Use of 3D Printing in Model Manufacturing for Minor Surgery Training of General Practitioners in Primary Care
Abstract
:Featured Application
Abstract
1. Introduction
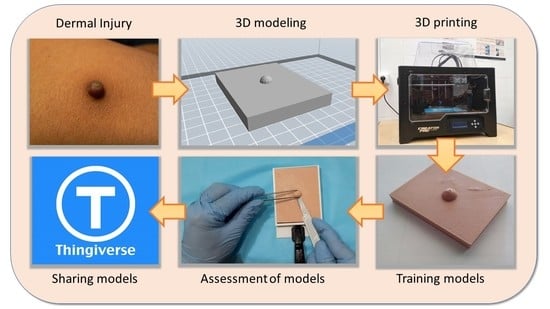
2. Materials and Methods
2.1. Initial Stage
2.2. 3D Modeling
2.3. Slicing
2.4. 3D Printing
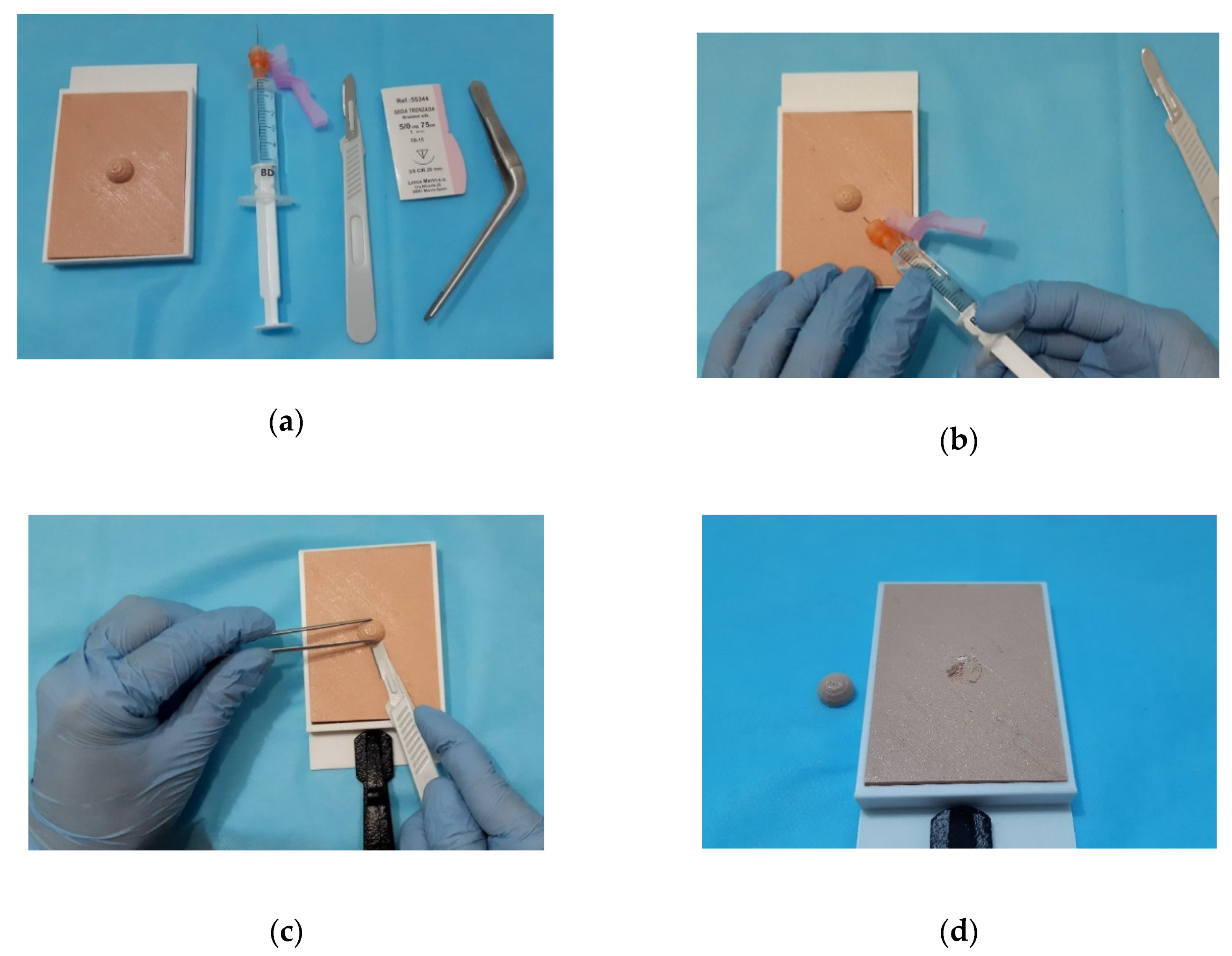
2.5. Assessment
2.6. Sharing the Models
3. Results
3.1. Aesthetic Recreation Level
3.2. Realism During Anesthesia Infiltration
3.3. Realism During Removal of the Lesion
3.4. Realism During Surgical Wound Closure
3.5. Cost of Models
4. Discussion
- Primary care centers can now access 3D printing. In hospitals, 3D-printed models have been used for several years to train surgeons [11,19]. Waran et al. [17] have found that the use of training models manufactured using 3D printing increases the success rate in major surgery operations and reduces the time spent on each intervention. Driven by this reality, the authors propose the use of this methodology in primary care centers, to carry out practical courses that serve to initiate GPs in minor surgery.
- The cost of the proposed models is low. FDM 3D printing allows healthcare resources to be manufactured at a low cost [32]. The training models proposed in this work have a cost of 6 Euros, compared to 38 Euros for commercial training models. This detail is important in a public health system such as the Spanish one, or in developing countries [33]. In addition, the proposed process allows a user to customize the models, and to manufacture those that have interest in each geographic point [34].
- The proposed models have a high level of aesthetic recreation. In major surgery, when lesions have some complexity, images taken by computed tomography (CT) and magnetic resonance imaging (MRI) are used to model the lesion in 3D [35]. In this case, the models have been performed in parametric design software from photographs and drawings made by one of the authors, an expert in minor surgery. However, the panel of experts have positively assessed the level of aesthetic recreation in the models.
- The models have been shared on Thingiverse. In the ‘maker’ world it is common to share designed models. This is one of the main attractions of 3D printing. Thingiverse is a widely used platform for sharing general models, although there are specific platforms for biomedical models, such as one developed by the National Institutes of Health of United States (NIH 3D) [36].
- FDM 3D printing technology is suitable for this purpose. There are 3D printing technologies that can print models of great complexity [37], although their cost cannot be borne by a primary care center. In the present work, the use of FDM technology has been proposed, which is the cheapest technology, and which provides a surface finish suitable for the intended use.
- The filament used is not elastic enough and it is not possible to close the surgical wound. It is necessary to look in the market for more elastic filaments that are available in skin color to overcome this handicap.
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lipson, H.; Kurman, M. Fabricated: The New World of 3D Printing; John Wiley & Sons Inc.: Indianapolis, IN, USA, 2013. [Google Scholar]
- Wong, K.V.; Hernandez, A. A Review of Additive Manufacturing. ISRN Mech. Eng. 2012, 2012, 1–10. [Google Scholar] [CrossRef]
- Sun, Z.; Lau, I.; Wong, Y.H.; Yeong, C.H. Personalized Three-Dimensional Printed Models in Congenital Heart Disease. J. Clin. Med. 2019, 8, 522. [Google Scholar] [CrossRef] [PubMed]
- Ahn, S.; Montero, M.; Odel, D.; Roundy, S.; Wright, P.K. Anisotropic material properties of fused deposition modeling ABS. Rapid Prototyp. J. 2002, 8, 248–257. [Google Scholar] [CrossRef]
- Ngo, T.D.; Kashani, A.; Imbalzano, G.; Nguyen, K.T.Q.; Hui, D. Additive manufacturing (3D printing): A review of materials, methods, applications and challenges. Compos. Part B Eng. 2018, 143, 172–196. [Google Scholar] [CrossRef]
- Ten Kate, J.; Smit, G.; Breedveld, P. 3D-printed upper limb prostheses: A review. Disabil. Rehabil. Assist. Technol. 2017, 12, 300–314. [Google Scholar] [CrossRef]
- Turner, B.N.; Strong, R.; Gold, S.A. A review of melt extrusion additive manufacturing processes: I. Process design and modeling. Rapid Prototyp. J. 2014, 20, 192–204. [Google Scholar] [CrossRef]
- Barrios, J.M.; Romero, P.E. Improvement of surface roughness and hydrophobicity in PETG parts manufactured via fused deposition modeling (FDM): An application in 3D printed self—Cleaning parts. Materials 2019, 12, 2499. [Google Scholar] [CrossRef]
- Smart Materials 3D. Available online: https://www.smartmaterials3d.com/en/ (accessed on 17 January 2019).
- Lee Ventola, C. Medical applications for 3D printing: Current and projected uses. Pharm. Ther. 2014, 39, 704–711. [Google Scholar]
- Tack, P.; Victor, J.; Gemmel, P.; Annemans, L. 3D-printing techniques in a medical setting: A systematic literature review. Biomed. Eng. Online 2016, 15, 115. [Google Scholar] [CrossRef]
- Mcmenamin, P.G.; Quayle, M.R.; Mchenry, C.R.; Adams, J.W. The production of anatomical teaching resources using three-dimensional (3D) printing technology. Anat. Sci. Educ. 2014, 7, 479–486. [Google Scholar] [CrossRef]
- Barber, S.R.; Kozin, E.D.; Dedmon, M.; Lin, B.M.; Lee, K.; Sinha, S.; Black, N.; Remenschneider, A.K.; Lee, D.J. 3D-printed pediatric endoscopic ear surgery simulator for surgical training. Int. J. Pediatr. Otorhinolaryngol. 2016, 90, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Ho, D.; Squelch, A.; Sun, Z. Modelling of aortic aneurysm and aortic dissection through 3D printing. J. Med. Radiat. Sci. 2017, 64, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Mañanes, R.; Calvo-Haro, J.; Arnal-Burró, J.; Chana-Rodríguez, F.; Sanz-Ruiz, P.; Vaquero-Martín, J. Our experience with domestic 3D printing in Orthopedic Surgery and Traumatology. Do it yourself. Rev. Latinoam. Cirugía Ortopédica 2016, 1, 47–53. [Google Scholar] [CrossRef]
- Allan, A.; Kealley, C.; Squelch, A.; Wong, Y.H.; Yeong, C.H.; Sun, Z. Patient-specific 3D printed model of biliary ducts with congenital cyst. Quant. Imaging Med. Surg. 2019, 9, 86–93. [Google Scholar] [CrossRef]
- Waran, V.; Narayanan, V.; Karuppiah, R.; Pancharatnam, D.; Chandran, H.; Raman, R.; Rahman, Z.A.A.; Owen, S.L.F.; Aziz, T.Z. Injecting realism in surgical training—Initial simulation experience with custom 3D models. J. Surg. Educ. 2014, 71, 193–197. [Google Scholar] [CrossRef]
- Michalski, M.H.; Ross, J.S. The shape of things to come: 3D printing in medicine. JAMA 2014, 312, 2213–2214. [Google Scholar] [CrossRef]
- Martelli, N.; Serrano, C.; Van Den Brink, H.; Pineau, J.; Prognon, P.; Borget, I.; El Batti, S. Advantages and disadvantages of 3-dimensional printing in surgery: A systematic review. Surgery 2016, 159, 1485–1500. [Google Scholar] [CrossRef]
- Tárraga López, P.J.; Marín Nieto, E.; García Olmo, D.; Celada Rodríguez, A.; Solera Albero, J. Economic impact of the introduction of a minor surgery program in primary care. Aten. Primaria 2001, 27, 335–338. [Google Scholar] [CrossRef]
- Gokani, V.J.; Ferguson, H.J.M.; Fitzgerald, J.E.F.; Beamish, A.J. Surgical training in primary care: Consensus recommendations by the Association of Surgeons in Training. Int. J. Surg. 2014, 12, S1–S4. [Google Scholar] [CrossRef]
- Serra, M.; Arevalo, A.; Ortega, C.; Ripoll, A.; Giménez, N. Minor surgery activity in primary care. J. R. Soc. Med. Short Rep. 2010, 1, 1–8. [Google Scholar] [CrossRef]
- Puche, J.M.; Muñoz, P.A. Program to introduce and develop minor surgery at a primary-care center in Spain. Arch. Med. Fam. 2009, 11, 39–49. [Google Scholar]
- Garrido, S.E.; García, R.V.; Nogales, P.A. Continuing education in primary care: The educational needs of its professionals. Aten. Primaria 2002, 30, 368–373. [Google Scholar]
- Brown, J. Minor Surgery, a Text and Atlas, 4th ed.; CRC Press: London, UK, 2001; ISBN 978-0340761137. [Google Scholar]
- Thompson, M.K.; Moroni, G.; Vaneker, T.; Fadel, G.; Campbell, R.I.; Gibson, I.; Bernard, A.; Schulz, J.; Graf, P.; Ahuja, B.; et al. Design for additive manufacturing: Trends, opportunities, considerations, and constraints. CIRP Ann. Manuf. Technol. 2016, 65, 737–760. [Google Scholar] [CrossRef]
- SolidWorks. Available online: https://www.solidworks.com/ (accessed on 1 November 2019).
- FlashForge. Available online: https://www.flashforge.com/ (accessed on 1 November 2019).
- FlashPrint. Available online: https://www.flashforge.com/download-center (accessed on 1 November 2019).
- Hyrkäs, K.; Appelqvist-Schmidlechner, K.; Oksa, L. Validating an instrument for clinical supervision using an expert panel. Int. J. Nurs. Stud. 2003, 40, 619–625. [Google Scholar] [CrossRef]
- Thingiverse. Available online: https://www.thingiverse.com/ (accessed on 1 November 2019).
- Rismani, S.; Van der Loos, H.F.M. The Competitive Advantage of Using 3D-Printing in Low-Resource Healthcare Settings. In Proceedings of the 20th International Conference on Engineering Design, Milan, Italy, 27–30 July 2015; pp. 1–10. [Google Scholar]
- Corsini, L.; Aranda-Jan, C.B.; Moultrie, J. Using digital fabrication tools to provide humanitarian and development aid in low-resource settings. Technol. Soc. 2019, 58, 101117. [Google Scholar] [CrossRef]
- Petrick, I.J.; Simpson, T.W. 3D printing disrupts manufacturing. Res. Technol. Manag. 2013, 56, 12–16. [Google Scholar] [CrossRef]
- Rengier, F.; Mehndiratta, A.; Von Tengg-Kobligk, H.; Zechmann, C.M.; Unterhinninghofen, R.; Kauczor, H.U.; Giesel, F.L. 3D printing based on imaging data: Review of medical applications. Int. J. Comput. Assist. Radiol. Surg. 2010, 5, 335–341. [Google Scholar] [CrossRef]
- Coakley, M.F.; Hurt, D.E.; Weber, N.; Mtingwa, M.; Fincher, E.C.; Alekseyev, V.; Chen, D.T.; Yun, A.; Gizaw, M.; Swan, J.; et al. The NIH 3D print exchange: A public resource for bioscientific and biomedical 3D prints. 3D Print. Addit. Manuf. 2014, 1, 137–140. [Google Scholar] [CrossRef]
- Jacobs, S.; Grunert, R.; Mohr, F.W.; Falk, V. 3D-Imaging of cardiac structures using 3D heart models for planning in heart surgery: A preliminary study. Interact. Cardiovasc. Thorac. Surg. 2008, 7, 6–9. [Google Scholar] [CrossRef] [Green Version]






| Initial Decisions | Have Influence on |
|---|---|
| Size | Print time |
| Print position | Possibility of printing Surface roughness |
| Entities that make up the model | Procedure to model the lesion in 3D |
| Combination of materials | Using the two 3D printer extruders |
| Print density | Flexibility of the model Print time |
| Pattern | Flexibility of the model |
| Print Parameter | Value |
|---|---|
| Extrusion Temperature | 225 °C |
| Bed Temperature | 50 °C |
| Layer Height | 0.18 mm |
| First-Level Layer Height | 0.27 mm |
| Retraction Length | 3.7 mm |
| Fill Density | 90% |
| Fill Pattern | Hexagon |
| Parameter | Value |
|---|---|
| Cost of plastic (€/kg) | 60 |
| Cost of electrical energy (€/kWh) | 0.15 |
| 3D Printer power (kW) | 0.500 |
| Cost of the 3D printer (€) | 599 |
| Amortization period (years) | 1 |
| Days active per year | 250 |
| Hours per day (h) | 8 |
| Failure rate (%) | 5 |
| Parameter | Dermal Nevus | Seborrheic Keratosis | Epidermal Cyst | Ingrown Nail |
|---|---|---|---|---|
| Workpiece mass (kg) | 0.06 | 0.05 | 0.06 | 0.01 |
| Printing time (h) | 5.9 | 5.80 | 6.00 | 2.01 |
| Cost of plastic material (€) | 3.61 | 3.10 | 3.61 | 0.98 |
| Cost of electricity (€) | 0.44 | 0.44 | 0.45 | 0.15 |
| Equipment amortization cost (€) | 1.77 | 1.74 | 1.80 | 0.60 |
| Cost of failures (€) | 0.29 | 0.26 | 0.29 | 0.09 |
| Total (€) | 6.11 | 5.53 | 6.15 | 1.81 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luque, M.C.; Calleja-Hortelano, A.; Romero, P.E. Use of 3D Printing in Model Manufacturing for Minor Surgery Training of General Practitioners in Primary Care. Appl. Sci. 2019, 9, 5212. https://doi.org/10.3390/app9235212
Luque MC, Calleja-Hortelano A, Romero PE. Use of 3D Printing in Model Manufacturing for Minor Surgery Training of General Practitioners in Primary Care. Applied Sciences. 2019; 9(23):5212. https://doi.org/10.3390/app9235212
Chicago/Turabian StyleLuque, M.C., A. Calleja-Hortelano, and P.E. Romero. 2019. "Use of 3D Printing in Model Manufacturing for Minor Surgery Training of General Practitioners in Primary Care" Applied Sciences 9, no. 23: 5212. https://doi.org/10.3390/app9235212