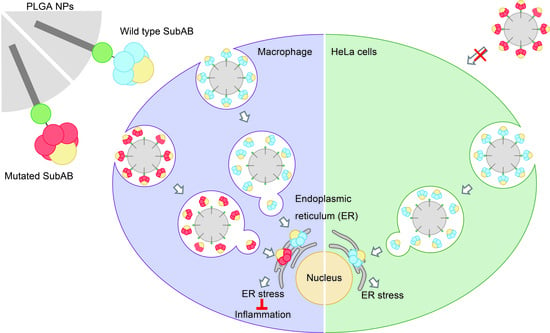
Controlled Delivery of an Anti-Inflammatory Toxin to Macrophages by Mutagenesis and Nanoparticle Modification
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Purification of His-Tagged Toxins
2.3. Site-Directed Mutagenesis of B Subunit of SubAB
2.4. HiLyte Fluor™ 555 (HF555) Labeling of Toxins
2.5. Cell Culture
2.6. Fluorescence Microscopy
2.7. Preparation of PLGA NPs
2.8. Preparation of FITC-Conjugated Oleylamine
2.9. Preparation of FITC-Labeled PLGA NPs
2.10. Characterization of PLGA NPs
2.11. Surface Modification of PLGA NPs with SubAB Toxins
2.12. Evaluation of pH-Dependent Release of His-Tagged SubAB Toxins
2.13. Intracellular Uptake of SubAB Toxin-PLGA NPs
2.14. Western Blotting
2.15. MTT Assay
2.16. Griess Assay
2.17. Statistical Analysis
3. Results and Discussion
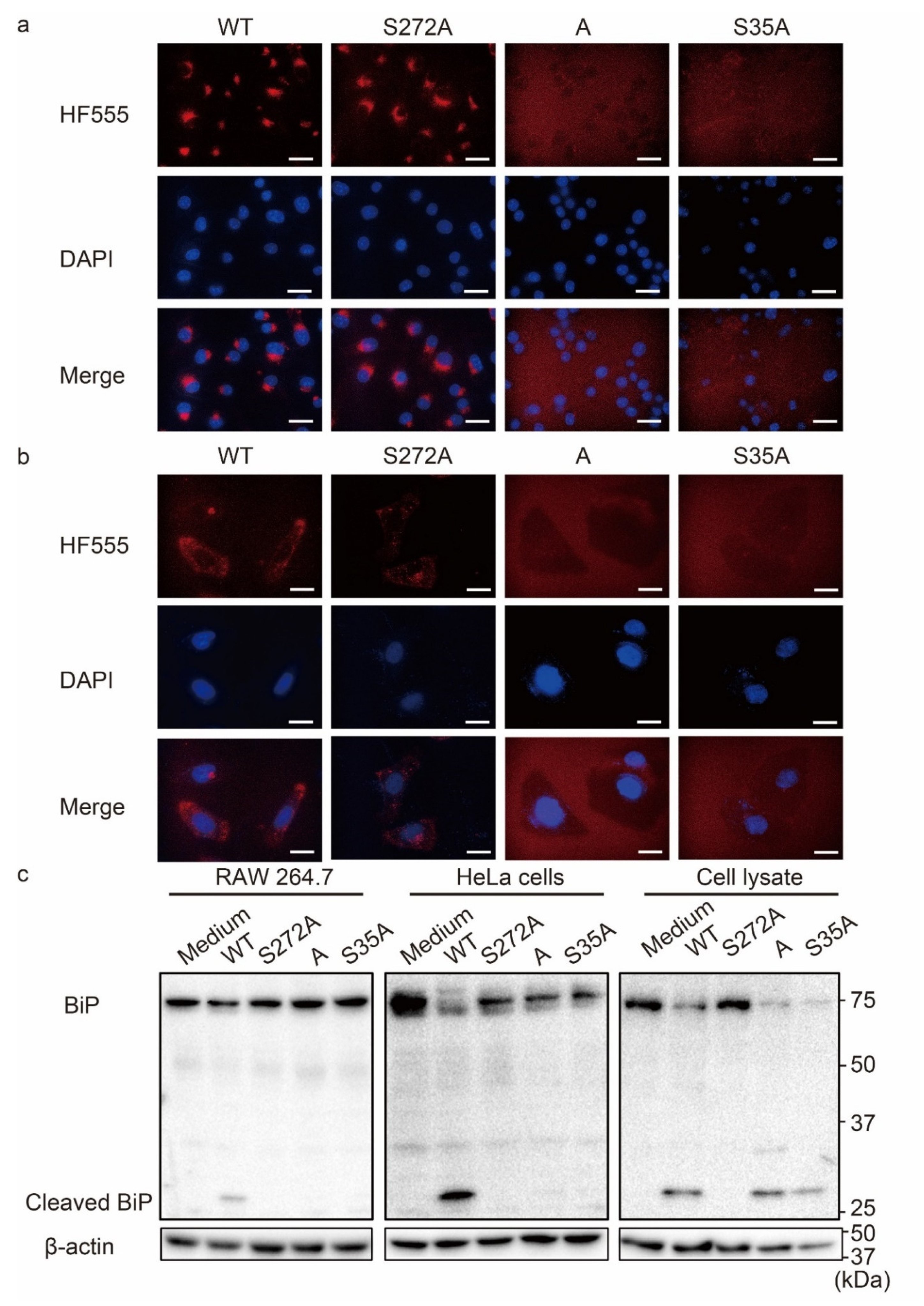
3.1. Cell Recognition-Inactivated SubABS35A (S35A) Mutant Had Decreased Uptake by Cells
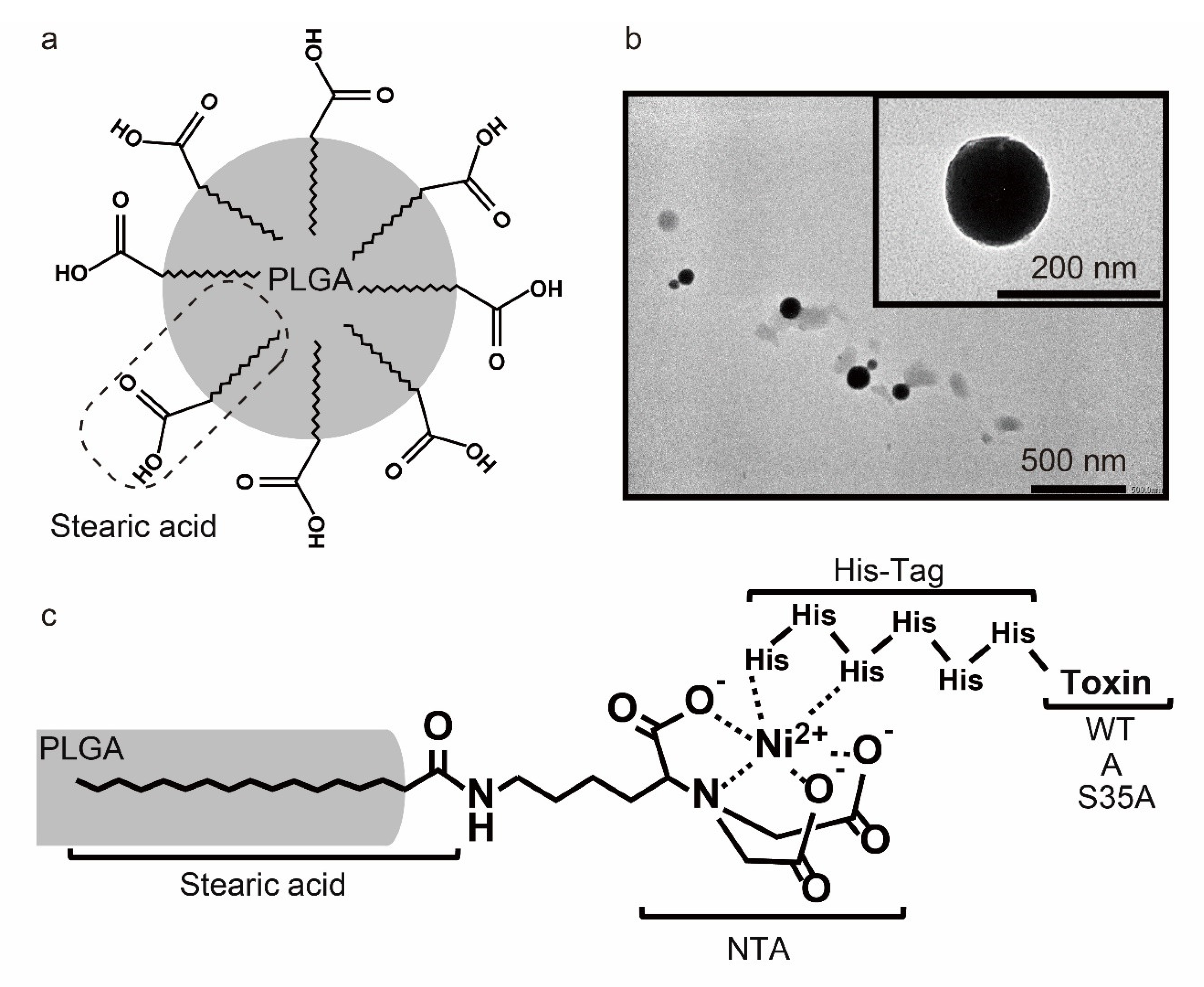
3.2. Preparation and Characterization of PLGA NPs Modified with Various SubAB Toxins
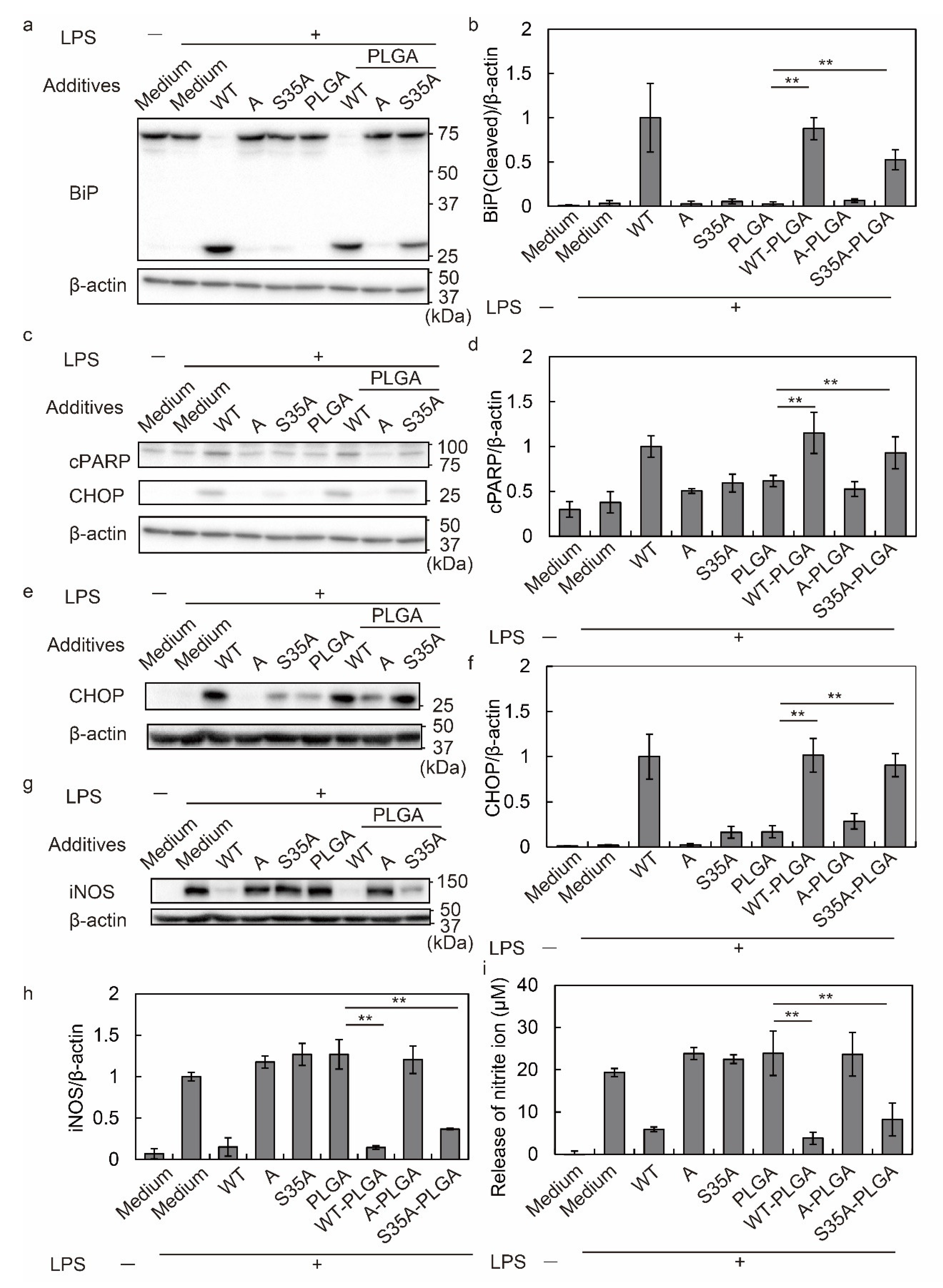
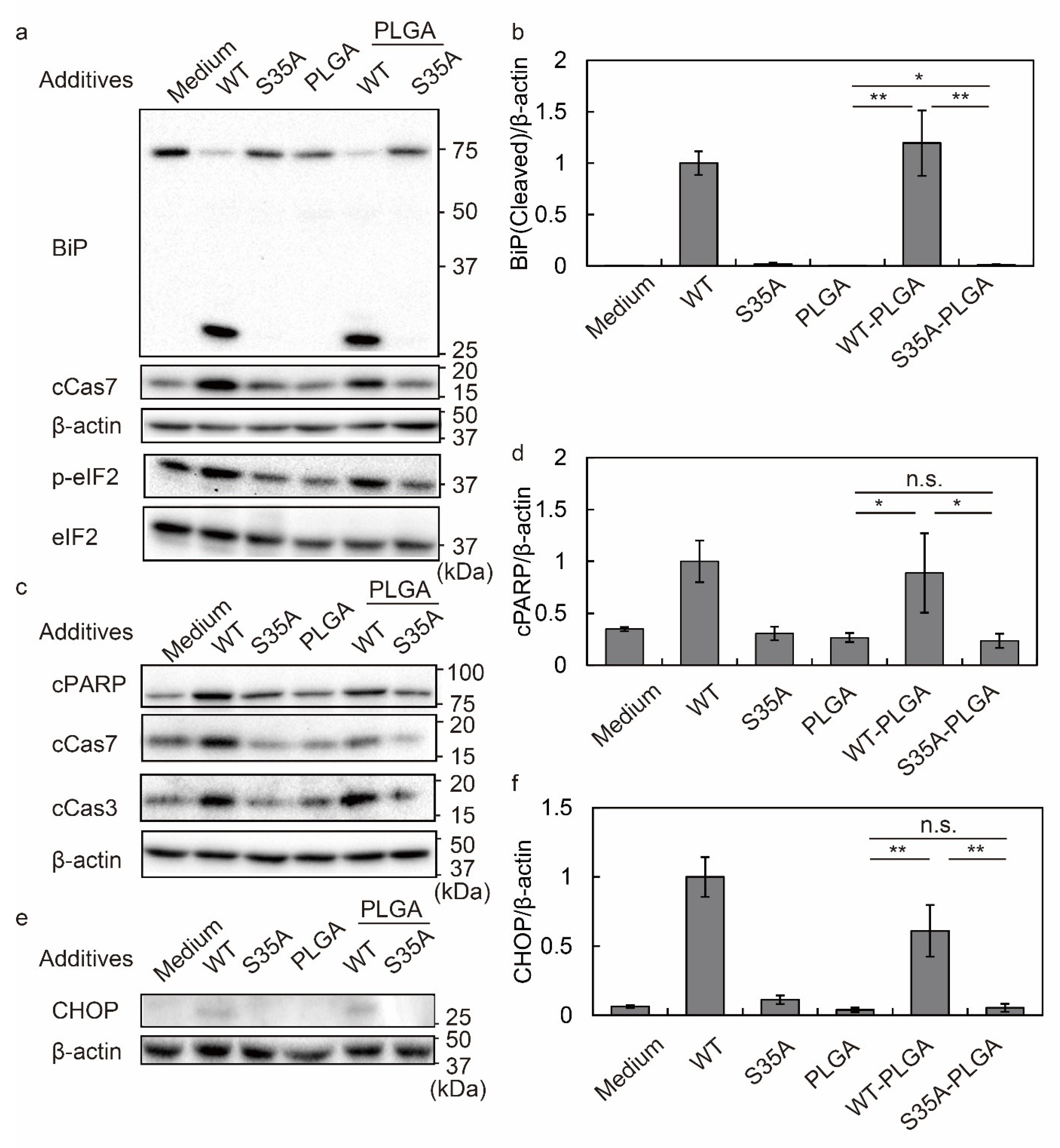
3.3. WT- and S35A-PLGA NPs Induce ER Stress and Inhibit iNOS Expression in Macrophages
3.4. S35A-PLGA NPs Do Not Induce ER Stress or Cytotoxicity in HeLa Cells
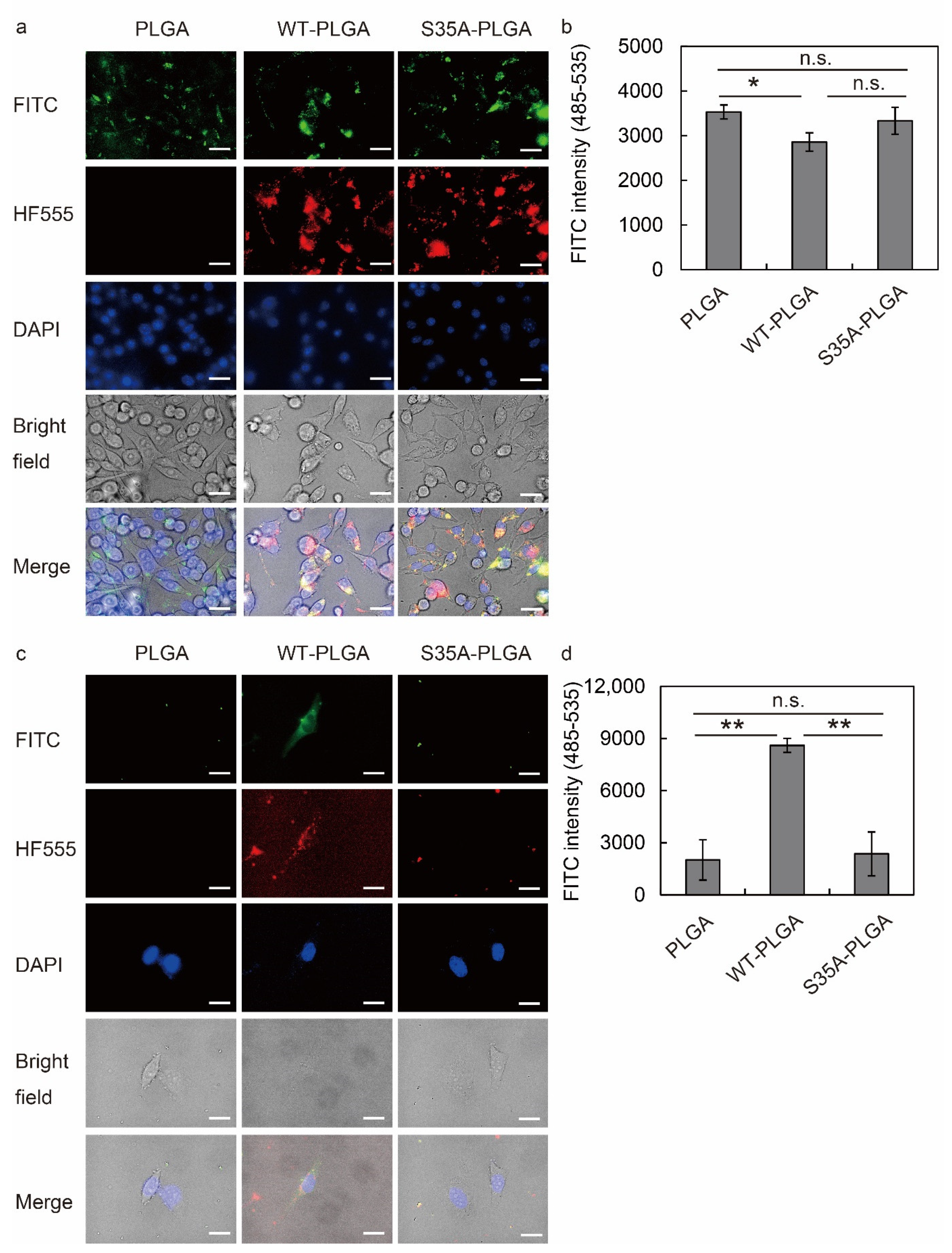
3.5. S35A-PLGA NPs Specifically Enter Macrophages, but Not Epithelial Cells
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vargason, A.M.; Anselmo, A.C.; Mitragotri, S. The evolution of commercial drug delivery technologies. Nat. Biomed. Eng. 2021, 5, 951–967. [Google Scholar] [CrossRef] [PubMed]
- Hu, G.; Guo, M.; Xu, J.; Wu, F.; Fan, J.; Huang, Q.; Yang, G.; Lv, Z.; Wang, X.; Jin, Y. Nanoparticles Targeting Macrophages as Potential Clinical Therapeutic Agents Against Cancer and Inflammation. Front. Immunol. 2019, 10, 1998. [Google Scholar] [CrossRef] [PubMed]
- Karchemski, F.; Zucker, D.; Barenholz, Y.; Regev, O. Carbon nanotubes-liposomes conjugate as a platform for drug delivery into cells. J. Control. Release 2012, 160, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Lv, B.; Zheng, J.; Lu, C.; Liu, J.; Lei, Y.; Yang, M.; Wang, Y.; Li, Z.; Yang, Y.; et al. RBC-hitchhiking chitosan nanoparticles loading methylprednisolone for lung-targeting delivery. J. Control. Release 2022, 341, 702–715. [Google Scholar] [CrossRef]
- Heo, R.; You, D.G.; Um, W.; Choi, K.Y.; Jeon, S.; Park, J.S.; Choi, Y.; Kwon, S.; Kim, K.; Kwon, I.C.; et al. Dextran sulfate nanoparticles as a theranostic nanomedicine for rheumatoid arthritis. Biomaterials 2017, 131, 15–26. [Google Scholar] [CrossRef]
- Yang, Y.; Chen, F.; Xu, N.; Yao, Q.; Wang, R.; Xie, X.; Zhang, F.; He, Y.; Shao, D.; Dong, W.F.; et al. Red-light-triggered self-destructive mesoporous silica nanoparticles for cascade-amplifying chemo-photodynamic therapy favoring antitumor immune responses. Biomaterials 2022, 281, 121368. [Google Scholar] [CrossRef]
- Chang, Y.; Cho, B.; Lee, E.; Kim, J.; Yoo, J.; Sung, J.S.; Kwon, Y.; Kim, J. Electromagnetized gold nanoparticles improve neurogenesis and cognition in the aged brain. Biomaterials 2021, 278, 121157. [Google Scholar]
- Cruz, L.J.; van Dijk, T.; Vepris, O.; Li, T.; Schomann, T.; Baldazzi, F.; Kurita, R.; Nakamura, Y.; Grosveld, F.; Philipsen, S.; et al. PLGA-Nanoparticles for Intracellular Delivery of the CRISPR-Complex to Elevate Fetal Globin Expression in Erythroid Cells. Biomaterials 2021, 268, 120580. [Google Scholar] [CrossRef]
- Yan, J.; Yao, Y.; Yan, S.; Gao, R.; Lu, W.; He, W. Chiral Protein supraparticles for tumor suppression and synergistic immunotherapy: An enabling strategy for bioactive supramolecular chirality construction. Nano Lett. 2020, 20, 5844–5852. [Google Scholar] [CrossRef]
- Lai, W.F. Non-conjugated polymers with intrinsic luminescence for drug delivery. J. Drug Deliv. Sci. Technol. 2020, 59, 101916. [Google Scholar] [CrossRef]
- Lai, W.F.; Huang, E.; Lui, K.H. Alginate-based complex fibers with the janus morphology for controlled release of co-delivered drugs. Asian J. Pharm. Sci. 2021, 16, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Arkaban, H.; Barani, M.; Akbarizadeh, M.R.; Pal Singh Chauhan, N.; Jadoun, S.; Dehghani Soltani, M.; Zarrintaj, P. polyacrylic acid nanoplatforms: Antimicrobial, tissue engineering, and cancer theranostic applications. Polymers 2022, 14, 1259. [Google Scholar] [CrossRef] [PubMed]
- Han, G.; You, C.C.; Kim, B.J.; Turingan, R.S.; Forbes, N.S.; Martin, C.T.; Rotello, V.M. Light-regulated release of DNA and its delivery to nuclei by means of photolabile gold nanoparticles. Angew. Chem. Int. Ed. Engl. 2006, 45, 3165–3169. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.; Jin, F.; Liu, D.; Shu, G.; Wang, X.; Qi, J.; Sun, M.; Yang, P.; Jiang, S.; Ying, X.; et al. ROS-responsive nano-drug delivery system combining mitochondria-targeting ceria nanoparticles with atorvastatin for acute kidney injury. Theranostics 2020, 10, 2342–2357. [Google Scholar] [CrossRef] [PubMed]
- Piao, S.; Amaravadi, R.K. Targeting the lysosome in cancer. Ann. N. Y. Acad. Sci. 2016, 1371, 45–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwarz, D.S.; Blower, M.D. The endoplasmic reticulum: Structure, function and response to cellular signaling. Cell Mol. Life Sci. 2016, 73, 79–94. [Google Scholar] [CrossRef] [Green Version]
- Gidalevitz, T.; Stevens, F.; Argon, Y. Orchestration of secretory protein folding by ER chaperones. Biochim. Biophys. Acta 2013, 1833, 2410–2424. [Google Scholar] [CrossRef] [Green Version]
- Fuson, K.L.; Zheng, M.; Craxton, M.; Pataer, A.; Ramesh, R.; Chada, S.; Sutton, R.B. Structural mapping of post-translational modifications in human interleukin-24: Role of N-linked glycosylation and disulfide bonds in secretion and activity. J. Biol. Chem. 2009, 284, 30526–30533. [Google Scholar] [CrossRef] [Green Version]
- Jäger, R.; Bertrand, M.J.; Gorman, A.M.; Vandenabeele, P.; Samali, A. The unfolded protein response at the crossroads of cellular life and death during endoplasmic reticulum stress. Biol. Cell 2012, 104, 259–270. [Google Scholar] [CrossRef]
- Salminen, A.; Kaarniranta, K.; Kauppinen, A. ER stress activates immunosuppressive network: Implications for aging and Alzheimer’s disease. J. Mol. Med. 2020, 98, 633–650. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Y.; Cheung, Y.K.; Ma, C.; Zhao, S.; Gao, D.; Lo, P.C.; Fong, W.P.; Wong, K.S.; Ng, D.K.P. Endoplasmic Reticulum-Localized Two-Photon-Absorbing Boron Dipyrromethenes as Advanced Photosensitizers for Photodynamic Therapy. J. Med. Chem. 2018, 61, 3952–3961. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Gao, X.; Yuan, W.; Xu, L.; Deng, H.; Wu, C.; Yang, J.; Jin, X.; Zhang, C.; Zhu, X. Endoplasmic Reticulum-Targeted Fluorescent Nanodot with Large Stokes Shift for Vesicular Transport Monitoring and Long-Term Bioimaging. Small 2018, 14, e1800223. [Google Scholar] [CrossRef] [PubMed]
- Le Nours, J.; Paton, A.W.; Byres, E.; Troy, S.; Herdman, B.P.; Johnson, M.D.; Paton, J.C.; Rossjohn, J.; Beddoe, T. Structural basis of subtilase cytotoxin SubAB assembly. J. Biol. Chem. 2013, 288, 27505–27516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beddoe, T.; Paton, A.W.; Le Nours, J.; Rossjohn, J.; Paton, J.C. Structure, biological functions and applications of the AB5 toxins. Trends Biochem. Sci. 2010, 35, 411–418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paton, A.W.; Srimanote, P.; Talbot, U.M.; Wang, H.; Paton, J.C. A new family of potent AB(5) cytotoxins produced by Shiga toxigenic Escherichia coli. J. Exp. Med. 2004, 200, 35–46. [Google Scholar] [CrossRef] [Green Version]
- Nagasawa, S.; Ogura, K.; Tsutsuki, H.; Saitoh, H.; Moss, J.; Iwase, H.; Noda, M.; Yahiro, K. Uptake of Shiga-toxigenic Escherichia coli SubAB by HeLa cells requires an actin- and lipid raft-dependent pathway. Cell Microbiol. 2014, 16, 1582–1601. [Google Scholar] [CrossRef] [Green Version]
- Paton, A.W.; Beddoe, T.; Thorpe, C.M.; Whisstock, J.C.; Wilce, M.C.; Rossjohn, J.; Talbot, U.M.; Paton, J.C. AB5 subtilase cytotoxin inactivates the endoplasmic reticulum chaperone BiP. Nature 2006, 443, 548–552. [Google Scholar] [CrossRef]
- Chong, D.C.; Paton, J.C.; Thorpe, C.M.; Paton, A.W. Clathrin-dependent trafficking of subtilase cytotoxin, a novel AB5 toxin that targets the endoplasmic reticulum chaperone BiP. Cell Microbiol. 2008, 10, 795–806. [Google Scholar] [CrossRef]
- Smith, R.D.; Willett, R.; Kudlyk, T.; Pokrovskaya, I.; Paton, A.W.; Paton, J.C.; Lupashin, V.V. The COG complex, Rab6 and COPI define a novel Golgi retrograde trafficking pathway that is exploited by SubAB toxin. Traffic 2009, 10, 1502–1517. [Google Scholar] [CrossRef] [Green Version]
- Wolfson, J.J.; May, K.L.; Thorpe, C.M.; Jandhyala, D.M.; Paton, J.C.; Paton, A.W. Subtilase cytotoxin activates PERK, IRE1 and ATF6 endoplasmic reticulum stress-signalling pathways. Cell Microbiol. 2008, 10, 1775–1786. [Google Scholar] [CrossRef] [Green Version]
- Tsutsuki, H.; Yahiro, K.; Ogura, K.; Ichimura, K.; Iyoda, S.; Ohnishi, M.; Nagasawa, S.; Seto, K.; Moss, J.; Noda, M. Subtilase cytotoxin produced by locus of enterocyte effacement-negative Shiga-toxigenic Escherichia coli induces stress granule formation. Cell Microbiol. 2016, 18, 1024–1040. [Google Scholar] [CrossRef] [PubMed]
- Yahiro, K.; Tsutsuki, H.; Ogura, K.; Nagasawa, S.; Moss, J.; Noda, M. A negative regulator of autophagy, controls SubAB-mediated apoptosis and autophagy. Infect. Immun. 2014, 82, 4899–4908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsutsuki, H.; Zhang, T.; Yahiro, K.; Ono, K.; Fujiwara, Y.; Iyoda, S.; Wei, F.Y.; Monde, K.; Seto, K.; Ohnishi, M.; et al. Subtilase cytotoxin from Shiga-toxigenic Escherichia coli impairs the inflammasome and exacerbates enteropathogenic bacterial infection. iScience 2022, 25, 104050. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, T.; Yahiro, K.; Tsuji, A.B.; Terasaki, Y.; Morinaga, N.; Miyazaki, M.; Fukuda, Y.; Saga, T.; Moss, J.; Noda, M. Fatal hemorrhage induced by subtilase cytotoxin from Shiga-toxigenic Escherichia coli. Microb. Pathog. 2011, 50, 159–167. [Google Scholar] [CrossRef] [Green Version]
- Tsutsuki, H.; Yahiro, K.; Suzuki, K.; Suto, A.; Ogura, K.; Nagasawa, S.; Ihara, H.; Shimizu, T.; Nakajima, H.; Moss, J.; et al. Subtilase cytotoxin enhances Escherichia coli survival in macrophages by suppression of nitric oxide production through the inhibition of NF-kappaB activation. Infect. Immun. 2012, 80, 3939–3951. [Google Scholar] [CrossRef] [Green Version]
- Harada, A.; Tsutsuki, H.; Zhang, T.; Lee, R.; Yahiro, K.; Sawa, T.; Niidome, T. Preparation of Biodegradable PLGA-Nanoparticles Used for pH-Sensitive Intracellular Delivery of an Anti-inflammatory Bacterial Toxin to Macrophages. Chem. Pharm. Bull. 2020, 68, 363–368. [Google Scholar] [CrossRef] [Green Version]
- Nakamura, Y.; Kitagawa, T.; Ihara, H.; Kozaki, S.; Moriyama, M.; Kannan, Y. Potentiation by high potassium of lipopolysaccharide-induced nitric oxide production from cultured astrocytes. Neurochem. Int. 2006, 48, 43–49. [Google Scholar] [CrossRef]
- Yahiro, K.; Morinaga, N.; Satoh, M.; Matsuura, G.; Tomonaga, T.; Nomura, F.; Moss, J.; Noda, M. Identification and characterization of receptors for vacuolating activity of subtilase cytotoxin. Mol. Microbiol. 2006, 62, 480–490. [Google Scholar] [CrossRef]
- Morinaga, N.; Yahiro, K.; Matsuura, G.; Watanabe, M.; Nomura, F.; Moss, J.; Noda, M. Two distinct cytotoxic activities of subtilase cytotoxin produced by shiga-toxigenic Escherichia coli. Infect. Immun. 2007, 75, 488–496. [Google Scholar] [CrossRef] [Green Version]
- Tsutsuki, H.; Zhang, T.; Harada, A.; Rahman, A.; Ono, K.; Yahiro, K.; Niidome, T.; Sawa, T. Involvement of protein disulfide isomerase in subtilase cytotoxin-induced cell death in HeLa cells. Biochem. Biophys. Res. Commun. 2020, 525, 1068–1073. [Google Scholar] [CrossRef]
- Yamaji, T.; Hanamatsu, H.; Sekizuka, T.; Kuroda, M.; Iwasaki, N.; Ohnishi, M.; Furukawa, J.I.; Yahiro, K.; Hanada, K. A CRISPR Screen Using Subtilase Cytotoxin Identifies SLC39A9 as a Glycan-Regulating Factor. iScience 2019, 15, 407–420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yahiro, K.; Satoh, M.; Morinaga, N.; Tsutsuki, H.; Ogura, K.; Nagasawa, S.; Nomura, F.; Moss, J.; Noda, M. Identification of subtilase cytotoxin (SubAB) receptors whose signaling, in association with SubAB-induced BiP cleavage, is responsible for apoptosis in HeLa cells. Infect. Immun. 2011, 79, 617–627. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Byres, E.; Paton, A.W.; Paton, J.C.; Lofling, J.C.; Smith, D.F.; Wilce, M.C.; Talbot, U.M.; Chong, D.C.; Yu, H.; Huang, S.; et al. Incorporation of a non-human glycan mediates human susceptibility to a bacterial toxin. Nature 2008, 456, 648–652. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deng, L.; Song, J.; Gao, X.; Wang, J.; Yu, H.; Chen, X.; Varki, N.; Naito-Matsui, Y.; Galan, J.E.; Varki, A. Host adaptation of a bacterial toxin from the human pathogen Salmonella Typhi. Cell 2014, 159, 1290–1299. [Google Scholar] [CrossRef] [Green Version]
- Khan, N.; Sasmal, A.; Khedri, Z.; Secrest, P.; Verhagen, A.; Srivastava, S.; Varki, N.; Chen, X.; Yu, H.; Beddoe, T.; et al. Sialoglycan binding patterns of bacterial AB5 toxin B subunits correlate with host range and toxicity, indicating evolution independent of A subunits. J. Biol. Chem. 2022, 298, 101900. [Google Scholar] [CrossRef]
- Silva, A.T.C.R.; Cardoso, B.C.O.; e Silva, M.E.S.R.; Freitas, R.F.S.; Sousa, R.G. Synthesis, Characterization, and study of PLGA copolymer in vitro degradation. J. Biomater. Nanobiotechnol. 2015, 6, 8–19. [Google Scholar] [CrossRef] [Green Version]
- Yuan, Z.; Wei, P.; Huang, Y.; Zhang, W.; Chen, F.; Zhang, X.; Mao, J.; Chen, D.; Cai, Q.; Yang, X. Injectable PLGA microspheres with tunable magnesium ion release for promoting bone regeneration. Acta Biomater. 2019, 85, 294–309. [Google Scholar] [CrossRef]
- Kim, J.H.; Park, J.S.; Yang, H.N.; Woo, D.G.; Jeon, S.Y.; Do, H.J.; Lim, H.Y.; Kim, J.M.; Park, K.H. The use of biodegradable PLGA nanoparticles to mediate SOX9 gene delivery in human mesenchymal stem cells (hMSCs) and induce chondrogenesis. Biomaterials 2011, 32, 268–278. [Google Scholar] [CrossRef]
- Blasi, P.; D’Souza, S.S.; Selmin, F.; DeLuca, P.P. Plasticizing effect of water on poly(lactide-co-glycolide). J. Control. Release 2005, 108, 1–9. [Google Scholar] [CrossRef]
- Rapier, C.E.; Shea, K.J.; Lee, A.P. Investigating PLGA microparticle swelling behavior reveals an interplay of expansive intermolecular forces. Sci. Rep. 2021, 11, 14512. [Google Scholar] [CrossRef]
- Courant, T.; Roullin, V.G.; Cadiou, C.; Delavoie, F.; Molinari, M.; Andry, M.C.; Chuburu, F. Development and physic chemical characterization of copper complexes-loaded PLGA nanoparticles. Int. J. Pharm. 2009, 379, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Garms, B.C.; Poli, H.; Baggley, D.; Han, F.Y.; Whittaker, A.K.; Anitha, A.; Grøndahl, L. Evaluating the effect of synthesis, isolation, and characterisation variables on reported particle size and dispersity of drug loaded PLGA nanoparticles. Mater. Adv. 2021, 2, 5657–5671. [Google Scholar] [CrossRef]
- Liu, X.; Gillespie, M.; Ozel, A.D.; Dikici, E.; Daunert, S.; Bachas, L.G. Electrochemical properties and temperature dependence of a recombinant laccase from Thermus thermophilus. Anal. Bioanal. Chem. 2011, 399, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.D.; O’Carra, R.; Jones, J.; Woodward, J.G.; Mumper, R.J. Preparation and characterization of nickel nanoparticles for binding to his-tag proteins and antigens. Pharm. Res. 2007, 24, 343–352. [Google Scholar] [CrossRef] [PubMed]
- Khan, D.H.; Bashir, S.; Khan, M.I.; Figueiredo, P.; Santos, H.A.; Peltonen, L. Formulation optimization and in vitro characterization of rifampicin and ceftriaxone dual drug loaded niosomes with high energy probe sonication technique. J. Drug Deliv. Sci. Technol. 2020, 58, 101763. [Google Scholar] [CrossRef]
- Barani, M.; Sargazi, S.; Hajinezhad, M.R.; Rahdar, A.; Sabir, F.; Pardakhty, A.; Zargari, F.; Anwer, M.K.; Aboudzadeh, M.A. Preparation of pH-responsive vesicular deferasirox: Evidence from in silico, in vitro, and in vivo evaluations. ACS Omega 2021, 6, 24218–24232. [Google Scholar] [CrossRef] [PubMed]
- Barani, M.; Hajinezhad, M.R.; Sargazi, S.; Rahdar, A.; Shahraki, S.; Lohrasbi-Nejad, A.; Baino, F. In vitro and in vivo anticancer effect of pH-responsive paclitaxel-loaded niosomes. J. Mater. Sci.-Mater. Med. 2021, 32, 147. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhong, J.; Dong, D.; Liu, G.; Yang, P. Endoplasmic Reticulum Stress-Induced CHOP Inhibits PGC-1alpha and Causes Mitochondrial Dysfunction in Diabetic Embryopathy. Toxicol. Sci. 2017, 158, 275–285. [Google Scholar] [CrossRef] [Green Version]
- Song, J.; Zhang, Q.; Wang, S.; Yang, F.; Chen, Z.; Dong, Q.; Ji, Q.; Yuan, X.; Ren, D. Cleavage of caspase-12 at Asp94, mediated by endoplasmic reticulum stress (ERS), contributes to stretch-induced apoptosis of myoblasts. J. Cell Physiol. 2018, 233, 9473–9487. [Google Scholar] [CrossRef]
- Cornelis, R.; Hahne, S.; Taddeo, A.; Petkau, G.; Malko, D.; Durek, P.; Thiem, M.; Heiberger, L.; Peter, L.; Mohr, E.; et al. Stromal Cell-Contact Dependent PI3K and APRIL Induced NF-kappaB Signaling Prevent Mitochondrial- and ER Stress Induced Death of Memory Plasma Cells. Cell Rep. 2020, 32, 107982. [Google Scholar] [CrossRef]
- Rubiolo, J.A.; Lence, E.; Gonzalez-Bello, C.; Roel, M.; Gil-Longo, J.; Campos-Toimil, M.; Ternon, E.; Thomas, O.P.; Gonzalez-Cantalapiedra, A.; Lopez-Alonso, H.; et al. Crambescin C1 Acts as A Possible Substrate of iNOS and eNOS Increasing Nitric Oxide Production and Inducing In Vivo Hypotensive Effect. Front. Pharm. 2021, 12, 694639. [Google Scholar] [CrossRef] [PubMed]
- Danilov, A.I.; Andersson, M.; Bavand, N.; Wiklund, N.P.; Olsson, T.; Brundin, L. Nitric oxide metabolite determinations reveal continuous inflammation in multiple sclerosis. J. Neuroimmunol. 2003, 136, 112–118. [Google Scholar] [CrossRef]
- Stornaiuolo, M.; Lotti, L.V.; Borgese, N.; Torrisi, M.R.; Mottola, G.; Martire, G.; Bonatti, S. KDEL and KKXX retrieval signals appended to the same reporter protein determine different trafficking between endoplasmic reticulum, intermediate compartment, and Golgi complex. Mol. Biol. Cell 2003, 14, 889–902. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fuchs, Y.; Steller, H. Programmed cell death in animal development and disease. Cell 2011, 147, 742–758. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, D.; Palam, L.R.; Jiang, L.; Narasimhan, J.; Staschke, K.A.; Wek, R.C. Phosphorylation of eIF2 directs ATF5 translational control in response to diverse stress conditions. J. Biol. Chem. 2008, 283, 7064–7073. [Google Scholar] [CrossRef] [Green Version]
- Schroder, M. Endoplasmic reticulum stress responses. Cell Mol. Life Sci. 2008, 65, 862–894. [Google Scholar] [CrossRef]
- Kim, K.W.; Moretti, L.; Mitchell, L.R.; Jung, D.K.; Lu, B. Endoplasmic reticulum stress mediates radiation-induced autophagy by perk-eIF2alpha in caspase-3/7-deficient cells. Oncogene 2010, 29, 3241–3251. [Google Scholar] [CrossRef] [Green Version]
- Chan, S.W.; Egan, P.A. Hepatitis C virus envelope proteins regulate CHOP via induction of the unfolded protein response. FASEB J. 2005, 19, 1510–1512. [Google Scholar] [CrossRef] [Green Version]
- Pan, M.Y.; Shen, Y.C.; Lu, C.H.; Yang, S.Y.; Ho, T.F.; Peng, Y.T.; Chang, C.C. Prodigiosin activates endoplasmic reticulum stress cell death pathway in human breast carcinoma cell lines. Toxicol. Appl. Pharm. 2012, 265, 325–334. [Google Scholar] [CrossRef]
- Zhao, Y.; Tian, T.; Huang, T.; Nakajima, S.; Saito, Y.; Takahashi, S.; Yao, J.; Paton, A.W.; Paton, J.C.; Kitamura, M. Subtilase cytotoxin activates MAP kinases through PERK and IRE1 branches of the unfolded protein response. Toxicol. Sci. 2011, 120, 79–86. [Google Scholar] [CrossRef] [Green Version]
- Morinaga, N.; Yahiro, K.; Matsuura, G.; Moss, J.; Noda, M. Subtilase cytotoxin, produced by Shiga-toxigenic Escherichia coli, transiently inhibits protein synthesis of Vero cells via degradation of BiP and induces cell cycle arrest at G1 by downregulation of cyclin D1. Cell Microbiol. 2008, 10, 921–929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsuura, G.; Morinaga, N.; Yahiro, K.; Komine, R.; Moss, J.; Yoshida, H.; Noda, M. Novel subtilase cytotoxin produced by Shiga-toxigenic Escherichia coli induces apoptosis in vero cells via mitochondrial membrane damage. Infect. Immun. 2009, 77, 2919–2924. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Size (nm) | Polydispersity Index | Zeta Potential (mV) | |
|---|---|---|---|
| PLGA NPs | 260.7 ± 14.7 | 0.215 ± 0.012 | −32.8 ± 0.32 |
| WT-PLGA NPs | 303.4 ± 4.9 | 0.367 ± 0.030 | 7.09 ± 1.32 |
| A-PLGA NPs | 302.5 ± 5.6 | 0.355 ±0.008 | 8.89 ± 0.73 |
| S35A-PLGA NPs | 302.7 ± 2.3 | 0.362 ±0.035 | 3.19 ± 0.15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harada, A.; Tsutsuki, H.; Zhang, T.; Yahiro, K.; Sawa, T.; Niidome, T. Controlled Delivery of an Anti-Inflammatory Toxin to Macrophages by Mutagenesis and Nanoparticle Modification. Nanomaterials 2022, 12, 2161. https://doi.org/10.3390/nano12132161
Harada A, Tsutsuki H, Zhang T, Yahiro K, Sawa T, Niidome T. Controlled Delivery of an Anti-Inflammatory Toxin to Macrophages by Mutagenesis and Nanoparticle Modification. Nanomaterials. 2022; 12(13):2161. https://doi.org/10.3390/nano12132161
Chicago/Turabian StyleHarada, Ayaka, Hiroyasu Tsutsuki, Tianli Zhang, Kinnosuke Yahiro, Tomohiro Sawa, and Takuro Niidome. 2022. "Controlled Delivery of an Anti-Inflammatory Toxin to Macrophages by Mutagenesis and Nanoparticle Modification" Nanomaterials 12, no. 13: 2161. https://doi.org/10.3390/nano12132161
APA StyleHarada, A., Tsutsuki, H., Zhang, T., Yahiro, K., Sawa, T., & Niidome, T. (2022). Controlled Delivery of an Anti-Inflammatory Toxin to Macrophages by Mutagenesis and Nanoparticle Modification. Nanomaterials, 12(13), 2161. https://doi.org/10.3390/nano12132161