AI-Driven Telerehabilitation: Benefits and Challenges of a Transformative Healthcare Approach
Abstract
1. Introduction
Rationale, Objective, and Theory Framework
2. Technology’s Role in Modern Telerehabilitation
Dual Edge of IoMT: Enhancing Care and Ensuring Security
3. The Role of Artificial Intelligence in Enhancing Telerehabilitation Outcomes
Meeting User Preferences: AI-Driven Customization in Remote Rehabilitation
4. Real-Time Adaptation and Model Transparency: Technical and Ethical Strategies in AI Telerehabilitation
Integrating AI into Healthcare Systems: EHRs and Telemedicine Platforms
5. Discussion
5.1. Navigating the Landscape of AI-Driven Telerehabilitation
5.2. Addressing Complexity and Ensuring Balance: Key Considerations for AI in Telerehabilitation
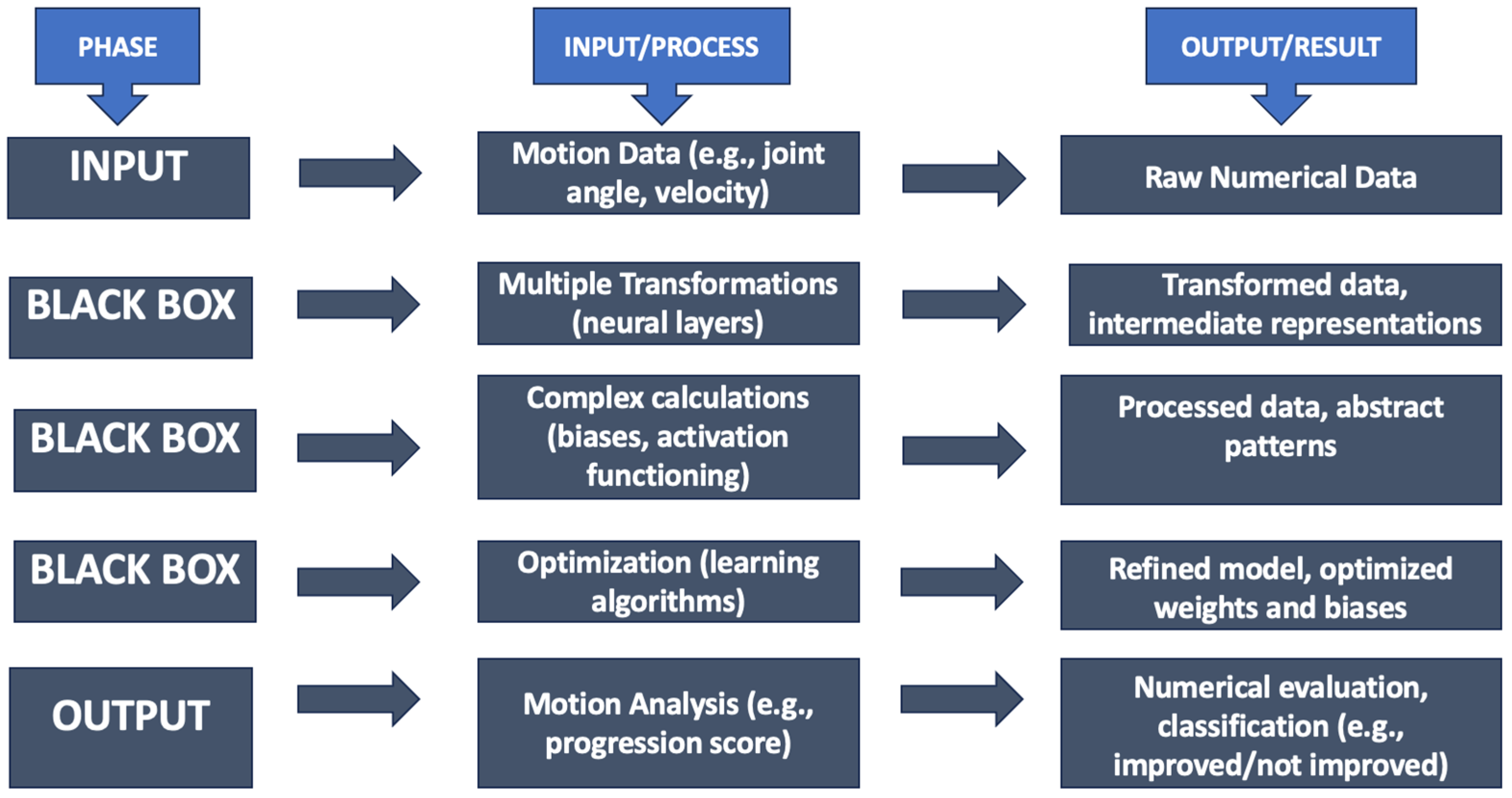
5.3. Illuminating the Black Box: Future Directions for Explainable AI in Telerehabilitation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alkatheiri, M.S. Artificial intelligence assisted improved human-computer interactions for computer systems. Comput. Electr. Eng. 2022, 101, 107950. [Google Scholar] [CrossRef]
- Bin Rashid, A.; Kausik, A.K. AI revolutionizing industries worldwide: A comprehensive overview of its diverse applications. Hybrid Adv. 2024, 7, 100277. [Google Scholar] [CrossRef]
- Akinola, S. Advancing healthcare with AI: Designing frameworks for diagnostics, personalized treatment, and enhanced efficiency. AIMS Med. Sci. 2024, 11, 248–264. [Google Scholar] [CrossRef]
- Brennan, D.M.; Mawson, S.; Brownsell, S. Telerehabilitation: Enabling the remote delivery of healthcare, rehabilitation, and self management. Stud. Health Technol. Inform. 2009, 145, 231–248. [Google Scholar] [CrossRef] [PubMed]
- Lanotte, F.; O’brien, M.K.; Jayaraman, A. AI in Rehabilitation Medicine: Opportunities and Challenges. Ann. Rehabil. Med. 2023, 47, 444–458. [Google Scholar] [CrossRef]
- McMaughan, D.J.; Oloruntoba, O.; Smith, M.L. Socioeconomic Status and Access to Healthcare: Interrelated Drivers for Healthy Aging. Front. Public Health 2020, 8, 231. [Google Scholar] [CrossRef]
- World Health Organization; United Nations Children’s Fund (UNICEF). Global Report on Assistive Technology; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Layton, N.; Borg, J. (Eds.) Global Perspectives on Assistive Technology: Proceedings of the GReAT Consultation 2019; World Health Organization: Geneva, Switzerland, 2019; Volume 1. [Google Scholar]
- National Institute of Dental and Craniofacial Research (US). Oral Health in America: Advances and Challenges; National Institute of Dental and Craniofacial Research: Bethesda, MD, USA, 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK578297/ (accessed on 16 December 2024).
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Health Care Services; Committee on Health Care Utilization and Adults with Disabilities. Health-Care Utilization as a Proxy in Disability Determination; National Academies Press: Washington, DC, USA, 2018. Available online: https://www.ncbi.nlm.nih.gov/books/NBK500097/ (accessed on 16 December 2024).
- Andrade, R.M.; Santana, B.G.; Schmidt, A.V.; Barsotti, C.E.; Baroni, M.P.; Saragiotto, B.T.; Ribeiro, A.P. Effect of traditional rehabilitation programme versus telerehabilitation in adolescents with idiopathic scoliosis during the COVID-19 pandemic: A cohort study. J. Rehabil. Med. 2024, 56, jrm5343. [Google Scholar] [CrossRef]
- Zhang, Y.; Jin, Q.; Ji, C.; Yuan, P.; Chen, L. Innovative Telerehabilitation Enhanced Care Programme (ITECP) in young and middle-aged patients with haemorrhagic stroke to improve exercise adherence: Protocol of a multicentre randomised controlled trial. BMJ Open 2023, 13, e072268. [Google Scholar] [CrossRef]
- Serrano, L.P.; Maita, K.C.; Avila, F.R.; A Torres-Guzman, R.; Garcia, J.P.; Eldaly, A.S.; Haider, C.R.; Felton, C.L.; Paulson, M.R.; Maniaci, M.J.; et al. Benefits and Challenges of Remote Patient Monitoring as Perceived by Health Care Practitioners: A Systematic Review. Perm. J. 2023, 27, 100–111. [Google Scholar] [CrossRef]
- Thomas, E.E.; Taylor, M.L.; Banbury, A.; Snoswell, C.L.; Haydon, H.M.; Rejas, V.M.G.; Smith, A.C.; Caffery, L.J. Factors influencing the effectiveness of remote patient monitoring interventions: A realist review. BMJ Open 2021, 11, e051844. [Google Scholar] [CrossRef]
- Tan, S.Y.; Sumner, J.; Wang, Y.; Yip, A.W. A systematic review of the impacts of remote patient monitoring (RPM) interventions on safety, adherence, quality-of-life and cost-related outcomes. NPJ Digit. Med. 2024, 7, 192. [Google Scholar] [CrossRef]
- Shajari, S.; Kuruvinashetti, K.; Komeili, A.; Sundararaj, U. The Emergence of AI-Based Wearable Sensors for Digital Health Technology: A Review. Sensors 2023, 23, 9498. [Google Scholar] [CrossRef] [PubMed]
- Sabry, F.; Eltaras, T.; Labda, W.; Alzoubi, K.; Malluhi, Q. Machine Learning for Healthcare Wearable Devices: The Big Picture. J. Healthc. Eng. 2022, 2022, 4653923. [Google Scholar] [CrossRef] [PubMed]
- Rahimi, B.; Nadri, H.; Afshar, H.L.; Timpka, T. A Systematic Review of the Technology Acceptance Model in Health Informatics. Appl. Clin. Inform. 2018, 9, 604–634. [Google Scholar] [CrossRef] [PubMed]
- Santana, M.J.; Manalili, K.; Jolley, R.J.; Zelinsky, S.; Quan, H.; Lu, M. How to practice person-centred care: A conceptual framework. Health Expect. 2018, 21, 429–440. [Google Scholar] [CrossRef]
- Bougea, A. Application of Wearable Sensors in Parkinson’s Disease: State of the Art. J. Sens. Actuator Netw. 2025, 14, 23. [Google Scholar] [CrossRef]
- Jolly, A.; Pandey, V.; Sahni, M.; Leon-Castro, E.; Perez-Arellano, L.A. Modern Smart Gadgets and Wearables for Diagnosis and Management of Stress, Wellness, and Anxiety: A Comprehensive Review. Healthcare 2025, 13, 411. [Google Scholar] [CrossRef]
- George, A.S.; Shahul, A.; George, A.S. Wearable sensors: A new way to track health and wellness. Partn. Univers. Int. Innov. J. 2023, 1, 15–34. [Google Scholar] [CrossRef]
- Bateni, H.; Carruthers, J.; Mohan, R.; Pishva, S. Use of Virtual Reality in Physical Therapy as an Intervention and Diagnostic Tool. Rehabil. Res. Pract. 2024, 2024, 1122286. [Google Scholar] [CrossRef]
- Kouijzer, M.M.T.E.; Kip, H.; Bouman, Y.H.A.; Kelders, S.M. Implementation of virtual reality in healthcare: A scoping review on the implementation process of virtual reality in various healthcare settings. Implement. Sci. Commun. 2023, 4, 67. [Google Scholar] [CrossRef]
- Oluwaseyi, J.; Olanite, E. Patient Engagement: AI Tools That Enhance Patient Communication, Education, and Adherence to Treatment Plans. 2024. Available online: https://www.researchgate.net/publication/384774304_Patient_Engagement_AI_tools_that_enhance_patient_communication_education_and_adherence_to_treatment_plans (accessed on 16 December 2024).
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 100117. [Google Scholar] [CrossRef]
- Wickramasinghe, N.; Andargoli, A. The enabling role of 5G in the digital transformation of healthcare. In Digitalization and the Transformation of the Healthcare Sector; IGI Global: Hershey, PA, USA, 2024. [Google Scholar] [CrossRef]
- Osama, M.; Ateya, A.A.; Sayed, M.S.; Hammad, M.; Pławiak, P.; El-Latif, A.A.A.; Elsayed, R.A. Internet of Medical Things and Healthcare 4.0: Trends, Requirements, Challenges, and Research Directions. Sensors 2023, 23, 7435. [Google Scholar] [CrossRef] [PubMed]
- Georgiou, K.E.; Georgiou, E.; Satava, R.M. 5G Use in Healthcare: The Future is Present. JSLS J. Soc. Laparosc. Robot. Surg. 2021, 25, e2021.00064. [Google Scholar] [CrossRef]
- Yeh, S.-J.; Wang, Y.-C.; Fang, W.-C.; Huang, S.-C.; Yang, Y.-S. Effectiveness of Powered Hand Exoskeleton on Upper Extremity Function in People with Chronic Stroke. Actuators 2025, 14, 67. [Google Scholar] [CrossRef]
- Calafiore, D.; Negrini, F.; Tottoli, N.; Ferraro, F.; Ozyemisci-Taskiran, O.; de Sire, A. Efficacy of robotic exoskeleton for gait rehabilitation in patients with subacute stroke: A systematic review. Eur. J. Phys. Rehabil. Med. 2022, 58, 1–8. [Google Scholar] [CrossRef]
- Alturki, B.; Abu Al-Haija, Q.; Alsemmeari, R.A.; Alsulami, A.A.; Alqahtani, A.; Alghamdi, B.M.; Bakhsh, S.T.; Shaikh, R.A. IoMT landscape: Navigating current challenges and pioneering future research trends. Discov. Appl. Sci. 2024, 7, 26. [Google Scholar] [CrossRef]
- Wagan, S.A.; Koo, J.; Siddiqui, I.F.; Attique, M.; Shin, D.R.; Qureshi, N.M.F. Internet of medical things and trending converged technologies: A comprehensive review on real-time applications. J. King Saud Univ. Comput. Inf. Sci. 2022, 34 Pt B, 9228–9251. [Google Scholar] [CrossRef]
- Ahmed, S.F.; Bin Alam, S.; Afrin, S.; Rafa, S.J.; Rafa, N.; Gandomi, A.H. Insights into Internet of Medical Things (IoMT): Data fusion, security issues and potential solutions. Inf. Fusion 2023, 102, 102060. [Google Scholar] [CrossRef]
- Sarkar, M.; Lee, T.-H.; Sahoo, P.K. Smart Healthcare: Exploring the Internet of Medical Things with Ambient Intelligence. Electronics 2024, 13, 2309. [Google Scholar] [CrossRef]
- Mazhar, T.; Shah, S.F.A.; Inam, S.A.; Awotunde, J.B.; Saeed, M.M.; Hamam, H. Analysis of integration of IoMT with blockchain: Issues, challenges and solutions. Discov. Internet Things 2024, 4, 21. [Google Scholar] [CrossRef]
- Premakanthan, N. Cyber Security Threats and Mitigations in the Healthcare Sector with Emphasis on IoMT Security and Software Defined Networking. 2024. Available online: https://www.researchgate.net/publication/377382276_Cyber_Security_Threats_and_Mitigations_in_the_Healthcare_Sector_with_emphasis_on_IoMT_security_and_Software_Defined_Networking (accessed on 11 January 2025).
- Mennella, C.; Maniscalco, U.; De Pietro, G.; Esposito, M. Ethical and regulatory challenges of AI technologies in healthcare: A narrative review. Heliyon 2024, 10, e26297. [Google Scholar] [CrossRef] [PubMed]
- Varnosfaderani, S.M.; Forouzanfar, M. The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century. Bioengineering 2024, 11, 337. [Google Scholar] [CrossRef]
- Johnson, K.B.; Wei, W.; Weeraratne, D.; Frisse, M.E.; Misulis, K.; Rhee, K.; Zhao, J.; Snowdon, J.L. Precision Medicine, AI, and the Future of Personalized Health Care. Clin. Transl. Sci. 2021, 14, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Gayathri, K.; Bella, K.M. Role of Artificial Intelligence Technology and Its Impact on Transformation of Human Resources Management. 2023. Available online: https://www.researchgate.net/publication/376580780_ROLE_OF_ARTIFICIAL_INTELLIGENCE_TECHNOLOGY_AND_ITS_IMPACT_ON_TRANSFORMATION_OF_HUMAN_RESOURCES_MANAGEMENT (accessed on 11 January 2025).
- Burdea, G.; Kim, N.; Polistico, K.; Kadaru, A.; Grampurohit, N.; Roll, D.; Damiani, F. Assistive game controller for artificial intelligence-enhanced telerehabilitation post-stroke. Assist. Technol. 2021, 33, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Kuo, L.-C.; Yang, K.-C.; Lin, Y.-C.; Yeh, C.-H.; Su, F.-C.; Hsu, H.-Y. Internet of Things (IoT) Enables Robot-Assisted Therapy as a Home Program for Training Upper Limb Functions in Chronic Stroke: A Randomized Control Crossover Study. Arch. Phys. Med. Rehabil. 2023, 104, 363–371. [Google Scholar] [CrossRef]
- Capecci, M.; Cima, R.; Barbini, F.A.; Mantoan, A.; Sernissi, F.; Lai, S.; Fava, R.; Tagliapietra, L.; Ascari, L.; Izzo, R.N.; et al. Telerehabilitation with ARC Intellicare to Cope with Motor and Respiratory Disabilities: Results about the Process, Usability, and Clinical Effect of the “Ricominciare” Pilot Study. Sensors 2023, 23, 7238. [Google Scholar] [CrossRef]
- Amorim, P.; Paiva, J.; de Lima, J.S.; da Fonseca, L.P.; Martins, H.; Silva, P.A. Lessons learned from investigating patients’ and physiotherapists’ perspectives on the design of a telerehabilitation platform. Disabil. Rehabil. Assist. Technol. 2024, 19, 2377–2388. [Google Scholar] [CrossRef]
- Khalid, U.B.; Naeem, M.; Stasolla, F.; Syed, M.H.; Abbas, M.; Coronato, A. Impact of AI-Powered Solutions in Rehabilitation Process: Recent Improvements and Future Trends. Int. J. Gen. Med. 2024, 17, 943–969. [Google Scholar] [CrossRef]
- Dixon, D.; Sattar, H.; Moros, N.; Kesireddy, S.R.; Ahsan, H.; Lakkimsetti, M.; Fatima, M.; Doshi, D.; Sadhu, K.; Hassan, M.J. Unveiling the Influence of AI Predictive Analytics on Patient Outcomes: A Comprehensive Narrative Review. Cureus 2024, 16, e59954. [Google Scholar] [CrossRef]
- El-Tallawy, S.N.; Pergolizzi, J.V.; Vasiliu-Feltes, I.; Ahmed, R.S.; LeQuang, J.K.; El-Tallawy, H.N.; Varrassi, G.; Nagiub, M.S. Incorporation of “Artificial Intelligence” for Objective Pain Assessment: A Comprehensive Review. Pain Ther. 2024, 13, 293–317. [Google Scholar] [CrossRef]
- Wei, M.; Meng, D.; He, S.; Lv, Z.; Guo, H.; Yang, G.; Wang, Z. Investigating the efficacy of AI-enhanced telerehabilitation in sarcopenic older individuals. Eur. Geriatr. Med. 2024, 16, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Ye, Q.; Xia, J. Unbox the black-box for the medical explainable AI via multi-modal and multi-centre data fusion: A mini-review, two showcases and beyond. Inf. Fusion 2022, 77, 29–52. [Google Scholar] [CrossRef]
- Swarnakar, R.; Yadav, S.L. Artificial intelligence and machine learning in motor recovery: A rehabilitation medicine perspective. World J. Clin. Cases 2023, 11, 7258–7260. [Google Scholar] [CrossRef]
- Celesti, A.; Celesti, F.; Fazio, M.; Villari, M. Improving tele-rehabilitation therapy through machine learning with a NoSQL graph DBMS approach. In Proceedings of the IEEE Global Communications Workshop, Taipei, Taiwan, 7–11 December 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Wood, J.M.; Kim, H.E.; Morton, S.M. Reinforcement Learning during Locomotion. eNeuro 2024, 11, 1–12. [Google Scholar] [CrossRef]
- Wubineh, B.Z.; Deriba, F.G.; Woldeyohannis, M.M. Exploring the opportunities and challenges of implementing artificial intelligence in healthcare: A systematic literature review. Urol. Oncol. Semin. Orig. Investig. 2024, 42, 48–56. [Google Scholar] [CrossRef]
- Al-Kfairy, M.; Alomari, A.; Al-Bashayreh, M.; Alfandi, O.; Tubishat, M. Unveiling the Metaverse: A survey of user perceptions and the impact of usability, social influence and interoperability. Heliyon 2024, 10, e31413. [Google Scholar] [CrossRef] [PubMed]
- Shoabjareh, A.H.; Ghasri, M.; Roberts, T.; Lapworth, A.; Dobos, N.; Burken, C.B.-V. The role of trust and distrust in technology usage: An in-depth investigation of traffic information apps usage for mandatory and non-mandatory trips. Travel Behav. Soc. 2024, 37, 100816. [Google Scholar] [CrossRef]
- Lawrence, E. User-Centered Design to Enhance Accessibility and Usability in Digital Systems. 2024. Available online: https://www.researchgate.net/publication/386339454_User_centered_design_to_enhance_accessibility_and_usability_in_digital_systems (accessed on 11 January 2025).
- Bajwa, J.; Munir, U.; Nori, A.; Williams, B. Artificial intelligence in healthcare: Transforming the practice of medicine. Futur. Healthc. J. 2021, 8, e188–e194. [Google Scholar] [CrossRef] [PubMed]
- Tsvetanov, F. Integrating AI Technologies into Remote Monitoring Patient Systems. Eng. Proc. 2024, 70, 54. [Google Scholar] [CrossRef]
- David-Olawade, A.C.; Olawade, D.B.; Ojo, I.O.; Famujimi, M.E.; Olawumi, T.T.; Esan, D.T. Nursing in the Digital Age: Harnessing telemedicine for enhanced patient care. Inform. Health 2024, 1, 100–110. [Google Scholar] [CrossRef]
- Tilala, M.H.; Chenchala, P.K.; Choppadandi, A.; Kaur, J.; Naguri, S.; Saoji, R.; Devaguptapu, B. Ethical Considerations in the Use of Artificial Intelligence and Machine Learning in Health Care: A Comprehensive Review. Cureus 2024, 16, e62443. [Google Scholar] [CrossRef]
- Mahmood, U.; Shukla-Dave, A.; Chan, H.-P.; Drukker, K.; Samala, R.K.; Chen, Q.; Vergara, D.; Greenspan, H.; Petrick, N.; Sahiner, B.; et al. Artificial intelligence in medicine: Mitigating risks and maximizing benefits via quality assurance, quality control, and acceptance testing. BJR Artif. Intell. 2024, 1, ubae003. [Google Scholar] [CrossRef]
- Pantanowitz, L.; Hanna, M.; Pantanowitz, J.; Lennerz, J.; Henricks, W.H.; Shen, P.; Quinn, B.; Bennet, S.; Rashidi, H.H. Regulatory Aspects of Artificial Intelligence and Machine Learning. Mod. Pathol. 2024, 37, 100609. [Google Scholar] [CrossRef] [PubMed]
- Gala, D.; Behl, H.; Shah, M.; Makaryus, A.N. The Role of Artificial Intelligence in Improving Patient Outcomes and Future of Healthcare Delivery in Cardiology: A Narrative Review of the Literature. Healthcare 2024, 12, 481. [Google Scholar] [CrossRef]
- Willingham, T.B.; Stowell, J.; Collier, G.; Backus, D. Leveraging Emerging Technologies to Expand Accessibility and Improve Precision in Rehabilitation and Exercise for People with Disabilities. Int. J. Environ. Res. Public Health 2024, 21, 79. [Google Scholar] [CrossRef] [PubMed]
- Jungherr, A. Artificial Intelligence and Democracy: A Conceptual Framework. Soc. Media Soc. 2023, 9, 1–14. [Google Scholar] [CrossRef]
- Yelne, S.; Chaudhary, M.; Dod, K.; Sayyad, A.; Sharma, R. Harnessing the Power of AI: A Comprehensive Review of Its Impact and Challenges in Nursing Science and Healthcare. Cureus 2023, 15, e49252. [Google Scholar] [CrossRef]
- Lythreatis, S.; Singh, S.K.; El-Kassar, A.-N. The digital divide: A review and future research agenda. Technol. Forecast. Soc. Change 2021, 175, 121359. [Google Scholar] [CrossRef]
- Rane, J.; Kaya, Ö.; Mallick, S.K.; Rane, N.L. Enhancing black-box models: Advances in explainable artificial intelligence for ethical decision-making. In Future Research Opportunities for Artificial Intelligence in Industry 4.0 and 5.0; Deep Science Publishing: Mumbai, India, 2024; pp. 136–180. [Google Scholar] [CrossRef]
- Kornhaber, R.; Walsh, K.; Duff, J.; Walker, K. Enhancing adult therapeutic interpersonal relationships in the acute health care setting: An integrative review. J. Multidiscip. Healthc. 2016, 9, 537–546. [Google Scholar] [CrossRef]
- Dolev, T.; Zilcha-Mano, S. The role of the therapeutic relationship in the association between interpersonal behaviors and outcome: Comparison of two competing models. Psychother. Res. 2019, 29, 553–564. [Google Scholar] [CrossRef]
- Alowais, S.A.; Alghamdi, S.S.; Alsuhebany, N.; Alqahtani, T.; Alshaya, A.I.; Almohareb, S.N.; Aldairem, A.; Alrashed, M.; Bin Saleh, K.; Badreldin, H.A.; et al. Revolutionizing healthcare: The role of artificial intelligence in clinical practice. BMC Med. Educ. 2023, 23, 689. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Rodríguez, N.; Del Ser, J.; Coeckelbergh, M.; de Prado, M.L.; Herrera-Viedma, E.; Herrera, F. Connecting the dots in trustworthy Artificial Intelligence: From AI principles, ethics, and key requirements to responsible AI systems and regulation. Inf. Fusion 2023, 99, 101896. [Google Scholar] [CrossRef]
- Bhushan, B.; Kumar, A.; Agarwal, A.K.; Kumar, A.; Bhattacharya, P.; Kumar, A. Towards a Secure and Sustainable Internet of Medical Things (IoMT): Requirements, Design Challenges, Security Techniques, and Future Trends. Sustainability 2023, 15, 6177. [Google Scholar] [CrossRef]
- Kruk, M.E.; Gage, A.D.; Arsenault, C.; Jordan, K.; Leslie, H.H.; Roder-DeWan, S.; Adeyi, O.; Barker, P.; Daelmans, B.; Doubova, S.V.; et al. High-quality health systems in the Sustainable Development Goals era: Time for a revolution. Lancet Glob. Health 2018, 6, e1196–e1252. [Google Scholar] [CrossRef]
- Wallace, P.J. Gaining Trust: Lessons and Opportunities for Artificial Intelligence in Health Care. Perm. J. 2024, 28, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Khan, B.; Fatima, H.; Qureshi, A.; Kumar, S.; Hanan, A.; Hussain, J.; Abdullah, S. Drawbacks of Artificial Intelligence and Their Potential Solutions in the Healthcare Sector. Biomed. Mater. Devices 2023, 1, 731–738. [Google Scholar] [CrossRef]
- Arntz, A.; Weber, F.; Handgraaf, M.; Lällä, K.; Korniloff, K.; Murtonen, K.-P.; Chichaeva, J.; Kidritsch, A.; Heller, M.; Sakellari, E.; et al. Technologies in Home-Based Digital Rehabilitation: Scoping Review. JMIR Rehabil. Assist. Technol. 2023, 10, e43615. [Google Scholar] [CrossRef]
- Borges do Nascimento, I.J.; Abdulazeem, H.; Vasanthan, L.T.; Martinez, E.Z.; Zucoloto, M.L.; Østengaard, L.; Azzopardi-Muscat, N.; Zapata, T.; Novillo-Ortiz, D. Barriers and facilitators to utilizing digital health technologies by healthcare professionals. NPJ Digit. Med. 2023, 6, 161. [Google Scholar] [CrossRef]
- Maqbool, B.; Herold, S. Potential effectiveness and efficiency issues in usability evaluation within digital health: A systematic literature review. J. Syst. Softw. 2024, 208, 111881. [Google Scholar] [CrossRef]
- Williamson, S.M.; Prybutok, V. Balancing Privacy and Progress: A Review of Privacy Challenges, Systemic Oversight, and Patient Perceptions in AI-Driven Healthcare. Appl. Sci. 2024, 14, 675. [Google Scholar] [CrossRef]
- Frank, E.; Ok, E. The Role of Artificial Intelligence in Transforming Patient Care and Diagnostic Processes. 2024. Available online: https://www.researchgate.net/publication/383660380_The_Role_of_Artificial_Intelligence_in_Transforming_Patient_Care_and_Diagnostic_Processes (accessed on 16 December 2024).
- Cingolani, M.; Scendoni, R.; Fedeli, P.; Cembrani, F. Artificial intelligence and digital medicine for integrated home care services in Italy: Opportunities and limits. Front. Public Health 2023, 10, 1095001. [Google Scholar] [CrossRef] [PubMed]
- Kr, P.; Kinkar, R.; Kumar, G.; Anand, N.; Rama, K.; Singhal, P.; Sharma, A. Intelligent integration of wearable sensors and artificial intelligence for real-time athletic performance enhancement. J. Intell. Syst. Internet Things 2024, 13, 60–77. [Google Scholar] [CrossRef]
- Esmaeilzadeh, P. Challenges and strategies for wide-scale artificial intelligence (AI) deployment in healthcare practices: A perspective for healthcare organizations. Artif. Intell. Med. 2024, 151, 102861. [Google Scholar] [CrossRef] [PubMed]
- European Commission; Joint Research Centre; Rak, R.; Quinn, P. Enhancing Digital Health Innovation in the EU with Effective Industrial Strategy Policies—A Focus on Wearable Medical Devices; Ciui, B., Ed.; Publications Office of the European Union: Luxembourg, 2024; JRC138798; Available online: https://publications.jrc.ec.europa.eu/repository/handle/JRC138798 (accessed on 16 December 2024).
| Aspect | Pros | Cons/Challenges | Potential Solutions |
|---|---|---|---|
| Personalization | Tailored rehabilitation plans based on real-time patient data [77]. | Risk of algorithmic bias leading to suboptimal care for underrepresented groups [77]. | Use diverse and representative training datasets; implement regular audits for bias detection and correction [77]. |
| Patient Engagement | Immersive VR and gamified environments boost motivation and adherence [78]. | High cost of advanced technologies, like VR systems and AI-enabled wearables [78]. | Seek cost-effective alternatives; explore funding options and partnerships with tech companies to lower costs [78]. |
| Accessibility | Enables home-based care, reducing the need for travel [79]. | Digital divide limits access for rural and underserved populations [79]. | Implement mobile-friendly platforms and low-cost devices; provide subsidies or support for disadvantaged populations [79]. |
| Clinician Support | Provides precise feedback, enhancing decision making [80]. | Risk of over-reliance on AI, potentially reducing the clinician’s role [80]. | Promote a hybrid approach combining clinician expertise with AI insights to ensure that AI complements rather than replaces clinical judgment [80]. |
| Data Insights | Analyzes large datasets for trends, improving evidence-based practices [81]. | Privacy and security concerns with sensitive health data storage and transmission [81]. | Strengthen encryption methods, comply with regulations, and use secure cloud platforms for data storage [81]. |
| Efficiency | Automates administrative tasks, freeing up clinicians for patient care [82]. | Integration into existing workflows requires training and resistance to change [82]. | Provide comprehensive training programs; create user-friendly AI tools that fit seamlessly into current clinical workflows [82]. |
| Collaboration | Centralized platforms enable interdisciplinary teamwork [83]. | Inconsistent standards across platforms and healthcare settings hinder interoperability [83]. | Develop universal standards and protocols for AI in telerehabilitation; foster collaboration between tech developers and healthcare providers [83]. |
| Real-Time Monitoring | Wearable sensors detect subtle progress or setbacks during exercises [84]. | Ensuring reliability and accuracy of AI-powered devices remains a technical challenge [84]. | Regular calibration and testing of wearable devices; continuous refinement of AI algorithms to improve accuracy [84]. |
| Scalability | AI enables a wider reach of rehabilitation services [85]. | Ethical concerns over transparency and decision-making processes [85]. | Implement explainable AI models and ensure clinical oversight; involve patients in decision making where possible [85]. |
| Future Potential | Integration with IoMT, robotics, and 5G for enhanced capabilities [86]. | High development and maintenance costs; requires continuous innovation and investment [86]. | Partner with tech companies for joint ventures, reduce development costs through collaboration, and secure funding for ongoing innovation [86]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calabrò, R.S.; Mojdehdehbaher, S. AI-Driven Telerehabilitation: Benefits and Challenges of a Transformative Healthcare Approach. AI 2025, 6, 62. https://doi.org/10.3390/ai6030062
Calabrò RS, Mojdehdehbaher S. AI-Driven Telerehabilitation: Benefits and Challenges of a Transformative Healthcare Approach. AI. 2025; 6(3):62. https://doi.org/10.3390/ai6030062
Chicago/Turabian StyleCalabrò, Rocco Salvatore, and Sepehr Mojdehdehbaher. 2025. "AI-Driven Telerehabilitation: Benefits and Challenges of a Transformative Healthcare Approach" AI 6, no. 3: 62. https://doi.org/10.3390/ai6030062
APA StyleCalabrò, R. S., & Mojdehdehbaher, S. (2025). AI-Driven Telerehabilitation: Benefits and Challenges of a Transformative Healthcare Approach. AI, 6(3), 62. https://doi.org/10.3390/ai6030062







