Strawberries Improve Pain and Inflammation in Obese Adults with Radiographic Evidence of Knee Osteoarthritis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
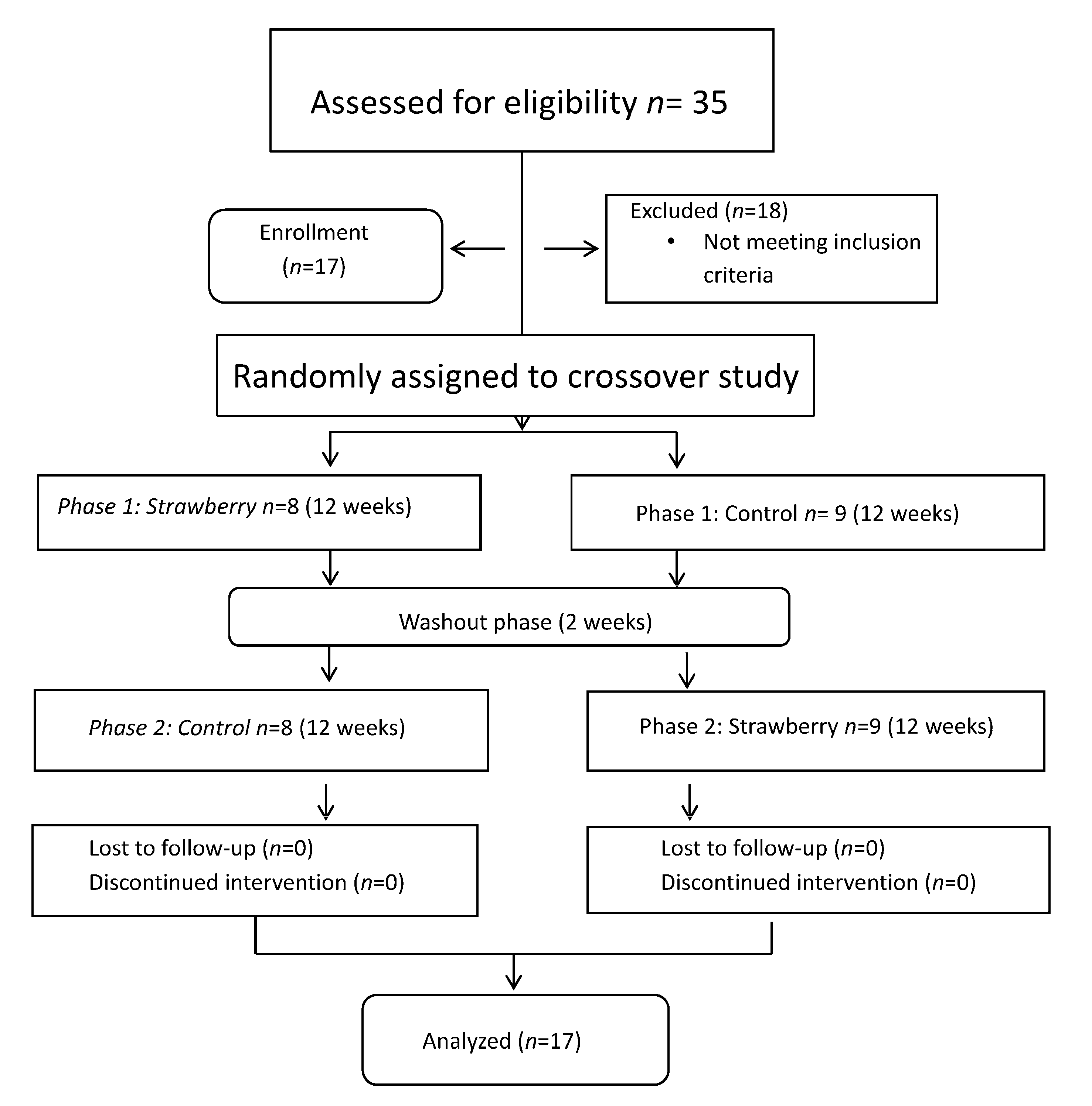
2.2. Study Design and Intervention
2.3. Biochemical Variables
2.4. Pain Scores and Quality of Life Indicators
2.5. Dietary Analysis
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Hochberg, M.C.; Altman, R.D.; April, K.T.; Benkhalti, M.; Guyatt, G.; McGowan, J.; Towheed, T.; Welch, V.; Wells, G.; Tugwell, P.; et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. (Hoboken) 2012, 64, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Meneses, S.R.; Goode, A.P.; Nelson, A.E.; Lin, J.; Jordan, J.M.; Allen, K.D.; Bennell, K.L.; Lohmander, L.S.; Fernandes, L.; Hochberg, M.C.; et al. Clinical algorithms to aid osteoarthritis guideline dissemination. Osteoarthr. Cartil. 2016. [Google Scholar] [CrossRef]
- McAlindon, T.E.; Bannuru, R.R.; Sullivan, M.C.; Arden, N.K.; Berenbaum, F.; Bierma-Zeinstra, S.M.; Hawker, G.A.; Henrotin, Y.; Hunter, D.J.; Kawaguchi, H.; et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthr. Cartil. 2014, 22, 363–388. [Google Scholar] [CrossRef] [PubMed]
- Wandel, S.; Juni, P.; Tendal, B.; Nuesch, E.; Villiger, P.M.; Welton, N.J.; Reichenbach, S.; Trelle, S. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: Network meta-analysis. BMJ 2010, 341, c4675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Christiansen, B.A.; Bhatti, S.; Goudarzi, R.; Emami, S. Management of Osteoarthritis with Avocado/Soybean Unsaponifiables. Cartilage 2015, 6, 30–44. [Google Scholar] [CrossRef] [PubMed]
- Ameye, L.G.; Chee, W.S. Osteoarthritis and nutrition. From nutraceuticals to functional foods: A systematic review of the scientific evidence. Arthr. Res. Ther. 2006, 8, R127. [Google Scholar] [CrossRef] [PubMed]
- Grotle, M.; Hagen, K.B.; Natvig, B.; Dahl, F.A.; Kvien, T.K. Obesity and osteoarthritis in knee, hip and/or hand: An epidemiological study in the general population with 10 years follow-up. BMC Musculoskelet. Disord. 2008, 9, 132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thijssen, E.; van Caam, A.; van der Kraan, P.M. Obesity and osteoarthritis, more than just wear and tear: Pivotal roles for inflamed adipose tissue and dyslipidaemia in obesity-induced osteoarthritis. Rheumatology (Oxf.) 2015, 54, 588–600. [Google Scholar] [CrossRef] [PubMed]
- Perruccio, A.V.; Chandran, V.; Power, J.D.; Kapoor, M.; Mahomed, N.N.; Gandhi, R. Systemic inflammation and painful joint burden in osteoarthritis: A matter of sex? Osteoarthr. Cartil. 2017, 25, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.; Englund, M.; Struglics, A.; Lohmander, L.S. Interleukin-6 and tumor necrosis factor alpha in synovial fluid are associated with progression of radiographic knee osteoarthritis in subjects with previous meniscectomy. Osteoarthr. Cartil. 2015, 23, 1906–1914. [Google Scholar] [CrossRef] [PubMed]
- Ling, S.M.; Patel, D.D.; Garnero, P.; Zhan, M.; Vaduganathan, M.; Muller, D.; Taub, D.; Bathon, J.M.; Hochberg, M.; Abernethy, D.R.; et al. Serum protein signatures detect early radiographic osteoarthritis. Osteoarthr. Cartil. 2009, 17, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Pelletier, J.P.; Raynauld, J.P.; Caron, J.; Mineau, F.; Abram, F.; Dorais, M.; Haraoui, B.; Choquette, D.; Martel-Pelletier, J. Decrease in serum level of matrix metalloproteinases is predictive of the disease-modifying effect of osteoarthritis drugs assessed by quantitative MRI in patients with knee osteoarthritis. Ann. Rheum. Dis. 2010, 69, 2095–2101. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Rahimnia, A.R.; Sharafi, M.; Alishiri, G.; Saburi, A.; Sahebkar, A. Curcuminoid treatment for knee osteoarthritis: A randomized double-blind placebo-controlled trial. Phytother. Res. 2014, 28, 1625–1631. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Alishiri, G.H.; Parvin, S.; Sahebkar, A. Mitigation of Systemic Oxidative Stress by Curcuminoids in Osteoarthritis: Results of a Randomized Controlled Trial. J. Diet. Suppl. 2016, 13, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Naderi, Z.; Mozaffari-Khosravi, H.; Dehghan, A.; Nadjarzadeh, A.; Huseini, H.F. Effect of ginger powder supplementation on nitric oxide and C-reactive protein in elderly knee osteoarthritis patients: A 12-week double-blind randomized placebo-controlled clinical trial. J. Tradit. Complement. Med. 2016, 6, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Hashempur, M.H.; Sadrneshin, S.; Mosavat, S.H.; Ashraf, A. Green tea (Camellia sinensis) for patients with knee osteoarthritis: A randomized open-label active-controlled clinical trial. Clin. Nutr. 2016. [Google Scholar] [CrossRef] [PubMed]
- Connelly, A.E.; Tucker, A.J.; Tulk, H.; Catapang, M.; Chapman, L.; Sheikh, N.; Yurchenko, S.; Fletcher, R.; Kott, L.S.; Duncan, A.M.; et al. High-rosmarinic acid spearmint tea in the management of knee osteoarthritis symptoms. J. Med. Food 2014, 17, 1361–1367. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, A.; O’Reilly, E.J.; Kay, C.; Sampson, L.; Franz, M.; Forman, J.P.; Curhan, G.; Rimm, E.B. Habitual intake of flavonoid subclasses and incident hypertension in adults. Am. J. Clin. Nutr. 2011, 93, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Wedick, N.M.; Pan, A.; Cassidy, A.; Rimm, E.B.; Sampson, L.; Rosner, B.; Willett, W.; Hu, F.B.; Sun, Q.; van Dam, R.M. Dietary flavonoid intakes and risk of type 2 diabetes in US men and women. Am. J. Clin. Nutr. 2012, 95, 925–933. [Google Scholar] [CrossRef] [PubMed]
- Cassidy, A.; Rogers, G.; Peterson, J.J.; Dwyer, J.T.; Lin, H.; Jacques, P.F. Higher dietary anthocyanin and flavonol intakes are associated with anti-inflammatory effects in a population of US adults. Am. J. Clin. Nutr. 2015, 102, 172–181. [Google Scholar] [CrossRef] [PubMed]
- Figueira, M.E.; Camara, M.B.; Direito, R.; Rocha, J.; Serra, A.T.; Duarte, C.M.; Fernandes, A.; Freitas, M.; Fernandes, E.; Marques, M.C.; et al. Chemical characterization of a red raspberry fruit extract and evaluation of its pharmacological effects in experimental models of acute inflammation and collagen-induced arthritis. Food Funct. 2014, 5, 3241–3251. [Google Scholar] [CrossRef] [PubMed]
- Figueira, M.E.; Oliveira, M.; Direito, R.; Rocha, J.; Alves, P.; Serra, A.T.; Duarte, C.; Bronze, R.; Fernandes, A.; Brites, D.; et al. Protective effects of a blueberry extract in acute inflammation and collagen-induced arthritis in the rat. Biomed. Pharmacother. 2016, 83, 1191–1202. [Google Scholar] [CrossRef] [PubMed]
- Basu, A.; Du, M.; Leyva, M.J.; Sanchez, K.; Betts, N.M.; Wu, M.; Aston, C.E.; Lyons, T.J. Blueberries decrease cardiovascular risk factors in obese men and women with metabolic syndrome. J. Nutr. 2010, 140, 1582–1587. [Google Scholar] [CrossRef]
- Basu, A.; Betts, N.M.; Nguyen, A.; Newman, E.D.; Fu, D.; Lyons, T.J. Freeze-dried strawberries lower serum cholesterol and lipid peroxidation in adults with abdominal adiposity and elevated serum lipids. J. Nutr. 2014, 144, 830–837. [Google Scholar] [CrossRef] [PubMed]
- Basu, A.; Wilkinson, M.; Penugonda, K.; Simmons, B.; Betts, N.M.; Lyons, T.J. Freeze-dried strawberry powder improves lipid profile and lipid peroxidation in women with metabolic syndrome: Baseline and post intervention effects. Nutr. J. 2009, 8, 43. [Google Scholar] [CrossRef] [PubMed]
- Peat, G.; Thomas, E.; Duncan, R.; Wood, L.; Hay, E.; Croft, P. Clinical classification criteria for knee osteoarthritis: Performance in the general population and primary care. Ann. Rheum. Dis. 2006, 65, 1363–1367. [Google Scholar] [CrossRef] [PubMed]
- Seeram, N.P.; Lee, R.; Heber, D. Bioavailability of ellagic acid in human plasma after consumption of ellagitannins from pomegranate (Punica granatum L.) juice. Clin. Chim. Acta 2004, 348, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.P.; Sankar, A.; Venkataramanan, V.; Lohmander, L.S.; Katz, J.N.; Hawker, G.A.; Gossec, L.; Roos, E.M.; Maillefert, J.F.; Kloppenburg, M.; et al. Cross-cultural validation of the ICOAP and physical function short forms of the HOOS and KOOS in a multi-country study of patients with hip and knee osteoarthritis. Osteoarthr. Cartil. 2016, 24, 2077–2081. [Google Scholar] [CrossRef]
- Risser, R.C.; Hochberg, M.C.; Gaynor, P.J.; D’Souza, D.N.; Frakes, E.P. Responsiveness of the Intermittent and Constant Osteoarthritis Pain (ICOAP) scale in a trial of duloxetine for treatment of osteoarthritis knee pain. Osteoarthr. Cartil. 2013, 21, 691–694. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.L.; Kim, D.; Jang, E.J.; Lee, M.Y.; Song, H.J.; Park, S.Y.; Cha, H.S.; Choe, J.Y.; Chung, W.T.; Hong, S.J.; et al. Mapping health assessment questionnaire disability index (HAQ-DI) score, pain visual analog scale (VAS), and disease activity score in 28 joints (DAS28) onto the EuroQol-5D (EQ-5D) utility score with the KORean Observational study Network for Arthritis (KORONA) registry data. Rheumatol. Int. 2016, 36, 505–513. [Google Scholar]
- Messier, S.P.; Mihalko, S.L.; Legault, C.; Miller, G.D.; Nicklas, B.J.; DeVita, P.; Beavers, D.P.; Hunter, D.J.; Lyles, M.F.; Eckstein, F.; et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: The IDEA randomized clinical trial. JAMA 2013, 310, 1263–1273. [Google Scholar] [CrossRef] [PubMed]
- Andriacchi, T.P.; Favre, J. The nature of in vivo mechanical signals that influence cartilage health and progression to knee osteoarthritis. Curr. Rheumatol. Rep. 2014, 16, 463. [Google Scholar] [CrossRef]
- Muraki, S.; Akune, T.; En-Yo, Y.; Yoshida, M.; Suzuki, T.; Yoshida, H.; Ishibashi, H.; Tokimura, F.; Yamamoto, S.; Tanaka, S.; et al. Joint space narrowing, body mass index, and knee pain: The ROAD study (OAC1839R1). Osteoarthr. Cartil. 2015, 23, 874–881. [Google Scholar] [CrossRef] [PubMed]
- Regan, E.; Flannelly, J.; Bowler, R.; Tran, K.; Nicks, M.; Carbone, B.D.; Glueck, D.; Heijnen, H.; Mason, R.; Crapo, J.; et al. Extracellular superoxide dismutase and oxidant damage in osteoarthritis. Arthr. Rheum. 2005, 52, 3479–3491. [Google Scholar] [CrossRef] [PubMed]
- Basu, A.; Nguyen, A.; Betts, N.M.; Lyons, T.J. Strawberry as a functional food: An evidence-based review. Crit. Rev. Food Sci. Nutr. 2014, 54, 790–806. [Google Scholar] [CrossRef] [PubMed]
- Belcaro, G.; Dugall, M.; Luzzi, R.; Ledda, A.; Pellegrini, L.; Cesarone, M.R.; Hosoi, M.; Errichi, M. Meriva(R) + Glucosamine versus Condroitin + Glucosamine in patients with knee osteoarthritis: An observational study. Eur. Rev. Med. Pharmacol. Sci. 2014, 18, 3959–6393. [Google Scholar] [PubMed]
- Ruyssen-Witrand, A.; Fernandez-Lopez, C.J.; Gossec, L.; Anract, P.; Courpied, J.P.; Dougados, M. Psychometric properties of the OARSI/OMERACT osteoarthritis pain and functional impairment scales: ICOAP, KOOS-PS and HOOS-PS. Clin. Exp. Rheumatol. 2011, 29, 231–237. [Google Scholar] [PubMed]
- Mabey, T.; Honsawek, S.; Saetan, N.; Poovorawan, Y.; Tanavalee, A.; Yuktanandana, P. Angiogenic cytokine expression profiles in plasma and synovial fluid of primary knee osteoarthritis. Int. Orthop. 2014, 38, 1885–1892. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, M.; Martel-Pelletier, J.; Lajeunesse, D.; Pelletier, J.P.; Fahmi, H. Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat. Rev. Rheumatol. 2011, 7, 33–42. [Google Scholar] [CrossRef]
- Burrage, P.S.; Mix, K.S.; Brinckerhoff, C.E. Matrix metalloproteinases: Role in arthritis. Front. Biosci. 2006, 11, 529–543. [Google Scholar] [CrossRef] [PubMed]
- Comblain, F.; Sanchez, C.; Lesponne, I.; Balligand, M.; Serisier, S.; Henrotin, Y. Curcuminoids extract, hydrolyzed collagen and green tea extract synergically inhibit inflammatory and catabolic mediator’s synthesis by normal bovine and osteoarthritic human chondrocytes in monolayer. PLoS ONE 2015, 10, e0121654. [Google Scholar] [CrossRef] [PubMed]
- Nirmal, P.S.; Jagtap, S.D.; Narkhede, A.N.; Nagarkar, B.E.; Harsulkar, A.M. New herbal composition (OA-F2) protects cartilage degeneration in a rat model of collagenase induced osteoarthritis. BMC Complement. Altern. Med. 2017, 17, 6. [Google Scholar] [CrossRef] [PubMed]
- Rahimnia, A.R.; Panahi, Y.; Alishiri, G.; Sharafi, M.; Sahebkar, A. Impact of Supplementation with Curcuminoids on Systemic Inflammation in Patients with Knee Osteoarthritis: Findings from a Randomized Double-Blind Placebo-Controlled Trial. Drug. Res. (Stuttg.) 2015, 65, 521–525. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, Y.; Mukai, S.; Yamada, S.; Matsuoka, M.; Tarumi, E.; Hashimoto, T.; Tamura, C.; Imaizumi, A.; Nishihira, J.; Nakamura, T.; et al. Short-term effects of highly-bioavailable curcumin for treating knee osteoarthritis: A randomized, double-blind, placebo-controlled prospective study. J. Orthop. Sci. 2014, 19, 933–939. [Google Scholar] [CrossRef]
- Manicourt, D.H.; Azria, M.; Mindeholm, L.; Thonar, E.J.; Devogelaer, J.P. Oral salmon calcitonin reduces Lequesne’s algofunctional index scores and decreases urinary and serum levels of biomarkers of joint metabolism in knee osteoarthritis. Arthr. Rheum. 2006, 54, 3205–3211. [Google Scholar] [CrossRef] [PubMed]
- Martel-Pelletier, J.; Raynauld, J.P.; Mineau, F.; Abram, F.; Paiement, P.; Delorme, P.; Pelletier, J. Levels of serum biomarkers from a two-year multicentre trial are associated with treatment response on knee osteoarthritis cartilage loss as assessed by magnetic resonance imaging: An exploratory study. Arthr. Res. Ther. 2017, 19, 169. [Google Scholar] [CrossRef] [PubMed]
- Kullich, W.C.; Niksic, F.; Klein, G. Effect of nimesulide on metalloproteinases and matrix degradation in osteoarthritis: A pilot clinical study. Int. J. Clin. Pract. Suppl. 2002, 128, 24–29. [Google Scholar]
- Bellometti, S.; Richelmi, P.; Tassoni, T.; Berte, F. Production of matrix metalloproteinases and their inhibitors in osteoarthritic patients undergoing mud bath therapy. Int. J. Clin. Pharmacol. Res. 2005, 25, 77–94. [Google Scholar] [PubMed]
- Livshits, G.; Zhai, G.; Hart, D.J.; Kato, B.S.; Wang, H.; Williams, F.M.; Spector, T.D. Interleukin-6 is a significant predictor of radiographic knee osteoarthritis: The Chingford Study. Arthr. Rheum. 2009, 60, 2037–2045. [Google Scholar] [CrossRef] [PubMed]
- Esposito, K.; Marfella, R.; Ciotola, M.; Di Palo, C.; Giugliano, F.; Giugliano, G.; D’Armiento, M.; D’Andrea, F.; Giugliano, D. Effect of a mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: A randomized trial. JAMA 2004, 292, 1440–1446. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beavers, K.M.; Beavers, D.P.; Newman, J.J.; Anderson, A.M.; Loeser, R.F., Jr.; Nicklas, B.J.; Lyles, M.F.; Miller, G.D.; Mihalko, S.L.; Messier, S.P. Effects of total and regional fat loss on plasma CRP and IL-6 in overweight and obese, older adults with knee osteoarthritis. Osteoarthr. Cartil. 2015, 23, 249–256. [Google Scholar] [CrossRef] [PubMed]
| Nutrients/Compounds | Strawberry Powder | Control Powder |
|---|---|---|
| Dose, g | 50 | 50 |
| Calories, kcal | 160 | 172 |
| Carbohydrates, g | 35 | 38 |
| Total polyphenols, mg GAE | 1585 | 75 |
| Total anthocyanins, mg cyanidin-3-glucoside equivalents | 66 | - |
| Ellagic acid, mg | 220 | - |
| Phytosterols, mg | 50 | - |
| Dietary fiber, g | 8 | 5 |
| N | 17 |
| Age (years) | 57 ± 7 |
| Gender M/F | 4/13 |
| Anti-hypertensive medications (%) | 65 |
| Lipid lowering medications (%) | 35 |
| Oral hypoglycemic agents (%) | 12 |
| Vitamin supplement users (%) | 65 |
| Kellgren–Lawrence grade | 2.1 ± 0.7 |
| Serum Variable | ICOAP (Constant Pain) % | ICOAP (Intermittent Pain) % | ICOAP (Total Pain) % | HAQ-DI |
|---|---|---|---|---|
| hs-CRP (mg/L) | 1.9 ± 1.3 | 1.7 ± 1.4 | 1.8 ± 1.1 | 0.03 ± 0.04 |
| p-value * | 0.18 | 0.24 | 0.25 | 0.28 |
| IL-6 (pg/mL) | 5.7 ± 2.8 | 1.8 ± 2.9 | 3.6 ± 2.4 | 0.003 ± 0.08 |
| p-value | 0.03 | 0.23 | 0.37 | 0.42 |
| IL-1β (pg/mL) | 0.4 ± 0.3 | 0.04 ± 0.3 | 0.2 ± 0.1 | 0.003 ± 0.007 |
| p-value | 0.21 | 0.32 | 0.42 | 0.46 |
| MMP-3 (ng/mL) | 1.6 ± 1.7 | 1.9 ± 1.8 | 1.8 ± 1.5 | 0.03 ± 0.05 |
| p-value | 0.34 | 0.23 | 0.21 | 0.53 |
| MMP-8 (ng/mL) | 2.7 ± 3.4 | 6.9 ± 3.5 | 5.0 ± 2.9 | 0.01 ± 0.09 |
| p-value | 0.32 | 0.006 | 0.42 | 0.21 |
| Variables | Baseline | Strawberry (12-Week) | Washout (2-Week) | Control (12-Week) | p-Value * |
|---|---|---|---|---|---|
| BMI (kg/m2) | 39.1 ± 1.5 | 39.3 ± 1.4 | 39.3 ± 1.5 | 39.3 ± 1.5 | 0.41 |
| Body weight (lb) | 246.4 ± 7.3 | 245.6 ± 7.4 | 245.1 ± 7.1 | 245.0 ± 7.2 | 0.32 |
| Waist circumference (inches) | 46.4 ± 1.1 | 46.5 ± 1.1 | 46.1 ± 1.0 | 46.8 ± 1.1 | 0.26 |
| Systolic blood pressure (mm Hg) | 125 ± 3.0 | 125 ± 2.0 | 126 ± 3.0 | 127 ± 2.0 | 0.37 |
| Diastolic blood pressure (mm Hg) | 80 ± 2.0 | 82 ± 1.0 | 81 ± 2.0 | 82 ± 1.0 | 0.41 |
| Fasting glucose (mg/dL) | 113.4 ± 5.6 | 118.9 ± 8.7 | 114.7 ± 4.5 | 112.3 ± 5.1 | 0.31 |
| HbA1c (%) | 5.9 ± 0.2 | 6.1 ± 0.1 | 5.99 ± 0.2 | 6.1 ± 0.2 | 0.88 |
| Total Cholesterol (mg/dL) | 189 ± 6.2 | 188 ± 7.6 | 182 ± 7.0 | 188 ± 8.7 | 0.86 |
| LDL Cholesterol (mg/dL) | 109 ± 6.3 | 108 ± 6.9 | 105 ± 6.8 | 105 ± 7.6 | 0.65 |
| HDL Cholesterol (mg/dL) | 51 ± 3.0 | 52 ± 2.9 | 50 ± 2.5 | 54 ± 3.3 | 0.12 |
| Triglycerides (mg/dL) | 129 ± 14.3 | 136 ± 16.1 | 128 ± 15.0 | 130 ± 12.9 | 0.54 |
| ALT (U/L) | 40.5 ± 2.8 | 38.6 ± 2.3 | 39.5 ± 2.1 | 40.6 ± 2.9 | 0.42 |
| AST (U/L) | 30.1 ± 2.6 | 28.9 ± 2.3 | 28.6 ± 1.7 | 31.4 ± 2.1 | 0.52 |
| Creatinine (mg/dL) | 0.75 ± 0.03 | 0.78 ± 0.03 | 0.75 ± 0.03 | 0.77 ± 0.02 | 0.42 |
| BUN (mg/dL) | 15.5 ± 0.9 | 14.5 ± 0.7 | 15.3 ± 1.0 | 14.5 ± 1.0 | 0.36 |
| hs-CRP (mg/L) | 5.7 ± 1.2 | 4.6 ± 0.9 | 5.4 ± 1.1 | 4.8 ± 0.8 | 0.74 |
| IL-6 (pg/mL) | 8.8 ± 0.4 | 3.4 ± 0.5 | 8.1 ± 0.9 | 8.7 ± 1.4 | 0.006 |
| IL-1β (pg/mL) | 18.6 ± 4.0 | 7.5 ± 0.7 | 16.3 ± 3.1 | 16.2 ± 1.2 | <0.0001 |
| MMP-3 (ng/mL) | 6.9 ± 0.6 | 5.3 ± 0.5 | 7.1 ± 0.6 | 6.8 ± 0.5 | 0.004 |
| MMP-8 (ng/mL) | 1.8 ± 0.3 | 2.2 ± 0.3 | 2.4 ± 0.2 | 2.1 ± 0.2 | 0.26 |
| Nitrite (μM) | 6.4 ± 0.7 | 9.9 ± 2.2 | 6.4 ± 0.8 | 7.5 ± 0.8 | 0.23 |
| Variables | Baseline | Strawberry (12-Week) | Washout (2-Week) | Control (12-Week) | p-Value * |
|---|---|---|---|---|---|
| HAQ-DI | 0.6 ± 0.1 | 0.4 ± 0.1 | 0.5 ± 0.1 | 0.6 ± 0.1 | 0.026 |
| VAS PAIN | 1.4 ± 0.2 | 0.8 ± 0.1 | 1.1 ± 0.1 | 1.0 ± 0.2 | 0.17 |
| VAS HEALTH | 0.7 ± 0.1 | 1.0 ± 0.2 | 0.9 ± 0.2 | 0.7 ± 0.1 | 0.13 |
| ICOAP (Constant pain) % | 31.8 ± 3.5 | 13.8 ± 3.6 | 32.1 ± 3.7 | 24.2 ± 4.1 | 0.01 |
| ICOAP (Intermittent pain) % | 38.5 ± 3.4 | 24.3 ± 4.7 | 34.1 ± 2.2 | 34.6 ± 3.0 | 0.02 |
| ICOAP (Total pain) % | 35.4 ± 3.1 | 19.4 ± 3.7 | 33.2 ± 2.2 | 29.9 ± 3.0 | 0.007 |
| Nutrients | Baseline | Strawberry (12-Week) | Washout (2-Week) | Control (12-Week) | p-Value * |
|---|---|---|---|---|---|
| Calories (kcal) | 2026 ± 183 | 2604 ± 441 | 2004 ± 184 | 1901 ± 203 | 0.12 |
| Carbohydrates (g) | 215 ± 19 | 320 ± 56 | 216 ± 20 | 228 ± 29 | 0.21 |
| Fats (g) | 90 ± 12 | 100 ± 22 | 89 ± 12 | 78 ± 9 | 0.31 |
| Proteins (g) | 92 ± 11 | 107 ± 19 | 96 ± 10 | 76 ± 7 | 0.43 |
| Saturated fats (g) | 30 ± 4 | 32 ± 6 | 28 ± 3 | 26 ± 3 | 0.31 |
| MUFA (g) | 17 ± 4 | 22 ± 6 | 17 ± 4 | 13 ± 3 | 0.18 |
| PUFA (g) | 8 ± 2 | 12 ± 3 | 7 ± 1.5 | 6 ± 2 | 0.11 |
| Fiber (g) | 18 ± 2 | 23 ± 3 | 19 ± 2 | 20 ± 3 | 0.43 |
| Vitamin C (mg) | 45 ± 9 | 81 ± 17 | 42 ± 9 | 75 ± 28 | 0.77 |
| Vitamin E (mg) | 5 ± 2 | 7 ± 2 | 4 ± 1 | 5 ± 2 | 0.34 |
| Beta-carotene (μg) | 590 ± 303 | 890 ± 203 | 580 ± 311 | 828 ± 400 | 0.63 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schell, J.; Scofield, R.H.; Barrett, J.R.; Kurien, B.T.; Betts, N.; Lyons, T.J.; Zhao, Y.D.; Basu, A. Strawberries Improve Pain and Inflammation in Obese Adults with Radiographic Evidence of Knee Osteoarthritis. Nutrients 2017, 9, 949. https://doi.org/10.3390/nu9090949
Schell J, Scofield RH, Barrett JR, Kurien BT, Betts N, Lyons TJ, Zhao YD, Basu A. Strawberries Improve Pain and Inflammation in Obese Adults with Radiographic Evidence of Knee Osteoarthritis. Nutrients. 2017; 9(9):949. https://doi.org/10.3390/nu9090949
Chicago/Turabian StyleSchell, Jace, R. Hal Scofield, James R. Barrett, Biji T. Kurien, Nancy Betts, Timothy J. Lyons, Yan Daniel Zhao, and Arpita Basu. 2017. "Strawberries Improve Pain and Inflammation in Obese Adults with Radiographic Evidence of Knee Osteoarthritis" Nutrients 9, no. 9: 949. https://doi.org/10.3390/nu9090949
APA StyleSchell, J., Scofield, R. H., Barrett, J. R., Kurien, B. T., Betts, N., Lyons, T. J., Zhao, Y. D., & Basu, A. (2017). Strawberries Improve Pain and Inflammation in Obese Adults with Radiographic Evidence of Knee Osteoarthritis. Nutrients, 9(9), 949. https://doi.org/10.3390/nu9090949





