Do Subjects from Different Occupational Groups Experience Dental Fear and Anxiety Equally?
Abstract
:1. Introduction
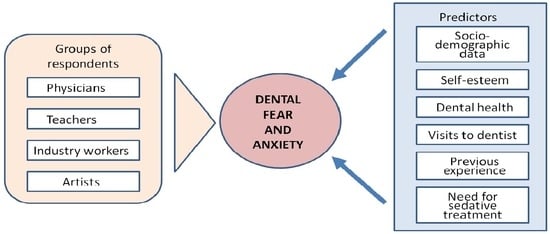
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
2.3. Statistical Analysis
3. Results
3.1. Descriptive Analysis of Occupational Groups
3.2. Associations among Variables
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stein Duker, L.I.; Grager, M.; Giffin, W.; Hikita, N.; Polido, J.C. The relationship between dental fear and anxiety, general anxiety/fear, sensory over-responsivity, and oral health behaviors and outcomes: A conceptual model. Int. J. Environ. Res. Public. Health 2022, 19, 2380. [Google Scholar] [CrossRef] [PubMed]
- Silveira, E.R.; Cademartori, M.G.; Schuch, H.S.; Armfield, J.A.; Demarco, F.F. Estimated prevalence of dental fear in adults: A systematic review and meta-analysis. J. Dent. 2021, 108, 103632. [Google Scholar] [CrossRef] [PubMed]
- Cianetti, S.; Lombardo, G.; Lupatelli, E.; Pagano, S.; Abraha, I.; Montedori, A.; Caruso, S.; Gatto, R.; De Giorgio, S. Dental fear/anxiety among children and adolescents. A systematic review. Eur. J. Paediatr. Dent. 2017, 18, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M. How do we measure dental fear and what are we measuring anyway? Oral. Health Prev. Dent. 2010, 8, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Thomson, W.M.; Broadbent, J.M.; Locker, D.; Poulton, R. Trajectories of dental anxiety in a Birth Cohort. Community Dent. Oral. Epidemiol. 2009, 37, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M.; Stewart, J.F.; Spencer, A.J. The vicious cycle of dental fear: Exploring the interplay between oral health, service utilization and dental fear. BMC Oral. Health 2007, 7, 1. [Google Scholar] [CrossRef]
- Armfield, J.M. What goes around comes around: Revisiting the hypothesized vicious cycle of dental fear and avoidance. Community Dent. Oral. Epidemiol. 2013, 41, 279–287. [Google Scholar] [CrossRef]
- Crego, A.; Carrillo-Diaz, M.; Armfield, J.M.; Romero, M. From public mental health to community oral health: The impact of dental anxiety and fear on dental status. Front. Public. Health 2014, 2, 16. [Google Scholar] [CrossRef]
- Grisolia, B.M.; Dos Santos, A.P.P.; Dhyppolito, I.M.; Buchanan, H.; Hill, K.; Oliveira, B.H. Prevalence of dental anxiety in children and adolescents globally: A systematic review with meta-analyses. Int. J. Paediatr. Dent. 2021, 31, 168–183. [Google Scholar] [CrossRef]
- Vasiliauskas, K.; Klasavičiūtė, K.; Vasiliauskienė, I.; Andruškevičienė, V.; Saldūnaitė, K.; Slabšinskienė, E. Indicators affecting dental fear in adults. Sveik. Moksl./Health Sci. East. Eur. 2018, 28, 69–73. (In Lithuanian) [Google Scholar]
- Murad, M.H.; Ingle, N.A.; Assery, M.K. Evaluating factors associated with fear and anxiety to dental treatment—A systematic review. J. Fam. Med. Prim. Care 2020, 9, 4530–4535. [Google Scholar] [CrossRef] [PubMed]
- Mohammed, R.B.; Lalithamma, T.; Varma, D.M.; Sudhakar, K.N.; Srinivas, B.; Krishnamraju, P.V.; Shaik, A.B. Prevalence of dental anxiety and its relation to age and gender in coastal Andhra (Visakhapatnam) population, India. J. Nat. Sci. Biol. Med. 2014, 5, 409–514. [Google Scholar] [CrossRef] [PubMed]
- Slabšinskienė, E.; Kavaliauskienė, A.; Žemaitienė, M.; Vasiliauskienė, I.; Zaborskis, A. Dental fear and associated factors among children and adolescents: A school-based study in Lithuania. Int. J. Environ. Res. Public. Health 2021, 18, 8883. [Google Scholar] [CrossRef] [PubMed]
- Thakur, S.; Kadam, H.; Jha, S.; Lall, A.; Kondreddy, K.; Singh, A. Assessment of anxiety associated with the dental treatments on the quality of life: An original research. J. Pharm. Bioall Sci. 2021, 13, S1713–S1716. [Google Scholar] [CrossRef] [PubMed]
- Muneer, M.U.; Ismail, F.; Munir, N.; Shakoor, A.; Das, G.; Ahmed, A.R.; Ahmed, M.A. Dental anxiety and influencing factors in adults. Healthcare 2022, 10, 2352. [Google Scholar] [CrossRef] [PubMed]
- Svensson, L.; Hakeberg, M.; Wideboman, U. Dental anxiety, concomitant factors and change in prevalence over 50 years. Community Dent. Health 2016, 33, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M. A comparison of three continuous scales used to determine the prevalence of clinically significant dental fear. Community Dent. Oral. Epidemiol. 2011, 39, 554–563. [Google Scholar] [CrossRef]
- Humphris, G.M.; Dyer, T.A.; Robinson, P.G. The modified dental anxiety scale: UK general public population norms in 2008 with further psychometrics and effects of age. BMC Oral Health 2009, 9, 20. [Google Scholar] [CrossRef]
- Locker, D.; Liddell, A.; Burman, D. Dental fear and anxiety in an older adult population. Community Dent. Oral. Epidemiol. 1991, 19, 120–124. [Google Scholar] [CrossRef]
- Locker, D.; Liddell, A.M. Correlates of dental anxiety among older adults. J. Dent. Res. 1991, 70, 198–203. [Google Scholar] [CrossRef]
- Hagglin, C.; Hakeberg, M.; Ahlqwist, M.; Sullivan, M.; Berggren, U. Factors associated with dental anxiety and attendance in middle-aged and elderly women. Community Dent. Oral. Epidemiol. 2000, 28, 451–460. [Google Scholar] [CrossRef] [PubMed]
- Lahti, S.; Vehkalahti, M.M.; Nordblad, A.; Hausen, H. Dental fear among population aged 30 years and older in Finland. Acta Odontol. Scand. 2007, 65, 97–102. [Google Scholar] [CrossRef] [PubMed]
- White, A.M.; Giblin, L.; Boyd, L.D. The prevalence of dental anxiety in dental practice settings. J. Dent. Hyg. 2017, 91, 30–34. [Google Scholar] [PubMed]
- Armfield, J.M.; Heaton, L.J. Management of fear and anxiety in the dental clinic: A review. Aust. Dent. J. 2013, 58, 390–407, quiz 531. [Google Scholar] [CrossRef] [PubMed]
- Badran, A.; Keraa, K.; Farghaly, M.M. The impact of oral health literacy on dental anxiety and utilization of oral health services among dental patients: A cross sectional study. BMC Oral. Health 2023, 23, 146. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, T.T. Evaluating the relationship of dental fear with dental health status and awareness. J. Clin. Diagn. Res. 2016, 10, Zc105–Zc109. [Google Scholar] [CrossRef] [PubMed]
- Jeddy, N.; Nithya, S.; Radhika, T.; Jeddy, N. Dental anxiety and influencing factors: A cross-sectional questionnaire-based survey. Indian. J. Dent. Res. 2018, 29, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Saatchi, M.; Abtahi, M.; Mohammadi, G.; Mirdamadi, M.; Binandeh, E.S. The prevalence of dental anxiety and fear in patients referred to Isfahan Dental School, Iran. Dent. Res. J. 2015, 12, 248–253. [Google Scholar]
- Xiang, B.; Wong, H.M.; Perfecto, A.P.; McGrath, C.P.J. The association of socio-economic status, dental anxiety, and behavioral and clinical variables with adolescents’ oral health-related quality of life. Qual. Life Res. 2020, 29, 2455–2464. [Google Scholar] [CrossRef]
- Singh, S.; Almulhim, B.; Alghamdi, S.; Alaasaf, A. Effect of age, gender and socioeconomic status on perceived dental anxiety. Rev. Argent. Clínica Psicol. 2021, 30, 525–530. [Google Scholar] [CrossRef]
- Chauvel, L.; Leist, A.K. Social Epidemiology. In International Encyclopedia of the Social & Behavioral Sciences, 2nd ed.; Wright, J.D., Ed.; Elsevier Ltd.: Amsterdam, The Netherlands, 2015; pp. 275–281. [Google Scholar] [CrossRef]
- Twenge, J.M.; Campbell, W.K. Self-esteem and socioeconomic status: A meta-analytic review. Personal. Soc. Psychol. Rev. 2002, 6, 59–71. [Google Scholar] [CrossRef]
- Alharbi, A. Dental anxiety, child-oral health-related quality of life and self-esteem in children and adolescents: A systematic review and meta-analysis. Commun. Dent. Health J. 2021, 38, 8. [Google Scholar] [CrossRef]
- Alharbi, A.; Humphris, G.; Freeman, R. The associations among dental anxiety, self-esteem, and oral health-related quality of life in children: A cross-sectional study. Dent. J. 2023, 11, 179. [Google Scholar] [CrossRef]
- Fernandes, B.; Newton, J.; Essau, C.A. The mediating effects of self-esteem on anxiety and emotion regulation. Psychol. Rep. 2022, 125, 787–803. [Google Scholar] [CrossRef]
- Sowislo, J.F.; Orth, U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol. Bull. 2013, 139, 213–240. [Google Scholar] [CrossRef]
- Locker, D. Psychosocial consequences of dental fear and anxiety. Community Dent. Oral. Epidemiol. 2003, 31, 144–151. [Google Scholar] [CrossRef]
- Doron, J.; Thomas-Ollivier, V.; Vachon, H.; Fortes-Bourbousson, M. Relationships between cognitive coping, self-esteem, anxiety and depression: A cluster-analysis approach. Pers. Individ. Differ. 2013, 55, 515–520. [Google Scholar] [CrossRef]
- Guil, R.; Gómez-Molinero, R.; Merchan-Clavellino, A.; Gil-Olarte, P.; Zayas, A. Facing anxiety, growing up. Trait emotional intelligence as a mediator of the relationship between self-esteem and university anxiety. Front. Psychol. 2019, 10, 567. [Google Scholar] [CrossRef]
- Manna, G.; Giorgio, F.; Sonia, I.; Como, M.R.; De Santis, S. The relationship between self-esteem, depression and anxiety: Comparing vulnerability and scar model in the italian context. Mediterr. J. Clin. Psychol. 2016, 4, 1–16. [Google Scholar] [CrossRef]
- Kankaala, T.; Laine, H.; Laitala, M.L.; Rajavaara, P.; Vähänikkilä, H.; Pesonen, P.; Anttonen, V. 10-year follow-up study on attendance pattern after dental treatment in primary oral health care clinic for fearful patients. BMC Oral. Health 2021, 21, 522. [Google Scholar] [CrossRef] [PubMed]
- Furgała, D.; Markowicz, K.; Koczor-Rozmus, A.; Zawilska, A. Causes and severity of dentophobia in Polish adults—A Questionnaire Study. Healthcare 2021, 9, 819. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Zhang, Y.Y.; Xiang, B.; Peng, S.M.; Gu, M.; Wong, H.M. Management of fear and anxiety in dental treatments: A systematic review and meta-analysis of randomized controlled trials. Odontology 2023, 111, 20–32. [Google Scholar] [CrossRef] [PubMed]
- Stienen, M.N.; Scholtes, F.; Samuel, R.; Weil, A.; Weyerbrock, A.; Surbeck, W. Different but similar: Personality traits of surgeons and internists—Results of a cross-sectional observational study. BMJ Open 2018, 8, e021310. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, F.; Ertl, B. Big Five personality trait differences between students from different majors aspiring to the teaching profession. Curr. Psychol. 2023, 42, 12070–12086. [Google Scholar] [CrossRef]
- Afhami, R.; Mohammadi-Zarghan, S. The Big Five, aesthetic judgment styles, and art interest. Eur. J. Psychol. 2018, 14, 764–775. [Google Scholar] [CrossRef] [PubMed]
- Aarabi, G.; Walther, C.; Bunte, K.; Spinler, K.; Buczak-Stec, E.; König, H.-H.; Hajek, A. The Big Five personality traits and regularity of lifetime dental visit attendance: Evidence of the Survey of Health, Ageing, and Retirement in Europe. Aging Clin. Exp. Res. 2022, 34, 1439–1445. [Google Scholar] [CrossRef] [PubMed]
- Nicolas, E.; Collado, V.; Faulks, D.; Bullier, B.; Hennequin, M. A national cross-sectional survey of dental anxiety in the French adult population. BMC Oral. Health 2007, 7, 12. [Google Scholar] [CrossRef] [PubMed]
- Akiskal, K.K.; Savino, M.; Akiskal, H.S. Temperament profiles in physicians, lawyers, managers, industrialists, architects, journalists, and artists: A study in psychiatric outpatients. J. Affect. Disord. 2005, 85, 201–206. [Google Scholar] [CrossRef] [PubMed]
- G*Power 3.1 Manual. Die Heinrich Heine Universitӓt, Düsseldorf, Germany. 2020. Available online: http://www.gpower.hhu.de/fileadmin/redaktion/Fakultaeten/Mathematisch-Naturwissenschaftliche_Fakultaet/Psychologie/AAP/gpower/GPowerManual.pdf. (accessed on 24 February 2024).
- Corah, N.L. Development of dental anxiety scale. J. Dent. Res. 1969, 48, 596. [Google Scholar] [CrossRef]
- Corah, N.L.; Gale, E.N.; Illig, S.J. Assessment of a dental anxiety scale. J. Am. Dent. Assoc. 1978, 97, 816–819. [Google Scholar] [CrossRef]
- Kleinknecht, R.A.; Klepac, R.K.; Alexander, L.D. Origins and characteristics of fear of dentistry. J. Am. Dent. Assoc. 1973, 86, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Kleinknecht, R.A.; Bernstein, D.A. Assessment of dental fear. Behav. Ther. 1978, 9, 626–634. [Google Scholar] [CrossRef]
- Newton, J.T.; Buck, D.J. Anxiety and pain measures in dentistry: A guide to their quality and application. J. Am. Dent. Assoc. 2000, 131, 1449–1457. [Google Scholar] [CrossRef] [PubMed]
- Račienė, R. Moksleivių Dantų Gydymo Baimė ir su ja Susiję Socialiniai Bei Psichologiniai Veiksniai (Schoolchildren’s Fear of Dental Treatment and Related Social and Psychological Factors). Ph.D. Dissertation, Kauno Medicinos Universitetas, Kaunas, Lithuania, 2009. (In Lithuanian). [Google Scholar]
- Hakeberg, M.; Berggren, U. Dimensions of the Dental Fear Survey among patients with dental phobia. Acta Odontol. Scand. 1997, 55, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Venckutė, R. Rosenbergo Savigarbos Skalė. [Rosenberg‘s Self-Esteem Scale]. 2012. Available online: https://psichika.eu/blog/testas-rosenbergo-savigarbos-skale/ (accessed on 24 February 2024).
- Čekanavičius, V.; Murauskas, G. Statistika ir Jos Taikymai (Statistics and Its Applications), 3 Knyga; REV UAB BĮ: Vilnius, Lithuania, 2009. (In Lithuanian) [Google Scholar]
- Arbuckle, J.L. IBM SPSS AMOS 21 User’s Guide; Amos Development Corporation: New York, NY, USA, 2012. [Google Scholar]
- Hooper, D.; Caughlan, J.; Mullen, M.R. Structural equation modeling: Guidelines for determining model fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar] [CrossRef]
- Xia, Y.; Yang, Y. RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: The story they tell depends on the estimation methods. Behav. Res. Methods 2019, 51, 409–428. [Google Scholar] [CrossRef] [PubMed]
- Chi, S.I. What is the gold standard of the dental anxiety scale? J. Dent. Anesth. Pain. Med. 2023, 23, 193–212. [Google Scholar] [CrossRef] [PubMed]
- Noda, S.; Nishiuchi, M.; Shirotsukim, K. Awareness and acceptance in anxiety-provoking social situations and social anxiety: Development and initial validation of the social anxiety-awareness and acceptance scale. Jpn. Psychol. Res. 2023. Online Version. [Google Scholar] [CrossRef]
- Yildirim, T.T.; Dundar, S.; Bozoglan, A.; Karaman, T.; Dildes, N.; Acun Kaya, F.; Alan, H. Is there a relation between dental anxiety, fear and general psychological status? Peer J. 2017, 5, e2978. [Google Scholar] [CrossRef] [PubMed]
- Bourne, E.J. The Anxiety and Phobia Workbook, 7th ed.; New Harbinger Publications, Inc.: Oakland, CA, USA, 2020. [Google Scholar]
- Kyaga, S.; Landén, M.; Boman, M.; Hultman, C.M.; Långström, N.; Lichtenstein, P. Mental illness, suicide and creativity: 40-year prospective total population study. J. Psychiatry Res. 2013, 47, 83–90. [Google Scholar] [CrossRef]
- Armfield, J.; Spencer, A.; Stewart, J. Dental fear in Australia: Who’s afraid of the dentist? Aust. Dent. J. 2006, 51, 78–85. [Google Scholar] [CrossRef]
- Skaret, E.; Kvale, G.; Raadal, M. General self-efficacy, dental anxiety and multiple fears among 20-year-olds in Norway. Scand. J. Psychol. 2003, 44, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Kaur, P.; Singh, S.; Mathur, A.; Makkar, D.K.; Aggarwal, V.P.; Batra, M.; Sharma, A.; Goyal, N. Impact of dental disorders and its influence on self esteem levels among adolescents. J. Clin. Diagn. Res. 2017, 11, ZC05–ZC08. [Google Scholar] [CrossRef] [PubMed]
- How Oral Problems Affect Our Self-Esteem. Australian & New Zealand Mental Health Association. 2023. Available online: https://anzmh.asn.au/blog/how-oral-problems-affect-your-self-esteem (accessed on 6 February 2024).
- Abun, D.; Nicolas, M.T.; Apollo, E.; Magallanes, T.; Encarnacion, M.J. Employees’ self-efficacy and work performance of employees as mediated by work environment. Int. J. Res. Bus. Soc. Sci. 2021, 10, 1–15. [Google Scholar] [CrossRef]
- Erten, H.; Akarslan, Z.Z.; Bodrumlu, E. Dental fear and anxiety levels of patients attending a dental clinic. Quintessence Int. 2006, 37, 304–310. [Google Scholar] [PubMed]
- Do Nascimento, D.L.; da Silva Araújo, A.C.; Gusmão, E.S.; Cimões, R. Anxiety and fear of dental treatment among users of public health services. Oral. Health Prev. Dent. 2011, 9, 329–337. [Google Scholar] [PubMed]
- Milgrom, P.; Newton, J.T.; Boyle, C.; Heaton, L.J.; Donaldson, N. The effects of dental anxiety and irregular attendance on referral for dental treatment under sedation within the National Health Service in London. Community Dent. Oral. Epidemiol. 2010, 38, 453–459. [Google Scholar] [CrossRef] [PubMed]
- Vigu, A.; Stanciu, D. When the fear of dentist is relevant for more than one’s oral health. A structural equation model of dental fear, self-esteem, oral-health-related well-being, and general well-being. Patient Prefer. Adherence 2019, 13, 1229–1240. [Google Scholar] [CrossRef]
- Armfield, J.M. Predicting dental avoidance among dentally fearful Australian adults. Eur. J. Oral. Sci. 2013, 121, 240–246. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Conrad, F. Speeding in web surveys: The tendency to answer very fast and its association with straightlining. Surv. Res. Methods 2014, 8, 127–135. [Google Scholar] [CrossRef]
- Lindberg, P.; Vingard, E. Indicators of healthy work environments-a systematic review. Work 2012, 41 (Suppl. S1), 3032–3038. [Google Scholar] [CrossRef]


| Characteristics | Physicians | Teachers | Industry Workers | Artists | Total | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | ||
| Gender: | |||||||||||
| Males | 6 | (5.7 *) | 2 | (1.9 *) | 33 | (31.4 +) | 32 | (30.2 +) | 73 | (17.3) | <0.001 c |
| Females | 99 | (94.3 *) | 104 | (98.1 *) | 72 | (68.6 +) | 74 | (69.8 +) | 349 | (82.7) | |
| Age: | |||||||||||
| Mean (SE) | 37.4 * | (1.18) | 47.5 + | (1.05) | 36.6 * | (1.20) | 33.7 * | (1.17) | 38.8 | (0.63) | <0.001 b |
| ≤40 years | 64 | (61.0 *) | 24 | (22.6 +) | 70 | (66.7 *) | 79 | (74.5 *) | 237 | (56.2) | <0.001 c |
| >40 years | 41 | (39.0 *) | 82 | (77.4 +) | 35 | (33.3 *) | 27 | (25.5 *) | 185 | (43.8) | |
| Education: | |||||||||||
| Less than higher | 0 | (0 *) | 3 | (2.8 *) | 51 | (48.6 +) | 29 | (27.4 °) | 83 | (19.7) | <0.001 c |
| Higher | 105 | (100 *) | 103 | (97.2 *) | 54 | (51.4 +) | 77 | (72.6 °) | 339 | (80.3) | |
| Marital status: | |||||||||||
| Married | 59 | (56.2 *) | 72 | (67.9 *) | 50 | (47.6 +) | 27 | (25.5 °) | 208 | (49.3) | <0.001 c |
| Unmarried | 46 | (43.8 *) | 34 | (32.1 *) | 55 | (52.4 +) | 79 | (74.5 °) | 214 | (50.7) | |
| Personal income: | |||||||||||
| ≤900 EUR/month | 30 | (28.6 *) | 49 | (46.2 +) | 51 | (48.6 +) | 72 | (67.9 °) | 202 | (47.9) | <0.001 c |
| >900 EUR/month | 75 | (71.4 *) | 57 | (53.8 +) | 54 | (51.4 +) | 34 | (32.1 °) | 220 | (52.1) | |
| Characteristics | Physicians | Teachers | Industry Workers | Artists | Total | p-Value b | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | ||
| V1: Frequency of visits to the dentist: | |||||||||||
| Once a year or more often | 67 | (63.8) | 52 | (49.1) | 51 | (48.6) | 50 | (47.2) | 220 | (52.1) | 0.052 |
| Less often | 38 | (36.2) | 54 | (50.9) | 54 | (51.4) | 56 | (52.8) | 202 | (47.9) | |
| V2: Decayed teeth in need of treatment: | |||||||||||
| Yes | 23 | (21.9 *) | 30 | (28.3) | 37 | (35.2) | 46 | (43.4 +) | 136 | (32.2) | 0.006 |
| No/does not know | 82 | (78.1 *) | 76 | (71.7) | 68 | (64.8) | 60 | (56.6 +) | 286 | (67.8) | |
| V3: Ever had a toothache: | |||||||||||
| Yes | 88 | (83.0 *) | 101 | (95.3 +) | 100 | (95.2 +) | 104 | (98.1 +) | 393 | (92.9) | <0.001 |
| No | 18 | (17.0 *) | 5 | (4.7 +) | 5 | (4.8 +) | 2 | (1.9 +) | 30 | (7.1) | |
| V4: Satisfied with the state of the teeth: | |||||||||||
| Yes | 73 | (69.5 *) | 60 | (56.6 *) | 66 | (62.9 *) | 43 | (40.6 +) | 242 | (57.3) | <0.001 |
| No | 32 | (30.5 *) | 46 | (43.4 *) | 39 | (37.1 *) | 63 | (59.4 +) | 180 | (42.7) | |
| V5: Had an unpleasant experience at the dentist’s office: | |||||||||||
| Yes | 76 | (72.4) | 66 | (62.3 *) | 62 | (59.0 *) | 84 | (79.2 +) | 288 | (68.2) | 0.006 |
| No | 29 | (27.6) | 40 | (37.7 *) | 43 | (41.0 *) | 22 | (20.8 +) | 134 | (31.8) | |
| V6: Would like dental treatment procedures to be performed under sedation: | |||||||||||
| Yes | 19 | (18.1 *) | 19 | (17.9 *) | 40 | (38.1 +) | 44 | (41.5 +) | 122 | (28.9) | <0.001 |
| No | 86 | (81.9 *) | 87 | (82.1 *) | 65 | (61.9 +) | 62 | (58.5 +) | 300 | (71.1) | |
| Measures | Physicians | Teachers | Industry Workers | Artists | Total | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dental Anxiety Scale (DAS): | |||||||||||
| Mean (SE) | 9.29 * | (0.39) | 9.51 | (0.29) | 10.13 | (0.37) | 10.74 + | (0.38) | 9.92 | (0.18) | 0.020 b |
| <10 scores, n (%) | 69 | (65.7 *) | 64 | (60.4) | 58 | (55.2) | 50 | (47.2 +) | 241 | (57.1) | 0.045 c |
| ≥10 scores, n (%) | 36 | (34.3 *) | 42 | (39.6) | 47 | (44.8) | 56 | (52.8 +) | 181 | (42.9) | |
| Dental Fear Survey (DFS-1): | |||||||||||
| Mean (SE) | 14.67 * | (0.63) | 14.79 * | (0.54) | 15.46 | (0.61) | 17.19 + | (0.71) | 15.53 | (0.31) | 0.016 b |
| <14 scores, n (%) | 62 | (59.0 *) | 55 | (51.9) | 55 | (52.4) | 43 | (40.6 +) | 215 | (50.9) | 0.059 c |
| ≥14 scores, n (%) | 43 | (41.0 *) | 51 | (48.1) | 50 | (47.6) | 63 | (59.4 +) | 207 | (49.1) | |
| Dental Fear Survey (DFS-2): | |||||||||||
| Mean (SE) | 33.94 * | (1.69) | 32.89 * | (1.38) | 36.58 | (1.87) | 41.34 + | (1.92) | 36.19 | (0.88) | 0.003 b |
| <30 scores, n (%) | 58 | (55.2 *) | 50 | (47.2) | 54 | (51.4) | 39 | (36.8 +) | 201 | (47.6) | 0.045 c |
| ≥30 scores, n (%) | 47 | (44.8 *) | 56 | (52.8) | 51 | (48.6) | 67 | (63.2 +) | 221 | (52.4) | |
| Estimates | Physicians | Teachers | Industry Workers | Artists | Entire Sample | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| β/r | p | β/r | p | β/r | p | β/r | p | β/r | p | |
| Standardized regression coefficients: | ||||||||||
| DAS ← DFA | 0.61 | <0.001 | 0.70 | <0.001 | 0.79 | <0.001 | 0.83 | <0.001 | 0.74 | <0.001 |
| DFS−1 ← DFA | 0.57 | <0.001 | 0.84 | <0.001 | 0.92 | <0.001 | 0.92 | <0.001 | 0.81 | <0.001 |
| DFS−2 ← DFA a | 0.59 | 0.73 | 0.57 | 0.72 | 0.72 | |||||
| DFA ← Age | −0.47 | <0.001 | 0.03 | 0.762 | −0.03 | 0.777 | −0.29 | 0.020 | −0.17 | 0.005 |
| DFA ← Marital status | −0.31 | 0.002 | −0.22 | 0.032 | −0.12 | 0.264 | 0.14 | 0.272 | −0.09 | 0.136 |
| DFA ← Personal income | 0.12 | 0.189 | 0.12 | 0.250 | −0.26 | 0.056 | 0.32 | 0.011 | 0.01 | 0.848 |
| DFA ← Self−esteem | 0.23 | 0.015 | 0.42 | <0.001 | 0.03 | 0.780 | 0.40 | 0.002 | 0.24 | <0.001 |
| Self−esteem ← Age | −0.14 | 0.082 | −0.04 | 0.664 | −0.27 | 0.010 | 0.06 | 0.629 | −0.08 | 0.118 |
| Self−esteem ← Marital status | 0.08 | 0.310 | −0.04 | 0.713 | 0.11 | 0.244 | 0.34 | 0.011 | 0.08 | 0.119 |
| Self−esteem ← Personal income | −0.21 | 0.007 | −0.10 | 0.304 | −0.49 | <0.001 | 0.12 | 0.357 | −0.19 | <0.001 |
| V1 ← DFA | 0.43 | <0.001 | 0.35 | 0.003 | 0.13 | 0.236 | 0.24 | 0.084 | 0.23 | <0.001 |
| V2 ← DFA | −0.45 | <0.001 | −0.61 | <0.001 | −0.21 | 0.089 | −0.14 | 0.285 | −0.37 | <0.001 |
| V4 ← DFA | 0.67 | <0.001 | 0.37 | 0.002 | 0.25 | 0.063 | 0.16 | 0.223 | 0.39 | <0.001 |
| V5 ← DFA | −0.18 | 0.062 | −0.17 | 0.122 | −0.51 | 0.009 | −0.50 | <0.001 | −0.31 | <0.001 |
| V6 ← DFA | −0.42 | <0.001 | −0.43 | <0.001 | −0.39 | 0.018 | −0.82 | <0.001 | −0.56 | <0.001 |
| Pearson’s correlation coefficients: | ||||||||||
| Marital status ↔ Personal income | 0.01 | 0.938 | −0.13 | 0.185 | 0.14 | 0.176 | −0.31 | 0.009 | −0.07 | 0.165 |
| Personal income ↔ Age | 0.19 | 0.015 | 0.23 | 0.015 | −0.41 | <0.001 | 0.21 | 0.086 | 0.06 | 0.188 |
| Marital status ↔ Age | −0.27 | <0.001 | −0.12 | 0.219 | −0.26 | 0.012 | −0.32 | 0.012 | −0.31 | <0.001 |
| eDFS−1 ↔ eDFS−2 | 0.71 | <0.001 | 0.60 | 0.033 | 0.85 | <0.001 | 0.17 | 0.592 | 0.52 | 0.003 |
| eDAS ↔ eDFS−1 | 0.73 | <0.001 | 0.57 | 0.033 | 0.32 | 0.695 | 0.24 | 0.555 | 0.54 | 0.003 |
| eDAS ↔ eDFS−2 | 0.77 | <0.001 | 0.51 | 0.015 | 0.77 | 0.027 | 0.61 | 0.020 | 0.64 | <0.001 |
| eV2 ↔ eV4 b | −0.22 | 0.049 | −0.11 | 0.324 | −0.70 | <0.001 | −0.71 | <0.001 | −0.45 | <0.001 |
| eV6 ↔ Marital status b | −0.24 | <0.001 | −0.21 | <0.001 | ||||||
| eV4 ↔ Age b | 0.31 | 0.002 | ||||||||
| eV1 ↔ eV2 b | 0.41 | <0.001 | ||||||||
| eV4 ↔ Personal income b | 0.27 | 0.006 | ||||||||
| eV5 ↔ Marital status b | 0.29 | 0.021 | ||||||||
| Model | Constraints | Difference in df | Difference in Chi-Squared | p-Value |
|---|---|---|---|---|
| Model 1 | DFA loadings to DAS, DFS, and DBS; V1 to V6 are constant across occupational groups | 21 | 53.75 | <0.001 |
| Model 2 | All of the above, and intercepts in the equations for predicting measured variables of DFA, are constant across occupational groups | 42 | 101.61 | <0.001 |
| Model 3 | All the above, and the regression weights for predicting self-esteem and DFA by socio-demographic variables, are constant across occupational groups | 63 | 160.82 | <0.001 |
| Model 4 | All the above, and intercepts in the equations for predicting self-esteem and DFA by sociodemographic variables, are constant across occupational groups | 69 | 177.38 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Slabšinskienė, E.; Radlinskaitė, K.; Kavaliauskienė, A.; Vasiliauskienė, I.; Zūbienė, J.; Saldūnaitė-Mikučionienė, K.; Zaborskis, A. Do Subjects from Different Occupational Groups Experience Dental Fear and Anxiety Equally? Medicina 2024, 60, 674. https://doi.org/10.3390/medicina60040674
Slabšinskienė E, Radlinskaitė K, Kavaliauskienė A, Vasiliauskienė I, Zūbienė J, Saldūnaitė-Mikučionienė K, Zaborskis A. Do Subjects from Different Occupational Groups Experience Dental Fear and Anxiety Equally? Medicina. 2024; 60(4):674. https://doi.org/10.3390/medicina60040674
Chicago/Turabian StyleSlabšinskienė, Eglė, Karolina Radlinskaitė, Aistė Kavaliauskienė, Ingrida Vasiliauskienė, Jūratė Zūbienė, Kristina Saldūnaitė-Mikučionienė, and Apolinaras Zaborskis. 2024. "Do Subjects from Different Occupational Groups Experience Dental Fear and Anxiety Equally?" Medicina 60, no. 4: 674. https://doi.org/10.3390/medicina60040674