Abstract
Here we describe a rare case of a 48-year-old woman with a previous history of malignant melanoma (pT2a pathological stage, IB clinical stage) occurring about five years previously. She complained of abdominal pain and pelvic discomfort, diagnosed as a consequence of a bilateral ovarian solid masses completely occupying the recto-uterine space. She underwent laparotomy surgery with total hysterectomy and bilateral salpingo-oophorectomy. Gross examination of the excised material revealed an unusual grey-black bilateral ovarian tumor; a histopathological diagnosis of ovarian bilateral metastatic melanoma was made. Imaging study (CT/MRI) did not reveal metastasis in other zones of the body. Melanoma metastasis usually affects the skin, liver, brain and lungs, and rarely gynecological localizations. On the other hand, most bilateral ovarian tumors are comprised of serous carcinoma, mature teratoma and gastrointestinal carcinoma metastasis. Exceptionally, primary ovarian melanoma may arise in mature ovarian cystic teratomas.
A 48-year-old woman was referred to our hospital with a previous history of melanoma occurring about five years previously (2015). At the time, she underwent surgery with a wide excision of a skin lesion (3 × 2.5 cm) in the left lumbar region, which had developed a few months earlier. It was a malignant cutaneous epithelioid cell melanoma, with a Breslow thickness of 1.5 mm (pT2a) with free surgical resection margins and a negative sentinel lymph node biopsy. About two years later (2017) she developed satellitosis within 2 cm of the former surgical excision in the region of the left flank. From this point on, the patient entered clinical stage III and, according to guidelines, adjuvant chemotherapy with Dacarbazine was started.
She underwent left axillary lymphadenectomy which showed metastases in 3 lymph nodes.
After a further three years (2020), she complained of abdominal pain and pelvic discomfort. She had ascites and bilateral ovarian solid masses completely occupying the recto-uterine space. Magnetic resonance imaging (MRI) and whole-body computed tomography (CT) revealed only enlarged pelvic lymph nodes. In addition, the patient was subjected to PET 5FDG which indicated pelvic uptake. Among tumor markers, Cancer Antigen 125 (CA125) was 247 IU/L while levels of carcinoembryonic antigen (CEA), alpha feto-protein (AFP) and human chorionic gonadotrophin (beta HCG) were normal. At this point, a differential diagnosis was made between a primary neoplastic lesion of the ovary or a repetition of melanoma. The absence of elevated tumor markers appeared very strange.
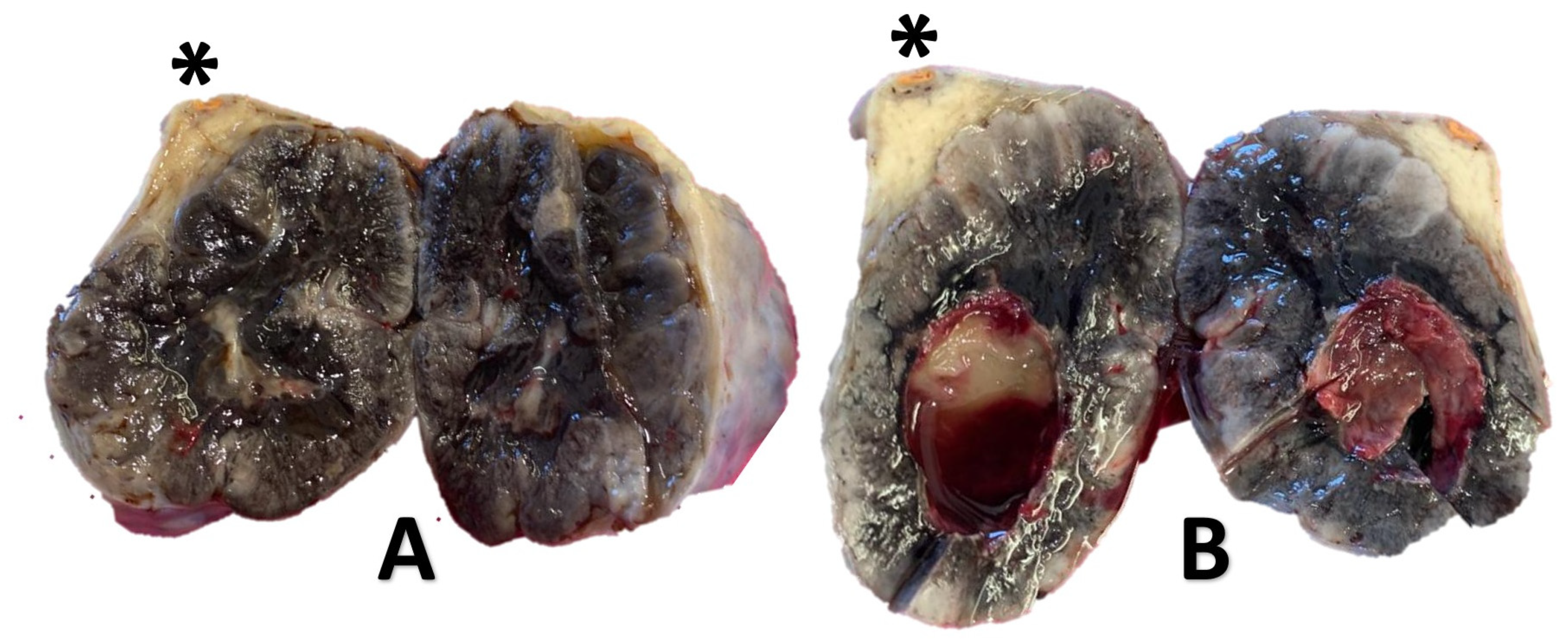
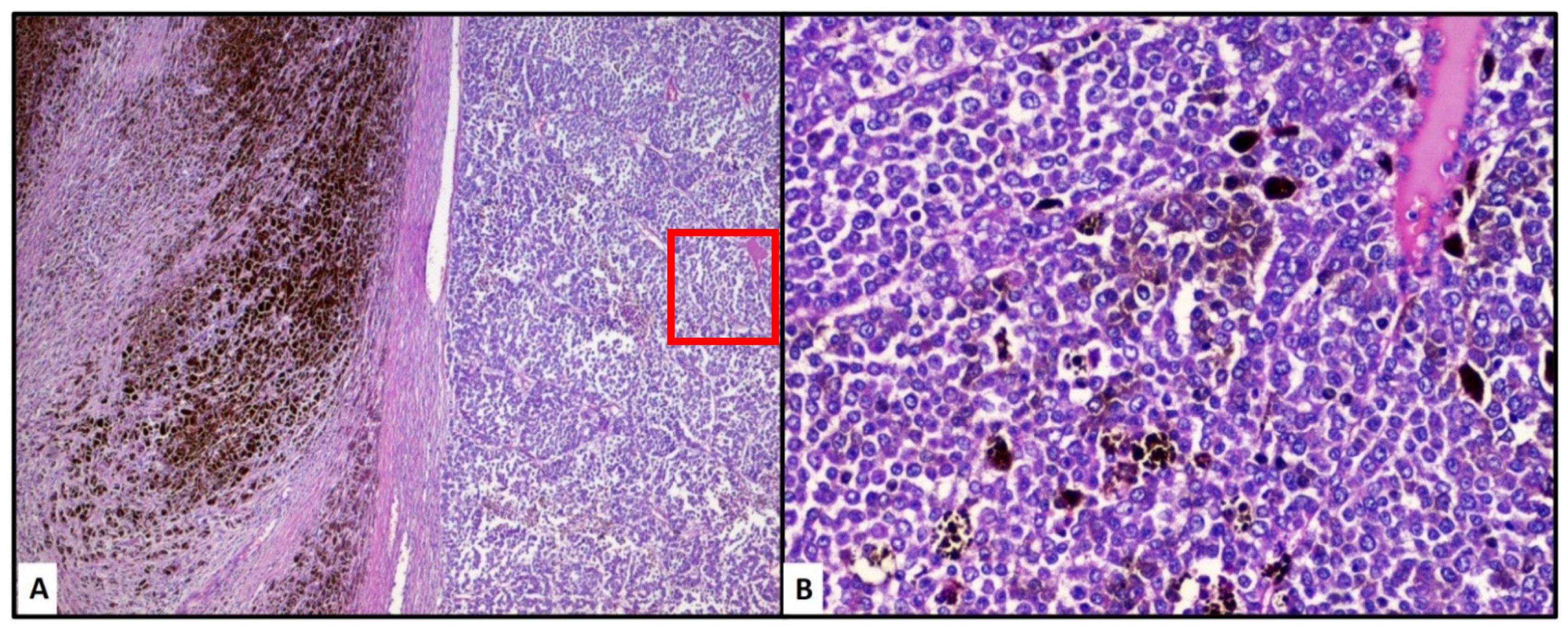
She underwent laparotomy surgery with total hysterectomy and bilateral salpingo-oophorectomy, omentectomy and peritoneal biopsies. Gross examination of the excised material revealed a grey-black bilateral ovarian tumor, with largest diameters of 4.5 cm (right ovary, Figure 1A) and 7.3 cm (left ovary, Figure 1B), and they weighed 170 g and 210 g respectively. The external surface was smooth and intact. The cut surface showed tumoral mass with necrotic hemorrhagic foci, and the remnant of normal ovarian parenchyma was barely visible (Figure 1, *). The uterus appeared normal. There were no peritoneal nodular locations in infracolic-omentum and on the peritoneal surface. Histology and immunohistochemistry showed epithelioid cells, with occasional nuclear pseudoinclusion and strongly pigmented [Figure 2A,B]. The cells were positive for Melan-A, HMB-45, S-100, and had no staining for cytokeratin and inhibin. Therefore, a diagnosis of ovarian bilateral metastatic melanoma was made. Molecular analyses were performed if paraffin tissue sections of both the primary lesion and the secondary metastatic ovarian lesion and the BRAFV600E mutation were found in last sample.
Figure 1.
Gross examination of metastatic ovaries (right, A and left, B), almost completely replaced by a localization of melanotic melanoma which occupies almost the entire organ and which has undergone necrotic cystic cavitation inside it. Asterisk (*) indicates remaining healthy ovarian parenchyma.
Figure 2.
The neoplastic lesion was characterized by a heterogeneous distribution of melanic deposits (Hematoxylin-Eosin, (A): original magnification 40×). At higher magnification, the neoplastic cells showed a typical epithelioid morphology (Hematoxylin-Eosin, (B): 200×).
As a result, the patient underwent immunotherapy with Ipilimumab and Nivolumab, and no progression of the disease was observed at a follow-up 6 months later.
Melanoma usually affects the skin, mucosal membrane and ocular choroids with frequent sites of metastasis being the skin, brain and lungs, and rarely gynecological localizations. These are mostly endometrials [1,2]. Secondary breast involvement remains exceptional [3]. Rare cases of ovarian metastases of malignant melanoma have been reported in the Literature [3,4,5,6,7]. The distinction between a primary ovarian malignant melanoma from a metastatic tumor must be made. Unilateral metastatic ovarian malignant melanomas are more common than primary ovarian malignant melanomas [1,2].
For example, in a study of 20 cases [8] of metastatic ovarian melanoma, 12 patients had a history of cutaneous melanoma, and more than half died shortly after the diagnosis of systemic disease. On the other hand, a bilateral localization to the ovaries of melanoma has also been described [9] in a patient with an occult primary lesion. This makes it particularly important to adequately reconstruct the clinical history. Moreover, primary ovarian melanoma may arise in mature ovarian cystic teratomas [6,10,11]. Available data suggest that prognosis of metastatic ovary malignant melanoma is pejorative (5% 5 year survival) [2,3]. The diagnosis of certainty is histological and immunohistochemical, with a typical expression of melanocytic markers [5].
In this brief report we have described a rare case of bilateral ovarian metastasis in a woman who, a few years earlier, had been diagnosed with primary cutaneous melanoma. Although it is established that melanoma can metastasize in any part of the body, metastases of the female genital tract are not a frequent occurrence, even less so when bilateral ovarian. It is important to keep in mind the possibility that a previous neoplasm may recur even after a few years and to keep in mind the polymorphic spectrum that melanoma is able to express.
Author Contributions
Conceptualization, G.C. and G.I.; methodology, F.A., L.R.; investigation, A.C.; data curation, G.C.; writing—original draft preparation, G.C. and G.I.; writing-review and editing, G.C.; supervision, G.I. and G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study, due to the description of a single clinical case.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Sbitti, Y.; Fadoukhair, Z.; Kadiri, H.; Oukabli, M.; Essaidi, I.; Kharmoum, S.; M’rabti, H.; Albouzidi, A.; Ichou, M.; Errihani, H. Diagnostic challenge for ovarian malignant melanoma in premenopausal women: Primary or metastatic? World J. Surg. Oncol. 2011, 9, 65. [Google Scholar] [CrossRef] [PubMed]
- Boscaino, A.; D’Antonio, A.; Orabona, P.; Tornillo, L.; Staibano, S.; De Rosa, G. Primary malignant melanoma of the ovary. Pathologica 1995, 87, 685–688. [Google Scholar] [PubMed]
- Mendel, A.; Terzibachian, J.J.; Aubin, F.; Malicenco, L.; Ramanah, R.; Riethmuller, D. Ovarian metastasis of a malignant melanoma: A case report. J. Gynecol. Obstet. Hum. Reprod. 2017, 46, 461–462. [Google Scholar] [CrossRef]
- Oliver, R.; Dasgupta, C.; Coker, A.; Al-Okati, D.; Weekes, A.R. Ovarian malignant melanoma: Unusual presentation of a solitary metastasis. Gynecol. Oncol. 2005, 99, 412–414. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.; Deavers, M.T.; Silva, E.G.; Malpica, A. Malignant melanoma involving the ovary: A clinicopathologic and immunohistochemical study of 23 cases. Am. J. Surg. Pathol. 2004, 28, 771–780. [Google Scholar] [CrossRef] [PubMed]
- Lengyel, K.; Young, F.; Kucukmetin, A.; Cresti, N.; Plummer, R.; Ralte, A.; O’Donnell, R.L. BRAF Wild-type, PTEN Mutant Malignant Uveal Melanoma Arising Within a Mature Ovarian Teratoma: A Case Report and Review of the Literature. Int. J. Gynecol. Pathol. 2020, 39, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Boespflug, A.; Combemale, P.; de la Fouchardiere, A.; Neidhardt, E.M. Metastatic melanoma of the ovary and circulating S100B. Eur. J. Dermatol. 2013, 23, 719–720. [Google Scholar] [CrossRef] [PubMed]
- Karateke, A.; Tuğ, N.; Sahin, D. Metastatic ovarian malignant melanoma with no obvious primary. J. Turk Ger. Gynecol. Assoc. 2011, 12, 181–182. [Google Scholar] [CrossRef]
- Fitzgibbons, P.L.; Martin, S.E.; Simmons, T.J. Malignant melanoma metastatic to the ovary. Am. J. Surg. Pathol. 1987, 11, 959–964. [Google Scholar] [CrossRef] [PubMed]
- Gök, N.D.; Yildiz, K.; Corakçi, A. Primary malignant melanoma of the ovary: Case report and review of the literature. Turk Patol. Derg. 2011, 27, 169–172. [Google Scholar]
- Zikry, J.; Korta, D.Z.; Chapman, L.W.; Linden, K.G. Melanoma arising in an ovarian cystic teratoma: A systematic review of presentation, treatment, and outcomes. Arch. Gynecol. Obstet. 2017, 296, 397–404. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).