An In Silico Model for Predicting Drug-Induced Hepatotoxicity
Abstract
:1. Introduction
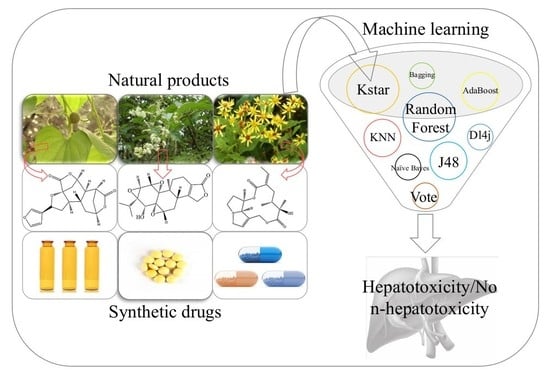
2. Results
2.1. Optimizing the Training Set
2.2. Data Analysis
2.3. Model Construction and Evaluation
2.4. External Validation
3. Discussion
- (1)
- In this work, all of the parameters and configurations of the machine learning algorithms were set to the default values provided by Waikato Environment for Knowledge Analysis (WEKA). The performance of our model may be improved by adopting more appropriate parameters.
- (2)
- In the development of the ensemble model, averaging method was utilized to integrate multiple classifiers. Actually, there have been many other classifier fusion strategies: Mean, Maximum, Multiple, and so forth. In future research, comparisons among different classifier fusion strategies are needed.
- (3)
- In addition, only 55 molecular descriptors were used in the development of the in silico model. With the development of computational chemistry, hundreds of molecular descriptors are available as well as dozens of molecular fingerprint systems. The introduction of more molecular descriptors/molecular fingerprints may contribute to acquiring an in silico model with better performance.
4. Materials and Methods
4.1. Datasets
4.2. Data Preprocessing
- (1)
- The simplified molecular input line entry system (SMILES) information of each compound was retrieved from PubChem Compound database by name/CAS matching.
- (2)
- Any compounds containing metal and rare atoms were discarded, as well as inorganic compounds and mixtures.
- (3)
- The standardizer tool (Version 18.23.0) from Marvin was used to unify the structures of compounds. (I) Salts were converted into the corresponding bases or acids; (II) water molecules and solvents were deleted; (III) all aromatic compounds were normalized to kekule form; (IV) Neutralize model was implemented to neutralize the molecules. Finally, Clear Stereo model was utilized to clear the stereo information of the molecule.
- (4)
- Compounds containing carbon atoms fewer than 4 or with molecular weight greater than 900 were deleted from the datasets.
- (5)
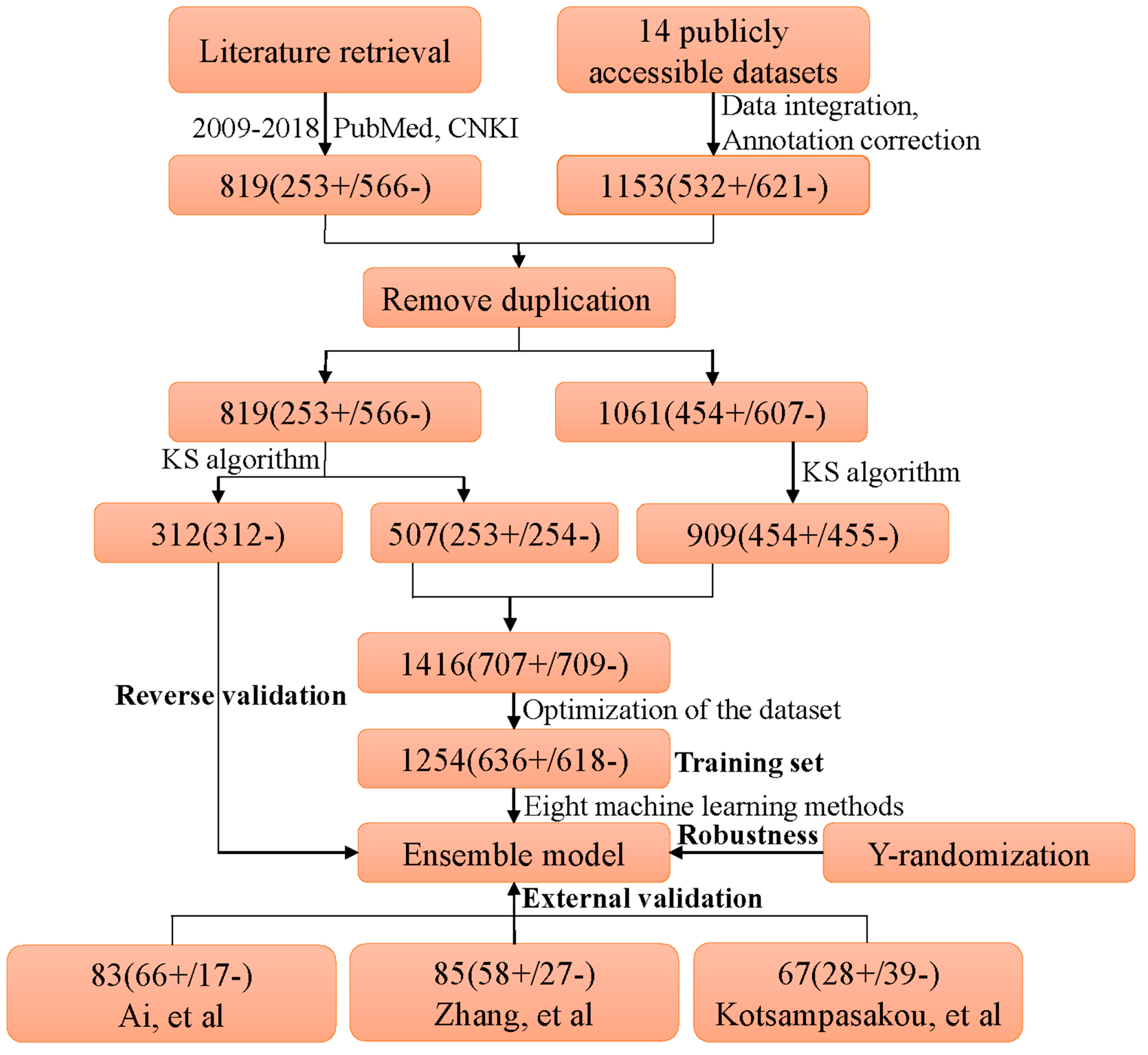
- High-quality label annotation always assists in creating accurate and reliable in silico models. To minimize the risk brought by ambiguous data, a critical data screening strategy was established. Data from DILIrank [42], Livertox [44], and LTKB [45] were retained directly and marked as dataset 1. For other datasets, the compounds included in dataset 1 were discarded, and the remaining data were named as dataset 2. Compounds with conflicting class labels were removed from dataset 2, and the remaining data were utilized to develop a large-scale dataset for hepatotoxicity in combination with dataset 1. Finally, a total of 1880 compounds were retained, 707 positives and 1173 negatives. As shown in Figure 4, a total of 1153 compounds originated from datasets of prior studies, and the present study provided 819 compounds (727 new compounds).
- (6)
- Machine learning algorithms are known to work best on balanced datasets. Imbalanced datasets usually bring challenges to the development of in silico models, and may lead to biased performance of prediction models established [51]. To avoid the risk brought by unbalanced datasets, the Kennard–Stone algorithm was used to balance the datasets provided by prior studies and the present study. Finally, we acquired a large-scale balanced dataset for hepatotoxicity, including 707 positives and 709 negatives, which were used for the following analysis.
4.3. External Validation
4.4. Molecular Descriptors
4.5. Feature Selection
4.6. Model Construction
4.7. Performance Evaluation
4.8. Y-Randomization
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| DILI | Drug-induced liver injury |
| CNKI | China National Knowledge Infrastructure |
| SMILES | Simplified molecular-input line-entry system |
| QSAR | Quantitative structure–activity relationship |
| ACC | Accuracy |
| SE | Sensitivity |
| SP | Specificity |
| AUC | Area under the receiver-operating characteristic curve |
| BACC | Balanced accuracy |
| WEKA | Waikato environment for knowledge analysis |
| KNN | K-nearest neighbor |
| J48 | C4.5 decision tree |
| Dl4j | Deeplearning4j |
| ROC | Receiver operating characteristic analysis |
| TCMs | Traditional Chinese medicines |
References
- Cheng, A.; Dixon, S.L. In silico models for the prediction of dose-dependent human hepatotoxicity. J. Comput. Aided Mol. Des. 2003, 17, 811–823. [Google Scholar] [CrossRef]
- Almazroo, O.A.; Miah, M.K.; Venkataramanan, R. Drug Metabolism in the Liver. Clin. Liver Dis. 2017, 21, 1–20. [Google Scholar] [CrossRef]
- Real, M.; Barnhill, M.S.; Higley, C.; Rosenberg, J.; Lewis, J.H. Drug-Induced Liver Injury: Highlights of the Recent Literature. Drug Saf. 2018. [Google Scholar] [CrossRef]
- Lee, W.M. Drug-induced hepatotoxicity. N. Engl. J. Med. 2003, 349, 474–485. [Google Scholar] [CrossRef]
- Regev, A. Drug-induced liver injury and drug development: Industry perspective. Semin. Liver Dis. 2014, 34, 227–239. [Google Scholar] [CrossRef]
- Ailan, C. In Silico Prediction of Hepatotoxicity. Curr. Comput. Aided Drug Des. 2009, 5, 122–127. [Google Scholar]
- Assis, D.N.; Navarro, V.J. Human drug hepatotoxicity: A contemporary clinical perspective. Expert Opin. Drug Metab. Toxicol. 2009, 5, 463–473. [Google Scholar] [CrossRef]
- Chen, M.; Borlak, J.; Tong, W. Predicting idiosyncratic drug-induced liver injury: Some recent advances. Expert Rev. Gastroenterol. Hepatol. 2014, 8, 721–723. [Google Scholar] [CrossRef]
- Chen, M.; Bisgin, H.; Tong, L.; Hong, H.; Fang, H.; Borlak, J.; Tong, W. Toward predictive models for drug-induced liver injury in humans: Are we there yet? Biomark. Med. 2014, 8, 201–213. [Google Scholar] [CrossRef]
- Chen, M.; Vijay, V.; Shi, Q.; Liu, Z.; Fang, H.; Tong, W. FDA-approved drug labeling for the study of drug-induced liver injury. Drug Discov. Today 2011, 16, 697–703. [Google Scholar] [CrossRef]
- Banerjee, P.; Eckert, A.; Schrey, A.; Preissner, R. ProTox-II: A webserver for the prediction of toxicity of chemicals. Nucleic Acids Res. 2018, 46, 257–263. [Google Scholar] [CrossRef]
- Cheng, F.; Li, W.; Liu, G.; Tang, Y. In silico ADMET prediction: Recent advances, current challenges and future trends. Curr. Top. Med. Chem. 2013, 13, 1273–1289. [Google Scholar] [CrossRef]
- Hewitt, M.; Przybylak, K. In Silico Models for Hepatotoxicity. In In Silico Methods for Predicting Drug Toxicity; Benfenati, E., Ed.; Springer: New York, NY, USA, 2016; pp. 201–236. [Google Scholar]
- Pizzo, F.; Lombardo, A.; Manganaro, A.; Benfenati, E. A New Structure-Activity Relationship (SAR) Model for Predicting Drug-Induced Liver Injury, Based on Statistical and Expert-Based Structural Alerts. Front. Pharmacol. 2016, 7, 442. [Google Scholar] [CrossRef]
- Funk, C.; Roth, A. Current limitations and future opportunities for prediction of DILI from in vitro. Arch. Toxicol. 2017, 91, 131–142. [Google Scholar] [CrossRef]
- Przybylak, K.R.; Cronin, M.T. In silico models for drug-induced liver injury—Current status. Expert Opin. Drug Metab. Toxicol. 2012, 8, 201–217. [Google Scholar] [CrossRef]
- Olson, H.; Betton, G.; Robinson, D.; Thomas, K.; Monro, A.; Kolaja, G.; Lilly, P.; Sanders, J.; Sipes, G.; Bracken, W.; et al. Concordance of the toxicity of pharmaceuticals in humans and in animals. Regul. Toxicol. Pharmacol. 2000, 32, 56–67. [Google Scholar] [CrossRef]
- Marchant, C.A.; Fisk, L.; Note, R.R.; Patel, M.L.; Suarez, D. An expert system approach to the assessment of hepatotoxic potential. Chem. Biodivers. 2009, 6, 2107–2114. [Google Scholar] [CrossRef]
- Greene, N.; Fisk, L.; Naven, R.T.; Note, R.R.; Patel, M.L.; Pelletier, D.J. Developing structure-activity relationships for the prediction of hepatotoxicity. Chem. Res. Toxicol. 2010, 23, 1215–1222. [Google Scholar] [CrossRef]
- Fourches, D.; Barnes, J.C.; Day, N.C.; Bradley, P.; Reed, J.Z.; Tropsha, A. Cheminformatics analysis of assertions mined from literature that describe drug-induced liver injury in different species. Chem. Res. Toxicol. 2010, 23, 171–183. [Google Scholar] [CrossRef]
- Stepan, A.F.; Walker, D.P.; Bauman, J.; Price, D.A.; Baillie, T.A.; Kalgutkar, A.S.; Aleo, M.D. Structural alert/reactive metabolite concept as applied in medicinal chemistry to mitigate the risk of idiosyncratic drug toxicity: A perspective based on the critical examination of trends in the top 200 drugs marketed in the United States. Chem. Res. Toxicol. 2011, 24, 1345–1410. [Google Scholar] [CrossRef]
- Fraser, K.; Bruckner, D.M.; Dordick, J.S. Advancing Predictive Hepatotoxicity at the Intersection of Experimental, in Silico, and Artificial Intelligence Technologies. Chem. Res. Toxicol. 2018, 31, 412–430. [Google Scholar] [CrossRef]
- Ekins, S.; Williams, A.J.; Xu, J.J. A predictive ligand-based Bayesian model for human drug-induced liver injury. Drug Metab. Dispos. 2010, 38, 2302–2308. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.; Nam, H. Prediction models for drug-induced hepatotoxicity by using weighted molecular fingerprints. BMC Bioinform. 2017, 18, 227. [Google Scholar] [CrossRef]
- Huang, S.H.; Tung, C.W.; Fulop, F.; Li, J.H. Developing a QSAR model for hepatotoxicity screening of the active compounds in traditional Chinese medicines. Food Chem. Toxicol. 2015, 78, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; Liu, B.; Wang, C. Hepatotoxicity evaluation of traditional Chinese medicines using a computational molecular model. Clin. Toxicol. 2017, 55, 996–1000. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Monteagudo, M.; Cordeiro, M.N.; Borges, F. Computational chemistry approach for the early detection of drug-induced idiosyncratic liver toxicity. J. Comput. Chem. 2008, 29, 533–549. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, A.D.; Zhu, H.; Fourches, D.; Rusyn, I.; Tropsha, A. Modeling liver-related adverse effects of drugs using knearest neighbor quantitative structure-activity relationship method. Chem. Res. Toxicol. 2010, 23, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Matthews, E.J.; Ursem, C.J.; Kruhlak, N.L.; Benz, R.D.; Sabate, D.A.; Yang, C.; Klopman, G.; Contrera, J.F. Identification of structure-activity relationships for adverse effects of pharmaceuticals in humans: Part B. Use of (Q)SAR systems for early detection of drug-induced hepatobiliary and urinary tract toxicities. Regul. Toxicol. Pharmacol. 2009, 54, 23–42. [Google Scholar] [CrossRef]
- Zhang, C.; Cheng, F.; Li, W.; Liu, G.; Lee, P.W.; Tang, Y. In silico Prediction of Drug Induced Liver Toxicity Using Substructure Pattern Recognition Method. Mol. Inform. 2016, 35, 136–144. [Google Scholar] [CrossRef]
- Liew, C.Y.; Lim, Y.C.; Yap, C.W. Mixed learning algorithms and features ensemble in hepatotoxicity prediction. J. Comput. Aided Mol. Des. 2011, 25, 855–871. [Google Scholar] [CrossRef]
- Xu, Y.; Dai, Z.; Chen, F.; Gao, S.; Pei, J.; Lai, L. Deep Learning for Drug-Induced Liver Injury. J. Chem. Inf. Model. 2015, 55, 2085–2093. [Google Scholar] [CrossRef]
- Kotsampasakou, E.; Montanari, F.; Ecker, G.F. Predicting drug-induced liver injury: The importance of data curation. Toxicology 2017, 389, 139–145. [Google Scholar] [CrossRef]
- Zhu, X.W.; Li, S.J. In Silico Prediction of Drug-Induced Liver Injury Based on Adverse Drug Reaction Reports. Toxicol. Sci. 2017, 158, 391–400. [Google Scholar] [CrossRef]
- Liu, Z.; Shi, Q.; Ding, D.; Kelly, R.; Fang, H.; Tong, W. Translating clinical findings into knowledge in drug safety evaluation—Drug induced liver injury prediction system (DILIps). PLoS Comput. Biol. 2011, 7, e1002310. [Google Scholar] [CrossRef]
- Mulliner, D.; Schmidt, F.; Stolte, M.; Spirkl, H.P.; Czich, A.; Amberg, A. Computational Models for Human and Animal Hepatotoxicity with a Global Application Scope. Chem. Res. Toxicol. 2016, 29, 757–767. [Google Scholar] [CrossRef]
- Ai, H.; Chen, W.; Zhang, L.; Huang, L.; Yin, Z.; Hu, H.; Zhao, Q.; Zhao, J.; Liu, H. Predicting Drug-Induced Liver Injury Using Ensemble Learning Methods and Molecular Fingerprints. Toxicol. Sci. 2018, 165, 100–107. [Google Scholar] [CrossRef]
- Ortega-Alonso, A.; Stephens, C.; Lucena, M.I.; Andrade, R.J. Case Characterization, Clinical Features and Risk Factors in Drug-Induced Liver Injury. Int. J. Mol. Sci. 2016, 17, 714. [Google Scholar] [CrossRef]
- Teo, D.C.; Ng, P.S.; Tan, S.H.; Lim, A.T.; Toh, D.S.; Chan, S.Y.; Cheong, H.H. Drug-induced liver injury associated with Complementary and Alternative Medicine: A review of adverse event reports in an Asian community from 2009 to 2014. BMC Complement. Altern. Med. 2016, 16, 192. [Google Scholar] [CrossRef]
- Frenzel, C.; Teschke, R. Herbal Hepatotoxicity: Clinical Characteristics and Listing Compilation. Int. J. Mol. Sci. 2016, 17, 588. [Google Scholar] [CrossRef]
- Chalasani, N.; Bonkovsky, H.L.; Fontana, R.; Lee, W.; Stolz, A.; Talwalkar, J.; Reddy, K.R.; Watkins, P.B.; Navarro, V.; Barnhart, H.; et al. Features and Outcomes of 899 Patients With Drug-Induced Liver Injury: The DILIN Prospective Study. Gastroenterology 2015, 148, 1340–1352. [Google Scholar] [CrossRef]
- Chen, M.; Suzuki, A.; Thakkar, S.; Yu, K.; Hu, C.; Tong, W. DILIrank: The largest reference drug list ranked by the risk for developing drug-induced liver injury in humans. Drug Discov. Today 2016, 21, 648–653. [Google Scholar] [CrossRef]
- Hong, H.; Thakkar, S.; Chen, M.; Tong, W. Development of Decision Forest Models for Prediction of Drug-Induced Liver Injury in Humans Using A Large Set of FDA-approved Drugs. Sci. Rep. 2017, 7, 17311. [Google Scholar] [CrossRef] [Green Version]
- Hoofnagle, J.H.; Serrano, J.; Knoben, J.E.; Navarro, V.J. LiverTox: A website on drug-induced liver injury. Hepatology 2013, 57, 873–874. [Google Scholar] [CrossRef]
- Chen, M.; Zhang, J.; Wang, Y.; Liu, Z.; Kelly, R.; Zhou, G.; Fang, H.; Borlak, J.; Tong, W. The liver toxicity knowledge base: A systems approach to a complex end point. Clin. Pharmacol. Ther. 2013, 93, 409–412. [Google Scholar] [CrossRef]
- Xu, J.J.; Henstock, P.V.; Dunn, M.C.; Smith, A.R.; Chabot, J.R.; de Graaf, D. Cellular imaging predictions of clinical drug-induced liver injury. Toxicol. Sci. 2008, 105, 97–105. [Google Scholar] [CrossRef]
- Low, Y.; Uehara, T.; Minowa, Y.; Yamada, H.; Ohno, Y.; Urushidani, T.; Sedykh, A.; Muratov, E.; Kuz’min, V.; Fourches, D.; et al. Predicting drug-induced hepatotoxicity using QSAR and toxicogenomics approaches. Chem. Res. Toxicol. 2011, 24, 1251–1262. [Google Scholar] [CrossRef]
- O’Brien, P.J.; Irwin, W.; Diaz, D.; Howard-Cofield, E.; Krejsa, C.M.; Slaughter, M.R.; Gao, B.; Kaludercic, N.; Angeline, A.; Bernardi, P.; et al. High concordance of drug-induced human hepatotoxicity with in vitro cytotoxicity measured in a novel cell-based model using high content screening. Arch. Toxicol. 2006, 80, 580–604. [Google Scholar] [CrossRef]
- Chen, M.; Hong, H.; Fang, H.; Kelly, R.; Zhou, G.; Borlak, J.; Tong, W. Quantitative structure-activity relationship models for predicting drug-induced liver injury based on FDA-approved drug labeling annotation and using a large collection of drugs. Toxicol. Sci. 2013, 136, 242–249. [Google Scholar] [CrossRef]
- Zhu, X.; Kruhlak, N.L. Construction and analysis of a human hepatotoxicity database suitable for QSAR modeling using post-market safety data. Toxicology 2014, 321, 62–72. [Google Scholar] [CrossRef]
- Jain, S.; Kotsampasakou, E.; Ecker, G.F. Comparing the performance of meta-classifiers—A case study on selected imbalanced data sets relevant for prediction of liver toxicity. J. Comput. Aided Mol. Des. 2018, 32, 583–590. [Google Scholar] [CrossRef]
- Peng, C.R.; Lu, W.C.; Niu, B.; Li, Y.J.; Hu, L.L. Prediction of the functional roles of small molecules in lipid metabolism based on ensemble learning. Protein Pept. Lett. 2012, 19, 108–112. [Google Scholar] [CrossRef] [PubMed]
- He, S.; Li, M.; Ye, X.; Wang, H.; Yu, W.; He, W.; Wang, Y.; Qiao, Y. Site of metabolism prediction for oxidation reactions mediated by oxidoreductases based on chemical bond. Bioinformatics 2017, 33, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; He, S.; Du, L.; Lv, Z.; Zhang, Y.; Zhang, Q.; Wang, Y. Using chemical bond-based method to predict site of metabolism for five biotransformations mediated by CYP 3A4, 2D6, and 2C9. Biochem. Pharmacol. 2018, 152, 302–314. [Google Scholar] [CrossRef] [PubMed]
- He, S.B.; Li, M.M.; Zhang, B.X.; Ye, X.T.; Du, R.F.; Wang, Y.; Qiao, Y.J. Construction of Metabolism Prediction Models for CYP450 3A4, 2D6, and 2C9 Based on Microsomal Metabolic Reaction System. Int. J. Mol. Sci. 2016, 17, 1686. [Google Scholar] [CrossRef] [PubMed]
- Kotsampasakou, E.; Ecker, G.F. Predicting Drug-Induced Cholestasis with the Help of Hepatic Transporters-An in Silico Modeling Approach. J. Chem. Inf. Model. 2017, 57, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Borlak, J.; Tong, W. High lipophilicity and high daily dose of oral medications are associated with significant risk for drug-induced liver injury. Hepatology 2013, 58, 388–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saeys, Y.; Inza, I.; Larranaga, P. A review of feature selection techniques in bioinformatics. Bioinformatics 2007, 23, 2507–2517. [Google Scholar] [CrossRef] [Green Version]
- Frank, E.; Hall, M.; Holmes, G.; Kirkby, R.; Pfahringer, B.; Witten, I.H.; Trigg, L. Weka-A Machine Learning Workbench for Data Mining. In Data Mining & Knowledge Discovery Handbook; Springer: Boston, MA, USA, 2005; pp. 1269–1277. [Google Scholar]
- Linden, A. Measuring diagnostic and predictive accuracy in disease management: An introduction to receiver operating characteristic (ROC) analysis. J. Eval. Clin. Pract. 2006, 12, 132–139. [Google Scholar] [CrossRef]
- Rucker, C.; Rucker, G.; Meringer, M. y-Randomization and its variants in QSPR/QSAR. J. Chem. Inf. Model. 2007, 47, 2345–2357. [Google Scholar] [CrossRef]





| Classifier | Training Set | ||||
|---|---|---|---|---|---|
| SE | SP | ACC | BACC | AUC | |
| NaiveBayes | 0.857 | 0.401 | 0.632 | 0.629 | 0.662 |
| KNN | 0.792 | 0.761 | 0.777 | 0.777 | 0.780 |
| KStar | 0.737 | 0.735 | 0.736 | 0.736 | 0.824 |
| AdaBoostM1 | 0.774 | 0.723 | 0.749 | 0.749 | 0.818 |
| Bagging | 0.764 | 0.754 | 0.759 | 0.759 | 0.820 |
| J48 | 0.662 | 0.672 | 0.667 | 0.667 | 0.682 |
| Randomforest | 0.785 | 0.736 | 0.761 | 0.761 | 0.852 |
| Dl4j | 0.608 | 0.592 | 0.600 | 0.600 | 0.648 |
| Vote | 0.818 | 0.748 | 0.783 | 0.783 | 0.859 |
| Dataset | References | Size of Dataset | SE | SP | ACC | BACC |
|---|---|---|---|---|---|---|
| Training | Present study | 1254 (636+/618−) | 0.818 | 0.748 | 0.783 | 0.783 |
| [37] | 1241 (683+/558−) | 0.799 | 0.603 | 0.711 | 0.701 | |
| [30] | 978 (571+/407−) | 0.948 | 0.585 | 0.797 | 0.767 | |
| [33] | 996 (541+/455−) | 0.680 | 0.610 | 0.650 | 0.645 | |
| Test | [37] | 83 (66+/17−) | 0.879 | 0.647 | 0.831 | 0.763 |
| (0.909) | (0.529) | (0.831) | (0.719) | |||
| [30] | 85 (58+/27−) | 0.707 | 0.815 | 0.741 | 0.761 | |
| (0.848) | (0.345) | (0.682) | (0.597) | |||
| [33] | 67 (28+/39−) | 0.786 | 0.590 | 0.672 | 0.688 | |
| (0.536) | (0.641) | (0.597) | (0.588) | |||
| Present study (Entire external test set) | 204 (125+/79−) | 0.773 | 0.658 | 0.730 | 0.716 | |
| Present study (Reverse validation) | 312 (0+/312−) | - | - | 0.689 | - | |
| (0.301) |
| ID | Source Name | Type of Data | No. of Compound (Positive/Negative) | DILI Categories |
|---|---|---|---|---|
| 1 | (Xu et al., 2008) [46] | Clinical data for hepatotoxicity | 344 (200/144) | Authors definition |
| 2 | (Low et al., 2011) [47] | Animal experiment | 127 (53/74) | Authors definition |
| 3 | (O’Brien et al., 2006) [48] | In vitro cell-based assay | 83 (42/41) | Severely hepatotoxic drugs and nontoxic drugs were considered as positives and negatives, respectively |
| 4 | (Rodgers et al., 2010) [28] | Clinical data for hepatotoxicity | 393 (75/318) | Actives were defined as positives, and inactives were considered as negatives |
| 5 | (Greene et al., 2010) [19] | Literature reviews and medical monographs | 425 (273/152) | HH and NE represented positives and negatives, respectively |
| 6 | (Ekins et al., 2010) [23] | Clinical data for hepatotoxicity | 532 (311/221) | Authors definition |
| 7 | (Liew et al., 2011) [31] | Medical monographs | 1274 (759/515) | Authors definition |
| 8 | (Liu et al., 2011) [35] | Drug labeling and clinical case reports | 1294 (724/570) | Authors definition |
| 9 | (Chen et al., 2013) [49] | FDA-approved drug labeling | 387 (176/211) | Authors definition |
| 10 | (Zhu and Kruhlak, 2014) [50] | Postmarket safety data | 282 (177/105) | Authors definition |
| 11 | (Huang et al., 2015) [25] | Scientific literature | 91 (83/8) | Authors definition |
| 12 | DILIrank [42] | Drug labeling and clinical data | 504 (192/312) | Only vMost-DILI-Concern were considered as positives, and vNo-DILI-Concern were considered as negatives |
| 13 | Livertox [44] | Scientific literature and public databases | 343 (119/224) | Category A and Category B were combined into positives, and Category E was considered as negatives |
| 14 | LTKB [45] | FDA-approved drug labeling | 195 (113/82) | Only vMost-DILI-Concern were considered as positives, and vNo-DILI-Concern were considered as negatives |
| Search Terms 1 | Search Terms 2 |
|---|---|
| Herbal | Hepatotoxicity |
| Medicinal plant | Liver Toxicity |
| Traditional Chinese medicine | Liver failure |
| Liver injury | |
| Liver damage | |
| Hepatitis | |
| Liver cancer | |
| Liver Tumors | |
| Hepatocellular carcinoma | |
| Liver cirrhosis | |
| Hepatomegaly | |
| Liver neoplasms | |
| Fatty liver | |
| Jaundice | |
| Cholestasis | |
| Hepatoma | |
| Liver fibrosis | |
| Liver protection | |
| Hepatoprotective |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
He, S.; Ye, T.; Wang, R.; Zhang, C.; Zhang, X.; Sun, G.; Sun, X. An In Silico Model for Predicting Drug-Induced Hepatotoxicity. Int. J. Mol. Sci. 2019, 20, 1897. https://doi.org/10.3390/ijms20081897
He S, Ye T, Wang R, Zhang C, Zhang X, Sun G, Sun X. An In Silico Model for Predicting Drug-Induced Hepatotoxicity. International Journal of Molecular Sciences. 2019; 20(8):1897. https://doi.org/10.3390/ijms20081897
Chicago/Turabian StyleHe, Shuaibing, Tianyuan Ye, Ruiying Wang, Chenyang Zhang, Xuelian Zhang, Guibo Sun, and Xiaobo Sun. 2019. "An In Silico Model for Predicting Drug-Induced Hepatotoxicity" International Journal of Molecular Sciences 20, no. 8: 1897. https://doi.org/10.3390/ijms20081897