Mass Spectrometry-Based Proteomic Profiling of Thrombotic Material Obtained by Endovascular Thrombectomy in Patients with Ischemic Stroke
Abstract
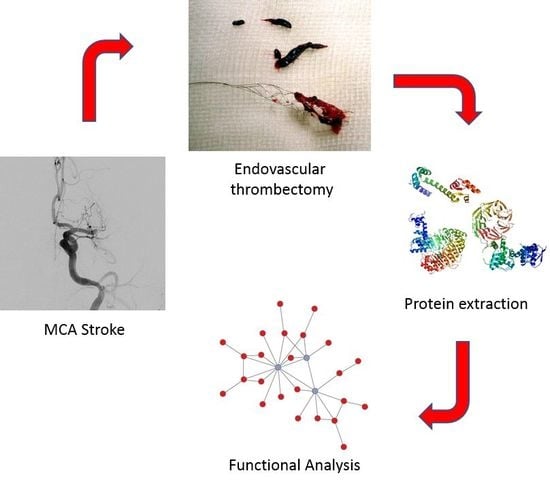
:1. Introduction
2. Results
2.1. Proteme Exploration of Human Thrombus by Mass Spectrometry
2.2. Functional Mapping of Human Thrombotic Proteome Isolated by Endovascular Thrombectomy
2.3. Protein Interaction Networks for Common Proteins Present in the Thrombus
3. Discussion
Study Limitations
4. Materials and Methods
4.1. Ethics Considerations
4.2. Endovascular Thrombectomy
4.3. Periprocedural Work-Up
4.4. Processing of Thrombus Material
4.5. Sample Preparation for Proteomic Analysis
4.6. Protein Analysis by LC-MS/MS
4.7. Peptide Identification
4.8. Bioinformatic Analysis
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Mukherjee, D.; Patil, C.G. Epidemiology and the global burden of Stroke. World Neurosurg. 2011, 76, S85–S90. [Google Scholar] [CrossRef] [PubMed]
- Adams, H.P., Jr.; Bendixen, B.H.; Kappelle, L.J.; Biller, J.; Love, B.B.; Gordon, D.L.; Marsh, E.E. Classification of subtype of acute ischemic Stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993, 24, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Ionita, C.C.; Xavier, A.R.; Kirmani, J.F.; Dash, S.; Divani, A.A.; Qureshi, A.I. What proportion of Stroke is not explained by classic risk factors? Prev. Cardiol. 2005, 8, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Jickling, G.C.; Sharp, F.R. Biomarker panels in ischemic Stroke. Stroke 2015, 46, 915–920. [Google Scholar] [CrossRef] [PubMed]
- Liumbruno, G.M.; Franchini, M. Proteomic analysis of venous thromboembolism: An update. Expert Rev. Proteom. 2013, 10, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Berkhemer, O.A.; Fransen, P.S.; Beumer, D.; van den Berg, L.A.; Lingsma, H.F.; Yoo, A.J.; Schonewille, W.J.; Vos, J.A.; Nederkoorn, P.J.; Wermer, M.J.; et al. A randomized trial of intraarterial treatment for acute ischemic Stroke. N. Engl. J. Med. 2015, 372, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Campbell, B.C.; Mitchell, P.J.; Kleinig, T.J.; Dewey, H.M.; Churilov, L.; Yassi, N.; Yan, B.; Dowling, R.J.; Parsons, M.W.; Oxley, T.J.; et al. Endovascular therapy for ischemic Stroke with perfusion-imaging selection. N. Engl. J. Med. 2015, 372, 1009–1018. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Demchuk, A.M.; Menon, B.K.; Eesa, M.; Rempel, J.L.; Thornton, J.; Roy, D.; Jovin, T.G.; Willinsky, R.A.; Sapkota, B.L.; et al. Randomized assessment of rapid endovascular treatment of ischemic Stroke. N. Engl. J. Med. 2015, 372, 1019–1030. [Google Scholar] [CrossRef] [PubMed]
- Jovin, T.G.; Chamorro, A.; Cobo, E.; de Miquel, M.A.; Molina, C.A.; Rovira, A.; San Roman, L.; Serena, J.; Abilleira, S.; Ribo, M.; et al. Thrombectomy within 8 hours after symptom onset in ischemic Stroke. N. Engl. J. Med. 2015, 372, 2296–2306. [Google Scholar] [CrossRef] [PubMed]
- Saver, J.L.; Goyal, M.; Bonafe, A.; Diener, H.C.; Levy, E.I.; Pereira, V.M.; Albers, G.W.; Cognard, C.; Cohen, D.J.; Hacke, W.; et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in Stroke. N. Engl. J. Med. 2015, 372, 2285–2295. [Google Scholar] [CrossRef] [PubMed]
- Goyal, M.; Menon, B.K.; van Zwam, W.H.; Dippel, D.W.; Mitchell, P.J.; Demchuk, A.M.; Davalos, A.; Majoie, C.B.; van der Lugt, A.; de Miquel, M.A.; et al. Endovascular thrombectomy after large-vessel ischaemic Stroke: A meta-analysis of individual patient data from five randomised trials. Lancet 2016, 387, 1723–1731. [Google Scholar] [CrossRef]
- De Meyer, S.F.; Andersson, T.; Baxter, B.; Bendszus, M.; Brouwer, P.; Brinjikji, W.; Campbell, B.C.; Costalat, V.; Davalos, A.; Demchuk, A.; et al. Analyses of thrombi in acute ischemic Stroke: A consensus statement on current knowledge and future directions. Int. J. Stroke 2017, 12, 606–614. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Orgaz, S.; Moreno-Luna, R.; Lopez, J.A.; Gil-Dones, F.; Padial, L.R.; Moreu, J.; de la Cuesta, F.; Barderas, M.G. Proteomic characterization of human coronary thrombus in patients with ST-segment elevation acute myocardial infarction. J. Proteom. 2014, 109, 368–381. [Google Scholar] [CrossRef] [PubMed]
- Burkhart, J.M.; Vaudel, M.; Gambaryan, S.; Radau, S.; Walter, U.; Martens, L.; Geiger, J.; Sickmann, A.; Zahedi, R.P. The first comprehensive and quantitative analysis of human platelet protein composition allows the comparative analysis of structural and functional pathways. Blood 2012, 120, e73–e82. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Chae, S.; Park, J.; Bae, J.; Go, E.B.; Kim, S.J.; Kim, H.; Hwang, D.; Lee, S.W.; Lee, S.Y. Comprehensive Proteome Profiling of Platelet Identified a Protein Profile Predictive of Responses to an Antiplatelet Agent Sarpogrelate. Mol. Cell. Proteom. 2016, 15, 3461–3472. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Pinto, S.M.; Getnet, D.; Nirujogi, R.S.; Manda, S.S.; Chaerkady, R.; Madugundu, A.K.; Kelkar, D.S.; Isserlin, R.; Jain, S.; et al. A draft map of the human proteome. Nature 2014, 509, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Aebersold, R.; Mann, M. Mass-spectrometric exploration of proteome structure and function. Nature 2016, 537, 347–355. [Google Scholar] [CrossRef] [PubMed]
- Cuadrado, E.; Rosell, A.; Colome, N.; Hernandez-Guillamon, M.; Garcia-Berrocoso, T.; Ribo, M.; Alcazar, A.; Ortega-Aznar, A.; Salinas, M.; Canals, F.; et al. The proteome of human brain after ischemic Stroke. J. Neuropathol. Exp. Neurol. 2010, 69, 1105–1115. [Google Scholar] [CrossRef] [PubMed]
- Maestrini, I.; Ducroquet, A.; Moulin, S.; Leys, D.; Cordonnier, C.; Bordet, R. Blood biomarkers in the early stage of cerebral ischemia. Rev. Neurol. 2016, 172, 198–219. [Google Scholar] [CrossRef] [PubMed]
- Piccardi, B.; Giralt, D.; Bustamante, A.; Llombart, V.; Garcia-Berrocoso, T.; Inzitari, D.; Montaner, J. Blood markers of inflammation and endothelial dysfunction in cardioembolic Stroke: Systematic review and meta-analysis. Biomarkers 2017, 22, 200–209. [Google Scholar] [CrossRef] [PubMed]
- Prentice, R.L.; Paczesny, S.; Aragaki, A.; Amon, L.M.; Chen, L.; Pitteri, S.J.; McIntosh, M.; Wang, P.; Buson Busald, T.; Hsia, J.; et al. Novel proteins associated with risk for coronary heart disease or Stroke among postmenopausal women identified by in-depth plasma proteome profiling. Genome Med. 2010, 2, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lind, L.; Siegbahn, A.; Lindahl, B.; Stenemo, M.; Sundstrom, J.; Arnlov, J. Discovery of new risk markers for ischemic Stroke using a novel targeted proteomics chip. Stroke 2015, 46, 3340–3347. [Google Scholar] [CrossRef] [PubMed]
- Almekhlafi, M.A.; Hu, W.Y.; Hill, M.D.; Auer, R.N. Calcification and endothelialization of thrombi in acute Stroke. Ann. Neurol. 2008, 64, 344–348. [Google Scholar] [CrossRef] [PubMed]
- Boeckh-Behrens, T.; Kleine, J.F.; Zimmer, C.; Neff, F.; Scheipl, F.; Pelisek, J.; Schirmer, L.; Nguyen, K.; Karatas, D.; Poppert, H. Thrombus histology suggests cardioembolic cause in cryptogenic Stroke. Stroke 2016, 47, 1864–1871. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, T.; Hayakawa, M.; Funatsu, N.; Yamagami, H.; Satow, T.; Takahashi, J.C.; Nagatsuka, K.; Ishibashi-Ueda, H.; Kira, J.I.; Toyoda, K. Histopathologic analysis of retrieved thrombi associated with successful reperfusion after acute Stroke thrombectomy. Stroke 2016, 47, 3035–3037. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.K.; Yoon, W.; Kim, T.S.; Kim, H.S.; Heo, T.W.; Park, M.S. Histologic analysis of retrieved clots in acute ischemic Stroke: Correlation with Stroke etiology and gradient-echo MRI. Am. J. Neuroradiol. 2015, 36, 1756–1762. [Google Scholar] [CrossRef] [PubMed]
- Niesten, J.M.; van der Schaaf, I.C.; van Dam, L.; Vink, A.; Vos, J.A.; Schonewille, W.J.; de Bruin, P.C.; Mali, W.P.; Velthuis, B.K. Histopathologic composition of cerebral thrombi of acute Stroke patients is correlated with Stroke subtype and thrombus attenuation. PLoS ONE 2014, 9, e88882. [Google Scholar] [CrossRef] [PubMed]
- Simons, N.; Mitchell, P.; Dowling, R.; Gonzales, M.; Yan, B. Thrombus composition in acute ischemic Stroke: A histopathological study of thrombus extracted by endovascular retrieval. J. Neuroradiol. 2015, 42, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Sporns, P.B.; Hanning, U.; Schwindt, W.; Velasco, A.; Minnerup, J.; Zoubi, T.; Heindel, W.; Jeibmann, A.; Niederstadt, T.U. Ischemic Stroke: What does the histological composition tell us about the origin of the thrombus? Stroke 2017, 48, 2206–2210. [Google Scholar] [CrossRef] [PubMed]
- Brinjikji, W.; Duffy, S.; Burrows, A.; Hacke, W.; Liebeskind, D.; Majoie, C.; Dippel, D.W.J.; Siddiqui, A.H.; Khatri, P.; Baxter, B.; et al. Correlation of imaging and histopathology of thrombi in acute ischemic Stroke with etiology and outcome: A systematic review. J. Neurointerv. Surg. 2017, 9, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Dargazanli, C.; Rigau, V.; Eker, O.; Bareiro, C.R.; Machi, P.; Gascou, G.; Arquizan, C.; Ayrignac, X.; Mourand, I.; Corlobe, A.; et al. High CD3+ Cells in Intracranial Thrombi Represent a Biomarker of Atherothrombotic Stroke. PLoS ONE 2016, 11, e0154945. [Google Scholar] [CrossRef] [PubMed]
- Lackovic, J.; Howitt, J.; Callaway, J.K.; Silke, J.; Bartlett, P.; Tan, S.S. Differential regulation of Nedd4 ubiquitin ligases and their adaptor protein Ndfip1 in a rat model of ischemic Stroke. Exp. Neurol. 2012, 235, 326–335. [Google Scholar] [CrossRef] [PubMed]
- Prentice, H.; Modi, J.P.; Wu, J.Y. Mechanisms of neuronal protection against excitotoxicity, endoplasmic reticulum stress, and mitochondrial dysfunction in Stroke and neurodegenerative diseases. Oxid. Med. Cell. Longev. 2015, 2015, 964518. [Google Scholar] [CrossRef] [PubMed]
- Castellanos, M.; Castillo, J.; Garcia, M.M.; Leira, R.; Serena, J.; Chamorro, A.; Davalos, A. Inflammation-mediated damage in progressing lacunar infarctions: A potential therapeutic target. Stroke 2002, 33, 982–987. [Google Scholar] [CrossRef] [PubMed]
- Esenwa, C.C.; Elkind, M.S. Inflammatory risk factors, biomarkers and associated therapy in ischaemic Stroke. Nat. Rev. Neurol. 2016, 12, 594–604. [Google Scholar] [CrossRef] [PubMed]
- Montaner, J.; Salat, D.; Garcia-Berrocoso, T.; Molina, C.A.; Chacon, P.; Ribo, M.; Alvarez-Sabin, J.; Rosell, A. Reperfusion therapy for acute Stroke improves outcome by decreasing neuroinflammation. Transl. Stroke Res. 2010, 1, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Rallidis, L.S.; Vikelis, M.; Panagiotakos, D.B.; Rizos, I.; Zolindaki, M.G.; Kaliva, K.; Kremastinos, D.T. Inflammatory markers and in-hospital mortality in acute ischaemic Stroke. Atherosclerosis 2006, 189, 193–197. [Google Scholar] [CrossRef] [PubMed]
- Sairanen, T.; Carpen, O.; Karjalainen-Lindsberg, M.L.; Paetau, A.; Turpeinen, U.; Kaste, M.; Lindsberg, P.J. Evolution of cerebral tumor necrosis factor-α production during human ischemic Stroke. Stroke 2001, 32, 1750–1758. [Google Scholar] [CrossRef] [PubMed]
- Vila, N.; Castillo, J.; Davalos, A.; Chamorro, A. Proinflammatory cytokines and early neurological worsening in ischemic Stroke. Stroke 2000, 31, 2325–2329. [Google Scholar] [CrossRef] [PubMed]
- Castillo, J.; Alvarez-Sabin, J.; Martinez-Vila, E.; Montaner, J.; Sobrino, T.; Vivancos, J. Inflammation markers and prediction of post-Stroke vascular disease recurrence: The MITICO study. J. Neurol. 2009, 256, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Juurlink, B.H.; Sweeney, M.I. Mechanisms that result in damage during and following cerebral ischemia. Neurosci. Biobehav. Rev. 1997, 21, 121–128. [Google Scholar] [CrossRef]
- Castellanos, M.; Leira, R.; Serena, J.; Blanco, M.; Pedraza, S.; Castillo, J.; Davalos, A. Plasma cellular-fibronectin concentration predicts hemorrhagic transformation after thrombolytic therapy in acute ischemic Stroke. Stroke 2004, 35, 1671–1676. [Google Scholar] [CrossRef] [PubMed]
- Castellanos, M.; Sobrino, T.; Millan, M.; Garcia, M.; Arenillas, J.; Nombela, F.; Brea, D.; Perez de la Ossa, N.; Serena, J.; Vivancos, J.; et al. Serum cellular fibronectin and matrix metalloproteinase-9 as screening biomarkers for the prediction of parenchymal hematoma after thrombolytic therapy in acute ischemic Stroke: A multicenter confirmatory study. Stroke 2007, 38, 1855–1859. [Google Scholar] [CrossRef] [PubMed]
- Serena, J.; Blanco, M.; Castellanos, M.; Silva, Y.; Vivancos, J.; Moro, M.A.; Leira, R.; Lizasoain, I.; Castillo, J.; Davalos, A. The prediction of malignant cerebral infarction by molecular brain barrier disruption markers. Stroke 2005, 36, 1921–1926. [Google Scholar] [CrossRef] [PubMed]
- Andrews, R.K.; Berndt, M.C. Adhesion-dependent signalling and the initiation of haemostasis and thrombosis. Histol. Histopathol. 1998, 13, 837–844. [Google Scholar] [PubMed]
- Zhou, X.Y.; Hu, D.X.; Chen, R.Q.; Chen, X.Q.; Dong, W.L.; Yi, C.L. 14-3-3 isoforms differentially regulate NFκB signaling in the brain after ischemia-reperfusion. Neurochem. Res. 2017, 42, 2354–2362. [Google Scholar] [CrossRef] [PubMed]
- Cekanaviciute, E.; Fathali, N.; Doyle, K.P.; Williams, A.M.; Han, J.; Buckwalter, M.S. Astrocytic transforming growth factor-β signaling reduces subacute neuroinflammation after Stroke in mice. Glia 2014, 62, 1227–1240. [Google Scholar] [CrossRef] [PubMed]
- Cipollone, F.; Fazia, M.; Mincione, G.; Iezzi, A.; Pini, B.; Cuccurullo, C.; Ucchino, S.; Spigonardo, F.; di Nisio, M.; Cuccurullo, F.; et al. Increased expression of transforming growth factor-β1 as a stabilizing factor in human atherosclerotic plaques. Stroke 2004, 35, 2253–2257. [Google Scholar] [CrossRef] [PubMed]
- Dejana, E.; Tournier-Lasserve, E.; Weinstei, B.M. The control of vascular integrity by endothelial cell junctions: Molecular basis and pathological implications. Dev. Cell 2009, 16, 209–221. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, T.J.; Huston, J., 3rd; Mandrekar, J.N.; Schleck, C.D.; Thielen, K.R.; Kallmes, D.F. Complications of diagnostic cerebral angiography: Evaluation of 19,826 consecutive patients. Radiology 2007, 243, 812–819. [Google Scholar] [CrossRef] [PubMed]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. 2018 Guidelines for the early management of patients with acute ischemic Stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018. [Google Scholar] [CrossRef] [PubMed]
- Powers, W.J.; Derdeyn, C.P.; Biller, J.; Coffey, C.S.; Hoh, B.L.; Jauch, E.C.; Johnston, K.C.; Johnston, S.C.; Khalessi, A.A.; Kidwell, C.S.; et al. American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2015, 46, 3020–3035. [Google Scholar] [PubMed]
- Park, H.; Hwang, G.J.; Jin, S.C.; Jung, C.K.; Bang, J.S.; Han, M.K.; Bae, H.J.; Choe, G.Y.; Oh, C.W.; Kwon, O.K. A retrieval thrombectomy technique with the Solitaire stent in a large cerebral artery occlusion. Acta Neurochir. 2011, 153, 1625–1631. [Google Scholar] [CrossRef] [PubMed]
- Zaidat, O.O.; Yoo, A.J.; Khatri, P.; Tomsick, T.A.; von Kummer, R.; Saver, J.L.; Marks, M.P.; Prabhakaran, S.; Kallmes, D.F.; Fitzsimmons, B.F.; et al. Recommendations on angiographic revascularization grading standards for acute ischemic Stroke: A consensus statement. Stroke 2013, 44, 2650–2663. [Google Scholar] [CrossRef] [PubMed]
- Shevchenko, A.; Tomas, H.; Havlis, J.; Olsen, J.V.; Mann, M. In-gel digestion for mass spectrometric characterization of proteins and proteomes. Nat. Protoc. 2006, 1, 2856–2860. [Google Scholar] [CrossRef] [PubMed]
- Lachen-Montes, M.; Gonzalez-Morales, A.; Zelaya, M.V.; Perez-Valderrama, E.; Ausin, K.; Ferrer, I.; Fernandez-Irigoyen, J.; Santamaria, E. Olfactory bulb neuroproteomics reveals a chronological perturbation of survival routes and a disruption of prohibitin complex during Alzheimer’s disease progression. Sci. Rep. 2017, 7, 9115. [Google Scholar] [CrossRef] [PubMed]
- Shilov, I.V.; Seymour, S.L.; Patel, A.A.; Loboda, A.; Tang, W.H.; Keating, S.P.; Hunter, C.L.; Nuwaysir, L.M.; Schaeffer, D.A. The Paragon Algorithm, a next generation search engine that uses sequence temperature values and feature probabilities to identify peptides from tandem mass spectra. Mol. Cell. Proteom. 2007, 6, 1638–1655. [Google Scholar] [CrossRef] [PubMed]
- Tang, W.H.; Shilov, I.V.; Seymour, S.L. Nonlinear fitting method for determining local false discovery rates from decoy database searches. J. Proteom. Res. 2008, 7, 3661–3667. [Google Scholar] [CrossRef] [PubMed]
- Vizcaino, J.A.; Deutsch, E.W.; Wang, R.; Csordas, A.; Reisinger, F.; Rios, D.; Dianes, J.A.; Sun, Z.; Farrah, T.; Bandeira, N.; et al. ProteomeXchange provides globally coordinated proteomics data submission and dissemination. Nat. Biotechnol. 2014, 32, 223–226. [Google Scholar] [CrossRef] [PubMed]







| Clinical variables | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| Age (years) | 72 | 50 | 78 | 70 |
| Gender | male | male | male | male |
| Stroke subtype | CE 1 | AT 2 | AT 2 | CE 1 |
| Hypertension | + | − | + | + |
| Dyslipemia | + | − | + | − |
| Diabetes Mellitus | − | − | + | − |
| Atrial Fibrilation | + | − | − | + |
| Ipsilateral internal carotid status | non stenosing plaques | occlusion | 50–69% stenosis | non stenosing plaques |
| Smoke | + | + | + | + |
| Stroke Therapy | ev Rtpa 3 + Thrombectomy | Rtpa 3 + Thrombectomy + Angioplasty/Stenting | ev Rtpa 3 + Thrombectomy | ev Rtpa 3 + Thrombectomy |
| Onset to recanalization time (min) | 210 | 360 | 320 | 210 |
| Arterial Segment | Left MCA 4 | Left ICA + MCA 4 | Right MCA 4 | Left MCA 4 + left ACA 5 |
| Stent Retriever Dispositive | pREset | pREset | pREset | pREset |
| Number of passes 6 | 3 | 1 | 1 | 2(MCA 4) + 2(ACA 5) |
| TICI 7 scale | 3 | 3 | 3 | 3 |
| Canonical Pathways | -Log (p-Value) | % | Thrombotic Proteins |
|---|---|---|---|
| Remodeling of Epithelial Adherens Junctions | 2.51 × 10−1 | 56.1 | 37 |
| Protein Ubiquitination Pathway | 2.47 × 10−1 | 28.3 | 72 |
| Mitochondrial Dysfunction | 2.36 × 10−1 | 33.9 | 56 |
| Acute Phase Response Signaling | 2.23 × 10−1 | 32.7 | 55 |
| Clathrin-mediated Endocytosis Signaling | 2.18 × 10−1 | 30.1 | 59 |
| Integrin Signaling | 2.14 × 10−1 | 28.8 | 61 |
| Caveolar-mediated Endocytosis Signaling | 2.02 × 10−1 | 47.9 | 34 |
| Phagosome Maturation | 1.97 × 10−1 | 34.3 | 46 |
| LXR/RXR Activation | 1.83 × 10−1 | 34.7 | 42 |
| Actin Cytoskeleton Signaling | 1.82 × 10−1 | 26.1 | 58 |
| Fcγ Receptor-mediated Phagocytosis in Macrophages and Monocytes | 1.75 × 10−1 | 38.7 | 36 |
| RhoGDI Signaling | 1.49 × 10−1 | 26.7 | 46 |
| Leukocyte Extravasation Signaling | 1.44 × 10−1 | 24.4 | 50 |
| Ephrin Receptor Signaling | 1.42 × 10−1 | 26.2 | 45 |
| Gap Junction Signaling | 1.37 × 10−1 | 26.2 | 43 |
| NRF2-mediated Oxidative Stress Response | 1.32 × 10−1 | 24.2 | 46 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muñoz, R.; Santamaría, E.; Rubio, I.; Ausín, K.; Ostolaza, A.; Labarga, A.; Roldán, M.; Zandio, B.; Mayor, S.; Bermejo, R.; et al. Mass Spectrometry-Based Proteomic Profiling of Thrombotic Material Obtained by Endovascular Thrombectomy in Patients with Ischemic Stroke. Int. J. Mol. Sci. 2018, 19, 498. https://doi.org/10.3390/ijms19020498
Muñoz R, Santamaría E, Rubio I, Ausín K, Ostolaza A, Labarga A, Roldán M, Zandio B, Mayor S, Bermejo R, et al. Mass Spectrometry-Based Proteomic Profiling of Thrombotic Material Obtained by Endovascular Thrombectomy in Patients with Ischemic Stroke. International Journal of Molecular Sciences. 2018; 19(2):498. https://doi.org/10.3390/ijms19020498
Chicago/Turabian StyleMuñoz, Roberto, Enrique Santamaría, Idoya Rubio, Karina Ausín, Aiora Ostolaza, Alberto Labarga, Miren Roldán, Beatriz Zandio, Sergio Mayor, Rebeca Bermejo, and et al. 2018. "Mass Spectrometry-Based Proteomic Profiling of Thrombotic Material Obtained by Endovascular Thrombectomy in Patients with Ischemic Stroke" International Journal of Molecular Sciences 19, no. 2: 498. https://doi.org/10.3390/ijms19020498