Pneumothorax, an Uncommon but Devastating Complication Following Shoulder Arthroscopy: Case Reports
Abstract
:1. Introduction
2. Clinical Cases
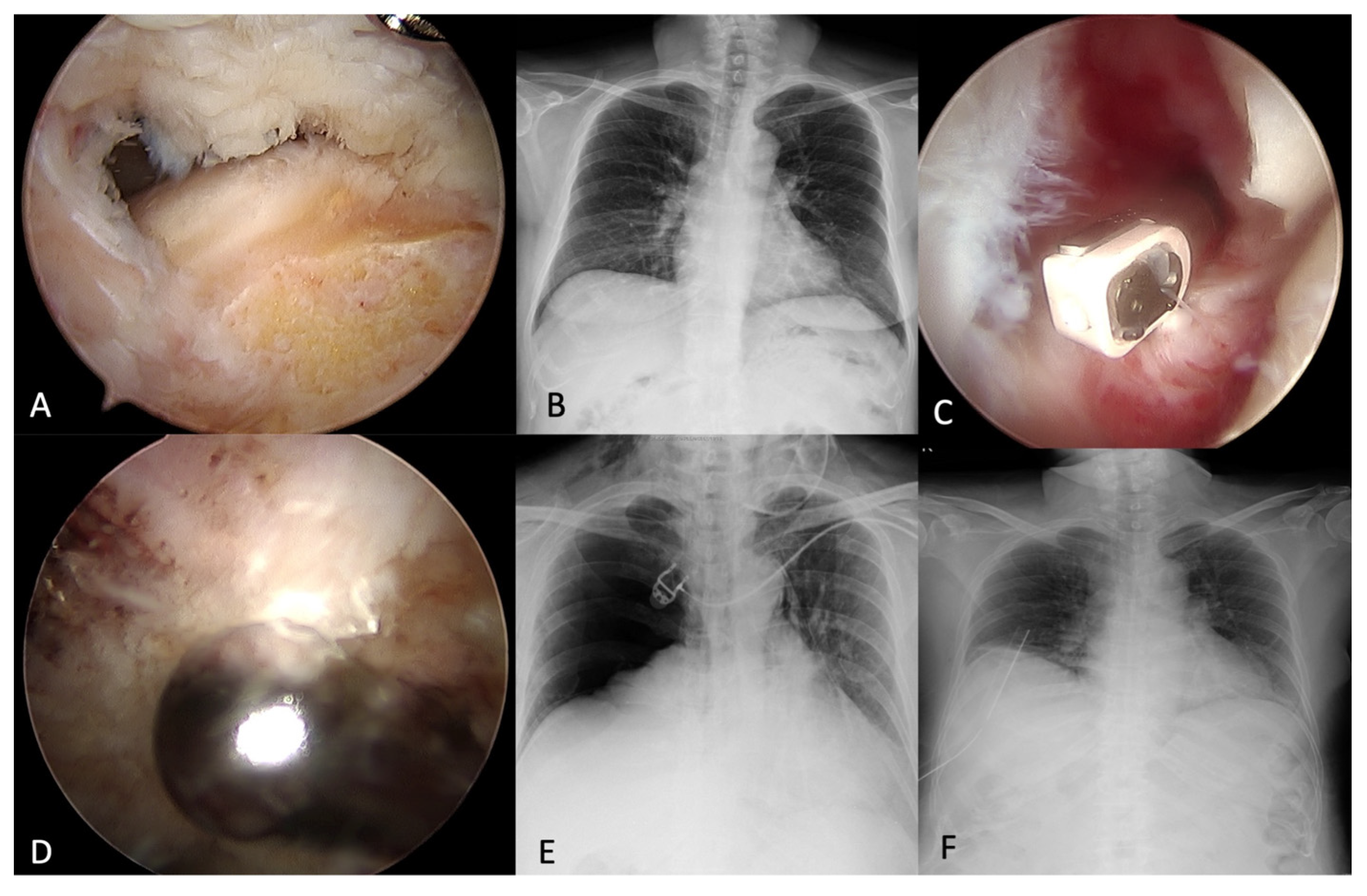
2.1. Case 1
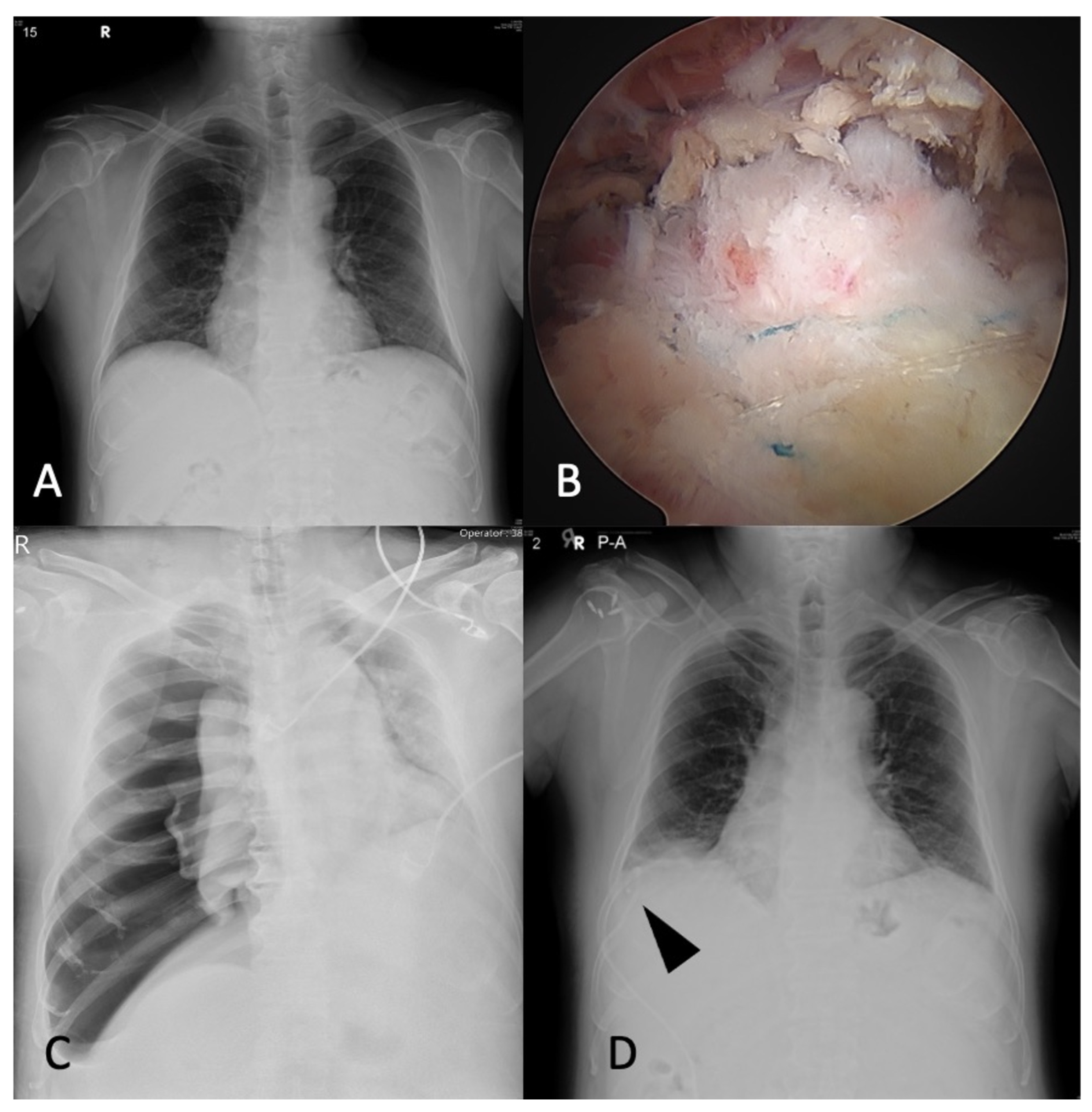
2.2. Case 2
2.3. Case 3
3. Discussion
- 1
- Patient positioning
- 2
- Interscalene nerve block
- 3
- Surgical time
- 4
- The size of rotator cuff tear
- 5
- Irrigation system
Management
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Horner, N.S.; de Sa, D.; Heaven, S.; Simunovic, N.; Bedi, A.; Athwal, G.S.; Ayeni, O.R. Indications and outcomes of shoulder arthroscopy after shoulder arthroplasty. J. Shoulder Elbow Surg. 2016, 25, 510–518. [Google Scholar] [CrossRef] [PubMed]
- Sugaya, H.; Kon, Y.; Tsuchiya, A. Arthroscopic repair of glenoid fractures using suture anchors. Arthroscopy 2005, 21, 635. [Google Scholar] [CrossRef] [PubMed]
- Moen, T.C.; Rudolph, G.H.; Caswell, K.; Espinoza, C.; Burkhead, W.Z.J.; Krishnan, S.G. Complications of Shoulder Arthroscopy. JAAOS J. Am. Acad. Orthop. Surg. 2014, 22, 410–419. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Eichinger, J.K.; Hartshorn, T.; Zhou, H.; Matzkin, E.G.; Warner, J.P. A comparison of the lateral decubitus and beach-chair positions for shoulder surgery: Advantages and complications. J. Am. Acad. Orthop. Surg. 2015, 23, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Collin, P.; McCoubrey, G.; Lädermann, A. Posterosuperior rotator cuff repair by an independent double-row technique. Technical note and radiological and clinical results. Orthop. Traumatol. Surg. Res. 2016, 102, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.C.; Shin, H.D.; Lee, W.Y. Repair Integrity and Functional Outcomes After Arthroscopic Suture-Bridge Rotator Cuff Repair. JBJS 2012, 94, e48. [Google Scholar] [CrossRef] [PubMed]
- Bamps, S.; Renson, D.; Nijs, S.; Sermo. Pneumothorax after Shoulder Arthroscopy: A Rare but Life-threatening Complication. J. Orthop. Case Rep. 2016, 6, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Cassone, M.A.; Kish, K.L.; Nester, J.R.; Hoffman, L.M. Case Report and Literature Review: Post-Arthroscopy Pneumothorax with Anterior Decompression. Clin. Pract. Cases Emerg. Med. 2020, 4, 580–583. [Google Scholar] [CrossRef]
- Tang, D.; Liu, Q.; Chen, C.; Zhu, W. Pneumothorax after shoulder arthroscopy: A case report and literature review. JSES Rev. Rep. Tech. 2021, 1, 194–197. [Google Scholar] [CrossRef]
- Dietzel, D.P.; Ciullo, J.V. Spontaneous pneumothorax after shoulder arthroscopy: A report of four cases. Arthroscopy 1996, 12, 99–102. [Google Scholar] [CrossRef]
- Bishop, J.Y.; Sprague, M.; Gelber, J.; Krol, M.; Rosenblatt, M.A.; Gladstone, J.; Flatow, E.L. Interscalene regional anesthesia for shoulder surgery. J. Bone Joint Surg. Am. 2005, 87, 974–979. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Lall, A.; Lai, E.; Gruson, K.I. Tension Pneumothorax After Ultrasound-Guided Interscalene Block and Shoulder Arthroscopy. Am. J. Orthop. 2015, 44, E407–E410. [Google Scholar] [PubMed]
- Bhatia, A.; Lai, J.; Chan, V.W.; Brull, R. Case report: Pneumothorax as a complication of the ultrasound-guided supraclavicular approach for brachial plexus block. Anesth. Analg. 2010, 111, 817–819. [Google Scholar] [CrossRef] [PubMed]
- Leander-Olsson, O.; Borglund-Hemph, A.; Jakobsson, J.G. Pneumothorax following shoulder arthroscopy under combined regional and general anaesthesia-A case report. Int. J. Surg. Case Rep. 2016, 24, 73–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shariyate, M.J.; Kachooei, A.R.; Ebrahimzadeh, M.H. Massive Emphysema and Pneumothorax Following Shoulder Arthroscopy under General Anaesthesia: A Case Report. Arch. Bone Jt. Surg. 2017, 5, 459–463. [Google Scholar] [PubMed]
- Lau, K.Y. Pneumomediastinum caused by subcutaneous emphysema in the shoulder. A rare complication of arthroscopy. Chest 1993, 103, 1606–1607. [Google Scholar] [CrossRef] [PubMed]
- Sahn, S.A.; Heffner, J.E. Spontaneous Pneumothorax. N. Engl. J. Med. 2000, 342, 868–874. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacDuff, A.; Arnold, A.; Harvey, J. Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline 2010. Thorax 2010, 65 (Suppl. 2), ii18–ii31. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, W.-C.; Kuo, L.-T.; Yu, P.-A.; Yang, C.-P.; Sheu, H.; Tang, H.-C.; Chan, Y.-S.; Chen, A.C.-Y.; Hsu, K.-Y.; Weng, C.-J.; et al. Pneumothorax, an Uncommon but Devastating Complication Following Shoulder Arthroscopy: Case Reports. Medicina 2022, 58, 1603. https://doi.org/10.3390/medicina58111603
Sun W-C, Kuo L-T, Yu P-A, Yang C-P, Sheu H, Tang H-C, Chan Y-S, Chen AC-Y, Hsu K-Y, Weng C-J, et al. Pneumothorax, an Uncommon but Devastating Complication Following Shoulder Arthroscopy: Case Reports. Medicina. 2022; 58(11):1603. https://doi.org/10.3390/medicina58111603
Chicago/Turabian StyleSun, Wei-Chien, Liang-Tseng Kuo, Pei-An Yu, Cheng-Pang Yang, Huan Sheu, Hao-Che Tang, Yi-Sheng Chan, Alvin Chao-Yu Chen, Kuo-Yao Hsu, Chun-Jui Weng, and et al. 2022. "Pneumothorax, an Uncommon but Devastating Complication Following Shoulder Arthroscopy: Case Reports" Medicina 58, no. 11: 1603. https://doi.org/10.3390/medicina58111603
APA StyleSun, W. -C., Kuo, L. -T., Yu, P. -A., Yang, C. -P., Sheu, H., Tang, H. -C., Chan, Y. -S., Chen, A. C. -Y., Hsu, K. -Y., Weng, C. -J., Cheng, Y. -H., & Chiu, C. -H. (2022). Pneumothorax, an Uncommon but Devastating Complication Following Shoulder Arthroscopy: Case Reports. Medicina, 58(11), 1603. https://doi.org/10.3390/medicina58111603







