Plasma Amino Acid Abnormalities in Chronic Heart Failure. Mechanisms, Potential Risks and Targets in Human Myocardium Metabolism
Abstract
:1. Introduction
2. Methods
2.1. Study Population
2.2. Protocol Procedures
2.2.1. Cardiac Catheterization
2.2.2. Pro-B-Type Natriuretic Peptide (NT-Pro-BNP)
2.2.3. Arterial Amino Acid Concentrations
2.2.4. Nutritional Intakes
2.2.5. Resting Energy Expenditure (REE)
2.2.6. Estimation of Calorie-Protein Adequacy
2.2.7. Double Product
2.2.8. Anthropometrics
2.3. Statistical Analysis
3. Results
3.1. Arterial Amino Acids
3.2. Energy Expenditure and Adequate Nutrition
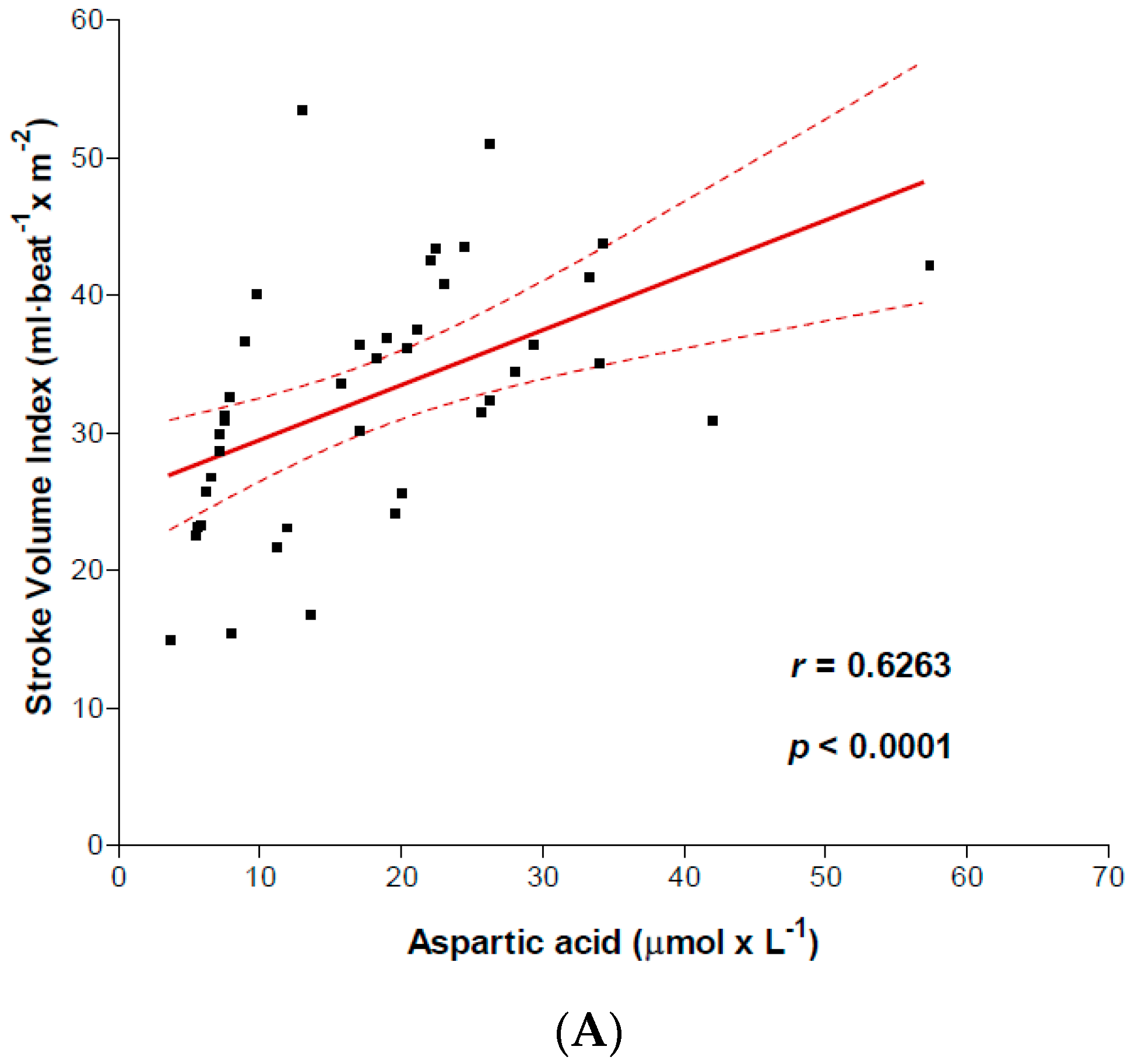
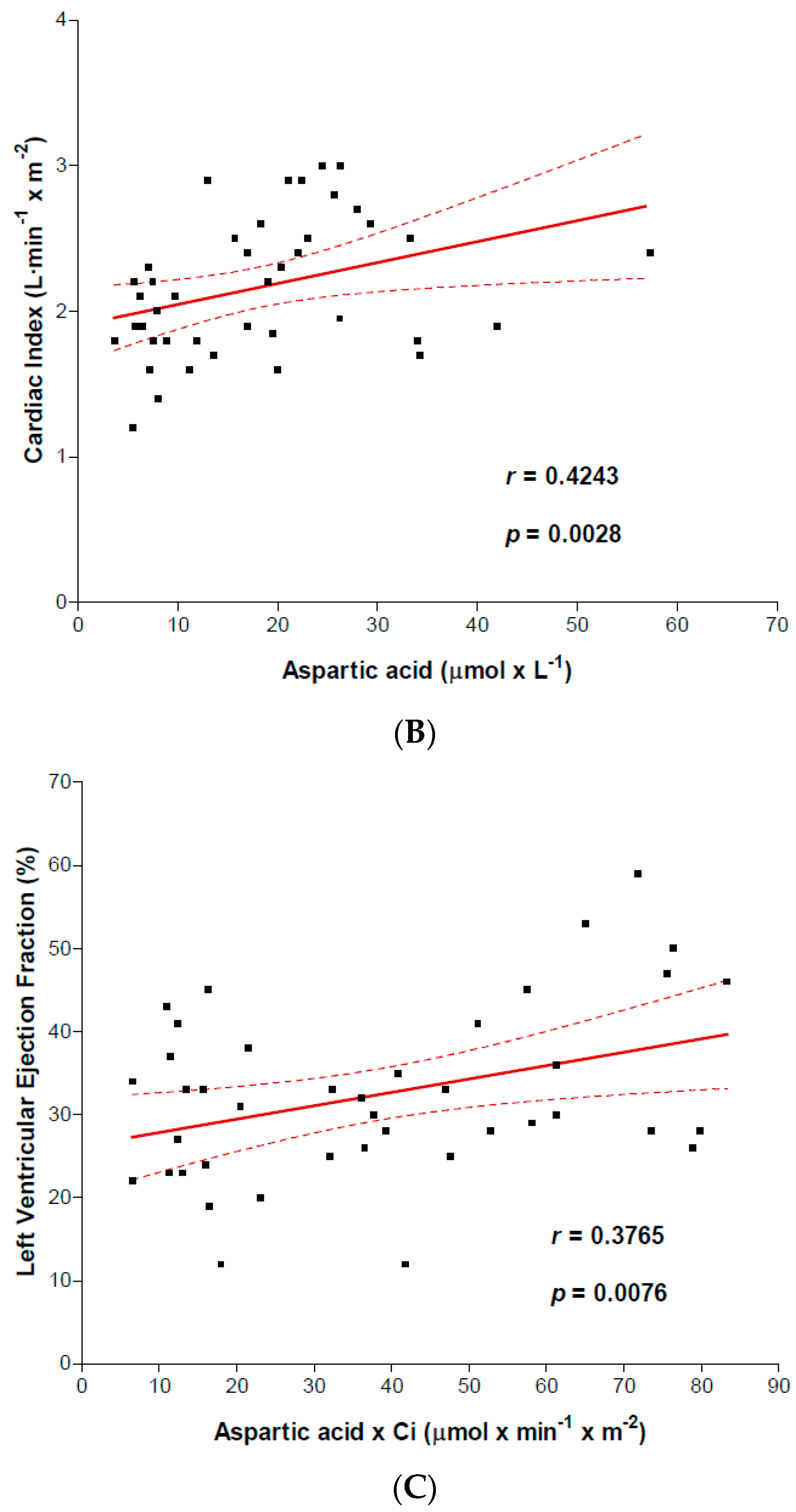
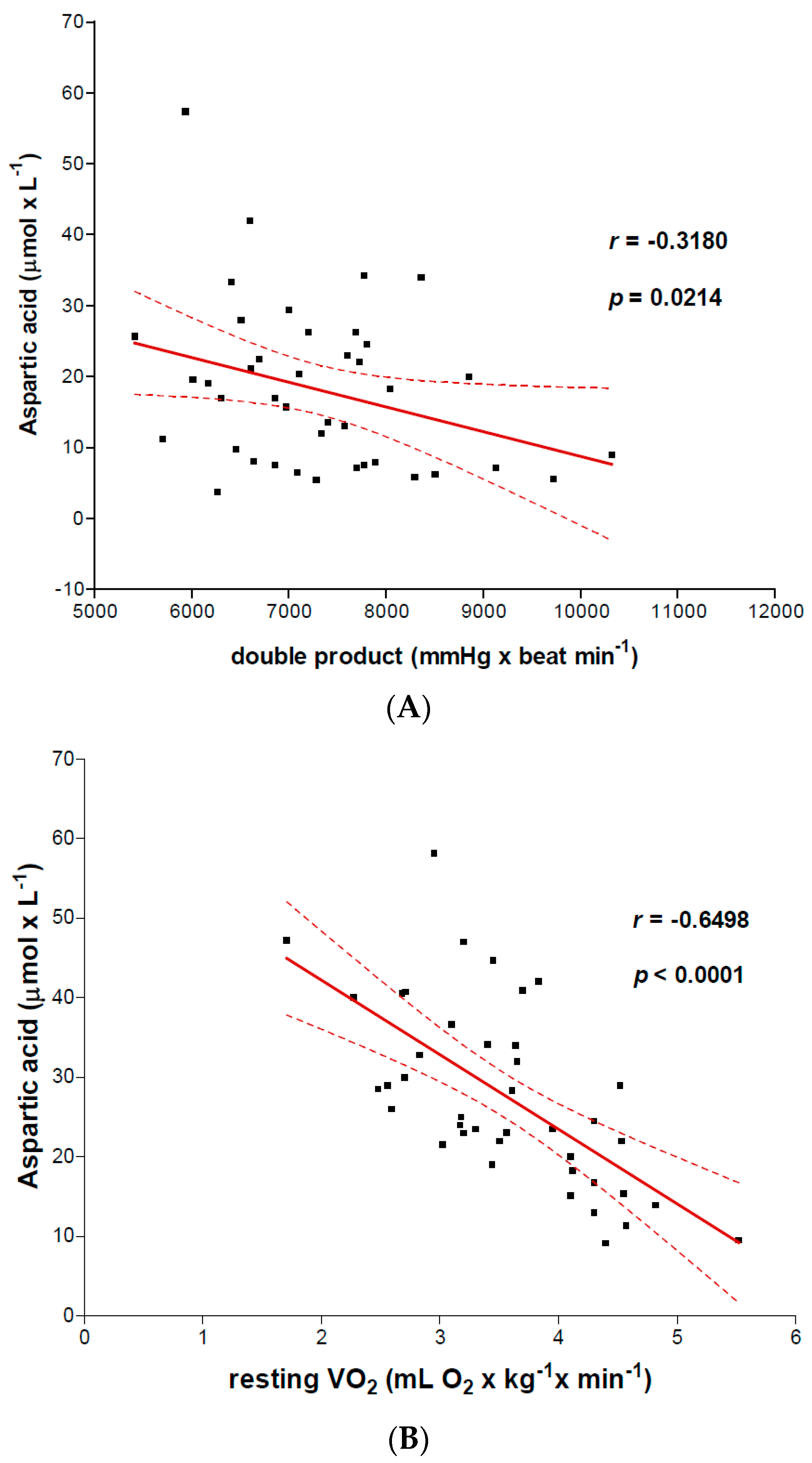
3.3. Relation between Arterial Amino Acid Levels and Left Ventricular (LV) Function
4. Discussion
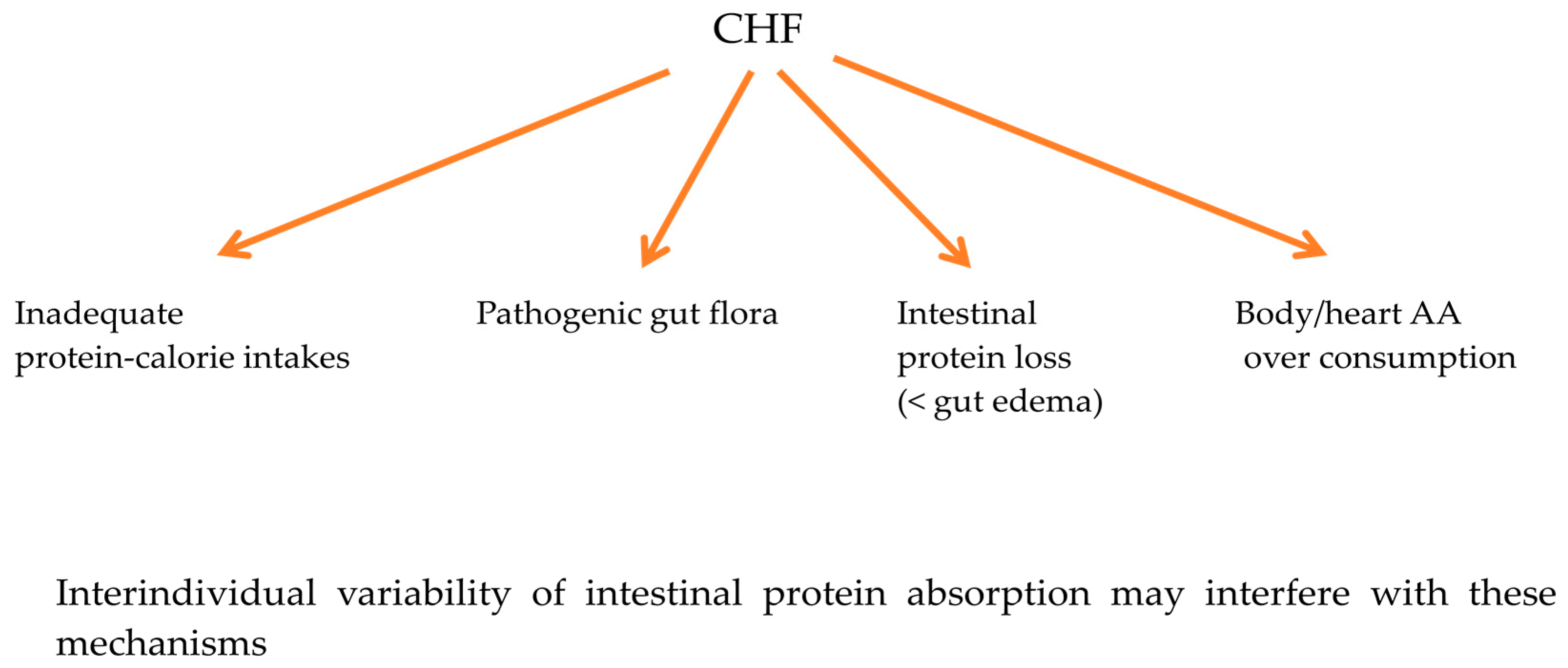
4.1. Mechanisms Underlying Low Arterial AAs
4.2. Risk of Low Arterial AAs on Myocardial Energetics
4.3. Risk of Low Arterial AAs on Heart Oxidative Stress
4.4. Risk of Low Arterial AAs on Heart Protein Metabolism Remodelling
5. Limitations of This Study
6. Future Directions for Clinical Practice
- The intake of protein with high biological value providing adequate amounts of EAAs should be ensured in CHF patients and mandatory in NYHA class IV patients. If these proteins are not adequately ingested, a supplementation with physiological doses of EAAs (7–8 g/die) can compensate for deficient intake of an individual serving of protein with high biological value; for example 7–8 g of free essential amino acids are the equivalent to the amount of EAAs contained in 500 mL of milk.Protein ingestion should be supplemented with free essential amino acids in subjects in IV NYHA class association, particularly during the metabolic recovery after acute decompensation. Normal protein intake requires too much time to restore reduced circulating amino acids.
- Given the mutual influence between inflammation and oxidative stress, patient selection of food with anti-inflammatory and antioxidant properties could be useful for CHF patients from II to IV NYHA classes.Oatmeal, milk, orange juice and raisins may all prevent postprandial endotoxemia [51] as well as a rise in various markers of oxidative stress. Orange juice neutralizes [52] the pro-inflammatory effect of high fat, high carbohydrate intakes, typical of western diet. High amounts of cystin and methionine are contained in wheat, toasted peanuts, red meat, rabbit, sardines, egg and chicken. Fruits, vegetables, tea and wine contain flavonoid antioxidants (quercetin, myricetin, apicetin and luteolin). The intake of the potent antioxidant vitamins (A, C and E) as well as enzymin factors (zinc, selenium and copper), should be recommended in all CHF subjects.
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Bing, R.J.; Siegel, A.; Ungar, I.; Gilbert, M. Metabolism of the human heart: II. Studies on fat, ketone and amino acid metabolism. Am. J. Med. 1954, 16, 504–515. [Google Scholar] [CrossRef]
- Morgan, H.E.; Earl, D.C.; Broadus, A.; Wolpert, E.B.; Giger, K.E.; Jefferson, L.S. Regulation of protein synthesis in heart muscle I. Effect of amino acid levels on protein synthesis. J. Biol. Chem. 1971, 246, 2152–2162. [Google Scholar]
- Young, L.H.; McNulty, P.H.; Morgan, C.; Deckelbaum, L.I.; Zaret, B.L.; Barrett, E.J. Myocardial protein turnover in patients with coronary artery disease. Effect of branched chain amino acid infusion. J. Clin. Investig. 1991, 87, 554–560. [Google Scholar] [CrossRef]
- Martin, A.F. Turnover of cardiac troponin subunits. Kinetic evidence for a precursor pool of troponin-I. J. Biol. Chem. 1981, 256, 964–968. [Google Scholar]
- Davis, E.J.; Bremer, J. Studies with isolated surviving rat hearts. Interdependence of free amino acids and citric-acid-cycle intermediates. Eur. J. Biochem. 1973, 38, 86–97. [Google Scholar] [CrossRef]
- Burns, A.H.; Reddy, W.J. Amino acid stimulation of oxygen and substrate utilization by cardiac myocytes. Am. J. Physiol. 1978, 235, E461–E466. [Google Scholar]
- Rosenkranz, E.R.; Okamoto, F.; Buckberg, G.D.; Robertson, J.M.; Vinten-Johansen, J.; Bugyi, H.I. Safety of prolonged aortic clamping with blood cardioplegia. III. Aspartate enrichment of glutamate-blood cardioplegia in energy-depleted hearts after ischemic and reperfusion injury. J. Thorac. Cardiovasc. Surg. 1986, 91, 428–435. [Google Scholar]
- Barrio, J.R.; Egbert, J.E.; Henze, E.; Schelbert, H.R.; Baumgartner, F.J. L-[4-11C]aspartic acid: Enzymatic synthesis, myocardial uptake, and metabolism. J. Med. Chem. 1982, 25, 93–96. [Google Scholar] [CrossRef]
- Neubauer, S.; Horn, M.; Cramer, M.; Harre, K.; Newell, J.B.; Peters, W.; Pabst, T.; Ertl, G.; Hahn, D.; Ingwall, J.S.; et al. Myocardial phosphocreatine-to-ATP ratio is a predictor of mortality in patients with dilated cardiomyopathy. Circulation 1997, 96, 2190–2196. [Google Scholar] [CrossRef]
- Chua, B.; Siehl, D.L.; Morgan, H.E. Effect of leucine and metabolites of branched chain amino acids on protein turnover in heart. J. Biol. Chem. 1979, 254, 8358–8362. [Google Scholar]
- Stanley, W.C.; Recchia, F.A.; Lopaschuk, G.D. Myocardial substrate metabolism in the normal and failing heart. Physiol. Rev. 2005, 85, 1093–1129. [Google Scholar] [CrossRef] [PubMed]
- Schisler, J.C.; Grevengoed, T.J.; Pascual, F.; Cooper, D.E.; Ellis, J.M.; Paul, D.S.; Willis, M.S.; Patterson, C.; Jia, W.; Coleman, R.A. Cardiac energy dependence on glucose increases metabolites related to glutathione and activates metabolic genes controlled by mechanistic target of rapamycin. J. Am. Heart Assoc. 2015, 4. [Google Scholar] [CrossRef] [PubMed]
- Lai, L.; Leone, T.C.; Keller, M.P.; Martin, O.J.; Broman, A.T.; Nigro, J.; Kapoor, K.; Koves, T.R.; Stevens, R.; Ilkayeva, O.R.; et al. Energy metabolic reprogramming in the hypertrophied and early stage failing heart: A multisystems approach. Circ. Heart Fail. 2014, 7, 1022–1031. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, R.G.; Barret, E.J.; Francis, C.K.; Jacob, R.; Zaret, B.L. Regulation of myocardial amino acid balance in the conscious dog. J. Clin. Investig. 1985, 75, 1204–1211. [Google Scholar] [CrossRef] [PubMed]
- Chess, D.J.; Stanley, W.C. Role of diet and fuel overabundance in the development and progression of heart failure. Cardiovasc. Res. 2008, 79, 269–278. [Google Scholar] [CrossRef] [PubMed]
- McNulty, P.H.; Louard, R.J.; Deckelbaum, L.I.; Zaret, B.L.; Young, L.H. Hyperinsulinemia inhibits myocardial protein degradation in patients with cardiovascular disease and insulin resistance. Circulation 1995, 92, 2151–2156. [Google Scholar] [CrossRef] [PubMed]
- Aquilani, R.; Opasich, C.; Verri, M.; Boschi, F.; Febo, O.; Pasini, E.; Pastoris, O. Is nutritional intake adequate in chronic heart failure patients? J. Am. Coll. Cardiol. 2003, 42, 1218–1223. [Google Scholar] [CrossRef]
- Frey, N.; Olson, E.N. Cardiac hypertrophy: The good, the bad, and the ugly. Annu. Rev. Physiol. 2003, 65, 45–79. [Google Scholar] [CrossRef] [PubMed]
- Aquilani, R.; La Rovere, M.T.; Febo, O.; Baiardi, P.; Boschi, F.; Iadarola, P.; Viglio, S.; Dossena, M.; Bongiorno, A.I.; Pastoris, O.; et al. Lung anabolic activity in patients with chronic heart failure: Potential implications for clinical practice. Nutrition 2012, 28, 1002–1007. [Google Scholar] [CrossRef] [PubMed]
- Pasini, E.; Aquilani, R.; Testa, C.; Baiardi, P.; Angioletti, S.; Boschi, F.; Verri, M.; Dioguardi, F. Pathogenic gut flora in patients with chronic heart failure. JACC Heart Fail. 2016, 4, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Aquilani, R.; La Rovere, M.T.; Febo, O.; Boschi, F.; Iadarola, P.; Corbellini, D.; Viglio, S.; Bongiorno, A.I.; Pastoris, O.; Verri, M. Preserved muscle protein metabolism in obese patients with chronic heart failure. Int. J. Cardiol. 2012, 160, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Aquilani, R.; Iadarola, P.; Boschi, F.; Pistarini, C.; Arcidiaco, P.; Contardi, A. Reduced plasma levels of tyrosine, precursor of brain catecholamines, and of essential amino acids in patients with severe traumatic brain injury after rehabilitation. Arch. Phys. Med. Rehabil. 2003, 84, 1258–1265. [Google Scholar] [CrossRef]
- Aquilani, R.; Opasich, C.; Gualco, A.; Verri, M.; Testa, A.; Pasini, E.; Viglio, S.; Iadarola, P.; Pastoris, O.; Dossena, M.; et al. Adequate energy-protein intake is not enough to improve nutritional and metabolic status in muscle-depleted patients with chronic heart failure. Eur. J. Heart Fail. 2008, 10, 1127–1135. [Google Scholar] [CrossRef] [PubMed]
- Weir, J.B. New methods for calculating metabolic rate with special reference to protein metabolism. J. Physiol. 1949, 109, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Toth, M.J.; Gottlieb, S.S.; Fisher, M.L.; Poehlman, E.T. Daily energy requirements in heart failure patients. Metabolism 1997, 46, 1294–1298. [Google Scholar] [CrossRef]
- Schutte, R.; Thijs, L.; Asayama, K.; Boggia, J.; Li, Y.; Hansen, T.W.; Liu, Y.P.; Kikuya, M.; Björklund-Bodegård, K.; Ohkubo, T.; et al. Double product reflects the predictive power of systolic pressure in the general population: Evidence from 9937 participants. Am. J. Hypertens. 2013, 26, 665–672. [Google Scholar] [CrossRef] [PubMed]
- Chacko, A.; Cummings, J.H. Nitrogen losses from the human small bowel: Obligatory losses and the effect of physical form of food. Gut 1988, 29, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Coggins, M.; Rosenzweig, A. The fire within: Cardiac inflammatory signaling in health and disease. Circ. Res. 2012, 110, 116–125. [Google Scholar] [CrossRef] [PubMed]
- Von Haehling, S.; Lainscak, M.; Springer, J.; Anker, S.D. Cardiac cachexia: A systematic overview. Pharmacol. Ther. 2009, 121, 227–252. [Google Scholar] [CrossRef] [PubMed]
- Conraads, V.M.; Bosmans, J.M.; Vrints, C.J. Chronic heart failure: An example of a systemic chronic inflammatory disease resulting in cachexia. Int. J. Cardiol. 2002, 85, 33–49. [Google Scholar] [CrossRef]
- Anker, S.D.; Lechat, P.; Dargie, H.J. Prevention and reversal of cachexia in patients with chronic heart failure by bisoprolol: Results from the CIBIS-II study. J. Am. Coll. Cardiol. 2003, 41, 156–157. [Google Scholar] [CrossRef]
- Plumley, D.A.; Austgen, T.R.; Salloum, R.M.; Souba, W.W. Role of the lungs in maintaining amino acid homeostasis. JPEN J. Parenter. Enter. Nutr. 1990, 14, 569–573. [Google Scholar] [CrossRef] [PubMed]
- Taegtmeyer, H.; Harinstein, M.E.; Gheorghiade, M. More than bricks and mortar: Comments on protein and amino acid metabolism in the heart. Am. J. Cardiol. 2008, 101, 3E–7E. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Block, G.; Horwich, T.; Fonarow, G.C. Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J. Am. Coll. Cardiol. 2004, 43, 1439–1444. [Google Scholar] [CrossRef] [PubMed]
- Rau, E.E.; Shine, K.I.; Gervais, A.; Douglas, A.M.; Amos, E.C., 3rd. Enhanced mechanical recovery of anoxic and ischemic myocardium by amino acid perfusion. Am. J. Physiol. 1979, 236, H873–H879. [Google Scholar] [PubMed]
- Arsenian, M.A. Carnitine and its derivatives in cardiovascular disease. Prog. Cardiovasc. Dis. 1997, 40, 265–286. [Google Scholar] [CrossRef]
- Nakae, I.; Mitsunami, K.; Omura, T.; Yabe, T.; Tsutamoto, T.; Matsuo, S.; Takahashi, M.; Morikawa, S.; Inubushi, T.; Nakamura, Y.; et al. Proton magnetic resonance spectroscopy can detect creatine depletion associated with the progression of heart failure in cardiomyopathy. J. Am. Coll. Cardiol. 2003, 42, 1587–1593. [Google Scholar] [CrossRef] [PubMed]
- Akhmedov, A.T.; Rybin, V.; Marín-García, J. Mitochondrial oxidative metabolism and uncoupling proteins in the failing heart. Heart Fail. Rev. 2015, 20, 227–249. [Google Scholar] [CrossRef] [PubMed]
- Hakuno, D.; Hamba, Y.; Toya, T.; Adachi, T. Plasma amino acid profiling identifies specific amino acid associations with cardiovascular function in patients with systolic heart failure. PLoS ONE 2015, 10, e117325. [Google Scholar] [CrossRef] [PubMed]
- Grimble, R.F.; Jackson, A.A.; Persaud, C.; Wride, M.J.; Delers, F.; Engler, R. Cysteine and glycine supplementation modulate the metabolic response to tumor necrosis factor alpha in rats fed a low protein diet. J. Nutr. 1992, 122, 2066–2073. [Google Scholar] [PubMed]
- Carubelli, V.; Castrini, A.I.; Lazzarini, V.; Gheorghiade, M.; Metra, M.; Lombardi, C. Amino acids and derivatives, a new treatment of chronic heart failure? Heart Fail. Rev. 2015, 20, 39–51. [Google Scholar] [CrossRef] [PubMed]
- Azuma, J.; Sawamura, A.; Awata, N. Usefulness of taurine in chronic congestive heart failure and its prospective application. Jpn. Circ. J. 1992, 56, 95–99. [Google Scholar] [CrossRef] [PubMed]
- Azuma, J.; Sawamura, A.; Awata, N.; Ohta, H.; Hamaguchi, T.; Harada, H.; Takihara, K.; Hasegawa, H.; Yamagami, T.; Ishiyama, T.; et al. Therapeutic effect of taurine in congestive heart failure: A double-blind crossover trial. Clin. Cardiol. 1985, 8, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Jeejeebhoy, F.; Keith, M.; Freeman, M.; Barr, A.; McCall, M.; Kurian, R.; Mazer, D.; Errett, L. Nutritional supplementation with MyoVive repletes essential cardiac myocyte nutrients and reduces left ventricular size in patients with left ventricular dysfunction. Am. Heart J. 2002, 143, 1092–1100. [Google Scholar] [CrossRef] [PubMed]
- Beyranvand, M.R.; Khalafi, M.K.; Roshan, V.D.; Choobineh, S.; Parsa, S.A.; Piranfar, M.A. Effect of taurine supplementation on exercise capacity of patients with heart failure. J. Cardiol. 2011, 57, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhou, M.; Sun, H.; Wang, Y. Branched-chain amino acid metabolism in heart disease: An epiphenomenon or a real culprit? Cardiovasc. Res. 2011, 90, 220–223. [Google Scholar] [CrossRef] [PubMed]
- Divakaran, V.; Mann, D.L. The emerging role of microRNAs in cardiac remodeling and heart failure. Circ. Res. 2008, 103, 1072–1083. [Google Scholar] [CrossRef] [PubMed]
- El-Sayed, H.L.; Nassar, M.F.; Habib, N.M.; Elmasry, O.A.; Gomaa, S.M. Structural and functional affection of the heart in protein energy malnutrition patients on admission and after nutritional recovery. Eur. J. Clin. Nutr. 2006, 60, 502–510. [Google Scholar] [CrossRef] [PubMed]
- King, D.; Smith, M.L.; Lye, M. Gastro-intestinal protein loss in elderly patients with cardiac cachexia. Age Ageing 1996, 25, 221–223. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Canela, M.; Hruby, A.; Clish, C.B.; Liang, L.; Martínez-González, M.A.; Hu, F.B. Comprehensive metabolic profiling and incidence cardiovascular disease. A systematic review. J. Am. Heart Assoc. 2017, 6. [Google Scholar] [CrossRef] [PubMed]
- Ghanim, H.; Abuaysheh, S.; Sia, C.L.; Korzeniewski, K.; Chaudhuri, A.; Fernandez-Real, J.M.; Dandona, P. Increase in plasma endotoxin concentrations and the expression of Toll-like receptors and suppressor of cytokine signaling-3 in mononuclear cells after a high-fat, high-carbohydrate meal: Implications for insulin resistance. Diabetes Care 2009, 32, 2281–2287. [Google Scholar] [CrossRef] [PubMed]
- Ghanim, H.; Sia, C.L.; Upadhyay, M.; Korzeniewski, K.; Viswanathan, P.; Abuaysheh, S.; Mohanty, P.; Dandona, P. Orange juice neutralizes the proinflammatory effect of a high-fat, high-carbohydrate meal and prevents endotoxin increase and Toll-like receptor expression. Am. J. Clin. Nutr. 2010, 91, 940–949. [Google Scholar] [CrossRef] [PubMed]
| All CHF (n = 41) | NYHA II (n = 12) | NYHA III (n = 19) | NYHA IV (n = 10) | ||
|---|---|---|---|---|---|
| Demographic | Age (years) | 60 ± 8.2 | 57 ± 13.1 | 57.0 ± 8.4 | 61 ± 3.9 |
| Sex (male/female) | 30/11 | 8/4 | 12/7 | 8/2 | |
| Anthropometrics | Body weight (kg) | 78.5 ± 15.2 | 82 ± 21.3 | 82.1 ± 14.7 | 73 ± 2.8 |
| BMI (kg m−2) | 27.7 ± 5 | 29.2 ± 5.5 | 28.8 ± 5.5 | 24 ± 0.7 * | |
| Etiology | Ischemic | 21 pts (51.2%) | 6/12 | 8/19 | 7/10 |
| Idiopathic dilated cardiomyopathy | 13 pts (31.7%) | 4/12 | 6/19 | 3/10 | |
| Valvular | 7 pts (17.1%) | 2/12 | 5/19 | 0/10 | |
| Functional class | NYHA | 2.9 ± 0.7 | 2 ± 0 | 3 ± 0 | 4 ± 0 |
| SBP/DPB | Blood pressure | 109.7 ± 14.7 | 117 ± 16.9 | 107 ± 13 | 105 ± 14.3 |
| Systolic blood pressure mmHg/diastolic blood pressure mmHg | 67 ± 14.5 | 71 ± 13.5 | 68 ± 14 | 63 ± 16 | |
| Medications | ACE inhibition | 41 pts (100%) | 12 pts | 19 pts | 10 pts |
| β blockers | 41 pts (100%) | 12 pts | 19 pts | 10 pts | |
| Digoxin | 13 pts (31.7%) | 5 pts | 3 pts | 5 pts | |
| Diuretics | 41 pts (100%) | 12 pts | 19 pts | 10 pts | |
| Spironolactone | 4 pts (9.7%) | - | 1 pts | 3 pts | |
| Blood | Glucose (mg dL−1; nv = 80–110) | 97.5 ± 18.1 | 92 ± 15.5 | 102.5 ± 20.9 | 98.5 ± 19.1 |
| Albumin (g dL−1; nv = 3.5–5) | 4.4 ± 0.4 | 4.5 ± 0.4 | 4.5 ± 0.5 | 4.4 ± 0.1 | |
| Hemoglobin (g dL−1; nv = 12–15) | 13.0 ± 12.0 | 12.4 ± 1.7 | 12.7 ± 1.6 | 11.3 ± 3.2 | |
| Sodium (mEq L−1; nv = 135–145) | 135.4 ± 5.1 | 138.4 ± 2.9 | 135 ± 5 | 137 ± 2.8 | |
| Potassium (mEq L−1; nv = 3.5–5.0 | 4.0 ± 0.5 | 4.3 ± 0.2 | 3.9 ± 0.6 | 3.7 ± 0.1 | |
| Creatinine (mg dL−1; nv = 0.6–1.2) | 1.5 ± 0.5 | 1.3 ± 0.4 | 1.6 ± 0.7 | 1.3 ± 0.1 | |
| Urea (mg dL−1; NV = 20–40) | 78.8 ± 58.2 | 67 ± 38.4 | 88.4 ± 75.6 | 62.5 ± 30.4 | |
| NT-pro-BNP (pg mL−1; nv < 125 for age < 75 years) | 1680.6 ± 983.6 | 347 ± 215.6 | 2022.3 ± 813.5 | 2699 ± 1750 | |
| Physical performance | VO2 rest (mL O2 kg−1 min−1) | 3.4 ± 1 | 3.2 ± 0.01 | 3.4 ± 1.1 | 4.1 ± 1.4 |
| VO2 peak (mL O2 kg−1 min−1) | 12.4 ± 3 | 12.1 ± 1.0 | 11.2 ± 2.3 | nd | |
| HR peak (beat min−1) | 109.2 ± 22.7 | 111.3 ± 11.7 | 95.2 ± 22.1 | nd | |
| Hemodynamic variables | CO (L min−1) | 3.9 ± 1.1 | 4.7 ± 1.4 | 4 ± 1.0 | 3.0 ± 1.6 |
| CI (L min−1 m−2) | 2.2 ± 0.5 | 2.4 ± 0.4 | 2.2 ± 0.5 | 1.9 ± 0.3 £ | |
| SV (mL beat−1) | 57.5 ± 19.5 | 66 ± 26.8 | 61.6 ± 19.3 | 49.5 ± 30.4 | |
| SVI (mL beat−1 m−2) | 32.1 ± 8.9 | 34.3 ± 7.4 | 34.2 ± 9.7 | 25.5 ± 5.5 £ | |
| LVEF (%; nv > 55) | 32.4 ± 10.4 | 39.3 ± 10.7 | 33.5 ± 8.3 | 27.5 ± 8.9 *£ | |
| WP (mmHg) | 19.2 ± 9.3 | 15.4 ± 7.6 | 17.6 ± 9.5 | 24.8 ± 11 |
| HEALTHY | CHF | ||||
|---|---|---|---|---|---|
| All-CHF | NYHA | ||||
| (n = 8) | (n = 41) | II (n = 12) | III (n = 19) | IV (n = 10) | |
| AAtot | 2530.7 ± 55.84 | 1954 ± 1042 | 2459 ± 108 | 2318 ± 1075 | 655.6 ± 97.34 ‡•& |
| EAAs | 616.2 ± 20.3 | 601 ± 356.01 | 727.5 ± 110 | 748.4 ± 370.1 | 169.4 ± 26.59 †•& |
| BCAAs | 286.5 ± 13.57 | 264.9 ± 160.7 | 310.6 ± 62.89 | 331.5 ± 174.8 | 83.73 ± 15.49 *∞& |
| Aspartic acid | 112.1 ± 8.858 | 16.41 ± 11.44 ‡ | 23.47 ± 5.527 ‡ | 17.16 ± 13.51 ‡ | 6.511 ± 1.492 ‡• |
| Glutamic acid | 198.6 ± 10.61 | 134.0 ± 54.22 † | 191.5 ± 20.46 | 126.7 ± 47.52 † | 78.67 ± 11.22 ‡•& |
| Asparagine | 61.04 ± 1.987 | 49.29 ± 21.86 | 60.18 ± 2.512 | 55.56 ± 23.75 | 24.32 ± 7.299 ‡• |
| Serine | 88.39 ± 4.251 | 84.38 ± 52.34 | 93.51 ± 8.853 | 111.1 ± 55.73 | 22.71 ± 5.196 *∞£ |
| Glutamine | 464.9 ± 13.98 | 397.8 ± 267.9 | 498.8 ± 55.49 | 498.1 ± 292.8 | 86.15 ± 32.68 †•£ |
| Hystidine | 58 ± 5.155 | 50.78 ± 34.9 | 62.92 ± 8.836 | 65.17 ± 36.72 | 8.868 ± 5.402 †•£ |
| Glycine | 268.3 ± 11.97 | 205.2 ± 118.3 | 265.8 ± 14.06 | 247.3 ± 116.8 | 52.33 ± 5.963 ‡•£ |
| Threonine | 111.6 ± 7.3 | 77.34 ± 47.37 | 114.7 ± 13.63 | 84.82 ± 43.79 | 18.27 ± 5.284 ‡•£ |
| Citrulline | 24.58 ± 3.661 | 28.83 ± 20.65 | 28.49 ± 6.965 | 39.66 ± 22.65 | 6.471 ± 1.171 ∞& |
| Alanine | 312.6 ± 15.67 | 236.6 ± 145.5 | 324.9 ± 23.35 | 274.3,4 ± 149.9 | 59.08 ± 6.012 ‡•& |
| Arginine | 59.28 ± 7.607 | 52.89 ± 23.35 | 61.53 ± 7.889 | 61.71 ± 24.54 | 25.75 ± 7.758 †•& |
| Tyrosine | 56.25 ± 6.112 | 51.14 ± 29.92 | 57.29 ± 5.224 | 65.29 ± 32.81 | 16.87 ± 3.573 *∞& |
| Cystein | 77.13 ± 5.139 | 36.57 ± 19.48 ‡ | 60.88 ± 8.241 | 31.69 ± 11.90 ‡ | 16.69 ± 6.602 ‡• |
| Valine | 160.0 ± 15.8 | 145.5 ± 87.75 | 173.6 ± 38.04 | 178.1 ± 97.26 | 49.83 ± 8.432 ∞& |
| Methionine | 9.7 ± 2.8 | 4.872 ± 1.861 ‡ | 7.196 ± 1.18 ‡ | 4.244 ± 1.086 ‡ | 3.279 ± 0.692 ‡• |
| Tryptophan | 50.1 ± 4.9 | 39.93 ± 23.77 | 50 ± 5.481 | 49.10 ± 24.36 | 10.43 ± 3.011 ‡•& |
| Phenylalanine | 51.3 ± 5.1 | 44.67 ± 27.75 | 50.25 ± 7.518 | 58.51 ± 29.09 | 11.68 ± 2.327 *∞& |
| Isoleucine | 47.4 ± 4.1 | 41.83 ± 26.52 | 48.33 ± 6.597 | 53.79 ± 28.88 | 11.28 ± 2.949 *∞& |
| Leucine | 79.1 ± 8.5 | 74.72 ± 48.84 | 90.21 ± 20.51 | 92.37 ± 53.13 | 22.62 ± 4.539 ∞& |
| Lysine | 107 ± 114 | 119.9 ± 72.45 | 137.6 ± 33.55 | 154.0 ± 73.57 | 33.8 ± 5.485 ∞& |
| Taurine | 133.3 ± 23.03 | 86.02 ± 28.26 ‡ | 97.17 ± 14.14 * | 93.86 ± 29.25 † | 57.75 ± 20.26 ‡∞@ |
| HEALTHY | CHF | |||||
|---|---|---|---|---|---|---|
| All CHF | NYHA | |||||
| II | III | IV | ||||
| Weight | 66.4 ± 8.6 | 78.5 ± 15.2 | 82.2 ± 21.3 | 82.11 ± 14.7 | 73.4 ± 2.8 | |
| H-B | Kcal/day | 1351 ± 120 | 1568 ± 185 * | 1561.5 ± 245 * | 1534 ± 251 * | 1677.7 ± 209 * |
| REE: | ||||||
| Kcal/day | 1384 ± 127.8 | 1584 ± 195 | 1637.7 ± 273 | 1532.1 ± 202 | 1890.7 ± 151 | |
| REE/H-B (%) | 102.4 ± 0.8 | 101 ± 5.7 | 104.9 ± 3.8 | 99.8 ± 3.3 ** | 113 ± 1.3 ** | |
| Kcal/kg | 20.2 ± 0.7 | 20.2 ± 3.7 | 20.0 ± 3.9 | 18.7 ± 4.9 | 25.9 ± 3.1 * | |
| Nutritional Intakes: | ||||||
| Energy: | ||||||
| Kcal I/day | 1797 ± 195 | 2220 ± 393.3 | 2361.6 ± 361 | 2167.4 ± 337 | 2132 ± 482 | |
| Kcal I/kg | 28.5 ± 1.1 | 28.1 ± 5.0 | 28.8 ± 4.4 | 26.4 ± 4.1 | 29.2 ± 4.6 | |
| CHO: | ||||||
| g/day | 264.6 ± 31 | 271.8 ± 11.4 | 280.6 ± 17.8 | 275.9 ± 13.3 | 259.8 ± 3.1 | |
| g/kg | 4.2 ± 0.5 | 3.3 ± 0.9 | 3.4 ± 0.8 | 3.4 ± 0.9 | 3.6 ± 1.1 | |
| Proteins: | ||||||
| g/day | 70 ± 12 | 92.9 ± 10.5 | 92.7 ± 13.1 | 92 ± 11.5 | 94.35 ± 7.1 | |
| g/kg | 1.1 ± 0.2 | 1.18 ± 0.2 | 1.1 ± 0.2 | 1.12 ± 0.14 | 1.31 ± 0.31 | |
| Lipids: | ||||||
| g/day | 51 ± 12 | 84.0 ± 10.6 | 95.9 ± 5.3 | 77.1 ± 9.9 | 79.3 ± 16.6 | |
| g/kg | 0.8 ± 0.2 | 1.0 ± 0.2 | 1.2 ± 0.2 * | 0.9 ± 0.1 | 1.1 ± 0.2 | |
| Adequacy of calorie Intakes | ||||||
| Kcal I/TEE (%) | 130 ± 1.2 | 140.1 ± 3.8 ** | 144.2 ± 5.2 ** | 141.4 ± 4.3 ** | 112.8 ± 4.1 ∞ ** | |
| Amino Acids | p Value |
|---|---|
| Asparagine | 0.052 |
| Serine | 0.006 |
| Glutamine | 0.02 |
| Threonine | 0.02 |
| Alanine | 0.0499 |
| Arginine | 0.127 |
| Tyrosine | 0.0139 |
| Valine | 0.0227 |
| Tryptophan | 0.0134 |
| Phenylalanine | 0.0184 |
| Leucine | 0.0086 |
| Lysine | 0.018 |
| AA tot | 0.0128 |
| EAA tot | 0.014 |
| BCAA | 0.0185 |
| Severity (NYHA) | Reduced Amino Acids |
|---|---|
| II class | Aspartic acid methionine, taurine |
| III class | Aspartic acid, methionine, taurine. Glutamic acid, cysteine |
| IV class | All the standard amino acids |
| Severity (NYHA) | Effects on Myocardium Metabolism |
|---|---|
| II and III classes | Aggravation of mitochondrial energy production
Increased heart oxidative stress |
| IV class | The above + alterations in protein metabolism remodelling |
| The biochemical effects may potentially impact on heart contractility, function | |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aquilani, R.; La Rovere, M.T.; Corbellini, D.; Pasini, E.; Verri, M.; Barbieri, A.; Condino, A.M.; Boschi, F. Plasma Amino Acid Abnormalities in Chronic Heart Failure. Mechanisms, Potential Risks and Targets in Human Myocardium Metabolism. Nutrients 2017, 9, 1251. https://doi.org/10.3390/nu9111251
Aquilani R, La Rovere MT, Corbellini D, Pasini E, Verri M, Barbieri A, Condino AM, Boschi F. Plasma Amino Acid Abnormalities in Chronic Heart Failure. Mechanisms, Potential Risks and Targets in Human Myocardium Metabolism. Nutrients. 2017; 9(11):1251. https://doi.org/10.3390/nu9111251
Chicago/Turabian StyleAquilani, Roberto, Maria Teresa La Rovere, Daniela Corbellini, Evasio Pasini, Manuela Verri, Annalisa Barbieri, Anna Maria Condino, and Federica Boschi. 2017. "Plasma Amino Acid Abnormalities in Chronic Heart Failure. Mechanisms, Potential Risks and Targets in Human Myocardium Metabolism" Nutrients 9, no. 11: 1251. https://doi.org/10.3390/nu9111251




