Study on the Prevalence of Severe Anemia among Non-Pregnant Women of Reproductive Age in Rural China: A Large Population-Based Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Case Definition of Severe Anemia
2.3. Methods Used for Statistical Analysis
2.4. Ethical Approval
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization (WHO). The Global Prevalence of Anaemia in 2011; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- World Health Organization (WHO). The Prevalence of Anaemia in Women: A Tabulation of Available Information; World Health Organization: Geneva, Switzerland, 1992. [Google Scholar]
- Alem, M.; Enawgaw, B.; Gelaw, A.; Kenaw, T.; Seid, M.; Olkeba, Y. Prevalence of anemia and associated risk factors among pregnant women attending antenatal care in Azezo Health Center Gondar town, Northwest Ethiopia. J. Interdiscip. Histopathol. 2013, 1, 137–144. [Google Scholar] [CrossRef]
- Balarajan, Y.; Ramakrishnan, U.; Ozaltin, E.; Shankar, A.H.; Subramanian, S.V. Anaemia in low-income and middle-income countries. Lancet 2011, 378, 2123–2135. [Google Scholar] [CrossRef]
- Adamu, A.L.; Crampin, A.; Kayuni, N.; Amberbir, A.; Koole, O.; Phiri, A.; Nyirenda, M.; Fine, P. Prevalence and risk factors for anemia severity and type in Malawian men and women: Urban and rural differences. Popul. Health Metr. 2017, 15, 12. [Google Scholar] [CrossRef] [PubMed]
- Kassebaum, N.J.; Jasrasaria, R.; Naghavi, M.; Wulf, S.K.; Johns, N.; Lozano, R.; Regan, M.; Weatherall, D.; Chou, D.P.; Eisele, T.P.; et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood 2014, 123, 615–624. [Google Scholar] [CrossRef] [PubMed]
- Toteja, G.S.; Singh, P.; Dhillon, B.S.; Saxena, B.N.; Ahmed, F.U.; Singh, R.P.; Prakash, B.; Vijayaraghavan, K.; Singh, Y.; Rauf, A.; et al. Prevalence of anemia among pregnant women and adolescent girls in 16 districts of India. Food Nutr. Bull. 2006, 27, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Hashim, N.; Farooqi, M.; Naqvi, S.; Jaffery, H.F. Anemia; moderate to severe during pregnancy. Prof. Med. J. 2014, 21, 247–252. [Google Scholar]
- Ransom, E.I.; Elder, L.K. Nutrition of Women and Adolescent Girls: Why It Matters; Population Reference Bureau: Washington, DC, USA, 2003. [Google Scholar]
- Rahmati, S.; Delpisheh, A.; Parizad, N.; Sayehmiri, K. Maternal anemia and pregnancy outcomes: A systematic review and meta-analysis. Int. J. Pediatr. 2016, 4, 3323–3342. [Google Scholar]
- Lone, F.W.; Qureshi, R.N.; Emanuel, F. Maternal anaemia and its impact on perinatal outcome. Trop Med. Int. Health 2004, 9, 486–490. [Google Scholar] [CrossRef] [PubMed]
- Gomes da Costa, A.; Vargas, S.; Clode, N.; Graça, L.M. Prevalence and risk factors for iron deficiency anemia and iron depletion during pregnancy: A prospective study. Acta Med. Port. 2016, 29, 514–518. [Google Scholar] [CrossRef] [PubMed]
- Stevens, G.A.; Finucane, M.M.; De-Regil, L.M.; Paciorek, C.J.; Flaxman, S.R.; Branca, F.; Peña-Rosas, J.P.; Bhutta, Z.A.; Ezzati, M.; Nutrition Impact Model Study Group. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: A systematic analysis of population-representative data. Lancet Glob. Health 2013, 1, e16–e25. [Google Scholar] [CrossRef]
- Chang, S.C.; O’Brien, K.O.; Nathanson, M.S.; Mancini, J.; Witter, F.R. Hemoglobin concentrations influence birth outcomes in pregnant African-American adolescents. J. Nutr. 2003, 133, 2348–2355. [Google Scholar] [PubMed]
- Sharma, P.; Mehta, S.; Nagar, R. Prevalence of anemia and socio-demographic factors associated with anemia among pregnant women attending antenatal Hospital in Jaipur City, India. IOSR J. Pharm. Biol. Sci. 2013, 6, 1–5. [Google Scholar]
- Bentley, M.E.; Griffiths, P.L. The burden of anemia among women in India. Eur. J. Clin. Nutr. 2003, 57, 52–60. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Capital Institute of Pediatrics, 11 Provinces Maternal Child Health Hospital. Survey of women anaemia status at child-bearing age in China in 1998. Chin. J. Reprod. Health 2002, 13, 102–107. [Google Scholar]
- Zhang, S.K.; Wang, Q.M.; Shen, H.P. Design of the National Free Preconception Health Examination Project in China. Chin. Med. J. 2015, 95, 162–165. [Google Scholar] [CrossRef]
- Wang, Q.M.; Zhang, S.K.; Hu, M.; Kang, X.X. Establishment of quality assurance system of the National Free Preconception Health Examination Project in China. Chin. Med. J. 2015, 95, 166–168. [Google Scholar] [CrossRef]
- Le, C.H.H. The prevalence of anemia and moderate-severe anemia in the US population (NHANES 2003–2012). PLoS ONE 2016, 11, e0166635. [Google Scholar] [CrossRef] [PubMed]
- Kamruzzaman, M.; Rabbani, M.G.; Saw, A.; Sayem, A.; Hossain, G. Differentials in the prevalence of anemia among non-pregnant, ever-married women in Bangladesh: Multilevel logistic regression analysis of data from the 2011 Bangladesh Demographic and Health Survey. BMC Womens Health 2015, 15, 54. [Google Scholar] [CrossRef] [PubMed]
- Wilunda, C.; Massawe, S.; Jackson, C. Determinants of moderate-to-severe anaemia among women of reproductive age in Tanzania: Analysis of data from the 2010 Tanzania Demographic and Health Survey. Trop Med. Int. Health 2013, 18, 1488–1497. [Google Scholar] [CrossRef] [PubMed]
- Moor, M.A.; Fraga, M.A.; Garfein, R.S.; Harbertson, J.; Rodriguez-Lainz, A.; Rashidi, H.H.; Elder, J.P.; Brodine, S.K. Decreased anemia prevalence among women and children in Rural Baja California, Mexico: A 6-year comparative study. J. Community Health 2016, 41, 780–789. [Google Scholar] [CrossRef] [PubMed]
- Haas, J.D.; Brownlie, T. Iron deficiency and reduced work capacity: A critical review of the research to determine a causal relationship. J. Nutr. 2001, 131, 676S–690S. [Google Scholar] [PubMed]
- Miller, J.L. Iron deficiency anemia: A common and curable disease. Cold Spring Harb. Perspect. Med. 2013, 3, a011866. [Google Scholar] [CrossRef] [PubMed]
- Behboudi-Gandevani, S.; Imani, S.; Moghaddam-Banaem, L.; Roudbar-Mohammadi, S. Can intrauterine contraceptive devices lead to VulvoVaginal Candidiasis (VVC) and Anemia in Iranian new users? Sex. Reprod. Healthc. 2015, 6, 40–43. [Google Scholar] [CrossRef] [PubMed]
- National Health and Family Planning Commission of the PRC. Report of investigation on the contraception effect of intrauterine device by one hundred and twenty thousand cases. Chin. J. Family Plan. 2007, 15, 132–136. [Google Scholar] [CrossRef]
- Borghei, A.; Qorbani, M.; Borghei, N.S.; Kazeminejad, V.; Seifi, F. Effects of IUD on iron status in IUD users in Gorgan, Iran. Med. J. Islam. Repub. Iran 2011, 25, 131–135. [Google Scholar]
- Blanco-Rojo, R.; Toxqui, L.; Lopez-Parra, A.M.; Arroyo-Pardo, E.; Vaquero, M.P. Influence of diet, menstruation and genetic factors on iron status: A cross-sectional study in Spanish women of childbearing age. Int. J. Mol. Sci. 2014, 15, 4077–4087. [Google Scholar] [CrossRef] [PubMed]
- Karakochuk, C.D.; Whitfield, K.C.; Barr, S.I.; Lamers, Y.; Devlin, A.M.; Vercauteren, S.M.; Kroeun, H.; Talukder, A.; McLean, J.; Green, T.J. Genetic hemoglobin disorders rather than iron deficiency are a major predictor of hemoglobin concentration in women of reproductive age in rural prey Veng, Cambodia. J. Nutr. 2015, 145, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Alaunyte, I.; Stojceska, V.; Plunkett, A. Iron and the female athlete: A review of dietary treatment methods for improving iron status and exercise performance. J. Int. Soc. Sports Nutr. 2015, 12, 38. [Google Scholar] [CrossRef] [PubMed]
- Harvey, L.J.; Armah, C.N.; Dainty, J.R.; Foxall, R.J.; John Lewis, D.; Langford, N.J.; Fairweather-Tait, S.J. Impact of menstrual blood loss and diet on iron deficiency among women in the UK. Br. J. Nutr. 2005, 94, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Li, L.M.; Rao, K.Q.; Kong, L.Z.; Yao, C.H.; Xiang, H.D.; Zhai, F.Y.; Ma, G.S.; Yang, X.G.; Technical Working Group of China National Nutrition and Health Survey. A description on the Chinese national nutrition and health survey in 2002. Chin. J. Epidemiol. 2005, 26, 478–484. [Google Scholar] [CrossRef]
- Hu, Y.C.; Chen, J.; Li, M.; Li, W.; Yang, Y.; Wang, R.; Piao, J. Study on the anemia status of Chinese urban residents in 2010–2012. Chin. J. Prev. Med. 2016, 50, 213–216. [Google Scholar] [CrossRef]
| Number | % | Severe Anemia (n) | Prevalence of Severe Anemia (% (95% CI)) | cOR (95% CI) | aOR a (95% CI) | |
|---|---|---|---|---|---|---|
| All participants | 712,101 | 100.00 | 1728 | 0.24 (0.23–0.25) | _ | _ |
| Age group, years | ||||||
| 21–24 | 216,573 | 30.41 | 448 | 0.21 (0.19–0.23) | 1.00 | 1.00 |
| 25–29 | 315,673 | 44.33 | 636 | 0.20 (0.19–0.22) | 0.97 (0.86–1.10) | 0.94 (0.82–1.07) |
| 30–34 | 120,336 | 16.90 | 372 | 0.31 (0.28–0.34) | 1.50 (1.30–1.72) | 1.19 (1.02–1.38) |
| 35–39 | 40,199 | 5.65 | 141 | 0.35 (0.29–0.41) | 1.70 (1.41–2.05) | 1.10 (0.89–1.36) |
| 40–44 | 16,155 | 2.27 | 102 | 0.63 (0.51–0.75) | 3.07 (2.47–3.80) | 2.16 (1.71–2.73) |
| 45–49 | 3165 | 0.44 | 29 | 0.92 (0.58–1.25) | 4.46 (3.06–6.51) | 3.08 (2.07–4.60) |
| Education | ||||||
| Primary school or below | 31,150 | 4.37 | 140 | 0.45 (0.38–0.52) | 1.00 | 1.00 |
| Junior high school | 444,510 | 62.42 | 1287 | 0.29 (0.27–0.31) | 0.64 (0.54–0.77) | 0.78 (0.65–0.94) |
| Senior high school | 131,986 | 18.53 | 192 | 0.15 (0.12–0.17) | 0.32 (0.26–0.40) | 0.54 (0.43–0.69) |
| College or higher | 92,826 | 13.04 | 94 | 0.10 (0.08–0.12) | 0.23 (0.17–0.29) | 0.43 (0.32–0.58) |
| Not available | 11,629 | 1.63 | _ | _ | _ | _ |
| Occupation | ||||||
| Farmers | 518,803 | 72.86 | 1473 | 0.28 (0.27–0.30) | 1.00 | 1.00 |
| Workers | 64,527 | 9.06 | 88 | 0.14 (0.11–0.16) | 0.48 (0.39–0.60) | 0.65 (0.52–0.82) |
| Others | 113,606 | 15.95 | 149 | 0.13 (0.11–0.15) | 0.46 (0.39–0.55) | 0.76 (0.62–0.93) |
| Not available | 15,165 | 2.13 | _ | _ | _ | _ |
| Ethnic origin | ||||||
| Han | 640,820 | 89.99 | 1425 | 0.22 (0.21–0.23) | 1.00 | 1.00 |
| Others | 62,262 | 8.74 | 293 | 0.47 (0.42–0.52) | 2.12 (1.87–2.41) | 1.28 (1.11–1.49) |
| Not available | 9019 | 1.27 | _ | _ | _ | _ |
| Region | ||||||
| Southwest | 92,598 | 13.00 | 157 | 0.17 (0.14–0.20) | 1.00 | 1.00 |
| Central south | 246,735 | 34.65 | 382 | 0.15 (0.14–0.17) | 0.91 (0.76–1.10) | 1.16 (0.95–1.42) |
| North | 87,890 | 12.34 | 220 | 0.25 (0.22–0.28) | 1.48 (1.20–1.81) | 1.65 (1.32–2.06) |
| Northeast | 47,767 | 6.71 | 153 | 0.32 (0.27–0.37) | 1.89 (1.51–2.36) | 1.81 (1.42–2.30) |
| East | 151,866 | 21.33 | 381 | 0.25 (0.23–0.28) | 1.48 (1.23–1.78) | 1.84 (1.51–2.26) |
| Northwest | 85,245 | 11.97 | 435 | 0.51 (0.46–0.56) | 3.02 (2.52–3.63) | 2.88 (2.37–3.51) |
| Number | % | Severe Anemia (n) | Prevalence of Severe Anemia (% (95% CI)) | cOR (95% CI) | aOR a (95% CI) | |
|---|---|---|---|---|---|---|
| All participants | 712,101 | 100.00 | 1728 | 0.24 (0.23–0.25) | _ | _ |
| History of using IUD | ||||||
| No | 601,121 | 84.42 | 1186 | 0.20 (0.19–0.21) | 1.00 | 1.00 |
| Yes | 110,980 | 15.58 | 542 | 0.49 (0.45–0.53) | 2.48 (2.24–2.75) | 1.47 (1.30–1.67) |
| History on pregnancy | ||||||
| No | 388,597 | 54.57 | 628 | 0.16 (0.15–0.17) | 1.00 | 1.00 |
| Yes | 319,189 | 44.82 | 1096 | 0.34 (0.32–0.36) | 2.13 (1.93–2.35) | 1.38 (1.21–1.59) |
| Not available | 4315 | 0.61 | _ | _ | _ | _ |
| History on miscarriage | ||||||
| No | 598,045 | 83.98 | 1424 | 0.24 (0.23–0.25) | 1.00 | 1.00 |
| Yes | 114,056 | 16.02 | 304 | 0.27 (0.24–0.30) | 1.12 (0.99–1.27) | 0.85 (0.74–0.98) |
| History on anemia | ||||||
| No | 703,399 | 98.78 | 1633 | 0.23 (0.22–0.24) | 1.00 | 1.00 |
| Yes | 8702 | 1.22 | 95 | 1.09 (0.87–1.31) | 4.74 (3.85–5.84) | 5.76 (4.63–7.18) |
| Menstrual blood loss | ||||||
| Minor | 20,033 | 2.81 | 36 | 0.18 (0.12–0.24) | 1.00 | 1.00 |
| Medium | 661,682 | 92.92 | 1589 | 0.24 (0.23–0.25) | 1.34 (0.96–1.86) | 1.31 (0.94–1.83) |
| Heavy | 24,023 | 3.37 | 95 | 0.40 (0.32–0.47) | 2.21 (1.50–3.24) | 1.84 (1.25–2.71) |
| Not available | 6363 | 0.89 | _ | _ | _ | _ |
| BMI | ||||||
| <18.5 | 77,389 | 10.87 | 170 | 0.22 (0.19–0.25) | 1.00 | 1.00 |
| 18.5–24 | 514,707 | 72.28 | 1274 | 0.25 (0.23–0.26) | 1.13 (0.96–1.32) | 0.93 (0.79–1.09) |
| ≥24 | 77,308 | 10.86 | 186 | 0.24 (0.21–0.28) | 1.10 (0.89–1.35) | 0.76 (0.61–0.94) |
| Not available | 42,697 | 6.00 | _ | _ | _ | _ |
| Meat and egg eaters | ||||||
| Yes | 699,519 | 98.23 | 1700 | 0.24 (0.23–0.25) | 1.00 | 1.00 |
| No | 7379 | 1.04 | 17 | 0.23 (0.12–0.34) | 0.95 (0.59–1.53) | 0.82 (0.47–1.41) |
| Not available | 5203 | 0.73 | _ | _ | _ | _ |
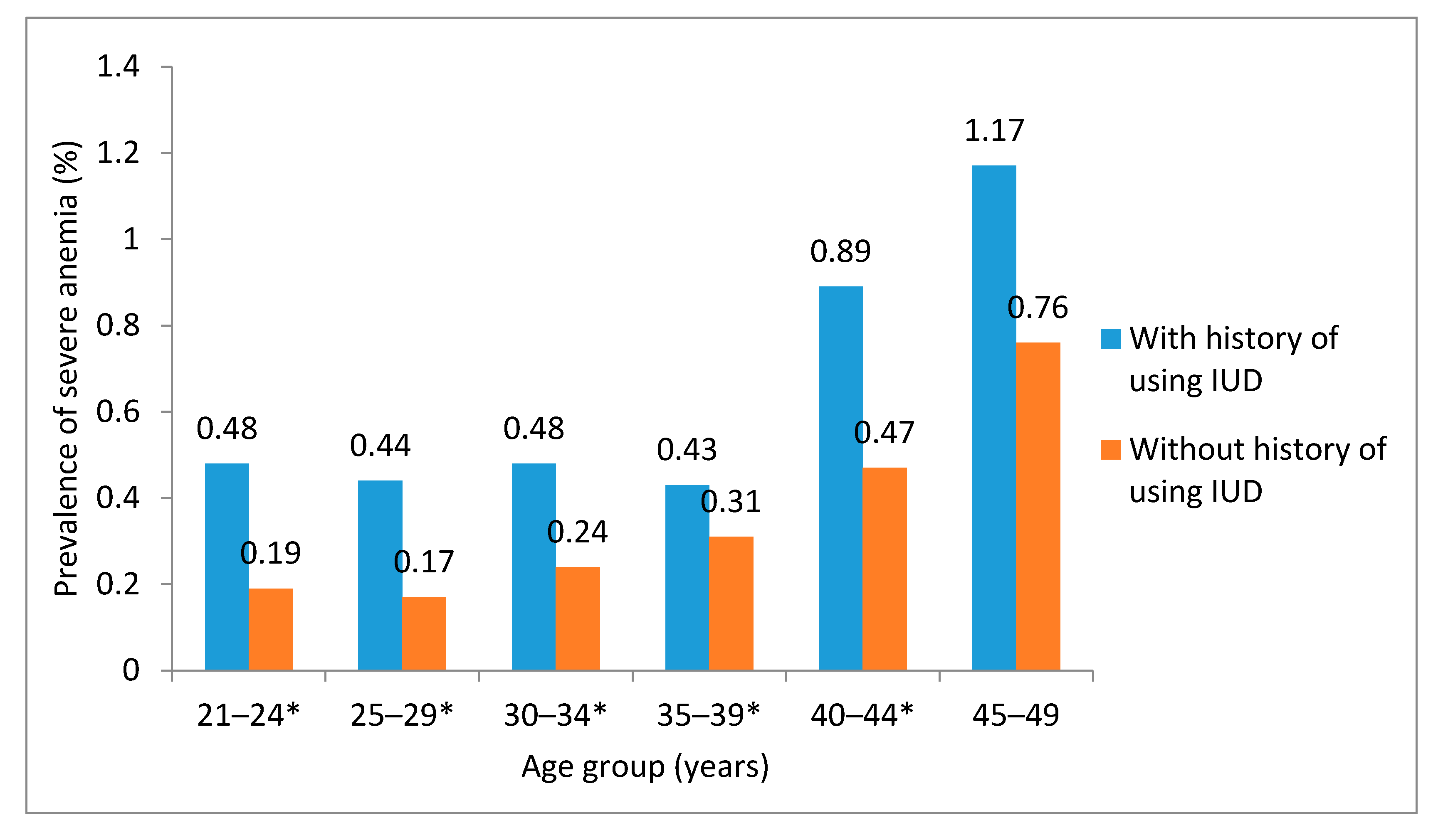
| With History of Using IUD | Without History of Using IUD | |||||||
|---|---|---|---|---|---|---|---|---|
| Number | Severe Anemia, n (%) | cOR (95% CI) | aOR a (95% CI) | Number | Severe Anemia, n (%) | cOR (95% CI) | aOR a (95% CI) | |
| Age group, years | ||||||||
| 21–24 | 11,618 | 56 (0.48) | 1.00 | 1.00 | 204,955 | 392 (0.19) | 1.00 | 1.00 |
| 25–29 | 41,879 | 184 (0.44) | 0.91 (0.68–1.23) | 1.03 (0.75–1.41) | 273,794 | 452 (0.17) | 0.86 (0.75–0.99) | 0.90 (0.78–1.04) |
| 30–34 | 35,262 | 169 (0.48) | 0.99 (0.73–1.35) | 1.20 (0.87–1.65) | 85,074 | 203 (0.24) | 1.25 (1.05–1.48) | 1.19 (0.99–1.43) |
| 35–39 | 14,733 | 63 (0.43) | 0.89 (0.62–1.27) | 0.95 (0.64–1.40) | 25,466 | 78 (0.31) | 1.60 (1.26–2.05) | 1.26 (0.96–1.65) |
| 40–44 | 6293 | 56 (0.89) | 1.85 (1.28–2.69) | 2.41 (1.63–3.57) | 9862 | 46 (0.47) | 2.45 (1.80–3.32) | 1.90 (1.36–2.65) |
| 45–49 | 1195 | 14 (1.17) | 2.45(1.36–4.41) | 2.90 (1.55–5.41) | 1970 | 15 (0.76) | 4.00 (2.39–6.72) | 3.23 (1.87–5.56) |
| Education | ||||||||
| Primary school or below | 9079 | 66 (0.73) | 1.00 | 1.00 | 22,071 | 74 (0.34) | 1.00 | 1.00 |
| Junior high school | 88,897 | 442 (0.50) | 0.68 (0.53–0.89) | 0.72 (0.55–0.96) | 355,613 | 845 (0.24) | 0.71 (0.56–0.90) | 0.82 (0.63–1.05) |
| Senior high school | 9719 | 30 (0.31) | 0.42 (0.27–0.65) | 0.53 (0.34–0.84) | 122,267 | 162 (0.13) | 0.39 (0.30–0.52) | 0.56 (0.42–0.75) |
| College or higher | 2233 | 4 (0.18) | 0.25(0.09–0.67) | 0.32 (0.11–0.90) | 90,593 | 90 (0.10) | 0.30 (0.22–0.40) | 0.46 (0.32–0.65) |
| Occupation | ||||||||
| Farmers | 99,730 | 508 (0.51) | 1.00 | 1.00 | 419,073 | 965 (0.23) | 1.00 | 1.00 |
| Workers | 4799 | 15 (0.31) | 0.61 (0.37,1.02) | 0.71 (0.42–1.21) | 59,728 | 73 (0.12) | 0.53 (0.42–0.67) | 0.63 (0.49–0.82) |
| Others | 5042 | 17 (0.34) | 0.66 (0.41,1.07) | 0.89 (0.54–1.48) | 108,564 | 132 (0.12) | 0.53 (0.44–0.63) | 0.73 (0.59–0.91) |
| Ethnic origin | ||||||||
| Han | 90,262 | 408 (0.45) | 1.00 | 1.00 | 550,558 | 1017 (0.18) | 1.00 | 1.00 |
| Others | 20,359 | 134 (0.66) | 1.46 (1.20–1.78) | 1.21 (0.96–1.54) | 41,903 | 159 (0.38) | 2.06 (1.74–2.43) | 1.34 (1.10–1.62) |
| Region | ||||||||
| Southwest | 16,655 | 47 (0.28) | 1.00 | 1.00 | 75,943 | 110 (0.14) | 1.00 | 1.00 |
| Central south | 21,128 | 63 (0.30) | 1.06 (0.72–1.54) | 1.31 (0.87–1.97) | 225,607 | 319 (0.14) | 0.98 (0.79–1.21) | 1.09 (0.86–1.38) |
| North | 14,832 | 75 (0.51) | 1.80 (1.25–2.59) | 2.34 (1.57–3.49) | 73,058 | 145 (0.20) | 1.37 (1.07–1.76) | 1.40 (1.07–1.83) |
| Northeast | 11,141 | 69 (0.62) | 2.20 (1.52–3.19) | 2.62 (1.74–3.94) | 36,626 | 84 (0.23) | 1.59 (1.19–2.11) | 1.44 (1.06–1.96) |
| East | 28,914 | 127 (0.44) | 1.56 (1.12–2.18) | 2.11 (1.45–3.06) | 122,952 | 254 (0.21) | 1.43 (1.14–1.79) | 1.74 (1.37–2.22) |
| Northwest | 18,310 | 161 (0.88) | 3.14 (2.26–4.34) | 3.41 (2.40–4.85) | 66,935 | 274 (0.41) | 2.83 (2.27–3.54) | 2.66 (2.10–3.38) |
| History on pregnancy | ||||||||
| No | 2684 | 7 (0.26) | 1.00 | 1.00 | 385,913 | 621 (0.16) | 1.00 | 1.00 |
| Yes | 108,223 | 535 (0.49) | 1.90(0.90–4.01) | 1.55(0.73–3.28) | 210,966 | 561 (0.27) | 1.65 (1.48–1.86) | 1.39 (1.19–1.61) |
| History on miscarriage | ||||||||
| No | 84,429 | 416 (0.49) | 1.00 | 1.00 | 513,616 | 1008 (0.20) | 1.00 | 1.00 |
| Yes | 26,551 | 126 (0.47) | 0.96 (0.79–1.18) | 0.98(0.79–1.21) | 87,505 | 178 (0.20) | 1.04 (0.88–1.22) | 0.77 (0.64–0.93) |
| History on anemia | ||||||||
| No | 109,641 | 516 (0.47) | 1.00 | 1.00 | 593,758 | 1117 (0.19) | 1.00 | 1.00 |
| Yes | 1339 | 26 (1.94) | 4.19(2.81–6.23) | 4.74(3.13–7.17) | 7363 | 69 (0.94) | 5.02 (3.93–6.41) | 6.33 (4.89–8.20) |
| Menstrual blood loss | ||||||||
| Minor | 2497 | 7 (0.28) | 1.00 | 1.00 | 17,536 | 29 (0.17) | 1.00 | 1.00 |
| Medium | 102,324 | 497 (0.49) | 1.74 (0.82–3.67) | 1.81 (0.85–3.83) | 559,358 | 1092 (0.20) | 1.18 (0.82–1.71) | 1.20 (0.83–1.74) |
| Heavy | 5690 | 37 (0.65) | 2.33 (1.04–5.23) | 2.22 (0.98–5.02) | 18,333 | 58 (0.32) | 1.92 (1.23–2.99) | 1.80 (1.14–2.83) |
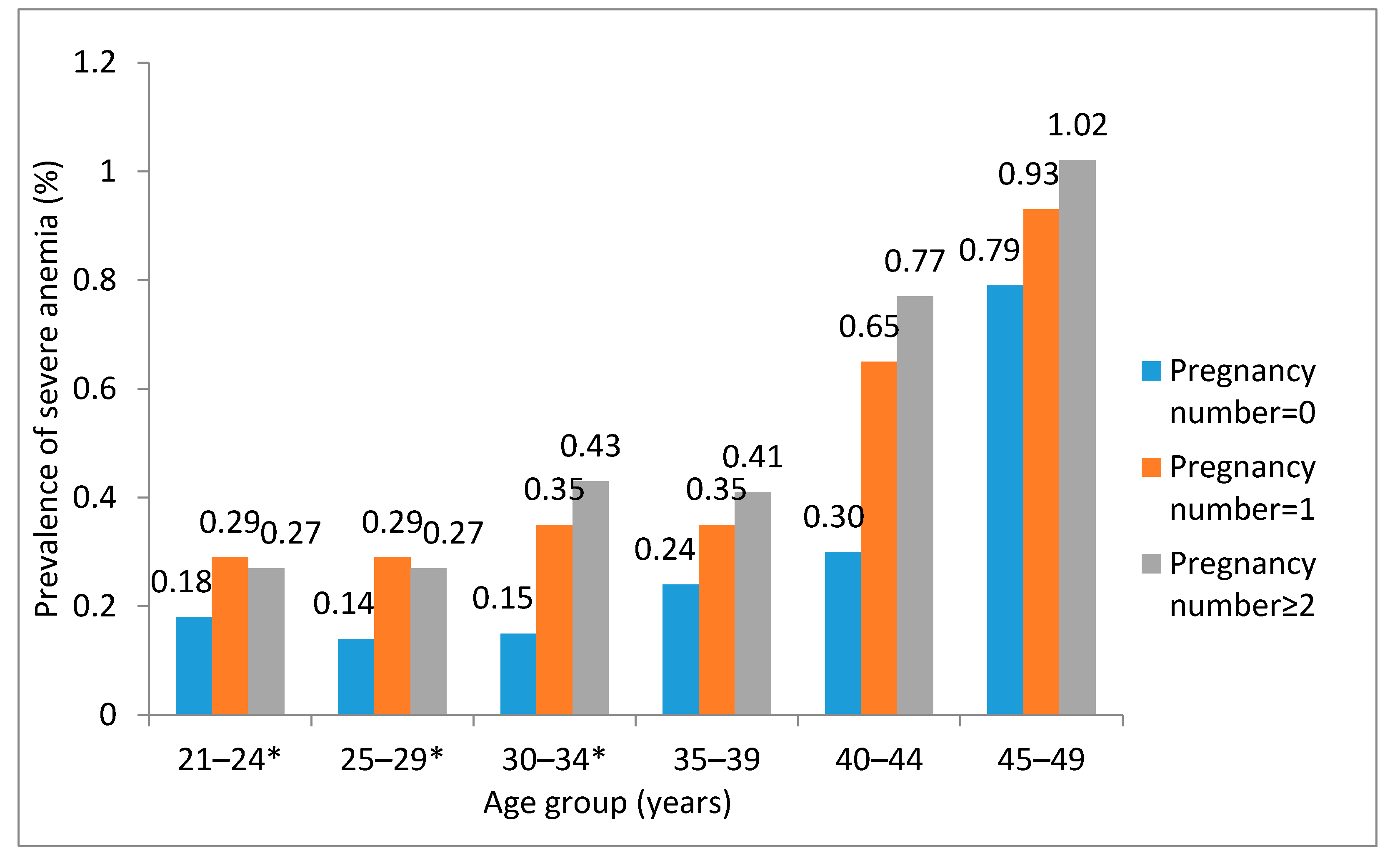
| Age Group, Years | With Pregnancy History | Without Pregnancy History | ||||||
|---|---|---|---|---|---|---|---|---|
| Number | Severe Anemia, n (%) | cOR (95% CI) | aOR a (95% CI) | Number | Severe Anemia, n (%) | cOR (95% CI) | aOR a (95% CI) | |
| 21–24 | 54,794 | 159 (0.29) | 1.00 | 1.00 | 160,081 | 288 (0.18) | 1.00 | 1.00 |
| 25–29 | 131,040 | 377 (0.29) | 0.99 (0.82–1.19) | 1.00 (0.82–1.22) | 182,968 | 258 (0.14) | 0.78 (0.66–0.93) | 0.89 (0.74–1.06) |
| 30–34 | 84,108 | 317 (0.38) | 1.30 (1.07–1.57) | 1.29 (1.05–1.57) | 35,558 | 54 (0.15) | 0.84 (0.63–1.13) | 1.01 (0.74–1.36) |
| 35–39 | 32,791 | 123 (0.38) | 1.29 (1.02–1.64) | 1.15 (0.89–1.48) | 7218 | 17 (0.24) | 1.31 (0.80–2.14) | 1.15 (0.66–2.01) |
| 40–44 | 13,798 | 95 (0.69) | 2.38 (1.85–3.07) | 2.39 (1.83–3.12) | 2280 | 7 (0.31) | 1.71 (0.81–3.62) | 1.04 (0.39–2.80) |
| 45–49 | 2658 | 25 (0.94) | 3.26 (2.14–4.98) | 3.06 (1.96–4.80) | 492 | 4 (0.81) | 4.55 (1.69–12.25) | 5.05 (1.86–13.66) |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, Q.; Zhang, S.; Liu, J.; Wang, Q.; Shen, H.; Zhang, Y.; Liu, M. Study on the Prevalence of Severe Anemia among Non-Pregnant Women of Reproductive Age in Rural China: A Large Population-Based Cross-Sectional Study. Nutrients 2017, 9, 1298. https://doi.org/10.3390/nu9121298
Ma Q, Zhang S, Liu J, Wang Q, Shen H, Zhang Y, Liu M. Study on the Prevalence of Severe Anemia among Non-Pregnant Women of Reproductive Age in Rural China: A Large Population-Based Cross-Sectional Study. Nutrients. 2017; 9(12):1298. https://doi.org/10.3390/nu9121298
Chicago/Turabian StyleMa, Qiuyue, Shikun Zhang, Jue Liu, Qiaomei Wang, Haiping Shen, Yiping Zhang, and Min Liu. 2017. "Study on the Prevalence of Severe Anemia among Non-Pregnant Women of Reproductive Age in Rural China: A Large Population-Based Cross-Sectional Study" Nutrients 9, no. 12: 1298. https://doi.org/10.3390/nu9121298




