Toric Intraocular Lens Results Considering Posterior Corneal Astigmatism with Online Calculators: Phacoemulsification vs. Femtosecond
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects and Procedures
2.2. Surgery and Intraocular Lens
2.3. Statistical Analysis
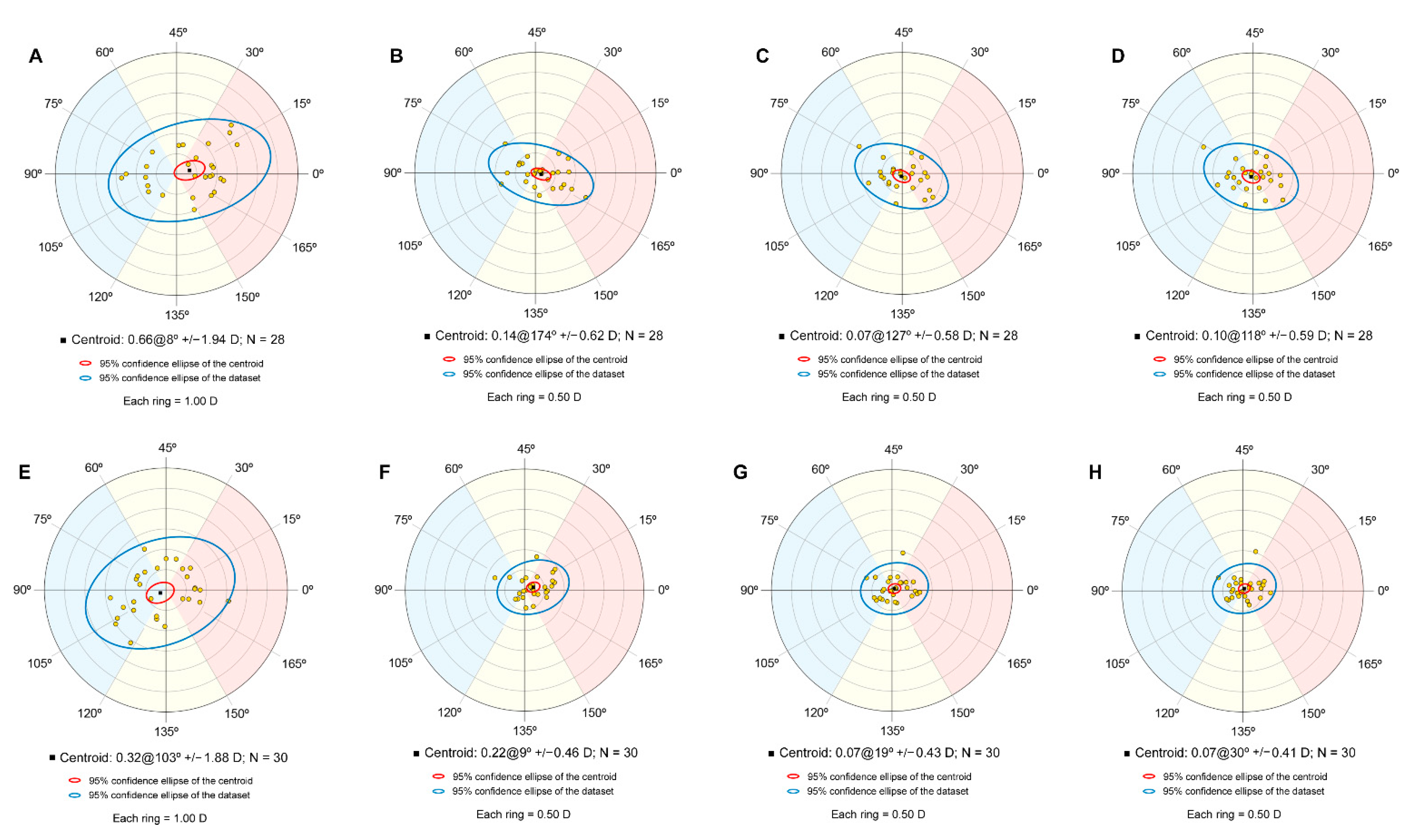
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Koch, D.D.; Ali, S.F.; Weikert, M.P. Contribution of posterior corneal astigmatism to total corneal astigmatism. J. Cataract Refract. Surg. 2012, 38, 2080–2087. [Google Scholar] [CrossRef]
- Yoon, C.H.; Kim, M.K. Improving the toric intraocular lens calculation by considering posterior corneal astigmatism and surgically-induced corneal astigmatism. Korean J. Ophthalmol. 2018, 32, 265–272. [Google Scholar] [CrossRef]
- Canovas, C.; Alarcon, A.; Rosén, R.; Kasthurirangan, S.; Ma, J.J.K.; Koch, D.D.; Piers, P. New algorithm for toric intraocular lens power calculation considering the posterior corneal astigmatism. J. Cataract Refract. Surg. 2018, 44, 168–174. [Google Scholar] [CrossRef]
- Abulafia, A.; Koch, D.D.; Wang, L.; Hill, W.E.; Assia, E.I.; Franchina, M.; Barrett, G.D. New regression formula for toric intraocular lens calculations. J. Cataract Refract. Surg. 2016, 42, 663–671. [Google Scholar] [CrossRef] [PubMed]
- Reitblat, O.; Levy, A.; Kleinmann, G.; Abulafia, A.; Assia, E.I. Effect of posterior corneal astigmatism on power calculation and alignment of toric intraocular lenses: Comparison of methodologies. J. Cataract Refract. Surg. 2016, 42, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Eom, Y.; Rhim, J.W.; Kang, S.; Kim, S.; Song, J.S.; Kim, H.M. Toric intraocular lens calculations using ratio of anterior to posterior corneal cylinder power. Am. J. Ophthalmol. 2015. [Google Scholar] [CrossRef]
- Barrett, G.D. An improved universal theoretical formula for intraocular lens power prediction. J. Cataract Refract. Surg. 1993, 19, 713–720. [Google Scholar] [CrossRef]
- Kessel, L.; Andresen, J.; Tendal, B.; Erngaard, D.; Flesner, P.; Hjortdal, J. Toric Intraocular Lenses in the Correction of Astigmatism During Cataract Surgery: A Systematic Review and Meta-analysis. Ophthalmology 2016, 123, 275–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoffer, K.J.; Savini, G. Update on Intraocular Lens Power Calculation Study Protocols. Ophthalmology 2020, in press. [Google Scholar] [CrossRef]
- ISO. ISO 11979-7:2018 Ophthalmic Implants—Intraocular Lenses—Part 7: Clinical Investigations of Intraocular Lenses for the Correction of Aphakia; ISO: Geneva, Switzerland, 2018. [Google Scholar]
- Armstrong, R.A. Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic Physiol. Opt. 2013, 33, 7–14. [Google Scholar] [CrossRef]
- Abulafia, A.; Koch, D.D.; Holladay, J.T.; Wang, L.; Hill, W. Pursuing perfection in intraocular lens calculations: IV. Rethinking astigmatism analysis for intraocular lens-based surgery: Suggested terminology, analysis, and standards for outcome reports. J. Cataract Refract. Surg. 2018, 44, 1169–1174. [Google Scholar] [CrossRef] [PubMed]
- Alpins, N.A. A new method of analyzing vectors for changes in astigmatism. J. Cataract Refract. Surg. 1993, 19, 524–533. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Profile analysis: The multivariate approach to repeated measures. In Using Multivariate Statistics; Pearson Education: Boston, MA, USA, 2013; Chapter 8; p. 343. [Google Scholar]
- Rodríguez-Vallejo, M. Refractive Analysis. (v.1.0.4). A Matlab Toolbox for the Analysis of Refractive Results in Anterior Segment Surgery. Available online: http://test-eye.com/index.php/en/refractive-analysis (accessed on 1 April 2020).
- Lehmann, R.P.; Houtman, D.M. Visual performance in cataract patients with low levels of postoperative astigmatism: Full correction versus spherical equivalent correction. Clin. Ophthalmol. 2012, 6, 333. [Google Scholar] [CrossRef] [Green Version]
- Hayashi, K.; Manabe, S.I.; Yoshida, M.; Hayashi, H. Effect of astigmatism on visual acuity in eyes with a diffractive multifocal intraocular lens. J. Cataract Refract. Surg. 2010, 36, 1323–1329. [Google Scholar] [CrossRef]
- Villegas, E.A.; Alcón, E.; Artal, P. Minimum amount of astigmatism that should be corrected. J. Cataract Refract. Surg. 2014, 40, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Koch, D.D.; Jenkins, R.B.; Weikert, M.P.; Yeu, E.; Wang, L. Correcting astigmatism with toric intraocular lenses: Effect of posterior corneal astigmatism. J. Cataract Refract. Surg. 2013, 39, 1803–1809. [Google Scholar] [CrossRef] [PubMed]
- Goggin, M.; van Zyl, L.; Caputo, S.; Esterman, A. Outcome of adjustment for posterior corneal curvature in toric intraocular lens calculation and selection. J. Cataract Refract. Surg. 2016, 42, 1441–1448. [Google Scholar] [CrossRef]
- Ferreira, T.B.; Ribeiro, P.; Ribeiro, F.J.; O’Neill, J.G. Comparison of astigmatic prediction errors associated with new calculation methods for toric intraocular lenses. J. Cataract Refract. Surg. 2017, 43, 340–347. [Google Scholar] [CrossRef]
- Preussner, P.R.; Hoffmann, P.; Wahl, J. Impact of posterior corneal surface on toric intraocular lens (IOL) calculation. Curr. Eye Res. 2015, 40, 809–814. [Google Scholar] [CrossRef]
- Nanavaty, M.A.; Teeluck, K.; Bardan, A.S.; Bedi, K.K.; Ali, S. Residual refractive astigmatism following toric intraocular lens implantation without consideration of posterior corneal astigmatism during cataract surgery with low anterior keratometric astigmatism upto 2.5 dioptres. Curr. Eye Res. 2019, 44, 1399–1406. [Google Scholar] [CrossRef]
- Yeu, E.; Cheung, A.Y.; Potvin, R. Clinical outcomes of toric intraocular lenses: Differences in expected outcomes when using a calculator that considers effective lens position and the posterior cornea vs. one that does not. Clin. Ophthalmol. 2020, 14, 815–822. [Google Scholar] [CrossRef] [Green Version]
- Holladay, J.T.; Pettit, G. Improving toric intraocular lens calculations using total surgically induced astigmatism for a 2.5 mm temporal incision. J. Cataract Refract. Surg. 2019, 45, 272–283. [Google Scholar] [CrossRef]
- Fernández, J.; Rodríguez-Vallejo, M.; Martínez, J.; Tauste, A.; Piñero, D.P. Prediction of surgically induced astigmatism in manual and femtosecond laser-assisted clear corneal incisions. Eur. J. Ophthalmol. 2018, 28, 398–405. [Google Scholar] [CrossRef]
- Li, X.; Chen, X.; He, S.; Xu, W. Effect of 1.8-mm steep-axis clear corneal incision on the posterior corneal astigmatism in candidates for toric IOL implantation. BMC Ophthalmol. 2020, 20, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Garzón, N.; Rodríguez-Vallejo, M.; Carmona, D.; Calvo-Sanz, J.A.; Poyales, F.; Palomino, C.; Zato-Gómez de Liaño, M.; Fernández, J. Comparing surgically induced astigmatism calculated by means of simulated keratometry versus total corneal refractive power. Eur. J. Ophthalmol. 2018, 28, 573–581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohnen, T.; Löffler, F.; Herzog, M.; Petermann, K.; Böhm, M. Tomographic analysis of anterior and posterior surgically induced astigmatism after 2.2 mm temporal clear corneal incisions in femtosecond laser–assisted cataract surgery. J. Cataract Refract. Surg. 2019, 45, 1602–1611. [Google Scholar] [CrossRef] [PubMed]
- Kern, C.; Kortüm, K.; Müller, M.; Kampik, A.; Priglinger, S.; Mayer, W.J. Comparison of Two Toric IOL Calculation Methods. J. Ophthalmol. 2018, 2018. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Sy, M.E.; Mai, H.; Yu, F.; Rex Hamilton, D. Effect of posterior corneal astigmatism on refractive outcomes after toric intraocular lens implantation. J. Cataract Refract. Surg. 2015, 41, 84–89. [Google Scholar] [CrossRef]
- Sano, M.; Hiraoka, T.; Ueno, Y.; Itagaki, H.; Ogami, T.; Oshika, T. Influence of posterior corneal astigmatism on postoperative refractive astigmatism in pseudophakic eyes after cataract surgery. BMC Ophthalmol. 2016, 16, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Kane, J.X.; Connell, B. A Comparison of the Accuracy of 6 Modern Toric Intraocular Lens Formulas. Ophthalmology 2020, 127, 1472–1486. [Google Scholar] [CrossRef]
- Ueno, Y.; Hiraoka, T.; Beheregaray, S.; Miyazaki, M.; Ito, M.; Oshika, T. Age-related changes in anterior, posterior, and total corneal astigmatism. J. Refract. Surg. 2014, 30, 192–197. [Google Scholar] [CrossRef] [PubMed]

| Variable | Phaco Mean ± SD; Median (IQR) | Femto Mean ± SD; Median (IQR) | Statistic; p-Value |
|---|---|---|---|
| N (WTR, Oblique, ATR) | 28 (8, 3, 17) | 30 (12, 8, 10) | χ2 = 4.82; 0.1 |
| Age | 73.93 ± 10.43; 75 (12) | 67.43 ± 8.36; 69 (13.75) | z = 605; 0.004 * |
| Anterior Corneal Preoperative Astigmatism (D) | 1.89 ± 0.70; 1.70 (0.74) | 1.76 ± 0.63; 1.57 (0.63) | z = 490; 0.276 |
| Axial length (mm) | 24.06 ± 1.58; 23.87 (1.08) | 24.25 ± 1.85; 23.81 (2.32) | z = 416; 0.85 |
| Anterior chamber depth (mm) | 3.09 ± 0.34; 3.08 (0.50) | 3.07 ± 0.45; 3.02 (0.63) | t = −0.245; 0.808 |
| Postoperative CDVA | 0.12 ± 0.1; 0.1 (0.2) | 0.04 ± 0.08; 0 (0.1) | z = 540; 0.057 |
| Postoperative UDVA | 0.21 ± 0.15; 0.2 (0.2) | 0.13 ± 0.15; 0.1 (0.22) | z = 608; 0.002 * |
| Intraocular lens power for Sphere (D) | 19.20 ± 3.72; 20 (4) | 17.58 ± 5.56; 19.5 (6.63) | z = 476; 0.383 |
| Intraocular lens power for Cylinder (D) | 2.42 ± 1.09; 2.25 (1.50) | 2 ± 0.84; 2.25 (0.88) | z = 513; 0.136 |
| Preoperative Type | Mean Difference (97.5% CI) | p-Value |
|---|---|---|
| X (D) | ||
| Non-PCA–AK | 0.15 (0.08 to 0.23) | <0.0005 |
| Non-PCA–Barret | 0.18 (0.08 to 0.29) | <0.0005 |
| AK-Barrett | 0.03 (−0.05 to 0.10) | 0.925 |
| Y (D) | ||
| Non-PCA–AK | 0.04 (−0.02 to 0.09) | 0.18 |
| Non-PCA–Barret | 0.03 (−0.02 to 0.09) | 0.32 |
| AK-Barrett | −0.002 (−0.03 to 0.03) | 1.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández, J.; Rodríguez-Vallejo, M.; Burguera, N.; Salvestrini, P.; Garzón, N. Toric Intraocular Lens Results Considering Posterior Corneal Astigmatism with Online Calculators: Phacoemulsification vs. Femtosecond. Optics 2021, 2, 184-192. https://doi.org/10.3390/opt2030017
Fernández J, Rodríguez-Vallejo M, Burguera N, Salvestrini P, Garzón N. Toric Intraocular Lens Results Considering Posterior Corneal Astigmatism with Online Calculators: Phacoemulsification vs. Femtosecond. Optics. 2021; 2(3):184-192. https://doi.org/10.3390/opt2030017
Chicago/Turabian StyleFernández, Joaquín, Manuel Rodríguez-Vallejo, Noemí Burguera, Patrizia Salvestrini, and Nuria Garzón. 2021. "Toric Intraocular Lens Results Considering Posterior Corneal Astigmatism with Online Calculators: Phacoemulsification vs. Femtosecond" Optics 2, no. 3: 184-192. https://doi.org/10.3390/opt2030017
APA StyleFernández, J., Rodríguez-Vallejo, M., Burguera, N., Salvestrini, P., & Garzón, N. (2021). Toric Intraocular Lens Results Considering Posterior Corneal Astigmatism with Online Calculators: Phacoemulsification vs. Femtosecond. Optics, 2(3), 184-192. https://doi.org/10.3390/opt2030017








