Treatment of Class III Malocclusion and Anterior Crossbite with Aligners: A Case Report
Abstract
:1. Introduction
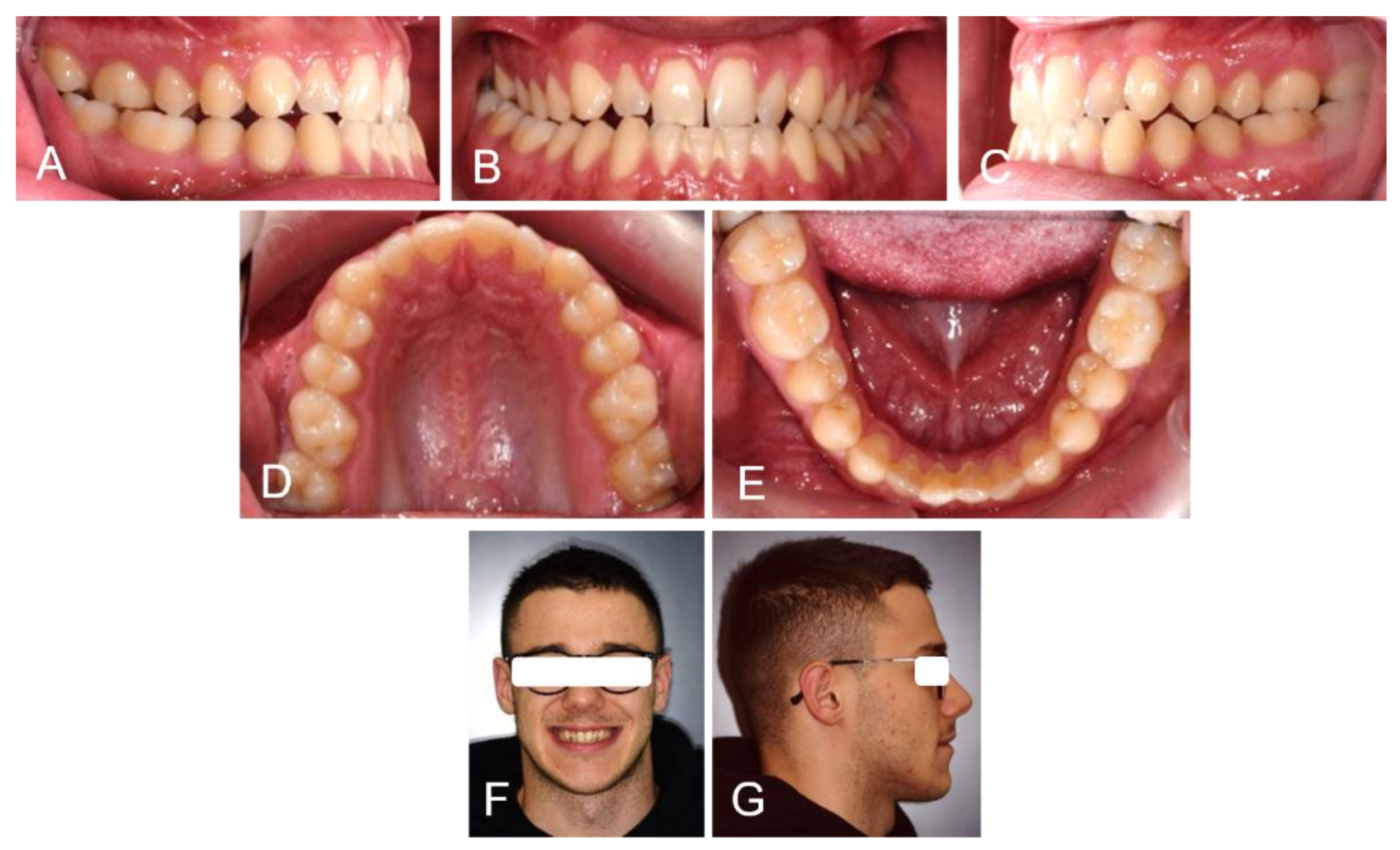
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dehesa-Santos, A.; Iber-Diaz, P.; Iglesias-Linares, A. Genetic Factors Contributing to Skeletal Class III Malocclusion: A Systematic Review and Meta-Analysis. Clin. Oral Investig. 2021, 25, 1587–1612. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Silva, A.; Carnevali-Arellano, R.; Vivanco-Coke, S.; Tobar-Reyes, J.; Araya-Díaz, P.; Palomino-Montenegro, H. Craniofacial Growth Predictors for Class II and III Malocclusions: A Systematic Review. Clin. Exp. Dent. Res. 2021, 7, 242–262. [Google Scholar] [CrossRef] [PubMed]
- Rongo, R.; D’Antò, V.; Bucci, R.; Polito, I.; Martina, R.; Michelotti, A. Skeletal and Dental Effects of Class III Orthopaedic Treatment: A Systematic Review and Meta-Analysis. J. Oral Rehabil. 2017, 44, 545–562. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Palmieri, G.; et al. Genetic Pattern, Orthodontic and Surgical Management of Multiple Supplementary Impacted Teeth in a Rare, Cleidocranial Dysplasia Patient: A Case Report. Medicina 2021, 57, 1350. [Google Scholar] [CrossRef] [PubMed]
- Ngan, P. Early Timely Treatment of Class III Malocclusion. Semin. Orthod. 2005, 11, 140–145. [Google Scholar] [CrossRef]
- Nucci, L.; Costanzo, C.; Carfora, M.; d’Apuzzo, F.; Franchi, L.; Perillo, L. Dentoskeletal Effects of Early Class III Treatment Protocol Based on Timing of Intervention in Children. Prog. Orthod. 2021, 22, 49. [Google Scholar] [CrossRef]
- Maspero, C.; Abate, A.; Inchingolo, F.; Dolci, C.; Cagetti, M.G.; Tartaglia, G.M. Incidental Finding in Pre-Orthodontic Treatment Radiographs of an Aural Foreign Body: A Case Report. Children 2022, 9, 421. [Google Scholar] [CrossRef]
- Alfaifi, A.H. Restorative Management and Treatment of Pseudo-Class III Malocclusion. Case Rep. Dent. 2021, 2021, 8470222. [Google Scholar] [CrossRef]
- Kale, B.; Buyukcavus, M.H. Comparison of Three-Dimensional Soft-Tissue Evaluations between Skeletal and Pseudo-Class III Malocclusions. Sci. Rep. 2020, 10, 14717. [Google Scholar] [CrossRef]
- Patianna, A.G.; Ballini, A.; Meneghello, M.; Cantore, S.; Inchingolo, A.M.; Dipalma, G.; Inchingolo, A.D.; Inchingolo, F.; Malcangi, G.; Lucchese, A.; et al. Comparison of Conventional Orthognathic Surgery and “Surgery-First” Protocol: A New Weapon against Time. J. Biol. Regul. Homeost. Agents 2019, 33, 59–67. [Google Scholar]
- Adina, S.; Dipalma, G.; Bordea, I.R.; Lucaciu, O.; Feurdean, C.; Inchingolo, A.D.; Septimiu, R.; Malcangi, G.; Cantore, S.; Martin, D.; et al. Orthopedic Joint Stability Influences Growth and Maxillary Development: Clinical Aspects. J. Biol. Regul. Homeost. Agents 2020, 34, 747–756. [Google Scholar] [CrossRef]
- Cardarelli, F.; Patano, A.; Montenegro, V.; Malcangi, G.; Coloccia, G.; Inchingolo, A.D.; Marinelli, G.; Laudadio, C.; Dipalma, G.; Di Venere, D.; et al. Elastodontic therapy un nuovo approccio alla terapia ortodontica funzionale. Il Dent. Mod. 2021, 10, 48–63. [Google Scholar]
- Fabozzi, F.F.; Nucci, L.; Correra, A.; d’Apuzzo, F.; Franchi, L.; Perillo, L. Comparison of Two Protocols for Early Treatment of Dentoskeletal Class III Malocclusion: Modified SEC III versus RME/FM. Orthod. Craniofac. Res. 2021, 24, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Mora Martínez, M.A.; Pesqueira Melgarejo, R.; Hernández Espinosa, G.; De Silva Dávila, J.L.; Rodríguez Chávez, J.A. Alteración dentofacial clase III tratado con camuflaje: Reporte de caso clínico. Rev. Mex. Ortod. 2015, 3, 62–69. [Google Scholar] [CrossRef]
- Farronato, M.; Maspero, C.; Abate, A.; Grippaudo, C.; Connelly, S.T.; Tartaglia, G.M. 3D Cephalometry on Reduced FOV CBCT: Skeletal Class Assessment through AF-BF on Frankfurt Plane—Validity and Reliability through Comparison with 2D Measurements. Eur. Radiol. 2020, 30, 6295–6302. [Google Scholar] [CrossRef] [PubMed]
- Montinaro, F.; Nucci, L.; Carfora, M.; d’Apuzzo, F.; Franchi, L.; Perillo, L. Modified SEC III Protocol: Vertical Control Related to Patients’ Compliance with the Chincup. Eur. J. Orthod. 2021, 43, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Malekian, K.; Parrini, S.; Garino, F.; Deregibus, A.; Castroflorio, T. Mandibular Molar Distalization with Clear Aligners in Class III Patients. J. Aligner Orthod. 2019, 3, 7–14. [Google Scholar]
- Papadimitriou, A.; Mousoulea, S.; Gkantidis, N.; Kloukos, D. Clinical Effectiveness of Invisalign® Orthodontic Treatment: A Systematic Review. Prog. Orthod. 2018, 19, 37. [Google Scholar] [CrossRef]
- Laudadio, C.; Inchingolo, A.D.; Malcangi, G.; Limongelli, L.; Marinelli, G.; Coloccia, G.; Montenegro, V.; Patano, A.; Inchingolo, F.; Bordea, I.R.; et al. Management of Anterior Open-Bite in the Deciduous, Mixed and Permanent Dentition Stage: A Descriptive Review. J. Biol. Regul. Homeost. Agents 2021, 35, 271–281. [Google Scholar] [CrossRef]
- Di Venere, D.; Corsalini, M.; Nardi, G.M.; Laforgia, A.; Grassi, F.R.; Rapone, B.; Pettini, F. Obstructive Site Localization in Patients with Obstructive Sleep Apnea Syndrome: A Comparison between Otolaryngologic Data and Cephalometric Values. Oral Implantol. 2017, 10, 295–310. [Google Scholar] [CrossRef]
- De Felice, M.E.; Nucci, L.; Fiori, A.; Flores-Mir, C.; Perillo, L.; Grassia, V. Accuracy of Interproximal Enamel Reduction during Clear Aligner Treatment. Prog. Orthod. 2020, 21, 28. [Google Scholar] [CrossRef] [PubMed]
- Robertson, L.; Lee, D.; Eimar, H.; El-Bialy, T. Treatment of a Challenging Class III Malocclusion Case Using Invisalign Clear Aligners and Micro-Osteoperforation: A Case Report. J. Aligner Orthod. 2019, 3, 229–241. [Google Scholar]
- Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; Debernardi, C.L. Efficacy of Clear Aligners in Controlling Orthodontic Tooth Movement: A Systematic Review. Angle Orthod. 2014, 85, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, L.; Colonna, A.; Carlucci, A.; Oliverio, T.; Siciliani, G. Class II Subdivision Correction with Clear Aligners Using Intermaxilary Elastics. Prog. Orthod. 2018, 19, 32. [Google Scholar] [CrossRef]
- Caruso, S.; Nota, A.; Ehsani, S.; Maddalone, E.; Ojima, K.; Tecco, S. Impact of Molar Teeth Distalization with Clear Aligners on Occlusal Vertical Dimension: A Retrospective Study. BMC Oral Health 2019, 19, 182. [Google Scholar] [CrossRef]
- Wheeler, T.T. Orthodontic Clear Aligner Treatment. Semin. Orthod. 2017, 23, 83–89. [Google Scholar] [CrossRef]
- Jindal, P.; Juneja, M.; Siena, F.L.; Bajaj, D.; Breedon, P. Mechanical and Geometric Properties of Thermoformed and 3D Printed Clear Dental Aligners. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 694–701. [Google Scholar] [CrossRef]
- Marinelli, G.; Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Limongelli, L.; Montenegro, V.; Coloccia, G.; Laudadio, C.; Patano, A.; Inchingolo, F.; et al. White Spot Lesions in Orthodontics: Prevention and Treatment. A Descriptive Review. J. Biol. Regul. Homeost. Agents 2021, 35, 227–240. [Google Scholar] [CrossRef]
- Patano, A.; Cirulli, N.; Beretta, M.; Plantamura, P.; Inchingolo, A.D.; Inchingolo, A.M.; Bordea, I.R.; Malcangi, G.; Marinelli, G.; Scarano, A.; et al. Education Technology in Orthodontics and Paediatric Dentistry during the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 6056. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Montenegro, V.; Laudadio, C.; Pede, C.D.; et al. The Efficacy of a New AMCOP® Elastodontic Protocol for Orthodontic Interceptive Treatment: A Case Series and Literature Overview. Int. J. Environ. Res. Public Health 2022, 19, 988. [Google Scholar] [CrossRef]
- Farronato, M.; Farronato, D.; Inchingolo, F.; Grassi, L.; Lanteri, V.; Maspero, C. Evaluation of Dental Surface after De-Bonding Orthodontic Bracket Bonded with a Novel Fluorescent Composite: In Vitro Comparative Study. Appl. Sci. 2021, 11, 6354. [Google Scholar] [CrossRef]
- Cantore, S.; Ballini, A.; Farronato, D.; Malcangi, G.; Dipalma, G.; Assandri, F.; Garagiola, U.; Inchingolo, F.; De Vito, D.; Cirulli, N. Evaluation of an Oral Appliance in Patients with Mild to Moderate Obstructive Sleep Apnea Syndrome Intolerant to Continuous Positive Airway Pressure Use: Preliminary Results. Int. J. Immunopathol. Pharmacol. 2016, 29, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Brugnami, F.; Meuli, S.; Caiazzo, A.; Marrocco, S.; Scopelliti, D. Three-Dimensional Digital Planning of Class III Decompensation with Clear Aligners: Hard and Soft Tissue Augmentation with Concomitant Corticotomy to Stretch the Limits of Safe Orthodontic Treatment. J. Oral Biol. Craniofacial Res. 2021, 11, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.; Patel, D.; Yadav, S. Staging Orthodontic Aligners for Complex Orthodontic Tooth Movement. Turk. J. Orthod. 2021, 34, 202–206. [Google Scholar] [CrossRef]
- Edelmann, A.; English, J.D.; Chen, S.J.; Kasper, F.K. Analysis of the Thickness of 3-Dimensional-Printed Orthodontic Aligners. Am. J. Orthod. Dentofac. Orthop. 2020, 158, e91–e98. [Google Scholar] [CrossRef]
- Cozzani, M.; Sadri, D.; Nucci, L.; Jamilian, P.; Pirhadirad, A.P.; Jamilian, A. The Effect of Alexander, Gianelly, Roth, and MBT Bracket Systems on Anterior Retraction: A 3-Dimensional Finite Element Study. Clin. Oral Investig. 2020, 24, 1351–1357. [Google Scholar] [CrossRef]
- Sahm, G.; Bartsch, A.; Witt, E. Reliability of Patient Reports on Compliance. Eur. J. Orthod. 1990, 12, 438–446. [Google Scholar] [CrossRef]
- Montenegro, V.; Inchingolo, A.D.; Malcangi, G.; Limongelli, L.; Marinelli, G.; Coloccia, G.; Laudadio, C.; Patano, A.; Inchingolo, F.; Bordea, I.R.; et al. Compliance of Children with Removable Functional Appliance with Microchip Integrated during COVID-19 Pandemic: A Systematic Review. J. Biol. Regul. Homeost. Agents 2021, 35, 365–377. [Google Scholar] [CrossRef]
- Di Venere, D. Correlation between Parodontal Indexes and Orthodontic Retainers: Prospective Study in a Group of 16 Patients. Oral Implantol. 2017, 10, 78. [Google Scholar] [CrossRef]
- Putrino, A.; Barbato, E.; Galluccio, G. Clear Aligners: Between Evolution and Efficiency-A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 2870. [Google Scholar] [CrossRef]
- Ballini, A.; Cantore, S.; Scacco, S.; Perillo, L.; Scarano, A.; Aityan, S.K.; Contaldo, M.; Cd Nguyen, K.; Santacroce, L.; Syed, J.; et al. A Comparative Study on Different Stemness Gene Expression between Dental Pulp Stem Cells vs. Dental Bud Stem Cells. Eur. Rev. Med. Pharmacol. Sci. 2019, 23, 1626–1633. [Google Scholar] [CrossRef] [PubMed]
- Kravitz, N.D.; Moshiri, M.; Nicozisis, J.; Miller, S. Mechanical Considerations for Deep-Bite Correction with Aligners. Semin. Orthod. 2020, 26, 134–138. [Google Scholar] [CrossRef]
- Marra, P.; Nucci, L.; Jamilian, A.; Perillo, L.; Itro, A.; Grassia, V. Odontoma in a Young and Anxious Patient Associated with Unerupted Permanent Mandibular Cuspid: A Case Report. J. Int. Oral Health 2020, 12, 182. [Google Scholar] [CrossRef]
- Di Venere, D.; Nardi, G.M.; Lacarbonara, V.; Laforgia, A.; Stefanachi, G.; Corsalini, M.; Grassi, F.R.; Rapone, B.; PETTINI, F. Early Mandibular Canine-Lateral Incisor Transposition: Case Report. Oral Implantol. 2017, 10, 181–189. [Google Scholar] [CrossRef]
- Hu, H.; Chen, J.; Guo, J.; Li, F.; Liu, Z.; He, S.; Zou, S. Distalization of the Mandibular Dentition of an Adult with a Skeletal Class III Malocclusion. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 854–862. [Google Scholar] [CrossRef]
- Cirulli, N.; Ballini, A.; Cantore, S.; Farronato, D.; Inchingolo, F.; Dipalma, G.; Gatto, M.R.; Alessandri Bonetti, G. Mixed dentition space analysis of a southern italian population: New regression equations for unerupted teeth. J. Biol. Regul. Homeost. Agents 2015, 29, 515–520. [Google Scholar]
- El-Bialy, T. The Use of High Frequency Vibration and Clear Aligners in Management of an Adult Patient with Class III Skeletal Malocclusion with Open Bite and Severe Bimaxillary Protrusion: Case Report. Dent. J. 2020, 8, 75. [Google Scholar] [CrossRef]
- Coloccia, G.; Inchingolo, A.D.; Inchingolo, A.M.; Malcangi, G.; Montenegro, V.; Patano, A.; Marinelli, G.; Laudadio, C.; Limongelli, L.; Di Venere, D.; et al. Effectiveness of Dental and Maxillary Transverse Changes in Tooth-Borne, Bone-Borne, and Hybrid Palatal Expansion through Cone-Beam Tomography: A Systematic Review of the Literature. Medicina 2021, 57, 288. [Google Scholar] [CrossRef]
- Simon, M.; Keilig, L.; Schwarze, J.; Jung, B.A.; Bourauel, C. Forces and Moments Generated by Removable Thermoplastic Aligners: Incisor Torque, Premolar Derotation, and Molar Distalization. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 728–736. [Google Scholar] [CrossRef]
- Dianiskova, S.; Rongo, R.; Buono, R.; Franchi, L.; Michelotti, A.; D’Antò, V. Treatment of Mild Class II Malocclusion in Growing Patients with Clear Aligners versus Fixed Multibracket Therapy: A Retrospective Study. Orthod. Craniofacial Res. 2022, 25, 96–102. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Ceci, S.; Patano, A.; Inchingolo, A.M.; Montenegro, V.; Di Pede, C.; Malcangi, G.; Marinelli, G.; Coloccia, G.; Garibaldi, M.; et al. Elastodontic Therapy of Hyperdivergent Class II Patients Using AMCOP® Devices: A Retrospective Study. Appl. Sci. 2022, 12, 3259. [Google Scholar] [CrossRef]
- Maspero, C.; Cappella, A.; Dolci, C.; Cagetti, M.G.; Inchingolo, F.; Sforza, C. Is Orthodontic Treatment with Microperforations Worth It? A Scoping Review. Children 2022, 9, 208. [Google Scholar] [CrossRef] [PubMed]
- Di Venere, D.; Rapone, B.; Corsalini, M. Dental Trauma in the Anterior Sector: An Analysis of the Predisposing Factors in a Group of Orthodontic Patients. Clin. Ther. 2020, 171, e481–e485. [Google Scholar] [CrossRef] [PubMed]
- Ravera, S.; Castroflorio, T.; Garino, F.; Daher, S.; Cugliari, G.; Deregibus, A. Maxillary Molar Distalization with Aligners in Adult Patients: A Multicenter Retrospective Study. Prog. Orthod. 2016, 17, 12. [Google Scholar] [CrossRef]
- Patano, A.; Di Venere, D.; Ceci, S.; Berate, P.; Candrea, S.; Babtan, A.-M.; Azzollini, D.; Piras, F.; Curatoli, L.; Corriero, A.; et al. Essential Oils Utility Implications in Symptomatic Burning Mouth Syndrome. Balneo PRM Res. J. 2021, 12, 381–385. [Google Scholar] [CrossRef]
- Ceci, S.; Berate, P.; Candrea, S.; Babtan, A.-M.; Azzollini, D.; Piras, F.; Curatoli, L.; Corriero, A.; Patano, A.; Valente, F.; et al. The Oral and Gut Microbiota: Beyond a Short Communication. Balneo PRM Res. J. 2021, 12, 405–411. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Cazzolla, A.P.; Di Cosola, M.; Greco Lucchina, A.; Santacroce, L.; Charitos, I.A.; Topi, S.; Malcangi, G.; Hazballa, D.; Scarano, A.; et al. The Integumentary System and Its Microbiota between Health and Disease. J. Biol. Regul. Homeost. Agents 2021, 35, 303–321. [Google Scholar] [CrossRef]
- Dimonte, M.; Inchingolo, F.; Minonne, A.; Arditi, G.; Dipalma, G. Bone SPECT in Management of Mandibular Condyle Hyperplasia. Report of a Case and Review of Literature. Minerva Stomatol. 2004, 53, 281–285. [Google Scholar]
- Sangalli, L.; Laffranchi, L. Skeletal Class III Malocclusion Treated with Clear Aligners and Remote Digital Monitoring during the COVID-19 Pandemic. A Case Report. Sci. Arch. Dent. Sci. 2022, 5, 26–34. [Google Scholar]
- Staderini, E.; Meuli, S.; Gallenzi, P. Orthodontic Treatment of Class Three Malocclusion Using Clear Aligners: A Case Report. J. Oral Biol. Craniofacial Res. 2019, 9, 360–362. [Google Scholar] [CrossRef]
- d’Apuzzo, F.; Minervini, G.; Grassia, V.; Rotolo, R.P.; Perillo, L.; Nucci, L. Mandibular Coronoid Process Hypertrophy: Diagnosis and 20-Year Follow-Up with CBCT, MRI and EMG Evaluations. Appl. Sci. 2021, 11, 4504. [Google Scholar] [CrossRef]
- Malcangi, G.; Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Garibaldi, M.; Inchingolo, A.M.; Piras, F.; Cardarelli, F.; Settanni, V.; et al. Impacted Central Incisors in the Upper Jaw in an Adolescent Patient: Orthodontic-Surgical Treatment—A Case Report. Appl. Sci. 2022, 12, 2657. [Google Scholar] [CrossRef]







| Cephalometric Parameters | Min | Mean | Max | t0 |
|---|---|---|---|---|
| Sagittal Skeletal Relations | ||||
| Maxillary Position | 78.5° | 82° | 85.5° | 82.5° |
| Mandibular Position | 76.5° | 80° | 83.5° | 84.4° |
| Sagittal Jaw Relation | −0.5° | 2° | 4.5° | −1.9° |
| Vertical Skeletal Relations | ||||
| Maxillary Inclination | 5° | 8° | 11° | 4.3° |
| Mandibular Inclination | 30.5° | 33° | 35.5° | 31° |
| Vertical Jaw Relation | 19° | 25° | 31° | 27.6° |
| Dento Basal Relations | ||||
| Maxillary Incisor Inclination | 104° | 110° | 116° | 106.9° |
| Mandibular Incisor Inclination | 87° | 94° | 101° | 81.4° |
| Mandibular Incisor Compensation | 0 | 2 | 4 | 3.7 |
| Dental Relations | ||||
| Overjet | 1 | 3.5 | 6 | −0.9 |
| Overbite | −0.5 | 2 | 4.5 | −0.9 |
| Interincisal Angle | 126° | 132° | 138° | 140.6° |
| Cephalometric Parameters | Min | Mean | Max | t1 |
|---|---|---|---|---|
| Sagittal Skeletal Relations | ||||
| Maxillary Position | 78.5° | 82° | 85.5° | 82.5° |
| Mandibular Position | 76.5° | 80° | 83.5° | 84.4° |
| Sagittal Jaw Relation | −0.5° | 2° | 4.5° | −1.9° |
| Vertical Skeletal Relations | ||||
| Maxillary Inclination | 5° | 8° | 11° | 4.3° |
| Mandibular Inclination | 30.5° | 33° | 35.5° | 31° |
| Vertical Jaw Relation | 19° | 25° | 31° | 26.7° |
| Dento Basal Relations | ||||
| Maxillary Incisor Inclination | 104° | 110° | 116° | 115.2° |
| Mandibular Incisor Inclination | 87° | 94° | 101° | 84.9° |
| Mandibular Incisor Compensation | 0 | 2 | 4 | 1.9 |
| Dental Relations | ||||
| Overjet | 1 | 3.5 | 6 | 3.5 |
| Overbite | −0.5 | 2 | 4.5 | 3.4 |
| Interincisal Angle | 126° | 132° | 138° | 145° |
| Cephalometric Parameters | Min | Mean | Max | t0 | t1 |
|---|---|---|---|---|---|
| Sagittal Skeletal Relations | |||||
| Maxillary Position | 78.5° | 82° | 85.5° | 82.5° | 82.5° |
| Mandibular Position | 76.5° | 80° | 83.5° | 84.4° | 84.4° |
| Sagittal Jaw Relation | −0.5° | 2° | 4.5° | −1.9° | −1.9° |
| Vertical Skeletal Relations | |||||
| Maxillary Inclination | 5° | 8° | 11° | 4.3° | 4.3° |
| Mandibular Inclination | 30.5° | 33° | 35.5° | 31° | 31° |
| Vertical Jaw Relation | 19° | 25° | 31° | 27.6° | 26.7° |
| Dento Basal Relations | |||||
| Maxillary Incisor Inclination | 104° | 110° | 116° | 106.9° | 115.2° |
| Mandibular Incisor Inclination | 87° | 94° | 101° | 81.4° | 84.9° |
| Mandibular Incisor Compensation | 0 | 2 | 4 | 3.7 | 1.9 |
| Dental Relations | |||||
| Overjet | 1 | 3.5 | 6 | −0.9 | 3.5 |
| Overbite | −0.5 | 2 | 4.5 | −0.9 | 3.4 |
| Interincisal Angle | 126° | 132° | 138° | 140.6° | 145° |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Di Pede, C.; Garibaldi, M.; Ciocia, A.M.; et al. Treatment of Class III Malocclusion and Anterior Crossbite with Aligners: A Case Report. Medicina 2022, 58, 603. https://doi.org/10.3390/medicina58050603
Inchingolo AD, Patano A, Coloccia G, Ceci S, Inchingolo AM, Marinelli G, Malcangi G, Di Pede C, Garibaldi M, Ciocia AM, et al. Treatment of Class III Malocclusion and Anterior Crossbite with Aligners: A Case Report. Medicina. 2022; 58(5):603. https://doi.org/10.3390/medicina58050603
Chicago/Turabian StyleInchingolo, Alessio Danilo, Assunta Patano, Giovanni Coloccia, Sabino Ceci, Angelo Michele Inchingolo, Grazia Marinelli, Giuseppina Malcangi, Chiara Di Pede, Mariagrazia Garibaldi, Anna Maria Ciocia, and et al. 2022. "Treatment of Class III Malocclusion and Anterior Crossbite with Aligners: A Case Report" Medicina 58, no. 5: 603. https://doi.org/10.3390/medicina58050603
APA StyleInchingolo, A. D., Patano, A., Coloccia, G., Ceci, S., Inchingolo, A. M., Marinelli, G., Malcangi, G., Di Pede, C., Garibaldi, M., Ciocia, A. M., Mancini, A., Palmieri, G., Rapone, B., Piras, F., Cardarelli, F., Nucci, L., Bordea, I. R., Scarano, A., Lorusso, F., ... Inchingolo, F. (2022). Treatment of Class III Malocclusion and Anterior Crossbite with Aligners: A Case Report. Medicina, 58(5), 603. https://doi.org/10.3390/medicina58050603




















