Effects of Wildfire Exposure on the Human Immune System
Abstract
:Highlights
- Wildfire smoke contains immuno-toxic components, including fine particles, VOCs, and PAHs.
- Chronic exposure to wildfire smoke can induce oxidative stress, inflammation, and long-term effects on the immune system.
- Wildfire smoke poses significant risks to immune health due to the presence of toxic com-ponents.
- Ongoing exposure to these toxic components may lead to persistent health effects, underlining the need for intervention and protective measures.
Abstract
1. Introduction
2. Composition of Wildfire Smoke and Immunotoxins
3. Acute Immune Responses to Wildfire Smoke Exposure
4. Chronic Immune Effects of Prolonged Wildfire Smoke Exposure
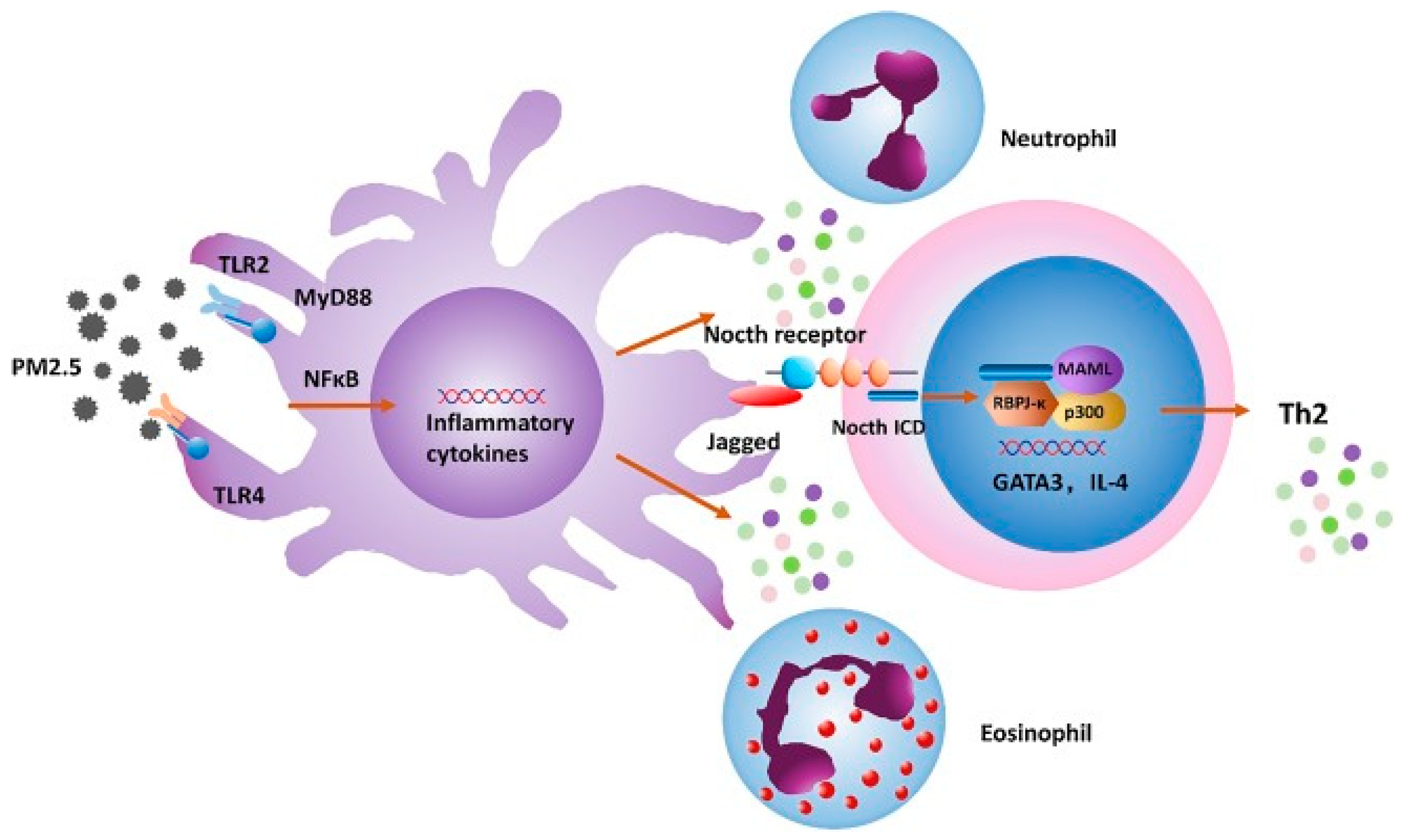
5. Mechanisms of Immune Modulation by Wildfire Smoke
6. Vulnerable Populations
7. Effects on Asthma
8. Long-Term Outcomes
9. Effects on Upper Respiratory Illnesses
10. Implications for Public Health and Future Research
11. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Flannigan, M.D.; Krawchuk, M.A.; de Groot, W.J.; Wotton, B.M.; Gowman, L.M. Implications of changing climate for global wildland fire. Int. J. Wildland Fire 2009, 18, 483–507. [Google Scholar] [CrossRef]
- Naeher, L.P.; Brauer, M.; Lipsett, M.; Bevan, A. Wood smoke health effects: A review. Inhal. Toxicol. 2007, 19, 67–106. [Google Scholar] [CrossRef] [PubMed]
- Reid, C.E.; Brauer, M.; Johnston, F.H.; Jerrett, M.; Balmes, J.R.; Elliott, C.T. Critical review of health impacts of wildfire smoke exposure. Environ. Health Perspect. 2016, 124, 1334–1343. [Google Scholar] [CrossRef] [PubMed]
- Black, C.; Gerriets, J.E.; Fontaine, J.H.; Harper, R.W.; Kenyon, N.J.; Tablin, F.; Schelegle, E.S.; Miller, L.A. Early Life Wildfire Smoke Exposure Is Associated with Immune Dysregulation and Lung Function Decrements in Adolescence. Am. J. Respir. Cell Mol. Biol. 2017, 56, 657–666. [Google Scholar] [CrossRef]
- Prunicki, M.M.; Dant, C.C.; Cao, S.; Maecker, H.; Haddad, F.; Kim, J.B.; Snyder, M.; Wu, J.; Nadeau, K. Immunologic effects of forest fire exposure show increases in IL-1β and CRP. Allergy 2020, 75, 2356–2358. [Google Scholar] [CrossRef]
- Ishihara, Y.; Kado, S.Y.; Bein, K.J.; He, Y.; Pouraryan, A.A.; Urban, A.; Haarmann-Stemmann, T.; Sweeney, C.; Vogel, C.F.A. Aryl hydrocarbon receptor signaling synergizes with TLR/NF-κB-signaling for induction of IL-22 through canonical and non-canonical AhR pathways. Front. Toxicol. 2021, 3, 787360. [Google Scholar] [CrossRef]
- Ferguson, M.D.; Semmens, E.O.; Dumke, C.; Quindry, J.C.; Ward, T.J. Measured pulmonary and systemic markers of inflammation and oxidative stress following wildland firefighter simulations. J. Occup. Environ. Med. 2016, 58, 407–413. [Google Scholar] [CrossRef]
- Main, L.C.; Wolkow, A.P.; Tait, J.L.; Della Gatta, P.; Raines, J.; Snow, R.; Aisbett, B. Firefighter’s acute inflammatory response to wildfire suppression. J. Occup. Environ. Med. 2020, 62, 145–148. [Google Scholar] [CrossRef]
- Dickinson, G.N.; Miller, D.D.; Bajracharya, A.; Bruchard, W.; Durbin, T.A.; McGarry, J.K.P.; Moser, E.P.; Nuñez, L.A.; Pukkila, E.J.; Scott, P.S.; et al. Health Risk Implications of Volatile Organic Compounds in Wildfire Smoke During the 2019 FIREX-AQ Campaign and Beyond. Geohealth 2022, 6, e2021GH000546. [Google Scholar] [CrossRef]
- Wentworth, G.R.; Aklilu, Y.A.; Landis, M.S.; Hsu, Y.M. Impacts of a large boreal wildfire on ground level atmospheric concentrations of PAHs, VOCs and ozone. Atmos. Environ. 2018, 178, 19–30. [Google Scholar] [CrossRef]
- Blando, J.; Allen, M.; Galadima, H.; Tolson, T.; Akpinar-Elci, M.; Szklo-Coxe, M. Observations of Delayed Changes in Respiratory Function among Allergy Clinic Patients Exposed to Wildfire Smoke. Int. J. Environ. Res. Public Health 2022, 19, 1241. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.A.; Dockery, D.W. Health effects of fine particulate air pollution: Lines that connect. J. Air Waste Manag. Assoc. 2006, 56, 709–742. [Google Scholar] [CrossRef]
- Bargagli, E.; Rottoli, P. Fine particulate matter and systemic inflammation: A review of recent evidence. J. Environ. Sci. Health 2012, 47, 1853–1865. [Google Scholar]
- Gong, J.; Xu, X.; Liu, T. Wildfire smoke exposure and its effects on human health: A review. Environ. Pollut. 2022, 298, 118773. [Google Scholar] [CrossRef]
- Kok, L.H.; Martin, R.M. The effects of polycyclic aromatic hydrocarbons on immune cells and immune responses. Environ. Toxicol. Pharmacol. 2015, 287, 83–91. [Google Scholar] [CrossRef]
- Riediker, M.; Schilter, B. Air pollutants and the immune system: Formaldehyde and benzene. J. Environ. Sci. Health Part C 2008, 26, 17–28. [Google Scholar]
- Yu, Y.Y.; Jin, H.; Lu, Q. Effect of polycyclic aromatic hydrocarbons on immunity. J. Transl. Autoimmun. 2022, 5, 100177. [Google Scholar] [CrossRef] [PubMed]
- Gould, C.F.; Heft-Neal, S.; Johnson, M.; Aguilera, J.; Burke, M.; Nadeau, K. Health Effects of Wildfire Smoke Exposure. Annu. Rev. Med. 2024, 75, 277–292. [Google Scholar] [CrossRef]
- Reid, C.E.; Brines, S.J. Crisis in the air: Wildfires and respiratory health. Environ. Health Perspect. 2005, 113, 1055–1058. [Google Scholar]
- Miller, A.K.; Burch, R.E. Impact of wildfire smoke on immune response and cytokine release: Evidence from recent studies. Front. Public Health 2019, 7, 148. [Google Scholar] [CrossRef]
- Moore, M.W.; Ketchum, K. Elevated C-reactive protein levels in response to wildfire smoke exposure: Evidence from epidemiological studies. Environ. Health Perspect. 2006, 114, 1442–1447. [Google Scholar] [CrossRef]
- Sies, H. Oxidative stress: A concept in redox biology and medicine. Redox Biol. 2015, 4, 180–183. [Google Scholar] [CrossRef] [PubMed]
- Cascio, W.E. Wildland fire smoke and respiratory health: A review of the evidence on oxidative stress and inflammation. Int. J. Environ. Res. Public Health 2018, 15, 1611. [Google Scholar] [CrossRef]
- Schafer, M.; Matheis, K.A. Oxidative stress and its role in macrophage dysfunction and chronic inflammation. Immunol. Cell Biol. 2014, 92, 301–309. [Google Scholar] [CrossRef]
- Elliott, C.T.; Henderson, S.B.; Wan, V. Time series analysis of fine particulate matter and asthma reliever dispensations in populations affected by forest fires. Environ. Health 2013, 12, 11. [Google Scholar] [CrossRef]
- Johnston, F.H.; Webby, R.J.; Pilotto, L.S.; Bailie, R.S.; Parry, D.L.; Halpin, S.J. Vegetation fires, particulate air pollution and asthma: A panel study in the Australian monsoon tropics. Int. J. Environ. Health Res. 2006, 16, 391–404. [Google Scholar] [CrossRef]
- Künzli, N.; Avol, E.; Wu, J.; Gauderman, W.J.; Rappaport, E.; Millstein, J.; Bennion, J.; McConnell, R.; Gilliland, F.D.; Berhane, K. Health effects of the 2003 Southern California wildfires on children. Am. J. Respir. Crit. Care Med. 2006, 174, 1221–1228. [Google Scholar] [CrossRef] [PubMed]
- Sutherland, E.R.; Make, B.J.; Vedal, S.; Zhang, L.; Dutton, S.J.; Murphy, J.R.; Silkoff, P.E. Wildfire smoke and respiratory symptoms in patients with chronic obstructive pulmonary disease. J. Allergy Clin. Immunol. 2005, 115, 420–422. [Google Scholar] [CrossRef]
- Rappold, A.G.; Liu, Y. Chronic effects of exposure to wildfire smoke on human health: An epidemiological study. Am. J. Respir. Crit. Care Med. 2019, 199, 1596–1604. [Google Scholar]
- Chen, R.; Kan, H. Long-term exposure to fine particulate matter (PM2.5) and health outcomes: A review. Environ. Int. 2018, 116, 134–146. [Google Scholar] [CrossRef]
- Bowatte, G.; Lodge, C.J. Association between particulate matter and health effects: A review of the evidence from wildfire smoke studies. Environ. Health Perspect. 2015, 123, 866–873. [Google Scholar]
- Cohen, A.J.; Brauer, M. Long-term effects of air pollution exposure on immune responses: A review of the evidence. Environ. Res. Lett. 2017, 12, 113001. [Google Scholar]
- Liu, X.; Zhang, Y. Autoimmune and allergic disease risk associated with chronic exposure to wildfire smoke: A review of epidemiological studies. Environ. Pollut. 2021, 274, 115919. [Google Scholar]
- Huang, Y.; Chen, Y. Wildfire smoke exposure and the development of autoimmune and allergic diseases: A review. Environ. Res. Lett. 2019, 14, 093004. [Google Scholar]
- Cascio, W.E.; Rappold, A.G. Adjuvant effects of wildfire smoke on allergic diseases: Mechanisms and implications. Toxicol. Appl. Pharmacol. 2021, 426, 115612. [Google Scholar]
- Akdis, C.A.; Nadeau, K.C. Human and planetary health on fire. Nat. Rev. Immunol. 2022, 22, 651–652. [Google Scholar] [CrossRef]
- Hirota, J.A.; Gold, M.J.; Hiebert, P.R.; Parkinson, L.G.; Wee, T.; Smith, D. The nucleotide-binding domain, leucine-rich repeat protein 3 inflammasome/IL-1 receptor I axis mediates innate, but not adaptive, immune responses after exposure to particulate matter under 10 μm. Am. J. Respir. Cell. Mol. Biol. 2015, 52, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Mou, Y.; Liao, W.; Liang, Y.; Li, Y.; Zhao, M.; Guo, Y. Environmental pollutants induce NLRP3 inflammasome activation and pyroptosis: Roles and mechanisms in various diseases. Sci. Total Environ. 2023, 900, 165851. [Google Scholar] [CrossRef]
- Wang, L.Q.; Liu, T.; Yang, S.; Sun, L.; Zhao, Z.Y.; Li, L.Y. Perfluoroalkyl substance pollutants activate the innate immune system through the AIM2 inflammasome. Nat. Commun. 2021, 12, 2915. [Google Scholar] [CrossRef]
- Alijagic, A.; Hedbrant, A.; Persson, A.; Larsson, M.; Engwall, M.; Särndahl, E. NLRP3 inflammasome as a sensor of micro- and nanoplastics immunotoxicity. Front. Immunol. 2023, 14, 1178434. [Google Scholar] [CrossRef]
- Hoffmann, A. Epigenetic and inflammatory responses to wildfire smoke exposure: Implications for immune system health. Front. Immunol. 2021, 12, 643264. [Google Scholar]
- Jaffe, D.A.; Croft, D.P. Oxidative stress and inflammation in response to wildfire smoke exposure: Mechanistic insights and public health implications. J. Expo. Sci. Environ. Epidemiol. 2020, 30, 571–579. [Google Scholar]
- Croft, D.P. Wildfire smoke and the role of NADPH oxidase in oxidative stress and inflammation. Toxicol. Appl. Pharmacol. 2020, 399, 115033. [Google Scholar] [CrossRef]
- González, M. Epigenetic changes induced by wildfire smoke exposure: DNA methylation and histone modifications. Environ. Health Perspect. 2019, 127, 087001. [Google Scholar] [CrossRef]
- Dominguez, A. Epigenetic regulation of immune responses: Implications for disease susceptibility following exposure to environmental toxins. Toxicol. Appl. Pharmacol. 2019, 377, 114603. [Google Scholar] [CrossRef]
- O’Donovan, D. Impact of wildfire smoke on the microbiome: Implications for respiratory and gut health. Environ. Microbiol. Rep. 2023, 15, 108–115. [Google Scholar] [CrossRef]
- Round, J.L. The gut microbiome and immune system: Insights from microbial dysbiosis and its impact on immune function and disease. Nat. Rev. Immunol. 2016, 16, 287–299. [Google Scholar] [CrossRef]
- Leonardi, G.S.; Houthuijs, D.; Steerenberg, P.A.; Fletcher, T.; Armstrong, B.; Antova, T.; Van Loveren, H. Immune biomarkers in relation to exposure to particulate matter: A Cross-Sectional Survey in 17 Cities of Central Europe. Inhal. Toxicol. 2000, 12 (Suppl. S4), 1–14. [Google Scholar] [CrossRef]
- van Eeden, S.F.; Yeung, A.; Quinlam, K.; Hogg, J.C. Systemic response to ambient particulate matter: Relevance to chronic obstructive pulmonary disease. Proc. Am. Thorac. Soc. 2005, 2, 61–67. [Google Scholar] [CrossRef]
- Ramanathan, M., Jr.; London, N.R., Jr.; Tharakan, A.; Surya, N.; Sussan, T.E.; Rao, X.; Lin, S.Y.; Toskala, E.; Rajagopalan, S.; Biswal, S. Airborne Particulate Matter Induces Nonallergic Eosinophilic Sinonasal Inflammation in Mice. Am. J. Respir. Cell Mol. Biol. 2017, 57, 59–65. [Google Scholar] [CrossRef]
- Alwarawrah, Y.; Kiernan, K.; MacIver, N.J. Changes in Nutritional Status Impact Immune Cell Metabolism and Function. Front. Immunol. 2018, 9, 1055. [Google Scholar] [CrossRef] [PubMed]
- Garg, S. Vulnerable populations and wildfire smoke: Effects on respiratory and immune health. Environ. Res. 2018, 166, 214–223. [Google Scholar] [CrossRef]
- Gong, H. Children’s health and wildfire smoke exposure: Immunotoxic effects and long-term consequences. Curr. Environ. Health Rep. 2022, 9, 186–197. [Google Scholar]
- Fulop, T. Immunosenescence: Impact of aging on the immune system and implications for environmental health risks. Front. Immunol. 2018, 9, 2160. [Google Scholar] [CrossRef]
- Barton, J.R. Vulnerable populations and wildfire smoke: Effects on respiratory and cardiovascular health. J. Environ. Health 2020, 83, 12–20. [Google Scholar]
- Jaffe, D.A. Wildfire smoke and its public health implications: Increased frequency and intensity in the context of climate change. Front. Public Health 2020, 8, 456. [Google Scholar] [CrossRef]
- Reid, C.E.; Maestas, M.M. Wildfire smoke exposure under climate change: Impact on respiratory health of affected communities. Curr. Opin. Pulm. Med. 2019, 25, 179–187. [Google Scholar] [CrossRef]
- Reid, C.E.; Jerrett, M.; Tager, I.B.; Petersen, M.L.; Mann, J.K.; Balmes, J.R. Differential respiratory health effects from the 2008 northern California wildfires: A spatiotemporal approach. Environ. Res. 2016, 150, 227–235. [Google Scholar] [CrossRef]
- Gan, R.W.; Ford, B.; Lassman, W.; Pfister, G.; Vaidyanathan, A.; Fischer, E. Comparison of wildfire smoke estimation methods and associations with cardiopulmonary-related hospital admissions. Geohealth 2017, 1, 122–136. [Google Scholar] [CrossRef]
- Hutchinson, J.A.; Vargo, J.; Milet, M.; French, N.H.F.; Billmire, M.; Johnson, J.; Hoshiko, S. The San Diego 2007 wildfires and Medi-Cal emergency department presentations, inpatient hospitalizations, and outpatient visits: An observational study of smoke exposure periods and a bidirectional case-crossover analysis. PLoS Med. 2018, 15, e1002601. [Google Scholar] [CrossRef]
- DeFlorio-Barker, S.; Crooks, J.; Reyes, J.; Rappold, A.G. Cardiopulmonary effects of fine particulate matter exposure among older adults, during wildfire and non-wildfire periods, in the United States 2008–2010. Environ. Health Perspect. 2019, 127, 37006. [Google Scholar] [CrossRef] [PubMed]
- Stowell, J.D.; Geng, G.; Saikawa, E.; Chang, H.H.; Fu, J.; Yang, C.E. Associations of wildfire smoke PM2.5 exposure with cardiorespiratory events in Colorado 2011–2014. Environ. Int. 2019, 133, 105151. [Google Scholar] [CrossRef] [PubMed]
- Reid, C.E.; Considine, E.M.; Watson, G.L.; Telesca, D.; Pfister, G.G.; Jerrett, M. Associations between respiratory health and ozone and fine particulate matter during a wildfire event. Environ. Int. 2019, 129, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Lipner, E.M.; O’Dell, K.; Brey, S.J.; Ford, B.; Pierce, J.R.; Fischer, E.V.; Crooks, J.L. The associations between clinical respiratory outcomes and ambient wildfire smoke exposure among pediatric asthma patients at National Jewish Health, 2012–2015. Geohealth 2019, 3, 146–159. [Google Scholar] [CrossRef]
- Gan, R.W.; Liu, J.; Ford, B.; O’Dell, K.; Vaidyanathan, A.; Wilson, A. The association between wildfire smoke exposure and asthma-specific medical care utilization in Oregon during the 2013 wildfire season. J. Expo. Sci. Environ. Epidemiol. 2020, 30, 618–628. [Google Scholar] [CrossRef] [PubMed]
- Kiser, D.; Metcalf, W.J.; Elhanan, G.; Schnieder, B.; Schlauch, K.; Joros, A. Particulate matter and emergency visits for asthma: A time-series study of their association in the presence and absence of wildfire smoke in Reno, Nevada, 2013–2018. Environ. Health 2020, 19, 92. [Google Scholar] [CrossRef]
- Magzamen, S.; Gan, R.W.; Liu, J.; O’Dell, K.; Ford, B.; Berg, K. Differential cardiopulmonary health impacts of local and long-range transport of wildfire smoke. Geohealth 2021, 5, e2020GH000330. [Google Scholar] [CrossRef]
- Tornevi, A.; Andersson, C.; Carvalho, A.C.; Langner, J.; Stenfors, N.; Forsberg, B. Respiratory health effects of wildfire smoke during summer of 2018 in the JämtlandHärjedalen region, Sweden. Int. J. Environ. Res. Public Health 2021, 18, 6987. [Google Scholar] [CrossRef]
- Malig, B.J.; Fairley, D.; Pearson, D.; Wu, X.; Ebisu, K.; Basu, R. Examining fine particulate matter and cause-specific morbidity during the 2017 North San Francisco Bay wildfires. Sci. Total Environ. 2021, 787, 147507. [Google Scholar] [CrossRef]
- Hahn, M.B.; Kuiper, G.; O’Dell, K.; Fischer, E.V.; Magzamen, S. Wildfire smoke Is associated with an increased risk of cardiorespiratory emergency department visits in Alaska. Geohealth 2021, 5, e2020GH000349. [Google Scholar] [CrossRef]
- Howard, C.; Rose, C.; Dodd, W.; Kohle, K.; Scott, C.; Scott, P.; Cunsolo, A.; Orbinski, J. SOS! Summer of Smoke: A retrospective cohort study examining the cardiorespiratory impacts of a severe and prolonged wildfire season in Canada’s high subarctic. BMJ Open 2021, 11, e037029. [Google Scholar] [CrossRef] [PubMed]
- Beyene, T.; Harvey, E.S.; Van Buskirk, J.; McDonald, V.M.; Jensen, M.E.; Horvat, J.C. ‘Breathing fire’: Impact of prolonged bushfire smoke exposure in people with severe asthma. Int. J. Environ. Res. Public Health 2022, 19, 7419. [Google Scholar] [CrossRef] [PubMed]
- Heaney, A.; Stowell, J.D.; Liu, J.C.; Basu, R.; Marlier, M.; Kinney, P. Impacts of fine particulate matter from wildfire smoke on respiratory and cardiovascular health in California. Geohealth 2022, 6, e2021GH000578. [Google Scholar] [CrossRef]
- Moore, L.E.; Oliveira, A.; Zhang, R.; Behjat, L.; Hicks, A. Impacts of wildfire smoke and air pollution on a pediatric population with asthma: A population-based study. Int. J. Environ. Res. Public Health 2023, 20, 1937. [Google Scholar] [CrossRef]
- Cherry, N.; Barrie, J.R.; Beach, J.; Galarneau, J.M.; Mhonde, T.; Wong, E. Respiratory outcomes of firefighter exposures in the Fort McMurray fire: A cohort study from Alberta Canada. J. Occup. Environ. Med. 2021, 63, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Gianniou, N.; Giannakopoulou, C.; Dima, E.; Kardara, M.; Katsaounou, P.; Tsakatikas, A. Acute effects of smoke exposure on airway and systemic inflammation in forest firefighters. J. Asthma Allergy 2018, 11, 81–88. [Google Scholar] [CrossRef]
- Gianniou, N.; Katsaounou, P.; Dima, E.; Giannakopoulou, C.; Kardara, M.; Saltagianni, V. Prolonged occupational exposure leads to allergic airway sensitization and chronic airway and systemic inflammation in professional firefighters. Respir. Med. 2016, 118, 7. [Google Scholar] [CrossRef]
- O’Dell, K.; Bilsback, K.; Ford, B.; Martenies, S.E.; Magzamen, S.; Fischer, E.V.; Pierce, J.R. Estimated mortality and morbidity attributable to smoke plumes in the United States: Not just a western US Problem. Geohealth 2021, 5, e2021GH000457. [Google Scholar] [CrossRef]
- Holm, S.M.; Miller, M.D.; Balmes, J.R. Heath effects of wildfire smoke in children and public health tools: A narrative review. J. Expos. Sci. Environ. Epidemiol. 2021, 31, 1–20. [Google Scholar] [CrossRef]
- Noah, T.L.; Worden, C.P.; Rebuli, M.E.; Jaspers, I. The Effects of Wildfire Smoke on Asthma and Allergy. Curr. Allergy Asthma Rep. 2023, 23, 375–387. [Google Scholar] [CrossRef]
- Dhingra, R.; Keeler, C.; Staley, B.S.; Jardel, H.V.; Ward-Caviness, C.; Rebuli, M.E. Wildfire smoke exposure and early childhood respiratory health: A study of prescription claims data. Environ. Health 2023, 22, 48. [Google Scholar] [CrossRef] [PubMed]
- Doubleday, A.; Sheppard, L.; Austin, E.; Busch Isaksen, T. Wildfire smoke exposure and emergency department visits in Washington State. Environ. Res. Health 2023, 1, 025006. [Google Scholar] [CrossRef]
- Henry, S.; Ospina, M.B.; Dennett, L.; Hicks, A. Assessing the Risk of Respiratory-Related Healthcare Visits Associated with Wildfire Smoke Exposure in Children 0–18 Years Old: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 8799. [Google Scholar] [CrossRef]
- Wilgus, M.L.; Merchant, M. Clearing the Air: Understanding the Impact of Wildfire Smoke on Asthma and COPD. Healthcare 2024, 12, 307. [Google Scholar] [CrossRef]
- Gallanter, T.; Bozeman, W.P. Firefighter illnesses and injuries at a major fire disaster. Prehosp. Emerg. Care 2002, 6, 22–26. [Google Scholar] [CrossRef]
- Duclos, P.; Sanderson, L.M.; Lipsett, M. The 1987 forest fire disaster in California: Assessment of emergency room visits. Arch. Environ. Health 1990, 45, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Vicedo-Cabrera, A.M.; Esplugues, A.; Iñíguez, C.; Estarlich, M.; Ballester, F. Health effects of the 2012 Valencia (Spain) wildfires on children in a cohort study. Environ. Geochem. Health 2016, 38, 703–712. [Google Scholar] [CrossRef]
- Fadadu, R.P.; Grimes, B.; Jewell, N.P.; Vargo, J.; Young, A.T.; Abuabara, K. Association of wildfire air pollution and health care use for atopic dermatitis and itch. JAMA Dermatol. 2021, 157, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Kamil, R.J.; London, N.R.; Lee, S.E.; Sidhaye, V.K.; Biswal, S.; Lane, A.P.; Pinto, J.M.; Ramanathan, M., Jr. Long-term exposure to particulate matter air pollution and chronic rhinosinusitis in nonallergic patients. Am. J. Respir. Crit. Care Med. 2021, 204, 859–862. [Google Scholar] [CrossRef]
- Padhye, L.V.; Kish, J.L.; Batra, P.S.; Miller, G.E.; Mahdavinia, M. The impact of levels of particulate matter with an aerodynamic diameter smaller than 2.5 μm on the nasal microbiota in chronic rhinosinusitis and healthy individuals. Ann. Allergy Asthma Immunol. 2021, 126, 195–197. [Google Scholar] [CrossRef]
- Patel, T.R.; Tajudeen, B.A.; Brown, H.; Gattuso, P.; LoSavio, P.; Papagiannopoulos, P.; Batra, P.S.; Mahdavinia, M. Association of air pollutant exposure and sinonasal histopathology findings in chronic rhinosinusitis. Am. J. Rhinol. Allergy 2021, 35, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Shen, S.; Deng, Y.; Wang, C.; Zhang, L. Air pollution exposure affects severity and cellular endotype of chronic rhinosinusitis with nasal polyps. Laryngoscope 2022, 132, 2103–2110. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y. Assessing the long-term impacts of wildfire smoke on human health: Recommendations for future research. Environ. Res. Lett. 2022, 17, 024012. [Google Scholar]
- McDonald, J.D. Wildfire smoke and immune system function: What we know and what we need to learn. J. Environ. Health 2021, 84, 22–30. [Google Scholar]
- Bourgeois, M. Evaluating and developing strategies to protect at-risk populations from wildfire smoke: A systematic review. Environ. Res. Lett. 2022, 17, 074027. [Google Scholar]
| Study [Reference] | Population and Location | Exposure Assessment | Outcome | Comments |
|---|---|---|---|---|
| Hutchinson et al. [60] | October 2007 fire complex, Medi-Cal beneficiaries, San Diego County | Spatiotemporal model using wildland fire emission system and atmospheric dispersion | Hospital admissions, outpatient visits | 243% increase in asthma diagnosis for age 0–1 yr |
| DeFlorio-Barker et al. [61] | Hospitalized adults ≥ 65 yr, all US counties within 200 km of large wildfires 2008–2010 (asthma admissions, Medicare database) | Fixed monitor data, adjusted for “smoke” days from wildfires | Hospital admissions | Increased asthma risk |
| Stowell JD et al. [62] | Colorado 2011–2014 fire seasons (May–August) | Ground PM2.5 from EPA monitors, plus high-resolution satellite optical density data for WFS | ED and hospital admissions | Similar asthma results for adults and children |
| Reid et al. [63] | Northern California, zip codes exposed to June–July 2008 wildfires | Spatiotemporal model, fixed monitors, machine learning algorithm | ED visits and hospital admissions | Unlike PM2.5, O3 effect was not significant in the multivariate model |
| Lipner et al. [64] | Pediatric asthma patients at National Jewish Health (Western U.S.) 2012–2015 | Retrospective; assessed local WFS-related PM2.5 during clinic visits | Asthma symptom score, PFT during routine (not sick) clinic visits | Assessed non-urgent visits, unlike all other studies |
| Gan et al. [65] | 2013 Oregon wildfire season; asthma claims Time-stratified, case-crossover design | Blended model of in situ monitoring, chemical transport models and satellite-based data | Asthma healthcare utilization (insurance claims) | Similar results for office visits and refills of rescue inhalers |
| Kiser et al. [66] | Reno, NV 2013–2018; data from a regional health system | Local fixed monitors for PM2.5, with dates when WFS was present | ED or urgent care visits | Similar outcome to DeFlorio-Barker [41] |
| Magzamen et al. [67] | Colorado Front Range area, 2012 and 2015 Time-stratified, case-crossover analysis | Surface monitors for Western US, plus satellite-based smoke plume estimates | Hospital admissions | This relationship was seen for “long-range transport” WFS events, but not local wildfires |
| Tornevi et al. [68] | Sweden, 2018 wildfire events in Jamtland Harjedalen region | Modeled WFS PM2.5 exposures using MATCH model (complex meteorological and atmospheric chemical data) | Clinic visits | - |
| Malig et al. [69] | San Francisco Bay area, October 2017 wildfires | County-level monitoring avg PM2.5 during wildfire period compared to adjacent periods | ED visits and hospital admissions | - |
| Hahn et al. [70] | Alaska (3 cities) during 2015–2019 wildfire seasons | Ground-based monitors and satellite-based smoke plume estimates | ED visits | Similar for >65 year-olds, Native Alaskans |
| Howard et al. [71] | Northwest Territories (Canada), summer 2014 prolonged, severe wildfire period | Compared WFS period to before and after periods | Hospital admissions, ED visits; SABA prescriptions | Median 24-h mean PM2.5 fivefold higher in the summer of 2014 compared with 2012, 2013 and 2015 (median = 30.8 ìg/m3), with mean peaking at 320.3 ìg/m3. Inuit more affected |
| Beyene et al. [72] | Eastern Australia asthma registry, 2019–2020 bushfires | 24 h avg PM2.5 at fixed monitoring stations; satellite imagery for bushfire component | Self-reported symptoms | Mean PM2.5 exposure 32.5 ìg/m3 on bushfire days |
| Heaney et al. [73] | California, 2004–2009 wildfire seasons | Goddard Earth-Observing System (GEOS-Chem), all-source vs. without wildfire-specific PM2.5 | Unscheduled hospital visits for asthma and other conditions | Largest effect for 0–5 year-old subjects |
| Moore et al. [74] | Calgary, Canada 2010–2021 | Ground-level monitors with WFS dates estimated from satellite images | Health insurance claims for asthma exacerbation in children | Exacerbations significantly reduced during periods of COVID-19 healthcare precautions |
| Blando et al. [11] | Northeastern North Carolina, patients at allergy clinic, studied before, during and after Dismal Swap peat bog fires in 2008 and 2011 | Wind blowing from fire area toward community as proxy for exposure | Peak flow | Study conducted 1 year after exposures |
| Cherry et al. [75] | Fort McMurray fire in Alberta, Canada 2016, firefighters and controls | Exposure to fire-related PM2.5 from Alberta Environment monitoring stations and satellite imagery | Spirometry and asthma consultation | Individuals with ongoing symptoms also had a higher occurrence of positive methacholine challenge and bronchial wall thickening (OR 4.35; 95% CI 1.11–17.12. Lower diffusion capacity also related to increased exposure |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frumento, D.; Țãlu, Ș. Effects of Wildfire Exposure on the Human Immune System. Fire 2024, 7, 469. https://doi.org/10.3390/fire7120469
Frumento D, Țãlu Ș. Effects of Wildfire Exposure on the Human Immune System. Fire. 2024; 7(12):469. https://doi.org/10.3390/fire7120469
Chicago/Turabian StyleFrumento, Davide, and Ștefan Țãlu. 2024. "Effects of Wildfire Exposure on the Human Immune System" Fire 7, no. 12: 469. https://doi.org/10.3390/fire7120469
APA StyleFrumento, D., & Țãlu, Ș. (2024). Effects of Wildfire Exposure on the Human Immune System. Fire, 7(12), 469. https://doi.org/10.3390/fire7120469







