1. Introduction
Posttraumatic stress disorder (PTSD) is a common reaction to traumatic events. PTSD becomes persistent when individuals process the trauma that leads to a sense of serious, current threat. PTSD is an anxiety disorder which occurs after exposure to stressful events that are beyond usual human experience. Depending on the time of onset and duration of symptoms after exposure to a traumatic event, PTSD is categorized according to the Diagnostic and Statistical Manual (DSM-5) into the following: acute PTSD (symptoms last less than 3 months) and chronic PTSD (symptoms last for more than 3 months) [
1]. PTSD after recovery from addiction to drugs is related to chronic trauma and psychopathology. However, the relationship of drug abuse with PTSD is double sided, people with PTSD report more intense drug abuse and seem to relapse faster than other people without PTSD. Most individuals, who have suffered from traumatic experiences eventually overcome depression and anxiety but when PTSD develops, it is very difficult for the symptoms to vanish and they might last for months or years after the event [
2].
Research has demonstrated that most harmful addictions are underlined by trauma. Traumatic childhood or early adolescence experiences can be a cause of addictions and rarely is there no association between drug addiction and trauma. In particular, childhood trauma can have a long-lasting effect if not resolved. Overtime, a sense of fear and helplessness lays down the foundation for further traumas in adulthood. The person who abuses drugs feels relieved quickly because the drug releases dopamine and blocks out the pain caused by trauma; this behavior is repeated and soon a neural pathway is laid down [
3]. Upon the consolidation of this behavior, the user feels more traumatized because of this process, which is a vicious circle, and then uses more drugs to numb the pain From then on, the user has become addicted [
4].The majority of people addicted to drugs exhibit significant symptoms related to sexual abuse, assault or contact with death, which can cause chronic PTSD. Therefore, the coexistence of traumas and other mental disorders makes the treatment of these people more complicated [
5].
Addiction is a chronic relapsing disorder with compulsive drug seeking, constant use despite disastrous long-lasting changes in the brain. Addiction is the most severe of all use disorders; it is considered both as a mental illness and a complex brain disorder; however, addiction is not a specific disorder in the Diagnostic and Statistical Manual-5th edition (DSM-5). The new manual describes this disorder as a problematic pattern of substance use, leading to significant impairment and distress with 11 diagnostic criteria, occurring within a period of 12 months [
6]. Women despite using drugs at lower levels than men, typically progress to addiction more quickly than men. Also, women experience the consequences of drug addiction sooner and more intensely than their male counterparts [
7].
On the other hand, a traumatic childbirth experience is usually associated with psychological impairments that can lead to a postpartum PTSD. Childbirth experience as a traumatic event can overshadow the mother–child attachment, the partnership, the general adaptability, and negatively influence the future decision to have another child [
8].Many studies have shown that different risk factors contribute to the development of PTSD after childbirth, including obstetric procedures, anxiety, negative aspects, sense of control, and social support [
9]. Some studies suggest that the unpleasant experiences during pregnancy, obstetric interventions, cesarean section, and previous psychiatric disorders could play a role in postpartum PTSD [
10]. Other research has indicated that childhood sexual abuse or other history of trauma, such as addiction to drugs, might be strong risk factors for high stress levels in the postpartum period. If these risk factors are identified early in pregnancy, they could be prevented by support from health care providers [
11]. Women with a drug abuse record may have faced criminal justice procedures and they are a major public health problem because of their disease. In these cases, health professionals must be particularly aware [
12].
The co-occurrence of PTSD after drug abuse with postpartum psychological factors can cause significant problems to postpartum women and to their children. Specifically, there is evidence to suggest that PTSD is more common among pregnant and postpartum women who have used in the past or are currently using substances. There is an urgent need for this population to address their trauma as practically there is a big deficit in health services and their accessibility to them [
13].
2. Case Presentation Section
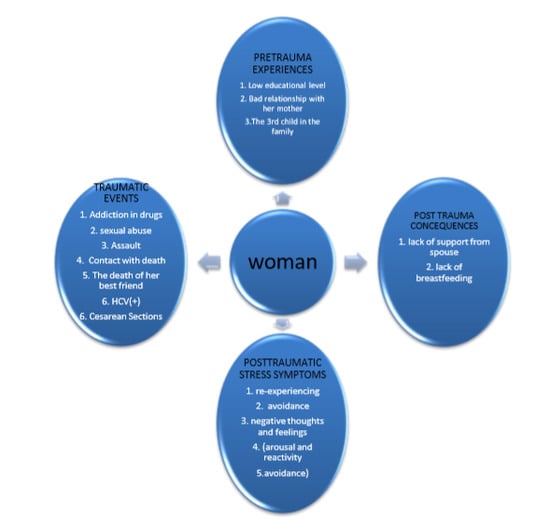
The 37-year-old, well-dressed woman was stressful and restless but very friendly with the interviewer. It took place on day 2 postpartum after an elective cesarean section due to her two previous cesarean sections delivering a healthy boy. Throughout the interview, she held her baby boy in her arms, but did not breastfeed. She stated that she had not breastfed her other two children (girls). She had hepatitis C and had not been properly treated, something she was upset about. The woman described her cesarean section as traumatic but she did not meet criterion A. When asked by the researcher to complete the traumatic Life Events Checklist (LEC-5) she showed great willingness to talk about her life. The woman was not coherent in her speech, becoming lost with her memories when she began to recall her addiction to drugs, focusing on the death of her best friend who had died in her arms.
She is the third child of a family of five, she has got two brothers and her parents divorced when she was 12 but she does not express emotion when she talks about it. After that she lived with her mother and her brothers; she was a good student and dreamed of the future. She was about 17 when she started using drugs and abandoned school and her home only to start living with marginalized drug users groups. She was able to maintain a linear train of thought with no irrational or disorganization connections when expressing her traumatic experiences. She described her drug hallucinations, her many sexual abuses, an assault with weapon and her contact with death frequently but her thought content centered on the death of her best friend. She talked about her with deep emotions and described that this friend had a role of a mother figure in their relationship (her friend had recently lost her baby girl).
Her friend’s death was the reason why she decided to leave drug addiction behind (after 4 years) and start a new life in her mother’s old cottage house. She described the horror of withdrawal symptoms and her fight with her desire to return to drug abuse. After a year free of drugs and substitutes she met a man in the local community who accepted her; they got married and had two children. Up to her third pregnancy, there was no problem in her life, in her pregnancies and her postpartum periods. During the third pregnancy she began feeling lonely and unhappy, while her spouse made her feel guilty of her past life. He discouraged her from having Hepatitis C treatment because that would mean being hospitalized and thus, be away from her family. She now felt tired of living in the village, but was afraid to return to the big city where she was born and raised. She was also afraid to meet her old friends, but seemed more afraid of herself. At this point the woman reminded the interviewer that her friend was the most important person in her life. Up to then, she had never visited a psychiatrist or a psychologist.
2.1. Data and Measures
The ethics committee of University Hospital of Larisa approved the study: 18838/8 May 2019. We obtained written informed consent from the postpartum woman after comprehensive explanation of the procedure involved. The examination was done in 2 phases: (a) on 2nd day postpartum and (b) on the 6th week postpartum.
2.1.1. Medical/Demographic Questionnaire
A researcher-made customized form included maternal, neonatal, mental, and social characteristics of the postpartum women.
2.1.2. LEC-5 (DSM-5)
The Life Events Checklist is a self-report measure, designed from the National Center of PTSD to screen traumatic events in a person’s life-time. LEC-5 assesses exposure to 16 events known to result in PTSD or distress and one additional item assessing any other stressful event not included in the first 16 items. Respondents indicate varying levels of exposure traumatic events included in a 6-point scale and they may endorse multiple levels of exposure to the same traumatic life event [
14].
2.1.3. PCL-5 (DSM-5)
The PCL-5 is a self-report measure which assesses the 20 symptoms of PTSD. The meter has a variety of purposes, including making a provisional diagnosis of PTSD, screening individuals for PTSD, and monitoring symptoms during and after treatment. PCL-5 can be completed by participants as part of a research study. The PCL-5 has excellent psychometric properties, high internal consistency, and adequate convergent validity. In this case study both scoring modes were used; the sum of the 20 questions score (with a cut point of 33) and the coverage of the diagnostic criteria (A, B, C, D, E) [
15,
16].
2.1.4. Criterion A (DSM-5)
The stressor criterion A specifies that a person has been exposed to a traumatic event involving actual or threatened death or injury or sexual violence. The indirect exposure includes learning about the accidental or violent death or sexual violence to a loved one. A repeat in directed exposure (as a part of professional responsibilities) is considered a traumatic experience [
17].
2.1.5. Criterion A and PCL-5-AC
The stressor Criterion A which detects a mother’s stress before, during, and after cesarean section includes questions about the sense of loss to her life and her baby’s life. Furthermore, questions about any complications after cesarean section in either or each of them are included. PCL-5-AC includes 20 PTSD screening questions tailored for women after cesarean section.
2.2. Mental State Examination
A woman after completing 8 traumatic life events in LEC-5 in the 2ndpostpartum day was given Criterion A to complete for any event, and then answered the 8 Posttraumatic Checklists (PCL-5). The woman was asked to rate how bothered she had been by each of 20 items in the past month on a 5-point scale ranging from 0–4.
The provisional diagnosis was determined in 2 ways. (A) All items were summed to provide a total severity score (range 0–80) with a cut-point score of 33. (B) Treating each item rate as 2 = moderately, or higher as PTSD symptom, then according to the DSM-5 diagnostic rule which requires at least: 1 Criterion B item (1–5 question), 1 Criterion C item (6–7 questions), 2 Criterion D items (8–14 questions), and 2 Criterion E items (15–20 questions) [
15].
In all 8 events that took place between 7 and 15 years ago, the woman had a provisional diagnosis of chronic PTSD in both methods [
18]. The score of all scales varied between 48 and 69. The highest score was exposure to death of her best friend (
Figure 1). Furthermore, the woman met all the diagnostic criteria of PTSD (A, B, C, D, and E). These scores suggested that the woman may benefit from PTSD treatment.
Follow up
After 6 weeks the woman answered via telephone, 20 more questions of adapted Criterion A and PCL-5 women after cesarean, to diagnose possible PTSD-After Cesarean (AC) [
19]. The woman was told again to answer if she felt the same symptoms regarding her cesarean section during the last month but, although the PCL-5 score was 80 (the highest score), she did not meet all PTSD criteria; the stressor Criterion A was not satisfied (
Figure 2).The third cesarean section was characterized as a traumatic experience by the woman without the stress of losing a life or complications; however, these severe PTSD symptoms caused significant distress and had an impact on her social life and her baby’s care. At this point the woman was referred to visit a psychiatrist to determine the symptoms and proceed to appropriate treatment.
3. Discussion
This woman is a typical example of the effects that follow traumatic addiction experiences. She was suffering from chronic PTSD which revived during her third postpartum period due to the fact that suitable circumstances were created. It is very common for people having recovered from PTSD to re-experience emotions from past traumas particularly when triggered. These feelings are often disproportionate to the present status and are known as emotional flashbacks.
The above chronic PTSD case describes the recurrent trauma of a woman having recovered from addiction to drugs and the cumulative effect of these traumas on the appearance of postpartum PTSD [
20].This new threat, which is the expression of the past trauma that was handled with unsuitable strategies, is triggered by the experience of motherhood reinforced and perpetuates the emotional pain. The appearance of PTSD in the third postpartum period coincided with the emotional absence of the spouse leading to emotions of inadequacy and inferiority towards him. In addition, the birth of the third child brought back memories of her own place inside the family causing stress. The serious health problem resulted in her refusal to breastfeed and was a constant reminder of her past addiction as well. Furthermore, the forced choice of living in the village was a social factor of her emotional isolation. The criticality of the problem was shown through the emotional armlock of the mother—friend search as an escape from stressful reality and eventually, triggering a new PTSD.
4. Conclusions
The absence of a family supportive system, the lack of breastfeeding, and a cesarean section are powerful factors of PTSD development. If there is additional untreated past PTSD, the possibility of its reoccurrence exists due to a new stressful experience. Addiction to drugs is accompanied by adverse situations and disorders which require psychological and psychiatric support for the smooth inclusion of the individual to society. A woman is a biopsychosocial entity so, a biopsychosocial approach is essential in including all aspects of the woman’s history in a meaningful way in order to provide substantial help. The appropriate medical approach during the perinatal period and proper obstetric care are factors of essential importance for the mental health of the mother and the infant.