Indoor Exposure to Selected Air Pollutants in the Home Environment: A Systematic Review
Abstract
:1. Introduction
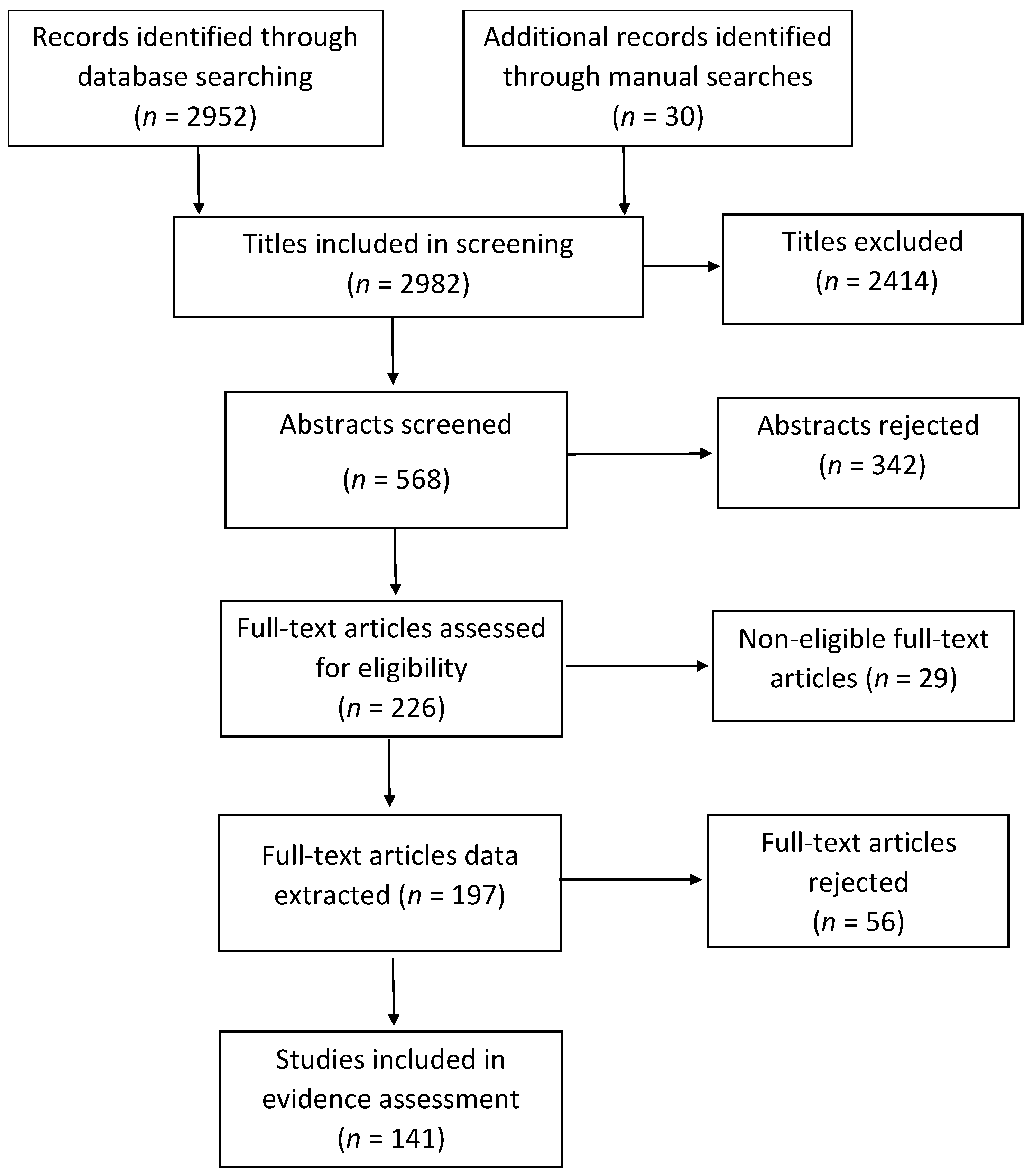
2. Methods
2.1. Literature Searches
2.2. Paper Screening and Data Extraction
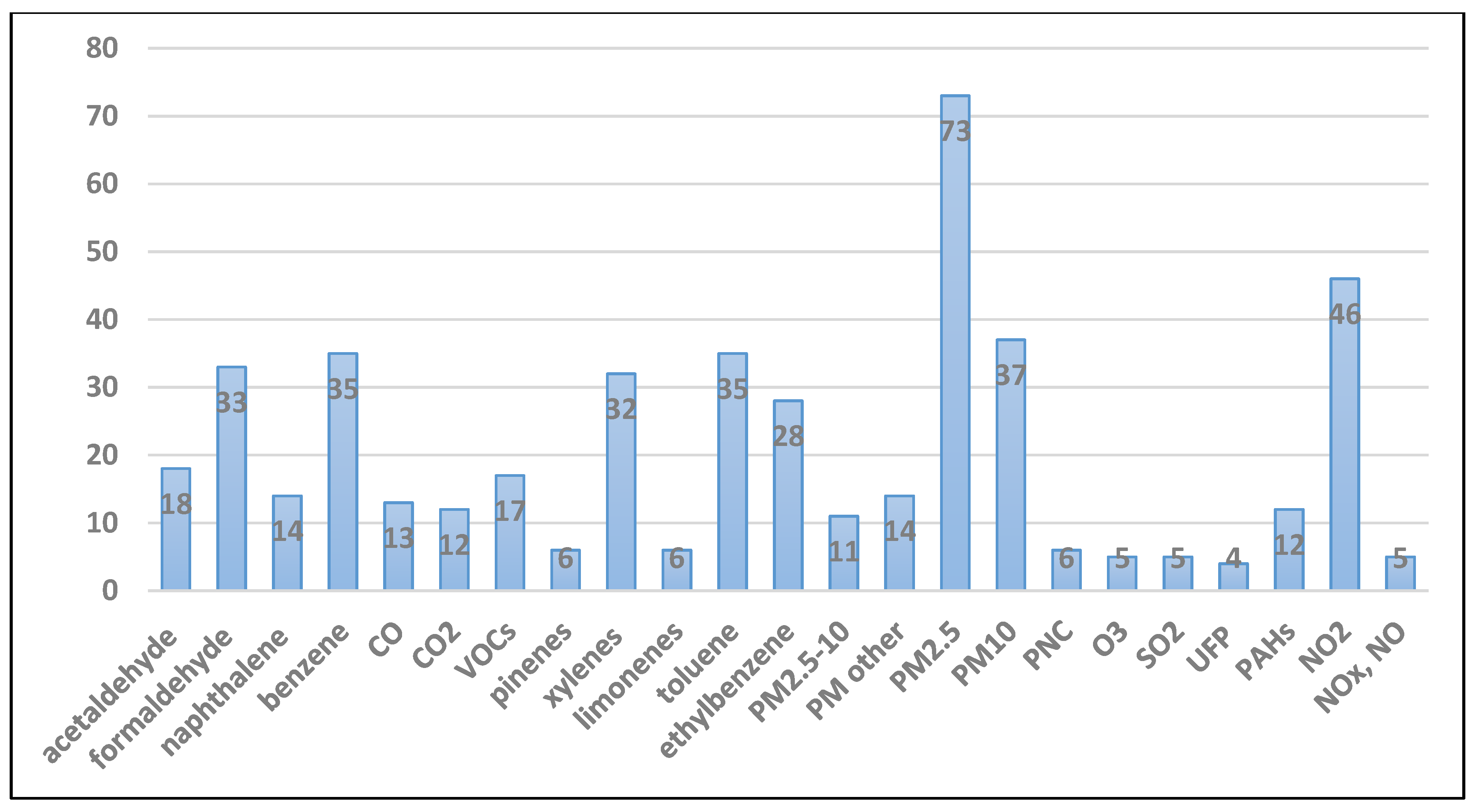
3. Results
3.1. Particulate Matter
3.1.1. Exposure Levels, Sources and Determinants
3.1.2. Health Effects
3.2. Nitrogen Dioxide
3.2.1. Exposure Levels, Sources and Determinants
3.2.2. Health Effects
3.3. Volatile Organic Compounds
3.3.1. Exposure Levels, Sources and Determinants
3.3.2. Health Effects
3.4. Formaldehyde and Other Carbonyls
3.4.1. Exposure Levels, Sources and Determinants
3.4.2. Health Effects
3.5. Polycyclic Aromatic Hydrocarbons
3.5.1. Exposure Levels, Sources and Determinants
3.5.2. Health Effects
3.6. Naphthalene
3.6.1. Exposure Levels, Sources and Determinants
3.6.2. Health Effects
3.7. Other Indoor Pollutants
4. Key Determinants of Indoor Air Pollution
4.1. Housing Characteristics
4.2. Occupancy, Natural Ventilation and Activity Patterns
4.3. Seasonal and Climatic Influences
4.4. Dwelling Location, Setting and Within-Building Variability
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Guidelines for Indoor Air Quality: Selected Pollutants; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2010; Available online: https://www.euro.who.int/__data/assets/pdf_file/0009/128169/e94535.pdf (accessed on 10 November 2020).
- Lai, H.K.; Kendall, M.; Ferrier, H.; Lindup, I.; Alm, S.; Hänninen, O.; Jantunen, M.; Mathys, P.; Colvile, R.; Ashmore, M.R.; et al. Personal exposures and microenvironment concentrations of PM2.5, VOC, NO2 and CO in Oxford, UK. Atmos. Environ. 2004, 38, 6399–6410. [Google Scholar] [CrossRef]
- Vardoulakis, S.; Kinney, P. Grand Challenges in Sustainable Cities and Health. Front. Sustain. Cities 2019, 1. [Google Scholar] [CrossRef] [Green Version]
- de Juniac, A.; Kreis, I.; Ibison, J.; Murray, V. Epidemiology of unintentional carbon monoxide fatalities in the UK. Int. J. Environ. Health Res. 2012, 22, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Sarigiannis, D.A.; Karakitsios, S.P.; Gotti, A.; Liakos, I.L.; Katsoyiannis, A. Exposure to major volatile organic compounds and carbonyls in European indoor environments and associated health risk. Environ. Int. 2011, 37, 743–765. [Google Scholar] [CrossRef]
- Jordan, R.E.; Cheng, K.K.; Miller, M.R.; Adab, P. Passive smoking and chronic obstructive pulmonary disease: Cross-sectional analysis of data from the Health Survey for England. BMJ Open 2011, 1, e000153. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanc, P.D.; Eisner, M.D.; Katz, P.P.; Yen, I.H.; Archea, C.; Earnest, G.; Janson, S.; Masharani, U.B.; Quinlan, P.J.; Hammond, S.K.; et al. Impact of the home indoor environment on adult asthma and rhinitis. J. Occup. Environ. Med. 2005, 47, 362–372. [Google Scholar] [CrossRef]
- Rushton, L. Health impact of environmental tobacco smoke in the home. Rev. Environ. Health 2004, 19, 291–309. [Google Scholar]
- Jones, A.P. Indoor air quality and health. Atmos. Environ. 1999, 33, 4535–4564. [Google Scholar] [CrossRef]
- Vardoulakis, S.; Fisher, B.E.A.; Pericleous, K.; Gonzalez-Flesca, N. Modelling air quality in street canyons: A review. Atmos. Environ. 2003, 37, 155–182. [Google Scholar] [CrossRef] [Green Version]
- Crump, D.; Brown, V.; Rowley, J.; Squire, R. Reducing ingress of organic vapours into homes situated on contaminated land. Environ. Technol. 2004, 25, 443–450. [Google Scholar] [CrossRef]
- Vardoulakis, S.; Dimitrova, R.; Richards, K.; Hamlyn, D.; Camilleri, G.; Weeks, M.; Sini, J.-F.; Britter, R.; Borrego, C.; Schatzmann, M.; et al. Numerical Model Inter-comparison for Wind Flow and Turbulence Around Single-Block Buildings. Environ. Model. Assess. 2011, 16, 169–181. [Google Scholar] [CrossRef]
- Hall, D.J.S.; Spanton, A.M. Ingress of External Contaminants into Buildings–A Review. Atmospheric Dispersion Modelling Liaison Committee. 2012. ADMLC/2012/01. Available online: https://admlc.files.wordpress.com/2014/05/admlc-r7-2012-1.pdf (accessed on 10 November 2020).
- Milner, J.; Vardoulakis, S.; Chalabi, Z.; Wilkinson, P. Modelling inhalation exposure to combustion-related air pollutants in residential buildings: Application to health impact assessment. Environ. Int. 2011, 37, 268–279. [Google Scholar] [CrossRef]
- Nazaroff, W. Exploring the consequences of climate change for indoor air quality*. Environ. Res. Lett. 2013, 8, 015022. [Google Scholar] [CrossRef] [Green Version]
- Ryan, P.H.; Brokamp, C.; Fan, Z.H.; Rao, M.B. Analysis of personal and home characteristics associated with the elemental composition of PM2.5 in indoor, outdoor, and personal air in the RIOPA Study. Res. Rep. Health Eff. Inst. 2015, 185, 3–40. [Google Scholar]
- Clougherty, J.E.; Houseman, E.A.; Levy, J.I. Source apportionment of indoor residential fine particulate matter using land use regression and constrained factor analysis. Indoor Air 2011, 21, 53–66. [Google Scholar] [CrossRef]
- MacNeill, M.; Kearney, J.; Wallace, L.; Gibson, M.; Héroux, M.E.; Kuchta, J.; Guernsey, J.R.; Wheeler, A.J. Quantifying the contribution of ambient and indoor-generated fine particles to indoor air in residential environments. Indoor Air 2014, 24, 362–375. [Google Scholar] [CrossRef]
- Mohammadyan, M.; Ashmore, M. Personal Exposure and Indoor PM2.5 Concentrations in an Urban Population. Indoor Built Environ. 2005, 14, 313–320. [Google Scholar] [CrossRef]
- Wallace, L.; Mitchell, H.; O’Connor, G.; Neas, L.; Lippmann, M.; Kattan, M.; Koenig, J.; Stout, J.; Vaughn, B.; Wallace, D.; et al. Particle concentrations in inner-city homes of children with asthma: The effect of smoking, cooking, and outdoor pollution. Environ. Health Perspect. 2003, 111, 1265–1272. [Google Scholar] [CrossRef] [Green Version]
- Rojas-Bracho, L.; Suh, H.H.; Catalano, P.J.; Koutrakis, P. Personal exposures to particles and their relationships with personal activities for chronic obstructive pulmonary disease patients living in Boston. J. Air Waste Manag. Assoc. 2004, 54, 207–217. [Google Scholar] [CrossRef] [Green Version]
- Rosen, L.; Zucker, D.; Hovell, M.; Brown, N.; Ram, A.; Myers, V. Feasibility of Measuring Tobacco Smoke Air Pollution in Homes: Report from a Pilot Study. Int. J. Environ. Res. Public Health 2015, 12, 15129–15142. [Google Scholar] [CrossRef] [Green Version]
- Wyss, A.B.; Jones, A.C.; Bølling, A.K.; Kissling, G.E.; Chartier, R.; Dahlman, H.J.; Rodes, C.E.; Archer, J.; Thornburg, J.; Schwarze, P.E.; et al. PM2.5 exposure and self-reported use of wood stoves and other indoor combustion sources in urban nonsmoking homes in Norway. PLoS ONE 2016, 11, e0166440. [Google Scholar] [CrossRef] [Green Version]
- Brown, D.R.; Alderman, N.; Weinberger, B.; Lewis, C.; Bradley, J.; Curtis, L. Outdoor wood furnaces create significant indoor particulate pollution in neighboring homes. Inhal. Toxicol. 2014, 26, 628–635. [Google Scholar] [CrossRef]
- McNamara, M.; Thornburg, J.; Semmens, E.; Ward, T.; Noonan, C. Coarse particulate matter and airborne endotoxin within wood stove homes. Indoor Air 2013, 23, 498–505. [Google Scholar] [CrossRef]
- Mills, L.M.; Semple, S.E.; Wilson, I.S.; MacCalman, L.; Amos, A.; Ritchie, D.; O’Donnell, R.; Shaw, A.; Turner, S.W. Factors influencing exposure to secondhand smoke in preschool children living with smoking mothers. Nicotine Tob. Res. 2012, 14, 1435–1444. [Google Scholar] [CrossRef]
- Lajoie, P.; Aubin, D.; Gingras, V.; Daigneault, P.; Ducharme, F.; Gauvin, D.; Fugler, D.; Leclerc, J.M.; Won, D.; Courteau, M.; et al. The IVAIRE project—A randomized controlled study of the impact of ventilation on indoor air quality and the respiratory symptoms of asthmatic children in single family homes. Indoor Air 2015, 25, 582–597. [Google Scholar] [CrossRef]
- Weitzman, M.; Yusufali, A.H.; Bali, F.; Vilcassim, M.J.R.; Gandhi, S.; Peltier, R.; Nadas, A.; Sherman, S.; Lee, L.; Hong, Z.; et al. Effects of hookah smoking on indoor air quality in homes. Tob. Control 2016, 26, 586–591. [Google Scholar] [CrossRef] [Green Version]
- Jones, N.C.; Thornton, C.A.; Mark, D.; Harrison, R.M. Indoor/outdoor relationships of particulate matter in domestic homes with roadside, urban and rural locations. Atmos. Environ. 2000, 34, 2603–2612. [Google Scholar] [CrossRef]
- Wigzell, E.; Kendall, M.; Nieuwenhuijsen, M.J. The spatial and temporal variation of particulate matter within the home. J. Expo. Sci. Environ. Epidemiol. 2000, 10, 307–314. [Google Scholar] [CrossRef] [Green Version]
- Tunno, B.J.; Kyra Naumoff, S.; Cambal, L.; Tripathy, S.; Holguin, F.; Lioy, P.; Clougherty, J.E. Indoor air sampling for fine particulate matter and black carbon in industrial communities in Pittsburgh. Sci. Total Environ. 2015, 536, 108–115. [Google Scholar] [CrossRef] [Green Version]
- Hu, J.; Li, N.; Lv, Y.; Liu, J.; Xie, J.; Zhang, H. Investigation on Indoor Air Pollution and Childhood Allergies in Households in Six Chinese Cities by Subjective Survey and Field Measurements. Int. J. Environ. Res. Public Health 2017, 14, 979. [Google Scholar] [CrossRef]
- Lai, S.; Ho, K.F.; Zhang, Y.; Lee, S.; Huang, Y.; Zou, S. Characteristics of Residential Indoor Carbonaceous Aerosols: A Case Study in Guangzhou, Pearl River Delta Region. Aerosol Air Qual. Res. 2010, 10, 472–478. [Google Scholar] [CrossRef] [Green Version]
- Li, T.; Cao, S.; Fan, D.; Zhang, Y.; Wang, B.; Zhao, X.; Leaderer, B.P.; Shen, G.; Zhang, Y.; Duan, X. Household concentrations and personal exposure of PM2.5 among urban residents using different cooking fuels. Sci. Total Environ. 2016, 548–549, 6–12. [Google Scholar] [CrossRef] [Green Version]
- Cao, J.J.; Lee, S.C.; Chow, J.C.; Cheng, Y.; Ho, K.F.; Fung, K.; Liu, S.X.; Watson, J.G. Indoor/outdoor relationships for PM2.5 and associated carbonaceous pollutants at residential homes in Hong Kong-case study. Indoor Air 2005, 15, 197–204. [Google Scholar] [CrossRef]
- Gurley, E.S.; Salje, H.; Homaira, N.; Ram, P.K.; Haque, R.; Petri, W.A., Jr.; Bresee, J.; Moss, W.J.; Luby, S.P.; Breysse, P.; et al. Seasonal concentrations and determinants of indoor particulate matter in a low-income community in Dhaka, Bangladesh. Environ. Res 2013, 121, 11–16. [Google Scholar] [CrossRef] [Green Version]
- Lévesque, B.; Allaire, S.; Gauvin, D.; Koutrakis, P.; Gingras, S.; Rhainds, M.; Prud’Homme, H.; Duchesne, J.-F. Wood-burning appliances and indoor air quality. Sci. Total Environ. 2001, 281, 47–62. [Google Scholar] [CrossRef]
- Morawska, L.; Mengersen, K.; Wang, H.; Tayphasavanh, F.; Darasavong, K.; Holmes, N.S. Pollutant concentrations within households in Lao PDR and association with housing characteristics and occupants’ activities. Environ. Sci. Technol. 2011, 45, 882–889. [Google Scholar] [CrossRef]
- Kulshreshtha, P.; Khare, M.; Seetharaman, P. Indoor air quality assessment in and around urban slums of Delhi city, India. Indoor Air 2008, 18, 488–498. [Google Scholar] [CrossRef]
- Taneja, A.; Saini, R.; Masih, A. Indoor air quality of houses located in the urban environment of Agra, India. Ann. N. Y. Acad. Sci. 2008, 1140, 228–245. [Google Scholar] [CrossRef]
- Custódio, D.; Pinho, I.; Cerqueira, M.; Nunes, T.; Pio, C. Indoor and outdoor suspended particulate matter and associated carbonaceous species at residential homes in northwestern Portugal. Sci. Total Environ. 2014, 473–474, 72–76. [Google Scholar] [CrossRef]
- BéruBé, K.A.; Sexton, K.J.; Jones, T.P.; Moreno, T.; Anderson, S.; Richards, R.J. The spatial and temporal variations in PM10 mass from six UK homes. Sci. Total Environ. 2004, 324, 41–53. [Google Scholar] [CrossRef]
- Chen, Y.; Li, X.; Zhu, T.; Han, Y.; Lv, D. PM2.5-bound PAHs in three indoor and one outdoor air in Beijing: Concentration, source and health risk assessment. Sci. Total Environ. 2017, 586, 255–264. [Google Scholar] [CrossRef]
- Wallace, L. Indoor sources of ultrafine and accumulation mode particles: Size distributions, size-resolved concentrations, and source strengths. Aerosol Sci. Technol. 2006, 40, 348–360. [Google Scholar] [CrossRef] [Green Version]
- Karottki, D.G.; Spilak, M.; Frederiksen, M.; Jovanovic Andersen, Z.; Madsen, A.M.; Ketzel, M.; Massling, A.; Gunnarsen, L.; Møller, P.; Loft, S. Indoor and outdoor exposure to ultrafine, fine and microbiologically derived particulate matter related to cardiovascular and respiratory effects in a panel of elderly urban citizens. Int. J. Environ. Res. Public Health 2015, 12, 1667–1686. [Google Scholar] [CrossRef]
- Bhangar, S.; Mullen, N.A.; Hering, S.V.; Kreisberg, N.M.; Nazaroff, W.W. Ultrafine particle concentrations and exposures in seven residences in northern California. Indoor Air 2011, 21, 132–144. [Google Scholar] [CrossRef]
- Weichenthal, S.; Dufresne, A.; Infante-Rivard, C.; Joseph, L. Indoor ultrafine particle exposures and home heating systems: A cross-sectional survey of Canadian homes during the winter months. J. Expo. Sci. Environ. Epidemiol. 2007, 17, 288–297. [Google Scholar] [CrossRef] [Green Version]
- Olsen, Y.; Karottki, D.G.; Jensen, D.M.; Bekö, G.; Kjeldsen, B.U.; Clausen, G.; Hersoug, L.-G.; Holst, G.J.; Wierzbicka, A.; Sigsgaard, T.; et al. Vascular and lung function related to ultrafine and fine particles exposure assessed by personal and indoor monitoring: A cross-sectional study. Environ. Health 2014, 13, 112. [Google Scholar] [CrossRef] [Green Version]
- McCormack, M.C.; Breysse, P.N.; Matsui, E.C.; Hansel, N.N.; Williams, D.; Curtin-Brosnan, J.; Eggleston, P.; Diette, G.B. In-home particle concentrations and childhood asthma morbidity. Environ. Health Perspect. 2009, 117, 294–298. [Google Scholar] [CrossRef] [Green Version]
- McCormack, M.C.; Breysse, P.N.; Matsui, E.C.; Hansel, N.N.; Peng, R.D.; Curtin-Brosnan, J.; Williams, D.L.; Wills-Karp, M.; Diette, G.B. Indoor particulate matter increases asthma morbidity in children with non-atopic and atopic asthma. Ann. Allergy Asthma Immunol. 2011, 106, 308–315. [Google Scholar] [CrossRef] [Green Version]
- Jung, K.H.; Hsu, S.I.; Yan, B.; Moors, K.; Chillrud, S.N.; Ross, J.; Wang, S.; Perzanowski, M.S.; Kinney, P.L.; Whyatt, R.M.; et al. Childhood exposure to fine particulate matter and black carbon and the development of new wheeze between ages 5 and 7 in an urban prospective cohort. Environ. Int. 2012, 45, 44–50. [Google Scholar] [CrossRef] [Green Version]
- Delfino, R.; Quintana, P.; Floro, J.; Gastañaga, V.; Samimi, B.; Kleinman, M.; Liu, L.J.; Bufalino, C.; Wu, C.-F.; McLaren, C. Association of FEV1 in Asthmatic Children with Personal and Microenvironmental Exposure to Airborne Particulate Matter. Environ. Health Perspect. 2004, 112, 932–941. [Google Scholar] [CrossRef] [Green Version]
- Chi, M.C.; Guo, S.E.; Hwang, S.L.; Chou, C.T.; Lin, C.M.; Lin, Y.C. Exposure to Indoor Particulate Matter Worsens the Symptoms and Acute Exacerbations in Chronic Obstructive Pulmonary Disease Patients of Southwestern Taiwan: A Pilot Study. Int. J. Environ. Res. Public Health 2016, 14, 4. [Google Scholar] [CrossRef] [PubMed]
- Osman, L.M.; Douglas, J.G.; Garden, C.; Reglitz, K.; Lyon, J.; Gordon, S.; Ayres, J.G. Indoor air quality in homes of patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2007, 176, 465–472. [Google Scholar] [CrossRef]
- Uchiyama, S.; Tomizawa, T.; Tokoro, A.; Aoki, M.; Hishiki, M.; Yamada, T.; Tanaka, R.; Sakamoto, H.; Yoshida, T.; Bekki, K.; et al. Gaseous chemical compounds in indoor and outdoor air of 602 houses throughout Japan in winter and summer. Environ. Res. 2015, 137, 364–372. [Google Scholar] [CrossRef]
- Hansel, N.; McCormack, M.; Belli, A.; Matsui, E.; Peng, R.; Aloe, C.; Paulin, L.; Williams, D.A.; Diette, G.; Breysse, P. In-home air pollution is linked to respiratory morbidity in former smokers with COPD. Am. J. Respir. Crit. Care Med. 2013, 187. [Google Scholar] [CrossRef] [Green Version]
- Belanger, K.; Holford, T.R.; Gent, J.F.; Hill, M.E.; Kezik, J.M.; Leaderer, B.P. Household levels of nitrogen dioxide and pediatric asthma severity. Epidemiology 2013, 24, 320–330. [Google Scholar] [CrossRef] [Green Version]
- Kornartit, C.; Sokhi, R.S.; Burton, M.A.; Ravindra, K. Activity pattern and personal exposure to nitrogen dioxide in indoor and outdoor microenvironments. Environ. Int. 2010, 36, 36–45. [Google Scholar] [CrossRef] [Green Version]
- Cyrys, J.; Heinrich, J.; Richter, K.; Wölke, G.; Wichmann, H.E. Sources and concentrations of indoor nitrogen dioxide in Hamburg (west Germany) and Erfurt (east Germany). Sci. Total Environ. 2000, 250, 51–62. [Google Scholar] [CrossRef]
- Mullen, N.A.; Li, J.; Russell, M.L.; Spears, M.; Less, B.D.; Singer, B.C. Results of the California Healthy Homes Indoor Air Quality Study of 2011–2013: Impact of natural gas appliances on air pollutant concentrations. Indoor Air 2016, 26, 231–245. [Google Scholar] [CrossRef] [Green Version]
- Cibella, F.; Cuttitta, G.; Della Maggiore, R.; Ruggieri, S.; Panunzi, S.; De Gaetano, A.; Bucchieri, S.; Drago, G.; Melis, M.R.; La Grutta, S.; et al. Effect of indoor nitrogen dioxide on lung function in urban environment. Environ. Res. 2015, 138, 8–16. [Google Scholar] [CrossRef] [Green Version]
- Zipprich, J.L.; Harris, S.A.; Fox, J.C.; Borzelleca, J.F. An analysis of factors that influence personal exposure to nitrogen oxides in residents of Richmond, Virginia. J. Expo. Anal. Environ. Epidemiol. 2002, 12, 273–285. [Google Scholar] [CrossRef]
- Belanger, K.; Gent, J.F.; Triche, E.W.; Bracken, M.B.; Leaderer, B.P. Association of indoor nitrogen dioxide exposure with respiratory symptoms in children with asthma. Am. J. Respir. Crit. Care Med. 2006, 173, 297–303. [Google Scholar] [CrossRef] [Green Version]
- Hansel, N.; Breysse, P.; McCormack, M.; Matsui, E.; Curtin-Brosnan, J.; Williams, D.A.; Moss, J.; Cuhran, J.; Diette, G. A Longitudinal Study of Indoor Nitrogen Dioxide Levels and Respiratory Symptoms in Inner-City Children with Asthma. Environ. Health Perspect. 2008, 116, 1428–1432. [Google Scholar] [CrossRef] [Green Version]
- Kattan, M.; Gergen, P.; Eggleston, P.; Visness, C.; Mitchell, H. Health effects of indoor nitrogen dioxide and passive smoking on urban asthmatic children. J. Allergy Clin. Immunol. 2007, 120, 618–624. [Google Scholar] [CrossRef]
- Gillespie-Bennett, J.; Pierse, N.; Wickens, K.; Crane, J.; Howden-Chapman, P. The respiratory health effects of nitrogen dioxide in children with asthma. Eur. Respir. J. 2011, 38, 303–309. [Google Scholar] [CrossRef] [Green Version]
- Paulin, L.M.; Williams, D.L.; Peng, R.; Diette, G.B.; McCormack, M.C.; Breysse, P.; Hansel, N.N. 24-h Nitrogen dioxide concentration is associated with cooking behaviors and an increase in rescue medication use in children with asthma. Environ. Res. 2017, 159, 118–123. [Google Scholar] [CrossRef]
- Delgado-Saborit, J.M.; Aquilina, N.J.; Meddings, C.; Baker, S.; Harrison, R.M. Relationship of personal exposure to volatile organic compounds to home, work and fixed site outdoor concentrations. Sci. Total Environ. 2011, 409, 478–488. [Google Scholar] [CrossRef]
- Tanaka-Kagawa, T.; Uchiyama, S.; Matsushima, E.; Sasaki, A.; Kobayashi, H.; Kobayashi, H.; Yagi, M.; Tsuno, M.; Arao, M.; Ikemoto, K.; et al. Survey of volatile organic compounds found in indoor and outdoor air samples from Japan. Bull. Natl. Inst. Health Sci. 2005, 123, 27–31. [Google Scholar]
- Wheeler, A.J.; Wong, S.L.; Khouri, C.; Zhu, J. Predictors of indoor BTEX concentrations in Canadian residences. Health Rep. 2013, 24, 11. [Google Scholar]
- Cheng, M.; Galbally, I.E.; Molloy, S.B.; Selleck, P.W.; Keywood, M.D.; Lawson, S.J.; Powell, J.C.; Gillett, R.W.; Dunne, E. Factors controlling volatile organic compounds in dwellings in Melbourne, Australia. Indoor Air 2016, 26, 219–230. [Google Scholar] [CrossRef]
- Adgate, J.L.; Eberly, L.E.; Stroebel, C.; Pellizzari, E.D.; Sexton, K. Personal, indoor, and outdoor VOC exposures in a probability sample of children. J. Expo. Anal. Environ. Epidemiol. 2004, 14 (Suppl. S1), S4–S13. [Google Scholar] [CrossRef] [Green Version]
- Chin, J.Y.; Godwin, C.; Parker, E.; Robins, T.; Lewis, T.; Harbin, P.; Batterman, S. Levels and sources of volatile organic compounds in homes of children with asthma. Indoor Air 2014, 24, 403–415. [Google Scholar] [CrossRef] [Green Version]
- Rumchev, K.; Spickett, J.; Bulsara, M.; Phillips, M.; Stick, S. Association of domestic exposure to volatile organic compounds with asthma in young children. Thorax 2004, 59, 746–751. [Google Scholar] [CrossRef] [Green Version]
- Kliucininkas, L.; Martuzevicius, D.; Krugly, E.; Prasauskas, T.; Kauneliene, V.; Molnar, P.; Strandberg, B. Indoor and outdoor concentrations of fine particles, particle-bound PAHs and volatile organic compounds in Kaunas, Lithuania. J. Environ. Monit. 2011, 13, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, F.; Tapia, A.; Amo-Salas, M.; Notario, A.; Cabañas, B.; Martínez, E. Levels and sources of volatile organic compounds including carbonyls in indoor air of homes of Puertollano, the most industrialized city in central Iberian Peninsula. Estimation of health risk. Int. J. Hyg. Environ. Health 2015, 218, 522–534. [Google Scholar] [CrossRef]
- Alexopoulos, E.C.; Chatzis, C.; Linos, A. An analysis of factors that influence personal exposure to toluene and xylene in residents of Athens, Greece. BMC Public Health 2006, 6, 50. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.H.; Lee, H.S.; Park, M.R.; Lee, S.W.; Kim, E.H.; Cho, J.B.; Kim, J.; Han, Y.; Jung, K.; Cheong, H.K.; et al. Relationship between indoor air pollutant levels and residential environment in children with atopic dermatitis. Allergy Asthma Immunol. Res. 2014, 6, 517–524. [Google Scholar] [CrossRef] [Green Version]
- Ferrero, A.; Esplugues, A.; Estarlich, M.; Llop, S.; Cases, A.; Mantilla, E.; Ballester, F.; Iñiguez, C. Infants’ indoor and outdoor residential exposure to benzene and respiratory health in a Spanish cohort. Environ. Pollut. 2017, 222, 486–494. [Google Scholar] [CrossRef]
- Adgate, J.L.; Church, T.R.; Ryan, A.D.; Ramachandran, G.; Fredrickson, A.L.; Stock, T.H.; Morandi, M.T.; Sexton, K. Outdoor, indoor, and personal exposure to VOCs in children. Environ. Health Perspect. 2004, 112, 1386–1392. [Google Scholar] [CrossRef] [Green Version]
- Phillips, M.L.; Esmen, N.A.; Hall, T.A.; Lynch, R. Determinants of exposure to volatile organic compounds in four Oklahoma cities. J. Expo. Anal. Environ. Epidemiol. 2005, 15, 35–46. [Google Scholar] [CrossRef] [Green Version]
- Du, L.; Batterman, S.; Godwin, C.; Rowe, Z.; Chin, J.Y. Air exchange rates and migration of VOCs in basements and residences. Indoor Air 2015, 25, 598–609. [Google Scholar] [CrossRef] [Green Version]
- Saijo, Y.; Kishi, R.; Sata, F.; Katakura, Y.; Urashima, Y.; Hatakeyama, A.; Kobayashi, S.; Jin, K.; Kurahashi, N.; Kondo, T.; et al. Symptoms in relation to chemicals and dampness in newly built dwellings. Int. Arch. Occup. Environ. Health 2004, 77, 461–470. [Google Scholar] [CrossRef]
- Harrison, R.M.; Delgado-Saborit, J.M.; Baker, S.J.; Aquilina, N.; Meddings, C.; Harrad, S.; Matthews, I.; Vardoulakis, S.; Anderson, H.R. Measurement and modeling of exposure to selected air toxics for health effects studies and verification by biomarkers. Res. Rep. Health Eff. Inst. 2009, 143, 3–100. [Google Scholar]
- Saraga, D.E.; Maggos, T.; Helmis, C.G.; Michopoulos, J.; Bartzis, J.G.; Vasilakos, C. PM1 and PM2.5 ionic composition and VOCs measurements in two typical apartments in Athens, Greece: Investigation of smoking contribution to indoor air concentrations. Environ. Monit. Assess. 2010, 167, 321–331. [Google Scholar] [CrossRef]
- Schneider, P.; Gebefügi, I.; Richter, K.; Wölke, G.; Schnelle, J.; Wichmann, H.E.; Heinrich, J. Indoor and outdoor BTX levels in German cities. Sci. Total Environ. 2001, 267, 41–51. [Google Scholar] [CrossRef]
- Jurvelin, J.A.; Edwards, R.D.; Vartiainen, M.; Pasanen, P.; Jantunen, M.J. Residential Indoor, Outdoor, and Workplace Concentrations of Carbonyl Compounds: Relationships with Personal Exposure Concentrations and Correlation with Sources. J. Air Waste Manag. Assoc. 2003, 53, 560–573. [Google Scholar] [CrossRef] [Green Version]
- Park, J.S.; Ikeda, K. Variations of formaldehyde and VOC levels during 3 years in new and older homes. Indoor Air 2006, 16 2, 129–135. [Google Scholar] [CrossRef]
- Guo, H.; Kwok, N.H.; Cheng, H.R.; Lee, S.C.; Hung, W.T.; Li, Y.S. Formaldehyde and volatile organic compounds in Hong Kong homes: Concentrations and impact factors. Indoor Air 2009, 19, 206–217. [Google Scholar] [CrossRef]
- Wang, C.M.; Barratt, B.; Carslaw, N.; Doutsi, A.; Dunmore, R.; Ward, M.; Lewis, A. Unexpectedly high concentrations of monoterpenes in a study of UK homes. Environ. Sci. Process. Impacts 2017, 19. [Google Scholar] [CrossRef] [Green Version]
- Gordian, M.E.; Stewart, A.W.; Morris, S.S. Evaporative gasoline emissions and asthma symptoms. Int. J. Environ. Res. Public Health 2010, 7, 3051–3062. [Google Scholar] [CrossRef] [Green Version]
- Singleton, R.; Salkoski, A.J.; Bulkow, L.; Fish, C.; Dobson, J.; Albertson, L.; Skarada, J.; Kovesi, T.; McDonald, C.; Hennessy, T.W.; et al. Housing characteristics and indoor air quality in households of Alaska Native children with chronic lung conditions. Indoor Air 2017, 27, 478–486. [Google Scholar] [CrossRef]
- Madureira, J.; Paciência, I.; Cavaleiro-Rufo, J.; Fernandes Ede, O. Indoor air risk factors for schoolchildren’s health in Portuguese homes: Results from a case-control survey. J. Toxicol. Environ. Health Part A 2016, 79, 938–953. [Google Scholar] [CrossRef]
- Kwon, J.H.; Kim, E.; Chang, M.H.; Park, E.A.; Hong, Y.C.; Ha, M.; Park, H.; Kim, Y.; Park, C.; Ha, E.H. Indoor total volatile organic compounds exposure at 6 months followed by atopic dermatitis at 3 years in children. Pediatric Allergy Immunol. 2015, 26, 352–358. [Google Scholar] [CrossRef]
- Takeda, M.; Saijo, Y.; Yuasa, M.; Kanazawa, A.; Araki, A.; Kishi, R. Relationship between sick building syndrome and indoor environmental factors in newly built Japanese dwellings. Int. Arch. Occup. Environ. Health 2009, 82, 583–593. [Google Scholar] [CrossRef]
- Marchand, C.; Bulliot, B.; Le Calvé, S.; Mirabel, P. Aldehyde measurements in indoor environments in Strasbourg (France). Atmos. Environ. 2006, 40, 1336–1345. [Google Scholar] [CrossRef]
- Lovreglio, P.; Carrus, A.; Iavicoli, S.; Drago, I.; Persechino, B.; Soleo, L. Indoor formaldehyde and acetaldehyde levels in the province of Bari, South Italy, and estimated health risk. J. Environ. Monit. 2009, 11, 955–961. [Google Scholar] [CrossRef]
- Maruo, Y.Y.; Yamada, T.; Nakamura, J.; Izumi, K.; Uchiyama, M. Formaldehyde measurements in residential indoor air using a developed sensor element in the Kanto area of Japan. Indoor Air 2010, 20, 486–493. [Google Scholar] [CrossRef]
- Takigawa, T.; Saijo, Y.; Morimoto, K.; Nakayama, K.; Shibata, E.; Tanaka, M.; Yoshimura, T.; Chikara, H.; Kishi, R. A longitudinal study of aldehydes and volatile organic compounds associated with subjective symptoms related to sick building syndrome in new dwellings in Japan. Sci. Total Environ. 2012, 417–418, 61–67. [Google Scholar] [CrossRef]
- Clarisse, B.; Laurent, A.M.; Seta, N.; Le Moullec, Y.; El Hasnaoui, A.; Momas, I. Indoor aldehydes: Measurement of contamination levels and identification of their determinants in Paris dwellings. Environ. Res. 2003, 92, 245–253. [Google Scholar] [CrossRef]
- Raw, G.J.; Coward, S.K.; Brown, V.M.; Crump, D.R. Exposure to air pollutants in English homes. J. Expo. Anal. Environ. Epidemiol. 2004, 14 (Suppl. S1), S85–S94. [Google Scholar] [CrossRef] [Green Version]
- Gilbert, N.L.; Guay, M.; David Miller, J.; Judek, S.; Chan, C.C.; Dales, R.E. Levels and determinants of formaldehyde, acetaldehyde, and acrolein in residential indoor air in Prince Edward Island, Canada. Environ. Res. 2005, 99, 11–17. [Google Scholar] [CrossRef]
- Gilbert, N.L.; Gauvin, D.; Guay, M.; Héroux, M.-È.; Dupuis, G.; Legris, M.; Chan, C.C.; Dietz, R.N.; Lévesque, B. Housing characteristics and indoor concentrations of nitrogen dioxide and formaldehyde in Quebec City, Canada. Environ. Res. 2006, 102, 1–8. [Google Scholar] [CrossRef]
- Rovira, J.; Roig, N.; Nadal, M.; Schuhmacher, M.; Domingo, J.L. Human health risks of formaldehyde indoor levels: An issue of concern. J. Environ. Sci. Health Part A 2016, 51, 357–363. [Google Scholar] [CrossRef] [Green Version]
- Rancière, F.; Dassonville, C.; Roda, C.; Laurent, A.M.; Le Moullec, Y.; Momas, I. Contribution of ozone to airborne aldehyde formation in Paris homes. Sci. Total Environ. 2011, 409, 4480–4483. [Google Scholar] [CrossRef]
- Herbarth, O.; Fritz, G.J.; Rehwagen, M.; Richter, M.; Röder, S.; Schlink, U. Association between indoor renovation activities and eczema in early childhood. Int. J. Hyg. Environ. Health 2006, 209, 241–247. [Google Scholar] [CrossRef]
- Yeatts, K.B.; El-Sadig, M.; Leith, D.; Kalsbeek, W.; Al-Maskari, F.; Couper, D.; Funk, W.E.; Zoubeidi, T.; Chan, R.L.; Trent, C.B.; et al. Indoor air pollutants and health in the United Arab Emirates. Environ. Health Perspect. 2012, 120, 687–694. [Google Scholar] [CrossRef]
- Takigawa, T.; Wang, B.L.; Saijo, Y.; Morimoto, K.; Nakayama, K.; Tanaka, M.; Shibata, E.; Yoshimura, T.; Chikara, H.; Ogino, K.; et al. Relationship between indoor chemical concentrations and subjective symptoms associated with sick building syndrome in newly built houses in Japan. Int. Arch. Occup. Environ. Health 2010, 83, 225–235. [Google Scholar] [CrossRef]
- Kume, K.; Ohura, T.; Noda, T.; Amagai, T.; Fusaya, M. Seasonal and spatial trends of suspended-particle associated polycyclic aromatic hydrocarbons in urban Shizuoka, Japan. J. Hazard. Mater. 2007, 144, 513–521. [Google Scholar] [CrossRef]
- Liu, Y.; Zhu, L.; Shen, X. Polycyclic Aromatic Hydrocarbons (PAHs) in Indoor and Outdoor Air of Hangzhou, China. Environ. Sci. Technol. 2001, 35, 840–844. [Google Scholar] [CrossRef]
- Ohura, T.; Sugiyama, T.; Amagai, T.; Fusaya, M.; Matsushita, H. Simultaneous liquid chromatographic determination of 39 polycyclic aromatic hydrocarbons in indoor and outdoor air and application to a survey on indoor air pollution in Fuji, Japan. J. AOAC Int. 2002, 85, 188–202. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, K.; Macova, M.; Leusch, F.; Bartkow, M.E.; Hawker, D.W.; Zhao, B.; Denison, M.S.; Mueller, J.F. Assessing indoor air exposures using passive sampling with bioanalytical methods for estrogenicity and aryl hydrocarbon receptor activity. Anal. Bioanal. Chem. 2009, 394, 1413–1421. [Google Scholar] [CrossRef] [Green Version]
- Lu, H.; Amagai, T.; Ohura, T. Comparison of polycyclic aromatic hydrocarbon pollution in Chinese and Japanese residential air. J. Environ. Sci. 2011, 23, 1512–1517. [Google Scholar] [CrossRef]
- Cirillo, T.; Montuori, P.; Mainardi, P.; Russo, I.; Triassi, M.; Amodio-Cocchieri, R. Multipathway Polycyclic Aromatic Hydrocarbon and Pyrene Exposure Among Children Living in Campania (Italy). J. Environ. Sci. Health Part A 2006, 41, 2089–2107. [Google Scholar] [CrossRef] [Green Version]
- Brender, J.D.; Pichette, J.L.; Suarez, L.; Hendricks, K.A.; Holt, M. Health risks of residential exposure to polycyclic aromatic hydrocarbons. Arch. Environ. Health 2003, 58, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Batterman, S.; Chin, J.-Y.; Jia, C.; Godwin, C.; Parker, E.; Robins, T.; Max, P.; Lewis, T. Sources, concentrations and risks of naphthalene in indoor and outdoor air. Indoor Air 2012, 22, 266–278. [Google Scholar] [CrossRef] [Green Version]
- Jia, C.; Batterman, S. A critical review of naphthalene sources and exposures relevant to indoor and outdoor air. Int. J. Environ. Res. Public Health 2010, 7, 2903–2939. [Google Scholar] [CrossRef]
- Masih, J.; Masih, A.; Kulshrestha, A.; Singhvi, R.; Taneja, A. Characteristics of polycyclic aromatic hydrocarbons in indoor and outdoor atmosphere in the North central part of India. J. Hazard. Mater. 2010, 177, 190–198. [Google Scholar] [CrossRef]
- Pickett, A.R.; Bell, M.L. Assessment of indoor air pollution in homes with infants. Int. J. Environ. Res. Public Health 2011, 8, 4502–4520. [Google Scholar] [CrossRef]
- Lee, K.; Xue, J.; Geyh, A.S.; Ozkaynak, H.; Leaderer, B.P.; Weschler, C.J.; Spengler, J.D. Nitrous acid, nitrogen dioxide, and ozone concentrations in residential environments. Environ. Health Perspect. 2002, 110, 145–150. [Google Scholar] [CrossRef] [Green Version]
- Héroux, M.E.; Clark, N.; Van Ryswyk, K.; Mallick, R.; Gilbert, N.L.; Harrison, I.; Rispler, K.; Wang, D.; Anastassopoulos, A.; Guay, M.; et al. Predictors of indoor air concentrations in smoking and non-smoking residences. Int. J. Environ. Res. Public Health 2010, 7, 3080–3099. [Google Scholar] [CrossRef] [Green Version]
- Jafta, N.; Barregard, L.; Jeena, P.M.; Naidoo, R.N. Indoor air quality of low and middle income urban households in Durban, South Africa. Environ. Res. 2017, 156, 47–56. [Google Scholar] [CrossRef]
- Simoni, M.; Scognamiglio, A.; Carrozzi, L.; Baldacci, S.; Angino, A.; Pistelli, F.; Di Pede, F.; Viegi, G. Indoor exposures and acute respiratory effects in two general population samples from a rural and an urban area in Italy. J. Expo. Anal. Environ. Epidemiol. 2004, 14 (Suppl. 1), S144–S152. [Google Scholar] [CrossRef] [Green Version]
- Batterman, S.; Jia, C.; Hatzivasilis, G. Migration of volatile organic compounds from attached garages to residences: A major exposure source. Environ. Res. 2007, 104, 224–240. [Google Scholar] [CrossRef]
- Rojas-Bracho, L.; Suh, H.H.; Koutrakis, P. Relationships among personal, indoor, and outdoor fine and coarse particle concentrations for individuals with COPD. J. Expo. Anal. Environ. Epidemiol. 2000, 10, 294–306. [Google Scholar] [CrossRef] [Green Version]
- Abt, E.; Suh, H.H.; Allen, G.; Koutrakis, P. Characterization of indoor particle sources: A study conducted in the metropolitan Boston area. Environ. Health Perspect. 2000, 108, 35–44. [Google Scholar] [CrossRef]
- Klepeis, N.E.; Bellettiere, J.; Hughes, S.C.; Nguyen, B.; Berardi, V.; Liles, S.; Obayashi, S.; Hofstetter, C.R.; Blumberg, E.; Hovell, M.F. Fine particles in homes of predominantly low-income families with children and smokers: Key physical and behavioral determinants to inform indoor-air-quality interventions. PLoS ONE 2017, 12, e0177718. [Google Scholar] [CrossRef]
- Gillespie-Bennett, J.; Pierse, N.; Wickens, K.; Crane, J.; Nicholls, S.; Shields, D.; Boulic, M.; Viggers, H.; Baker, M.; Woodward, A.; et al. Sources of nitrogen dioxide (NO2) in New Zealand homes: Findings from a community randomized controlled trial of heater substitutions. Indoor Air 2008, 18, 521–528. [Google Scholar] [CrossRef]
- Paulin, L.M.; Diette, G.B.; Scott, M.; McCormack, M.C.; Matsui, E.C.; Curtin-Brosnan, J.; Williams, D.L.; Kidd-Taylor, A.; Shea, M.; Breysse, P.N.; et al. Home interventions are effective at decreasing indoor nitrogen dioxide concentrations. Indoor Air 2014, 24, 416–424. [Google Scholar] [CrossRef] [Green Version]
- Colton, M.D.; MacNaughton, P.; Vallarino, J.; Kane, J.; Bennett-Fripp, M.; Spengler, J.D.; Adamkiewicz, G. Indoor air quality in green vs. conventional multifamily low-income housing. Environ. Sci. Technol. 2014, 48, 7833–7841. [Google Scholar] [CrossRef]
- Vardoulakis, S.; Dimitroulopoulou, C.; Thornes, J.; Lai, K.M.; Taylor, J.; Myers, I.; Heaviside, C.; Mavrogianni, A.; Shrubsole, C.; Chalabi, Z.; et al. Impact of climate change on the domestic indoor environment and associated health risks in the UK. Environ. Int. 2015, 85, 299–313. [Google Scholar] [CrossRef] [Green Version]
- Coombs, K.C.; Chew, G.L.; Schaffer, C.; Ryan, P.H.; Brokamp, C.; Grinshpun, S.A.; Adamkiewicz, G.; Chillrud, S.; Hedman, C.; Colton, M.; et al. Indoor air quality in green-renovated vs. non-green low-income homes of children living in a temperate region of US (Ohio). Sci. Total Environ. 2016, 554–555, 178–185. [Google Scholar] [CrossRef] [Green Version]
- Lung, S.-C.C.; Mao, I.F.; Liu, L.-J.S. Residents’ particle exposures in six different communities in Taiwan. Sci. Total Environ. 2007, 377, 81–92. [Google Scholar] [CrossRef] [PubMed]
- McCormack, M.C.; Breysse, P.N.; Hansel, N.N.; Matsui, E.C.; Tonorezos, E.S.; Curtin-Brosnan, J.; Williams, D.L.; Buckley, T.J.; Eggleston, P.A.; Diette, G.B. Common household activities are associated with elevated particulate matter concentrations in bedrooms of inner-city Baltimore pre-school children. Environ. Res. 2008, 106, 148–155. [Google Scholar] [CrossRef] [Green Version]
- Cortez-Lugo, M.; Moreno-Macias, H.; Holguin-Molina, F.; Chow, J.C.; Watson, J.G.; Gutiérrez-Avedoy, V.; Mandujano, F.; Hernández-Ávila, M.; Romieu, I. Relationship between indoor, outdoor, and personal fine particle concentrations for individuals with COPD and predictors of indoor-outdoor ratio in Mexico city. J. Expo. Sci. Environ. Epidemiol. 2008, 18, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Romagnoli, P.; Balducci, C.; Perilli, M.; Vichi, F.; Imperiali, A.; Cecinato, A. Indoor air quality at life and work environments in Rome, Italy. Environ. Sci. Pollut. Res. Int. 2016, 23, 3503–3516. [Google Scholar] [CrossRef]
- Byun, H.; Bae, H.; Kim, D.; Shin, H.; Yoon, C. Effects of socioeconomic factors and human activities on children’s PM10 exposure in inner-city households in Korea. Int. Arch. Occup. Environ. Health 2010, 83, 867–878. [Google Scholar] [CrossRef] [PubMed]
- Kovesi, T.; Creery, D.; Gilbert, N.L.; Dales, R.; Fugler, D.; Thompson, B.; Randhawa, N.; Miller, J.D. Indoor air quality risk factors for severe lower respiratory tract infections in Inuit infants in Baffin Region, Nunavut: A pilot study. Indoor Air 2006, 16, 266–275. [Google Scholar] [CrossRef]
- Raaschou-Nielsen, O.; Sørensen, M.; Hertel, O.; Chawes, B.L.; Vissing, N.; Bønnelykke, K.; Bisgaard, H. Predictors of indoor fine particulate matter in infants’ bedrooms in Denmark. Environ. Res. 2011, 111, 87–93. [Google Scholar] [CrossRef]
- Pavilonis, B.T.; Anthony, T.R.; O’Shaughnessy, P.T.; Humann, M.J.; Merchant, J.A.; Moore, G.; Thorne, P.S.; Weisel, C.P.; Sanderson, W.T. Indoor and outdoor particulate matter and endotoxin concentrations in an intensely agricultural county. J. Expo. Sci. Environ. Epidemiol. 2013, 23, 299–305. [Google Scholar] [CrossRef] [Green Version]
- García Algar, O.; Pichini, S.; Basagaña, X.; Puig, C.; Vall, O.; Torrent, M.; Harris, J.; Sunyer, J.; Cullinan, P. Concentrations and determinants of NO2 in homes of Ashford, UK and Barcelona and Menorca, Spain. Indoor Air 2004, 14, 298–304. [Google Scholar] [CrossRef]
- Massey, D.; Kulshrestha, A.; Masih, J.; Taneja, A. Seasonal trends of PM10, PM5.0, PM2.5 & PM1.0 in indoor and outdoor environments of residential homes located in North-Central India. Build. Environ. 2012, 47, 223–231. [Google Scholar] [CrossRef]
- Vanker, A.; Barnett, W.; Nduru, P.M.; Gie, R.P.; Sly, P.D.; Zar, H.J. Home environment and indoor air pollution exposure in an African birth cohort study. Sci. Total Environ. 2015, 536, 362–367. [Google Scholar] [CrossRef] [Green Version]
- Lawrence, A.J.; Masih, A.; Taneja, A. Indoor/outdoor relationships of carbon monoxide and oxides of nitrogen in domestic homes with roadside, urban and rural locations in a central Indian region. Indoor Air 2005, 15, 76–82. [Google Scholar] [CrossRef]
- Topp, R.; Cyrys, J.; Gebefügi, I.; Schnelle-Kreis, J.; Richter, K.; Wichmann, H.E.; Heinrich, J. Indoor and outdoor air concentrations of BTEX and NO2: Correlation of repeated measurements. J. Environ. Monit. 2004, 6, 807–812. [Google Scholar] [CrossRef]
- Khoder, M.; Shakour, A.; Farag, S.A.; Awad, A. Indoor and outdoor formaldehyde concentrations in homes in residential areas in Greater Cairo. J. Environ. Monit. 2000, 2, 123–126. [Google Scholar] [CrossRef]
- Su, F.C.; Mukherjee, B.; Batterman, S. Determinants of personal, indoor and outdoor VOC concentrations: An analysis of the RIOPA data. Environ. Res 2013, 126, 192–203. [Google Scholar] [CrossRef] [Green Version]
- Brown, K.W.; Sarnat, J.A.; Suh, H.H.; Coull, B.A.; Spengler, J.D.; Koutrakis, P. Ambient site, home outdoor and home indoor particulate concentrations as proxies of personal exposures. J. Environ. Monit. 2008, 10, 1041–1051. [Google Scholar] [CrossRef] [Green Version]
- Nazariah, S.; Jalaludin, J.; Md Akim, A. Interleukin-6 via Sputum Induction as Biomarker of Inflammation for Indoor Particulate Matter among Primary School Children in Klang Valley, Malaysia. Glob. J. Health Sci. 2013, 5, 93–105. [Google Scholar] [CrossRef] [Green Version]
- Brauer, M.; Hrubá, F.; Mihalíková, E.; Fabiánová, E.; Miskovic, P.; Plziková, A.; Lendacká, M.; Vandenberg, J.; Cullen, A. Personal exposure to particles in Banská Bystrica, Slovakia. J. Expo. Anal. Environ. Epidemiol. 2000, 10, 478–487. [Google Scholar] [CrossRef] [Green Version]
- Simons, E.; Curtin-Brosnan, J.; Buckley, T.; Breysse, P.; Eggleston, P.A. Indoor environmental differences between inner city and suburban homes of children with asthma. J. Urban Health 2007, 84, 577–590. [Google Scholar] [CrossRef] [Green Version]
- Hulin, M.; Caillaud, D.; Annesi-Maesano, I. Indoor air pollution and childhood asthma: Variations between urban and rural areas. Indoor Air 2010, 20, 502–514. [Google Scholar] [CrossRef]
- Chatzis, C.; Alexopoulos, E.C.; Linos, A. Indoor and outdoor personal exposure to benzene in Athens, Greece. Sci. Total Environ. 2005, 349, 72–80. [Google Scholar] [CrossRef]
- Jones, J.; Stick, S.; Dingle, P.; Franklin, P. Spatial variability of particulates in homes: Implications for infant exposure. Sci. Total Environ. 2007, 376, 317–323. [Google Scholar] [CrossRef]
- Nasir, Z.; Colbeck, I. Particulate pollution in different housing types in a UK suburban location. Sci. Total Environ. 2013, 445–446C, 165–176. [Google Scholar] [CrossRef] [Green Version]
- Russo, E.T.; Hulse, T.E.; Adamkiewicz, G.; Levy, D.E.; Bethune, L.; Kane, J.; Reid, M.; Shah, S.N. Comparison of indoor air quality in smoke-permitted and smoke-free multiunit housing: Findings from the Boston Housing Authority. Nicotine Tob. Res. 2015, 17, 316–322. [Google Scholar] [CrossRef] [Green Version]
- King, B.A.; Travers, M.J.; Cummings, K.M.; Mahoney, M.C.; Hyland, A.J. Secondhand smoke transfer in multiunit housing. Nicotine Tob. Res. 2010, 12, 1133–1141. [Google Scholar] [CrossRef]
- World Health Organization. Air Quality Guidelines for Europe, 2nd ed.; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2000; Available online: https://www.euro.who.int/__data/assets/pdf_file/0005/74732/E71922.pdf (accessed on 22 November 2020).
- World Health Organization. Air Quality Guidelines. Global Update 2005; World Health Organization Regional Office for Europe: Copenhagen, Denmark, 2006; Available online: https://www.euro.who.int/__data/assets/pdf_file/0005/78638/E90038.pdf (accessed on 22 November 2020).
- Vardoulakis, S.; Kettle, R.; Cosford, P.; Lincoln, P.; Holgate, S.; Grigg, J.; Kelly, F.; Pencheon, D. Local action on outdoor air pollution to improve public health. Int. J. Public Health 2018, 63, 557–565. [Google Scholar] [CrossRef]
- Baxter, L.K.; Clougherty, J.E.; Laden, F.; Levy, J.I. Predictors of concentrations of nitrogen dioxide, fine particulate matter, and particle constituents inside of lower socioeconomic status urban homes. J. Expo. Sci. Environ. Epidemiol. 2007, 17, 433–444. [Google Scholar] [CrossRef] [Green Version]
- Rotko, T.; Koistinen, K.; HÄNninen, O.; Jantunen, M. Sociodemographic descriptors of personal exposure to fine particles (PM2.5) in EXPOLIS Helsinki. J. Expo. Sci. Environ. Epidemiol. 2000, 10, 385–393. [Google Scholar] [CrossRef]
- Shrubsole, C.; Macmillan, A.; Davies, M.; May, N. 100 Unintended consequences of policies to improve the energy efficiency of the UK housing stock. Indoor Built Environ. 2014, 23, 340–352. [Google Scholar] [CrossRef]
- World Health Organization. Health in the Green Economy: Health Co-Benefits of Climate Change Mitigation-Housing Sector; World Health Organization: Geneva, Switzerland, 2011; Available online: https://www.who.int/publications/i/item/9789241501712 (accessed on 10 November 2020).
- Asikainen, A.; Carrer, P.; Kephalopoulos, S.; de Fernandes, E.O.; Wargocki, P.; Hänninen, O. Reducing burden of disease from residential indoor air exposures in Europe (HEALTHVENT project). Environ. Health 2016, 15, S35. [Google Scholar] [CrossRef]
- Kelly, F.J.; Fussell, J.C. Improving indoor air quality, health and performance within environments where people live, travel, learn and work. Atmos. Environ. 2019, 200, 90–109. [Google Scholar] [CrossRef] [Green Version]
- US EPA. Improving Indoor Air Quality. Indoor Air Quality (IAQ). US Environmental Protection Agency. 2020. Available online: https://www.epa.gov/indoor-air-quality-iaq/improving-indoor-air-quality (accessed on 10 November 2020).
- RCPCH & RCP. The inside story: Health effects of indoor air quality on children and young people. Royal College of Paediatrics and Child Health & Royal College of Physicians. 2020. Available online: https://www.rcpch.ac.uk/resources/inside-story-health-effects-indoor-air-quality-children-young-people (accessed on 10 November 2020).
- Vardoulakis, S.; Crawford, J.; Davis, A.; Steinle, S.; Sleeuwenhoek, A.; Galea, K.; Dixon, K. Indoor Exposure to Selected Air Pollutants and Associated Health Effects–a Global Review; IOM Technical Report; Institute of Occupational Medicine: Edinburgh, UK, 2019. [Google Scholar]

| Pollutant | Range (indoor) | WHO (indoor) | WHO (outdoor) |
|---|---|---|---|
| PM2.5 | 1.7–428.6 | - | 25/10 e |
| PM10 | 11.0–1275 | - | 50/20 e |
| NO2 | 3.4–1210 | 200/40 a | 200/40 a |
| Benzene | 0.6–24.8 | 1.7 b | 1.7 b |
| Toluene | 3.0–325.5 | - | 1000/260 f |
| Formaldehyde | 7.5–134.0 | 100 c | 100 c |
| Naphthalene | 0.12–26.3 | 10 d | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vardoulakis, S.; Giagloglou, E.; Steinle, S.; Davis, A.; Sleeuwenhoek, A.; Galea, K.S.; Dixon, K.; Crawford, J.O. Indoor Exposure to Selected Air Pollutants in the Home Environment: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 8972. https://doi.org/10.3390/ijerph17238972
Vardoulakis S, Giagloglou E, Steinle S, Davis A, Sleeuwenhoek A, Galea KS, Dixon K, Crawford JO. Indoor Exposure to Selected Air Pollutants in the Home Environment: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(23):8972. https://doi.org/10.3390/ijerph17238972
Chicago/Turabian StyleVardoulakis, Sotiris, Evanthia Giagloglou, Susanne Steinle, Alice Davis, Anne Sleeuwenhoek, Karen S. Galea, Ken Dixon, and Joanne O. Crawford. 2020. "Indoor Exposure to Selected Air Pollutants in the Home Environment: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 23: 8972. https://doi.org/10.3390/ijerph17238972
APA StyleVardoulakis, S., Giagloglou, E., Steinle, S., Davis, A., Sleeuwenhoek, A., Galea, K. S., Dixon, K., & Crawford, J. O. (2020). Indoor Exposure to Selected Air Pollutants in the Home Environment: A Systematic Review. International Journal of Environmental Research and Public Health, 17(23), 8972. https://doi.org/10.3390/ijerph17238972







