Smart Consumer Wearables as Digital Diagnostic Tools: A Review
Abstract
:1. Introduction
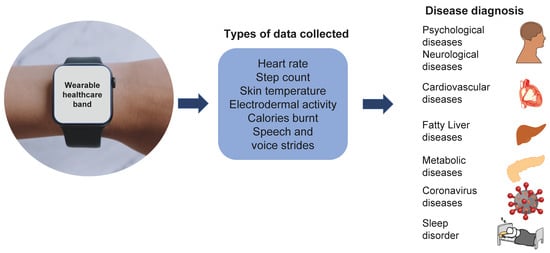
2. Wearables as Digital Diagnostics
2.1. Cardiovascular Diseases
2.2. Neurological Disorders and Stress
2.3. Fatty Liver Diseases
2.4. Corona Virus Diseases
2.5. Metabolic Disorders
2.6. Sleep Quality
2.7. Psychological Illness
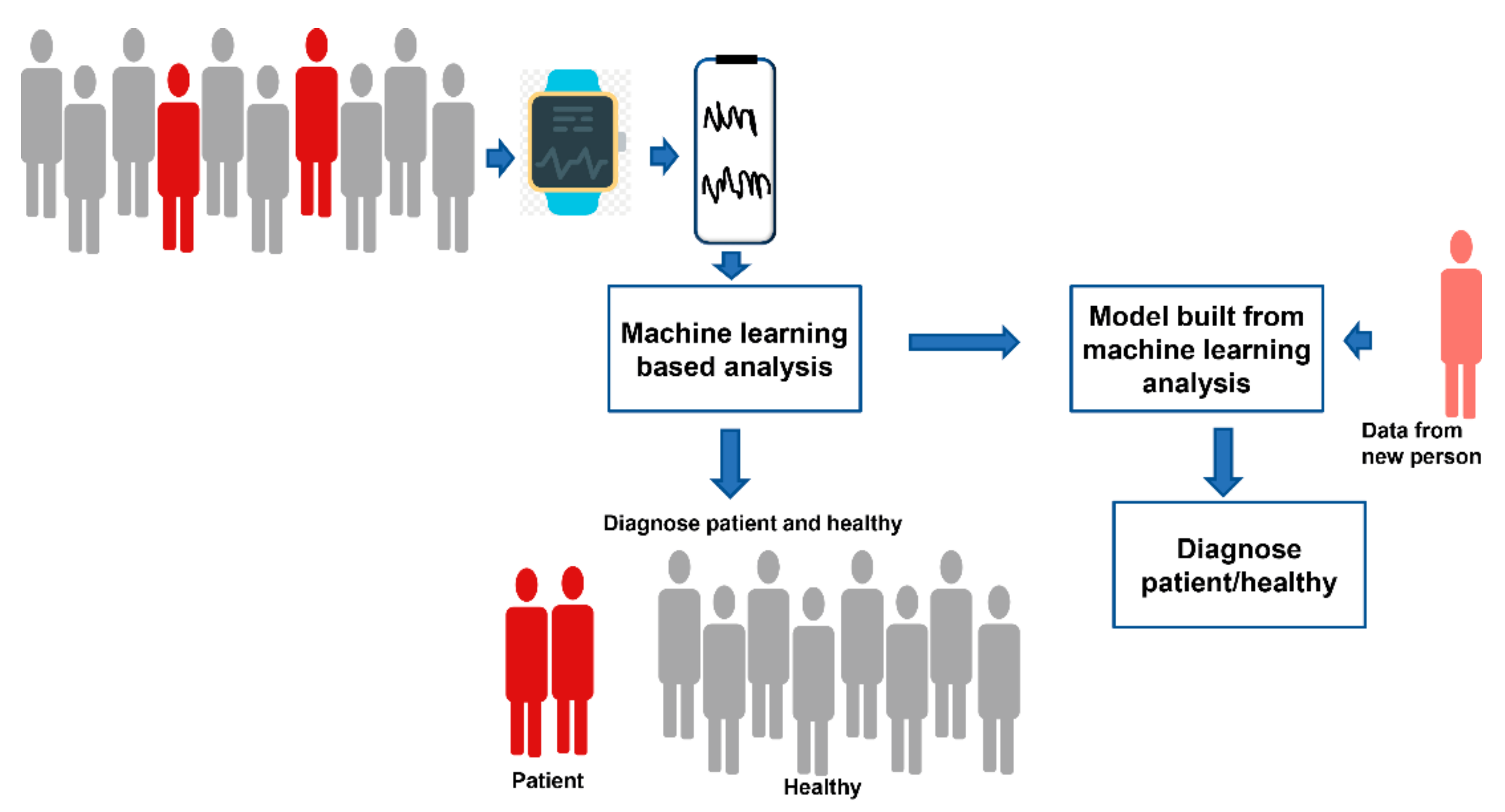
3. Role of Machine Learning in Diagnostics
4. Future Perspectives and Challenges
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, X.; Dunn, J.; Salins, D.; Zhou, G.; Zhou, W.; Schüssler-Fiorenza Rose, S.M.; Perelman, D.; Colbert, E.; Runge, R.; Rego, S.; et al. Digital Health: Tracking Physiomes and Activity Using Wearable Biosensors Reveals Useful Health-Related Information. PLoS Biol. 2001, 15, e2001402. [Google Scholar] [CrossRef] [PubMed]
- Ye, S.; Feng, S.; Huang, L.; Bian, S. Recent Progress in Wearable Biosensors: From Healthcare Monitoring to Sports Analytics. Biosensors 2020, 10, 205. [Google Scholar] [CrossRef] [PubMed]
- El-Rashidy, N.; El-Sappagh, S.; Riazul Islam, S.M.; El-Bakry, H.M.; Abdelrazek, S. Mobile Health in Remote Patient Monitoring for Chronic Diseases: Principles, Trends, and Challenges. Diagnostics 2021, 11, 607. [Google Scholar] [CrossRef] [PubMed]
- Cosoli, G.; Scalise, L.; Poli, A.; Spinsante, S. Wearable devices as a valid support for diagnostic excellence: Lessons from a pandemic going forward. Health Technol. 2021, 11, 673–675. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, A.; Mikalsen, M.H.; Woldaregay, A.Z.; Muzny, M.; Hartvigsen, G.; Hopstock, L.A.; Grimsgaard, S. Using Fitness Trackers and Smartwatches to Measure Physical Activity in Research: Analysis of Consumer Wrist-Worn Wearables. J. Med. Internet Res. 2018, 20, e110. [Google Scholar] [CrossRef] [PubMed]
- Ometov, A.; Shubina, V.; Klus, L.; Skibińska, J.; Saafi, S.; Pascacio, P.; Flueratoru, L.; Gaibor, D.Q.; Chukhno, N.; Chukhno, O.; et al. A Survey on Wearable Technology: History, State-of-the-Art and Current Challenges. Comput. Netw. 2021, 193, 108074. [Google Scholar] [CrossRef]
- Lu, L.; Zhang, J.; Xie, Y.; Gao, F.; Xu, S.; Wu, X.; Ye, Z. Wearable Health Devices in Health Care: Narrative Systematic Review. JMIR mHealth uHealth 2020, 8, e18907. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, S.M.A.; Mahgoub, I.; Du, E.; Leavitt, M.A.; Asghar, W. Advances in healthcare wearable devices. NPJ Flex. Electron. 2021, 5, 9. [Google Scholar] [CrossRef]
- Chowdhury, M.E.H.; Khandakar, A.; Alzoubi, K.; Mansoor, S.; Tahir, A.M.; Reaz, M.B.I.; Emadi, N. Al Real-Time Smart-Digital Stethoscope System for Heart Diseases Monitoring. Sensors 2019, 19, 2781. [Google Scholar] [CrossRef]
- Bogu, G.K.; Snyder, M.P. Deep learning-based detection of COVID-19 using wearables data. MedRxiv 2021. [Google Scholar] [CrossRef]
- Dunn, J.; Runge, R.; Snyder, M. Wearables and the medical revolution. Per. Med. 2018, 15, 429–448. [Google Scholar] [CrossRef]
- Chowdhury, M.E.H.; Khandakar, A.; Qiblawey, Y.; Bin, M.; Reaz, I.; Islam, M.T.; Touati, F. Machine Learning in Wearable Biomedical Systems. In Sports Science and Human Health—Different Approaches; Marinho, D.A., Neiva, H.P., Johnson, C.P., Mohamudally, N., Eds.; IntechOpen: London, UK, 2020; ISBN 978-1-83880-392-6. [Google Scholar]
- Wang, Y.C.; Xu, X.; Hajra, A.; Apple, S.; Kharawala, A.; Duarte, G.; Liaqat, W.; Fu, Y.; Li, W.; Chen, Y.; et al. Current Advancement in Diagnosing Atrial Fibrillation by Utilizing Wearable Devices and Artificial Intelligence: A Review Study. Diagnostics 2022, 12, 689. [Google Scholar] [CrossRef] [PubMed]
- Torres-Soto, J.; Ashley, E.A. Multi-task deep learning for cardiac rhythm detection in wearable devices. NPJ Digit. Med. 2020, 3, 116. [Google Scholar] [CrossRef]
- Tang, J.; El Atrache, R.; Yu, S.; Asif, U.; Jackson, M.; Roy, S.; Mirmomeni, M.; Cantley, S.; Sheehan, T.; Schubach, S.; et al. Seizure detection using wearable sensors and machine learning: Setting a benchmark. Epilepsia 2021, 62, 1807–1819. [Google Scholar] [CrossRef]
- Mishra, T.; Wang, M.; Metwally, A.A.; Bogu, G.K.; Brooks, A.W.; Bahmani, A.; Alavi, A.; Celli, A.; Higgs, E.; Dagan-Rosenfeld, O.; et al. Pre-symptomatic detection of COVID-19 from smartwatch data. Nat. Biomed. Eng. 2020, 4, 1208–1220. [Google Scholar] [CrossRef] [PubMed]
- Alavi, A.; Bogu, G.K.; Wang, M.; Rangan, E.S.; Brooks, A.W.; Wang, Q.; Higgs, E.; Celli, A.; Mishra, T.; Metwally, A.A.; et al. Real-time alerting system for COVID-19 and other stress events using wearable data. Nat. Med. 2022, 28, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Mitratza, M.; Mae Goodale, B.; Shagadatova, A.; Kovacevic, V.; van de Wijgert, J.; Brakenhoff, T.B.; Dobson, R.; Franks, B.; Veen, D.; Folarin, A.A.; et al. The performance of wearable sensors in the detection of SARS-CoV-2 infection: A systematic review. Lancet Digit. Health 2022, 4, e370–e383. [Google Scholar] [CrossRef]
- Ancona, S.; Faraci, F.D.; Khatab, E.; Fiorillo, L.; Gnarra, O.; Nef, T.; Bassetti, C.L.A.; Bargiotas, P. Wearables in the home-based assessment of abnormal movements in Parkinson’s disease: A systematic review of the literature. J. Neurol. 2022, 269, 100. [Google Scholar] [CrossRef] [PubMed]
- Vijayan, V.; Connolly, J.; Condell, J.; McKelvey, N.; Gardiner, P. Review of Wearable Devices and Data Collection Considerations for Connected Health. Sensors 2021, 21, 5589. [Google Scholar] [CrossRef] [PubMed]
- Brönneke, J.B.; Müller, J.; Mouratis, K.; Hagen, J.; Stern, A.D. Regulatory, Legal, and Market Aspects of Smart Wearables for Cardiac Monitoring. Sensors 2021, 21, 4937. [Google Scholar] [CrossRef] [PubMed]
- Rens, N.; Gandhi, N.; Mak, J.; Paul, J.; Bent, D.; Liu, S.; Savage, D.; Nielsen-Bowles, H.; Triggs, D.; Ata, G.; et al. Activity data from wearables as an indicator of functional capacity in patients with cardiovascular disease. PLoS ONE 2021, 16, e0247834. [Google Scholar] [CrossRef] [PubMed]
- Tison, G.H.; Sanchez, J.M.; Ballinger, B.; Singh, A.; Olgin, J.E.; Pletcher, M.J.; Vittinghoff, E.; Lee, E.S.; Fan, S.M.; Gladstone, R.A.; et al. Passive Detection of Atrial Fibrillation Using a Commercially Available Smartwatch. JAMA Cardiol. 2018, 3, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Samol, A.; Bischoff, K.; Luani, B.; Pascut, D.; Wiemer, M.; Kaese, S. Recording of Bipolar Multichannel ECGs by a Smartwatch: Modern ECG Diagnostic 100 Years after Einthoven. Sensors 2019, 19, 2894. [Google Scholar] [CrossRef] [PubMed]
- Spaccarotella, C.A.M.; Migliarino, S.; Mongiardo, A.; Sabatino, J.; Santarpia, G.; De Rosa, S.; Curcio, A.; Indolfi, C. Measurement of the QT interval using the Apple Watch. Sci. Rep. 2021, 11, 10817. [Google Scholar] [CrossRef] [PubMed]
- Hoilett, O.S.; Twibell, A.M.; Srivastava, R.; Linnes, J.C. Kick LL: A Smartwatch for Monitoring Respiration and Heart Rate using Photoplethysmography. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Honolulu, HI, USA, 18–21 July 2018; Volume 2018, p. 3824. [Google Scholar]
- Guo, Y.; Wang, H.; Zhang, H.; Liu, T.; Liang, Z.; Xia, Y.; Yan, L.; Xing, Y.; Shi, H.; Li, S.; et al. Mobile Photoplethysmographic Technology to Detect Atrial Fibrillation. J. Am. Coll. Cardiol. 2019, 74, 2365–2375. [Google Scholar] [CrossRef] [PubMed]
- Bashar, S.K.; Han, D.; Hajeb-Mohammadalipour, S.; Ding, E.; Whitcomb, C.; McManus, D.D.; Chon, K.H. Atrial Fibrillation Detection from Wrist Photoplethysmography Signals Using Smartwatches. Sci. Rep. 2019, 9, 15054. [Google Scholar] [CrossRef]
- Teo, J.X.; Davila, S.; Yang, C.; Hii, A.A.; Pua, C.J.; Yap, J.; Tan, S.Y.; Sahlén, A.; Chin, C.W.L.; Teh, B.T.; et al. Digital phenotyping by consumer wearables identifies sleep-associated markers of cardiovascular disease risk and biological aging. Commun. Biol. 2019, 2, 361. [Google Scholar] [CrossRef] [PubMed]
- Ozaslan, B.; Patek, S.D.; Breton, M.D. Impact of Daily Physical Activity as Measured by Commonly Available Wearables on Mealtime Glucose Control in Type 1 Diabetes. Diabetes Technol. Ther. 2020, 22, 742–748. [Google Scholar] [CrossRef]
- Weatherall, J.; Paprocki, Y.; Meyer, T.M.; Kudel, I.; Witt, E.A. Sleep Tracking and Exercise in Patients with Type 2 Diabetes Mellitus (Step-D): Pilot Study to Determine Correlations Between Fitbit Data and Patient-Reported Outcomes. JMIR mHealth uHealth 2018, 6, e8122. [Google Scholar] [CrossRef] [PubMed]
- Poh, M.Z.; Loddenkemper, T.; Swenson, N.C.; Goyal, S.; Madsen, J.R.; Picard, R.W. Continuous monitoring of electrodermal activity during epileptic seizures using a wearable sensor. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; pp. 4415–4418. [Google Scholar] [CrossRef]
- Iakovakis, D.; Mastoras, R.E.; Hadjidimitriou, S.; Charisis, V.; Bostanjopoulou, S.; Katsarou, Z.; Klingelhoefer, L.; Reichmann, H.; Trivedi, D.; Chaudhuri, R.K.; et al. Smartwatch-based Activity Analysis During Sleep for Early Parkinson’s Disease Detection. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 4326–4329. [Google Scholar]
- Kyritsis, K.; Fagerberg, P.; Ioakimidis, I.; Chaudhuri, K.R.; Reichmann, H.; Klingelhoefer, L.; Delopoulos, A. Assessment of real life eating difficulties in Parkinson’s disease patients by measuring plate to mouth movement elongation with inertial sensors. Sci. Rep. 2021, 11, 1632. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, A.L.; Pennypacker, M.L.; Thrush, A.H.; Leiper, C.I.; Craik, R.L. Validity of the stepwatch step activity monitor: Preliminary findings for use in persons with parkinson disease and multiple sclerosis. J. Geriatr. Phys. Ther. 2011, 34, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Dubey, H.; Goldberg, J.C.; Abtahi, M.; Mahler, L.; Mankodiya, K. EchoWear: Smartwatch technology for voice and speech treatments of patients with Parkinson’s disease. In Proceedings of the Proceedings of the conference on Wireless Health, New York, NY, USA, 14–16 October 2015; pp. 1–8. [Google Scholar]
- Sigcha, L.; Pavón, I.; Costa, N.; Costa, S.; Gago, M.; Arezes, P.; López, J.M.; Arcas, G. De Automatic Resting Tremor Assessment in Parkinson’s Disease Using Smartwatches and Multitask Convolutional Neural Networks. Sensors 2021, 21, 291. [Google Scholar] [CrossRef]
- Schneider, C.V.; Zandvakili, I.; Thaiss, C.A.; Schneider, K.M. Physical activity is associated with reduced risk of liver disease in the prospective UK Biobank cohort. JHEP Reports 2021, 3, 100263. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Seo, J.; An, S.Y.; Sinn, D.H.; Hwang, J.H. Efficacy and Safety of an mHealth App and Wearable Device in Physical Performance for Patients With Hepatocellular Carcinoma: Development and Usability Study. JMIR mHealth uHealth 2020, 8, e14435. [Google Scholar] [CrossRef]
- Akyol, E.; Cabral Ramos Mota, R.C.; Somanath, S. DiaFit: Designing Customizable Wearables for Type 1 Diabetes Monitoring. In Conference on Human Factors in Computing Systems—Proceedings; Association for Computing Machinery: Yokohama, Japan, 2021; p. 437. [Google Scholar]
- Lee, J.-H.; Lee, K.-H.; Kim, H.-J.; Youk, H.; Lee, H.-Y.; Lee, J.-H.; Lee, K.-H.; Kim, H.-J.; Youk, H.; Lee, H.-Y. Effective Prevention and Management Tools for Metabolic Syndrome Based on Digital Health-Based Lifestyle Interventions Using Healthcare Devices. Diagnostics 2022, 12, 1730. [Google Scholar] [CrossRef]
- Mehrabadi, M.A.; Azimi, I.; Sarhaddi, F.; Axelin, A.; Niela-Vilén, H.; Myllyntausta, S.; Stenholm, S.; Dutt, N.; Liljeberg, P.; Rahmani, A.M. Sleep Tracking of a Commercially Available Smart Ring and Smartwatch Against Medical-Grade Actigraphy in Everyday Settings: Instrument Validation Study. JMIR mHealth uHealth 2020, 8, e20465. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Wang, W.; Guo, Y.; Zhang, H.; Chen, Y.; Xie, L. A Single-Center Validation of the Accuracy of a Photoplethysmography-Based Smartwatch for Screening Obstructive Sleep Apnea. Nat. Sci. Sleep 2021, 13, 1533–1544. [Google Scholar] [CrossRef]
- Berryhill, S.; Morton, C.J.; Dean, A.; Berryhill, A.; Provencio-Dean, N.; Patel, S.I.; Estep, L.; Combs, D.; Mashaqi, S.; Gerald, L.B.; et al. Effect of wearables on sleep in healthy individuals: A randomized crossover trial and validation study. J. Clin. Sleep Med. 2020, 16, 775–783. [Google Scholar] [CrossRef]
- Rykov, Y.; Thach, T.Q.; Bojic, I.; Christopoulos, G.; Car, J. Digital Biomarkers for Depression Screening With Wearable Devices: Cross-sectional Study With Machine Learning Modeling. JMIR mHealth uHealth 2021, 9, e24872. [Google Scholar] [CrossRef]
- WHO. Fact Sheets on Cardiovascular Diseases [Internet]. 11 May 2022. Available online: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 15 June 2022).
- Bayoumy, K.; Gaber, M.; Elshafeey, A.; Mhaimeed, O.; Dineen, E.H.; Marvel, F.A.; Martin, S.S.; Muse, E.D.; Turakhia, M.P.; Tarakji, K.G.; et al. Smart wearable devices in cardiovascular care: Where we are and how to move forward. Nat. Rev. Cardiol. 2021, 18, 581–599. [Google Scholar] [CrossRef]
- Yen, H.Y.; Huang, W.H. The efficacy of commercial smartwatches with a blood pressure-monitoring feature: A pilot randomized controlled trial. J. Nurs. Scholarsh. 2022, 54, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Gkikopoulos, N.; Wenger, M.; Distler, O.; Becker, M. Self-monitoring of the resting heart rate using a fitness tracker smartwatch application leads to an early diagnosis of large vessel vasculitis. BMJ Case Rep. 2022, 15, e245021. [Google Scholar] [CrossRef] [PubMed]
- Kalla, M.; Fabritz, L.; Kirchhof, P. SMART About Watches: We Need Technical and Biological Validation of Atrial Fibrillation Screening. JACC Clin. Electrophysiol. 2019, 5, 209–211. [Google Scholar] [CrossRef] [PubMed]
- Inui, T.; Kohno, H.; Kawasaki, Y.; Matsuura, K.; Ueda, H.; Tamura, Y.; Watanabe, M.; Inage, Y.; Yakita, Y.; Wakabayashi, Y.; et al. Use of a Smart Watch for Early Detection of Paroxysmal Atrial Fibrillation: Validation Study. JMIR Cardio 2020, 4, e14857. [Google Scholar] [CrossRef] [PubMed]
- Koshy, A.N.; Sajeev, J.K.; Nerlekar, N.; Brown, A.J.; Rajakariar, K.; Zureik, M.; Wong, M.C.; Roberts, L.; Street, M.; Cooke, J.; et al. Smart watches for heart rate assessment in atrial arrhythmias. Int. J. Cardiol. 2018, 266, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Ukil, A.; Bandyopadhyay, S.; Puri, C.; Pal, A.; Mandana, K. Cardiac condition monitoring through photoplethysmogram signal denoising using wearables: Can we detect coronary artery disease with higher performance efficacy? In Proceedings of the IEEE Computing in Cardiology Conference, Vancouver, BC, Canada, 11–14 September 2016. [Google Scholar]
- Samol, A.; Bischof, K.; Luani, B.; Pascut, D.; Wiemer, M.; Kaese, S. Single-Lead ECG Recordings Including Einthoven and Wilson Leads by a Smartwatch: A New Era of Patient Directed Early ECG Differential Diagnosis of Cardiac Diseases? Sensors 2019, 19, 4377. [Google Scholar] [CrossRef]
- Fletcher, R.R.; Poh, M.Z.; Eydgahi, H. Wearable sensors: Opportunities and challenges for low-cost health care. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; pp. 1763–1766. [Google Scholar] [CrossRef]
- Turpin, G.; Shine, P.; Lader, M. Ambulatory Electrodermal Monitoring: Effects of Ambient Temperature, General Activity, Electrolyte Media, and Length of Recording. Psychophysiology 1983, 20, 219–224. [Google Scholar] [CrossRef]
- Qasim, M.S.; Bari, D.; Martinsen, O.G. Influence of ambient temperature on tonic and phasic electrodermal activity components. Physiol. Meas. 2022, 43, 065001. [Google Scholar] [CrossRef]
- Christie, M.J. Electrodermal activity in the 1980s: A review. J. R. Soc. Med. 1981, 74, 616–622. [Google Scholar] [CrossRef]
- Khan, T.H.; Villanueva, I.; Vicioso, P.; Husman, J. Exploring relationships between electrodermal activity, skin temperature, and performance during. In Proceedings of the 2019 IEEE Frontiers in Education Conference (FIE), Covington, KY, USA, 16–19 October 2019. [Google Scholar] [CrossRef]
- Onorati, F.; Regalia, G.; Caborni, C.; Migliorini, M.; Bender, D.; Poh, M.Z.; Frazier, C.; Kovitch Thropp, E.; Mynatt, E.D.; Bidwell, J.; et al. Multicenter clinical assessment of improved wearable multimodal convulsive seizure detectors. Epilepsia 2017, 58, 1870–1879. [Google Scholar] [CrossRef]
- Shaukat-Jali, R.; van Zalk, N.; Boyle, D.E. Detecting Subclinical Social Anxiety Using Physiological Data from a Wrist-Worn Wearable: Small-Scale Feasibility Study. JMIR Form. Res. 2021, 5, e32656. [Google Scholar] [CrossRef] [PubMed]
- Mc Ardle, R.; Del Din, S.; Galna, B.; Thomas, A.; Rochester, L. Differentiating dementia disease subtypes with gait analysis: Feasibility of wearable sensors? Gait Posture 2020, 76, 372–376. [Google Scholar] [CrossRef] [PubMed]
- Powers, R.; Etezadi-Amoli, M.; Arnold, E.M.; Kianian, S.; Mance, I.; Gibiansky, M.; Trietsch, D.; Alvarado, A.S.; Kretlow, J.D.; Herrington, T.M.; et al. Smartwatch inertial sensors continuously monitor real-world motor fluctuations in Parkinson’s disease. Sci. Transl. Med. 2021, 13, abd7865. [Google Scholar] [CrossRef]
- López-Blanco, R.; Velasco, M.A.; Méndez-Guerrero, A.; Romero, J.P.; del Castillo, M.D.; Serrano, J.I.; Rocon, E.; Benito-León, J. Smartwatch for the analysis of rest tremor in patients with Parkinson’s disease. J. Neurol. Sci. 2019, 401, 37–42. [Google Scholar] [CrossRef]
- Wile, D.J.; Ranawaya, R.; Kiss, Z.H.T. Smart watch accelerometry for analysis and diagnosis of tremor. J. Neurosci. Methods 2014, 230, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Khwaounjoo, P.; Singh, G.; Grenfell, S.; Özsoy, B.; MacAskill, M.R.; Anderson, T.J.; Çakmak, Y.O. Non-Contact Hand Movement Analysis for Optimal Configuration of Smart Sensors to Capture Parkinson’s Disease Hand Tremor. Sensors 2022, 22, 4613. [Google Scholar] [CrossRef]
- Varghese, J.; van Alen, C.M.; Fujarski, M.; Schlake, G.S.; Sucker, J.; Warnecke, T.; Thomas, C. Sensor validation and diagnostic potential of smartwatches in movement disorders. Sensors 2021, 21, 3139. [Google Scholar] [CrossRef]
- Sharma, V.; Mankodiya, K.; De La Torre, F.; Zhang, A.; Ryan, N.; Ton, T.G.N.; Gandhi, R.; Jain, S. Spark: Personalized parkinson disease interventions through synergy between a smartphone and a smartwatch. In Design, User Experience, and Usability. User Experience Design for Everyday Life Applications and Services; Springer: Cham, Switzerland, 2014; Volume 8519, pp. 103–114. [Google Scholar] [CrossRef]
- Kourtis, L.C.; Regele, O.B.; Wright, J.M.; Jones, G.B. Digital biomarkers for Alzheimer’s disease: The mobile/wearable devices opportunity. NPJ Digit. Med. 2019, 2, 9. [Google Scholar] [CrossRef]
- Alam, R.; Anderson, M.; Bankole, A.; Lach, J. Inferring physical agitation in dementia using smartwatch and sequential behavior models. In Proceedings of the IEEE EMBS International Conference on Biomedical and Health Informatics, BHI 2018, Las Vegas, NV, USA, 4–7 March 2018; Volume 2018-January, pp. 170–173. [Google Scholar]
- Gwak, M.; Woo, E.; Sarrafzadeh, M. The role of accelerometer and gyroscope sensors in identification of mild cognitive impairment. In Proceedings of the IEEE Global Conference on Signal and Information Processing, Anaheim, CA, USA, 26–29 November 2018; pp. 434–438. [Google Scholar]
- Maresova, P.; Tomsone, S.; Lameski, P.; Madureira, J.; Mendes, A.; Zdravevski, E.; Chorbev, I.; Trajkovik, V.; Ellen, M.; Rodile, K. Technological Solutions for Older People with Alzheimer’s Disease: Review. Curr. Alzheimer Res. 2018, 15, 975–983. [Google Scholar] [CrossRef]
- Al-Naami, B.; Owida, H.A.; Mallouh, M.A.; Al-Naimat, F.; Agha, M.; Al-Hinnawi, A.R. A New Prototype of Smart Wearable Monitoring System Solution for Alzheimer’s Patients. Med. Devices Evid. Res. 2021, 14, 423–433. [Google Scholar] [CrossRef]
- Dunn, M.A.; Kappus, M.R.; Bloomer, P.M.; Duarte-Rojo, A.; Josbeno, D.A.; Jakicic, J.M. Wearables, Physical Activity, and Exercise Testing in Liver Disease. Semin. Liver Dis. 2021, 41, 128–135. [Google Scholar] [CrossRef]
- Zhu, T.; Watkinson, P.; Clifton, D.A. Smartwatch data help detect COVID-19. Nat. Biomed. Eng. 2020, 4, 1125–1127. [Google Scholar] [CrossRef] [PubMed]
- Lonini, L.; Shawen, N.; Botonis, O.; Fanton, M.; Jayaraman, C.; Mummidisetty, C.K.; Shin, S.Y.; Rushin, C.; Jenz, S.; Xu, S.; et al. Rapid Screening of Physiological Changes Associated with COVID-19 Using Soft-Wearables and Structured Activities: A Pilot Study. IEEE J. Transl. Eng. Health Med. 2021, 9, 4900311. [Google Scholar] [CrossRef]
- Gadaleta, M.; Radin, J.M.; Baca-Motes, K.; Ramos, E.; Kheterpal, V.; Topol, E.J.; Steinhubl, S.R.; Quer, G. Passive detection of COVID-19 with wearable sensors and explainable machine learning algorithms. NPJ Digit. Med. 2021, 4, 166. [Google Scholar] [CrossRef]
- Quer, G.; Radin, J.M.; Gadaleta, M.; Baca-Motes, K.; Ariniello, L.; Ramos, E.; Kheterpal, V.; Topol, E.J.; Steinhubl, S.R. Wearable sensor data and self-reported symptoms for COVID-19 detection. Nat. Med. 2021, 27, 73–77. [Google Scholar] [CrossRef]
- Cho, H.R.; Kim, J.H.; Yoon, H.R.; Han, Y.S.; Kang, T.S.; Choi, H.; Lee, S. Machine learning-based optimization of pre-symptomatic COVID-19 detection through smartwatch. Sci. Rep. 2022, 12, 7886. [Google Scholar] [CrossRef]
- Ramesh, J.; Aburukba, R.; Sagahyroon, A. A remote healthcare monitoring framework for diabetes prediction using machine learning. Healthc. Technol. Lett. 2021, 8, 45. [Google Scholar] [CrossRef]
- Yavelberg, L.; Zaharieva, D.; Cinar, A.; Riddell, M.C.; Jamnik, V. A Pilot Study Validating Select Research-Grade and Consumer-Based Wearables throughout a Range of Dynamic Exercise Intensities in Persons with and without Type 1 Diabetes: A Novel Approach. J. Diabetes Sci. Technol. 2018, 12, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Sehgal, S.; De Bock, M.; Williman, J.; Taylor, B.; Elbalshy, M.; Galland, B.; Hall, R.; Paul, R.; Boucsein, A.; Jones, S.; et al. Study protocol: Safety and efficacy of smart watch integrated do-it-yourself continuous glucose monitoring in adults with Type 1 diabetes, a randomised controlled trial. J. Diabetes Metab. Disord. 2021, 20, 2103–2113. [Google Scholar] [CrossRef] [PubMed]
- Zilberstein, G.; Zilberstein, R.; Maor, U.; Righetti, P.G. Noninvasive wearable sensor for indirect glucometry. Electrophoresis 2018, 39, 2344–2350. [Google Scholar] [CrossRef]
- Rentz, L.E.; Ulman, H.K.; Galster, S.M. Deconstructing Commercial Wearable Technology: Contributions toward Accurate and Free-Living Monitoring of Sleep. Sensors 2021, 21, 5071. [Google Scholar] [CrossRef] [PubMed]
- Sathyanarayana, A.; Joty, S.; Fernandez-Luque, L.; Ofli, F.; Srivastava, J.; Elmagarmid, A.; Arora, T.; Taheri, S. Sleep Quality Prediction From Wearable Data Using Deep Learning. JMIR mHealth uHealth 2016, 4, e6562. [Google Scholar] [CrossRef]
- Lee, J.M.; Byun, W.; Keill, A.; Dinkel, D.; Seo, Y. Comparison of Wearable Trackers’ Ability to Estimate Sleep. Int. J. Environ. Res. Public Health 2018, 15, 1265. [Google Scholar] [CrossRef] [PubMed]
- Topalidis, P.; Florea, C.; Eigl, E.S.; Kurapov, A.; Leon, C.A.B.; Schabus, M. Evaluation of a Low-Cost Commercial Actigraph and Its Potential Use in Detecting Cultural Variations in Physical Activity and Sleep. Sensors 2021, 21, 3774. [Google Scholar] [CrossRef]
- Papini, G.B.; Fonseca, P.; van Gilst, M.M.; Bergmans, J.W.M.; Vullings, R.; Overeem, S. Wearable monitoring of sleep-disordered breathing: Estimation of the apnea–hypopnea index using wrist-worn reflective photoplethysmography. Sci. Rep. 2020, 10, 13512. [Google Scholar] [CrossRef] [PubMed]
- Ko, Y.F.; Kuo, P.H.; Wang, C.F.; Chen, Y.J.; Chuang, P.C.; Li, S.Z.; Chen, B.W.; Yang, F.C.; Lo, Y.C.; Yang, Y.; et al. Quantification Analysis of Sleep Based on Smartwatch Sensors for Parkinson’s Disease. Biosensors 2022, 12, 74. [Google Scholar] [CrossRef] [PubMed]
- Shah, R.V.; Grennan, G.; Zafar-Khan, M.; Alim, F.; Dey, S.; Ramanathan, D.; Mishra, J. Personalized machine learning of depressed mood using wearables. Transl. Psychiatry 2021, 11, 338. [Google Scholar] [CrossRef]
- Laureanti, R.; Bilucaglia, M.; Zito, M.; Circi, R.; Fici, A.; Rivetti, F.; Valesi, R.; Oldrini, C.; Mainardi, L.T.; Russo, V. Emotion assessment using Machine Learning and low-cost wearable devices. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 576–579. [Google Scholar]
- Pollreisz, D.; Taherinejad, N. A simple algorithm for emotion recognition, using physiological signals of a smart watch. In Proceedings of the 2017 39th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Jeju, Korea, 11–15 July 2017; pp. 2353–2356. [Google Scholar] [CrossRef]
- Quiroz, J.C.; Geangu, E.; Yong, M.H. Emotion Recognition Using Smart Watch Sensor Data: Mixed-Design Study. JMIR Ment. Health 2018, 5, e10153. [Google Scholar] [CrossRef] [PubMed]
- Priyadarshini, R.K.; Bazila Banu, A.; Nagamani, T. Gradient Boosted Decision Tree based Classification for Recognizing Human Behavior. In Proceedings of the 2019 International Conference on Advances in Computing and Communication Engineering (ICACCE), Sathyamangalam, India, 4–6 April 2019. [Google Scholar] [CrossRef]
- McGinnis, R.S.; McGinnis, E.W.; Hruschak, J.; Lopez-Duran, N.L.; Fitzgerald, K.; Rosenblum, K.L.; Muzik, M. Rapid Anxiety and Depression Diagnosis in Young Children Enabled by Wearable Sensors and Machine Learning. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; pp. 3983–3986. [Google Scholar] [CrossRef]
- Nath, R.K.; Thapliyal, H. Smart Wristband-Based Stress Detection Framework for Older Adults with Cortisol as Stress Biomarker. IEEE Trans. Consum. Electron. 2021, 67, 30–39. [Google Scholar] [CrossRef]
- Sabry, F.; Eltaras, T.; Labda, W.; Alzoubi, K.; Malluhi, Q. Machine Learning for Healthcare Wearable Devices: The Big Picture. J. Healthc. Eng. 2022, 2022, 4653923. [Google Scholar] [CrossRef]
- Sunny, J.S.; Patro, C.P.K.; Karnani, K.; Pingle, S.C.; Lin, F.; Anekoji, M.; Jones, L.D.; Kesari, S.; Ashili, S. Anomaly Detection Framework for Wearables Data: A Perspective Review on Data Concepts, Data Analysis Algorithms and Prospects. Sensors 2022, 22, 756. [Google Scholar] [CrossRef] [PubMed]
- Preatoni, E.; Nodari, S.; Lopomo, N.F. Supervised Machine Learning Applied to Wearable Sensor Data Can Accurately Classify Functional Fitness Exercises within a Continuous Workout. Front. Bioeng. Biotechnol. 2020, 8, 664. [Google Scholar] [CrossRef] [PubMed]
- Ho, T.K. The random subspace method for constructing decision forests. IEEE Trans. Pattern Anal. Mach. Intell. 1998, 20, 832–844. [Google Scholar] [CrossRef] [Green Version]
- Natekin, A.; Knoll, A. Gradient boosting machines, a tutorial. Front. Neurorobot. 2013, 7, 21. [Google Scholar] [CrossRef] [PubMed]
- Altman, N.S. An introduction to kernel and nearest-neighbor nonparametric regression. Am. Stat. 1992, 46, 175–185. [Google Scholar] [CrossRef]
- Site, A.; Nurmi, J.; Lohan, E.S. Systematic review on machine-learning algorithms used in wearable-based eHealth data analysis. IEEE Access 2021, 9, 112221–112235. [Google Scholar] [CrossRef]
- Dalmeida, K.M.; Masala, G.L. HRV Features as Viable Physiological Markers for Stress Detection Using Wearable Devices. Sensors 2021, 21, 2873. [Google Scholar] [CrossRef]
- Fei, C.; Liu, R.; Li, Z.; Wang, T.; Baig, F.N. Machine and Deep Learning Algorithms for Wearable Health Monitoring. In Computational Intelligence in Healthcare; Springer: Berlin/Heidelberg, Germany, 2021; pp. 105–160. [Google Scholar]
- Beniczky, S.; Karoly, P.; Nurse, E.; Ryvlin, P.; Cook, M. Machine learning and wearable devices of the future. Epilepsia 2021, 62, S116–S124. [Google Scholar] [CrossRef]
- Huang, W.; Ying, T.W.; Chin, W.L.C.; Baskaran, L.; Marcus, O.E.H.; Yeo, K.K.; Kiong, N.S. Application of ensemble machine learning algorithms on lifestyle factors and wearables for cardiovascular risk prediction. Sci. Rep. 2022, 12, 1033. [Google Scholar] [CrossRef]
- Hirten, R.P.; Tomalin, L.; Danieletto, M.; Golden, E.; Zweig, M.; Kaur, S.; Helmus, D.; Biello, A.; Pyzik, R.; Bottinger, E.P.; et al. Evaluation of a machine learning approach utilizing wearable data for prediction of SARS-CoV-2 infection in healthcare workers. JAMIA Open 2022, 5, ooac041. [Google Scholar] [CrossRef] [PubMed]
- Green, E.M.; van Mourik, R.; Wolfus, C.; Heitner, S.B.; Dur, O.; Semigran, M.J. Machine learning detection of obstructive hypertrophic cardiomyopathy using a wearable biosensor. NPJ Digit. Med. 2019, 2, 57. [Google Scholar] [CrossRef] [PubMed]
- Boyer, P.; Burns, D.; Whyne, C. Out-of-Distribution Detection of Human Activity Recognition with Smartwatch Inertial Sensors. Sensors 2021, 21, 1669. [Google Scholar] [CrossRef] [PubMed]
- Khashei, M.; Bijari, M. An artificial neural network (p, d, q) model for timeseries forecasting. Expert Syst. Appl. 2010, 37, 479–489. [Google Scholar] [CrossRef]
- Chiang, P.H.; Wong, M.; Dey, S. Using Wearables and Machine Learning to Enable Personalized Lifestyle Recommendations to Improve Blood Pressure. IEEE J. Transl. Eng. Health Med. 2021, 9, 2700513. [Google Scholar] [CrossRef] [PubMed]
- Hochreiter, S.; Schmidhuber, J. Long Short-Term Memory. Neural Comput. 1997, 9, 1735–1780. [Google Scholar] [CrossRef]
- Gers, F.A.; Schmidhuber, J.; Cummins, F. Learning to Forget: Continual Prediction with LSTM. Neural Comput. 2000, 12, 2451–2471. [Google Scholar] [CrossRef]
- Oyeleye, M.; Chen, T.; Titarenko, S.; Antoniou, G. A Predictive Analysis of Heart Rates Using Machine Learning Techniques. Int. J. Environ. Res. Public Health 2022, 19, 2417. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhou, X. Detection of Congestive Heart Failure Based on LSTM-Based Deep Network via Short-Term RR Intervals. Sensors 2019, 19, 1502. [Google Scholar] [CrossRef]
- Fedorin, I.; Slyusarenko, K. Consumer Smartwatches As a Portable PSG: LSTM Based Neural Networks for a Sleep-Related Physiological Parameters Estimation. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBS), Jalisco, Mexico, 1–5 November 2021; pp. 849–852. [Google Scholar]
- Kamdar, M.R.; Wu, M.J. PRISM: A data-driven platform for monitoring mental health. In Pacific Symposium on Biocomputing; World Scientific Publishing Co. Pte Ltd: Singapore, 2016; pp. 333–344. [Google Scholar]
- Zhang, T.; EI Ali, A.; Wang, C.; Hanjalic, A.; Cesar, P. CorrNet: Fine-Grained Emotion Recognition for Video Watching Using Wearable Physiological Sensors. Sensors 2020, 21, 52. [Google Scholar] [CrossRef] [PubMed]
- Kong, Y.; Chon, K.H. Heart Rate Tracking Using a Wearable Photoplethysmographic Sensor During Treadmill Exercise. Biosensors 2019, 7, 152421–152428. [Google Scholar] [CrossRef]
- Kheirkhahan, M.; Nair, S.; Davoudi, A.; Rashidi, P.; Wanigatunga, A.A.; Corbett, D.B.; Mendoza, T.; Manini, T.M.; Ranka, S. A smartwatch-based framework for real-time and online assessment and mobility monitoring. J. Biomed. Inform. 2019, 89, 29–40. [Google Scholar] [CrossRef]
- Mauldin, T.R.; Canby, M.E.; Metsis, V.; Ngu, A.H.H.; Rivera, C.C. SmartFall: A Smartwatch-Based Fall Detection System Using Deep Learning. Sensors 2018, 18, 3363. [Google Scholar] [CrossRef] [PubMed]
- Kwon, M.C.; Park, G.; Choi, S. Smartwatch User Interface Implementation Using CNN-Based Gesture Pattern Recognition. Sensors 2018, 18, 2997. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lipsmeier, F.; Taylor, K.I.; Postuma, R.B.; Volkova-Volkmar, E.; Kilchenmann, T.; Mollenhauer, B.; Bamdadian, A.; Popp, W.L.; Cheng, W.-Y.; Zhang, Y.-P.; et al. Reliability and validity of the Roche PD Mobile Application for remote monitoring of early Parkinson’s disease. Sci. Rep. 2022, 12, 12081. [Google Scholar] [CrossRef] [PubMed]
- Zylstra, B.; Netscher, G.; Jacquemot, J.; Schaffer, M.; Shen, G.; Bowhay, A.D.; Braley, T.L.; Possin, K.L.; Miller, B.L.; Bayen, A.M.; et al. Extended, continuous measures of functional status in community dwelling persons with Alzheimer’s and related dementia: Infrastructure, performance, tradeoffs, preliminary data, and promise. J. Neurosci. Methods 2018, 300, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Ciman, M.; Wac, K. Smartphones as Sleep Duration Sensors: Validation of the iSenseSleep Algorithm. JMIR mHealth uHealth 2019, 7, e11930. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Campbell, A.S.; Ávila, B.E.-F.; Wang, J. Wearable biosensors for healthcare monitoring. Nat. Biotechnol. 2019, 37, 389–406. [Google Scholar] [CrossRef]
- Piccinini, F.; Martinelli, G.; Carbonaro, A. Accuracy of Mobile Applications versus Wearable Devices in Long-Term Step Measurements. Sensors 2020, 20, 6293. [Google Scholar] [CrossRef] [PubMed]
- Cosoli, G.; Antognoli, L.; Veroli, V.; Scalise, L. Accuracy and Precision of Wearable Devices for Real-Time Monitoring of Swimming Athletes. Sensors 2022, 22, 4726. [Google Scholar] [CrossRef]
- Nazarian, S.; Lam, K.; Darzi, A.; Ashrafian, H. Diagnostic Accuracy of Smartwatches for the Detection of Cardiac Arrhythmia: Systematic Review and Meta-analysis. J. Med. Internet Res. 2021, 23, e28974. [Google Scholar] [CrossRef] [PubMed]
- Hahnen, C.; Freeman, C.G.; Haldar, N.; Hamati, J.N.; Bard, D.M.; Murali, V.; Merli, G.J.; Joseph, J.I.; Van Helmond, N. Accuracy of Vital Signs Measurements by a Smartwatch and a Portable Health Device: Validation Study. JMIR mHealth uHealth 2020, 8, e16811. [Google Scholar] [CrossRef] [PubMed]
- Nelson, B.W.; Allen, N.B. Accuracy of Consumer Wearable Heart Rate Measurement During an Ecologically Valid 24-Hour Period: Intraindividual Validation Study. JMIR mHealth uHealth 2019, 7, e10828. [Google Scholar] [CrossRef] [PubMed]
- Mittlesteadt, J.; Bambach, S.; Dawes, A.; Wentzel, E.; Debs, A.; Sezgin, E.; Digby, D.; Huang, Y.; Ganger, A.; Bhatnagar, S.; et al. Evaluation of an Activity Tracker to Detect Seizures Using Machine Learning. J. Child Neurol. 2020, 35, 873–878. [Google Scholar] [CrossRef] [PubMed]
- Williamson, J.; Liu, Q.; Lu, F.; Mohrman, W.; Li, K.; Dick, R.; Shang, L. Data sensing and analysis: Challenges for wearables. In Proceedings of the 20th Asia and South Pacific Design Automation Conference, ASP-DAC 2015, Chiba, Japan, 19–22 January 2015; pp. 136–141. [Google Scholar]
- Lymberis, A. Smart wearables for remote health monitoring, from prevention to rehabilitation: Current R&D, future challenges. In Proceedings of the 4th International IEEE EMBS Special Topic Conference on Information Technology Applications in Biomedicine, Birmingham, UK, 24–26 April 2003; pp. 272–275. [Google Scholar] [CrossRef]
- Tran, V.-T.; Riveros, C.; Ravaud, P. Patients’ views of wearable devices and AI in healthcare: Findings from the ComPaRe e-cohort. NPJ Digit. Med. 2019, 2, 53. [Google Scholar] [CrossRef]
- Ioannidou, I.; Sklavos, N. On General Data Protection Regulation Vulnerabilities and Privacy Issues, for Wearable Devices and Fitness Tracking Applications. Cryptography 2021, 5, 29. [Google Scholar] [CrossRef]
- Neumann, D.; Tiberius, V.; Biendarra, F. Adopting wearables to customize health insurance contributions: A ranking-type Delphi. BMC Med. Inform. Decis. Mak. 2022, 22, 1–7. [Google Scholar] [CrossRef] [PubMed]
- John Dian, F.; Vahidnia, R.; Rahmati, A. Wearables and the Internet of Things (IoT), Applications, Opportunities, and Challenges: A Survey. IEEE Access 2020, 8, 69200–69211. [Google Scholar] [CrossRef]
- Murray, T.M.; Krishnan, S.M. Medical Wearables for Monitoring Cardiovascular Disease Medical Wearables for Monitoring Cardiovascular Diseases. In Proceedings of the 2018 ASEE Mid-Atlantic Section Spring Conference, Washington, DC, USA, 6–7 April 2018. [Google Scholar]
- Smuck, M.; Odonkor, C.A.; Wilt, J.K.; Schmidt, N.; Swiernik, M.A. The emerging clinical role of wearables: Factors for successful implementation in healthcare. NPJ Digit. Med. 2021, 4, 45. [Google Scholar] [CrossRef] [PubMed]
- Habibzadeh, H.; Dinesh, K.; Rajabi Shishvan, O.; Boggio-Dandry, A.; Sharma, G.; Soyata, T. A Survey of Healthcare Internet-of-Things (HIoT): A Clinical Perspective. IEEE Internet Things J. 2020, 7, 71. [Google Scholar] [CrossRef]
| Smartwatch Brand | Acquisition Points | Data Collected | Usage | Benefits | References |
|---|---|---|---|---|---|
| Apple Watch | Wrist | Step count and heart rate | Monitors frailty in cardiovascular patients when 6MWTs are conducted in both clinical settings and at home. | Assesses frailty with 90% sensitivity in a clinical setting and with 83% sensitivity at home. | [22] |
| Detects AF by training using a deep-learning network. | Assesses heart beat rhythm by using a trained deep-learning algorithm with a sensitivity of 98%. | [23] | |||
| Wrist, finger, chest, and abdomen | Heart rate | Could be useful in the detection of several cardiovascular diseases such as myocardial ischemia or cardiac arrhythmias. | Recording from this smartwatch shows feasibility, with a good signal quality of ECG (QT interval) and a correlation of 0.994. | [24,25] | |
| Kick LL | Wrist | Respiration and heart rate | Measures respiration and heart rate using a PPG sensor. | Allows real-time and remote measurements. | [26] |
| Honor Band 4 and Huawei Watch GT | Wrist | Heart rate | Early AF screening and management with a CI of 91.5–91.8%. | Early detection of AF can prevent strokes or other complications. | [27] |
| Simband (Samsung) | Wrist | Heart rate | Detects AF using a PPG signal with an accuracy of 98.18%. | Enables easy and non-invasive monitoring of arrythmia. | [28] |
| Fitbit Charge HR | Wrist | Sleep | Acts as cardiovascular disease and leukocyte telomere length-shortening markers. | Monitors sleep patterns and quality to understand the cardiovascular risk and premature telomere shortening of an individual. | [29] |
| Step count and sleep | Tracks physical activity in diabetic patients. | The physical activity record could have an impact on glucose control. | [30,31] | ||
| E4 Empatica Wristband | Wrist | EDA and temperature | Uses EDA recordings to monitor the activity of the sympathetic nervous system during epileptic seizures. | Allows continuous and long-term measurements of EDA. | [32] |
| Huawei Watch 2 | Wrist | Sleep | Detects PD at an early state using the sleep patterns of an individual. | Smartwatch-based detection shows a significant correlation of 0.46 to the clinical setting. | [33] |
| The 3D acceleration and orientation of velocity signals | Measures movement with inertial sensors in PD patients. | Assesses the eating difficulties in PD patients. | [34] | ||
| StepWatch | Wrist | Step count | Step activity monitor (SAM) to count strides; shows a correlation of 0.99 and 1.0 with the gold standard (GaitMait) in PD and MS patients, respectively. | Reliable, easy-to-use, and valid step monitoring tool for PD and MS patients. | [35] |
| EchoWear | Wrist | Audio | Speech and voice exercise monitoring system for the detection of voice and speech disorders in PD patients. | Remotely monitors the improvements in speech and voice in PD patients. | [36] |
| Dytran 302M3 | Wrist | Tremor constancy and amplitude | Detects tremors in PD patients; shows a strong correlation of 0.969 with the clinical setting. | Provides relevant information about tremors during the early stages of PD and results in improvements in the clinical evaluation. | [37] |
| Axivity AX3 | Wrist | Heart rate, step count, and calories | Tracks physical activities to detect the risk of liver diseases. | Provides a framework for the personalized prevention of liver disease. | [38] |
| Neofit (Partron Co) | Wrist | Calories burnt, step count, exercise duration, and heart rate | Monitors physical activities in hepatocellular carcinoma patients. | Tracks the activities of patients using the wristband, which correlates with a significant improvement in their health. | [39] |
| Fitbit, Apple Watch, Garmin, and others | Wrist | Heart rate, calories burnt, step count, and sleep duration | Detects COVID-19 illness | Detects COVID-19 illness in a pre-symptomatic condition. | [16] |
| Diafit | Wrist, finger, and ear | Glucose | Monitors glucose for diabetic patients. | Consists of various modular accessories required for the assembling of customizable glucose monitors. | [40] |
| Galaxy Watch Active 1 | Wrist | Calories burnt, step count, exercise duration, and heart rate | Manages metabolic syndrome risks by tracking physical activities. | The tracking of physical activities using the smartwatch results in a reduction in waist circumference, blood pressure, and blood sugar by 40%. | [41] |
| Samsung Gear Sport Watch | Wrist | Sleep | Assesses sleep quality by evaluating sleep parameters; shows a significant correlation of 0.59 with an actigraphy report. | Enables long-term home-based sleep monitoring. | [42] |
| GT2 (Huawei) | Wrist | Sleep | Used in the screening of obstructive sleep apnea. | Compared to other sleep apnea tests, the smartwatch-based test outperformed the others with an accuracy of 87.9%. | [43] |
| WHOOP, Inc. | Wrist | Sleep | Tracks sleep with a low bias of 13.8 min and precision errors of 17.8 min. | Accurately measures both dream and slow-wave sleep. | [44] |
| FitBit Charge 2 | Wrist | Steps, heart rate, energy expenditure, and sleep | Tracks physical activity and sleep to understand the behavior and physiology to detect mental disorders such as depression. | A supervised machine-learning algorithm with these data was able to detect the risk of depression with an accuracy of 80%. | [45] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chakrabarti, S.; Biswas, N.; Jones, L.D.; Kesari, S.; Ashili, S. Smart Consumer Wearables as Digital Diagnostic Tools: A Review. Diagnostics 2022, 12, 2110. https://doi.org/10.3390/diagnostics12092110
Chakrabarti S, Biswas N, Jones LD, Kesari S, Ashili S. Smart Consumer Wearables as Digital Diagnostic Tools: A Review. Diagnostics. 2022; 12(9):2110. https://doi.org/10.3390/diagnostics12092110
Chicago/Turabian StyleChakrabarti, Shweta, Nupur Biswas, Lawrence D. Jones, Santosh Kesari, and Shashaanka Ashili. 2022. "Smart Consumer Wearables as Digital Diagnostic Tools: A Review" Diagnostics 12, no. 9: 2110. https://doi.org/10.3390/diagnostics12092110
APA StyleChakrabarti, S., Biswas, N., Jones, L. D., Kesari, S., & Ashili, S. (2022). Smart Consumer Wearables as Digital Diagnostic Tools: A Review. Diagnostics, 12(9), 2110. https://doi.org/10.3390/diagnostics12092110