The Link between Diabetes and Neurodegenerative Diseases
A special issue of Cells (ISSN 2073-4409). This special issue belongs to the section "Autophagy".
Deadline for manuscript submissions: closed (5 November 2022) | Viewed by 7851
Special Issue Editor
Interests: mtorc1; autophagy; pancreatic beta cells; diabetes; mitophagy; tsc2; er-stress; mvb; exosomes; aging
Special Issues, Collections and Topics in MDPI journals
Special Issue Information
Dear Colleagues,
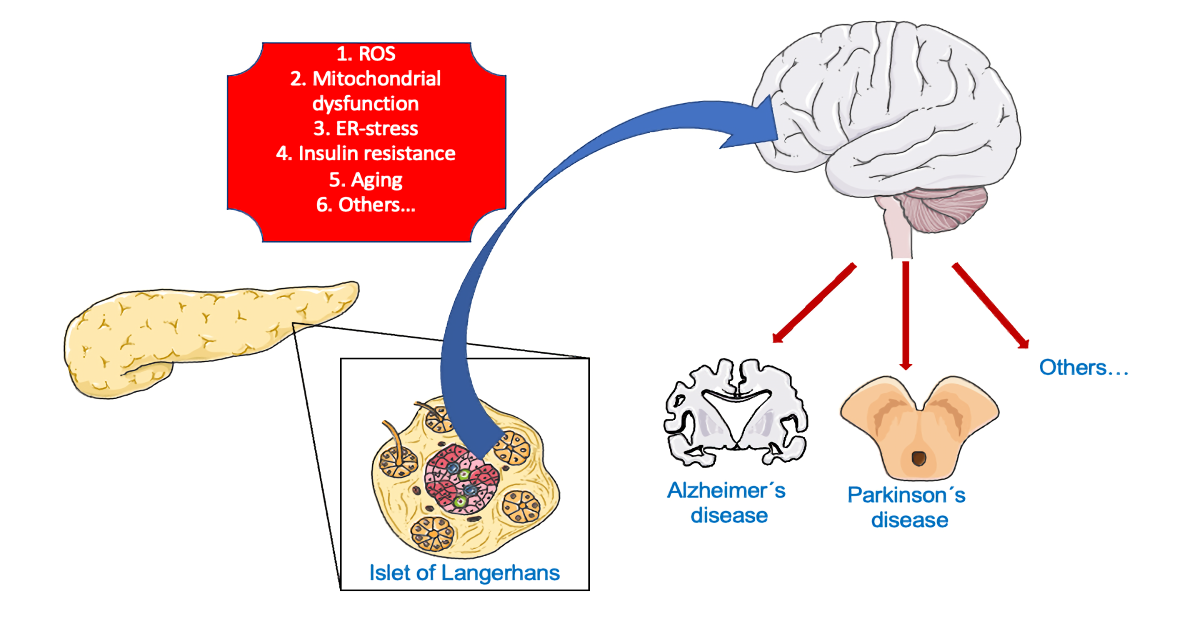
Nowadays, our society has a long life expectancy. Diabetes and neurodegeneration are two progressive and age-related groups of diseases, being interconnected. Although both pathologies have a genetic component, many other factors are involved in the appearance of both disorders. During recent years, different mechanisms have been proposed in the linkage between these two groups of affections. However, the precise molecular and cellular actors in the connection are unknown to this date.
In this Special Issue, the main pathways, molecules and structures implicated in the appearance, progression and susceptibility to suffer a neurodegenerative disease whilst having diabetes and vice versa will be analyzed.
Dr. Carlos Guillén Viejo
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All submissions that pass pre-check are peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Cells is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2700 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI's English editing service prior to publication or during author revisions.
Keywords
- type 2 diabetes
- Alzheimer’s
- Parkinson’s
- neurodegeneration
- exosomes
- amylin
- protein aggregates
- mitochondrial dysfunction
- ER stress
- autophagy
- mitophagy
- alpha-synuclein
- insulin resistance
- brain insulin resistance
- obesity
- aging






