The Efficacy of Psychological Therapies in Reducing Weight and Binge Eating in People with Bulimia Nervosa and Binge Eating Disorder Who Are Overweight or Obese—A Critical Synthesis and Meta-Analyses
Abstract
:1. Introduction
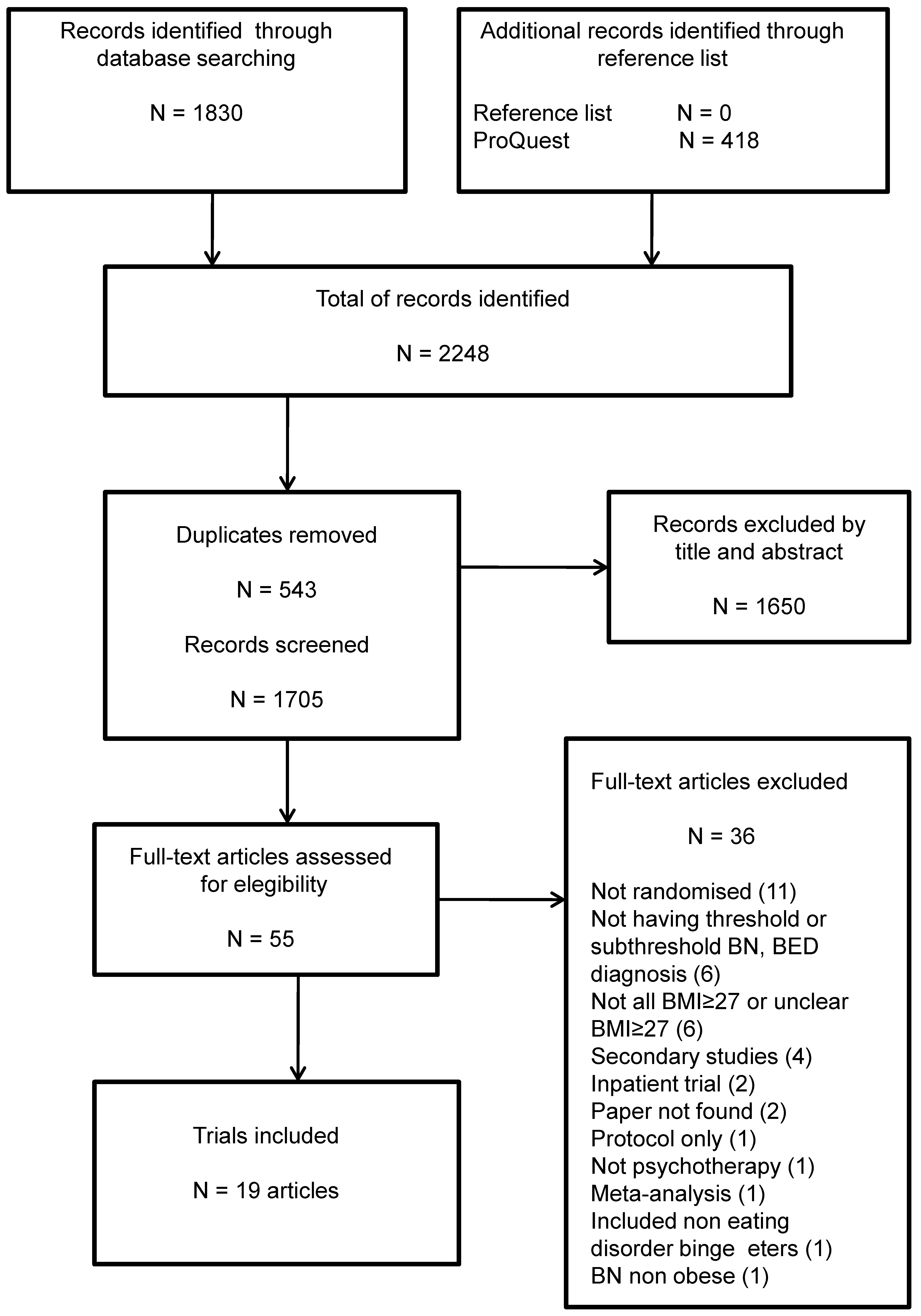
2. Materials and Methods
2.1. Literature Search Strategies
2.2. Selection Criteria
2.3. Quality Assessment
2.4. Outcome Measures
2.5. Meta-Analyses
3. Results
3.1. Characteristics of Included Trials
3.2. Quality Appraisal of Included Trials
3.3. Results of Studies Comparing Psychological Interventions for Binge Eating Disorder Associated with Obesity
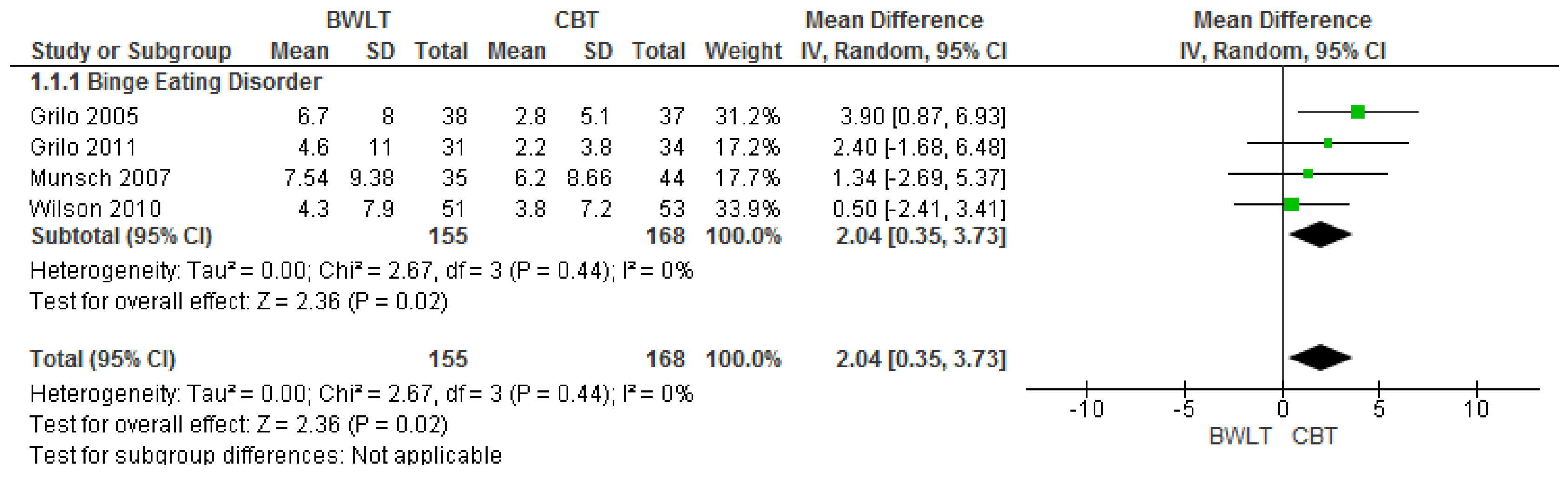
3.4. Results of Meta-Analyses of Studies Comparing BWLT versus CBT
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Conflicts of Interest
Abbreviations
| BN | Bulimia Nervosa |
| BED | Binge Eating Disorder |
| BMI | Body Mass Index |
| BWLT | Behavioural Weight Loss Therapy |
| CBT | Cognitive Behavioural Therapy |
| CBT-E | Cognitive Behavioural Therapy- Enhanced |
| CD-ROM | Compact Disc Read-Only Memory |
| CI | Confidence Intervals |
| DBT | Dialectical Behaviour Therapy |
| DSM-IV-TR | Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision |
| DSM-5 | Diagnostic and Statistical Manual of Mental Disorders, 5th Edition |
| EDs | Eating Disorders |
| EDE | Eating Disorder Examination |
| EDNOS | Eating Disorder Not Otherwise Specified |
| EMBASE | Excerpta Medica dataBASE |
| ICD-10 | International Classification of Diseases, 10th revision |
| ICD-11 | International Classification of Diseases, 11th revision |
| LILACS | Literatura Latino-Americana e do Caribe em Ciências da Saúde |
| MEDLINE | Medical Literature Analysis and Retrieval System Online |
| NCDs | Non communicable diseases |
| OSFED | Other Specified Feeding or Eating Disorder |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| RCT | Randomised Controlled Trial |
| REVMAN | Review Manager |
| SCID-I/P | Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition |
| SMD | Standardized Mean Difference |
| WHO | World Health Organization |
References
- Mitchison, D.; Hay, P.; Slewa-Younan, S.; Mond, J. The changing demographic profile of eating disorder behaviors in the community. BMC Public Health 2014, 11, 11. [Google Scholar] [CrossRef] [PubMed]
- Smink, F.R.; van Hoeken, D.; Hoek, H.W. Epidemiology, course, and outcome of eating disorders. Curr. Opin. Psychiatry 2013, 26, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Hay, P.; Girosi, F.; Mond, J. Prevalence and sociodemographic correlates of DSM-5 eating disorders in the Australian population. J. Eat. Disord. 2015, 25, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Qian, J.; Hu, Q.; Wan, Y.; Li, T.; Wu, M.; Ren, Z.; Yu, D. Prevalence of eating disorders in the general population: A systematic review. Shanghai Arch. Psychiatry 2013, 25, 212–223. [Google Scholar] [PubMed]
- American Psychiatric Association APA. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Johnson, J.G.; Spitzer, R.L.; Williams, J.B. Health problems, impairment and illnesses associated with bulimia nervosa and binge eating disorder among primary care and obstetric gynaecology patients. Psychol. Med. 2001, 31, 1455–1466. [Google Scholar] [CrossRef] [PubMed]
- Darby, A.; Hay, P.; Mond, J.; Quirk, F.; Buttner, P.; Kennedy, L. The rising prevalence of comorbid obesity and eating disorder behaviors from 1995 to 2005. Int. J. Eat. Disord. 2009, 42, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Mond, J.M.; Hay, P.J.; Paxton, S.J.; Rodgers, B.; Darby, A.; Nillson, J.; Quirk, F.; Owen, C. Eating disorders “mental health literacy” in low risk, high risk and symptomatic women: Implications for health promotion programs. Eat. Disord. 2010, 18, 267–285. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration (NCD-RisC). Trends in adult body-mass index in 200 countries from 1975 to 2014: A pooled analysis of 1698 population-based measurement studies with 19.2 million participants. Lancet 2016, 2, 1377–1396. [Google Scholar]
- Mitchell, J.E.; Devlin, M.J.; de Zwaan, M.; Crow, S.J.; Peterson, C.B. Binge-Eating Disorder: Clinical Foundations and Treatment, 1st ed.; The Guilford Press: New York, NY, USA, 2008; pp. 23–34. [Google Scholar]
- Bulik, C.M.; Marcus, M.D.; Zerwas, S.; Levine, M.D.; La Via, M. The changing “weightscape” of bulimia nervosa. Am. J. Psychiatry 2012, 169, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Hudson, J.I.; Hiripi, E.; Pope, H.G., Jr.; Kessler, R.C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol. Psychiatry 2007, 61, 348–358. [Google Scholar] [CrossRef] [PubMed]
- Clinical Practice Guidelines for the Management of Overweight and Obesity in Adults, Adolescents and Children in Australia. Available online: https://www.nhmrc.gov.au/guidelines-publications/n57 (accessed on 4 December 2016).
- Hay, P. A systematic review of evidence for psychological treatments in eating disorders: 2005–2012. Int. J. Eat. Disord. 2013, 46, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Da Luz, F.Q.; Hay, P.; Gibson, A.A.; Touyz, S.W.; Swinbourne, J.M.; Roekenes, J.A.; Sainsbury, A. Does severe dietary energy restriction increase binge eating in overweight or obese individuals? A systematic review. Obes. Rev. 2015, 16, 652–665. [Google Scholar] [CrossRef] [PubMed]
- McElroy, S.L.; Guerdjikova, A.I.; Mori, N.; Munoz, M.R.; Keck, P.E., Jr. Overview of the treatment of binge eating disorder. CNS Spectrum. 2015, 20, 546–556. [Google Scholar] [CrossRef] [PubMed]
- Wilson, G.T.; Wilfley, D.E.; Agras, S.; Bryson, S.W. Psychological treatments of binge eating disorder. Arch. Gen. Psychiatry 2010, 67, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Franz, M.J.; van Wormer, J.J.; Crain, A.L.; Boucher, J.L.; Histon, T.; Caplan, W.; Bowman, J.D.; Pronk, N.P. Weight-loss outcomes: A systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. J. Am. Diet. Assoc. 2007, 107, 1755–1767. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association APA. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines; World Health Organization: Geneva, Switzerland, 1992. [Google Scholar]
- Reed, G.M.; First, M.B.; Medina-Mora, M.E.; Gureje, O.; Pike, K.M.; Saxena, S. Draft diagnostic guidelines for ICD-11 mental and behavioural disorders available for review and comment. World Psychiatry 2016. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Cooper, Z.; O’Connor, M. The Eating Disorder Examination, 17th ed.; The Centre for Research on Eating Disorders: Oxford, UK, 2014; Available online: http://www.credo-oxford.com/pdfs/EDE_17.0D.pdf (accessed on 7 December 2016).
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Version 5.1.0; The Cochrane Collaboration: Copenhagen, Denmark, 2011; Available online: http://www.handbook.cochrane.org (accessed on 7 December 2016).
- Review Manager (RevMan). Copenhagen: The Nordic Cochrane Centre; Version 5.3; The Cochrane Collaboration: Copenhagen, Denmark, 2014. [Google Scholar]
- National Institute for Clinical Excellence (NICE). Eating Disorders—Core Interventions INTHE Treatment and Management of Anorexia Nervosa, Bulimia Nervosa and Related Eatingdisorders; NICE Clinical Practice Guideline CG9; National Institute for Clinical Excellence: London, UK, 2004; Available online: http://www.nice.org.uk/guidance/cg9 (accessed on 23 December 2016).
- Alfonsson, S.; Parling, T.; Ghaderi, A. Group behavioral activation for patients with severe obesity and binge eating disorder: A randomized controlled trial. Behav. Modif. 2015, 39, 270–294. [Google Scholar] [CrossRef] [PubMed]
- Gorin, A.A.; Le Grange, D.; Stone, A.A. Effectiveness of spouse involvement in cognitive behavioral therapy for binge eating disorder. Int. J. Eat. Disord. 2003, 33, 421–433. [Google Scholar] [CrossRef] [PubMed]
- Grilo, C.M.; Masheb, R.M. A randomized controlled comparison of guided self- help cognitive behavioral therapy and behavioral weight loss for binge eating disorder. Behav. Res. Ther. 2005, 43, 1509–1525. [Google Scholar] [CrossRef] [PubMed]
- Grilo, C.M.; Masheb, R.M.; Wilson, G.T.; Gueorguieva, R.; White, M.A. Cognitive-behavioral therapy, behavioral weight loss, and sequential treatment for obese patients with binge-eating disorder: A randomized controlled trial. J. Consult Clin. Psychol. 2011, 79, 675–685. [Google Scholar] [CrossRef] [PubMed]
- Grilo, C.M.; White, M.A.; Gueorguieva, R.; Barnes, R.D.; Masheb, R.M. Self-help for binge eating disorder in primary care: A randomized controlled trial with ethnically and racially diverse obese patients. Behav. Res. Ther. 2013, 51, 855–861. [Google Scholar] [CrossRef] [PubMed]
- Kristeller, J.; Wolever, R.Q.; Sheets, V. Mindfulness-based eating awareness training (MB-EAT) for binge eating: A randomized controlled trial. Mindfulness 2014, 5, 282–297. [Google Scholar] [CrossRef]
- Masheb, R.M.; Grilo, C.M.; Rolls, B.J. A randomized controlled trial for obesity and binge eating disorder: Low-energy-density dietary counseling and cognitive behavioral therapy. Behav. Res. Ther. 2011, 49, 821–829. [Google Scholar] [CrossRef] [PubMed]
- Munsch, S.; Biedert, E.; Meyer, A.; Michael, T.; Schlup, B.; Tuch, A.; Margraf, J. A randomized comparison of cognitive behavioral therapy and behavioral weight loss treatment for overweight individuals with binge eating disorder. Int. J. Eat. Disord. 2007, 40, 102–113. [Google Scholar] [CrossRef] [PubMed]
- Munsch, S.; Meyer, A.H.; Biedert, E. Efficacy and predictors of long-term treatment success for Cognitive-Behavioral Treatment and Behavioral Weight-Loss-Treatment in overweight individuals with binge eating disorder. Behav. Res. Ther. 2012, 50, 775–785. [Google Scholar] [CrossRef] [PubMed]
- Ricca, V.; Castellini, G.; Mannucci, E.; Lo Sauro, C.; Ravaldi, C.; Rotella, C.M.; Faravelli, C. Comparison of individual and group cognitive behavioral therapy for binge eating disorder. A randomized, three-year follow-up study. Appetite 2010, 55, 656–665. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, J.R.; Reba-Harrelson, L.; Dymek-Valentine, M.; Woolsom, S.L.; Hamer, R.M.; Bulik, C.M. Feasibility and acceptability of CD-ROM-based cognitive- behavioural treatment for binge-eating disorder. Eur. Eat. Disord. Rev. 2007, 15, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Wilfley, D.E.; Welch, R.R.; Stein, R.I.; Spurrell, E.B.; Cohen, L.R.; Saelens, B.E.; Dounchis, J.Z.; Frank, M.A.; Wiseman, C.V.; Matt, G.E. A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge-eating disorder. Arch. Gen. Psychiatry 2002, 59, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Agras, W.S.; Telch, C.F.; Arnow, B.; Eldredge, K.; Detzer, M.J.; Henderson, J.; Marnell, M. Does interpersonal therapy help patients with binge eating disorder who fail to respond to cognitive-behavioral therapy? J. Consult Clin. Psychol. 1995, 63, 356–360. [Google Scholar] [CrossRef] [PubMed]
- Dingemans, A.E.; Spinhoven, P.; van Furth, E.F. Predictors and mediators of treatment outcome in patients with binge eating disorder. Behav. Res. Ther. 2007, 45, 2551–2562. [Google Scholar] [CrossRef] [PubMed]
- Eldredge, K.L.; Agras, W.S.; Arnow, B.; Telch, C.F.; Bell, S.; Castonguay, L.; Marnell, M. The effects of extending cognitive-behavioral therapy for binge eating disorder among initial treatment nonresponders. Int. J. Eat. Disord. 1997, 21, 347–352. [Google Scholar] [CrossRef]
- Nauta, H.; Hospers, H.; Kok, G.; Jansen, A. A comparison between a cognitive and a behavioral treatment for obese binge eaters and obese non-binge eaters. Behav. Ther. 2000, 31, 441–461. [Google Scholar] [CrossRef]
- Pendleton, V.R.; Goodrick, G.K.; Poston, W.S.C.; Reeves, R.S.; Foreyt, J.P. Exercise augments the effects of cognitive-behavioral therapy in the treatment of binge eating. Int. J. Eat. Disord. 2002, 31, 172–184. [Google Scholar] [CrossRef] [PubMed]
- Safer, D.L.; Robinson, A.H.; Jo, B. Outcome from a randomized controlled trial of group therapy for binge eating disorder: Comparing dialectical behavior therapy adapted for binge eating to an active comparison group therapy. Behav. Ther. 2010, 41, 106–120. [Google Scholar] [CrossRef] [PubMed]
- First, M.B.; Spitzer, R.L.; Gibbon, M.; Williams, J.B.W. Structured Clinical Interviewfor DSM-IV Axis I Disorders-Patient Edition (SCID-I/P, Version 2.0); Biometric Research, New York State Psychiatric Institute: New York, NY, USA, 1996. [Google Scholar]
- Hay, P.; Chinn, D.; Forbes, D.; Madden, S.; Newton, R.; Sugenor, L.; Touyz, S.; Ward, W.; Royal Australian and New Zealand College of Psychiatrists. Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the treatment of eating disorders. Aust. N. Z. J. Psychiatry 2014, 48, 977–1008. [Google Scholar] [CrossRef] [PubMed]
- Iacovino, J.M.; Gredysa, D.M.; Altman, M.; Wilfley, D.E. Psychological treatments for binge eating disorder. Curr. Psychiatry Rep. 2012, 14, 432–446. [Google Scholar] [CrossRef] [PubMed]
- Vancampfort, D.; Vanderlinden, J.; De Hert, M.; Adámkova, M.; Skjaerven, L.H.; Catalán-Matamoros, D.; Lundvik-Gyllensten, A.; Gómez-Conesa, A.; Ijntema, R.; Probst, M. A systematic review on physical therapy interventions for patients with binge eating disorder. Disabil. Rehabil. 2013, 35, 2191–2196. [Google Scholar] [CrossRef] [PubMed]
| Trial | Sample | Diagnostic Criteria/Classification System (Instrument) | Intervention | Time Point of Assessments Relative to the Start of the Interventions | End of Treatment Outcomes (Binge Remission/Frequency and BMI/Weight Loss) | Follow-Up of Active Treatments Outcomes (Binge Remission/Frequency and BMI/Weight Loss) |
|---|---|---|---|---|---|---|
| Trials which all participants had BMI ≥ 27 and the eating disorder diagnosis was determined by a validated instrument | ||||||
| Alfonsson et al. Sweden/2015 [27] | n = 100# 94%♀/6%♂ Mean age 44.3 Mean BMI 41.1 | BED/DSM-5 (EDE) | 1. Behavioural activation 2. Delayed treatment Group sessions | Baseline EoT 10 weeks FU 3–6 months | No differences between groups in binge eating frequency. No BMI results. | Only for active treatment – no comparison. |
| Gorin et al. USA/2003 [28] | n = 94# 100%♀ Mean age 45.2 Mean BMI 39.42 | BED/DSM-IV (SCID-I/P) | 1. Standard cognitive behavioural therapy 2. CBT-spouse involvement 3. Delayed treatment Group sessions | Baseline EoT 12 weeks FU 6 months | Comparison between active treatments: no differences in binge eating frequency or BMI. Active treatments compared to wait-list: better results for binge eating frequency and BMI for CBT groups. | Only comparison between active treatments: no differences in binge eating frequency or BMI. |
| Grilo and Masheb USA/2005 [29] | n = 90 79%♀/21♂ Mean age 46.3 Mean BMI 35.5 | BED/DSM-IV (SCID-I/P+EDE) | 1. CBTgsh 2. BWLgsh 3. Self-monitoring control Individual sessions | Baseline EoT 12 weeks | CBTgsh had greater results for binge eating frequency compared to BWLgsh and the control. No differences between groups for BMI. | No follow-up. |
| Grilo et al. USA/2011 [30] | n = 125# 67%♀/33%♂ Mean age 44.8 Mean BMI 38.8 | BED/DSM-IV (SCIDI/P+ EDE) | 1. CBT 2. BWL 3. CBT + BWL Group sessions | Baseline EoT 24 weeks (CBT and BWL) FU 6–12 months | No differences between groups in binge remission and binge eating frequency. BWLT and CBT + BWL had significant greater per cent BMI loss than CBT. | No differences between groups in binge remission rates. Binge eating frequency significantly lower in CBT than BWL at both follow-up. At six-month significant BMI loss in BWL than CBT, but not sustained at 12-month. |
| Grilo et al. USA/2013 [31] | n = 48 79%♀/21%♂ Mean age 45.8 Mean BMI 37.62 | Threshold and subthreshold BED/DSM-IV (SCID-I/P + EDE) | 1. Self-help CBT 2. Usual care Self-help | Baseline EoT 4 months | No differences between groups in binge remission, frequency of binge eating or BMI. | No follow-up. |
| Kristeller et al. USA/2014 [32] | n = 150# 88%♀/12%♂ Mean age 46.5 Mean BMI 40.2 | Threshold and subthreshold BED/DSM-IV-R (EDE) | 1. Mindfulness-based eating awareness training 2. Psychoeducational cognitive-behavioural treatment 3. Delayed treatment Group sessions | Baseline EoT 1 month FU 4 months | Comparison between active treatments: no differences in binge eating frequency or BMI. Active treatments compared to wait-list: better results for binge eating frequency and BMI for both active interventions. | Same results found at end of treatment. |
| Masheb et al. USA/2011 [33] | n = 50# 76%♀/24♂ Mean age 45.8 Mean BMI 39.1 | BED/DSM-IV-TR (SCID-I/P+EDE) | 1. CBT + low-energy- density diet 2. CBT + general nutrition Individual sessions | Baseline EoT 6 months FU 12 months | No differences between groups in binge remission or BMI. | Same results found at end of treatment. |
| Munsch et al. Switzerland/2007 [34] and Munsch et al. Switzerland/2012 [35] | n = 80 89%♀/11%♂ Mean age 46.1 Mean BMI 34.0 n = 52 90%♀/10%♂ Mean age 52.3 Mean BMI 32.5 | BED/DSM-IV-TR (EDE) BED/DSM-IV-TR (EDE-Q) | 1. CBT 2. BWLT Group sessions | Baseline EoT 4 months FU 12 months FU 6 years | CBT improved significantly for binge remission and binge eating frequency. However, BWLT was significantly better in weight loss. | No differences between groups in binge remission, binge eating frequency or BMI. Comparing the end of treatment to six-year follow-up, these outcomes significantly worsened. Comparing the baseline to six-year follow-up these measures still improved with medium to large effect sizes. |
| Ricca et al. Italy/2010 [36] | n = 144# 86%♀/14%♂ Mean age 46.9 Mean BMI 38.1 | Threshold and subthreshold BED/DSM-IV (SCID-I/P) | 1. Individual CBT 2. Group CBT | Baseline EoT 24 weeks for I-CBT 22 weeks for G-CBT FU 3 years | No differences between groups in reduction of binge eating episodes and BMI. | Same results found at end of treatment. |
| Shapiro et al. USA/2007 [37] | n = 66 92%♀/8%♂ Mean age 39.5 Mean BMI 37.3 | Threshold and subthreshold BED/DSM-IV (SCID-I/P) | 1. Group CBT 2. CD-ROM 3. Delayed treatment | Baseline EoT 10 weeks FU 2 months | No differences between groups in binge eating frequency or BMI. | Same results found at end of treatment. |
| Wilfley et al. USA/2002 [38] | n = 162 83%♀/17%♂ Mean age 45.2 Mean BMI 37.4 | BED/DSM-IV (SCID for DSM-III-R + EDE) | 1. CBT 2. Interpersonal therapy Group sessions + three individual sessions | Baseline EoT 20 weeks FU 4–8–12 months | No differences between groups in binge eating frequency or BMI. | Same results found at end of treatment. |
| Wilson et al. USA/2010 [17] | n = 205# 79%♀/21%♂ Mean age 48.4 Mean BMI 36.4 | BED/DSM-IV (SCID-I + EDE) | 1. CBTgsh 2. Interpersonal therapy 3. BWLT Individual sessions for Interpersonal therapy and BWLT | Baseline EoT 24 weeks FU 12–24 months | No differences between groups in binge remission and binge eating frequency. BWLT was significantly more effective in BMI reduction than the two other treatments. | 1-year FU: no differences between groups in measures of binge eating and more significant BMI gain for the BWL group compared to CBTgsh group. Two-year FU: IPT and CBTgsh were more effective for remission of binge episodes. No difference for BMI comparing all groups. |
| Trials which included under 10% participants with BMI ≤ 27 and/or the eating disorder diagnosis was not determined by a validated instrument | ||||||
| Agras et al. USA/1995 [39] | n = 50 86%♀/14%♂ Mean age 47.6 Mean BMI 37.1 | BED/not specified (Structured clinical interview) | 1. CBT 12 weeks followed by 12 weeks of either IPT for non -responders or weight loss therapy for responders to CBT 2. Delayed treatment Group sessions | Baseline EoT 24 weeks | Active treatment compared to wait-list: better results for binge eating frequency and BMI for active intervention. IPT group: binge eating increased and weight increased with IPT not significant. Weight loss therapy: significant weight loss and maintained reduced binge eating. | No follow-up. |
| Dingemans et al. Netherlands/ 2007 [40] | n = 52 94%♀/6%♂ Mean age 37.6 Mean BMI 39.0 n = BMI < 27 * | BED/DSM-IV (Instrument not specified) | 1. CBT 2. Delayed treatment Group sessions | Baseline EoT 20 weeks FU 12 months | Significant binge remission and reduction in frequency in binge eating in CBT group. No significant BMI change. | Only for active treatment—no comparison. |
| Eldredge et al. USA/1997 [41] | n = 46 96%♀/4%♂ Mean age 45.2 Mean BMI 38.4 | BED (No other information) | 1. CBT 2. Delayed treatment Group sessions | Baseline EoT 12 weeks FU 24 weeks | Significant binge remission and reduction in frequency in binge eating in CBT group. No significant BMI change. | No information. |
| Nauta et al. Netherlands/2000 [42] | n = 74 100% ♀ Mean age 38.3 Mean BMI 33.1 Mixed sample of binge eating and non-binge eating participants | BED/DSM-IV (Structured interview) | 1. Cognitive treatment 2. Behavioural treatment Group sessions | Baseline EoT 15 weeks FU 6 months | At post-treatment 67% binge abstinence with cognitive treatment vs. 44% abstinence with behavioural treatment in obese binge eating participants. Other outcomes not reported separately for binge eating participants. | 86% binge abstinence with cognitive treatment vs. 44% abstinence with behavioural treatment in obese binge eating participants (significant p < 0.01). |
| Pendleton et al. USA/2002 [43] | n = 114 100% ♀ Mean age 45.0 Men BMI 36.2 | BED (no other information) | 1. CBT + exercise + maintenance 2. CBT + exercise − maintenance 3. CBT − exercise + maintenance 4. CBT − exercise − maintenance Group sessions | Baseline EoT 4 months FU 6–12 months | Exercisers had significantly greater reduction in binge frequency and BMI compared to non-exercisers groups. Addition of the maintenance program did not influence on binge eating behaviour but influenced changes in BMI. | Same results found at end of treatment. |
| Safer et al. USA/2010 [44] | n = 101 85% ♀/15%♂ Mean age 52.2 Mean BMI 36.3 n = 9 BMI < 27 * | BED/DSM-IV (EDE) | 1. Dialectical behaviour therapy adapted for binge eating (DBT-BED) 2. Active comparison group therapy (ACGT) Group sessions | Baseline EoT 21 weeks FU 3, 6, and 12 months | DBT-BED group achieved significant reduction in binge frequency than ACGT group. No differences found between groups for BMI. | No differences between groups in binge eating frequency or BMI. |
| Reference | Randomisation and Allocation Concealment | Blinding | Treatment Attrition | Reporting Bias | Overall Risk of Bias (Modal Assessment) |
|---|---|---|---|---|---|
| Trials which all participants had BMI > 27 kg/m2 and the eating disorder diagnosis was determined by a validated instrument | |||||
| Alfonsson et al. # 2015 [27] | Adequate randomisation Unclear allocation concealment Unclear RoB | No blinding High RoB | EoT 32% Unclear RoB | Used ITT MEM Trial registration not reported Unclear RoB | Unclear |
| Gorin et al. # 2003 [28] | Unclear randomisation and allocation concealment Unclear RoB | No blinding High RoB | EoT not reported Assessment attrition 34% Unclear RoB | Used ITT/LOCF Participant flow not reported Trial registration not reported Unclear RoB | Unclear |
| Grilo and Masheb 2005 [29] | Adequate randomisation and allocation concealment Low RoB | No blinding except for participant expectations High RoB | EoT 22% Attrition higher (33%) in BWLgsh Unclear RoB | Used ITT/LOCF Participant flow reported Trial registration not reported Unclear RoB | Unclear |
| Grilo et al. # 2011 [30] | Adequate randomisation Unclear allocation concealment Unclear RoB | No blinding High RoB | EoT 31% Unclear RoB | Used ITT/MEM Participant flow reported Trial registered, outcomes unchanged from protocol Low RoB | Unclear |
| Grilo et al. 2013 [31] | Adequate randomisation and allocation concealment Low Rob | Outcome assessment assessor blind Participants could not be blind Unclear RoB | No EoT attrition Low RoB | Used ITT/MEM Participant flow reported Trial registration not reported Unclear RoB | Unclear |
| Kristeller et al. # 2014 [32] | Inadequate randomisation Unclear allocation concealment High RoB | Unclear blinding Unclear RoB | Attrition 30% greater in control conditions but not significant Unclear RoB | Used ITT/MEM Participant flow reported Trial registration not reported Unclear RoB | Unclear |
| Masheb et al.# 2011 [33] | Adequate randomisation and allocation concealment Low Rob | Outcome assessment assessor blind Participants not reported blind Unclear RoB | EoT 14% Low RoB | Used ITT/MEM/LOCF Participant flow reported Trial registration reported Low RoB | Low |
| Munsch et al. 2007 [34] /2012 [35] | Unclear randomisation and allocation concealment Unclear RoB | Outcome assessment assessor not blind Participants blind unclear High RoB | EoT 27.5% Unclear RoB | Used ITT/LOCF and completer for univariate models Participant flow reported Trial registration not reported Unclear RoB | Unclear |
| Ricca et al. # 2010 [36] | Adequate randomisation and allocation concealment Low Rob | Outcome assessment assessor blind Participants could not be blind Unclear RoB | EoT 4.9% Low RoB | Used ITT/LOCF Participant flow reported Trial registration not reported Unclear RoB | Unclear |
| Shapiro et al. 2007 [37] | Unclear randomisation and allocation concealment Unclear RoB | Outcome assessment not blind Participants could not be blind. High RoB | EoT 41% High RoB | Used ITT/MEM Participant flow not reported Trial registration not reported Unclear RoB | High |
| Wilfley et al. 2002 [38] | Unclear randomisation and allocation concealment Unclear RoB | Blinding only for treatment fidelity assessment Assessors not consistently blind Participants blind unclear High RoB | EoT 9.9% Low RoB | Used ITT method unclear and completer analyses Participant flow reported Retrospective trial registered Unclear RoB | Unclear |
| Wilson et al. # 2010 [17] | Adequate randomisation Unclear allocation concealment Unclear RoB | Outcome assessment assessor blind Participants blinding unclear Unclear RoB | EoT 23.1% EoT Attrition 7% IPT/28% BWL/30% CBTgsh IPT significant lower attrition Unclear RoB | Used ITT/MEM Participant flow reported Trial registration reported Low RoB | Unclear |
| Trials which either did not use a validated instrument for eating disorder diagnosis and/or included under 10% participants with BMI < 27 kg/m2 | |||||
| Agras et al. 1995 [39] | Unclear randomisation and allocation concealment Unclear RoB | Unclear blinding Unclear RoB | EoT 12.8% Low RoB | Used ITT/LOCF and completer only analysis Participant flow not reported Trial registration not reported Unclear RoB | Unclear |
| Dingemans et al. 2007 [40] | Unclear randomisation Adequate allocation concealment Unclear RoB | Assessor blind to group Participants could not be blind Unclear RoB | EoT 7% Low RoB | Used MLA analysis Participant flow reported Trial registration not reported Unclear RoB | Unclear |
| Eldredge et al. 1997 [41] | Unclear randomisation and allocation concealment Unclear RoB | No blinding High RoB | EoT 19% Low RoB | No ITT reported Participant flow not reported Trial registration not reported High RoB | High |
| Nauta et al. 2000 [42] | Unclear randomisation and allocation concealment Unclear RoB | Blind not reported High RoB | EoT 13.5% Low RoB | Used ITT repeated-measures multivariate and univariate analysis of variance Participant flow not reported Trial registration not reported Unclear RoB | Unclear |
| Pendleton et al. 2002 [43] | Unclear randomisation and allocation concealment Unclear RoB | Unclear blinding Unclear RoB | EoT attrition unclear Assessment attrition 22.8% Unclear RoB | Not used ITT Participant flow not reported Trial registration not reported High RoB | Unclear |
| Safer et al. 2010 [44] | Unclear randomisation and allocation concealment Unclear RoB | No blinding reported Unclear RoB | EoT 19% but higher 33% in control group and 10% in DBT Unclear RoB | Used linear mixed models analysis Participant flow reported Trial registered Low RoB | Unclear |
| High Risk | Low Risk | Unclear Risk | |
|---|---|---|---|
| Randomisation and Allocation Concealment | n = 1 | n = 4 | n = 14 |
| [32] | [29,31,33,36] | [17,27,28,30,34,35,37,44] | |
| Blinding | n = 10 | n = 0 | n = 9 |
| [27,28,29,30,34,35,37,38,41,42] | [17,31,32,33,36,39,40,43,44] | ||
| Treatment Attrition | n = 1 | n = 8 | n = 10 |
| [37] | [31,33,36,38,39,40,41,42] | [17,27,28,29,30,32,34,35,43,44] | |
| Reporting Bias | n = 2 | n = 4 | n = 13 |
| [41,43] | [17,30,33,44] | [27,28,29,31,32,34,35,36,37,38,39,40,42] | |
| Overall Risk of Bias (Modal Assessment) | n = 2 | n = 1 | n = 16 |
| [37,41] | [33] | [17,27,28,29,30,31,32,34,35,36,38,39,40,42,43,44] |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palavras, M.A.; Hay, P.; Filho, C.A.d.S.; Claudino, A. The Efficacy of Psychological Therapies in Reducing Weight and Binge Eating in People with Bulimia Nervosa and Binge Eating Disorder Who Are Overweight or Obese—A Critical Synthesis and Meta-Analyses. Nutrients 2017, 9, 299. https://doi.org/10.3390/nu9030299
Palavras MA, Hay P, Filho CAdS, Claudino A. The Efficacy of Psychological Therapies in Reducing Weight and Binge Eating in People with Bulimia Nervosa and Binge Eating Disorder Who Are Overweight or Obese—A Critical Synthesis and Meta-Analyses. Nutrients. 2017; 9(3):299. https://doi.org/10.3390/nu9030299
Chicago/Turabian StylePalavras, Marly Amorim, Phillipa Hay, Celso Alves dos Santos Filho, and Angélica Claudino. 2017. "The Efficacy of Psychological Therapies in Reducing Weight and Binge Eating in People with Bulimia Nervosa and Binge Eating Disorder Who Are Overweight or Obese—A Critical Synthesis and Meta-Analyses" Nutrients 9, no. 3: 299. https://doi.org/10.3390/nu9030299
APA StylePalavras, M. A., Hay, P., Filho, C. A. d. S., & Claudino, A. (2017). The Efficacy of Psychological Therapies in Reducing Weight and Binge Eating in People with Bulimia Nervosa and Binge Eating Disorder Who Are Overweight or Obese—A Critical Synthesis and Meta-Analyses. Nutrients, 9(3), 299. https://doi.org/10.3390/nu9030299




