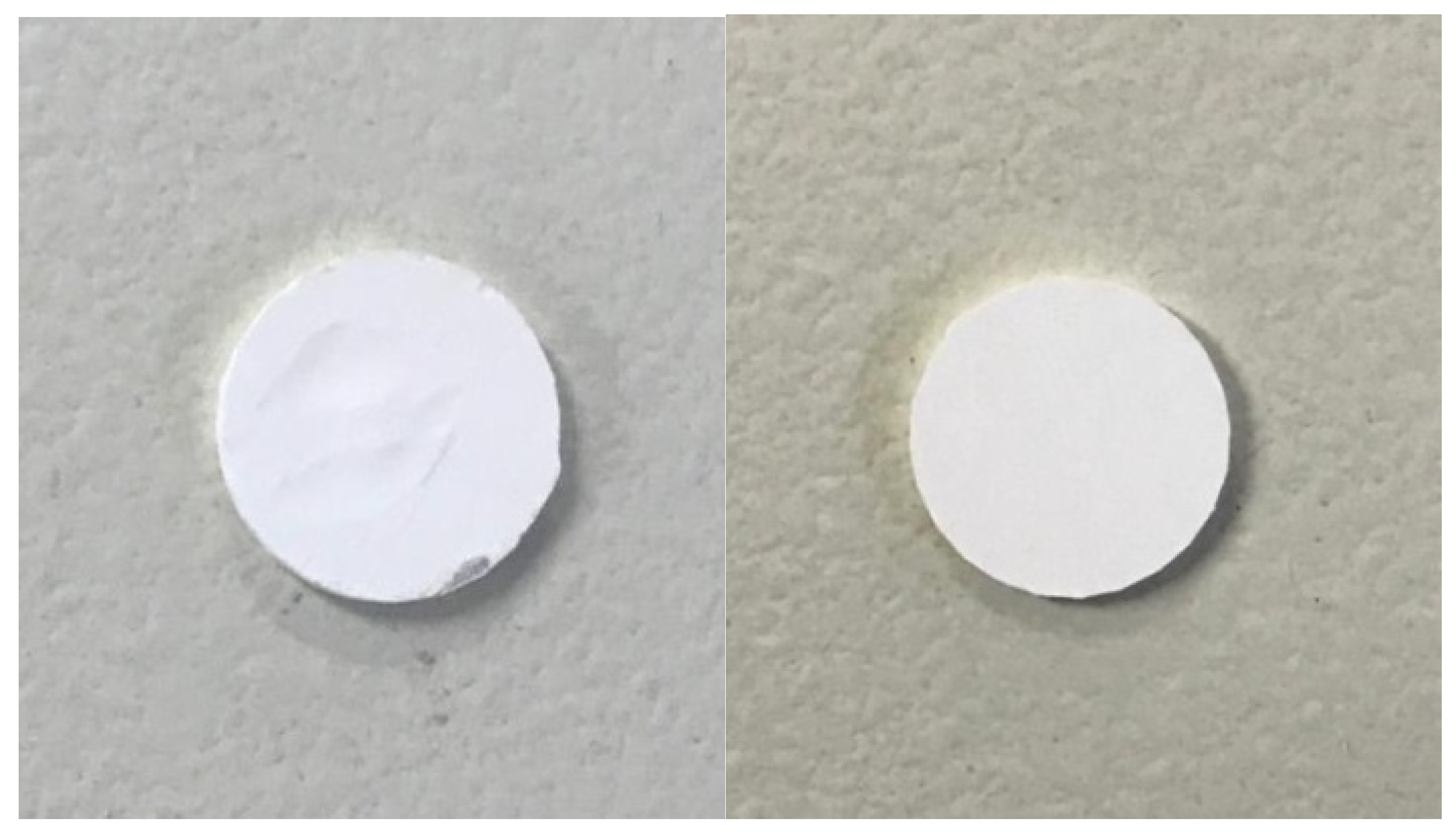
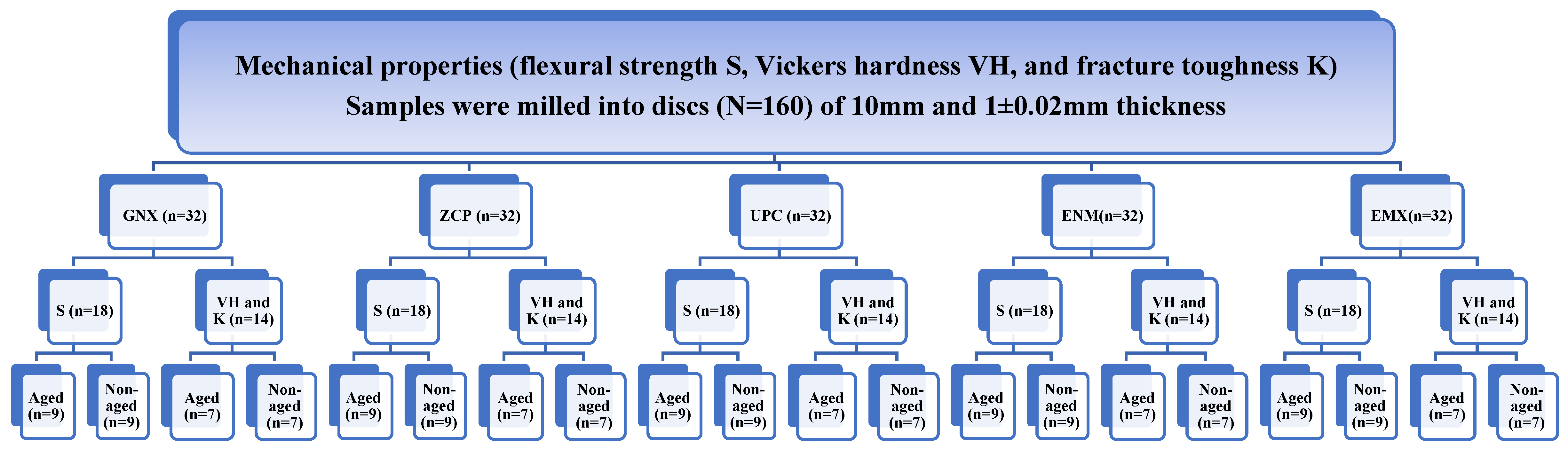
2. Materials and Methods
2.1. Aging Procedure
2.2. Biaxial Flexure Test (S)
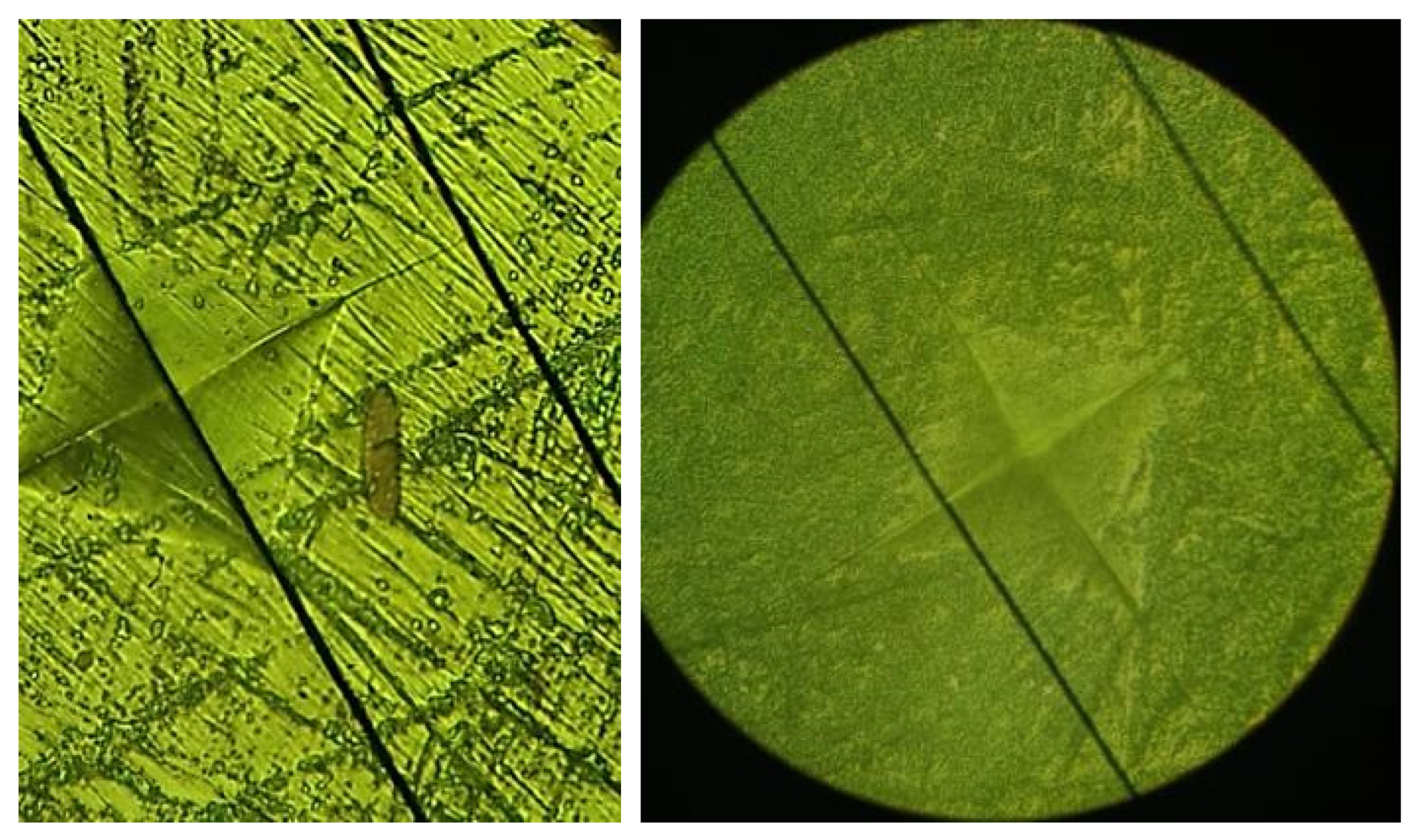
2.3. Vickers Hardness (VH)
2.4. Fracture Toughness
| Material | Elastic Moduli | Poisson’s Ratio |
|---|---|---|
| Polymer-infiltrated ceramic network | 30 GPa | 0.28 |
| Lithium disilicate | 95 GPa | 0.25 |
| Yttria-stabilized zirconia | 200 GPa | 0.31 |

2.5. Brittleness Index
2.6. Statistical Analysis
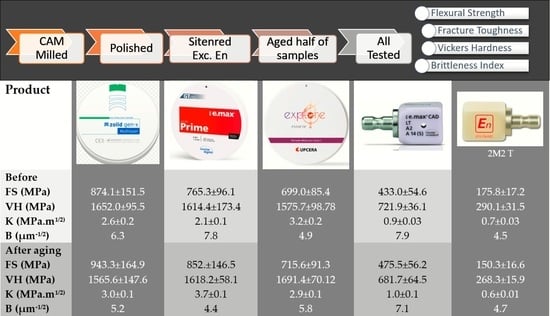
3. Results
4. Discussion
4.1. Biaxial Flexural Strength (S)
4.2. Hardness Evaluation
4.3. Fracture Toughness Evaluation (K)
4.4. Brittleness Evaluation
4.5. Limitations and Consideration for Further Studies
5. Conclusions
- At baseline, monolithic zirconia showed higher mechanical properties (flexural strength, hardness, and fracture toughness) compared with lithium disilicate, while hybrid ceramic ENM showed the lowest mechanical properties. However, all materials meet clinically accepted values for their indications.
- Monolithic zirconia groups showed a lower brittleness index compared with lithium disilicate, while hybrid ceramic ENM showed the lowest brittleness index. Consequently, ENM monolithic zirconia may have better machinability.
- All groups showed, to some extent, changes in mechanical properties (flexural strength, hardness, fracture toughness, and brittleness) with aging which was within the clinical acceptability range.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alqutaibi, A.Y.; Ghulam, O.; Krsoum, M.; Binmahmoud, S.; Taher, H.; Elmalky, W.; Zafar, M.S. Revolution of Current Dental Zirconia: A Comprehensive Review. Molecules 2022, 27, 1699. [Google Scholar] [CrossRef] [PubMed]
- Li, R.W.; Chow, T.W.; Matinlinna, J.P. Ceramic dental biomaterials and CAD/CAM technology: State of the art. J. Prosthodont. Res. 2014, 58, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Spitznagel, F.A.; Balmer, M.; Wiedemeier, D.B.; Jung, R.E.; Gierthmuehlen, P.C. Clinical outcomes of all-ceramic single crowns and fixed dental prostheses supported by ceramic implants: A systematic review and meta-analyses. Clin. Oral Implants Res. 2022, 33, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Kulyk, V.; Duriagina, Z.; Kostryzhev, A.; Vasyliv, B.; Vavrukh, V.; Marenych, O. The Effect of Yttria Content on Microstructure, Strength, and Fracture Behavior of Yttria-Stabilized Zirconia. Materials 2022, 15, 5212. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Xu, Y.L.; Hong, G.; Yu, H. Effects of low-temperature degradation on the surface roughness of yttria-stabilized tetragonal zirconia polycrystal ceramics: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 125, 222–230. [Google Scholar] [CrossRef] [PubMed]
- Jerman, E.; Lümkemann, N.; Eichberger, M.; Zoller, C.; Nothelfer, S.; Kienle, A.; Stawarczyk, B. Evaluation of translucency, Marten’s hardness, biaxial flexural strength and fracture toughness of 3Y-TZP, 4Y-TZP and 5Y-TZP materials. Dent. Mater. 2021, 37, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Sun, C.; Cao, J.; Wu, Y.; Cui, B.; Ma, J.; Wang, H. Mechanical Properties and In Vitro Biocompatibility of Hybrid Polymer-HA/BAG Ceramic Dental Materials. Polymers 2022, 14, 3774. [Google Scholar] [CrossRef] [PubMed]
- Fathy, H.; Hamama, H.H.; El-Wassefy, N.; Mahmoud, S.H. Clinical performance of resin-matrix ceramic partial coverage restorations: A systematic review. Clin. Oral Investig. 2022, 26, 3807–3822. [Google Scholar] [CrossRef]
- Available online: https://www.iso.org/obp/ui#iso:std:iso:6872:ed-4:v1:en (accessed on 22 March 2023).
- Silva, L.H.D.; Lima, E.; Miranda, R.B.P.; Favero, S.S.; Lohbauer, U.; Cesar, P.F. Dental ceramics: A review of new materials and processing methods. Braz. Oral Res. 2017, 31 (Suppl. S1), e58. [Google Scholar] [CrossRef]
- Almohammed, S.N.; Alshorman, B.; Abu-Naba’a, L.A. Optical Properties of Five Esthetic Ceramic Materials Used for Monolithic Restorations: A Comparative In Vitro Study. Ceramics 2022, 5, 961–980. [Google Scholar] [CrossRef]
- Alao, A.R.; Stoll, R.; Song, X.F.; Miyazaki, T.; Hotta, Y.; Shibata, Y.; Yin, L. Surface quality of yttria-stabilized tetragonal zirconia polycrystal in CAD/CAM milling, sintering, polishing and sandblasting processes. J. Mech. Behav. Biomed. Mater. 2017, 65, 102–116. [Google Scholar] [CrossRef] [PubMed]
- Chevalier, J.; Gremillard, L.; Deville, S. Low-temperature degradation of zirconia and implications for biomedical implants. Annu. Rev. Mater. Res. 2007, 37, 1–32. [Google Scholar] [CrossRef]
- Ban, S. Reliability and properties of core materials for all-ceramic dental restorations. Jpn. Dent. Sci. Rev. 2008, 44, 3–21. [Google Scholar] [CrossRef]
- Fischer, J.; Stawarczyk, B.; Hämmerle, C. Flexural strength of veneering ceramics for zirconia. J. Dent. 2008, 36, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Dowling, N. Mechanical Behavior of Materials; Prentice-Hall: Englewood Cliffs, NJ, USA, 1993; p. 347. [Google Scholar]
- Anstis, G.; Chantikul, P.; Lawn, B.R.; Marshall, D. A critical evaluation of indentation techniques for measuring fracture toughness: I, direct crack measurements. J. Am. Ceramic. Soc. 1981, 64, 533–538. [Google Scholar] [CrossRef]
- Yilmaz, H.; Aydin, C.; Gul, B.E. Flexural strength and fracture toughness of dental core ceramics. J. Prosthet. Dent. 2007, 98, 120–128. [Google Scholar] [CrossRef]
- Machry, R.V.; Borges, A.L.S.; Pereira, G.K.R.; Kleverlaan, C.J.; Venturini, A.B.; Valandro, L.F. Influence of the foundation substrate on the fatigue behavior of bonded glass, zirconia polycrystals, and polymer infiltrated ceramic simplified CAD-CAM restorations. J. Mech. Behav. Biomed. Mater. 2021, 117, 104391. [Google Scholar] [CrossRef]
- Sulaiman, T.A. Materials in digital dentistry-A review. J. Esthet. Restor. Dent. 2020, 32, 171–181. [Google Scholar] [CrossRef]
- Kelly, J.R.; Cesar, P.F.; Scherrer, S.S.; Della Bona, A.; van Noort, R.; Tholey, M.; Vichi, A.; Lohbauer, U. ADM guidance-ceramics: Fatigue principles and testing. Dent. Mater. 2017, 33, 1192–1204. [Google Scholar] [CrossRef]
- Xu, Y.; Han, J.; Lin, H.; An, L. Comparative study of flexural strength test methods on CAD/CAM Y-TZP dental ceramics. Regen. Biomater. 2015, 2, 239–244. [Google Scholar] [CrossRef]
- Ban, S.; Anusavice, K.J. Influence of test method on failure stress of brittle dental materials. J. Dent. Res. 1990, 69, 1791–1799. [Google Scholar] [CrossRef] [PubMed]
- Wendler, M.; Belli, R.; Petschelt, A.; Mevec, D.; Harrer, W.; Lube, T.; Danzer, R.; Lohbauer, U. Chairside CAD/CAM materials. Part 2: Flexural strength testing. Dent. Mater. 2017, 33, 99–109. [Google Scholar] [CrossRef] [PubMed]
- ASTM C1327-15; Standard Test Method for Vickers Indentation Hardness of Advanced Ceramics. ASTM International: West Conshohocken, PA, USA, 2019; p. 10.
- Reale Reyes, A.; Dennison, J.B.; Powers, J.M.; Sierraalta, M.; Yaman, P. Translucency and flexural strength of translucent zirconia ceramics. J. Prosthet. Dent. 2021. [Google Scholar] [CrossRef]
- Juntavee, N.; Attashu, S. Effect of sintering process on color parameters of nano-sized yttria partially stabilized tetragonal monolithic zirconia. J. Clin. Exp. Dent. 2018, 10, e794–e804. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Keul, C.; Eichberger, M.; Figge, D.; Edelhoff, D.; Lümkemann, N. Three generations of zirconia: From veneered to monolithic. Part I. Quintessence Int. 2017, 48, 369–380. [Google Scholar] [PubMed]
- Zhang, F.; Inokoshi, M.; Batuk, M.; Hadermann, J.; Naert, I.; Van Meerbeek, B.; Vleugels, J. Strength, toughness and aging stability of highly-translucent Y-TZP ceramics for dental restorations. Dent. Mater. 2016, 32, e327–e337. [Google Scholar] [CrossRef]
- Čokić, S.M.; Cóndor, M.; Vleugels, J.; Meerbeek, B.V.; Oosterwyck, H.V.; Inokoshi, M.; Zhang, F. Mechanical properties– translucency–microstructure relationships in commercial monolayer and multilayer monolithic zirconia ceramics. Dent. Mater. 2022, 38, 797–810. [Google Scholar] [CrossRef]
- Winter, A.; Schurig, A.; Odenthal, A.L.; Schmitter, M. Impact of different layers within a blank on mechanical properties of multi-layered zirconia ceramics before and after thermal aging. Dent. Mater. 2022, 38, e147–e154. [Google Scholar] [CrossRef] [PubMed]
- Strasser, T.; Wertz, M.; Koenig, A.; Koetzsch, T.; Rosentritt, M. Microstructure, composition, and flexural strength of different layers within zirconia materials with strength gradient. Dent. Mater. 2023. Epub ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.oraltec.co.nz/product/13670-ceramill-zolid-gen-x-a35-98x25mm (accessed on 15 April 2023).
- Available online: https://zirconiacontempo.com/product/product-1/ (accessed on 15 April 2023).
- Available online: https://downloadcenter.ivoclar.com/#search-text=34882&details=34882 (accessed on 15 April 2023).
- Inokoshi, M.; Liu, H.; Yoshihara, K.; Yamamoto, M.; Tonprasong, W.; Benino, Y.; Minakuchi, S.; Vleugels, J.; Van Meerbeek, B.; Zhang, F. Layer characteristics in strength-gradient multilayered yttria-stabilized zirconia. Dent. Mater. 2023, 39, 430–441. [Google Scholar] [CrossRef]
- Beyabanaki, E.; Ashtiani, R.E.; Moradi, M.; Namdari, M.; Mostafavi, D.; Zandinejad, A. Biaxial flexural strength and Weibull characteristics of a resin ceramic material after thermal-cycling. J. Prosthodont. 2022. Epub ahead of print. [Google Scholar] [CrossRef]
- Choi, B.J.; Yoon, S.; Im, Y.W.; Lee, J.H.; Jung, H.J.; Lee, H.H. Uniaxial/biaxial flexure strengths and elastic properties of resin-composite block materials for CAD/CAM. Dent. Mater. 2019, 35, 389–401. [Google Scholar] [CrossRef]
- Yin, R.; Kim, Y.K.; Jang, Y.S.; Lee, J.J.; Lee, M.H.; Bae, T.S. Comparative evaluation of the mechanical properties of CAD/CAM dental blocks. Odontology 2019, 107, 360–367. [Google Scholar] [CrossRef]
- Sen, N.; Us, Y.O. Mechanical and optical properties of monolithic CAD-CAM restorative materials. J. Prosthet. Dent. 2018, 119, 593–599. [Google Scholar] [CrossRef] [PubMed]
- Yin, R.; Jang, Y.S.; Lee, M.H.; Bae, T.S. Comparative Evaluation of Mechanical Properties and Wear Ability of Five CAD/CAM Dental Blocks. Materials 2019, 12, 2252. [Google Scholar] [CrossRef] [PubMed]
- Ramos Nde, C.; Campos, T.M.; Paz, I.S.; Machado, J.P.; Bottino, M.A.; Cesar, P.F.; Melo, R.M. Microstructure characterization and SCG of newly engineered dental ceramics. Dent. Mater. 2016, 32, 870–878. [Google Scholar] [CrossRef] [PubMed]
- Venturini, A.B.; Dapieve, K.S.; de Kok, P.; Pereira, G.K.R.; Valandro, L.F.; Kleverlaan, C.J. Effect of the region of the CAD/CAM block on the flexural strength and structural reliability of restorative materials. J. Mech. Behav. Biomed. Mater. 2023, 138, 105597. [Google Scholar] [CrossRef] [PubMed]
- Albero, A.; Pascual, A.; Camps, I.; Grau-Benitez, M. Comparative characterization of a novel cad-cam polymer-infiltrated-ceramic-network. J. Clin. Exp. Dent. 2015, 7, e495–e500. [Google Scholar] [CrossRef] [PubMed]
- Elraggal, A.; RAfifi, R.; Alamoush, R.A.; Raheem, I.A.; Watts, D.C. Effect of acidic media on flexural strength and fatigue of CAD-CAM dental materials. Dent. Mater. 2023, 39, 57–69. [Google Scholar] [CrossRef]
- Oliveira Junior, J.R.; Cruz, M.E.M.D.; Dovigo, L.N.; Fonseca, R.G. Long-term effects of simulated gastric juice alternated with brushing on hardness, substance loss, flexural strength and reliability of CAD-CAM monolithic materials. J. Appl. Oral Sci. 2022, 30, e20210536. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.; Yu, T.; Chen, J. Biaxial flexural strength and translucent characteristics of dental lithium disilicate glass ceramics with different translucencies. J. Prosthodont. Res. 2020, 64, 71–77. [Google Scholar] [CrossRef] [PubMed]
- FFonzar, R.; Carrabba, M.; Sedda, M.; Ferrari, M.; Goracci, C.; Vichi, A. Flexural resistance of heat-pressed and CAD-CAM lithium disilicate with different translucencies. Dent. Mater. 2017, 33, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.H.; Chang, J.; Son, H.H. Flexural strength and microstructure of two lithium disilicate glass ceramics for CAD/CAM restoration in the dental clinic. Restor. Dent. Endod. 2013, 38, 134–140. [Google Scholar] [CrossRef]
- Buso, L.; Oliveira-Júnior, O.B.; Hiroshi Fujiy, F.; Leão Lombardo, G.H.; Ramalho Sarmento, H.; Campos, F.; Assunção Souza, R.O. Biaxial flexural strength of CAD/CAM ceramics. Minerva Stomatol. 2011, 60, 311–319. [Google Scholar] [PubMed]
- Lin, W.S.; Ercoli, C.; Feng, C.; Morton, D. The effect of core material, veneering porcelain, and fabrication technique on the biaxial flexural strength and weibull analysis of selected dental ceramics. J. Prosthodont. 2012, 21, 353–362. [Google Scholar] [CrossRef] [PubMed]
- Kocjan, A.; Cotič, J.; Kosmač, T.; Jevnikar, P. In vivo aging of zirconia dental ceramics—Part I: Biomedical grade 3Y-TZP. Dent. Mater. 2021, 37, 443–453. [Google Scholar] [CrossRef] [PubMed]
- Cotič, J.; Kocjan, A.; Panchevska, S.; Kosmač, T.; Jevnikar, P. In vivo ageing of zirconia dental ceramics—Part II: Highly-translucent and rapid-sintered 3Y-TZP. Dent. Mater. 2021, 37, 454–463. [Google Scholar] [CrossRef]
- Pereira, G.K.; Guilardi, L.F.; Dapieve, K.S.; Kleverlaan, C.J.; Rippe, M.P.; Valandro, L.F. Mechanical reliability, fatigue strength and survival analysis of new polycrystalline translucent zirconia ceramics for monolithic restorations. J. Mech. Behav. Biomed. Mater. 2018, 85, 57–65. [Google Scholar] [CrossRef]
- Kim, J.W.; Covel, N.S.; Guess, P.C.; Rekow, E.D.; Zhang, Y. Concerns of hydrothermal degradation in CAD/CAM zirconia. J. Dent. Res. 2010, 89, 91–95. [Google Scholar] [CrossRef]
- Lucsanszky, I.J.; Ruse, N.D. Fracture toughness, flexural strength, and flexural modulus of new CAD/CAM resin composite blocks. J. Prosth. 2020, 29, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Egilmez, F.; Ergun, G.; Cekic-Nagas, I.; Vallittu, P.K.; Lassila, L.V. Does artificial aging affect mechanical properties of CAD/CAM composite materials. J. Prosth. Res. 2018, 62, 65–74. [Google Scholar] [CrossRef]
- Candido, L.; Miotto, L.; Fais, L.; Cesar, P.; Pinelli, L. Mechanical and surface properties of monolithic zirconia. Oper. Dent. 2018, 43, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, J.W.; Sidhu, S.K.; Czarnecka, B. Enhancing the mechanical properties of glassionomer dental cements: A review. Materials 2020, 13, 2510. [Google Scholar] [CrossRef] [PubMed]
- Lazar, D.R.; Bottino, M.C.; Özcan, M.; Valandro, L.F.; Amaral, R.; Ussui, V.; Bressiani, A.H.A. Y-TZP ceramic processing from co precipitated powders: A comparative study with three commercial dental ceramics. Dent. Mater. 2008, 24, 1676–1685. [Google Scholar] [CrossRef] [PubMed]
- Min, J.; Arola, D.D.; Yu, D.; Yu, P.; Zhang, Q.; Yu, H.; Gao, S. Comparison of human enamel and polymer-infiltrated-ceramic-network material “ENAMIC” through micro-and nano mechanical testing. Ceram. Int. 2016, 42, 10631–10637. [Google Scholar] [CrossRef]
- Kim, S.-H.; Choi, Y.-S.; Kang, K.-H.; Att, W. Effects of thermal and mechanical cycling on the mechanical strength and surface properties of dental CAD-CAM restorative materials. J. Prosth. Dent. 2021, 3913, 30727. [Google Scholar] [CrossRef] [PubMed]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical properties of polymer-infiltrated-ceramic network materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Vatali, A.; Kontonasaki, E.; Kavouras, P.; Lawrence, S.K.; Bahr, D.F. Effect of heat treatment and in vitro aging on the microstructure and mechanical properties of cold isostatic-pressed zirconia ceramics for dental restorations. Dent. Mater. 2014, 30, e272–e282. [Google Scholar] [CrossRef]
- De Souza, G.M.; Zykus, A.; Ghahnavyeh, R.R.; Lawrence, S.K.; Bahr, D.F. Effect of accelerated aging on dental zirconia-based materials. J. Mech. Behav. Biomed. Mater. 2017, 65, 256–263. [Google Scholar] [CrossRef]
- Moqbel, N.M.; Al-Akhali, M.; Wille, S.; Kern, M. Influence of Aging on Biaxial Flexural Strength and Hardness of Translucent 3Y-TZP. Materials 2019, 13, 27. [Google Scholar] [CrossRef]
- Alfrisany, N.M.; De Souza, G.M. Surface and bulk properties of zirconia as a function of composition and aging. J. Mech. Behav. Biomed. Mater. 2022, 126, 104994. [Google Scholar] [CrossRef]
- Gaillard, Y.; Jiménez-Piqué, E.; Soldera, F.; Mücklich, F.; Anglada, M. Quantification of hydrothermal degradation in zirconia by nanoindentation. Acta Mater. 2008, 56, 4206–4216. [Google Scholar] [CrossRef]
- Kim, H.-T.; Han, J.-S.; Yang, J.-H.; Lee, J.-B.; Kim, S.-H. The effect of low temperature aging on the mechanical property & phase stability of Y-TZP ceramics. J. Adv. Prosth. 2009, 1, 113–117. [Google Scholar]
- Tong, H.; Tanaka, C.B.; Kaizer, M.R.; Zhang, Y. Characterization of three commercial YTZP ceramics produced for their high-translucency, high-strength and high-surface area. Ceram. Int. 2016, 42, 1077–1085. [Google Scholar] [CrossRef] [PubMed]
- Byeon, S.-M.; Song, J.-J. Mechanical properties and microstructure of the leucitereinforced glass-ceramics for dental cad/cam. J. Dent. Hyg. Sci. 2018, 18, 42–49. [Google Scholar] [CrossRef]
- de Araújo-Júnior, E.N.S.; Bergamo, E.T.P.; Bastos, T.M.C.; Jalkh, E.B.B.; Lopes, A.C.O.; Monteiro, K.N.; Cesar, P.F.; Tognolo, F.C.; Migliati, R.; Tanaka, R.; et al. Ultra-translucent zirconia processing and aging effect on microstructural, optical, and mechanical properties. Dent. Mater. 2022, 38, 587–600. [Google Scholar] [CrossRef] [PubMed]
- Benalcázar Jalkh, E.B.; Bergamo, E.T.P.; Monteiro, K.N.; Cesar, P.F.; Genova, L.A.; Lopes, A.C.O.; Lisboa Filho, P.N.; Coelho, P.G.; Santos, C.F.; Bortolin, F.; et al. Aging resistance of an experimental zirconia-toughened alumina composite for large span dental prostheses: Optical and mechanical characterization. J. Mech. Behav. Biomed. Mater. 2020, 104, 103659. [Google Scholar] [CrossRef] [PubMed]
- Kanitkar, A.A.; Gandhi, P.; Kanitkar, A.; Priya, S.V.; Paranna, S.; Patil, S. Aging resistance of infiltrated monolithic zirconia compared to noninfiltrated monolithic zirconia: A systematic review of in vitro studies. J. Indian Prosthodont. Soc. 2022, 22, 131–142. [Google Scholar] [CrossRef]
- Zhang, F.; Reveron, H.; Spies, B.C.; Van Meerbeek, B.; Chevalier, J. Trade-off between fracture resistance and translucency of zirconia and lithium-disilicate glass ceramics for monolithic restorations. Acta Biomater. 2019, 91, 24–34. [Google Scholar] [CrossRef]
- Guess, P.C.; Schultheis, S.; Bonfante, E.A.; Coelho, P.G.; Ferencz, J.L.; Silva, N.R. All-ceramic systems: Laboratory and clinical performance. Dent. Clin. 2011, 55, 333–352. [Google Scholar] [CrossRef]
- Camposilvan, E.; Leone, R.; Gremillard, L.; Sorrentino, R.; Zarone, F.; Ferrari, M.; Chevalier, J. Aging resistance, mechanical properties and translucency of different yttria-stabilized zirconia ceramics for monolithic dental crown applications. Dent Mater. 2018, 34, 879–890. [Google Scholar] [CrossRef]
- Hampe, R.; Theelke, B.; Lümkemann, N.; Eichberger, M.; Stawarczyk, B. Fracture toughness analysis of ceramic and resin composite CAD/CAM material. Oper. Dent. 2019, 44, 190–201. [Google Scholar] [CrossRef]
- Lawn, B.; Marshall, D. Hardness, toughness, and brittleness: An indentation analysis. J. Am. Ceramic Soc. 1979, 62, 347–350. [Google Scholar] [CrossRef]
- Daguano, J.K.M.B.; Dantas, L.; Soares, V.O.; Alves, M.F.R.P.; Santos, C.D.; Zanotto, E.D. Optimizing the microstructure of a new machinable bioactive glass-ceramic. J. Mech. Behav. Biomed. Mater. 2021, 122, 104695. [Google Scholar] [CrossRef] [PubMed]
- Elsaka, S.E.; Elnaghy, A.M. Mechanical properties of zirconia reinforced lithium silicate glass-ceramic. Dent. Mater. 2016, 32, 908–914. [Google Scholar] [CrossRef] [PubMed]
- Pollington, S.; van Noort, R. Manufacture, characterisation and properties of novel fluorcanasite glass-ceramics. J. Dent. 2012, 40, 1006–1017. [Google Scholar] [CrossRef]
- Tsitrou, E.A.; Northeast, S.E.; van Noort, R. Brittleness index of machinable dental materials and its relation to the marginal chipping factor. J. Dent. 2007, 35, 897–902. [Google Scholar] [CrossRef] [PubMed]


| Material as Described by the Company | Subtype Numbers and Company Details | Trade Name and Specific Subtype Tested | Abbreviation | Basic chemical Structure (Chemical Composition, (wt%) |
|---|---|---|---|---|
| Multilayer highly translucent monolithic zirconia (4 layers) | Ceramill Zolid has 7 subtypes, Amann Girrbach AG, Germany | Ceramill Zolid® Gen-X | GNX | 4Y-TZP: ZrO2 + HfO2 + Y2O3 ≥ 99.0% Y2O3 6–7% HfO2 ≤ 5% Al2O3 ≤ 0. 5% Other oxides ≤ 1% |
| Natural esthetics and high-strength multilayer zirconia (3 layers) | IPS ZirCAD has 5 subtypes, Ivoclar Vivadent, Schaan, Liechtenstein | IPS e.max® ZirCAD Prime | ZCP | 3Y-TZP and 5Y-TZP: ZrO2 88–95.5% Y2O3 4.5–7% HfO2 < 5% AL2O3 < 1% Other oxides < 1.5% |
| Monolithic multilayer zirconia (5 Layers) | Upcera has 11 subtypes, Upcera, China | Upcera® Esthetic Explore Prime | UPC | 4Y-TZP and 5Y-TZP: ZrO2 + HfO2 86.3–94.2% Fe2O3 < 0.5 % Y2O3 5.8–9.7% Er2O3 < 2% Al2O3 < 0.5% Other oxides < 0.5% |
| Polymer infiltrated hybrid (Single layer) | Vita Enamic has 3 subtypes, Zahnfabrik H. Rauter GmbH, Germany | Vita® Enamic 2M2 T | ENM | 86% by weight (75% by volume) ceramic network and 14% by weight (25% by volume) polymerized methacrylate polymer network; UDMA and TEGDMA [SiO2 (58–63%), Al2O3 (20–23%), Na2O (9–11%), K2O (4–6%), B2O3 (0.5–2%), CaO (<1%) and TiO2 (<1%)]. |
| Highly esthetic lithium disilicate (Single layer) | IPS e.max CAD has 4 subtypes, Ivoclar Vivadent, Schaan, Liechtenstein | IPS e.max® CAD LT | EMX | SiO2 57–80 % Li2O 11–19% K2O 0–13% P2O5 0–11% ZrO2 0–8% ZnO 0–8% Al2O3 0–5% MgO 0–5% Coloring oxides 0–8% |
| Group | Heating Rate and Eventual Heating Steps | Final Temperature (°C) | Holding Time (min) | Cooling Rate up | Furnace Brand |
|---|---|---|---|---|---|
| GNX | 8 °C/min | 1450 °C | 120 | 20 °C/min | Ceramill Therm (Amann Girrbach) |
| ZCP | 10 °C/min until 900 °C is attained; after holding for 30 min, use a heating rate of 3.3 °C/min until 1500 °C | 1500 °C | 120 | 10 °C/min from 1500 °C to 900 °C, then 8 °C/min from 900 °C to 300 °C | Ceramill Therm (Amann Girrbach) |
| UPC | 10 °C/min until 300 °C, then 17.5 °C/min until 1000 °C, and 4 °C/min until 1530 °C | 1530 °C | 120 | 12.2 °C/min | Ceramill Therm (Amann Girrbach) |
| EMX | 60 °C/min until 770 °C is attained, hold for 5 min, then 30 °C/min until 850 °C | 850 °C | 10 | 20 °C/min | Programat EP5010 (Ivoclar Vivadent) |
| Aging | S (MPa) (n = 18) | VH (MPa) (n = 14) | K (MPa.m1/2) (n = 14) | B (µm−1/2) (n = 14) | |
|---|---|---|---|---|---|
| GNX | without | 874.1 ± 151.50 | 1652.0 ± 95.52 | 2.6 ± 0.24 | 6.3 |
| with | 943.3 ± 164.906 | 1565.6 ± 147.63 | 3.0 ± 0.13 | 5.2 | |
| ZCP | without | 765.3 ± 96.09 | 1614.4 ± 173.39 | 2.1 ± 0.05 | 7.8 |
| with | 852. ± 146.50 | 1618.2 ± 58.13 | 3.7 ± 0.067 | 4.4 | |
| UPC | without | 699.0 ± 85.41 | 1575.7 ± 98.75 | 3.2 ± 0.21 | 4.9 |
| with | 715.6 ± 91.32 | 1691.4 ± 70.18 | 2.9 ± 0.079 | 5.8 | |
| ENM | without | 175.8 ± 17.21 | 290.1 ± 31.49 | 0.7 ± 0.03 | 4.5 |
| with | 150.3 ± 16.61 | 268.3 ± 15.89 | 0.6 ± 0.01 | 4.7 | |
| EMX | without | 433.0 ± 54.61 | 721.9 ± 36.05 | 0.9 ± 0.03 | 7.9 |
| with | 475.5 ± 56.19 | 681.7 ± 64.50 | 1.0 ± 0.048 | 7.1 |
| (I) Material | (J) Material | S Value Sig. | VH Value Sig. | K Value Sig. |
|---|---|---|---|---|
| GNX | ZCP | 0.402 | 0.905 | 0.004 |
| UPC | 0.064 | 0.100 | 0.003 | |
| ENM | 0.000 | 0.000 | 0.000 | |
| EMX | 0.000 | 0.000 | 0.000 | |
| ZCP | UPC | 0.549 | 0.899 | 0.000 |
| ENM | 0.000 | 0.000 | 0.000 | |
| EMX | 0.000 | 0.000 | 0.000 | |
| UPC | ENM | 0.000 | 0.000 | 0.000 |
| EMX | 0.000 | 0.000 | 0.000 | |
| ENM | EMX | 0.000 | 0.000 | 0.000 |
| Material | Aging | S Value n = 9 Sig. (2-Tailed) | VH Value n = 7 Sig. (2-Tailed) | K Value n = 7 Sig. (2-Tailed) |
|---|---|---|---|---|
| GNX | without | 0.368 | 0.030 | 0.005 |
| with | 0.368 | 0.030 | 0.005 | |
| ZCP | without | 0.158 | 0.925 | 0.000 |
| with | 0.158 | 0.925 | 0.000 | |
| UPC | without | 0.696 | 0.000 | 0.005 |
| with | 0.696 | 0.000 | 0.005 | |
| ENM | without | 0.006 | 0.008 | 0.000 |
| with | 0.006 | 0.008 | 0.000 | |
| EMX | without | 0.123 | 0.018 | 0.071 |
| with | 0.123 | 0.018 | 0.071 |
| Material | Biaxial Flexure Strength | /Aging | Fracture Toughness | /Aging | Vickers Hardness | /Aging | Brittleness | /Aging |
|---|---|---|---|---|---|---|---|---|
| Ceramill Zolid Gen X | none | none | none | none | none | none | none | none |
| ZirCad prime | Multiple studies. | none | none | none | none | none | none | none |
| Upcera Explore Esthetic | none | none | none | none | none | none | none | none |
| Vita Enamic | Multiple studies | Multiple studies | Multiple studies | none | Multiple studies | none | none | none |
| IPS e.max CAD | Multiple studies | none | Multiple studies | none | Multiple studies | none | none | none |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Almohammed, S.N.; Alshorman, B.; Abu-Naba’a, L.A. Mechanical Properties of Five Esthetic Ceramic Materials Used for Monolithic Restorations: A Comparative In Vitro Study. Ceramics 2023, 6, 1031-1049. https://doi.org/10.3390/ceramics6020061
Almohammed SN, Alshorman B, Abu-Naba’a LA. Mechanical Properties of Five Esthetic Ceramic Materials Used for Monolithic Restorations: A Comparative In Vitro Study. Ceramics. 2023; 6(2):1031-1049. https://doi.org/10.3390/ceramics6020061
Chicago/Turabian StyleAlmohammed, Saleh N., Belal Alshorman, and Layla A. Abu-Naba’a. 2023. "Mechanical Properties of Five Esthetic Ceramic Materials Used for Monolithic Restorations: A Comparative In Vitro Study" Ceramics 6, no. 2: 1031-1049. https://doi.org/10.3390/ceramics6020061
APA StyleAlmohammed, S. N., Alshorman, B., & Abu-Naba’a, L. A. (2023). Mechanical Properties of Five Esthetic Ceramic Materials Used for Monolithic Restorations: A Comparative In Vitro Study. Ceramics, 6(2), 1031-1049. https://doi.org/10.3390/ceramics6020061