Serum Oxidative Status in People with Obesity: Relation to Tissue Losses, Glucose Levels, and Weight Reduction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Dietary and Physical Activity Intervention
2.3. Dividing Patients into Groups
| Group | Subgroups designation | |
| Weight loss | WL < 10% | WL > 10% |
| Visceral fat area loss | VFA < 15% | VFA > 15% |
| Total body water loss | TBW < 5% | TBW > 5% |
| Skeletal muscle mass loss | SMM < 5% | SMM > 5% |
2.4. Biochemical Assessment
2.5. Oxidative Status Parameters
2.6. Body Mass Parameters
2.7. Statistical Analysis
3. Results
3.1. Anthropometric Data of the Patients Included in the Study
3.2. Oxidative Stress Parameter Levels Related to Specific Compartment Loss
3.3. Correlation Analysis Revealed the Importance of Glucose Adjustment
4. Discussion
5. Conclusions
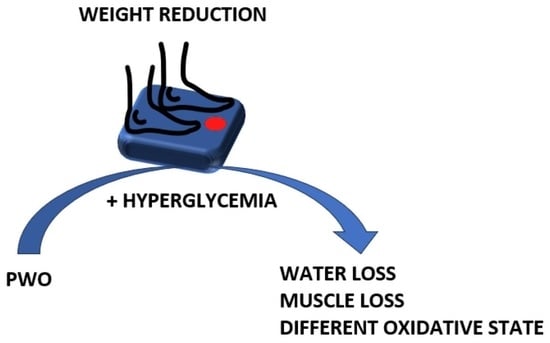
- The observed outcomes are a consequence of various processes that exacerbate and inhibit the severity of oxidative stress. On the one hand, obesity, hyperlipidemia, inflammation, and the process of active weight reduction generate increased amounts of reactive oxygen species (ROS); on the other hand, changes in dietary habits involving the introduction of a balanced diet based on healthy food items (vegetables, fruits, fish, oils, nuts, and seeds), reduced caloric intake, and moderate physical activity have led to an improvement in redox balance parameters;
- Regarding tissue loss, the levels of total cholesterol (t-CH) and low-density lipoprotein cholesterol (LDL-CH) did not change significantly. An interesting observation is that greater muscle losses were associated with a significant decrease in triglyceride (TG) levels, while smaller muscle losses were linked to a significant increase in high-density lipoprotein cholesterol (HDL-CH);
- A different pattern of changes in superoxide dismutase (SOD) isoenzymes’ activity was observed. Lower mitochondrial isoenzyme activity at the outset was associated with greater losses of skeletal muscle and water, in contrast to cytosolic isoenzyme activity, which was significantly lower before the diet in those who lost less water and skeletal muscle during the reduction;
- Glucose levels play a significant role in determining the course of weight reduction and influencing the redox state. Hyperglycemia is associated with higher total SOD levels, and improvements in glycemia lead to a significant increase in mitochondrial SOD isoenzyme activity;
- Overall, weight reduction is beneficial and leads to a decreased risk of cardiovascular diseases, but the pool of active antioxidant molecules is higher in cases of hyperglycemia, and it increases even more after glycemia improvement and weight reduction;
- It also appears from this study that body weight alone is not an adequate indicator to predict the glycemic and redox statuses of patients.
Study Limitation
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Obesity. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 6 December 2022).
- Health Status of Population in Poland in 2019. Główny Urząd Statystyczny. Available online: https://stat.gov.pl/obszary-tematyczne/zdrowie/zdrowie/stan-zdrowia-ludnosci-polski-w-2019-r-,6,7.htmL (accessed on 6 December 2022).
- Di Domenico, M.; Pinto, F.; Quagliuolo, L.; Contaldo, M.; Settembre, G.; Romano, A.; Coppola, M.; Ferati, K.; Bexheti-Ferati, A.; Sciarra, A.; et al. The Role of Oxidative Stress and Hormones in Controlling Obesity. Front. Endocrinol. 2019, 10, 540. [Google Scholar] [CrossRef]
- Zalejska-Fiolka, J.; Hubková, B.; Birková, A.; Veliká, B.; Puchalska, B.; Kasperczyk, S.; Błaszczyk, U.; Fiolka, R.; Bożek, A.; Maksym, B.; et al. Prognostic Value of the Modified Atherogenic Index of Plasma during Body Mass Reduction in Polish Obese/Overweight People. Int. J. Environ. Res. Public Health 2019, 16, 68. [Google Scholar] [CrossRef] [PubMed]
- Jakubiak, G.K.; Osadnik, K.; Lejawa, M.; Kasperczyk, S.; Osadnik, T.; Pawlas, N. Oxidative Stress in Association with Metabolic Health and Obesity in Young Adults. Oxidative Med. Cell. Longev. 2021, 2021, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Zielinska-Blizniewska, H.; Sitarek, P.; Merecz-Sadowska, A.; Malinowska, K.; Zajdel, K.; Jablonska, M.; Sliwinski, T.; Zajdel, R. Plant Extracts and Reactive Oxygen Species as Two Counteracting Agents with Anti- and Pro-Obesity Properties. Int. J. Mol. Sci. 2019, 20, 4556. [Google Scholar] [CrossRef] [PubMed]
- Manna, P.; Jain, S.K. Obesity, Oxidative Stress, Adipose Tissue Dysfunction, and the Associated Health Risks: Causes and Therapeutic Strategies. Metab. Syndr. Relat. Disord. 2015, 13, 423–444. [Google Scholar] [CrossRef]
- Vanacore, D.; Messina, G.; Lama, S.; Bitti, G.; Ambrosio, P.; Tenore, G.; Messina, A.; Monda, V.; Zappavigna, S.; Boccellino, M.; et al. Effect of restriction vegan diet’s on muscle mass, oxidative status, and myocytes differentiation: A pilot study. J. Cell. Physiol. 2018, 233, 9345–9353. [Google Scholar] [CrossRef]
- Zalejska-Fiolka, J.; Birková, A.; Hubková, B.; Wielkoszyński, T.; Čižmárová, B.; Szlachta, B.; Fiolka, R.; Błaszczyk, U.; Wylęgała, A.; Kasperczyk, S.; et al. Successful correction of hyperglycemia is critical for weight loss and a decrease in cardiovascular risk in obese patients. J. Nutr. Biochem. 2022, 106, 109021. [Google Scholar] [CrossRef]
- Pérez-Torres, I.; Castrejón-Téllez, V.; Soto, M.E.; Rubio-Ruiz, M.E.; Manzano-Pech, L.; Guarner-Lans, V. Oxidative Stress, Plant Natural Antioxidants, and Obesity. Int. J. Mol. Sci. 2021, 22, 1786. [Google Scholar] [CrossRef]
- Bray, G.A.; Heisel, W.E.; Afshin, A.; Jensen, M.D.; Dietz, W.H.; Long, M.; Kushner, R.F.; Daniels, S.R.; Wadden, T.A.; Tsai, A.G.; et al. The Science of Obesity Management: An Endocrine Society Scientific Statement. Endocr. Rev. 2018, 39, 79–132. [Google Scholar] [CrossRef]
- Poteryaeva, O.; Usynin, I. Antidiabetic role of high density lipoproteins. Biomeditsinskaya Khimiya 2018, 64, 463–471. [Google Scholar] [CrossRef]
- American Diabetes Association. Lifestyle Management. Diabetes Care 2017, 40, S33–S43. [Google Scholar] [CrossRef] [PubMed]
- Magkos, F.; Fraterrigo, G.; Yoshino, J.; Luecking, C.; Kirbach, K.; Kelly, S.C.; De Las Fuentes, L.; He, S.; Okunade, A.L.; Patterson, B.W.; et al. Effects of Moderate and Subsequent Progressive Weight Loss on Metabolic Function and Adipose Tissue Biology in Humans with Obesity. Cell Metab. 2016, 23, 591–601. [Google Scholar] [CrossRef] [PubMed]
- Ōyanagui, Y. Reevaluation of assay methods and establishment of kit for superoxide dismutase activity. Anal. Biochem. 1984, 142, 290–296. [Google Scholar] [CrossRef]
- Erel, O. A novel automated direct measurement method for total antioxidant capacity using a new generation, more stable ABTS radical cation. Clin. Biochem. 2004, 37, 277–285. [Google Scholar] [CrossRef]
- Richterich, R. Chemia Kliniczna; PZWL: Warszawa, Poland, 1971. [Google Scholar]
- Erel, O. A new automated colorimetric method for measuring total oxidant status. Clin. Biochem. 2005, 38, 1103–1111. [Google Scholar] [CrossRef] [PubMed]
- Ohkawa, H.; Ohishi, N.; Yagi, K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal. Biochem. 1979, 95, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.K. In vivo externalization of phosphatidylserine and phosphatidylethanolamine in the membrane bilayer and hypercoagulability by the lipid peroxidation of erythrocytes hemoerythrocytes in rats. J. Clin. Investig. 1985, 76, 281–286. [Google Scholar] [CrossRef]
- Koster, J.F.; Biemond, P.; Swaak, A.J. Intracellular and extracellular sulphydryl levels in rheumatoid arthritis. Ann. Rheum. Dis. 1986, 45, 44–46. [Google Scholar] [CrossRef]
- Södergren, E.; Nourooz-Zadeh, J.; Berglund, L.; Vessby, B. Re-evaluation of the ferrous oxidation in xylenol orange assay for the measurement of plasma lipid hydroperoxides. J. Biochem. Biophys. Methods 1998, 37, 137–146. [Google Scholar] [CrossRef]
- McLester, C.N.; Nickerson, B.S.; Kliszczewicz, B.M.; McLester, J.R. Reliability and Agreement of Various InBody Body Composition Analyzers as Compared to Dual-Energy X-Ray Absorptiometry in Healthy Men and Women. J. Clin. Densitom. 2020, 23, 443–450. [Google Scholar] [CrossRef]
- Chung, Y.J.; Kim, E.Y. Usefulness of bioelectrical impedance analysis and ECW ratio as a guidance for fluid management in critically ill patients after operation. Sci. Rep. 2021, 11, 12168. [Google Scholar] [CrossRef] [PubMed]
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.-P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation 2021, 143, e984–e1010. [Google Scholar] [CrossRef] [PubMed]
- Pi-Sunyer, X. Changes in body composition and metabolic disease risk. Eur. J. Clin. Nutr. 2018, 73, 231–235. [Google Scholar] [CrossRef]
- Zalejska-Fiolka, J.; Birková, A.; Wielkoszyński, T.; Hubková, B.; Szlachta, B.; Fiolka, R.; Błaszczyk, U.; Kuzan, A.; Gamian, A.; Mareková, M.; et al. Loss of Skeletal Muscle Mass and Intracellular Water as Undesired Outcomes of Weight Reduction in Obese Hyperglycemic Women: A Short-Term Longitudinal Study. Int. J. Environ. Res. Public Heal. 2022, 19, 1001. [Google Scholar] [CrossRef] [PubMed]
- Shida, T.; Oshida, N.; Oh, S.; Okada, K.; Shoda, J. Progressive reduction in skeletal muscle mass to visceral fat area ratio is associated with a worsening of the hepatic conditions of non-alcoholic fatty liver disease. Diabetes Metab. Syndr. Obes. Targets Ther. 2019, 12, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Schieber, M.; Chandel, N.S. ROS Function in Redox Signaling and Oxidative Stress. Curr. Biol. 2014, 24, R453–R462. [Google Scholar] [CrossRef]
- Dias, T.R.; Martin-Hidalgo, D.; Silva, B.M.; Oliveira, P.F.; Alves, M.G. Endogenous and Exogenous Antioxidants As a Tool to Ameliorate Male Infertility Induced by Reactive Oxygen Species. Antioxid. Redox Signal. 2020, 33, 767–785. [Google Scholar] [CrossRef]
- Dandona, P.; Mohanty, P.; Ghanim, H.; Aljada, A.; Browne, R.; Hamouda, W.; Prabhala, A.; Afzal, A.; Garg, R. The Suppressive Effect of Dietary Restriction and Weight Loss in the Obese on the Generation of Reactive Oxygen Species by Leukocytes, Lipid Peroxidation, and Protein Carbonylation1. J. Clin. Endocrinol. Metab. 2001, 86, 355–362. [Google Scholar] [CrossRef]
- Jung, T.; Bader, N.; Grune, T. Lipofuscin: Formation, distribution, and metabolic consequences. Ann. N. Y. Acad. Sci. 2007, 1119, 97–111. [Google Scholar] [CrossRef]
- Cazzola, R.; Rondanelli, M.; Russo-Volpe, S.; Ferrari, E.; Cestaro, B. Decreased membrane fluidity and altered susceptibility to peroxidation and lipid composition in overweight and obese female erythrocytes. J. Lipid Res. 2004, 45, 1846–1851. [Google Scholar] [CrossRef]
- Rupérez, A.I.; Gil, A.; Aguilera, C.M. Genetics of Oxidative Stress in Obesity. Int. J. Mol. Sci. 2014, 15, 3118–3144. [Google Scholar] [CrossRef] [PubMed]
- Fraga, C.G.; Oteiza, P.I.; Galleano, M. In vitro measurements and interpretation of total antioxidant capacity. Biochim. Biophys. Acta (BBA) Gen. Subj. 2014, 1840, 931–934. [Google Scholar] [CrossRef] [PubMed]
- Gać, P.; Poręba, M.; Januszewska, L.; Prokopowicz, A.; Martynowicz, H.; Mazur, G.; Poręba, R. The Total Antioxidant Status, Serum Selenium Concentrations and the Ultrasound Assessment Carotid Intima Media Thickness in Patients with Arterial Hypertension. Antioxidants 2021, 10, 63. [Google Scholar] [CrossRef] [PubMed]
- Matés, J.M.; Pérez-Gómez, C.; De Castro, I.N. Antioxidant enzymes and human diseases. Clin. Biochem. 1999, 32, 595–603. [Google Scholar] [CrossRef] [PubMed]
- Isogawa, A.; Yamakado, M.; Yano, M.; Shiba, T. Serum superoxide dismutase activity correlates with the components of metabolic syndrome or carotid artery intima-media thickness. Diabetes Res. Clin. Pract. 2009, 86, 213–218. [Google Scholar] [CrossRef]
- Yubero-Serrano, E.M.; Delgado-Lista, J.; Peña-Orihuela, P.; Perez-Martinez, P.; Fuentes, F.; Marin, C.; Tunez, I.; Tinahones, F.J.; Perez-Jimenez, F.; Roche, H.M.; et al. Oxidative stress is associated with the number of components of metabolic syndrome: LIPGENE study. Exp. Mol. Med. 2013, 45, e28. [Google Scholar] [CrossRef]
- Liu, Z.; Wang, M.; Zhang, C.; Zhou, S.; Ji, G. Molecular Functions of Ceruloplasmin in Metabolic Disease Pathology. Diabetes Metab. Syndr. Obes. Targets Ther. 2022, 15, 695–711. [Google Scholar] [CrossRef]




| Before Diet | After Diet | p | |
|---|---|---|---|
| Weight (kg) | 101.0 ± 21.0 | 90.7 ± 19.0 | <0.001 |
| BMI (kg/m2) | 36.1 ± 6.5 | 32.5 ± 6.1 | <0.001 |
| AC (cm) | 40.5 ± 6.2 | 35.7 ± 3.9 | <0.001 |
| WC (cm) | 109.8 ± 14.6 | 98.9 ± 14.5 | <0.001 |
| VFA (cm2) | 142.2 ± 34.3 | 115.5 ± 33.5 | <0.001 |
| PBF (%) | 39.9 ± 9.1 | 36.6 ± 9.5 | <0.001 |
| TBW (L) | 44.2 ± 9.5 | 41.2 ± 8.7 | <0.001 |
| SMM (kg) | 33.8 ± 7.7 | 31.2 ± 6.9 | <0.001 |
| Glucose (mg/dL) | 117.7 ± 38.7 | 90.6 ± 16.9 | <0.001 |
| FRU (umol/L) | 344.8 ± 76.8 | 314.6 ± 44.6 | <0.01 |
| FRU/PROT | 4.58 ± 1.03 | 4.2 ± 0.62 | <0.05 |
| INS (µIU/mL) | 12.0 ± 8.8 | 11.0 ± 8.5 | ns |
| HOMA-IR | 3.70 ± 3.38 | 2.53 ± 2.16 | <0.01 |
| CRP (mg/L) | 3.58 ± 4.6 | 3.08 ± 3.02 | ns |
| t-CH (mg/dL) | 223.1 ± 54.6 | 218.0 ± 44.9 | ns |
| TG (mg/dL) | 121.3 ± 56.8 | 102.9 ± 41.8 | <0.01 |
| HDL-CH (mg/dL) | 56.3 ± 11.0 | 61.2 ± 11.6 | <0.001 |
| LDL-CH (mg/dL) | 138.8 ± 41.6 | 129.9 ± 30.0 | ns |
| New-AIP | 0.90 ± 0.37 | 0.73 ± 0.31 | <0.001 |
| SOD (NU/mL) | 13.8 ± 3.9 | 17.0 ± 1.8 | <0.001 |
| MnSOD (NU/mL) | 7.4 ± 3.0 | 8.9 ± 2.0 | <0.01 |
| CuZnSOD (NU/mL) | 6.4 ± 4.6 | 8.2 ± 1.7 | 0.011 |
| CER (mg/dL) | 34.4 ± 9.1 | 36.1 ± 10.7 | ns |
| TAC (mmol/L) | 1.19 ± 0.19 | 1.25 ± 0.11 | <0.05 |
| TOS (μmol/L) | 5.94 ± 4.65 | 2.13 ± 1.86 | <0.001 |
| OSI (TOS/TAC) | 5.42 ± 4.19 | 1.80 ± 1.65 | <0.001 |
| MDA (μmol/L) | 2.93 ± 1.06 | 2.24 ± 0.74 | <0.001 |
| LPH (μmol/L) | 3.39 ± 2.79 | 1.19 ± 1.27 | <0.001 |
| LPS (RF) | 604.2 ± 320.9 | 582.8 ± 273.4 | ns |
| PSH (μmol/L) | 202.0 ± 45.7 | 221.3 ± 49.4 | <0.01 |
| PSH/g of protein (μmol/g) | 2.67 ± 0.60 | 2.94 ± 0.64 | <0.01 |
| Weight Loss | VFA Loss | TBW Loss | SMM Loss | ||||||
|---|---|---|---|---|---|---|---|---|---|
| WL < 10% | WL > 10% | VFA < 15% | VFA > 15% | TBW < 5% | TBW > 5% | SMM < 5% | SMM > 5% | ||
| Parameter | X | N = 34 | N = 19 | N = 21 | N = 31 | N = 27 | N = 20 | N = 24 | N = 24 |
| Age (y) | 49 ± 12 | 46 ± 10 # ns | 50 ± 11 | 46 ± 11 # ns | 50 ± 11 | 44 ± 12 # < 0.05 | 50 ± 11 | 47 ± 9 # ns | |
| Height (cm) | 166 ± 8 | 168 ± 9 # ns | 168 ± 9 | 167 ± 8 # ns | 165 ± 7 | 168 ± 9 # ns | 165 ± 7 | 168 ± 8 # ns | |
| Weight (kg) p (1 vs. 2) | 1 | 99.3 ± 22.1 | 104.1 ± 18.9 # ns | 102.7 ± 21.6 | 100.1 ± 21.2 # ns | 98.9 ± 19.8 | 105.5 ± 24.1 # ns | 97.7 ± 20.3 | 104.8 ± 21.8 # ns |
| 2 | 93.0 ± 20.6 | 86.7 ± 15.4 # ns | 95.1 ± 19.8 | 87.7 ± 18.4 # ns | 89.1 ± 19.4 | 93.0 ± 19.9 # ns | 89.0 ± 19.6 | 92.5 ± 19.2 # ns | |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| BMI (kg/m2) p (1 vs. 2) | 1 | 35.8 ± 7.2 | 36.7 ± 5.1 # ns | 36.3 ± 6.4 | 36.0 ± 6.7 # ns | 36.2 ± 6.8 | 37.1 ± 6.6 # ns | 36.1 ± 6.8 | 36.9 ± 6.3 # ns |
| 2 | 33.6 ± 6.7 | 30.6 ± 4.1 # < 0.05 | 33.7 ± 6.2 | 31.6 ± 6.0 # ns | 32.6 ± 6.8 | 32.8 ± 5.8 # ns | 32.9 ± 6.7 | 32.6 ± 5.8 # ns | |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| WC (cm) p (1 vs. 2) | 1 | 109.2 ± 15.4 | 110.8 ± 13.4 # ns | 112.1 ± 15.6 | 118.3 ± 14.1 # ns | 109.4 ± 15.6 | 111.0 ± 15.0 # ns | 107.5 ± 15.9 | 112.8 ± 14.1 # ns |
| 2 | 101.6 ± 14.0 | 94.0 ± 14.4 # ns | 102.1 ± 15.2 | 96.5 ± 14.0 # ns | 99.2 ± 15.5 | 98.6 ± 14.9 # ns | 97.6 ± 14.8 | 100.2 ± 15.0 # ns | |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| TBW (L) p (1 vs. 2) | 1 | 43.5 ± 9.8 | 45.4 ± 9.1 # ns | 45.6 ± 10.2 | 43.5 ± 9.1 # ns | 41.3 ± 6.7 | 47.5 ± 11.1 # ns | 40.5 ± 6.9 | 47.5 ± 9.9 # < 0.001 |
| 2 | 39.9 ± 8.5 | 42.9 ± 8.9 # ns | 43.3 ± 9.4 | 40.0 ± 8.2 # ns | 40.3 ± 7.0 | 42.4 ± 10.9 # ns | 39.6 ± 7.4 | 42.5 ± 9.8 # ns | |
| <0.001 | <0.05 | 0.001 | <0.01 | ns | <0.001 | ns | <0.001 | ||
| VFA (cm2) p (1 vs. 2) | 1 | 138.5 ± 33.7 | 148.8 ± 35.3 # ns | 141.3 ± 35.1 | 142.2 ± 34.8 # ns | 143.3 ± 32.9 | 144.8 ± 36.8 # ns | 142.5 ± 32.5 | 115.59 ± 34.0 # ns |
| 2 | 117.7 ± 33.3 | 111.6 ± 34.4 # ns | 130.1 ± 29.4 | 105.6 ± 32.9 # <0.001 | 115.9 ± 35.1 | 115.4 ± 32.6 # ns | 115.6 ± 34.0 | 116.2 ± 33.4 # ns | |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| AC (cm) p (1 vs. 2) | 1 | 40.2 ± 7.1 | 40.8 ± 4.4 # ns | 40.3 ± 4.9 | 40.7 ± 7.2 # ns | 39.9 ± 6.4 | 42.1 ± 6.6 # ns | 39.5 ± 6.5 | 41.8 ± 6.2 # ns |
| 2 | 36.4 ± 4.4 | 34.7 ± 3.0 # ns | 38.2 ± 4.0 | 34.3 ± 3.1 # < 0.001 | 35.5 ± 4.4 | 36.0 ± 3.2 # ns | 35.4 ± 4.2 | 36.3 ± 3.3 # ns | |
| <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | ||
| BFM (kg) p (1 vs. 2) | 1 | 40.1 ± 15.5 | 42.4 ± 13.2 # ns | 40.6 ± 13.6 | 40.8 ± 15.7 # ns | 42.8 ± 14.9 | 40.7 ± 15.0 # ns | 42.7 ± 15.0 | 40.0 ± 13.5 # ns |
| 2 | 36.8 ± 12.1 | 28.9 ± 9.7 # < 0.01 | 39.5 ± 12.1 | 29.9 ± 10.1 # < 0.001 | 32.6 ± 13.9 | 34.6 ± 7.6 # ns | 33.3 ± 16.6 | 33.7 ± 9.3 # ns | |
| <0.01 | <0.001 | <0.001 | <0.001 | <0.001 | <0.05 | <0.001 | <0.01 | ||
| Biochemical Parameters | Pearson’s r Significance p | ΔWeight | ΔVFA | ΔTBW | ΔSMM | ΔGlc | ΔCH | ΔTG |
|---|---|---|---|---|---|---|---|---|
| ΔGlucose | r | 0.207 | 0.028 | 0.214 | 0.166 | 0.177 | 0.141 | |
| p | ns | ns | ns | ns | ns | ns | ||
| Δt-CH | r | 0.094 | −0.011 | −0.014 | 0.022 | 0.177 | ||
| p | ns | ns | ns | ns | ns | |||
| ΔTG | r | 0.284 | 0.087 | −0.017 | 0.056 | 0.141 | 0.558 | |
| p | <0.05 | ns | ns | ns | ns | <0.0001 | ||
| ΔLDL-CH | r | 0.107 | 0.077 | −0.131 | −0.128 | 0.188 | 0.949 | 0.339 |
| p | ns | ns | ns | ns | ns | <0.0001 | <0.05 | |
| ΔHDL-CH | r | −0.062 | 0.032 | 0.111 | 0.129 | 0.051 | 0.359 | 0.055 |
| p | ns | ns | ns | ns | ns | <0.05 | ns | |
| ΔNew-AIP | r | 0.449 | 0.12 | −0.115 | −0.054 | 0.07 | 0.472 | 0.783 |
| p | <0.01 | ns | ns | ns | 0 ns | <0.01 | <0.0001 | |
| ΔSOD | r | 0.174 | 0.012 | 0.113 | 0.104 | 0.475 | 0.16 | 0.136 |
| p | ns | ns | ns | ns | <0.0001 | ns | ns | |
| ΔMnSOD | r | −0.305 | 0.104 | −0.151 | −0.153 | −0.039 | 0.038 | −0.101 |
| p | <0.05 | ns | ns | ns | ns | ns | ns | |
| ΔCuZnSOD | r | 0.346 | −0.068 | 0.19 | 0.186 | 0.368 | 0.087 | 0.171 |
| p | <0.05 | ns | ns | ns | <0.01 | ns | ns | |
| ΔMDA | r | 0.165 | 0.144 | −0.152 | −0.142 | 0.349 | 0.037 | 0.007 |
| p | ns | ns | ns | ns | <0.05 | ns | ns | |
| ΔPSH/PROT | r | 0.06 | 0.012 | 0.014 | 0.008 | −0.066 | 0.107 | 0.08 |
| p | ns | ns | ns | ns | ns | ns | ns | |
| ΔTOS | r | 0.166 | 0.093 | 0.197 | 0.167 | 0.214 | −0.120 | 0.03 |
| p | ns | ns | ns | ns | ns | ns | ns | |
| ΔLPH | r | 0.175 | 0.058 | 0.199 | 0.17 | 0.279 | −0.097 | 0.019 |
| p | ns | ns | ns | ns | <0.05 | ns | ns |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szlachta, B.; Birková, A.; Wielkoszyński, T.; Gospodarczyk, A.; Hubková, B.; Dydoń, M.; Zalejska-Fiolka, J. Serum Oxidative Status in People with Obesity: Relation to Tissue Losses, Glucose Levels, and Weight Reduction. Antioxidants 2023, 12, 1923. https://doi.org/10.3390/antiox12111923
Szlachta B, Birková A, Wielkoszyński T, Gospodarczyk A, Hubková B, Dydoń M, Zalejska-Fiolka J. Serum Oxidative Status in People with Obesity: Relation to Tissue Losses, Glucose Levels, and Weight Reduction. Antioxidants. 2023; 12(11):1923. https://doi.org/10.3390/antiox12111923
Chicago/Turabian StyleSzlachta, Beata, Anna Birková, Tomasz Wielkoszyński, Alicja Gospodarczyk, Beáta Hubková, Maria Dydoń, and Jolanta Zalejska-Fiolka. 2023. "Serum Oxidative Status in People with Obesity: Relation to Tissue Losses, Glucose Levels, and Weight Reduction" Antioxidants 12, no. 11: 1923. https://doi.org/10.3390/antiox12111923