Journal Description
Lymphatics
Lymphatics
is an international, peer-reviewed, open access journal on lymphatics and related disorders published quarterly online by MDPI.
- Open Access— free for readers, with article processing charges (APC) paid by authors or their institutions.
- Rapid Publication: manuscripts are peer-reviewed and a first decision is provided to authors approximately 32.3 days after submission; acceptance to publication is undertaken in 5.8 days (median values for papers published in this journal in the first half of 2025).
- Recognition of Reviewers: APC discount vouchers, optional signed peer review, and reviewer names published annually in the journal.
- Lymphatics is a companion journal of IJMS.
Latest Articles
Differentiating Afferent Lymphatic Channels Using a Dual-Dye Technique During Immediate Lymphatic Reconstruction
Lymphatics 2025, 3(4), 36; https://doi.org/10.3390/lymphatics3040036 - 27 Oct 2025
Abstract
►
Show Figures
Introduction: Axillary reverse mapping (ARM) aims to reduce the risk of breast cancer-related lymphedema (BCRL) by preserving and limiting dissection of arm-draining lymphatics. The ideal type of dye and the location of injection, which maximize the sparing of lymphatics and improve outcomes of
[...] Read more.
Introduction: Axillary reverse mapping (ARM) aims to reduce the risk of breast cancer-related lymphedema (BCRL) by preserving and limiting dissection of arm-draining lymphatics. The ideal type of dye and the location of injection, which maximize the sparing of lymphatics and improve outcomes of immediate lymphatic reconstruction (ILR), remain under-studied. The current literature reports inconsistent visualization of lymphatics using blue dye alone, whereas indocyanine green (ICG) near-infrared (NIR) lymphography has shown improved rates. However, optimized dual-dye workflows integrating breast–plastics co-surgery are lacking. Methods: A retrospective review of patients who underwent ILR following ALND for breast cancer between June 2021 and June 2023 was conducted. Patients who underwent ARM using our dual-dye technique were included, utilizing intradermal injections of indocyanine green (ICG) into the wrist and isosulfan blue (ISB) into the upper arm. Axillary reverse mapping channels were categorized by the type of dye used to visualize. Dye injection site, number of lymphatic channels visualized, channel diameter (mm), time-to-first channel, coordinates relative to fixed landmarks, ILR configuration, and pathologic findings were reviewed. Mann–Whitney U tests were used to compare channel visualization rates between types of dye. Results: Of 26 patients, 21 underwent dual-dye mapping and were included. A total of 115 ARM channels were identified: 99 (86%) via ICG and 29 (25%) via ISB. A total of 64 lymphaticovenous anastomoses were performed (mean: 2.46 per patient). Both dyes were identified in the axilla in only 11.7% of patients. At the end of the study, the lymphedema rate was 12%. Conclusions: We developed a reproducible dual-dye ARM technique for ALND with planned ILR, reducing lymphedema risk while maintaining oncologic safety. Dual-dye mapping reveals that proximal and distal lymphatics exhibit both overlapping and divergent drainage to axillary nodes. ICG’s higher axillary detection rate may reflect true anatomical differences or dye properties. These findings support the need for individualized lymphatic mapping during breast cancer surgery to guide preservation techniques and reduce the risk of BCRL.
Full article
Open AccessReview
Physiologic Lymphedema Surgery: Current Treatments and Future Trends
by
Ethan L. MacKenzie, Anne Huang, Min-Jeong Cho, Roman J. Skoracki and Rohini L. Kadle
Lymphatics 2025, 3(4), 35; https://doi.org/10.3390/lymphatics3040035 - 20 Oct 2025
Abstract
Lymphedema is a chronic, progressive, and debilitating disease of the lymphatic system with no current cure. Physiologic procedures, which address the underlying pathophysiology of lymphatic dysfunction, have gained traction in both treatment and prevention of lymphedema. This narrative review examines current physiologic lymphedema
[...] Read more.
Lymphedema is a chronic, progressive, and debilitating disease of the lymphatic system with no current cure. Physiologic procedures, which address the underlying pathophysiology of lymphatic dysfunction, have gained traction in both treatment and prevention of lymphedema. This narrative review examines current physiologic lymphedema surgical techniques and emerging developments in this rapidly evolving field. While the two most common physiologic surgeries remain lymphovenous bypass (LVB) and vascularized lymph node transfer (VLNT), newer physiologic surgery techniques such as vascularized lymph vessel transfer (VLVT) and lymph node to vein anastomosis (LNVA) have been described in an effort to reduce donor site morbidity, with early promising clinical outcomes. The use of bioengineering with stem cells, pro-lymphangiogenic growth factors, and biomaterials such as Biobridge can be applied in conjunction with surgery to help promote lymphangiogenesis. Technological advances in robotic surgical systems and 3D exoscopes are helping to make supermicrosurgery more technically feasible and ergonomic, and increasing accessibility to lymphedema surgery. As our surgical armamentarium expands, treatment algorithms must be updated to determine how various surgical techniques can be combined and sequenced, how the indications for physiologic surgery can be expanded, and how surgical treatment can be tailored to the patient and disease process.
Full article
Open AccessReview
Personalized Frontline Therapy in Diffuse Large B-Cell Lymphoma: Integrating Circulating Tumor DNA for Real-Time Adaptive Treatment Stratification
by
Vasisht Karri and Samir Dalia
Lymphatics 2025, 3(4), 34; https://doi.org/10.3390/lymphatics3040034 - 17 Oct 2025
Abstract
This review analyzed approximately 115 peer-reviewed studies published between 2010 and 2025, focusing on molecular subtyping and circulating tumor DNA (ctDNA)-guided approaches in Diffuse Large B-Cell Lymphoma (DLBCL). Evidence was synthesized from retrospective cohorts, prospective clinical trials, and translational studies, highlighting how molecular
[...] Read more.
This review analyzed approximately 115 peer-reviewed studies published between 2010 and 2025, focusing on molecular subtyping and circulating tumor DNA (ctDNA)-guided approaches in Diffuse Large B-Cell Lymphoma (DLBCL). Evidence was synthesized from retrospective cohorts, prospective clinical trials, and translational studies, highlighting how molecular heterogeneity, clonal evolution, and the tumor microenvironment complicate classification and treatment. While molecular subtypes such as MCD, BN2, EZB, A53, and ST2 have improved prognostication, their routine use in clinical practice remains limited due to cost, complexity, and restricted access to sequencing platforms. Tumor-informed ctDNA assays show promise for minimal residual disease (MRD) monitoring and adaptive therapy, yet their predictive power for CAR-T therapy, bispecific antibodies, and checkpoint inhibitors is still incompletely understood. Overall, the literature converges on the need for integrated strategies combining ctDNA, molecular subtyping, and immune microenvironment analysis to personalize frontline therapy.
Full article
(This article belongs to the Collection Lymphomas)
Open AccessReview
Relevance of AKT and RAS Signaling Pathways for Antibody–Drug Conjugate Immunotherapies in Acute Lymphoblastic Leukemia
by
Patrick A. H. Ehm and Christoph Rehbach
Lymphatics 2025, 3(4), 33; https://doi.org/10.3390/lymphatics3040033 - 13 Oct 2025
Abstract
Acute lymphoblastic leukemia is the most common cause of cancer-related death in children and represents a poor prognosis for patients in high-risk groups. Current treatment protocols are based on intensive polychemotherapy, which is associated with a significant toxicity profile. Due to their higher
[...] Read more.
Acute lymphoblastic leukemia is the most common cause of cancer-related death in children and represents a poor prognosis for patients in high-risk groups. Current treatment protocols are based on intensive polychemotherapy, which is associated with a significant toxicity profile. Due to their higher specificity and lower toxicity, immunotherapies based on monoclonal antibodies, in particular antibody–drug conjugates (ADCs), are revolutionizing cancer therapy. However, reports on the potential efficacy of ADC-targeted therapy in ALL and its subgroups are limited. Gene expression data suggest that potentially new ADC antigens are highly abundant in ALL subgroups and represent promising targets for cancer therapy. In addition, the PI3K/AKT and RAS/MAPK signaling pathways are often persistently activated in ALL and recent data showed that active feedback loops following inhibition of these pathways can lead to redundancy of cell surface receptors that can potentially serve as antigens for ADC treatment. Therefore, we provide here an overview of the most interesting receptors of the various ALL subgroups and discuss the influence that feedback loops of the PI3K/AKT and RAS/MAPK signaling pathways may have on increasing protein expression of the aforementioned receptors, which could lead to targeted combination therapy approaches in the future.
Full article
(This article belongs to the Special Issue Advances in Lymphoid Disorders: Immunological Insights and Therapeutic Innovations)
►▼
Show Figures

Figure 1
Open AccessCorrection
Correction: Koizumi et al. Lipoperoxides as Prognostic Markers in Pediatric B-Acute Lymphocytic Leukemia Patients Undergoing Induction Chemotherapy. Lymphatics 2025, 3, 11
by
Bruna Yukie Koizumi, Marina Rayciki Sotomayor, Carolina Coradi, Ana Luiza Goulart Starck, Anna Will Ribeiro, Maikely Bruna Leite, Maria Eduarda Pardal Simonato, Rafael Gomes Paz, Vinicius de Melo Tizzo, Stefania Tagliari Longo, Geise Ellen Broto, Fausto Celso Trigo and Carolina Panis
Lymphatics 2025, 3(4), 32; https://doi.org/10.3390/lymphatics3040032 - 13 Oct 2025
Abstract
In the original publication [...]
Full article
Open AccessReview
Gastrointestinal Lymphomas: A Comprehensive Review of Epidemiology, Clinical Features, Diagnosis, Histopathology, and Management
by
Vignesh Krishnan Nagesh, Ruchi Bhuju, Ahmed S. Mohammed, Emelyn Martinez, Marina Basta, Deepa Francis, Shraboni Dey, Maggie James, Damien Islek, Sanket Bhattarai, Mohammed A. Saafan, Shruthi Badam and Adam Atoot
Lymphatics 2025, 3(4), 31; https://doi.org/10.3390/lymphatics3040031 - 29 Sep 2025
Abstract
Gastrointestinal (GI) lymphomas are a diverse group of extranodal non-Hodgkin lymphomas primarily affecting the stomach, small intestine, and colon. They present with non-specific symptoms such as abdominal pain, weight loss, or GI bleeding, making early diagnosis challenging. Histologic subtypes vary, with mucosa-associated lymphoid
[...] Read more.
Gastrointestinal (GI) lymphomas are a diverse group of extranodal non-Hodgkin lymphomas primarily affecting the stomach, small intestine, and colon. They present with non-specific symptoms such as abdominal pain, weight loss, or GI bleeding, making early diagnosis challenging. Histologic subtypes vary, with mucosa-associated lymphoid tissue (MALT) lymphoma and diffuse large B-cell lymphoma (DLBCL) being the most common. Diagnosis involves endoscopic evaluation with biopsy, cross-sectional imaging, and often PET-CT. Management is subtype-dependent, including antibiotics for H. pylori-associated MALT lymphoma, chemotherapy, immunotherapy, and occasionally surgery. A multidisciplinary approach is essential for optimal outcomes. Core Tip: Gastrointestinal lymphomas are rare but clinically significant malignancies with variable presentations. Accurate diagnosis and tailored treatment based on the histologic subtype and site are critical, requiring close collaboration among gastroenterologists, pathologists, oncologists, and radiologists.
Full article
(This article belongs to the Collection Lymphomas)
►▼
Show Figures

Figure 1
Open AccessCase Report
Bronchiolitis Obliterans in a Young Female Patient with Paraneoplastic Pemphigus Associated with Unicentric Castleman’s Disease
by
Walid Kteiche, Vasiliki Besa, Stefanie Werther, Dirk Theegarten, Stefanie Bertram, Enno Schmidt, Anna Daniels and Silke C. Hofmann
Lymphatics 2025, 3(4), 30; https://doi.org/10.3390/lymphatics3040030 - 24 Sep 2025
Abstract
►▼
Show Figures
Background: Castleman’s disease (CD), also known as angiofollicular lymph node hyperplasia, describes a rare group of diseases manifesting with enlarged lymph nodes and various inflammatory symptoms. The association between Castleman’s disease, paraneoplastic pemphigus and bronchiolitis obliterans has been described in the literature and
[...] Read more.
Background: Castleman’s disease (CD), also known as angiofollicular lymph node hyperplasia, describes a rare group of diseases manifesting with enlarged lymph nodes and various inflammatory symptoms. The association between Castleman’s disease, paraneoplastic pemphigus and bronchiolitis obliterans has been described in the literature and is depicted thoroughly in this case. Case Presentation: We present a case of severe bronchiolitis obliterans developing in a 17-year-old female with paraneoplastic pemphigus and unicentric Castleman’s disease. Conclusion: Surgical resection of unicentric Castleman’s disease remains the treatment of choice due to its efficacy in preventing the recurrence of associated morbidity caused by bronchiolitis obliterans and paraneoplastic pemphigus.
Full article

Figure 1
Open AccessArticle
Transplanted Mesenteric Lymph Node Metastasis After Free Jejunal Reconstruction in Head and Neck Cancer
by
Yuki Asahi, Tatsuhiko Yamada, Masashi Kuroki, Yuta Sato, Yoshihiro Tanaka, Manato Matsubara, Saki Akita, Rina Kato, Ryota Iinuma, Ryo Kawaura, Hiroshi Okuda, Kosuke Terazawa, Kenichi Mori, Hirofumi Shibata, Natsuko Ueda, Keishi Kohyama, Hisakazu Kato and Takenori Ogawa
Lymphatics 2025, 3(4), 29; https://doi.org/10.3390/lymphatics3040029 - 24 Sep 2025
Abstract
►▼
Show Figures
Free jejunum is used for reconstruction after resection of advanced head and neck cancer. Postoperative transplanted mesenteric lymph nodes swelling is often experienced, but its clinical significance is unclear. This study included patients who underwent free jejunal reconstruction at Gifu University Hospital between
[...] Read more.
Free jejunum is used for reconstruction after resection of advanced head and neck cancer. Postoperative transplanted mesenteric lymph nodes swelling is often experienced, but its clinical significance is unclear. This study included patients who underwent free jejunal reconstruction at Gifu University Hospital between March 2017 and November 2023. Regarding the size change of postoperative mesenteric lymph node and risk factors, the correlation with metastasis and prognosis was investigated. This study included 51 patients, of whom 16 cases (31.4%) had postoperative mesenteric lymph node swelling and 2 cases (3.9%) had metastasis. Only two cases with metastasis showed an increase in size of 5 mm or more. Many cases without extracapsular extension and cases of salvage surgery had postoperative mesenteric lymph node swelling (p = 0.0429, p = 0.0269). No correlation was found between postoperative mesenteric lymph node swelling and prognosis. However, because all cases with metastasis were included in cases of postoperative mesenteric lymph node swelling, this could be one factor in determining whether or not metastasis occurred. The transplanted mesenteric lymph node swelling is one of the important postoperative evaluation items, and additional evaluation such as PET-CT may be recommended.
Full article

Figure 1
Open AccessCase Report
Lymphomatoid Granulomatosis and Tuberculosis, Coincidence or Cohabitation—A Case Report
by
Nicolas Giachetti, Sarah Bellal, Marianne Schwarz, Jérôme Paillassa, Aline Clavert, Mathilde Hunault-Berger and Firas Safa
Lymphatics 2025, 3(3), 28; https://doi.org/10.3390/lymphatics3030028 - 15 Sep 2025
Abstract
Background: Lymphomatoid granulomatosis (LYG) is a rare and atypical EBV-induced B-cell lymphoproliferative disorder. Clinical manifestations are mainly respiratory, with nodular infiltrates, varying in number and size, being responsible for respiratory distress. Cutaneous, hepatic, or neurological involvement is also possible. Although pathogenesis is not
[...] Read more.
Background: Lymphomatoid granulomatosis (LYG) is a rare and atypical EBV-induced B-cell lymphoproliferative disorder. Clinical manifestations are mainly respiratory, with nodular infiltrates, varying in number and size, being responsible for respiratory distress. Cutaneous, hepatic, or neurological involvement is also possible. Although pathogenesis is not clearly elucidated, quantitative or qualitative cellular immunodepression is thought to be a main factor. Here, we report a case of concomitant LYG and pulmonary tuberculosis. Case presentation: An 80-year-old female patient presented to the emergency unit for steadily increasing dyspnea, with workup revealing bilateral pulmonary nodules and mediastinal lymph node enlargement on chest imaging. Empiric antibiotic therapy was initially started with amoxicillin-clavulanate, which was later combined with azithromycin following respiratory deterioration. A CT-guided lung biopsy showed grade 2 LYG. Treatment with corticosteroids and weekly rituximab was initiated, leading to rapid improvement of respiratory symptoms. After the second dose of rituximab, sputum cultures that were initially collected were found to be positive for Mycobacterium tuberculosis. Rituximab was suspended, and antituberculous treatment was initiated. Rituximab was restarted once tuberculosis was controlled. Follow-up imaging later showed adequate control of both tuberculosis and LYG, with at least a partial remission of the latter. Conclusions: Our case highlights the importance of a complete diagnostic workup when a diagnosis of LYG is made, to avoid missing a concomitant pulmonary disease, such as tuberculosis, even when definite pathologic and clinical features of the former are present.
Full article
(This article belongs to the Special Issue Indolent Lymphomas and Lymphoreticular Proliferative Diseases)
►▼
Show Figures

Figure 1
Open AccessArticle
Non-Pneumatic Active Compression Device vs. Advanced Pneumatic Compression Device for Treating Lower Extremity Lymphedema: Impact on the Medicare-Eligible Population
by
Thomas S. Maldonado, Michael Barfield, Ron Winokur, Todd Berland, Sandi Davis, Vicky Ralph, Nancy Chatham and Stanley G. Rockson
Lymphatics 2025, 3(3), 27; https://doi.org/10.3390/lymphatics3030027 - 13 Sep 2025
Abstract
►▼
Show Figures
Objective: Chronic edema, whether systemic or localized, is often underrecognized by providers due to limited awareness of its prevalence and debilitating impact. As result, patients suffering from this condition live with suboptimal management, diminished quality of life, and increased healthcare costs. Non-pneumatic compression
[...] Read more.
Objective: Chronic edema, whether systemic or localized, is often underrecognized by providers due to limited awareness of its prevalence and debilitating impact. As result, patients suffering from this condition live with suboptimal management, diminished quality of life, and increased healthcare costs. Non-pneumatic compression devices (NPCDs) have been shown to be safe and more clinically effective in treating lymphedema (LED) than advanced pneumatic compression devices (APCD) in multiple published studies. In the latest study, the TEAYS trial, NPCDs showed superior clinical utility, better outcomes, and higher patient adherence than APCDs for managing lower extremity swelling. This sub-analysis of the TEAYS study focuses on outcomes for patients aged 65 and above diagnosed with lymphedema in the lower extremity. Methods: This trial was a randomized, crossover, head-to-head study across nine sites in the US in 2023. Patients were subjected to an initial 4-week washout period and then randomized to either the NPCD or a commercially available APCD. Patients used the randomly assigned initial device for 90 days followed by a second washout period before a 90-day use of the second device. Results: Analysis included a total of 71 patients with lower extremity lymphedema, 27 of whom were aged 65 or above, and this subset comprises the study cohort for the current study. These patients achieved statistically greater mean limb volume reduction (353.9 ± 99.17 mL) while on NPCD vs. APCD (−10.7 ± 125.59 mL). NPCD also showed significantly better improvement in overall quality of life (1.43 ± 0.45) vs. APCD (−0.10 ± 0.34). Statistically significant improvement in adherence was also observed while on NPCD (77%) vs. APCD (23%). No device-related adverse events were reported. Conclusions: For adults aged 65 and older with lower extremity lymphedema, non-pneumatic compression devices (NPCDs) demonstrated superior clinical outcomes—including greater limb volume reduction, improved mobility, higher adherence, and patient satisfaction—compared to advanced pneumatic compression devices (APCDs), supporting NPCDs as an effective, patient-preferred solution.
Full article

Figure 1
Open AccessReview
Beyond Swelling: A Review of Postoperative Lymphedema in Aesthetic Surgery
by
Varoon Phondge, Maya Dornbrand-Lo, Pooja Deshpande and Alex K. Wong
Lymphatics 2025, 3(3), 26; https://doi.org/10.3390/lymphatics3030026 - 9 Sep 2025
Abstract
Postoperative edema is a nearly universal consequence of aesthetic surgery, yet its clinical implications and potential progression to lymphedema remain underexplored. This review examines the prevalence, pathophysiology, diagnostic criteria, and management strategies for edema and lymphedema following aesthetic procedures. A comprehensive search of
[...] Read more.
Postoperative edema is a nearly universal consequence of aesthetic surgery, yet its clinical implications and potential progression to lymphedema remain underexplored. This review examines the prevalence, pathophysiology, diagnostic criteria, and management strategies for edema and lymphedema following aesthetic procedures. A comprehensive search of PubMed, Embase, and Cochrane databases identified studies involving adult patients undergoing aesthetic surgeries with documented postoperative edema or lymphedema. The review found that while edema is expected postoperatively and is generally self-limiting, persistent or disproportionate swelling may indicate early lymphedema. Risk factors include extensive liposuction, body contouring, and procedures involving lymphatic disruption. Despite its significance, lymphedema remains underdiagnosed due to a lack of standardized diagnostic criteria and low clinical suspicion. Emerging imaging modalities, such as indocyanine green lymphography, enhance early detection, while conservative treatments, such as manual lymphatic drainage, compression, and physical therapy, remain first-line interventions. Increased awareness among surgeons and incorporation of lymphatic-preserving techniques are vital to reducing morbidity. This review underscores the importance of distinguishing transient edema from chronic lymphedema and calls for further research to establish evidence-based guidelines for diagnosis, prevention, and management of postoperative lymphedema in aesthetic surgery.
Full article
Open AccessReview
Epidemiology of Systemic Light-Chain (AL) Amyloidosis
by
Rafael Ríos-Tamayo
Lymphatics 2025, 3(3), 25; https://doi.org/10.3390/lymphatics3030025 - 14 Aug 2025
Abstract
►▼
Show Figures
Systemic light-chain (AL) amyloidosis is a challenging, complex and heterogeneous disease. AL amyloidosis is classified under the category of plasma cell neoplasms and other diseases with paraproteins in the fifth edition of the World Health Organization classification of lymphoid tumors. Epidemiological information is
[...] Read more.
Systemic light-chain (AL) amyloidosis is a challenging, complex and heterogeneous disease. AL amyloidosis is classified under the category of plasma cell neoplasms and other diseases with paraproteins in the fifth edition of the World Health Organization classification of lymphoid tumors. Epidemiological information is limited, largely due to its low incidence and the lack of a global network of population-based specific registries. Despite recent advances, AL amyloidosis is still considered an incurable disease. The presence of a precursor disease, particularly monoclonal gammopathy of uncertain significance, is the main consolidated risk factor. Limited knowledge about other risk factors precludes the possibility of establishing preventive measures. A relevant percentage of AL amyloidosis patients fulfill the current diagnostic criteria of multiple myeloma. Incidence should be evaluated in the setting of population-based studies. On the one hand, incidence shows a slightly increasing pattern. On the other hand, survival is progressively increasing. Consequently, prevalence is also rising. Early mortality, commonly associated with advanced heart involvement, remains a serious drawback to improve the outcome. Epidemiology represents the first level of heterogeneity in AL amyloidosis. Both genomic and clinical epidemiological research in systemic AL amyloidosis have a crucial role in the global strategy to combat this multifaceted disease.
Full article

Figure 1
Open AccessReview
Precision Oncology in Hodgkin’s Lymphoma: Immunotherapy and Emerging Therapeutic Frontiers
by
Adit Singhal, David Mueller, Benjamin Ascherman, Pratik Shah, Wint Yan Aung, Edward Zhou and Maria J. Nieto
Lymphatics 2025, 3(3), 24; https://doi.org/10.3390/lymphatics3030024 - 6 Aug 2025
Abstract
►▼
Show Figures
Hodgkin’s Lymphoma (HL) affects approximately 8500 individuals annually in the United States. The 5-year relative survival rate has improved to 88.5%, driven by transformative advances in immunotherapy and precision oncology. The integration of Brentuximab vedotin (BV) and immune checkpoint inhibitors (ICIs) has redefined
[...] Read more.
Hodgkin’s Lymphoma (HL) affects approximately 8500 individuals annually in the United States. The 5-year relative survival rate has improved to 88.5%, driven by transformative advances in immunotherapy and precision oncology. The integration of Brentuximab vedotin (BV) and immune checkpoint inhibitors (ICIs) has redefined treatment paradigms. The phase III SWOG S1826 trial established nivolumab plus doxorubicin, vinblastine, and dacarbazine (N + AVD) as an emerging new standard for advanced-stage HL, achieving a 2-year progression-free survival (PFS) of 92% compared to 83% for BV plus AVD (HR 0.48, 95% CI: 0.33–0.70), with superior safety, particularly in patients over 60. In relapsed/refractory HL, pembrolizumab outperforms BV, with a median PFS of 13.2 versus 8.3 months (HR 0.65, 95% CI: 0.48–0.88), as demonstrated in the KEYNOTE-204 trial. Emerging strategies, including novel ICI combinations, minimal residual disease (MRD) monitoring via circulating tumor DNA (ctDNA), and artificial intelligence (AI)-driven diagnostics, promise to further personalize therapy. This review synthesizes HL’s epidemiology, pathogenesis, diagnostic innovations, and therapeutic advances, highlighting the role of precision medicine in addressing unmet needs and disparities in HL care.
Full article

Figure 1
Open AccessReview
A Review of the Latest Updates in Cytogenetic and Molecular Classification and Emerging Approaches in Identifying Abnormalities in Acute Lymphoblastic Leukemia
by
Chaimae El Mahdaoui, Hind Dehbi and Siham Cherkaoui
Lymphatics 2025, 3(3), 23; https://doi.org/10.3390/lymphatics3030023 - 5 Aug 2025
Abstract
Acute lymphoblastic leukemia (ALL) is a heterogeneous hematologic malignancy defined by the uncontrolled proliferation of lymphoid precursors. Accurate diagnosis and effective therapeutic strategies hinge on a comprehensive understanding of the genetic and molecular landscape of ALL. This review synthesizes the latest updates in
[...] Read more.
Acute lymphoblastic leukemia (ALL) is a heterogeneous hematologic malignancy defined by the uncontrolled proliferation of lymphoid precursors. Accurate diagnosis and effective therapeutic strategies hinge on a comprehensive understanding of the genetic and molecular landscape of ALL. This review synthesizes the latest updates in cytogenetic and molecular classifications, emphasizing the 2022 World Health Organization (WHO) and International Consensus Classification (ICC) revisions. Key chromosomal alterations such as BCR::ABL1 and ETV6::RUNX1 and emerging subtypes including Ph-like ALL, DUX4, and MEF2D rearrangements are examined for their prognostic significance. Furthermore, we assess novel diagnostic tools, notably next-generation sequencing (NGS) and optical genome mapping (OGM). While NGS excels at identifying point mutations and small indels, OGM offers high-resolution structural variant detection with 100% sensitivity in multiple validation studies. These advancements enhance our grasp of leukemogenesis and pave the way for precision medicine in both B- and T-cell ALL. Ultimately, integrating these innovations into routine diagnostics is crucial for personalized patient management and improving clinical outcomes.
Full article
(This article belongs to the Collection Acute Lymphoblastic Leukemia (ALL))
Open AccessArticle
Induction of Sustained Remissions Associated with Immune Activation by Idelalisib in Patients with Follicular Lymphoma
by
Anna-Carina Hund, Jörg Larsen and Gerald G. Wulf
Lymphatics 2025, 3(3), 22; https://doi.org/10.3390/lymphatics3030022 - 1 Aug 2025
Abstract
Phosphatidylinositol-3-kinase (PI3K) inhibition has emerged as a therapeutic option against indolent lymphoma, including relapsed follicular lymphoma (FL). While inhibition of active signaling in the lymphoma cell represents the primary mode of action, PI3K inhibition also exerts immunomodulatory effects. Here we have analyzed 17
[...] Read more.
Phosphatidylinositol-3-kinase (PI3K) inhibition has emerged as a therapeutic option against indolent lymphoma, including relapsed follicular lymphoma (FL). While inhibition of active signaling in the lymphoma cell represents the primary mode of action, PI3K inhibition also exerts immunomodulatory effects. Here we have analyzed 17 consecutive advanced treatment line FL patients treated with the delta-selective PI3K inhibitor idelalisib in a retrospective single-center observational study, with a specific focus on response and immune effects. Eleven patients achieved complete remission (CR) or partial remission (PR) with median response duration of 22 (11–88) months following a median idelalisib exposure of 15 (4–88) months. Disease response persisted in three patients for a median of 37 (21–63) months following cessation of idelalisib without another therapy being initiated. Autoimmune side effects occurred in eight of the eleven patients who responded, compared to none in six patients whose disease did not respond. In conclusion, a time-limited exposure to idelalisib may induce sustained remissions in a portion of patients with recurrent and/or refractory (r/r) FL, suggesting immunomodulatory effects of PI3K inhibition to be involved in the control of the disease.
Full article
(This article belongs to the Collection Lymphomas)
►▼
Show Figures

Figure 1
Open AccessReview
Genetic Landscape of Kawasaki Disease: An Update
by
Taru Goyal, Saniya Sharma, Rakesh Kumar Pilania, Kajol Jawallia, Sanchi Chawla, Madhubala Sharma, Monica Rawat, Vaishali Thakur, Urvi Arya, Anoop Kumar, Manpreet Dhaliwal, Vignesh Pandiarajan, Amit Rawat and Surjit Singh
Lymphatics 2025, 3(3), 21; https://doi.org/10.3390/lymphatics3030021 - 20 Jul 2025
Cited by 1
Abstract
Kawasaki disease (KD), first identified in 1967 by Dr. Tomisaku Kawasaki, is an acute, self-limited vasculitis and remains the leading cause of acquired heart disease in children worldwide, particularly affecting those under the age of five. Clinically, it presents with persistent fever, mucocutaneous
[...] Read more.
Kawasaki disease (KD), first identified in 1967 by Dr. Tomisaku Kawasaki, is an acute, self-limited vasculitis and remains the leading cause of acquired heart disease in children worldwide, particularly affecting those under the age of five. Clinically, it presents with persistent fever, mucocutaneous inflammation, skin rashes, and lymphadenopathy, with a marked tendency to involve the coronary arteries, potentially leading to serious complications such as coronary artery aneurysms. Despite extensive research spanning more than five decades, the precise etiology of KD remains unclear. However, accumulating evidence supports the significant role of genetic predisposition, highlighting the contribution of inherited factors in modulating immune responses and influencing disease susceptibility and severity. Emerging evidence highlights genetic susceptibility as pivotal, with genome-wide studies identifying polymorphisms in immune-related genes, such as ITPKC, CASP3, BLK, CD40, and ORAI1, which modulate disease risk and coronary complications. Epigenetic mechanisms, including DNA methylation and non-coding RNAs, bridge the gap between genetic and environmental factors, regulating immune responses and endothelial activation. Furthermore, emerging insights into autophagy-related processes provide a deeper understanding of the molecular mechanisms underlying the disease. This review aims to explore the current knowledge on the genetic landscape of KD, examine how these findings contribute to our understanding of its pathophysiology, and investigate the potential for genetically targeted therapeutic strategies in the future.
Full article
Open AccessReview
A Review of KSHV/HHV8-Associated Neoplasms and Related Lymphoproliferative Lesions
by
Jamie Rigney, Kevin Zhang, Michael Greas and Yan Liu
Lymphatics 2025, 3(3), 20; https://doi.org/10.3390/lymphatics3030020 - 15 Jul 2025
Abstract
►▼
Show Figures
There has been extensive research on the KSHV/HHV8 virus, which has led to a better understanding of viral transmission, pathogenesis, viral-driven lymphoid proliferation, neoplastic transformation, and how we might combat these processes clinically. On an extensive review of the literature, only two true
[...] Read more.
There has been extensive research on the KSHV/HHV8 virus, which has led to a better understanding of viral transmission, pathogenesis, viral-driven lymphoid proliferation, neoplastic transformation, and how we might combat these processes clinically. On an extensive review of the literature, only two true KSHV/HHV8-positive lymphoid neoplasms are described: primary effusion lymphoma (PEL), which can also present as solid or extracavitary primary effusion lymphoma (EC-PEL) and diffuse large B-cell lymphoma (DLBCL). Two lymphoproliferative disorders have also been described, and while they are not true monotypic neoplasms, these lesions can transform into neoplasms: KSHV/HHV8-positive germinotropic lymphoproliferative disorder (GLPD) and multicentric Castleman disease (MCD). This review provides a somewhat concise overview of information related to KSHV/HHV8-positive lymphoid neoplasms and pertinent associated lymphoproliferative lesions.
Full article

Figure 1
Open AccessPerspective
Biological Age, Aging Clocks, and the Interplay with Lymphoid Neoplasms: Mechanisms and Clinical Frontiers
by
Xiaocan Wu, Hanna Liu and Kejun Ying
Lymphatics 2025, 3(3), 19; https://doi.org/10.3390/lymphatics3030019 - 11 Jul 2025
Abstract
►▼
Show Figures
Lymphoid neoplasms (LN), a diverse group of malignancies arising from lymphocytes, exhibit a striking increase in incidence with chronological age, suggesting a deep connection with the aging process. While chronological age remains a primary risk factor, the concept of biological age, reflecting an
[...] Read more.
Lymphoid neoplasms (LN), a diverse group of malignancies arising from lymphocytes, exhibit a striking increase in incidence with chronological age, suggesting a deep connection with the aging process. While chronological age remains a primary risk factor, the concept of biological age, reflecting an individual’s physiological state and susceptibility to age-related diseases, offers a more nuanced understanding of this relationship. Aging clocks, particularly epigenetic clocks based on DNA methylation, provide quantitative measures of biological age and have revealed associations between accelerated aging and increased cancer risk, including LN. Immunosenescence, the age-related decline in immune function characterized by thymic involution, altered lymphocyte populations, and chronic inflammation (inflammaging), appears to be a key mechanistic link between aging and LN development, potentially providing a more accurate predictor of cancer risk than mutation accumulation alone. Accelerated biological aging, measured by various clocks, correlates with LN risk and progression (e.g., in chronic lymphocytic leukemia), and may influence treatment tolerance and outcomes, particularly in older adults who are often burdened by frailty and comorbidities like sarcopenia. Integrating biological age assessments into clinical practice holds promise for refining diagnosis, prognosis, and personalizing treatment strategies (including guiding intensity and considering anti-aging interventions), and improving outcomes for patients with LN. This review synthesizes the current understanding of the intricate relationship between LN, immunosenescence, biological age, and aging clocks, highlighting clinical implications and key future research directions aimed at translating these insights into better patient care.
Full article

Graphical abstract
Open AccessReview
Immediate Lymphatic Reconstruction: The Value of a Two Team Approach
by
Amanda Fazzalari, Ryoko Hamaguchi, Candice Leach, Justin Broyles and Anna Weiss
Lymphatics 2025, 3(3), 18; https://doi.org/10.3390/lymphatics3030018 - 8 Jul 2025
Abstract
►▼
Show Figures
Breast cancer-related lymphedema (BCRL) is a debilitating complication in breast cancer survivors, with axillary lymph node dissection (ALND) as the greatest independent risk factor. Beyond non-surgical therapies such as complete decongestive and compression therapy, there has been increased interest in immediate microsurgical reconstruction
[...] Read more.
Breast cancer-related lymphedema (BCRL) is a debilitating complication in breast cancer survivors, with axillary lymph node dissection (ALND) as the greatest independent risk factor. Beyond non-surgical therapies such as complete decongestive and compression therapy, there has been increased interest in immediate microsurgical reconstruction via immediate lymphatic reconstruction (ILR) anastomosing transected lymphatic vessels to a local venous recipient at the time of ALND to mitigate the risks of BCRL. This work provides a scoping review of the landscape surrounding ILR, spanning the updated literature investigating patient outcomes, current accepted best practices, and critical components of surgical techniques for a successful multidisciplinary approach. While limited by heterogeneity in the methods of lymphedema detection, a growing body of work demonstrates the protective effects of ILR. From the pioneering work by Boccardo et al. in 2009 and his introduction of Lymphatic Microsurgical Preventive Healing Approach (LYMPHA) using an intussusception-type end-to-end microanastmosis, to the first randomized control trial by Coriddi in 2023, which importantly employed relative upper extremity volume change as an outcome measure to circumvent the confounding effects of body size and BMI, the current literature supports ILR following ALND in the prevention of BCRL. Collaboration between the oncologic breast surgeon and reconstructive microsurgeon are central to the success of ILR. Critical components for operative success include preoperative and intraoperative lymphatic mapping, preservation of suitable venous targets, availability of supermicrosurgical instruments and sutures, as well as aptitude with a variety of microsurgical anastomotic techniques.
Full article
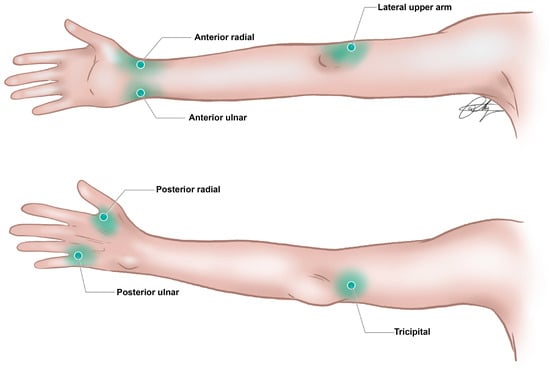
Figure 1
Open AccessReview
Cancer Metastasis Through the Lymphatics: Invasion and Dissemination
by
Chien-An A. Hu, Christina Baum and Yahui Xie
Lymphatics 2025, 3(3), 17; https://doi.org/10.3390/lymphatics3030017 - 24 Jun 2025
Abstract
►▼
Show Figures
Cancer metastasis often accounts for the primary cause of cancer-related mortality, with the lymphatic system playing a pivotal role in the dissemination of malignant cells. While hematogenous vessel spread is commonly associated with distant organ metastasis, the lymphatic system serves as an early
[...] Read more.
Cancer metastasis often accounts for the primary cause of cancer-related mortality, with the lymphatic system playing a pivotal role in the dissemination of malignant cells. While hematogenous vessel spread is commonly associated with distant organ metastasis, the lymphatic system serves as an early conduit for tumor cell invasion and dissemination. The process of lymphatic metastasis is a highly coordinated sequence of events that involves cancer cell invasion, intravasation into lymphatic vessels, survival, transport, and colonization of regional lymph nodes (LNs). Cancerous cells then establish micro-metastases at the colonized sites and expand in the new microenvironment, ultimately resulting in the generation of secondary tumors. Tumor-secreted factors, such as vascular endothelial growth factors (VEGF-C and VEGF-D), contribute to metastasis through lymphangiogenesis, the formation of new lymphatic vessels. In addition, cancer cells utilize pre-existing chemokine signaling pathways by expressing chemokine receptors, such as CCR7, which bind to chemokine ligands, such as CCL19 and CCL21, to facilitate targeted migration into the lymphatic vessels. LNs are often the initial sites for metastasis and therefore are indicators of distant organ involvement. It is well established that the location and extent of LN involvement provides significant prognostic information, although the optimal treatment approach for LN metastases remains a subject of debate. Understanding the mechanisms of lymphatic metastasis offers potential therapeutic targets to mitigate cancer progression.
Full article

Figure 1
Highly Accessed Articles
Latest Books
E-Mail Alert
News
Topics
Topic in
Biophysica, CIMB, IJMS, IJTM, Lymphatics, Sci. Pharm.
Smart Delivery Systems for Biomolecular Therapeutics
Topic Editors: Biana Godin, Vivek GuptaDeadline: 31 October 2026

Conferences
Special Issues
Special Issue in
Lymphatics
Chronic Lymphocytic Leukemia (CLL): From Benchside to Bedside
Guest Editor: Varsha GandhiDeadline: 30 December 2025
Special Issue in
Lymphatics
New Lymphology Combined with Lymphatic Physiology, Innate Immunology, and Oncology
Guest Editor: Toshio OhhashiDeadline: 30 December 2025
Special Issue in
Lymphatics
Radiation Therapy in Hematological Malignancies in the Era of Cellular Therapy
Guest Editor: Bouthaina S. DabajaDeadline: 30 December 2025
Special Issue in
Lymphatics
Adult Acute Lymphoblastic Leukemia (Adult ALL)
Guest Editor: Nicholas J. ShortDeadline: 28 February 2026
Topical Collections
Topical Collection in
Lymphatics
Acute Lymphoblastic Leukemia (ALL)
Collection Editors: Nitin Jain, Ibrahim Aldoss
Topical Collection in
Lymphatics
Radiation Oncology
Collection Editors: Bouthaina S. Dabaja, Andrea K. Ng, Paolo Strati, Michael T. Spiotto, Hans Theodor Eich, Nicholas J. Short, N. George Mikhaeel