Study of the Effect of Low-Intensity Sub- and Millimeter Waves on the Induction of Adaptation Reactions in Experimental Burn
Abstract
1. Introduction
2. Materials and Methods
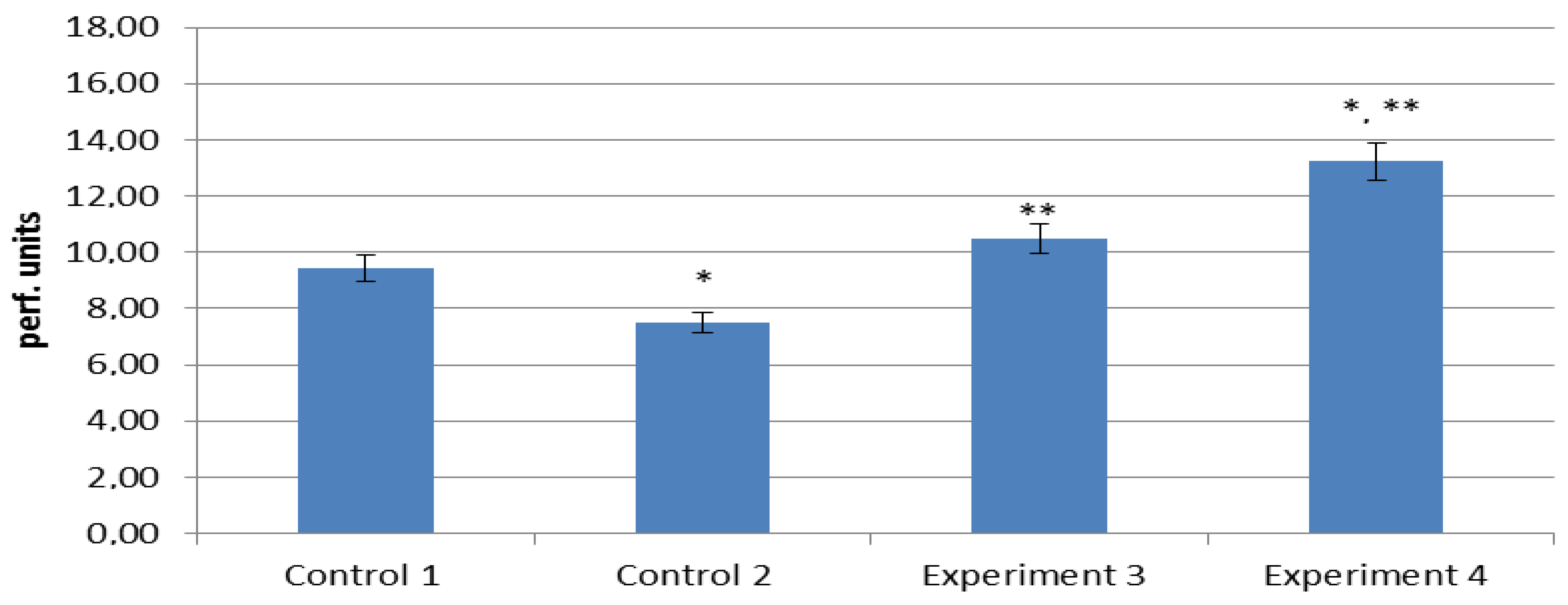
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Shabanov, V.E.; Savvin, Y.U.N.; Alekseev, A.A.; Krutikov, M.G.; Bobrovnikov, A.E.; Demenko, V.V. Klinicheskie Rekomendacii po Okazaniyu Medicinskoj Pomoshchi Postradavshim s Termicheskoj Travmoj v Chrezvychajnyh Situaciyah; Zashchita: Moscow, Russia, 2016; p. 240. [Google Scholar]
- Sidel’nikov, V.O.; Cygan, V.N.; Zinov’ev, E.V. Boevye Ozhogovye Porazheniya; SpecLit: Saint-Petersburg, Russia, 2019; p. 247. [Google Scholar]
- Van Lieshout, E.M.; Van Yperen, D.T.; Van Baar, M.E.; Polinder, S.; Boersma, D.; Cardon, A.Y.; De Rijcke, P.A.; Guijt, M.; Klem, T.M.; Lansink, K.W.; et al. Epidemiology of injuries, treatment (costs) and outcome in patients with burns admitted to the hospital with or without a dedicated burn center (Burn-Pro): Protocol of a multicenter prospective observational study. BMJ 2018, 8, 023709. [Google Scholar] [CrossRef] [PubMed]
- Alekseev, A.A.; Bobrovnikov, A.E.; Bogdanov, V.V. Evaluation of the effectiveness of innovative technologies for the treatment of burn victims. Med. Alfavit 2020, 13, 44–47. [Google Scholar] [CrossRef]
- Ubbink, D.T.; Brolmann, F.E.; Go, P.M.; Vermeule, N.H. Evidence-based care for acute wounds: A perspective. Adv. Wound Care 2015, 4, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Agadzhanova, K.V. Burns: Classification and treatment approaches depending on the severity. Colloquium-J. 2020, 1, 4. [Google Scholar]
- Bobrovnikov, A.E.; Alekseev, A.A. Personalized technologies for local treatment of burn wounds. Lechenie I Profil. 2017, 3, 75–78. [Google Scholar]
- Saeidinia, A.A.; Keihanian, F.; Lashari, A.P.; Lahiji, H.G.; Mobayyen, M.; Heidarzade, A.; Golchan, J. Healing of partial-thickness burn wounds with local treatment: A randomized controlled comparison of silver sulfadiazine and santiderma. Medicina 2017, 96, 61–68. [Google Scholar]
- Fayazov, A.D.; Tulyaganov, D.B.; Kamilov, U.R.; Ruzimuratov, D.A. Modern methods of local treatment of burn wounds. Vestn. Ekstrennoj Med. 2019, 12, 43–47. [Google Scholar]
- Tapbergenov, S.O.; Tapbergenov, T.S.; Sovetov, B.S. Funkcional’nye i Metabolicheskie Effekty Simpato-Adrenalovoj Sistemy i Stress; Akademiya Estestvoznaniya: Moscow, Russia, 2019; p. 138. [Google Scholar]
- Podoinitsyna, M.G.; Cepelev, A.V.; Stepanov, V.L. Clinical efficacy of magnetic laser therapy for skin burns. Zabajkal’skij Med. Vestn. 2015, 2, 99–102. [Google Scholar]
- Bailey, J.K.; Blackstone, B.N.; De Bruler, D.M.; Kim, J.Y.; Baumann, M.E.; McFanrland, K.L.; Imeokpana, F.O.; Supp, D.M.; Powell, H.M. Effects of early combinatorial processing of autologous split-thickness skin grafts in the Duroc red pig model using a pulsed dye laser and a fractional CO2 laser. Lazern. Hir. 2018, 50, 78–87. [Google Scholar]
- Moskvin, S.V.; Khadartsev, A.A. EHF-Laser Therapy; Publishing house “Triad”: Tver, Russia, 2016; p. 168. [Google Scholar]
- Vaks, V.L.; Anfertev, V.A.; Balakirev, V.Y.; Basov, S.A.; Domracheva, E.G.; Illyuk, A.V.; Kupriyanov, P.V.; Pripolzin, S.I.; Chernyaeva, M.B. High resolution terahertz spectroscopy for analytical applications. Phys. Usp. 2020, 63, 708–720. [Google Scholar] [CrossRef]
- KVCh-Terapija s Nizkointensivnym Shumovym Izlucheniem; Balchugov, V.A., Poljakova, A.G., Anisimov, S.I., Kornauchov, A.V.N., Eds.; NGU: Novgorod, Russia, 2002; p. 192. [Google Scholar]
- Kiryanova, V.V.; Zharova, E.N.; Bagraev, N.T.; Reukov, A.S.; Loginova, S.V. Prospects of application of electromagnetic waves of the terahertz range in physiotherapy (retrospective review). Physiother. Balneol. Rehabil. 2016, 4, 209–215. [Google Scholar] [CrossRef]
- Deryugina, A.V.; Talamanova, M.N.; Hlamova, Y.U.N.; Kuvaeva, S.S.; Shabalin, M.A.; Oshevenskij, L.V.; Cvetkov, A.I.; Glavin, M.Y. Adaptive reactions of red blood cells under the action of electromagnetic radiation of the terahertz range. Mezhdunarodnyj Nauchno-Issledovatel’skij Zhurnal 2017, 1–2, 6–8. [Google Scholar]
- Soloveva, A.G.; Polyakova, A.G.; Peretyagin, P.V.; Didenko, N.V. The influence of terahertz radiation on biochemical metabolism of blood in the experiment. EPJ Web Conf. 2018, 195, 32–33. [Google Scholar] [CrossRef][Green Version]
- Lukin, S.Y.; Soldatov, Y.P.; Stogov, M.V. Complex correction of pathophysiological disorders in orthopedic and traumatological patients with the use of electromagnetic waves of the terahertz range at the frequencies of nitric oxide radiation. Vopr. Kurortol. Fizioter. I Lech. Fiz. Kul’tury 2018, 95, 58–66. [Google Scholar] [CrossRef] [PubMed]
- Polyakova, A.G. Microwave Reflexotherapy in the Complex Rehabilitation of Patients with Traumatological and Orthopedic Profile Textbook Nizhny; PIMU: Novgorod, Russia, 2020; p. 56. [Google Scholar]
- Spasova, N.V.; Razumov, A.N.; Lyubovcev, V.B. The role of acupuncture points in the interaction of the human body with the interplanetary electromagnetic field. Vestn. Vosstanov. Med. 2007, 4, 103–104. [Google Scholar]
- Savin, L.A.; Panov, G.A.; Makashova, E.S. Neurophysiological changes that occur during the reflexotherapy procedure. Refleksoterapiya I Komplement. Med. 2017, 4, 25–26. [Google Scholar]
- Parshina, S.S.; Afanasyeva, T.N.; Vodolagin, A.V.; Petrova, V.D.; Ushakov VYu Kaplanova, T.I.; Potapova, M.V.; Ramazanova, Z.G. Terahertz therapy at frequencies of the molecular spectrum of nitric oxide: Results and prospects of clinical use. Sarat. Nauchno-Med. Zhurnal 2019, 15, 800–806. [Google Scholar]
- Subbotina, T.I.; Yashin, A.A. Effects of interaction of electromagnetic fields with biosystems. Vestn. Novyh Med. Tekhnologij Elektron. Zhurnal 2018, 4, 1–20. [Google Scholar]
- Peretyagin, P.V.; Solov’eva, A.G.; Luzan, A.S.; Vorob’ev, E.V.; Didenro, N.V. Ustrojstvo Dlya Esperimental’nogo Modelirovaniya Termicheskoj Travmy Kozhi. RU Patent 179 126 U1 MПK A61B 18/04, 26 April 2018. [Google Scholar]
- Sirota, T.V. A new approach to the study of the epinephrine auto-oxidation reaction: The possibility of polarographic determination of the activity of superoxide dismutase and the antioxidant properties of various drugs. Biomed. Him. 2012, 58, 77–87. [Google Scholar]
- Sibgatullina, G.V.; Haertdinova, L.R.; Gumerova, E.A.; Akulov, A.N.; Kostyukova, Y.U.A.; Nikonorova, N.A.; Rumyanceva, N.I. Metody Opredeleniya Redoks-Statusa Kul’tiviruemyh Kletok Rastenij:Uchebno-Metodicheskoe Posobie; Kazanskij (Privolzhskij) Federal’nyj Universitet: Kazan, Russia, 2011; p. 61. [Google Scholar]
- Kozlov, V.I.; Azolov, G.A.; Gurova, O.A.; Litvin, F.B. Lazernaya Dopplerovskaya Floumetriya v Ocenke Sostoyaniya i Rasstrojstv Mikrocirkulyacii Krovi. Metodicheskoe Posobie; RUDN GNC Lazer. Med.: Moscow, Russia, 2012; p. 32. [Google Scholar]
- Krupatkin, A.I.; Sidorov, V.V. Funkcional’naya Diagnostika Sostoyaniya Mikrocirkulyatorno-Tkanevyh Sistem: Kolebaniya, Informaciya, Nelinejnost’; Rukovodstvo Dlya Vrachej; Knizhnyj dom “LIBROKOM”: Moscow, Russia, 2013; p. 496. [Google Scholar]
- Martusevich, A.K.; Peretyagin, S.P.; Samodelkin, A.G.; Solov’eva, A.G.; Martusevich, A.A.; Ivashchenko, M.N. Biomedicina Oksida Azota (NO): Funkcional’no-Metabolicheskie Aspekty; Nizhegorodskaya Gosudarstvennaya Sel’skohozyajstvennaya Akademiya: Nizhny Novgorod, Russia, 2017; p. 261. [Google Scholar]
- Ushakova, T.A. Adaptation to Burn Injury: Problems and Prospects. Kombustiologiya 2009, 39. Available online: http://combustiolog.ru/journal/adaptatsiya-k-ozhogovoj-travme-problemy-i-perspektivy/ (accessed on 17 January 2022).
- Dmitriev, G.I.; Aref’ev, I.Y.U.; Korotkova, N.L.; Belousov, S.S.; Poyato, T.V.; Men’shenina, E.G.; Poluakova, A.G. Improving the rehabilitation of patients with the consequences of burn injury. Med. Al’manah 2010, 2, 225–228. [Google Scholar]
- Ivanov, D.V.; Lischuk, A.N.; Borisova, O.N. Effects of low-energy electromagnetic radiation of high frequencies when exposed to cells (literature review). Bulletin of New Medical Technologies. Electron. Ed. 2020, 3, 143–152. [Google Scholar]


| Groups Biochemical Parameters | Control 1 (Intact) | Control 2 (CThB) | Experiment 3 53.57–78.33 GHz | Experiment 4 130.0–170.0 GHz |
|---|---|---|---|---|
| GR, nmol NADPH/min × mg of protein | 89.99 ± 7.10 | 62.03 ± 5.24 * | 68.88 ± 2.67 * | 75.94 ± 6.02 ** |
| Gl-6-fDH, nmol NADPH/min × mg of protein | 42.03 ± 2.11 | 30.23 ± 1.44 * | 35.90 ± 2.00 */** | 37.42 ± 1.00 */** |
| LDHdir, nmol NADH/min × mg of protein | 39.78 ± 3.12 | 24.27 ± 1.09 * | 29.55 ± 0.89 */** | 30.90 ± 1.04 */** |
| LDHrev, nmol NADH/min × mg of protein | 164.54 ± 13.34 | 114.85 ± 10.06 * | 128.97 ± 7.53 * | 139.64 ± 6.10 */** |
| LPOplasma, RVU | 10.58 ± 0.52 | 14.99 ± 0.75 * | 12.50 ± 0.68 */** | 12.15 ± 0.59 */** |
| TAA, RVU | 0.91 ± 0.03 | 0.51 ± 0.02 * | 0.79 ± 0.03 */** | 0.59 ± 0.02 */** |
| LPOerythrocytes, RVU | 9.79 ± 0.411 | 10.47 ± 0.44 * | 7.82 ± 0.33 */** | 9.35 ± 0.47 ** |
| SOD, RVU/mg of protein | 917.67 ± 21.11 | 332.52 ± 7.65 * | 613.35 ± 14.32 */** | 702.52 ± 15.66 */** |
| Catalase, RVU/mg of protein | 30.24 ± 1.01 | 17.56 ± 0.98 * | 21.99 ± 1.53 */** | 25.38 ± 1.11 */** |
| MDAplasma, micmol/L | 1.07 ± 0.01 | 1.19 ± 0.09 * | 0.99 ± 0.02 */** | 1.025 ± 0.06 ** |
| MDAerythrocytes, micmol/L | 5.95 ± 0.07 | 10.97 ± 1.23 * | 8.79 ± 0.28 */** | 10.12 ± 1.23 * |
| Parameters | LI EMR 130.0–170.0 GHz (n = 18) | LI EMR 53.57–78.33 GHz (n = 11) | ||||
|---|---|---|---|---|---|---|
| Exposure Time (min) | Exposure Time (min) | |||||
| дo | 5 | 30 | дo | 5 | 30 | |
| R, min | 9.90 [8.00; 10.8] | 7.15 * [6.00; 8.60] | 7.60 * [6.70; 9.20] | 7.8 [6.2; 9.8] | 6.2 * [5.5; 7.7] | 6.3 * [5.2; 7.2] |
| k, min | 2.20 [2.10; 2.70] | 2.15 [1.60; 2.90] | 3.55 *,** [2.60; 4.40] | 2.2 [1.2; 2.7] | 1.8 * [1.2; 2.7] | 1.5 * [1.2; 2.0] |
| alfa, deg | 59.6 [55.8; 64.3] | 61.2 [53.0; 67.7] | 50.8 *,** [42.3; 60.2] | 68.4 [57.0; 74.1] | 70.0 [65.5; 73.3] | 69.3 [65.9; 74.0] |
| MA, mm | 61.6 [60.6; 62.9] | 61.9 * [54.1; 64.8] | 58.5 *,** [52.3; 63.0] | 68.4 [64.2; 73.8] | 70,5 [68.1; 74.6] | 68.7 [66.8; 73.5] |
| G, d/sc | 8.20 [7.80; 12.7] | 8.60 * [6.00; 9.80] | 7.50 *,** [5.80; 8.60] | 10.3 [8.8; 14.1] | 11.1 [10.6; 16.1] | 10.7 [9.7; 12.7] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Polyakova, A.G.; Soloveva, A.G.; Peretyagin, P.V.; Presnyakova, M.V.; Vaks, V.; Kornaukhov, A.V. Study of the Effect of Low-Intensity Sub- and Millimeter Waves on the Induction of Adaptation Reactions in Experimental Burn. Optics 2022, 3, 35-43. https://doi.org/10.3390/opt3010004
Polyakova AG, Soloveva AG, Peretyagin PV, Presnyakova MV, Vaks V, Kornaukhov AV. Study of the Effect of Low-Intensity Sub- and Millimeter Waves on the Induction of Adaptation Reactions in Experimental Burn. Optics. 2022; 3(1):35-43. https://doi.org/10.3390/opt3010004
Chicago/Turabian StylePolyakova, Alla Georgievna, Anna Gennadievna Soloveva, Petr Vladimirovich Peretyagin, Marina Vladimirovna Presnyakova, Vladimir Vaks, and Alexander Vasilyevich Kornaukhov. 2022. "Study of the Effect of Low-Intensity Sub- and Millimeter Waves on the Induction of Adaptation Reactions in Experimental Burn" Optics 3, no. 1: 35-43. https://doi.org/10.3390/opt3010004
APA StylePolyakova, A. G., Soloveva, A. G., Peretyagin, P. V., Presnyakova, M. V., Vaks, V., & Kornaukhov, A. V. (2022). Study of the Effect of Low-Intensity Sub- and Millimeter Waves on the Induction of Adaptation Reactions in Experimental Burn. Optics, 3(1), 35-43. https://doi.org/10.3390/opt3010004






