Emotional Response Inhibition: A Shared Neurocognitive Deficit in Eating Disorder Symptoms and Nonsuicidal Self-Injury
Abstract
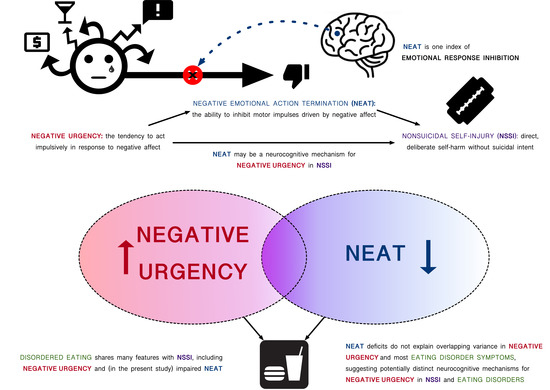
1. Introduction
2. Materials and Methods
3. Results
3.1. Demographics and ED Symptoms
3.2. Correlations among Negative Urgency, NEAT, NSSI history, and ED Symptoms
3.3. Hierarchical Linear Regression Analyses Predicting EDE-Q Scales from Negative Urgency and NEAT
3.4. Zero-Inflated Regression Analyses Predicting ED Behaviors from Negative Urgency and NEAT
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Fox, K.R.; Wang, S.B.; Boccagno, C.E.; Haynos, A.F.; Kleiman, E.; Hooley, J.M. Comparing self-harming intentions underlying eating disordered behaviors and NSSI: Evidence that distinctions are less clear than assumed. Int. J. Eat. Dis. 2019, 52, 564–575. [Google Scholar] [CrossRef] [PubMed]
- Cucchi, A.; Ryan, D.; Konstantakopoulos, G.; Stroumpa, S.; Kaçar, A.Ş.; Renshaw, S.; Ladau, S.; Kravariti, E. Lifetime prevalence of non-suicidal self-injury in patients with eating disorders: A systematic review and meta-analysis. Psychol. Med. 2016, 46, 1345–1358. [Google Scholar] [CrossRef] [PubMed]
- Svirko, E.; Hawton, K. Self-Injurious Behavior and Eating Disorders: The Extent and Nature of the Association. Suicide Life-Threat. Behav. 2007, 37, 409–421. [Google Scholar] [CrossRef] [PubMed]
- Claes, L.; Muehlenkamp, J.J. Eating disorders and NSSI. In Non-Suicidal Self-Injury in Eating Disorders; Claes, L., Muehlenkamp, J., Eds.; Springer: Berlin, Germany, 2016; pp. 21–22. [Google Scholar]
- St Germain, S.A.; Hooley, J.M. Direct and indirect forms of non-suicidal self-injury: Evidence for a distinction. Psychiatry Res. 2011, 197, 78–84. [Google Scholar] [CrossRef] [PubMed]
- Fischer, S.; Settles, R.; Collins, B.; Gunn, R.; Smith, G.T. The role of negative urgency and expectancies in problem drinking and disordered eating: Testing a model of comorbidity in pathological and at-risk samples. Psychol. Addict. Behav. 2012, 26, 112. [Google Scholar] [CrossRef]
- Fischer, S.; Peterson, C.M.; McCarthy, D. A prospective test of the influence of negative urgency and expectancies on binge eating and purging. Psychol. Addict. Behav. 2013, 27, 294. [Google Scholar] [CrossRef]
- Racine, S.E.; Keel, P.K.; Burt, S.A.; Sisk, C.L.; Neale, M.; Boker, S.; Klump, K.L. Exploring the relationship between negative urgency and dysregulated eating: Etiologic associations and the role of negative affect. J. Abnorm. Psychol. 2013, 122, 433–444. [Google Scholar] [CrossRef]
- Racine, S.E.; Burt, S.A.; Keel, P.K.; Sisk, C.L.; Neale, M.C.; Boker, S.; Klump, K.L. Examining associations between negative urgency and key components of objective binge episodes. Int. J. Eat. Dis. 2015, 48, 527–531. [Google Scholar] [CrossRef]
- Gordon, K.H.; Kwan, M.Y.; Minnich, A.M.; Carter, D.L. Etiological Models of Non-suicidal Self-Injury and Eating Disorders. In Non-Suicidal Self-Injury in Eating Disorders; Claes, L., Muehlenkamp, J., Eds.; Springer: Berlin, Germany, 2014; pp. 55–71. [Google Scholar] [CrossRef]
- Hamza, C.A.; Willoughby, T.; Heffer, T. Impulsivity and nonsuicidal self-injury: A review and meta-analysis. Clin. Psychol. Rev. 2015, 38, 13–24. [Google Scholar] [CrossRef]
- Allen, K.J.D.; Bozzay, M.L.; Edenbaum, E.R. Neurocognition and suicide risk in adults. Curr. Behav. Neurosci. Rep. 2019, 1–15. [Google Scholar] [CrossRef]
- Carlson, L.; Steward, T.; Agüera, Z.; Mestre-Bach, G.; Magaña, P.; Granero, R.; Jiménez-Murcia, S.; Claes, L.; Gearhardt, A.; Menchón, J.; et al. Associations of food addiction and nonsuicidal self-injury among women with an eating disorder: A common strategy for regulating emotions? Eur. Eat. Disord. Rev. 2018, 26, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Claes, L.; Islam, M.A.; Fagundo, A.B.; Jimenez-Murcia, S.; Granero, R.; Agüera, Z.; Rossi, E.; Menchón, J.M.; Fernández-Aranda, F. The relationship between non-suicidal self-injury and the UPPS-P impulsivity facets in eating disorders and healthy controls. PLoS ONE 2015, 10, e0126083. [Google Scholar] [CrossRef] [PubMed]
- Muehlenkamp, J.J.; Peat, C.M.; Claes, L.; Smits, D. Self-Injury and Disordered Eating: Expressing Emotion Dysregulation through the Body. Suicide Life-Threat. Behav. 2012, 42, 416–425. [Google Scholar] [CrossRef] [PubMed]
- Wolz, I.; Granero, R.; Fernández-Aranda, F. A comprehensive model of food addiction in patients with binge-eating symptomatology: The essential role of negative urgency. Compr. Psychiatry 2017, 74, 118–124. [Google Scholar] [CrossRef]
- Aldao, A.; Gee, D.G.; De Los Reyes, A.; Seager, I. Emotion regulation as a transdiagnostic factor in the development of internalizing and externalizing psychopathology: Current and future directions. Dev. Psychopathol. 2016, 28, 927–946. [Google Scholar] [CrossRef]
- Carver, C.S.; Johnson, S.L.; Timpano, K.R. Toward a functional view of the p factor in psychopathology. Clin. Psychol. Sci. 2017, 5, 880–889. [Google Scholar] [CrossRef]
- Dingemans, A.; Danner, U.; Parks, M. Emotion regulation in binge eating disorder: A review. Nutrients 2017, 9, 1274. [Google Scholar] [CrossRef]
- Doukas, A.M.; D’Andrea, W.M.; Gregory, W.E.; Joachim, B.; Lee, K.A.; Robinson, G.; Freed, S.J.; Khedari-DePierro, V.; Pfeffer, K.A.; Todman, M.; et al. Hurts so good: Pain as an emotion regulation strategy. Emotion 2019. [Google Scholar] [CrossRef]
- Klonsky, E.D. The functions of deliberate self-injury: A review of the evidence. Clin. Psychol. Rev. 2007, 27, 226–239. [Google Scholar] [CrossRef]
- Klonsky, E.D. The functions of self-injury in young adults who cut themselves: Clarifying the evidence for affect regulation. Psychiatry Res. 2009, 166, 260–268. [Google Scholar] [CrossRef]
- Hamza, C.A.; Willoughby, T. Nonsuicidal self-injury and affect regulation: Recent findings from experimental and ecological momentary assessment studies and future directions. J. Clin. Psychol. 2015, 71, 561–574. [Google Scholar] [CrossRef]
- Lavender, J.M.; Wonderlich, S.A.; Engel, S.G.; Gordon, K.H.; Kaye, W.H.; Mitchell, J.E. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clin. Psychol. Rev. 2015, 40, 111–122. [Google Scholar] [CrossRef]
- Nock, M.K.; Prinstein, M.J. A functional approach to the assessment of self-mutilative behavior. J. Consult. Clin. Psychol. 2004, 72, 885–890. [Google Scholar] [CrossRef]
- Berg, K.C.; Crosby, R.D.; Cao, L.; Peterson, C.B.; Engel, S.G.; Mitchell, J.E.; Wonderlich, S.A. Facets of negative affect prior to and following binge-only, purge-only, and binge/purge events in women with bulimia nervosa. J. Abnorm. Psychol. 2013, 122, 111–118. [Google Scholar] [CrossRef]
- Goldschmidt, A.B.; Wonderlich, S.A.; Crosby, R.D.; Engel, S.G.; Lavender, J.M.; Peterson, C.B.; Crow, S.J.; Cao, L.; Mitchell, J.E. Ecological momentary assessment of stressful events and negative affect in bulimia nervosa. J. Consult. Clin. Psychol. 2014, 82, 30. [Google Scholar] [CrossRef]
- Haedt-Matt, A.A.; Keel, P.K. Affect regulation and purging: An ecological momentary assessment study in purging disorder. J. Abnorm. Psychol. 2015, 124, 399. [Google Scholar] [CrossRef]
- Haynos, A.F.; Berg, K.C.; Cao, L.; Crosby, R.D.; Lavender, J.M.; Utzinger, L.M.; Peterson, C.B. Trajectories of higher- and lower-order dimensions of negative and positive affect relative to restrictive eating in anorexia nervosa. J. Abnorm. Psychol. 2017, 126, 495–505. [Google Scholar] [CrossRef]
- Nock, M.K.; Prinstein, M.J. Contextual features and behavioral functions of self-mutilation among adolescents. J. Abnorm. Psychol. 2005, 114, 140–146. [Google Scholar] [CrossRef]
- Rodriguez-Blanco, L.; Carballo, J.J.; Baca-Garcia, E. Use of ecological momentary assessment (EMA) in non-suicidal self-injury (NSSI): A systematic review. Psychiatry Res. 2018, 263, 212–219. [Google Scholar] [CrossRef]
- Schatten, H.T.; Allen, K.J.D.; Armey, M.F. Assessment of emotion dysregulation using ecological momentary assessment. In The Oxford Handbook of Emotion Dysregulation; Beauchaine, T., Crowell, S., Eds.; Oxford University Press: Cambridge, UK, 2019; pp. 1–31. [Google Scholar] [CrossRef]
- Riley, E.N.; Combs, J.L.; Jordan, C.E.; Smith, G.T. Negative urgency and lack of perseverance: Identification of differential pathways of onset and maintenance risk in the longitudinal prediction of nonsuicidal self-injury. Behav. Ther. 2015, 46, 439–448. [Google Scholar] [CrossRef]
- Berg, J.M.; Latzman, R.D.; Bliwise, N.G.; Lilienfeld, S.O. Parsing the Heterogeneity of Impulsivity: A Meta-Analytic Review of the Behavioral Implications of the UPPS for Psychopathology. Psychol. Assess. 2015, 27, 1129–1146. [Google Scholar] [CrossRef]
- Cyders, M.A.; Coskunpinar, A.; VanderVeen, J.D. Urgency: A common transdiagnostic endophenotype for maladaptive risk taking. In The Dark Side of Personality: Science and Practice in Social, Personality, and Clinical Psychology; Zeigler-Hill, V., Marcus, D., Eds.; American Psychological Association: Washington, DC, USA, 2016; pp. 157–188. [Google Scholar] [CrossRef]
- Dir, A.L.; Karyadi, K.; Cyders, M.A. The uniqueness of negative urgency as a common risk factor for self-harm behaviors, alcohol consumption, and eating problems. Addict. Behav. 2013, 38, 2158–2162. [Google Scholar] [CrossRef]
- Atiye, M.; Miettunen, J.; Raevuori-Helkamaa, A. A meta-analysis of temperament in eating disorders. Eur. Eat. Disord. Rev. 2015, 23, 89–99. [Google Scholar] [CrossRef] [PubMed]
- Claes, L.; Vandereycken, W.; Vertommen, H. Impulsive and compulsive traits in eating disordered patients compared with controls. Pers. Individ. Differ. 2002, 32, 707–714. [Google Scholar] [CrossRef]
- Farstad, S.M.; McGeown, L.M.; Von Ranson, K.M. Eating disorders and personality, 2004–2016: A systematic review and meta-analysis. Clin. Psychol. Rev. 2016, 46, 91–105. [Google Scholar] [CrossRef]
- Lavender, J.M.; Green, D.; Anestis, M.D.; Tull, M.T.; Gratz, K.L. Negative affect, negative urgency, thought suppression, and bulimic symptoms: A moderated mediation analysis in a sample at-risk for bulimic symptoms. Eur. Eat. Disord. Rev. 2015, 23, 246–250. [Google Scholar] [CrossRef]
- Cyders, M.A.; Smith, G.T. Emotion-based dispositions to rash action: Positive and negative urgency. Psychol. Bull. 2008, 134, 807. [Google Scholar] [CrossRef]
- Maxfield, B.L.; Pepper, C.M. Impulsivity and response latency in non-suicidal self-injury: The role of negative urgency in emotion regulation. Psychiatr. Q. 2018, 89, 417–426. [Google Scholar] [CrossRef]
- Peterson, C.M.; Fischer, S. A prospective study of the influence of the UPPS model of impulsivity on the co-occurrence of bulimic symptoms and non-suicidal self-injury. Eat. Behav. 2012, 13, 335–341. [Google Scholar] [CrossRef]
- Pisetsky, E.M.; Haynos, A.F.; Lavender, J.M.; Crow, S.J.; Peterson, C.B. Associations between emotion regulation difficulties, eating disorder symptoms, non-suicidal self-injury, and suicide attempts in a heterogeneous eating disorder sample. Compr. Psychiatry 2017, 73, 143–150. [Google Scholar] [CrossRef]
- Heatherton, T.F.; Baumeister, R.F. Binge eating as escape from self-awareness. Psychol. Bull. 1991, 110, 86. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.J.D.; Fox, K.R.; Schatten, H.T.; Hooley, J.M. Frequency of nonsuicidal self-injury is associated with impulsive decision-making during criticism. Psychiatry Res. 2019, 271, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Sebastian, A.; Pohl, M.F.; Klöppel, S.; Feige, B.; Lange, T.; Stahl, C.; Voss, A.; Klauer, K.C.; Lieb, K.; Tüscher, O. Disentangling common and specific neural subprocesses of response inhibition. Neuroimage 2013, 64, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Carver, C.S.; Johnson, S.L. Impulsive reactivity to emotion and vulnerability to psychopathology. Am. Psychol. 2018, 73, 1067–1078. [Google Scholar] [CrossRef]
- Cyders, M.A.; Coskunpinar, A. Measurement of constructs using self-report and behavioral lab tasks: Is there overlap in nomothetic span and construct representation for impulsivity? Clin. Psychol. Rev. 2011, 31, 965–982. [Google Scholar] [CrossRef]
- Cyders, M.A.; Coskunpinar, A. The relationship between self-report and lab task conceptualizations of impulsivity. J. Psychol. Res. 2012, 46, 121–124. [Google Scholar] [CrossRef]
- Sharma, L.; Markon, K.E.; Clark, L.A. Toward a theory of distinct types of “impulsive” behaviors: A meta-analysis of self-report and behavioral measures. Psychol. Bull. 2014, 140, 374. [Google Scholar] [CrossRef]
- Allen, K.J.D.; Hooley, J.M. Inhibitory control in people who self-injure: Evidence for impairment and enhancement. Psychiatry Res. 2015, 225, 631–637. [Google Scholar] [CrossRef]
- Allen, K.J.D.; Hooley, J.M. Negative Emotional Action Termination (NEAT): Support for a cognitive mechanism underlying negative urgency in nonsuicidal self-injury. Behav. Ther. 2019, 50, 924–937. [Google Scholar] [CrossRef]
- Billieux, J.; Gay, P.; Rochat, L.; Van Der Linden, M. The role of urgency and its underlying psychological mechanisms in problematic behaviours. Behav. Res. Ther. 2010, 48, 1085–1096. [Google Scholar] [CrossRef]
- Chester, D.S.; Lynam, D.R.; Milich, R.; Powell, D.K.; Andersen, A.H.; DeWall, C.N. How do negative emotions impair self-control? A neural model of negative urgency. NeuroImage 2016, 132, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Gay, P.; Rochat, L.; Billieux, J.; D’Acremont, M.; Van Der Linden, M. Heterogeneous inhibition processes involved in different facets of self-reported impulsivity: Evidence from a community sample. Acta Psychol. 2008, 129, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Allen, K.J.; Hooley, J.M. Negative mood and interference control in nonsuicidal self-injury. Compr. Psychiatry 2017, 73, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Best, S.G.; Allen, K.J.D.; Hooley, J.M. Directed forgetting and nonsuicidal self-injury. Psychiatry Res. 2019. (Under Review). [Google Scholar] [CrossRef]
- Burke, T.A.; Allen, K.J.D.; Carpenter, R.W.; Siegel, D.; Kautz, M.M.; Alloy, L.B. Emotional response inhibition to self-harm stimuli interacts with momentary negative affect and urgency to predict nonsuicidal self-injury urges. Clin. Psychol. Sci. (Under Review).
- Nock, M.K.; Holmberg, E.B.; Photos, V.I.; Michel, B.D. Self-Injurious Thoughts and Behaviors Interview: Development, reliability, and validity in an adolescent sample. Psychol. Assess. 2007, 19, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Beglin, S.J. Assessment of eating disorders: Interview or self-report questionnaire? Int. J. Eat. Disord. 1994, 16, 363–370. [Google Scholar] [CrossRef]
- Mond, J.; Hay, P.; Rodgers, B.; Owen, C.; Beumont, P. Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Behav. Res. Ther. 2004, 42, 551–567. [Google Scholar] [CrossRef]
- Lynam, D.R.; Smith, G.T.; Whiteside, S.P.; Cyders, M.A. The UPPS-P: Assessing Five Personality Pathways to Impulsive Behavior; Unpublished Report; Purdue University: West Lafayette, IN, USA, 2006. [Google Scholar]
- Cyders, M.A.; Smith, G.T.; Spillane, N.S.; Fischer, S.; Annus, A.M.; Peterson, C. Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychol. Assess. 2007, 19, 107–118. [Google Scholar] [CrossRef]
- Smith, G.T.; Fischer, S.; Cyders, M.A.; Annus, A.M.; Spillane, N.S.; McCarthy, D.M. On the validity and utility of discriminating among impulsivity-like traits. Assessment 2007, 14, 155–170. [Google Scholar] [CrossRef]
- Weafer, J.; Baggott, M.J.; De Wit, H. Test–retest reliability of behavioral measures of impulsive choice, impulsive action, and inattention. Exp. Clin. Psychopharmacol. 2013, 21, 475. [Google Scholar] [CrossRef] [PubMed]
- Lang, P.J.; Bradley, M.M.; Cuthbert, B.N. International Affective Picture System (IAPS): Affective Ratings of Pictures and Instruction Manual; Technical Report A-8; University of Florida: Gainesville, FL, USA, 2008. [Google Scholar]
- Verbruggen, F.; Logan, G.D. Response inhibition in the stop-signal paradigm. Trends Cogn. Sci. 2008, 12, 418–424. [Google Scholar] [CrossRef] [PubMed]
- Schaumberg, K.; Reilly, E.E.; Anderson, L.M.; Gorrell, S.; Wang, S.B.; Sala, M. Improving prediction of eating-related behavioral outcomes with zero-sensitive regression models. Appetite 2018, 129, 252–261. [Google Scholar] [CrossRef] [PubMed]
- Muehlenkamp, J.J. Body Regard in Nonsuicidal Self-Injury: Theoretical Explanations and Treatment Directions. J. Cogn. Psychother. 2012, 26, 331–347. [Google Scholar] [CrossRef]
- Muehlenkamp, J.J.; Bagge, C.L.; Tull, M.T.; Gratz, K.L. Body Regard as a Moderator of the Relation between Emotion Dysregulation and Nonsuicidal Self-Injury. Suicide Life-Threat. Behav. 2013, 43, 479–493. [Google Scholar] [CrossRef]
- Pérez, S.; Marco, J.H.; Cañabate, M. Non-suicidal self-injury in patients with eating disorders: Prevalence, forms, functions, and body image correlates. Compr. Psychiatry 2018, 84, 32–38. [Google Scholar] [CrossRef]
- Bartholdy, S.; Dalton, B.; O’Daly, O.G.; Campbell, I.C.; Schmidt, U. A systematic review of the relationship between eating, weight and inhibitory control using the stop signal task. Neurosci. Biobehav. Rev. 2016, 64, 35–62. [Google Scholar] [CrossRef]
- Auerbach, R.P.; Kim, J.C.; Chango, J.M.; Spiro, W.J.; Cha, C.; Gold, J.; Esterman, M.; Nock, M.K. Adolescent nonsuicidal self-injury: Examining the role of child abuse, comorbidity, and disinhibition. Psychiatry Res. 2014, 220, 579–584. [Google Scholar] [CrossRef]
- Fikke, L.T.; Melinder, A.; Landrø, N.I. Executive functions are impaired in adolescents engaging in nonsuicidal self-injury. Psychol. Med. 2011, 41, 601–610. [Google Scholar] [CrossRef]
- Glenn, C.R.; Klonsky, E.D. A multimethod analysis of impulsivity in nonsuicidal self-injury. Personal. Disord. 2011, 1, 67–75. [Google Scholar] [CrossRef]
- Janis, I.B.; Nock, M.K. Are self-injurers impulsive?: Results from two behavioral laboratory studies. Psychiatry Res. Neuroimaging 2009, 169, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Lengel, G.J.; DeShong, H.L.; Mullins-Sweatt, S.N. Impulsivity and nonsuicidal self-injury: Examining the role of affect manipulation. J. Psychopathol. Behav. Assess. 2016, 38, 101–112. [Google Scholar] [CrossRef]
- Mc Closkey, M.S.; Look, A.E.; Chen, E.Y.; Pajoumand, G.; Berman, M.E. Nonsuicidal Self-Injury: Relationship to Behavioral and Self-Rating Measures of Impulsivity and Self-Aggression. Suicide Life-Threat. Behav. 2012, 42, 197–209. [Google Scholar] [CrossRef] [PubMed]
- Dick, D.M.; Smith, G.; Olausson, P.; Mitchell, S.H.; Leeman, R.F.; O’Malley, S.S.; Sher, K. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addict. Boil. 2010, 15, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Steinglass, J.E.; Berner, L.A.; Attia, E. Cognitive neuroscience of eating disorders. Psychiatr. Clin. N. Am. 2019, 42, 75–91. [Google Scholar] [CrossRef] [PubMed]

| M (SD) | ||
|---|---|---|
| Age | 24.41 (8.04) | |
| Years of Education | 14.42 (1.90) | |
| n (%) | ||
| Sex | Female | 82 (78.1) |
| Male | 23 (21.9) | |
| Gender/Orientation | Heterosexual | 85 (81.0) |
| LGBTQ+ | 20 (19.0) | |
| Race/Ethnicity | White | 54 (51.4) |
| Black | 11 (10.5) | |
| Asian | 27 (25.7) | |
| Hispanic/Latinx | 4 (3.8) | |
| Mixed/Other | 9 (8.6) | |
| Relationship Status | Single | 49 (46.7) |
| Dating | 39 (37.1) | |
| Married | 10 (9.52) | |
| Divorced | 3 (2.9) | |
| Cohabitating | 3 (2.9) | |
| Other | 1 (0.95) | |
| M (SD) | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Negative Urgency | 25.52 (8.35) | |||||||||||
| 2. NEAT | 40.45 (14.13) | 0.26 ** | ||||||||||
| 3. NSSI History (binary) | 187.42 (519.07) a | 0.38 *** | 0.27 ** | |||||||||
| 4. EDE-Q Global | 1.53 (1.42) | 0.35 *** | 0.28 ** | 0.22 * | ||||||||
| 5. EDE-Q Eating Concerns | 0.89 (1.38) | 0.45 *** | 0.32 *** | 0.24 * | 0.81 *** | |||||||
| 6. EDE-Q Shape Concerns | 2.00 (1.68) | 0.43 *** | 0.27 ** | 0.28 ** | 0.93 *** | 0.76 *** | ||||||
| 7. EDE-Q Weight Concerns | 1.73 (1.69) | 0.31 *** | 0.26 ** | 0.20 * | 0.92 *** | 0.68 *** | 0.88 *** | |||||
| 8. EDE-Q Restraint | 1.52 (1.58) | 0.22 * | 0.20 * | 0.02 | 0.84 *** | 0.66 *** | 0.66 *** | 0.69 *** | ||||
| 9. EDE-Q Overeating | 2.67 (5.18) | 0.36 *** | 0.16 | 0.11 | 0.41 *** | 0.44 *** | 0.35 *** | 0.26 ** | 0.33 *** | |||
| 10. EDE-Q LOC Eating | 1.87 (4.79) | 0.30 ** | 0.26 ** | 0.14 | 0.43 *** | 0.57 *** | 0.38 *** | 0.36 *** | 0.30 ** | 0.60 *** | ||
| 11. EDE-Q Binge Eating | 1.55 (4.28) | 0.35 *** | 0.36 *** | 0.11 | 0.49 *** | 0.58 *** | 0.45 *** | 0.43 *** | 0.40 *** | 0.65 *** | 0.82 *** | |
| 12. EDE-Q Comp. Behaviors | 2.78 (6.60) | 0.13 | 0.23 * | −0.02 | 0.49 *** | 0.38 *** | 0.44 *** | 0.41 *** | 0.51 *** | 0.17 | 0.23 * | 0.30 ** |
| EDE-Q Global | EDE-Q Eating Concerns | EDE-Q Shape Concerns | EDE-Q Weight Concerns | |||||
|---|---|---|---|---|---|---|---|---|
| Step 1. | B (SE) | β | B (SE) | β | B (SE) | β | B (SE) | β |
| Sex a | 0.46 (0.34) | 0.13 | 0.48 (0.33) | 0.14 | 0.74 (0.40) * | 0.18 | 0.68 (0.40) | 0.16 |
| Gender/Orientation a | 0.09 (0.38) | 0.02 | 0.27 (0.36) | 0.08 | 0.11 (0.44) | 0.03 | 0.09 (0.44) | 0.02 |
| Race a | −0.34 (0.28) | −0.12 | −0.31 (0.27) | −0.11 | −0.30 (0.33) | −0.09 | −0.58 (0.32) | −0.17 |
| NSSI History a | 0.68 (0.30) * | 0.24 | 0.63 (0.29) * | 0.23 | 0.95 (0.35) * | 0.28 | 0.90 (0.40) * | 0.26 |
| ESST Accuracy | 0.01 (0.01) | 0.06 | 0.00 (0.01) | 0.03 | 0.01 (0.01) | 0.05 | 0.02 (0.01) | 0.12 |
| Step 1: | ΔF(5,96) = 2.19, ΔR2 = 0.10 | 2.42 *, ΔR2 = 0.11 | 2.88 *, ΔR2 = 0.13 | 3.43 **, ΔR2 = 0.15 | ||||
| Step 2. | B (SE) | β | B (SE) | β | B (SE) | β | B (SE) | β |
| Negative Urgency | 0.07 (0.02) *** | 0.41 | 0.08 (0.02) * | 0.51 | 0.08 (0.02) *** | 0.40 | 0.07 (0.02) ** | 0.33 |
| Step 2: | ΔF(1,95) = 17.33 ***, ΔR2 = 0.14 | 29.74 ***, ΔR2 = 0.21 | 16.93 ***, ΔR2 = 0.13 | 10.98 ***, ΔR2 = 0.09 | ||||
| Step 3. | B (SE) | β | B (SE) | β | B (SE) | β | B (SE) | β |
| Negative Urgency | 0.06 (0.02) ** | 0.37 | 0.08 (0.02) *** | 0.46 | 0.08 (0.02) *** | 0.37 | 0.06 (0.02) ** | 0.30 |
| NEAT | 0.02 (0.01) ** | 0.23 | 0.03 (0.01) ** | 0.29 | 0.02 (0.01) * | 0.19 | 0.02 (0.01) | 0.17 |
| Step 3: | ΔF(1,94) = 5.72 *, ΔR2 = 0.04 | 11.09 ***, ΔR2 = 0.07 | 3.94*, ΔR2 = 0.03 | 3.18, ΔR2 = 0.03 | ||||
| Full Model: | F(7,101) = 5.34 ***, R2 = 0.29 | 8.77 ***, R2 = 0.40 | 5.53 ***, R2 = 0.29 | 4.82 ***, R2 = 0.26 | ||||
| EDE-Q Restraint | EDE-Q Overeating a | EDE-Q LOC Eating a | EDE-Q Binge Eating a | EDE-Q Comp. Behaviors a | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Step 1. | B (SE) | β | B (SE) | IRR | B (SE) | IRR | B (SE) | IRR | B (SE) | IRR |
| Sex | −0.05 (0.40) | −0.01 | 0.53 (0.56) | 1.69 | 1.44 (0.69) * | 4.24 | 1.44 (0.58) * | 4.22 | 2.64 (0.43) *** | 13.96 |
| Orient. | −0.12 (0.44) | −0.03 | 0.66 (0.59) | 1.93 | 1.43 (0.69) * | 4.17 | 0.99 (0.54) | 2.51 | 2.31 (0.41) *** | 10.09 |
| Race | −0.17 (0.33) | −0.05 | −0.50 (0.34) | 0.61 | 0.28 (0.49) | 1.33 | −0.77 (0.51) | 0.46 | 0.67 (0.32) * | 1.96 |
| NSSI Hx. | 0.27 (0.36) | 0.08 | 0.10 (0.50) | 1.10 | −0.51 (0.56) | 0.60 | −0.34 (0.50) | 0.71 | −1.14 (0.36) ** | 0.32 |
| ESST Acc. | 0.00 (0.01) | 0.02 | −0.06 (0.21) ** | 0.95 | 0.03 (0.02) | 1.03 | 0.05 (0.02) * | 1.06 | 0.02 (0.01) | 1.02 |
| Step 1: | ΔF(5,96) = 0.20 ΔR2 = 0.10 | χ2(10,89) = 16.47 LL: −195.49 | χ2(10,89) = 22.74 * LL: −139.26 | χ2(10,89) = 21.34 * LL: −131.74 | χ2(10,89) = 54.29 *** LL: −153.51 | |||||
| Step 2. | B (SE) | β | B (SE) | IRR | B (SE) | IRR | B (SE) | IRR | B (SE) | IRR |
| Negative Urgency | 0.05 (0.02) * | 0.27 | 0.05 (0.02) ** | 1.06 | 0.06 (0.03) * | 1.06 | 0.07 (0.02) ** | 1.07 | 0.00 (0.02) | 1.00 |
| Step 2: | ΔF(1,95) = 5.82 * ΔR2 = 0.06 | χ2(2,87) = 19.44 *** LL: −186.08 | χ2(2,87) = 12.06 ** LL: −131.65 | χ2(2,87) = 18.93 *** LL: −121.60 | χ2(2,87) = 1.54 LL: −152.70 | |||||
| Step 3. | B (SE) | β | B (SE) | IRR | B (SE) | IRR | B (SE) | IRR | B (SE) | IRR |
| Negative Urgency | 0.05 (0.02) | 0.23 | 0.05 (0.02) ** | 1.05 | 0.06 (0.02) ** | 1.07 | 0.07 (0.02) *** | 1.08 | 0.01 (0.02) | 1.00 |
| NEAT | 0.02 (0.01) * | 0.19 | 0.02 (0.01) * | 1.02 | 0.03 (0.01) * | 1.03 | 0.02 (0.02) | 1.02 | −0.03 (0.02) | 0.98 |
| Step 3: | ΔF(1,94) = 2.94 ΔR2 = 0.03 | χ2(2,85) = 5.28 LL: −183.52 | χ2(2,85) = 9.86 ** LL: −129.62 | χ2(2,85) = 2.46 LL: −106.11 | χ2(2,85) = 7.98 * LL: −147.33 | |||||
| Full Model: | F(7,101) = 1.42 R2 = 0.10 | χ2(14,85) = 45.78 *** AIC: 401.04 | χ2(14,85) = 47.51 *** AIC: 293.25 | χ2(14,85) = 41.93 *** AIC: 246.22 | χ2(14,85) = 57.65 *** AIC: 328.65 | |||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Allen, K.J.D.; Sammon, M.M.; Fox, K.R.; Stewart, J.G. Emotional Response Inhibition: A Shared Neurocognitive Deficit in Eating Disorder Symptoms and Nonsuicidal Self-Injury. Brain Sci. 2020, 10, 104. https://doi.org/10.3390/brainsci10020104
Allen KJD, Sammon MM, Fox KR, Stewart JG. Emotional Response Inhibition: A Shared Neurocognitive Deficit in Eating Disorder Symptoms and Nonsuicidal Self-Injury. Brain Sciences. 2020; 10(2):104. https://doi.org/10.3390/brainsci10020104
Chicago/Turabian StyleAllen, Kenneth J. D., M. McLean Sammon, Kathryn R. Fox, and Jeremy G. Stewart. 2020. "Emotional Response Inhibition: A Shared Neurocognitive Deficit in Eating Disorder Symptoms and Nonsuicidal Self-Injury" Brain Sciences 10, no. 2: 104. https://doi.org/10.3390/brainsci10020104
APA StyleAllen, K. J. D., Sammon, M. M., Fox, K. R., & Stewart, J. G. (2020). Emotional Response Inhibition: A Shared Neurocognitive Deficit in Eating Disorder Symptoms and Nonsuicidal Self-Injury. Brain Sciences, 10(2), 104. https://doi.org/10.3390/brainsci10020104