Robotic-Assisted Total Knee Arthroplasty Utilizing NAVIO, CORI Imageless Systems and Manual TKA Accurately Restore Femoral Rotational Alignment and Yield Satisfactory Clinical Outcomes: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
- Participants-inclusion and exclusion criteria
- Study procedures and data collection
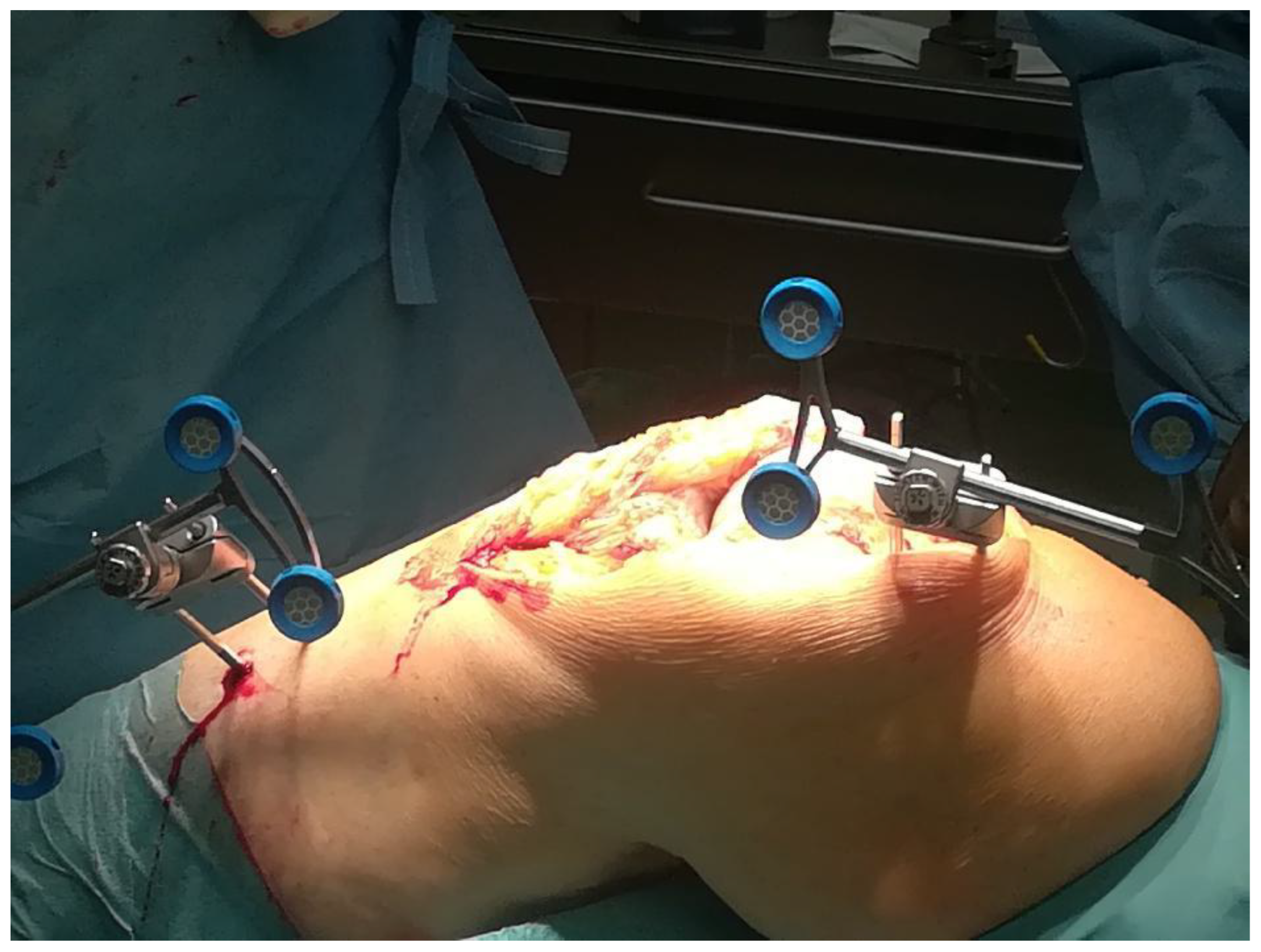
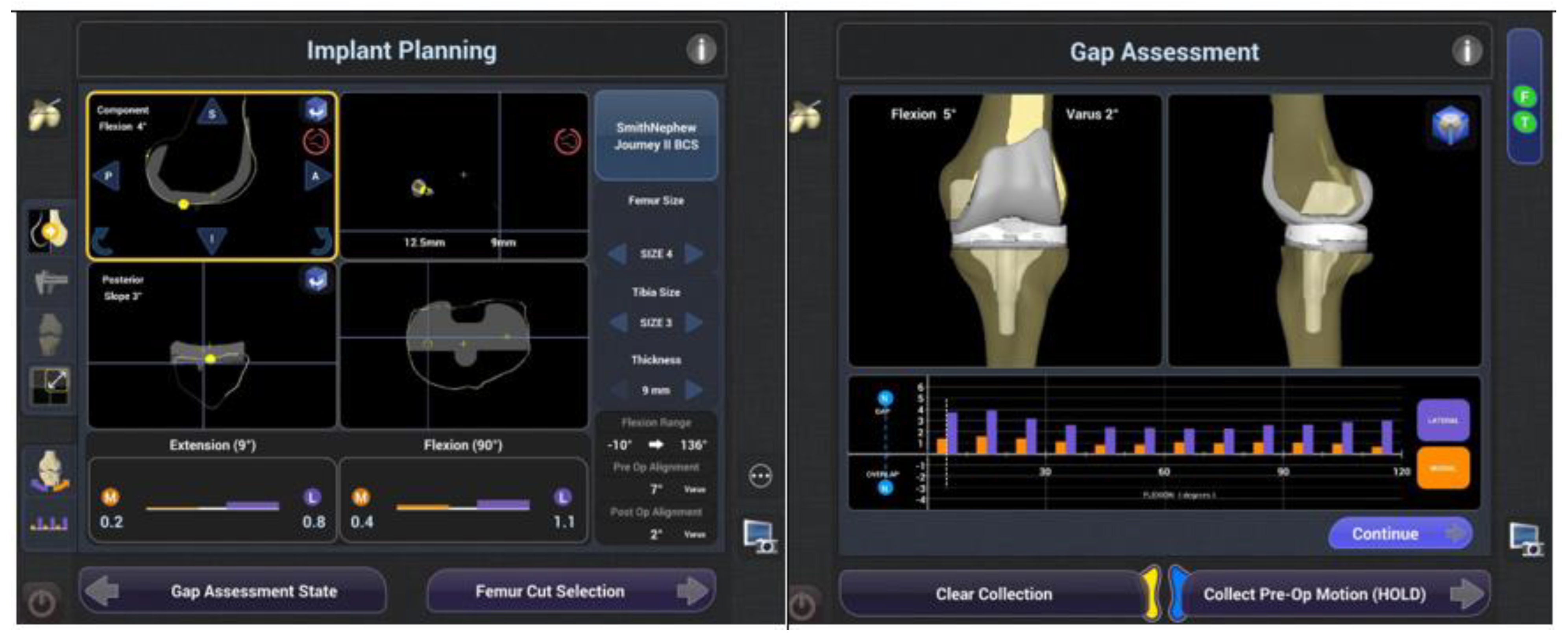
- Surgical technique
- Postoperative care
- Clinical assessment
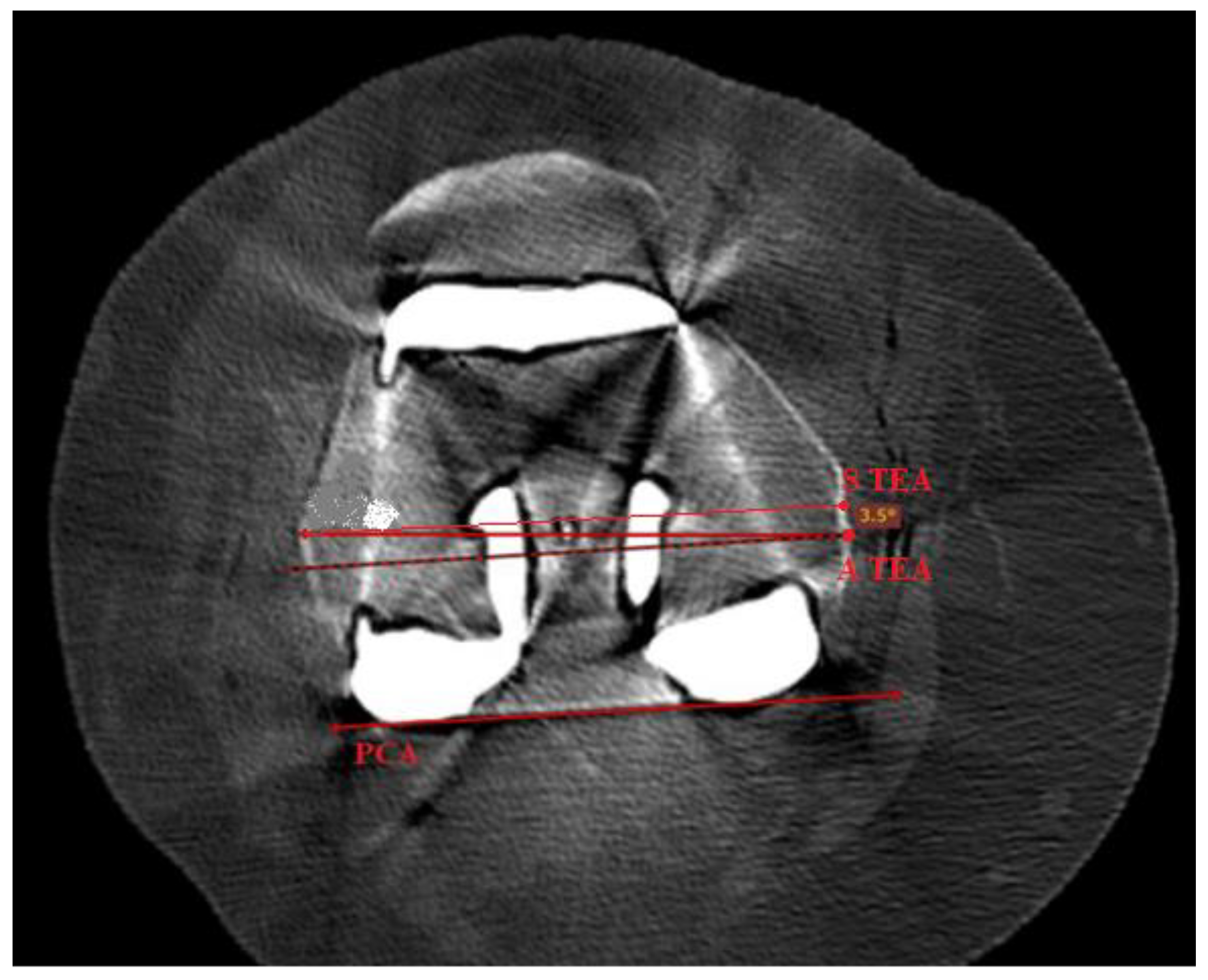
- Radiographic assessment
- Statistical analysis
3. Results
3.1. Demographics
| Characteristics | mTKA (n = 68) | NAVIO (n = 76) | CORI (n = 71) | p Value |
|---|---|---|---|---|
| Age at the surgery (SD) | 65 (±8.2) | 66 (±7.5) | 69 (±6.8) | 0.539 |
| Sex Female/ Male (%) | 35 (54%)/30 (46%) | 42 (64%)/22 (36%) | 35 (51%)/34 (49%) | 0.922 |
| BMI, kg/m2, mean (SD) | 26.0 (±3.17) | 25.8 (±3.3) | 25.5 (±2.9) | 0.996 |
| Site of surgery Left/Right (%) | 31 (48%)/34 (52%) | 34 (52%)/32 (48%) | 23 (33%)/46 (67%) | 0.478 |
| Epidural anaesthesia (%) | 100% | 100% | 100% | n.a. |
| Operative time, min, mean (SD) | 66.5 (±9) | 105 (±8.17) | 111 (±11.5) | 0.003 |
| Blood loss (Hb level difference before and after surgery), g/dL | 2.52 (±1.01) | 1.74 (±1.26) | 1.51 (±1.12) | 0.042 |
| Hospital stay, days, mean (SD) | 4.2 (±1.4) | 4.4 (±1.0) | 4.8 (±1.26) | 0.447 |
| Postoperative complications at 1 year, number (%) | 0 (0%) | 0 (0%) | 0 (0%) | - |
| Revision rate at 1 year, number (%) | 0 (0%) | 0 (0%) | 0 (0%) | - |
| mTKA (n = 68) | NAVIO (n = 76) | CORI (n = 71) | p Value | |
|---|---|---|---|---|
| Comorbidity, n (%) | 57 (83.8%) | 49 (64.5%) | 51 (71.8%) | 0.9733 |
| Hypertension | 16 (23.5%) | 18 (23.7%) | 19 (26.8%) | 0.0782 |
| Arrhythmias | 5 (7.4%) | 2 (2.7%) | 0 | 0.8793 |
| Hypothyroidism | 5 (7.4%) | 3 (3.9%) | 6 (8.5%) | 0.0812 |
| Diabetes mellitus | 13 (19.1 %) | 16 (21.1%) | 11 (15.5%) | 0.0765 |
| Asthma | 3 (4.4%) | 1 (1.3%) | 0 | 0.5210 |
| Depression | 3 (4.4%) | 0 | 1 (1.4%) | 0.9854 |
| Systemic lupus erythematosus | 1 (1.5%) | 0 | 2 (2.8%) | 0.9982 |
| Rheumatoid arthritis | 3 (4.4%) | 2 (2.7%) | 5 (7%) | 0.3965 |
| Gout | 7 (10.3%) | 4 (5.3%) | 5 (7%) | 0.2135 |
| Psoriatic arthritis | 1 (1.5%) | 3 (3.9%) | 2 (2.8%) | 0.0754 |
3.2. Functional Outcomes
3.3. Radiographic Evaluation of Femoral Component Rotational Alignment Postoperatively
| Characters | Intervention Group | Intervention Group | Kruskal-Wallis Test | Dunn’s Multiple Comparisons Test | |
|---|---|---|---|---|---|
| H | p | ||||
| KOOS | mTKA | NAVIO | 82.232 | 0.0498 | *** |
| mTKA | CORI | 24.672 | 0.0382 | ** | |
| NAVIO | CORI | 2.976 | 0.6459 | n.s. | |
| VAS | mTKA | NAVIO | 34.567 | 0.1852 | n.s. |
| mTKA | CORI | 47.160 | 0.6498 | n.s. | |
| NAVIO | CORI | 64.567 | 0.0783 | n.s. | |
| ROM in extension | mTKA | NAVIO | 48.322 | 0.0971 | n.s. |
| mTKA | CORI | 22.548 | 0.9447 | n.s. | |
| NAVIO | CORI | 36.901 | 0.7115 | n.s. | |
| ROM in flexion | mTKA | NAVIO | 35.230 | 0.3491 | n.s. |
| mTKA | CORI | 22.375 | 0.6948 | n.s. | |
| NAVIO | CORI | 3.578 | 0.0998 | n.s. | |
| Femoral Component Rotational Alignment | mTKA | NAVIO | 22.497 | 0.0376 | ** |
| mTKA | CORI | 48.345 | 0.0011 | *** | |
| NAVIO | CORI | 36.522 | 0.0935 | n.s. | |
3.4. Complications
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grässel, S.; Muschter, D. Recent advances in the treatment of osteoarthritis. F1000Research 2020, 9, 325. [Google Scholar] [CrossRef] [PubMed]
- Scaturro, D.; Vitagliani, F.; Terrana, P.; Cuntrera, D.; Falco, V.; Tomasello, S.; Mauro, G.L. Intra-Articular Hybrid Hyaluronic Acid Injection Treatment in Overweight Patients with Knee Osteoarthritis: A Single-Center, Open-Label, Prospective Study. Appl. Sci. 2021, 11, 8711. [Google Scholar] [CrossRef]
- Belluzzi, E.; Olivotto, E.; Toso, G.; Cigolotti, A.; Pozzuoli, A.; Biz, C.; Trisolino, G.; Ruggieri, P.; Grigolo, B.; Ramonda, R.; et al. Conditioned media from human osteoarthritic synovium induces inflammation in a synoviocyte cell line. Connect. Tissue Res. 2019, 60, 136–145. [Google Scholar] [CrossRef] [PubMed]
- Kayani, B.; Haddad, F.S. Robotic total knee arthroplasty: Clinical outcomes and directions for future research. Bone Jt. Res. 2019, 8, 438–442. [Google Scholar] [CrossRef]
- Migliore, A.; Gigliucci, G.; Alekseeva, L.; Avasthi, S.; Bannuru, R.R.; Chevalier, X.; Conrozier, T.; Crimaldi, S.; Damjanov, N.; de Campos, G.C.; et al. Treat-to-target strategy for knee osteoarthritis. International technical expert panel consensus and good clinical practice statements. Ther. Adv. Musculoskelet. Dis. 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Carter, J.; Springer, B.; Curtin, B.M. Early complications of revision total knee arthroplasty in morbidly obese patients. Eur. J. Orthop. Surg. Traumatol. 2019, 29, 1101–1104. [Google Scholar] [CrossRef]
- Mathis, D.T.; Hirschmann, M.T. Why do knees after total knee arthroplasty fail in different parts of the world? J. Orthop. 2020, 23, 52–59. [Google Scholar] [CrossRef]
- Delanois, R.E.; Mistry, J.B.; Gwam, C.U.; Mohamed, N.S.; Choksi, U.S.; Mont, M.A. Current Epidemiology of Revision Total Knee Arthroplasty in the United States. J. Arthroplast. 2017, 32, 2663–2668. [Google Scholar] [CrossRef]
- Siqueira, M.B.P.; Higuera, C.A.; Barsoum, W.K.; Klika, A.K. Modes of Failure of Total Knee Arthroplasty: Registries and Realities. J. Knee Surg. 2015, 28, 127–138. [Google Scholar] [CrossRef]
- Hofmann, A.A.; McCandless, J. Imageless Computer Navigation in Total Knee Arthroplasty. Available online: https://musculoskeletalkey.com/imageless-computer-navigation-in-total-knee-arthroplasty-the-simpler-wave-of-the-future/ (accessed on 16 August 2022).
- Bell, S.W.; Anthony, I.; Jones, B.; MacLean, A.; Rowe, P.; Blyth, M. Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: Data from a prospective, randomized controlled study. J. Bone Jt. Surg. Am. 2016, 98, 627–635. [Google Scholar] [CrossRef]
- Hampp, E.L.; Chughtai, M.; Scholl, L.Y.; Sodhi, N.; Bhowmik-Stoker, M.; Jacofsky, D.J.; Mont, M.A. Robotic-Arm Assisted Total Knee Arthroplasty Demonstrated Greater Accuracy and Precision to Plan Compared with Manual Techniques. J. Knee Surg. 2019, 32, 239–250. [Google Scholar] [CrossRef] [PubMed]
- Hampp, E.; Sodhi, N.; Scholl, L.; Deren, M.; Yenna, Z.; Westrich, G.; Mont, M. Less Iatrogenic Soft Tissue Damage Utilizing Robotic Assisted Total Knee Arthroplasty when Compared with a Manual Approach: A Blinded Assessment. Bone Jt. Res. 2019, 3, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Kayani, B.; Konan, S.; Tahmassebi, J.; Pietrzak, J.R.T.; Haddad, F.S. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: A prospective cohort study. Bone Jt. J. 2018, 100, 930–937. [Google Scholar] [CrossRef] [PubMed]
- Kayani, B.; Konan, S.; Tahmassebi, J.; Rowan, F.E.; Haddad, F.S. An assessment of early functional rehabilitation and hospital dis-charge in conventional versus robotic-arm assisted unicompartmental knee arthroplasty: A prospective cohort study. Bone Jt. J. 2019, 101, 24–33. [Google Scholar] [CrossRef]
- Blyth, M.J.G.; Anthony, I.; Rowe, P.; Banger, M.S.; MacLean, A.; Jones, B. Robotic arm-assisted versus conventional unicompartmental knee arthroplasty: Exploratory secondary analysis of a randomised controlled trial. Bone Jt. Res. 2017, 6, 631–639. [Google Scholar] [CrossRef]
- Canetti, R.; Batailler, C.; Bankhead, C.; Neyret, P.; Servien, E.; Lustig, S. Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: A comparative study. Arch. Orthop. Trauma Surg. 2018, 138, 1765–1771. [Google Scholar] [CrossRef]
- Iturriaga, C.; Salem, H.S.; Ehiorobo, J.O.; Sodhi, N.; Mont, M.A. Robotic-Assisted Versus Manual Unicompartmental Knee Arthro-plasty: A Systematic Review. Surg Technol. Int. 2020, 37, 275–279. [Google Scholar]
- Sun, Y.; Liu, W.; Hou, J.; Hu, X.; Zhang, W. Does robotic-assisted unicompartmental knee arthroplasty have lower complication and revision rates than the conventional procedure? A systematic review and meta-analysis. BMJ Open 2021, 11, e044778. [Google Scholar] [CrossRef]
- Haffar, A.; Krueger, C.A.; Goh, G.S.; Lonner, J.H. UKA with a handheld robotic device results in greater surgeon physiological stress than conventional instrumentation. Knee Surg. Sport. Traumatol. Arthrosc. 2022, 1–9, ahead of print. [Google Scholar] [CrossRef]
- Motesharei, A.; Rowe, P.; Blyth, M.; Jones, B.; Maclean, A. A comparison of gait one year post operation in an RCT of robotic UKA versus traditional Oxford UKA. Gait Posture 2018, 62, 41–45. [Google Scholar] [CrossRef]
- Clement, N.D.; Al-Zibari, M.; Afzal, I.; Deehan, D.J.; Kader, D. A systematic review of imageless hand-held robotic-assisted knee arthroplasty: Learning curve, accuracy, functional outcome and survivorship. EFORT Open Rev. 2020, 5, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.smith-nephew.com (accessed on 15 August 2022).
- Berger, R.A.; E Rubash, H.; Seel, M.J.; Thompson, W.H.; Crossett, L.S. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin. Orthop. Relat. Res. 1993, 286, 40–47. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Biz, C.; Maso, G.; Gambato, M.; Belluzzi, E.; Pozzuoli, A.; Favero, M.; Vigo, M.; Ruggieri, P. Challenging Surgical Treatment of Displaced Articular Tibial Plateau Fractures: Do Early Knee Radiographic Features Have a Predictive Value of the Mid-Term Clinical Functional Outcomes? Orthop. Surg. 2019, 11, 1149–1162. [Google Scholar] [CrossRef] [PubMed]
- Ren, Y.; Cao, S.; Wu, J.; Weng, X.; Feng, B. Efficacy and reliability of active robotic-assisted total knee arthroplasty compared with conventional total knee arthroplasty: A systematic review and meta-analysis. Postgrad. Med. J. 2019, 95, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Ndou, W.S.; Ng, N.; Gaston, P.; Simpson, P.M.; Macpherson, G.J.; Patton, J.T.; Clement, N.D. Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: A systematic review and meta-analysis. Knee Surg. Sport. Traumatol. Arthrosc. 2021, 30, 2677–2695. [Google Scholar] [CrossRef]
- Kim, Y.-H.; Yoon, S.-H.; Park, J.-W. Does Robotic-assisted TKA Result in Better Outcome Scores or Long-Term Survivorship Than Conventional TKA? A Randomized, Controlled Trial. Clin. Orthop. Relat. Res. 2020, 478, 266–275. [Google Scholar] [CrossRef]
- Batailler, C.; White, N.; Ranaldi, F.M.; Neyret, P.; Servien, E.; Lustig, S. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg. Sport. Traumatol. Arthrosc. 2019, 27, 1232–1240. [Google Scholar] [CrossRef]
- Held, M.B.; Gazgalis, A.; Neuwirth, A.L.; Shah, R.P.; Cooper, H.J.; Geller, J.A. Imageless robotic-assisted total knee arthroplasty leads to similar 24-month WOMAC scores as compared to conventional total knee arthroplasty: A retrospective cohort study. Knee Surg. Sport. Traumatol. Arthrosc. 2022, 30, 2631–2638. [Google Scholar] [CrossRef]
- Savov, P.; Tuecking, L.-R.; Windhagen, H.; Ehmig, J.; Ettinger, M. Imageless robotic handpiece-assisted total knee arthroplasty: A learning curve analysis of surgical time and alignment accuracy. Arch. Orthop. Trauma Surg. 2021, 141, 2119–2128. [Google Scholar] [CrossRef]
- Paolo, D.B.; Michele, M.B.; Stefano, M.; Vanni, C.; Araldo, C. Comparison between standard technique and image-free robotic technique in medial unicompartmental knee arthroplasty. Preliminary data. Acta Biomed. 2019, 90, 104–108. [Google Scholar] [CrossRef]
- Robertson, E.L.; Hengherr, M.; Amsler, F.; Hirschmann, M.T.; Mathis, D.T. A comparison of femoral component rotation after total knee arthroplasty in Kanekasu radiographs, axial CT slices and 3D reconstructed images. Skelet. Radiol. 2021, 50, 1389–1397. [Google Scholar] [CrossRef] [PubMed]
- Newman, C.R.; Walter, W.L.; Talbot, S. Femoral rotational asymmetry is a common anatomical variant. Clin. Anat. 2018, 31, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Twiggs, J.G.; Dickison, D.M.; Kolos, E.C.; Wilcox, C.E.; Roe, J.P.; Fritsch, B.A.; McMahon, S.J.; Miles, B.P.; Ruys, A.J. Patient Variation Limits Use of Fixed References for Femoral Rotation Component Alignment in Total Knee Arthroplasty. J. Arthroplast. 2018, 33, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Fitz, D.W.; Johnson, D.J.; Hartwell, M.J.; Sullivan, R.; Keller, T.J.; Manning, D.W. Relationship of the Posterior Condylar Line and the Transepicondylar Axis: A CT-Based Evaluation. J. Knee Surg. 2020, 33, 673–677. [Google Scholar] [CrossRef]
- Bell, C.; Grau, L.; Orozco, F.; Ponzio, D.; Post, Z.; Czymek, M.; Ong, A. The successful implementation of the Navio robotic technology required 29 cases. J. Robot. Surg. 2022, 16, 495–499. [Google Scholar] [CrossRef]
- Thiengwittayaporn, S.; Uthaitas, P.; Senwiruch, C.; Hongku, N.; Tunyasuwanakul, R. Imageless robotic-assisted total knee arthroplasty accurately restores the radiological alignment with a short learning curve: A randomized controlled trial. Int. Orthop. 2021, 45, 2851–2858. [Google Scholar] [CrossRef] [PubMed]
- Onggo, J.R.; Onggo, J.D.; De Steiger, R.; Hau, R. Robotic-assisted total knee arthroplasty is comparable to conventional total knee arthroplasty: A meta-analysis and systematic review. Arch. Orthop. Trauma Surg. 2020, 140, 1533–1549. [Google Scholar] [CrossRef]
- Song, E.-K.; Seon, J.-K.; Yim, J.-H.; Netravali, N.A.; Bargar, W.L. Robotic-assisted TKA Reduces Postoperative Alignment Outliers and Improves Gap Balance Compared to Conventional TKA. Clin. Orthop. Relat. Res. 2013, 471, 118–126. [Google Scholar] [CrossRef]
- Peersman, G.; Laskin, R.; Davis, J.; Peterson, M.G.E.; Richart, T. Prolonged Operative Time Correlates with Increased Infection Rate After Total Knee Arthroplasty. HSS J. 2006, 2, 70–72. [Google Scholar] [CrossRef]
- Ali, M.; Phillips, D.; Kamson, A.; Nivar, I.; Dahl, R.; Hallock, R. Learning Curve of Robotic-Assisted Total Knee Arthroplasty for Non-Fellowship-Trained Orthopedic Surgeons. Arthroplast. Today 2022, 13, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Neuprez, A.; Neuprez, A.H.; Kaux, J.-F.; Kurth, W.; Daniel, C.; Thirion, T.; Huskin, J.-P.; Gillet, P.; Bruyère, O.; Reginster, J.-Y. Total joint replacement improves pain, functional quality of life, and health utilities in patients with late-stage knee and hip osteoarthritis for up to 5 years. Clin. Rheumatol. 2020, 39, 861–871. [Google Scholar] [CrossRef]
- Nielsen, L.M.; Kirkegaard, H.; Østergaard, L.G.; Bovbjerg, K.; Breinholt, K.; Maribo, T. Comparison of self-reported and performance-based measures of functional ability in elderly patients in an emergency department: Implications for selection of clinical outcome measures. BMC Geriatr. 2016, 16, 199. [Google Scholar] [CrossRef] [PubMed]
- Brown, N.M.; Sheth, N.P.; Davis, K.; Berend, M.E.; Lombardi, A.V.; Berend, K.R.; Della Valle, C.J. Total Knee Arthroplasty Has Higher Postoperative Morbidity Than Unicompartmental Knee Arthroplasty: A Multicenter Analysis. J. Arthroplast. 2012, 27 (Suppl. 8), 86–90. [Google Scholar] [CrossRef]
- Lyons, M.C.; MacDonald, S.J.; Somerville, L.E.; Naudie, D.D.; McCalden, R.W. Unicompartmental Versus Total Knee Arthroplasty Database Analysis: Is There a Winner? Clin. Orthop. Relat. Res. 2012, 470, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Kremers, H.M.; Kremers, W.K.; Berry, D.J.; Lewallen, D.G. Social and Behavioral Factors in Total Knee and Hip Arthroplasty. J. Arthroplast. 2015, 30, 1852–1854. [Google Scholar] [CrossRef]
- Siviero, P.; Marseglia, A.; Biz, C.; Rovini, A.; Ruggieri, P.; Nardacchione, R.; Maggi, S. Quality of life outcomes in patients undergoing knee replacement surgery: Longitudinal findings from the QPro-Gin study. BMC Musculoskelet. Disord. 2020, 21, 436. [Google Scholar] [CrossRef]


| Variable | Time | Ra-TKA NAVIO n = 76 | Ra-TKA CORI n = 71 | Conventional TKA n = 68 | p Value |
|---|---|---|---|---|---|
| KOOS | Preoperative results | 30.79 ± 11.46 | 28.18 ± 8.45 | 30.3 ± 10.00 | 0.16174 |
| Postoperative results | 87.05 ± 7.74 | 85.59 ± 8.03 | 81.76 ± 8.95 | 0.0001 | |
| ROM in extension | Preoperative results | 6.5 ± 5.5 | 5.7 ± 3.2 | 6.2 ± 5.0 | 0.0902 |
| Postoperative results | 1.5 ± 3.8 | 1.8 ± 1.7 | 1.5 ± 1.3 | 0.9867 | |
| ROM in flexion | Preoperative results | 111.2 ± 10.4 | 113.1 ± 16.7 | 114.8 ± 11.3 | 0.5498 |
| Postoperative results | 126.3 ± 14.2 | 132.1 ± 9.0 | 124.3 ± 12.6 | 0.0621 | |
| VAS | Preoperative results | 7.4074 ± 1.3531 | 8.1152 ± 1.1314 | 8.23 ± 1.256 | 0.0062 |
| Postoperative results | 2 ± 1.3598 | 2.39 ± 1.012 | 2.12 ± 1.23 | 0.1098 | |
| Femoral Component Rotational Alignment | Postoperative results | 1.48 ± 1.117 | 1.33 ± 1.012 | 3.15 ± 1.2163 | 0.0013 |
| Intervention Group | Variable | Preoperative Values | Postoperative Values | p Value |
|---|---|---|---|---|
| Robotic-assisted TKA NAVIO n = 76 | KOOS | 30.79 ± 11.46 | 87.05 ± 7.74 | 0.0109 |
| ROM in extension | 6.5 ± 5.5 | 1.5 ± 3.8 | 0.0042 | |
| ROM in flexion | 111.2 ± 10.4 | 126.3 ± 14.2 | n.a. | |
| VAS | 7.4074 ± 1.3531 | 2 ± 1.3598 | 0 | |
| Femoral component rotational alignment | - | 1.48 ± 1.117 | 0.0006 | |
| Robotic-assisted TKA CORI n = 71 | KOOS | 28.18 ± 8.45 | 85.59 ± 8.03 | 0.0048 |
| ROM in extension | 5.7 ± 3.2 | 1.8 ± 1.7 | 0.0013 | |
| ROM in flexion | 113.1 ± 16.7 | 132.1 ± 9.0 | 0.115 | |
| VAS | 8.1152 ± 1.1314 | 2.39 ± 1.012 | 0.0003 | |
| Femoral component rotational alignment | - | 1.33 ± 1.012 | 0.0127 | |
| Conventional TKA n = 68 | KOOS | 30.3 ± 10.00 | 81.76 ± 8.95 | 0 |
| ROM in extension | 6.2 ± 5.0 | 1.5 ± 1.3 | 0 | |
| ROM in flexion | 114.8 ± 11.3 | 124.3 ± 12.6 | 0.3117 | |
| VAS | 8.23 ± 1.256 | 2.12 ± 1.23 | 0.0491 | |
| Femoral component rotational alignment | - | 3.15 ± 1.2163 | 0.0048 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adamska, O.; Modzelewski, K.; Szymczak, J.; Świderek, J.; Maciąg, B.; Czuchaj, P.; Poniatowska, M.; Wnuk, A. Robotic-Assisted Total Knee Arthroplasty Utilizing NAVIO, CORI Imageless Systems and Manual TKA Accurately Restore Femoral Rotational Alignment and Yield Satisfactory Clinical Outcomes: A Randomized Controlled Trial. Medicina 2023, 59, 236. https://doi.org/10.3390/medicina59020236
Adamska O, Modzelewski K, Szymczak J, Świderek J, Maciąg B, Czuchaj P, Poniatowska M, Wnuk A. Robotic-Assisted Total Knee Arthroplasty Utilizing NAVIO, CORI Imageless Systems and Manual TKA Accurately Restore Femoral Rotational Alignment and Yield Satisfactory Clinical Outcomes: A Randomized Controlled Trial. Medicina. 2023; 59(2):236. https://doi.org/10.3390/medicina59020236
Chicago/Turabian StyleAdamska, Olga, Krzysztof Modzelewski, Jakub Szymczak, Jakub Świderek, Bartosz Maciąg, Paweł Czuchaj, Małgorzata Poniatowska, and Artur Wnuk. 2023. "Robotic-Assisted Total Knee Arthroplasty Utilizing NAVIO, CORI Imageless Systems and Manual TKA Accurately Restore Femoral Rotational Alignment and Yield Satisfactory Clinical Outcomes: A Randomized Controlled Trial" Medicina 59, no. 2: 236. https://doi.org/10.3390/medicina59020236
APA StyleAdamska, O., Modzelewski, K., Szymczak, J., Świderek, J., Maciąg, B., Czuchaj, P., Poniatowska, M., & Wnuk, A. (2023). Robotic-Assisted Total Knee Arthroplasty Utilizing NAVIO, CORI Imageless Systems and Manual TKA Accurately Restore Femoral Rotational Alignment and Yield Satisfactory Clinical Outcomes: A Randomized Controlled Trial. Medicina, 59(2), 236. https://doi.org/10.3390/medicina59020236






