Morphological Evaluation of the Splenic Artery, Its Anatomical Variations and Irrigation Territory
Abstract
:1. Introduction
2. Materials and Methods
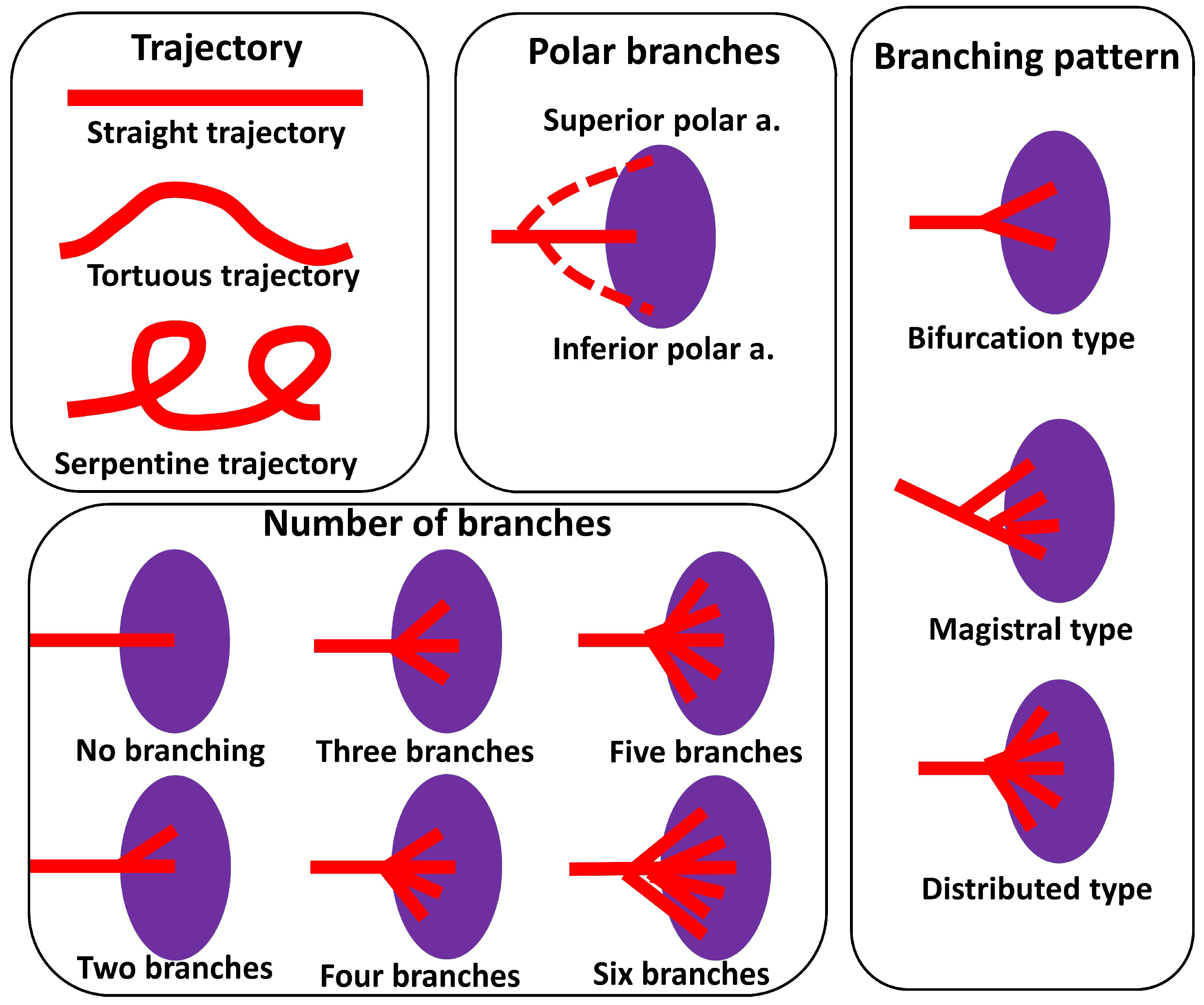
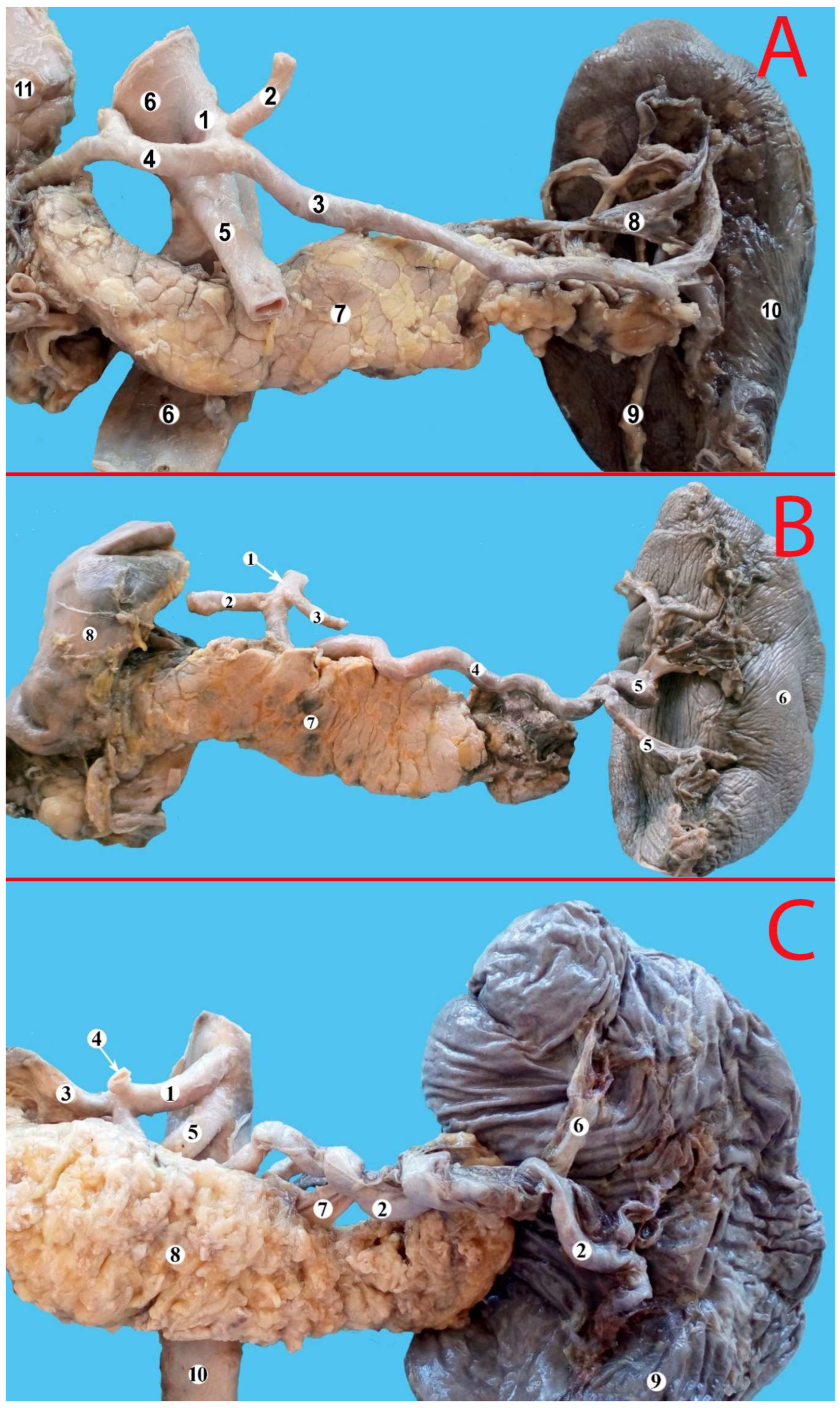
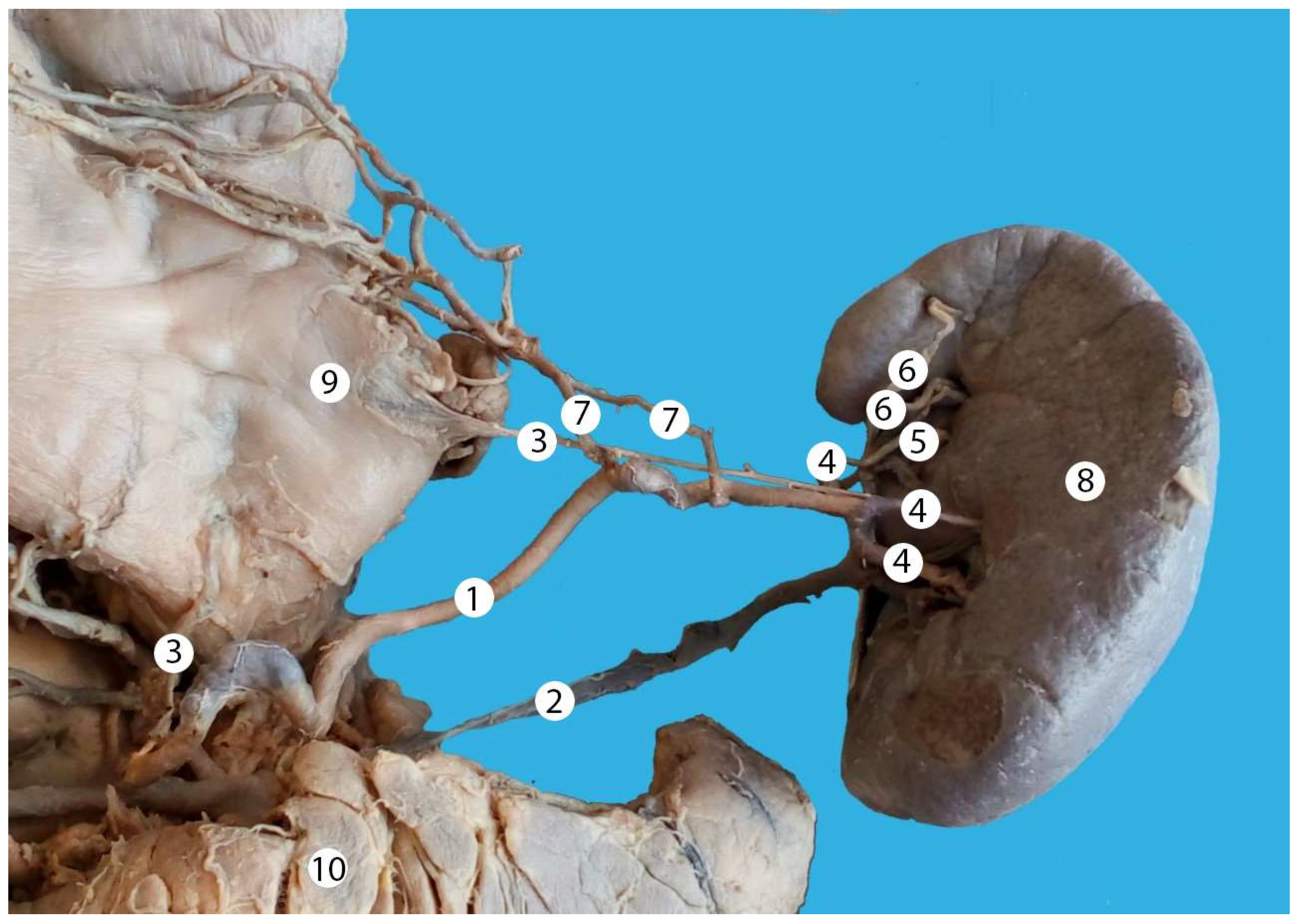
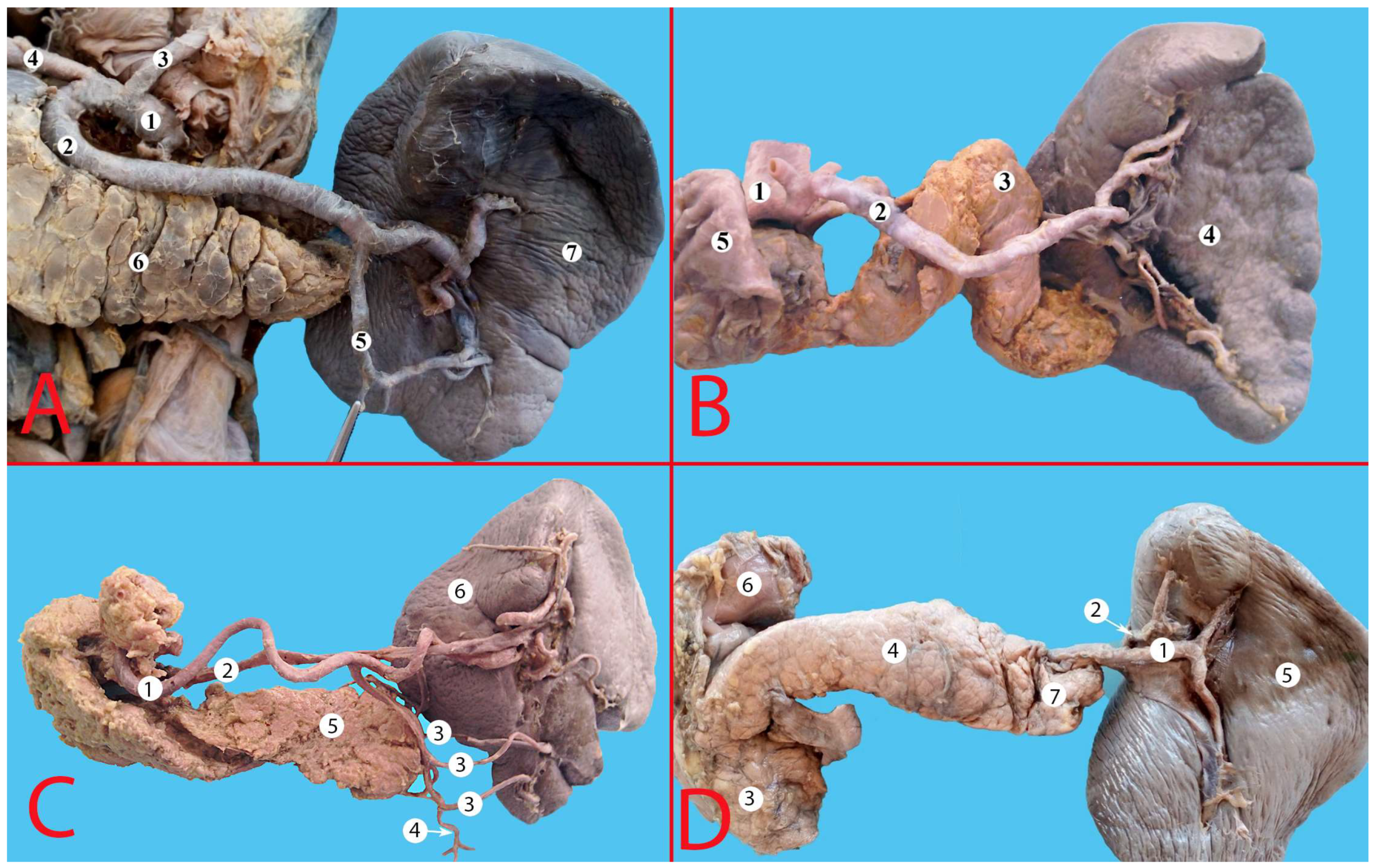
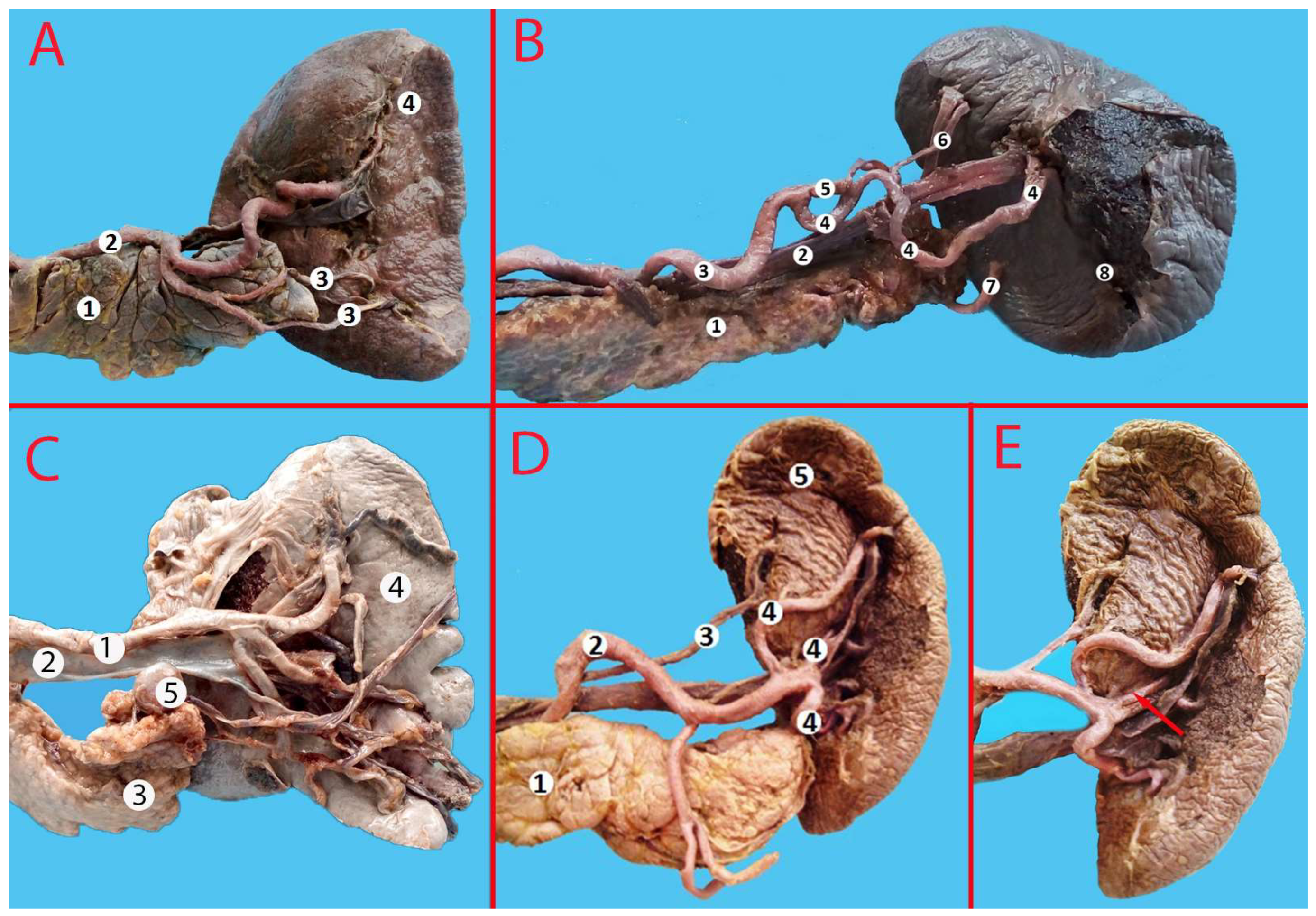
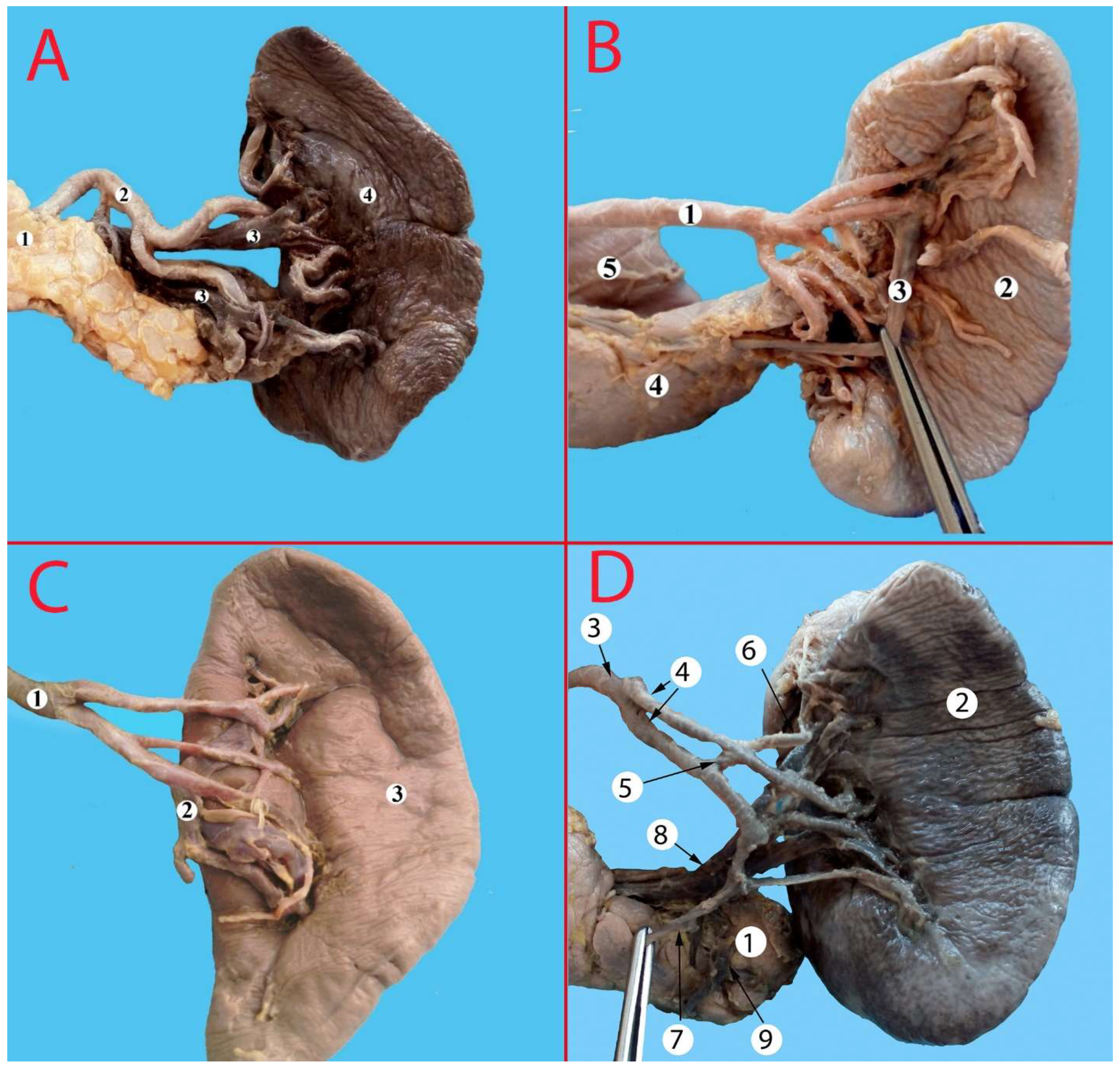
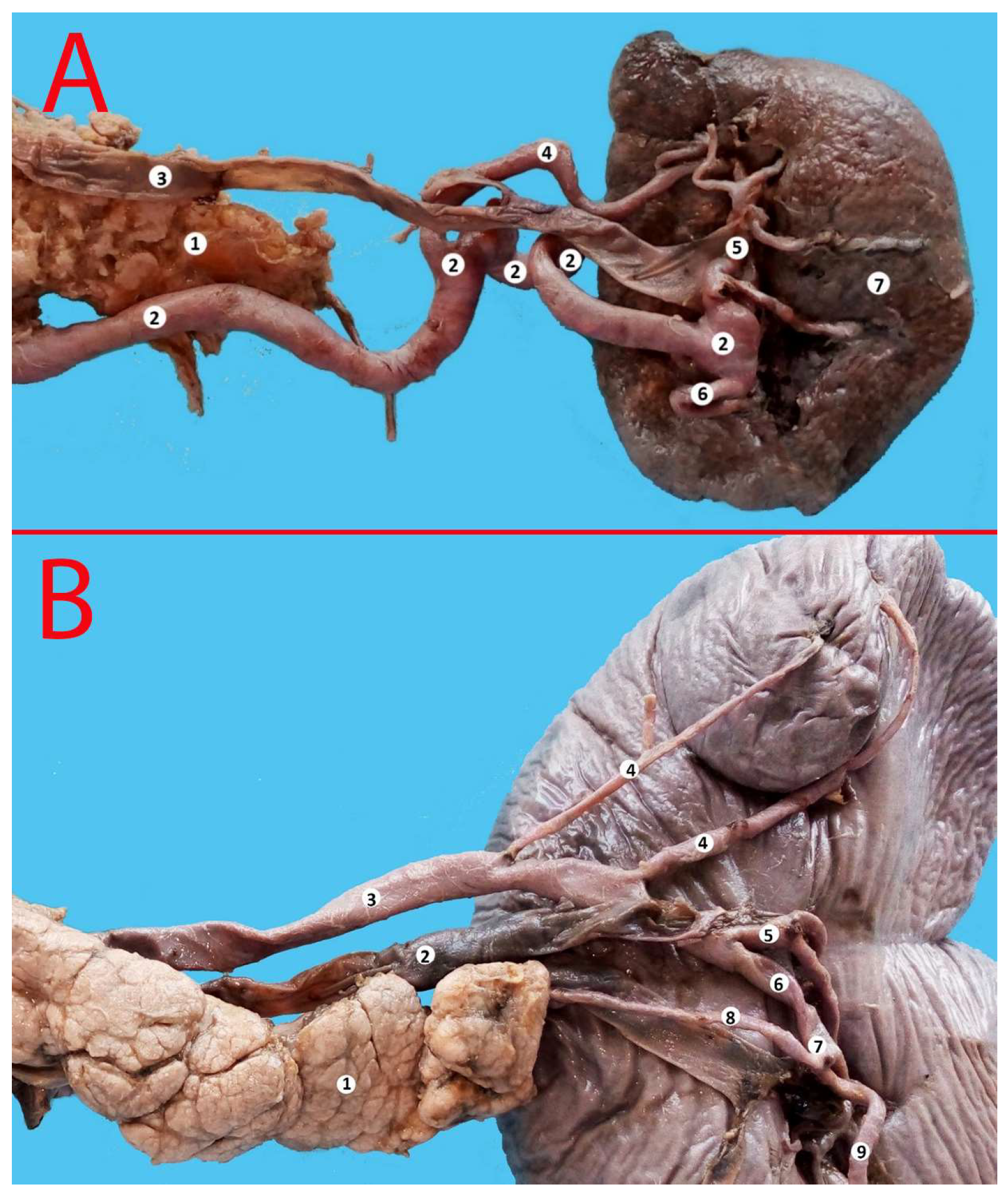
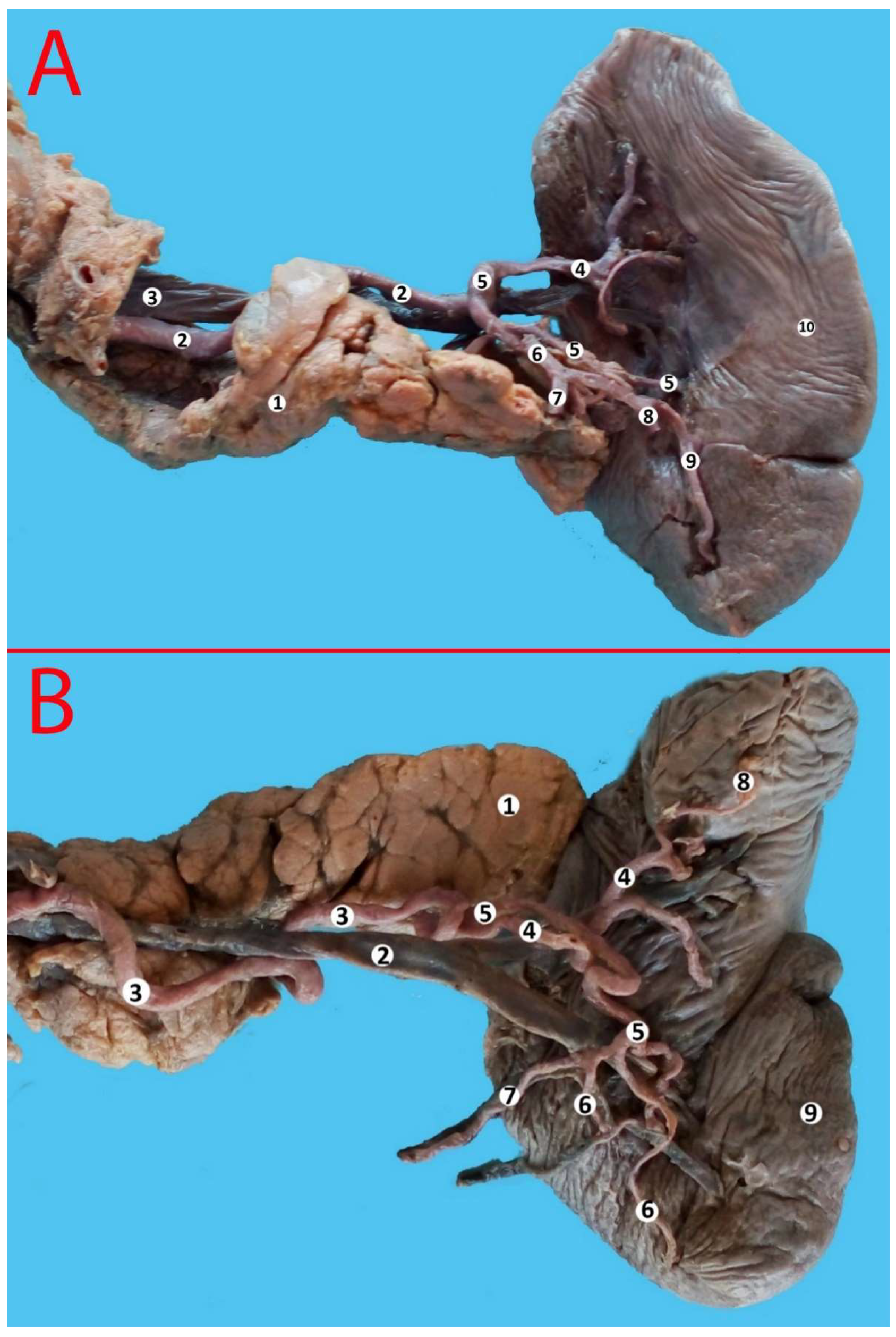
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Covantev, S.; Uzdenov, R.; Turovets, D.; Belic, O. Spleen: An organ of multiple shapes. Iberoam. J. Med. 2021, 3, 326–331. [Google Scholar] [CrossRef]
- Coccolini, F.; Montori, G.; Catena, F.; Kluger, Y.; Biffl, W.; Moore, E.E.; Reva, V.; Bing, C.; Bala, M.; Fugazzola, P.; et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J. Emerg. Surg. 2017, 12, 40. [Google Scholar] [CrossRef] [Green Version]
- Morgenstern, L. A history of Splenectomy. In Surgical Diseases of the Spleen; Hiatt, J.R., Phillips, E.H., Morgenstern, L., Eds.; Springer: Berlin/Heidelberg, Germany, 1997; pp. 3–14. [Google Scholar]
- El-Matbouly, M.; Jabbour, G.; El-Menyar, A.; Peralta, R.; Abdelrahman, H.; Zarour, A.; Al-Hassani, A.; Al-Thani, H. Blunt splenic trauma: Assessment, management and outcomes. Surgeon 2016, 14, 52–58. [Google Scholar] [CrossRef]
- Carlin, A.M.; Tyburski, J.G.; Wilson, R.F.; Steffes, C. Factors affecting the outcome of patients with splenic trauma. Am. Surgeon. 2002, 68, 232–239. [Google Scholar] [CrossRef]
- Kumari, M.; Parwez, M.; Jain, A.; Pandya, B. Management of a delayed, post-traumatic rupture of splenic artery pseudoaneurysm in a patient with life threatening co-morbidities: A treatment challenge. Int. J. Surg. Case Rep. 2020, 75, 479–482. [Google Scholar] [CrossRef]
- Madoff, D.C.; Denys, A.; Wallace, M.J.; Murthy, R.; Gupta, S.; Pillsbury, E.P.; Ahrar, K.; Bessoud, B.; Hicks, M.E. Splenic arterial interventions: Anatomy, indications, technical considerations, and potential complications. Radiographics 2005, 25 (Suppl. 1), S191–S211. [Google Scholar] [CrossRef]
- Guillon, R.; Garcier, J.M.; Abergel, A.; Mofid, R.; Garcia, V.; Chahid, T.; Ravel, A.; Pezet, D.; Boyer, L. Management of splenic artery aneurysms and false aneurysms with endovascular treatment in 12 patients. Cardiovasc. Interv. Radiol. 2003, 26, 256–260. [Google Scholar] [CrossRef]
- Poulin, E.C.; Thibault, C. The anatomical basis for laparoscopic splenectomy. Can. J. Surg. J. Can. Chir. 1993, 36, 484–488. [Google Scholar]
- Ekingen, A.; Hatipoğlu, E.S.; Hamidi, C.; Tuncer, M.C.; Ertuğrul, Ö. Splenic artery angiography: Clinical classification of origin and branching variations of splenic artery by multi-detector computed tomography angiography method. Folia Morphol. 2020, 79, 236–246. [Google Scholar] [CrossRef] [Green Version]
- Cleypool, C.G.J.; Lotgerink Bruinenberg, D.; Roeling, T.; Irwin, E.; Bleys, R. Splenic artery loops: Potential splenic plexus stimulation sites for neuroimmunomodulatory-based anti-inflammatory therapy? Clin. Anat. 2021, 34, 371–380. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, D.J.; Troquay, S.; de Jonge, W.J.; Irwin, E.D.; Vervoordeldonk, M.J.; Luyer, M.D.; Nederend, J. Morphometric analysis of the splenic artery using contrast-enhanced computed tomography (CT). Surg. Radiol. Anat. 2021, 43, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Sylvester, P.A.; Stewart, R.; Ellis, H. Tortuosity of the human splenic artery. Clin. Anat. 1995, 8, 214–218. [Google Scholar] [CrossRef]
- Golder, W.A. Tortuosity and calcification of the splenic artery. More than an additional finding. Der Radiol. 2008, 48, 1066–1067. [Google Scholar] [CrossRef]
- Fataftah, J.; Manasrah, Z.; Tayyem, R.; Qandeel, H.; Al-Omari, M.; Shatarat, A.; Badran, D.; Fataftah, J.; Manasrah, Z.; Tayyem, R.; et al. Splenic Artery Tortuosity Index on Abdominal CT Scan: Correlation with Age, Sex, BMI and Abdominal Cavity Diameters. Int. J. Morphol. 2020, 38, 17–22. [Google Scholar] [CrossRef] [Green Version]
- Michels, N.A. Blood Supply and Anatomy of the Upper Abdominal Organs; Pitman Medical Publishing Co., Ltd.: London, UK, 1995. [Google Scholar]
- Michels, N.A. The variational anatomy of the spleen and splenic artery. Am. J. Anat. 1942, 70, 21–72. [Google Scholar] [CrossRef]
- Covantev, S.; Mazuruc, N.; Belic, O. The Arterial Supply of the Distal Part of the Pancreas. Surg. Res. Pract. 2019, 2019, 5804047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Covantsev, S.; Chicu, C.; Mazuruc, N.; Belic, O. Pancreatic ductal anatomy: More than meets the eye. Surg. Radiol. Anat. 2022, 44, 1231–1238. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.H.; Xu, M.; Huang, C.M.; Li, P.; Xie, J.W.; Wang, J.B.; Lin, J.X.; Lu, J.; Chen, Q.Y.; Cao, L.L.; et al. Anatomy and influence of the splenic artery in laparoscopic spleen-preserving splenic lymphadenectomy. World J. Gastroenterol. 2015, 21, 8389–8397. [Google Scholar] [CrossRef]
- Ashok, K.R.; Kiran, T.V. Study of branching pattern of splenic artery. Int. J. Anat. Res. 2016, 4, 2073–2075. [Google Scholar]
- Krishna, M.; Oraon, S.; Thakur, N. Study of Anatomical Variation of The Segmental Branches of Splenic Artery in The Population of Jharkhand. J. Dent. Med. Sci. 2017, 16, 34–41. [Google Scholar]
- Gangadhara, R.P.; Hemasankar, C. Study on origin, course, branching pattern and morphometry of splenic artery and its branches supplying. Int. J. Curr. Res. Rev. 2014, 6, 16. [Google Scholar]
- Pandey, S.K.; Bhattacharya, S.; Mishra, R.N.; Shukla, V.K. Anatomical variations of the splenic artery and its clinical implications. Clin. Anat. 2004, 17, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Kong, S.H.; Kim, T.H.; Park, S.H.; Ang, R.R.G.; Diana, M.; Soler, L.; Suh, Y.S.; Lee, H.J.; Marescaux, J.; et al. The anatomical configuration of the splenic artery influences suprapancreatic lymph node dissection in laparoscopic gastrectomy: Analysis using a 3D volume rendering program. Surg. Endosc. 2018, 32, 3697–3705. [Google Scholar] [CrossRef] [PubMed]
- Wada, Y.; Aoki, T.; Murakami, M.; Fujimori, A.; Koizumi, T.; Kusano, T.; Matsuda, K.; Nogaki, K.; Hakozaki, T.; Shibata, H.; et al. Individualized procedures for splenic artery dissection during laparoscopic distal pancreatectomy. BMC Surg. 2020, 20, 32. [Google Scholar] [CrossRef] [PubMed]
- Xu, W.L.; Li, S.L.; Wang, Y.; Shi, B.J.; Li, M.; Li, Y.C.; Zhong, Z.Y.; Li, Z.D. Laparoscopic splenectomy: Color Doppler flow imaging for preoperative evaluation. Chin. Med. J. 2009, 122, 1203–1208. [Google Scholar] [PubMed]
- Sundar, G.; Sangeetha, V. Variation in branching pattern of splenic artery and its surgical importance. Indian J. Clin. Anat. Physiol. 2020, 7, 301–303. [Google Scholar]
- Silva, L.F.; Silveira, L.M.; Timbó, P.S.; Pinheiro, S.R.; Barros, L.V.; da Silva Filho, A.R. Morfometric study of arterial branching of the spleen compared to radiological study. Rev. Col. Bras. Cir. 2011, 38, 181–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Daisy Sahni, A.; Indar Jit, B.; Gupta, C.N.M.; Gupta, D.M.; Harjeet, E. Branches of the splenic artery and splenic arterial segments. Clin. Anat. 2003, 16, 371–377. [Google Scholar] [CrossRef]
- Shashikala Londhe, R. Study of vascular pattern in human spleen by corrosion cast method. Al Ameen J. Med. Sci. 2013, 6, 167–169. [Google Scholar]
- Liu, D.L.; Xia, S.; Xu, W.; Ye, Q.; Gao, Y.; Qian, J. Anatomy of vasculature of 850 spleen specimens and its application in partial splenectomy. Surgery 1996, 119, 27–33. [Google Scholar] [CrossRef]
- García-Porrero, J.A.; Lemes, A. Arterial segmentation and subsegmentation in the human spleen. Acta Anat. 1988, 131, 276–283. [Google Scholar] [CrossRef] [PubMed]


| SP | IP | RP | AP | Total | |
|---|---|---|---|---|---|
| Straight, n (%) | 109 (33.03) | 15 (4.55) | 16 (4.85) | 2 (0.61) | 142 (43.03) |
| Sinuous, n (%) | 56 (16.97) | 15 (4.55) | 9 (2.73) | 11 (3.33) | 91 (27.58) |
| Serpentine, n (%) | 45 (13.64) | 17 (5.15) | 7 (2.12) | 0 (0.00) | 69 (20.91) |
| Alternating, n (%) | 22 (6.67) | 2 (0.61) | 1 (0.30) | 3 (0.91) | 28 (8.48) |
| Total, n (%) | 232 (70.30) | 49 (14.85) | 33 (10.00) | 16 (4.85) | 330 (100) |
| Number of Branches | n (%) |
|---|---|
| No branching | 11 (3.33) |
| Two branches | 273 (82.73) |
| Three branches | 32 (9.70) |
| Four branches | 10 (3.03) |
| Five branches | 2 (0.61) |
| Six branches | 2 (0.61) |
| Total | 330 (100%) |
| Author, Year | Number of Specimens | SP | IP | RP | AP | References |
|---|---|---|---|---|---|---|
| Pandey et al., 2004 | 320 | 74.1% | 4.6% | 8.2% | 18.5 | [24] |
| Gangadhara et al., 2014 | 30 | 63.3% | - | 36.3% | - | [23] |
| Ashok et al., 2016 | 76 | 68% | - | 32% | - | [21] |
| Meet Krishna, 2017 | 317 | 99.3% | 6.66% | - | - | [22] |
| Zhu et al., 2018 | 169 | 36.7% | 14.2% | 49.1 | [25] | |
| Current study | 330 | 70.3% | 14.85% | 10% | 4.55% | |
| Author, Year | Number of Specimens | No Branching | Magistral Type | Distributed Type | References |
|---|---|---|---|---|---|
| Pandey et al., 2004 | 320 | 2.8% | 97.2 | [24] | |
| Xu et al., 2009 | 48 | - | 60.9 | 39.1 | [27] |
| Zheng et al., 2015 | 317 | - | 64.7 | 35.3 | [20] |
| Ashok et al., 2016 | 76 | 10.5 | 55.3 | 34.2 | [21] |
| Sangeetha, & Sundar, 2020 | 60 | 16.7 | 60 | 23.3 | [28] |
| Current study | 330 | 3.33 | 20 | 36.06 | |
| Author, Year | Number of Specimens, n | Number of Splenic Artery Branches, % | Polar Arteries, % | References | |||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | More than 3 | Superior | Inferior | Both | |||
| Liu et al., 1996 | 850 | 0.8 | 86 | 12.2 | 1 | ** 31.3 | ** 38.8 | ** 13.3 | [32] |
| Daisy Sahni et al., 2003 | 200 | - | 80 (M) 79.5 (F) | 20 (M) 19,5(F) | - | 53 | 33 | - | [30] |
| Pandey, 2004 | 320 | 2.8% | 63.1 | - | 4–18.8 6–9.7 >6–5.6 | - | [24] | ||
| Silva et al., 2011 | 60 + 30 * | - | 93.34 90 * | 6.66 10 * | - | 16% and 20% respectively | [29] | ||
| Shashikala Londhe, 2013 | 50 | 90 | 10 | - | 33 | 54 | 24.4 | [31] | |
| Gangadhara et al., 2014 | 30 | - | 80 | 16.6 | - | 26.6 | 36.6 | 16.6 | [23] |
| Zheng et al., 2015 | 317 | 6.9 | 78.9 | 13.6 | 0.6 | 16.4 | 5.05 | - | [20] |
| Meet Krishna, 2017 | 317 | - | 100 | - | - | 6.66 | - | 6.66 | [22] |
| Current study | 330 | 3.33 | 82.73 | 9.70 | 4.25 | 60.27 | 19.69 | 4.85 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Covantsev, S.; Alieva, F.; Mulaeva, K.; Mazuruc, N.; Belic, O. Morphological Evaluation of the Splenic Artery, Its Anatomical Variations and Irrigation Territory. Life 2023, 13, 195. https://doi.org/10.3390/life13010195
Covantsev S, Alieva F, Mulaeva K, Mazuruc N, Belic O. Morphological Evaluation of the Splenic Artery, Its Anatomical Variations and Irrigation Territory. Life. 2023; 13(1):195. https://doi.org/10.3390/life13010195
Chicago/Turabian StyleCovantsev, Serghei, Fariza Alieva, Karina Mulaeva, Natalia Mazuruc, and Olga Belic. 2023. "Morphological Evaluation of the Splenic Artery, Its Anatomical Variations and Irrigation Territory" Life 13, no. 1: 195. https://doi.org/10.3390/life13010195
APA StyleCovantsev, S., Alieva, F., Mulaeva, K., Mazuruc, N., & Belic, O. (2023). Morphological Evaluation of the Splenic Artery, Its Anatomical Variations and Irrigation Territory. Life, 13(1), 195. https://doi.org/10.3390/life13010195








