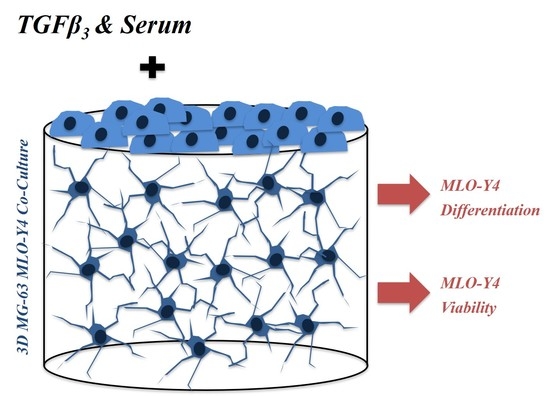
Phenotype and Viability of MLO-Y4 Cells Is Maintained by TGFβ3 in a Serum-Dependent Manner within a 3D-Co-Culture with MG-63 Cells
Abstract
:1. Introduction
2. Results
2.1. TGFβ3 Maintained Runx2 Expression in Co-Cultured MG-63 Osteoblast-Like Cells and Did not Affect the Increase in Osteocalcin Expression
2.2. TGFβ3 Maintained Osteocalcin Expression in 3D Co-Cultured MLO-Y4 Cells Serum-Independently and E11 Expression in a Serum-Dependent Manner
2.3. TGFβ3 Regulated Type I Collagen Expression in Co-Cultured MG-63 Osteoblast-Like Cells
2.4. TGFβ3 Reduced Cell Death of MLO-Y4 Osteocyte-Like Cells in a Serum-Dependent Manner
3. Discussion
4. Materials and Methods
4.1. Cell Culture
4.2. RT-qPCR
4.3. Immunocytochemical Staining
4.4. Viability and Cell Death
4.5. Statistical Analysis
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| 2/3D | Two-/Three-dimensional |
| TGFβ3 | Transforming growth factor beta 3 |
| RT-PCR | Reverse transcribed polymerase chain reaction |
| ECM | Extracellular matrix |
| SF | Serum free |
| FCS | Fetal calf serum |
References
- Tang, S.Y.; Alliston, T. Regulation of postnatal bone homeostasis by TGFβ. Bonekey Rep. 2013, 2, 255. [Google Scholar] [CrossRef] [PubMed]
- Robertson, I.B.; Rifkin, D.B. Regulation of the Bioavailability of TGF-β and TGF-β-Related Proteins. Cold Spring Harb. Perspect. Biol. 2016, 8, a021907. [Google Scholar] [CrossRef] [PubMed]
- Dallas, S.L.; Rosser, J.L.; Mundy, G.R.; Bonewald, L.F. Proteolysis of latent transforming growth factor-beta (TGF-beta)-binding protein-1 by osteoclasts. A cellular mechanism for release of TGF-beta from bone matrix. J. Biol. Chem. 2002, 277, 21352–21360. [Google Scholar] [CrossRef] [PubMed]
- Hinz, B. The extracellular matrix and transforming growth factor-β1: Tale of a strained relationship. Matrix Biol. 2015, 47, 54–65. [Google Scholar] [CrossRef] [PubMed]
- Oreffo, R.O.; Mundy, G.R.; Seyedin, S.M.; Bonewald, L.F. Activation of the bone-derived latent TGF beta complex by isolated osteoclasts. Biochem. Biophys. Res. Commun. 1989, 158, 817–823. [Google Scholar] [CrossRef]
- Wu, M.; Chen, G.; Li, Y.P. TGF-β and BMP signalling in osteoblast, skeletal development and bone formation, homeostasis and disease. Bone Res. 2016, 4, 16009. [Google Scholar] [CrossRef] [PubMed]
- Poniatowski, L.A.; Wojdasiewicz, P.; Gasik, R.; Szukiewicz, D. Transforming Growth Factor Beta Family: Insight into the Role of Growth Factors in Regulation of Fracture Healing Biology and Potential Clinical Applications. Mediat. Inflamm. 2015, 2015, 137823. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Deng, C.; Li, Y.P. TGF-β and BMP signalling in osteoblast differentiation and bone formation. Int. J. Biol. Sci. 2012, 8, 272–288. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Wang, X.F. Signaling cross-talk between TGF-beta/BMP and other pathways. Cell Res. 2009, 19, 71–88. [Google Scholar] [CrossRef] [PubMed]
- Matsunobu, T.; Torigoe, K.; Ishikawa, M.; de Vega, S.; Kulkarni, A.B.; Iwamoto, Y.; Yamada, Y. Critical roles of the TGF-beta type I receptor ALK5 in perichondrial formation and function, cartilage integrity and osteoblast differentiation during growth plate development. Dev. Biol. 2009, 332, 325–338. [Google Scholar] [CrossRef] [PubMed]
- Alliston, T.; Choy, L.; Ducy, P.; Karsenty, G.; Derynck, R. TGF-beta-induced repression of CBFA1 by Smad3 decreases cbfa1 and osteocalcin expression and inhibits osteoblast differentiation. EMBO J. 2001, 20, 2254–2272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klein Nulend, J.; van der Plas, A.; Semeins, C.M.; Ajubi, N.E.; Frangos, J.A.; Nijweide, P.J.; Burger, E.H. Sensitivity of osteocytes to biomechanical stress in vitro. FASEB 1995, 9, 441–445. [Google Scholar] [CrossRef]
- Dallas, S.L.; Prideaux, M.; Bonewald, L.F. The osteocyte: An endocrine cell ... and more. Endocr. Rev. 2013, 34, 658–690. [Google Scholar] [CrossRef] [PubMed]
- Prideaux, M.; Findlay, D.M.; Atkins, G.J. Osteocytes: The master cells in bone remodelling. Curr. Opin. Pharmacol. 2016, 28, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Richards, R.G.; Simpson, A.E.; Jähn, K.; Furlong, P.I.; Stoddart, M.J. Establishing a 3D Ex vivo culture system for investigations of bone metabolism and biomaterial interactions. ALTEX 2007, 24, 56–59. [Google Scholar] [PubMed]
- Simpson, A.E.; Stoddart, M.J.; Davies, C.M.; Jähn, K.; Furlong, P.I.; Gasser, J.A.; Jones, D.B.; Noble, B.S.; Richards, R.G. TGFβ3 and loading increases osteocyte survival in human cancellous bone cultured ex vivo. Cell Biochem. Funct. 2009, 27, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Stoddart, M.J.; Furlong, P.I.; Simpson, A.E.; Davies, C.M.; Richards, R.G. A comparison of non-radioactive methods for assessing viability in ex vivo cultured cancellous bone: Technical note. Eur. Cell Mater. 2006, 12, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Vazquez, M.; Evans, B.A.; Riccardi, D.; Evans, S.L.; Ralphs, J.R.; Dillingham, C.M.; Mason, D.J. A new method to investigate how mechanical loading of osteocytes controls osteoblasts. Front. Endocrinol. 2014, 5, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Tsao, Y.T.; Huang, Y.J.; Wu, H.H.; Liu, Y.A.; Liu, Y.S.; Lee, O.K. Osteocalcin Mediates Biomineralization during Osteogenic Maturation in Human Mesenchymal Stromal Cells. Int. J. Mol. Sci. 2017, 18, 159. [Google Scholar] [CrossRef] [PubMed]
- Zhang, K.; Barragan-Adjemian, C.; Ye, L.; Kotha, S.; Dallas, M.; Lu, Y.; Zhao, S.; Harris, M.; Harris, S.E.; Feng, J.Q.; et al. E11/gp38 selective expression in osteocytes: Regulation by mechanical strain and role in dendrite elongation. Mol. Cell Biol. 2006, 26, 4539–4552. [Google Scholar] [CrossRef] [PubMed]
- Busse, B.; Djonic, D.; Milovanovic, P.; Hahn, M.; Püschel, K.; Ritchie, R.O.; Djuric, M.; Amling, M. Decrease in the osteocyte lacunar density accompanied by hypermineralized lacunar occlusion reveals failure and delay of remodeling in aged human bone. Aging Cell 2010, 9, 1065–1075. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Milovanovic, P.; Zimmermann, E.A.; Hahn, M.; Djonic, D.; Püschel, K.; Djuric, M.; Amling, M.; Busse, B. Osteocytic Canalicular Networks: Morphological Implications for Altered Mechanosensitivity. ACS Nano 2013, 7, 7542–7551. [Google Scholar] [CrossRef] [PubMed]
- Ten Dijke, P.; Iwata, K.; Goddard, C.; Pieler, C.; Canalis, E.; McCarthy, T.L.; Centrella, M. Recombinant transforming growth factor type beta 3: Biological activities and receptor-binding properties in isolated bone cells. Mol. Cell Biol. 1990, 10, 4473–4479. [Google Scholar] [CrossRef] [PubMed]
- Janssens, K.; ten Dijke, P.; Janssens, S.; Van Hul, W. Transforming Growth Factor-β1 to the Bone. Endocr. Rev. 2005, 26, 743–774. [Google Scholar] [CrossRef] [PubMed]
- Kato, Y.; Windle, J.; Koop, B.; Mundy, G.R.; Bonewald, L.F. Establishment of an osteocyte-like cell line, MLO-Y4. J. Bone Miner. Res. 1997, 12, 2014–2023. [Google Scholar] [CrossRef] [PubMed]
- Karsdal, M.A.; Larsen, L.; Engsig, M.T.; Lou, H.; Ferreras, M.; Lochter, A.; Delaissé, J.M.; Foged, N.T. Matrix metalloproteinase-dependent activation of latent transforming growth factor-beta controls the conversion of osteoblasts into osteocytes by blocking osteoblast apoptosis. J. Biol. Chem. 2002, 277, 44061–44067. [Google Scholar] [CrossRef] [PubMed]
- Karsdal, M.A.; Andersen, T.A.; Bonewald, L.F.; Christiansen, C. Matrix metalloproteinases (MMPs) safeguard osteoblasts from apoptosis during transdifferentiation into osteocytes: MT1-MMP maintains osteocyte viability. DNA Cell Biol. 2004, 23, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Holmbeck, K.; Bianco, P.; Pidoux, I.; Inoue, S.; Billinghurst, R.C.; Wu, W.; Chrysovergis, K.; Yamada, S.; Birkedal-Hansen, H.; Poole, A.R. The metalloproteinase MT1-MMP is required for normal development and maintenance of osteocyte processes in bone. J. Cell Sci. 2005, 118, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Dole, N.S.; Mazur, C.S.; Acevedo, C.; Lopez, J.P.; Monteiro, D.A.; Fowler, T.W.; Gludovatz, B.; Walsh, F.; Regan, J.N.; Messina, S.; et al. Osteocyte-Intrinsic TGF-β Signaling Regulates Bone Quality through Perilacunar/Canalicular Remodeling. Cell Rep. 2017, 21, 2585–2596. [Google Scholar] [CrossRef] [PubMed]
- Jähn, K.; Stoddart, M.J. Viability assessment of osteocytes using histological lactate dehydrogenase activity staining on human cancellous bone sections. In Mammalian Cell Culture, 1st ed.; Stoddart, M.J., Ed.; Humana Press: New York, NY, USA, 2011; Volume 740, pp. 141–148. ISBN 978-1-61779-108-6. [Google Scholar]





| Gene | Forward Primer | Reverse Primer |
|---|---|---|
| human GAPDH | GGT ATC GTG GAA GGA CTC ATG A | GGC CAT CCA CAG TCT TCT G |
| human Runx2 | GTG GAC GAG GCA AGA GTT TC | TTC CCG AGG TCC ATC TAC TG |
| human osteocalcin | GGC AGC GAG GTA GTG AAG AG | GAT CCG GGT AGG GGA CTG |
| human type I collagen | CCC TGG AAA GAA TGG AGA TGA T | ACT GAA ACC TCT GTG TCC CTT CA |
| mouse 18SrRNA | GCA ATT ATT CCC CAT GAA CG | GGC CTC ACT AAA CCA TCC AA |
| mouse E11 | AAG ATG GCT TGC CAG TAG TCA | GGC GAG AAC CTT CCA GAA AT |
| mouse osteocalcin | CAGACAAGTCCCACACAGCA | GAA AT |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jähn, K.; Mason, D.J.; Ralphs, J.R.; Evans, B.A.J.; Archer, C.W.; Richards, R.G.; Stoddart, M.J. Phenotype and Viability of MLO-Y4 Cells Is Maintained by TGFβ3 in a Serum-Dependent Manner within a 3D-Co-Culture with MG-63 Cells. Int. J. Mol. Sci. 2018, 19, 1932. https://doi.org/10.3390/ijms19071932
Jähn K, Mason DJ, Ralphs JR, Evans BAJ, Archer CW, Richards RG, Stoddart MJ. Phenotype and Viability of MLO-Y4 Cells Is Maintained by TGFβ3 in a Serum-Dependent Manner within a 3D-Co-Culture with MG-63 Cells. International Journal of Molecular Sciences. 2018; 19(7):1932. https://doi.org/10.3390/ijms19071932
Chicago/Turabian StyleJähn, Katharina, Deborah J. Mason, Jim R. Ralphs, Bronwen A.J. Evans, Charles W. Archer, R. Geoff Richards, and Martin J. Stoddart. 2018. "Phenotype and Viability of MLO-Y4 Cells Is Maintained by TGFβ3 in a Serum-Dependent Manner within a 3D-Co-Culture with MG-63 Cells" International Journal of Molecular Sciences 19, no. 7: 1932. https://doi.org/10.3390/ijms19071932