A Comprehensive Review of Natural Flavonoids with Anti-SARS-CoV-2 Activity
Abstract
1. Introduction
2. Methods
3. Pathogenesis of SARS-CoV-2
4. Classification, Synthesis and Activity of Flavonoids
4.1. Structure and Classification of Flavonoids
4.2. Chemical Synthesis of Flavonoids
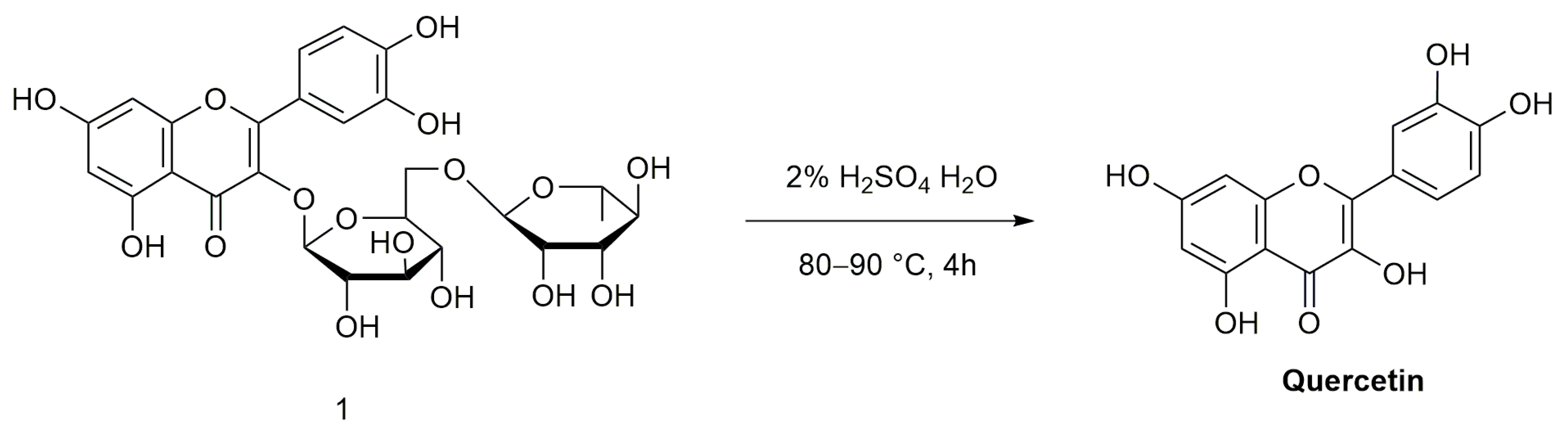
4.2.1. Quercetin
4.2.2. Baicalein and Baicalin
4.2.3. EGCG
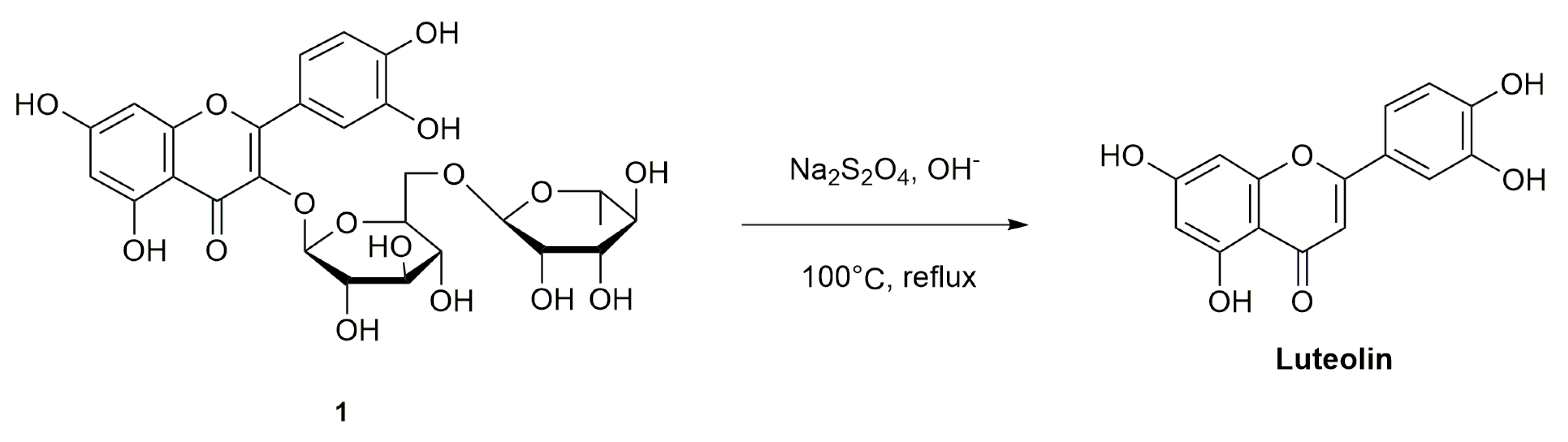
4.2.4. Luteolin
4.3. Pharmacological Activity of Flavonoid Compounds
4.3.1. Anti-Inflammatory Effect
4.3.2. Antiviral Effect
4.3.3. Antidiabetic Effect
4.3.4. Anticancer Effect
5. Anti-SARS-CoV-2 Activity of Flavonoids
5.1. Anti-SARS-CoV-2 Pharmacological Effects of Quercetin
5.2. Anti-SARS-CoV-2 Pharmacological Effects of Baicalein and Baicalin
5.3. Anti-SARS-CoV-2 Pharmacological Action of EGCG
5.4. Anti-SARS-CoV-2 Pharmacological Action of Luteolin
5.5. Other Flavonoids with Anti-SARS-CoV-2 Activity
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Available online: https://covid19.who.int/table (accessed on 30 November 2022).
- Malik, Y.S.; Sircar, S.; Bhat, S.; Sharun, K.; Dhama, K.; Dadar, M.; Tiwari, R.; Chaicumpa, W. Emerging novel coronavirus (2019-nCoV)-current scenario, evolutionary perspective based on genome analysis and recent developments. Vet. Q. 2020, 40, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Bodnar, B.H.; Meng, F.; Khan, A.I.; Wang, X.; Saribas, S.; Wang, T.; Lohani, S.C.; Wang, P.; Wei, Z.; et al. Epigallocatechin gallate from green tea effectively blocks infection of SARS-CoV-2 and new variants by inhibiting spike binding to ACE2 receptor. Cell Biosci. 2021, 11, 168. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Yin, W.; Zhang, Y.; Shang, W.; Wang, Z.; Luan, X.; Tian, G.; Aisa, H.A.; Xu, Y.; Xiao, G.; et al. Design and development of an oral remdesivir derivative VV116 against SARS-CoV-2. Cell Res. 2021, 31, 1212–1214. [Google Scholar] [CrossRef] [PubMed]
- Wu, R.; Wang, L.; Kuo, H.D.; Shannar, A.; Peter, R.; Chosu, P.J.; Li, S.; Hudlikar, R.; Liu, X.; Liu, Z.; et al. An Update on Current Therapeutic Drugs Treating COVID-19. Curr. Pharm. Rep. 2020, 6, 56–70. [Google Scholar] [CrossRef]
- Xu, J.; Zhao, S.; Teng, T.; Abdalla, A.E.; Zhu, W.; Xie, L.; Wang, Y.; Guo, X. Systematic Comparison of Two Animal-to-Human Transmitted Human Coronaviruses: SARS-CoV-2 and SARS-CoV. Viruses 2020, 12, 244. [Google Scholar] [CrossRef]
- Grifoni, A.; Sidney, J.; Zhang, Y.; Scheuermann, R.H.; Peters, B.; Sette, A. A Sequence Homology and Bioinformatic Approach Can Predict Candidate Targets for Immune Responses to SARS-CoV-2. Cell Host Microbe 2020, 27, 671–680.e672. [Google Scholar] [CrossRef]
- Nasreen, S.; Chung, H.; He, S.; Brown, K.A.; Gubbay, J.B.; Buchan, S.A.; Fell, D.B.; Austin, P.C.; Schwartz, K.L.; Sundaram, M.E.; et al. Effectiveness of COVID-19 vaccines against symptomatic SARS-CoV-2 infection and severe outcomes with variants of concern in Ontario. Nat. Microbiol. 2022, 7, 379–385. [Google Scholar] [CrossRef]
- Del Rio, C.; Omer, S.B.; Malani, P.N. Winter of Omicron-The Evolving COVID-19 Pandemic. J. Am. Med. Assoc. 2022, 327, 319–320. [Google Scholar] [CrossRef]
- Scott, L.; Hsiao, N.Y.; Moyo, S.; Singh, L.; Tegally, H.; Dor, G.; Maes, P.; Pybus, O.G.; Kraemer, M.U.G.; Semenova, E.; et al. Track Omicron’s spread with molecular data. Science 2021, 374, 1454–1455. [Google Scholar] [CrossRef]
- Sharma, V.; Rai, H.; Gautam, D.N.S.; Prajapati, P.K.; Sharma, R. Emerging evidence on Omicron (B.1.1.529) SARS-CoV-2 variant. J. Med. Virol. 2022, 94, 1876–1885. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, Y.; Chen, Y.; Qin, Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J. Med. Virol. 2020, 92, 568–576. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. J. Am. Med. Assoc. 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Mutiawati, E.; Fahriani, M.; Mamada, S.S.; Fajar, J.K.; Frediansyah, A.; Maliga, H.A.; Ilmawan, M.; Emran, T.B.; Ophinni, Y.; Ichsan, I.; et al. Anosmia and dysgeusia in SARS-CoV-2 infection: Incidence and effects on COVID-19 severity and mortality, and the possible pathobiology mechanisms—A systematic review and meta-analysis. F1000Research 2021, 10, 40. [Google Scholar] [CrossRef] [PubMed]
- Garnier-Crussard, A.; Forestier, E.; Gilbert, T.; Krolak-Salmon, P. Novel Coronavirus (COVID-19) Epidemic: What Are the Risks for Older Patients? J. Am. Geriatr. Soc. 2020, 68, 939–940. [Google Scholar] [CrossRef]
- Cook, T.M. The importance of hypertension as a risk factor for severe illness and mortality in COVID-19. Anaesthesia 2020, 75, 976–977. [Google Scholar] [CrossRef]
- Kashyap, P.; Thakur, M.; Singh, N.; Shikha, D.; Kumar, S.; Baniwal, P.; Yadav, Y.S.; Sharma, M.; Sridhar, K.; Inbaraj, B.S. In Silico Evaluation of Natural Flavonoids as a Potential Inhibitor of Coronavirus Disease. Molecules 2022, 27, 6374. [Google Scholar] [CrossRef]
- Drożdżal, S.; Rosik, J.; Lechowicz, K.; Machaj, F.; Szostak, B.; Przybyciński, J.; Lorzadeh, S.; Kotfis, K.; Ghavami, S.; Łos, M.J. An update on drugs with therapeutic potential for SARS-CoV-2 (COVID-19) treatment. Drug Resist. Updat. Rev. Comment. Antimicrob. Anticancer Chemother. 2021, 59, 100794. [Google Scholar] [CrossRef] [PubMed]
- Imran, M.; Kumar Arora, M.; Asdaq, S.M.B.; Khan, S.A.; Alaqel, S.I.; Alshammari, M.K.; Alshehri, M.M.; Alshrari, A.S.; Mateq Ali, A.; Al-Shammeri, A.M.; et al. Discovery, Development, and Patent Trends on Molnupiravir: A Prospective Oral Treatment for COVID-19. Molecules 2021, 26, 5795. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.Z.; Ai, J.W.; Lin, N.; Zhang, H.C.; Li, Y.; Wang, H.Y.; Wang, S.; Wang, Z.; Li, T.; Sun, F.; et al. An open, prospective cohort study of VV116 in Chinese participants infected with SARS-CoV-2 omicron variants. Emerg. Microbes Infect. 2022, 11, 1518–1523. [Google Scholar] [CrossRef]
- Alzaabi, M.M.; Hamdy, R.; Ashmawy, N.S.; Hamoda, A.M.; Alkhayat, F.; Khademi, N.N.; Al Joud, S.M.A.; El-Keblawy, A.A.; Soliman, S.S.M. Flavonoids are promising safe therapy against COVID-19. Phytochem. Rev. 2022, 21, 291–312. [Google Scholar] [CrossRef]
- Sharma, R.; Martins, N.; Chaudhary, A.; Garg, N.; Sharma, V.; Kuca, K.; Nepovimova, E.; Tuli, H.S.; Bishayee, A.; Chaudhary, A.; et al. Adjunct use of honey in diabetes mellitus: A consensus or conundrum? Trends Food Sci. Technol. 2020, 106, 254–274. [Google Scholar] [CrossRef]
- Mangiavacchi, F.; Botwina, P.; Menichetti, E.; Bagnoli, L.; Rosati, O.; Marini, F.; Fonseca, S.F.; Abenante, L.; Alves, D.; Dabrowska, A.; et al. Seleno-Functionalization of Quercetin Improves the Non-Covalent Inhibition of M(pro) and Its Antiviral Activity in Cells against SARS-CoV-2. Int. J. Mol. Sci. 2021, 22, 7048. [Google Scholar] [CrossRef]
- Su, H.X.; Yao, S.; Zhao, W.F.; Li, M.J.; Liu, J.; Shang, W.J.; Xie, H.; Ke, C.Q.; Gao, M.; Yu, K.Q.; et al. Discovery of baicalin and baicalein as novel, natural product inhibitors of SARS-CoV-2 3CL protease in vitro. bioRxiv 2020. [Google Scholar] [CrossRef]
- Munafo, F.; Donati, E.; Brindani, N.; Ottonello, G.; Armirotti, A.; De Vivo, M. Quercetin and luteolin are single-digit micromolar inhibitors of the SARS-CoV-2 RNA-dependent RNA polymerase. Sci. Rep. 2022, 12, 10571. [Google Scholar] [CrossRef] [PubMed]
- Zhan, Y.; Ta, W.; Tang, W.; Hua, R.; Wang, J.; Wang, C.; Lu, W. Potential antiviral activity of isorhamnetin against SARS-CoV-2 spike pseudotyped virus in vitro. Drug Dev. Res. 2021, 82, 1124–1130. [Google Scholar] [CrossRef]
- Khan, A.; Heng, W.; Wang, Y.; Qiu, J.; Wei, X.; Peng, S.; Saleem, S.; Khan, M.; Ali, S.S.; Wei, D.Q. In silico and in vitro evaluation of kaempferol as a potential inhibitor of the SARS-CoV-2 main protease (3CLpro). Phytother. Res. PTR 2021, 35, 2841–2845. [Google Scholar] [CrossRef]
- Cheng, F.J.; Huynh, T.K.; Yang, C.S.; Hu, D.W.; Shen, Y.C.; Tu, C.Y.; Wu, Y.C.; Tang, C.H.; Huang, W.C.; Chen, Y.; et al. Hesperidin Is a Potential Inhibitor against SARS-CoV-2 Infection. Nutrients 2021, 13, 2800. [Google Scholar] [CrossRef]
- Xiu, S.; Dick, A.; Ju, H.; Mirzaie, S.; Abdi, F.; Cocklin, S.; Zhan, P.; Liu, X. Inhibitors of SARS-CoV-2 Entry: Current and Future Opportunities. J. Med. Chem. 2020, 63, 12256–12274. [Google Scholar] [CrossRef]
- Krishnamoorthy, S.; Swain, B.; Verma, R.S.; Gunthe, S.S. SARS-CoV, MERS-CoV, and 2019-nCoV viruses: An overview of origin, evolution, and genetic variations. Virusdisease 2020, 31, 411–423. [Google Scholar] [CrossRef]
- Boopathi, S.; Poma, A.B.; Kolandaivel, P. Novel 2019 coronavirus structure, mechanism of action, antiviral drug promises and rule out against its treatment. J. Biomol. Struct. Dyn. 2021, 39, 3409–3418. [Google Scholar] [CrossRef]
- Huang, Y.; Yang, C.; Xu, X.F.; Xu, W.; Liu, S.W. Structural and functional properties of SARS-CoV-2 spike protein: Potential antivirus drug development for COVID-19. Acta Pharmacol. Sin. 2020, 41, 1141–1149. [Google Scholar] [CrossRef]
- Xia, S.; Zhu, Y.; Liu, M.; Lan, Q.; Xu, W.; Wu, Y.; Ying, T.; Liu, S.; Shi, Z.; Jiang, S.; et al. Fusion mechanism of 2019-nCoV and fusion inhibitors targeting HR1 domain in spike protein. Cell. Mol. Immunol. 2020, 17, 765–767. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, A.C.; Mohsin, I. The SARS-CoV-2 Spike Glycoprotein as a Drug and Vaccine Target: Structural Insights into Its Complexes with ACE2 and Antibodies. Cells 2020, 9, 2343. [Google Scholar] [CrossRef]
- Tang, T.; Bidon, M.; Jaimes, J.A.; Whittaker, G.R.; Daniel, S. Coronavirus membrane fusion mechanism offers a potential target for antiviral development. Antivir. Res. 2020, 178, 104792. [Google Scholar] [CrossRef] [PubMed]
- Ruan, Z.; Liu, C.; Guo, Y.; He, Z.; Huang, X.; Jia, X.; Yang, T. SARS-CoV-2 and SARS-CoV: Virtual screening of potential inhibitors targeting RNA-dependent RNA polymerase activity (NSP12). J. Med. Virol. 2021, 93, 389–400. [Google Scholar] [CrossRef]
- Gil, C.; Ginex, T.; Maestro, I.; Nozal, V.; Barrado-Gil, L.; Cuesta-Geijo, M.; Urquiza, J.; Ramírez, D.; Alonso, C.; Campillo, N.E.; et al. COVID-19: Drug Targets and Potential Treatments. J. Med. Chem. 2020, 63, 12359–12386. [Google Scholar] [CrossRef] [PubMed]
- Zheng, L.; Zhang, L.; Huang, J.; Nandakumar, K.S.; Liu, S.; Cheng, K. Potential treatment methods targeting 2019-nCoV infection. Eur. J. Med. Chem. 2020, 205, 112687. [Google Scholar] [CrossRef]
- Wang, Y.; Grunewald, M.; Perlman, S. Coronaviruses: An Updated Overview of Their Replication and Pathogenesis. Methods Mol. Biol. 2020, 2203, 1–29. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, N.; Nair, D.T. Vitamin B12 may inhibit RNA-dependent-RNA polymerase activity of nsp12 from the SARS-CoV-2 virus. IUBMB Life 2020, 72, 2112–2120. [Google Scholar] [CrossRef]
- Alnefaie, A.; Albogami, S. Current approaches used in treating COVID-19 from a molecular mechanisms and immune response perspective. Saudi Pharm. J. 2020, 28, 1333–1352. [Google Scholar] [CrossRef]
- Chen, Y.; Liu, Q.; Guo, D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J. Med. Virol. 2020, 92, 418–423. [Google Scholar] [CrossRef]
- Llivisaca-Contreras, S.A.; Naranjo-Morán, J.; Pino-Acosta, A.; Pieters, L.; Vanden Berghe, W.; Manzano, P.; Vargas-Pérez, J.; León-Tamariz, F.; Cevallos-Cevallos, J.M. Plants and Natural Products with Activity against Various Types of Coronaviruses: A Review with Focus on SARS-CoV-2. Molecules 2021, 26, 4099. [Google Scholar] [CrossRef]
- Brodowska, K. Natural flavonoids: Classification, potential role, and application of flavonoid analogues. Eur. J. Biol. Res. 2017, 7, 108–123. [Google Scholar]
- Middleton, E.J. Effect of plant flavonoids on immune and inflammatory cell function. Adv. Exp. Med. Biol. 1998, 439, 175–182. [Google Scholar] [CrossRef]
- Naghski, J.; Krewson, C.F. The preparation and analysis of quercetin. J. Am. Pharm. Association. Am. Pharm. Assoc. 1953, 42, 66–68. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.Z.; Yang, J.; Yang, B.; Wu, Y.S.; Wu, T. Total synthesis of baicalein. J. Asian Nat. Prod. Res. 2010, 12, 124–128. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.F.; Yu, B.; Sun, J.S.; Wang, R.X. Efficient synthesis of baicalin and its analogs. Tetrahedron Lett. 2015, 56, 3816–3819. [Google Scholar] [CrossRef]
- Tanaka, H.; Chino, A.; Takahashi, T. Reagent-controlled stereoselective synthesis of (±)-gallo- and (±)-epigallo-catechin gallates. Tetrahedron Lett. 2012, 53, 2493–2495. [Google Scholar] [CrossRef]
- Sun, W.L.; Yang, J.W.; Dou, H.Y.; Li, G.Q.; Li, X.Y.; Shen, L.; Ji, H.F. Anti-inflammatory effect of luteolin is related to the changes in the gut microbiota and contributes to preventing the progression from simple steatosis to nonalcoholic steatohepatitis. Bioorganic Chem. 2021, 112, 104966. [Google Scholar] [CrossRef]
- Wu, F.; Zhao, S.; Yu, B.; Chen, Y.M.; Wang, W.; Song, Z.G.; Hu, Y.; Tao, Z.W.; Tian, J.H.; Pei, Y.Y.; et al. A new coronavirus associated with human respiratory disease in China. Nature 2020, 579, 265–269. [Google Scholar] [CrossRef]
- Wang, J.; Li, Q.; Qiu, Y.W.; Lu, H.L. COVID-19: Imbalanced cell-mediated immune response drives to immunopathology. Emerg. Microbes Infect. 2022, 11, 2393–2404. [Google Scholar] [CrossRef]
- Maleki, S.J.; Crespo, J.F.; Cabanillas, B. Anti-inflammatory effects of flavonoids. Food Chem. 2019, 299, 125124. [Google Scholar] [CrossRef] [PubMed]
- Hou, D.D.; Zhang, W.; Gao, Y.L.; Sun, Y.Z.; Wang, H.X.; Qi, R.Q.; Chen, H.D.; Gao, X.H. Anti-inflammatory effects of quercetin in a mouse model of MC903-induced atopic dermatitis. Int. Immunopharmacol. 2019, 74, 105676. [Google Scholar] [CrossRef] [PubMed]
- Hannan, A.; Akhtar, B.; Sharif, A.; Anjum, F.; Pasha, I.; Khan, A.; Akhtar, M.F.; Saleem, A. Quercetin-loaded chitosan nanoparticles ameliorate adjuvant-induced arthritis in rats by regulating anti-oxidant enzymes and downregulating pro- and inflammatory cytokines. Inflammopharmacology 2022, 31, 287–300. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Ling, L.; Zhu, W.; Ying, T.; Yu, T.; Sun, M.; Zhu, X.; Du, Y.; Zhang, L. M1/M2 re-polarization of kaempferol biomimetic NPs in anti-inflammatory therapy of atherosclerosis. J. Control. Release Off. J. Control. Release Soc. 2023, 353, 1068–1083. [Google Scholar] [CrossRef]
- Torres-Villarreal, D.; Camacho, A.; Castro, H.; Ortiz-Lopez, R.; de la Garza, A.L. Anti-obesity effects of kaempferol by inhibiting adipogenesis and increasing lipolysis in 3T3-L1 cells. J. Physiol. Biochem. 2019, 75, 83–88. [Google Scholar] [CrossRef]
- Gao, J.F.; Tang, L.; Luo, F.; Chen, L.; Zhang, Y.Y.; Ding, H. Myricetin treatment has ameliorative effects in DNFB-induced atopic dermatitis mice under high-fat conditions. Toxicol. Sci. Off. J. Soc. Toxicol. 2022, 191, 308–320. [Google Scholar] [CrossRef]
- Sur, B.; Lee, B. Myricetin prevents sleep deprivation-induced cognitive impairment and neuroinflammation in rat brain via regulation of brain-derived neurotropic factor. Korean J. Physiol. Pharmacol. Off. J. Korean Physiol. Soc. Korean Soc. Pharmacol. 2022, 26, 415–425. [Google Scholar] [CrossRef]
- Wohlert, A.; Palkovicsné Pézsa, N.; Móritz, A.V.; Jerzsele, Á.; Farkas, O.; Pászti-Gere, E. Luteolin and Chrysin Could Prevent E. coli Lipopolysaccharide-Ochratoxin A Combination-Caused Inflammation and Oxidative Stress in In Vitro Porcine Intestinal Model. Anim. Open Access J. MDPI 2022, 12, 2747. [Google Scholar] [CrossRef]
- Wang, Y.L.; Gao, J.M.; Xing, L.Z. Therapeutic potential of Oroxylin A in rheumatoid arthritis. Int. Immunopharmacol. 2016, 40, 294–299. [Google Scholar] [CrossRef] [PubMed]
- Kwon, K.H.; Murakami, A.; Tanaka, T.; Ohigashi, H. Dietary rutin, but not its aglycone quercetin, ameliorates dextran sulfate sodium-induced experimental colitis in mice: Attenuation of pro-inflammatory gene expression. Biochem. Pharmacol. 2005, 69, 395–406. [Google Scholar] [CrossRef] [PubMed]
- Saeedi-Boroujeni, A.; Mahmoudian-Sani, M.R. Anti-inflammatory potential of Quercetin in COVID-19 treatment. J. Inflamm. 2021, 18, 3. [Google Scholar] [CrossRef] [PubMed]
- Badshah, S.L.; Faisal, S.; Muhammad, A.; Poulson, B.G.; Emwas, A.H.; Jaremko, M. Antiviral activities of flavonoids. Biomed. Pharmacother. 2021, 140, 111596. [Google Scholar] [CrossRef]
- Sithisarn, P.; Michaelis, M.; Schubert-Zsilavecz, M.; Cinatl, J.J. Differential antiviral and anti-inflammatory mechanisms of the flavonoids biochanin A and baicalein in H5N1 influenza A virus-infected cells. Antivir. Res. 2013, 97, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Michaelis, M.; Sithisarn, P.; Cinatl, J.J. Effects of flavonoid-induced oxidative stress on anti-H5N1 influenza a virus activity exerted by baicalein and biochanin A. BMC Res. Notes 2014, 7, 384. [Google Scholar] [CrossRef]
- Lin, Y.J.; Chang, Y.C.; Hsiao, N.W.; Hsieh, J.L.; Wang, C.Y.; Kung, S.H.; Tsai, F.J.; Lan, Y.C.; Lin, C.W. Fisetin and rutin as 3C protease inhibitors of enterovirus A71. J. Virol. Methods 2012, 182, 93–98. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.Q.; Zhang, D.J.; Ge, M.; Li, Z.R.; Jiang, J.D.; Li, Y.H. Formononetin inhibits enterovirus 71 replication by regulating COX-2/PGE2 expression. Virol. J. 2015, 12, 35. [Google Scholar] [CrossRef]
- Polyak, S.J.; Oberlies, N.H.; Pécheur, E.I.; Dahari, H.; Ferenci, P.; Pawlotsky, J.M. Silymarin for HCV infection. Antivir. Ther. 2013, 18, 141–147. [Google Scholar] [CrossRef]
- Low, Z.X.; OuYong, B.M.; Hassandarvish, P.; Poh, C.L.; Ramanathan, B. Antiviral activity of silymarin and baicalein against dengue virus. Sci. Rep. 2021, 11, 21221. [Google Scholar] [CrossRef]
- Ortega, J.T.; Serrano, M.L.; Suárez, A.I.; Baptista, J.; Pujol, F.H.; Cavallaro, L.V.; Campos, H.R.; Rangel, H.R. Antiviral activity of flavonoids present in aerial parts of Marcetia taxifolia against Hepatitis B virus, Poliovirus, and Herpes Simplex Virus in vitro. EXCLI J. 2019, 18, 1037–1048. [Google Scholar] [CrossRef]
- Guo, H.; Wan, X.H.; Niu, F.J.; Sun, J.J.; Shi, C.X.; Meng, Y.; Zhou, C.Z. Evaluation of antiviral effect and toxicity of total flavonoids extracted from Robinia pseudoacacia cv. idaho. Biomed. Pharmacother. 2019, 118, 109335. [Google Scholar] [CrossRef] [PubMed]
- Zandi, K.; Musall, K.; Oo, A.; Cao, D.; Liang, B.; Hassandarvish, P.; Lan, S.; Slack, R.L.; Kirby, K.A.; Bassit, L.; et al. Baicalein and Baicalin Inhibit SARS-CoV-2 RNA-Dependent-RNA Polymerase. Microorganisms 2021, 9, 893. [Google Scholar] [CrossRef] [PubMed]
- Henss, L.; Auste, A.; Schürmann, C.; Schmidt, C.; von Rhein, C.; Mühlebach, M.D.; Schnierle, B.S. The green tea catechin epigallocatechin gallate inhibits SARS-CoV-2 infection. J. Gen. Virol. 2021, 102, 1574. [Google Scholar] [CrossRef]
- Ohishi, T.; Hishiki, T.; Baig, M.S.; Rajpoot, S.; Saqib, U.; Takasaki, T.; Hara, Y. Epigallocatechin gallate (EGCG) attenuates severe acute respiratory coronavirus disease 2 (SARS-CoV-2) infection by blocking the interaction of SARS-CoV-2 spike protein receptor-binding domain to human angiotensin-converting enzyme 2. PLoS ONE 2022, 17, e0271112. [Google Scholar] [CrossRef] [PubMed]
- Al-Ishaq, R.K.; Abotaleb, M.; Kubatka, P.; Kajo, K.; Büsselberg, D. Flavonoids and Their Anti-Diabetic Effects: Cellular Mechanisms and Effects to Improve Blood Sugar Levels. Biomolecules 2019, 9, 430. [Google Scholar] [CrossRef]
- El-Ouady, F.; Bachir, F.; Eddouks, M. Flavonoids Extracted from Asteriscus graveolens Improve Glucose Metabolism and Lipid Profile in Diabetic Rats. Endocr. Metab. Immune Disord. Drug Targets 2021, 21, 895–904. [Google Scholar] [CrossRef] [PubMed]
- Sapian, S.; Taib, I.S.; Latip, J.; Katas, H.; Chin, K.Y.; Mohd Nor, N.A.; Jubaidi, F.F.; Budin, S.B. Therapeutic Approach of Flavonoid in Ameliorating Diabetic Cardiomyopathy by Targeting Mitochondrial-Induced Oxidative Stress. Int. J. Mol. Sci. 2021, 22, 11616. [Google Scholar] [CrossRef]
- Liu, H.; Guan, H.; Tan, X.; Jiang, Y.; Li, F.; Sun-Waterhouse, D.; Li, D. Enhanced alleviation of insulin resistance via the IRS-1/Akt/FOXO1 pathway by combining quercetin and EGCG and involving miR-27a-3p and miR-96-5p. Free Radic. Biol. Med. 2022, 181, 105–117. [Google Scholar] [CrossRef]
- Gui, L.; Wang, F.; Hu, X.; Liu, X.; Yang, H.; Cai, Z.; Qi, M.; Dai, C. Epigallocatechin Gallate Protects Diabetes Mellitus Rats Complicated with Cardiomyopathy through TGF-β1/JNK Signaling Pathway. Curr. Pharm. Des. 2022, 28, 2758–2770. [Google Scholar] [CrossRef] [PubMed]
- Meena, K.P.; Vijayakumar, M.R.; Dwibedy, P.S. Catechin-loaded Eudragit microparticles for the management of diabetes: Formulation, characterization and in vivo evaluation of antidiabetic efficacy. J. Microencapsul. 2017, 34, 342–350. [Google Scholar] [CrossRef]
- Ragheb, S.R.; El Wakeel, L.M.; Nasr, M.S.; Sabri, N.A. Impact of Rutin and Vitamin C combination on oxidative stress and glycemic control in patients with type 2 diabetes. Clin. Nutr. ESPEN 2020, 35, 128–135. [Google Scholar] [CrossRef]
- Tian, R.F.; Yang, W.Q.; Xue, Q.; Gao, L.; Huo, J.L.; Ren, D.Q.; Chen, X.Y. Rutin ameliorates diabetic neuropathy by lowering plasma glucose and decreasing oxidative stress via Nrf2 signaling pathway in rats. Eur. J. Pharmacol. 2016, 771, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Orhan, N.; Aslan, M.; Sukuroglu, M.; Deliorman Orhan, D. In vivo and in vitro antidiabetic effect of Cistus laurifolius L. and detection of major phenolic compounds by UPLC-TOF-MS analysis. J. Ethnopharmacol. 2013, 146, 859–865. [Google Scholar] [CrossRef] [PubMed]
- Cui, K.; Zhang, S.B.; Jiang, X.; Xie, W.D. Novel synergic antidiabetic effects of Astragalus polysaccharides combined with Crataegus flavonoids via improvement of islet function and liver metabolism. Mol. Med. Rep. 2016, 13, 4737–4744. [Google Scholar] [CrossRef]
- Grivas, P.; Khaki, A.R.; Wise-Draper, T.M.; French, B.; Hennessy, C.; Hsu, C.Y.; Shyr, Y.; Li, X.; Choueiri, T.K.; Painter, C.A.; et al. Association of clinical factors and recent anticancer therapy with COVID-19 severity among patients with cancer: A report from the COVID-19 and Cancer Consortium. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2021, 32, 787–800. [Google Scholar] [CrossRef] [PubMed]
- Yang, N.; Jia, X.B.; Zhang, Z.H.; Sun, E.; Yan, H.M. Advance in studies on anti-cancer activity and mechanism of flavonoids. China J. Chin. Mater. Med. 2015, 40, 373–381. [Google Scholar]
- Ravishankar, D.; Rajora, A.K.; Greco, F.; Osborn, H.M. Flavonoids as prospective compounds for anti-cancer therapy. Int. J. Biochem. Cell Biol. 2013, 45, 2821–2831. [Google Scholar] [CrossRef]
- Palko-Labuz, A.; Sroda-Pomianek, K.; Uryga, A.; Kostrzewa-Suslow, E.; Michalak, K. Anticancer activity of baicalein and luteolin studied in colorectal adenocarcinoma LoVo cells and in drug-resistant LoVo/Dx cells. Biomed. Pharmacother. 2017, 88, 232–241. [Google Scholar] [CrossRef]
- Yu, M.L.; Qi, B.Q.; Wu, X.X.; Xu, J.; Liu, X.L. Baicalein increases cisplatin sensitivity of A549 lung adenocarcinoma cells via PI3K/Akt/NF-kappaB pathway. Biomed. Pharmacother. 2017, 90, 677–685. [Google Scholar] [CrossRef]
- Yang, J.L.; Pi, C.C.; Wang, G.H. Inhibition of PI3K/Akt/mTOR pathway by apigenin induces apoptosis and autophagy in hepatocellular carcinoma cells. Biomed. Pharmacother. 2018, 103, 699–707. [Google Scholar] [CrossRef]
- Cao, Y.; Cao, W.; Qiu, Y.; Zhou, Y.; Guo, Q.; Gao, Y.; Lu, N. Oroxylin A suppresses ACTN1 expression to inactivate cancer-associated fibroblasts and restrain breast cancer metastasis. Pharm. Res 2020, 159, 104981. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.B.; Yao, Y.Y.; Zhao, K.; Huang, Y.J.; Zhou, Y.X.; Zhao, L.; Guo, Q.L.; Lu, N. Oroxylin A inhibits invasion and migration through suppressing ERK/GSK-3β signaling in snail-expressing non-small-cell lung cancer cells. Mol. Carcinog. 2016, 55, 2121–2134. [Google Scholar] [CrossRef] [PubMed]
- Yun, H.M.; Park, J.E.; Lee, J.Y.; Park, K.R. Latifolin, a Natural Flavonoid, Isolated from the Heartwood of Dalbergia odorifera Induces Bioactivities through Apoptosis, Autophagy, and Necroptosis in Human Oral Squamous Cell Carcinoma. Int. J. Mol. Sci. 2022, 23, 13629. [Google Scholar] [CrossRef]
- Zhang, L.; Xie, J.; Gan, R.; Wu, Z.; Luo, H.; Chen, X.; Lu, Y.; Wu, L.; Zheng, D. Synergistic inhibition of lung cancer cells by EGCG and NF-κB inhibitor BAY11-7082. J. Cancer 2019, 10, 6543–6556. [Google Scholar] [CrossRef]
- Polerà, N.; Badolato, M.; Perri, F.; Carullo, G.; Aiello, F. Quercetin and its Natural Sources in Wound Healing Management. Curr. Med. Chem. 2019, 26, 5825–5848. [Google Scholar] [CrossRef]
- Yi, H.; Peng, H.; Wu, X.; Xu, X.; Kuang, T.; Zhang, J.; Du, L.; Fan, G. The Therapeutic Effects and Mechanisms of Quercetin on Metabolic Diseases: Pharmacological Data and Clinical Evidence. Oxidative Med. Cell. Longev. 2021, 2021, 6678662. [Google Scholar] [CrossRef] [PubMed]
- Shen, D.; Feng, Y.; Zhang, X.; Gong, L.; Liu, J.; Li, Y.; Liao, H. Antiosteoporosis Studies of 20 Medicine Food Homology Plants Containing Quercetin, Rutin, and Kaempferol: TCM Characteristics, In Vivo and In Vitro Activities, Potential Mechanisms, and Food Functions. Evid.-Based Complement. Altern. Med. Ecam 2022, 2022, 5902293. [Google Scholar] [CrossRef]
- Costa, L.G.; Garrick, J.M.; Roquè, P.J.; Pellacani, C. Mechanisms of Neuroprotection by Quercetin: Counteracting Oxidative Stress and More. Oxidative Med. Cell. Longev. 2016, 2016, 2986796. [Google Scholar] [CrossRef]
- Swanson, K.V.; Deng, M.; Ting, J.P. The NLRP3 inflammasome: Molecular activation and regulation to therapeutics. Nat. Rev. Immunol. 2019, 19, 477–489. [Google Scholar] [CrossRef]
- Di Pierro, F.; Derosa, G.; Maffioli, P.; Bertuccioli, A.; Togni, S.; Riva, A.; Allegrini, P.; Khan, A.; Khan, S.; Khan, B.A.; et al. Possible Therapeutic Effects of Adjuvant Quercetin Supplementation Against Early-Stage COVID-19 Infection: A Prospective, Randomized, Controlled, and Open-Label Study. Int. J. Gen. Med. 2021, 14, 2359–2366. [Google Scholar] [CrossRef]
- Shohan, M.; Nashibi, R.; Mahmoudian-Sani, M.R.; Abolnezhadian, F.; Ghafourian, M.; Alavi, S.M.; Sharhani, A.; Khodadadi, A. The therapeutic efficacy of quercetin in combination with antiviral drugs in hospitalized COVID-19 patients: A randomized controlled trial. Eur. J. Pharmacol. 2022, 914, 174615. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Snyder, S.A.; Smith, J.N.; Chen, Y.C. Anticancer properties of baicalein: A review. Medicinal chemistry research: An international journal for rapid communications on design and mechanisms of action of biologically active agents. Med. Chem. Res. 2016, 25, 1515–1523. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Guan, Y.; Hu, W.; Xu, Z.; Ishfaq, M. An overview of pharmacological activities of baicalin and its aglycone baicalein: New insights into molecular mechanisms and signaling pathways. Iran. J. Basic Med. Sci. 2022, 25, 14–26. [Google Scholar] [CrossRef]
- Liu, H.; Ye, F.; Sun, Q.; Liang, H.; Li, C.; Li, S.; Lu, R.; Huang, B.; Tan, W.; Lai, L. Scutellaria baicalensis extract and baicalein inhibit replication of SARS-CoV-2 and its 3C-like protease in vitro. J. Enzym. Inhib. Med. Chem. 2021, 36, 497–503. [Google Scholar] [CrossRef]
- Mehmood, S.; Maqsood, M.; Mahtab, N.; Khan, M.I.; Sahar, A.; Zaib, S.; Gul, S. Epigallocatechin gallate: Phytochemistry, bioavailability, utilization challenges, and strategies. J. Food Biochem. 2022, 46, e14189. [Google Scholar] [CrossRef] [PubMed]
- Ohgitani, E.; Shin-Ya, M.; Ichitani, M.; Kobayashi, M.; Takihara, T.; Kawamoto, M.; Kinugasa, H.; Mazda, O. Significant Inactivation of SARS-CoV-2 In Vitro by a Green Tea Catechin, a Catechin-Derivative, and Black Tea Galloylated Theaflavins. Molecules 2021, 26, 3572. [Google Scholar] [CrossRef]
- Ohgitani, E.; Shin-Ya, M.; Ichitani, M.; Kobayashi, M.; Takihara, T.; Kawamoto, M.; Kinugasa, H.; Mazda, O. Rapid Inactivation In Vitro of SARS-CoV-2 in Saliva by Black Tea and Green Tea. Pathogens 2021, 10, 721. [Google Scholar] [CrossRef]
- Pillon, M.C.; Frazier, M.N.; Dillard, L.B.; Williams, J.G.; Kocaman, S.; Krahn, J.M.; Perera, L.; Hayne, C.K.; Gordon, J.; Stewart, Z.D.; et al. Cryo-EM structures of the SARS-CoV-2 endoribonuclease Nsp15 reveal insight into nuclease specificity and dynamics. Nat. Commun. 2021, 12, 636. [Google Scholar] [CrossRef]
- Hackbart, M.; Deng, X.; Baker, S.C. Coronavirus endoribonuclease targets viral polyuridine sequences to evade activating host sensors. Proc. Natl. Acad. Sci. USA 2020, 117, 8094–8103. [Google Scholar] [CrossRef]
- Hong, S.; Seo, S.H.; Woo, S.J.; Kwon, Y.; Song, M.; Ha, N.C. Epigallocatechin Gallate Inhibits the Uridylate-Specific Endoribonuclease Nsp15 and Efficiently Neutralizes the SARS-CoV-2 Strain. J. Agric. Food Chem. 2021, 69, 5948–5954. [Google Scholar] [CrossRef]
- Chiou, W.C.; Chen, J.C.; Chen, Y.T.; Yang, J.M.; Hwang, L.H.; Lyu, Y.S.; Yang, H.Y.; Huang, C. The inhibitory effects of PGG and EGCG against the SARS-CoV-2 3C-like protease. Biochem. Biophys. Res. Commun. 2022, 591, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Shaik, F.B.; Swarnalatha, K.; Mohan, M.C.; Thomas, A.; Chikati, R.; Sandeep, G.; Maddu, N. Novel antiviral effects of chloroquine, hydroxychloroquine, and green tea catechins against SARS CoV-2 main protease (Mpro) and 3C-like protease for COVID-19 treatment. Clin. Nutr. Open Sci. 2022, 42, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Park, R.; Jang, M.; Park, Y.I.; Park, Y.; Jung, W.; Park, J.; Park, J. Epigallocatechin Gallate (EGCG), a Green Tea Polyphenol, Reduces Coronavirus Replication in a Mouse Model. Viruses 2021, 13, 2533. [Google Scholar] [CrossRef]
- López-Lázaro, M. Distribution and biological activities of the flavonoid luteolin. Mini Rev. Med. Chem. 2009, 9, 31–59. [Google Scholar] [CrossRef] [PubMed]
- Yao, Z.H.; Yao, X.L.; Zhang, Y.; Zhang, S.F.; Hu, J.C. Luteolin Could Improve Cognitive Dysfunction by Inhibiting Neuroinflammation. Neurochem. Res. 2018, 43, 806–820. [Google Scholar] [CrossRef]
- Guo, Y.F.; Xu, N.N.; Sun, W.; Zhao, Y.; Li, C.Y.; Guo, M.Y. Luteolin reduces inflammation in Staphylococcus aureus-induced mastitis by inhibiting NF-kB activation and MMPs expression. Oncotarget 2017, 8, 28481–28493. [Google Scholar] [CrossRef]
- Xiao, Z.; Xu, H.; Qu, Z.Y.; Ma, X.Y.; Huang, B.X.; Sun, M.S.; Wang, B.Q.; Wang, G.Y. Active Ingredients of Reduning Injection Maintain High Potency against SARS-CoV-2 Variants. Chin. J. Integr. Med. 2023, 29, 205–212. [Google Scholar] [CrossRef]
- D’Ascanio, L.; Vitelli, F.; Cingolani, C.; Maranzano, M.; Brenner, M.J.; Di Stadio, A. Randomized clinical trial “olfactory dysfunction after COVID-19: Olfactory rehabilitation therapy vs. intervention treatment with Palmitoylethanolamide and Luteolin”: Preliminary results. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 4156–4162. [Google Scholar] [CrossRef]
- O’Byrne, L.; Webster, K.E.; MacKeith, S.; Philpott, C.; Hopkins, C.; Burton, M.J. Interventions for the treatment of persistent post-COVID-19 olfactory dysfunction. Cochrane Database Syst. Rev. 2022, 9, Cd013876. [Google Scholar] [CrossRef]
- Zalpoor, H.; Bakhtiyari, M.; Shapourian, H.; Rostampour, P.; Tavakol, C.; Nabi-Afjadi, M. Hesperetin as an anti-SARS-CoV-2 agent can inhibit COVID-19-associated cancer progression by suppressing intracellular signaling pathways. Inflammopharmacology 2022, 30, 1533–1539. [Google Scholar] [CrossRef]
- Dupuis, J.; Laurin, P.; Tardif, J.C.; Hausermann, L.; Rosa, C.; Guertin, M.C.; Thibaudeau, K.; Gagnon, L.; Cesari, F.; Robitaille, M.; et al. Fourteen-Day Evolution of COVID-19 Symptoms during the Third Wave in Nonvaccinated Subjects and Effects of Hesperidin Therapy: A Randomized, Double-Blinded, Placebo-Controlled Study. Evid. -Based Complement. Altern. Med. Ecam 2022, 2022, 3125662. [Google Scholar] [CrossRef]
- Tahir Ul Qamar, M.; Alqahtani, S.M.; Alamri, M.A.; Chen, L.L. Structural basis of SARS-CoV-2 3CL(pro) and anti-COVID-19 drug discovery from medicinal plants. J. Pharm. Anal. 2020, 10, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Clementi, N.; Scagnolari, C.; D’Amore, A.; Palombi, F.; Criscuolo, E.; Frasca, F.; Pierangeli, A.; Mancini, N.; Antonelli, G.; Clementi, M.; et al. Naringenin is a powerful inhibitor of SARS-CoV-2 infection in vitro. Pharmacol. Res. 2021, 163, 105255. [Google Scholar] [CrossRef]
- Feldo, M.; Wójciak-Kosior, M.; Sowa, I.; Kocki, J.; Bogucki, J.; Zubilewicz, T.; Kęsik, J.; Bogucka-Kocka, A. Effect of Diosmin Administration in Patients with Chronic Venous Disorders on Selected Factors Affecting Angiogenesis. Molecules 2019, 24, 3316. [Google Scholar] [CrossRef] [PubMed]
- Hu, X.; Qin, H.; Li, Y.; Li, J.; Fu, L.; Li, M.; Jiang, C.; Yun, J.; Liu, Z.; Feng, Y.; et al. Biochanin A protect against lipopolysaccharide-induced acute lung injury in mice by regulating TLR4/NF-κB and PPAR-γ pathway. Microb. Pathog. 2020, 138, 103846. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.M.; Sun, G.Y. Silymarin mitigates lung impairments in a rat model of acute respiratory distress syndrome. Inflammopharmacology 2018, 26, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Shi, H.; Zhang, Y.; Xing, J.; Liu, L.; Qiao, F.; Li, J.; Chen, Y. Baicalin attenuates hepatic injury in non-alcoholic steatohepatitis cell model by suppressing inflammasome-dependent GSDMD-mediated cell pyroptosis. Int. Immunopharmacol. 2020, 81, 106195. [Google Scholar] [CrossRef]
- Chen, J.; Zhang, R.; Wang, J.; Yu, P.; Liu, Q.; Zeng, D.; Song, H.P.; Kuang, Z.Y. Protective effects of baicalin on LPS-induced injury in intestinal epithelial cells and intercellular tight junctions. Can. J. Physiol. Pharmacol. 2015, 93, 233–237. [Google Scholar] [CrossRef]
- Orzechowska, B.U.; Wrobel, G.; Turlej, E.; Jatczak, B.; Sochocka, M.; Chaber, R. Antitumor effect of baicalin from the Scutellaria baicalensis radix extract in B-acute lymphoblastic leukemia with different chromosomal rearrangements. Int. Immunopharmacol. 2020, 79, 106114. [Google Scholar] [CrossRef]
- Gao, Y.; Liu, H.; Wang, H.Z.; Hu, H.L.; He, H.J.; Gu, N.; Han, X.; Guo, Q.; Liu, D.; Cui, S.; et al. Baicalin inhibits breast cancer development via inhibiting IĸB kinase activation in vitro and in vivo. Int. J. Oncol. 2018, 53, 2727–2736. [Google Scholar] [CrossRef]
- Oo, A.; Rausalu, K.; Merits, A.; Higgs, S.; Vanlandingham, D.; Bakar, S.A.; Zandi, K. Deciphering the potential of baicalin as an antiviral agent for Chikungunya virus infection. Antivir. Res. 2018, 150, 101–111. [Google Scholar] [CrossRef] [PubMed]
- Song, J.; Zhang, L.; Xu, Y.; Yang, D.; Zhang, L.; Yang, S.; Zhang, W.; Wang, J.; Tian, S.; Yang, S.; et al. The comprehensive study on the therapeutic effects of baicalein for the treatment of COVID-19 in vivo and in vitro. Biochem. Pharmacol. 2021, 183, 114302. [Google Scholar] [CrossRef]
- Kim, D.H.; Hossain, M.A.; Kang, Y.J.; Jang, J.Y.; Lee, Y.J.; Im, E.; Yoon, J.H.; Kim, H.S.; Chung, H.Y.; Kim, N.D. Baicalein, an active component of Scutellaria baicalensis Georgi, induces apoptosis in human colon cancer cells and prevents AOM/DSS-induced colon cancer in mice. Int. J. Oncol. 2013, 43, 1652–1658. [Google Scholar] [CrossRef] [PubMed]
- Hytti, M.; Szabo, D.; Piippo, N.; Korhonen, E.; Honkakoski, P.; Kaarniranta, K.; Petrovski, G.; Kauppinen, A. Two dietary polyphenols, fisetin and luteolin, reduce inflammation but augment DNA damage-induced toxicity in human RPE cells. J. Nutr. Biochem. 2017, 42, 37–42. [Google Scholar] [CrossRef]
- Yan, H.Y.; Ma, L.L.; Wang, H.Q.; Wu, S.; Huang, H.; Gu, Z.Y.; Jiang, J.D.; Li, Y.H. Luteolin decreases the yield of influenza A virus in vitro by interfering with the coat protein I complex expression. J. Nat. Med. 2019, 73, 487–496. [Google Scholar] [CrossRef]
- Fassina, G.; Buffa, A.; Benelli, R.; Varnier, O.E.; Noonan, D.M.; Albini, A. Polyphenolic antioxidant (-)-epigallocatechin-3-gallate from green tea as a candidate anti-HIV agent. AIDS 2002, 16, 939–941. [Google Scholar] [CrossRef] [PubMed]
- Bachmetov, L.; Gal-Tanamy, M.; Shapira, A.; Vorobeychik, M.; Giterman-Galam, T.; Sathiyamoorthy, P.; Golan-Goldhirsh, A.; Benhar, I.; Tur-Kaspa, R.; Zemel, R. Suppression of hepatitis C virus by the flavonoid quercetin is mediated by inhibition of NS3 protease activity. J. Viral Hepat. 2012, 19, e81–e88. [Google Scholar] [CrossRef] [PubMed]
- Khachatoorian, R.; Arumugaswami, V.; Raychaudhuri, S.; Yeh, G.K.; Maloney, E.M.; Wang, J.; Dasgupta, A.; French, S.W. Divergent antiviral effects of bioflavonoids on the hepatitis C virus life cycle. Virology 2012, 433, 346–355. [Google Scholar] [CrossRef]
- Yang, X.; Yang, J.; Zou, H.J. Baicalin inhibits IL-17-mediated joint inflammation in murine adjuvant-induced arthritis. Clin. Dev. Immunol. 2013, 2013, 268065. [Google Scholar] [CrossRef]
- Fang, P.H.; Yu, M.; Zhang, L.; Wan, D.; Shi, M.Y.; Zhu, Y.; Bo, P.; Zhang, Z.W. Baicalin against obesity and insulin resistance through activation of AKT/AS160/GLUT4 pathway. Mol. Cell. Endocrinol. 2017, 448, 77–86. [Google Scholar] [CrossRef]
- Wu, J.Y.; Tsai, K.W.; Li, Y.Z.; Chang, Y.S.; Lai, Y.C.; Laio, Y.H.; Wu, J.D.; Liu, Y.W. Anti-Bladder-Tumor Effect of Baicalein from Scutellaria baicalensis Georgi and Its Application In Vivo. Evid. -Based Complement. Altern. Med. Ecam 2013, 2013, 579751. [Google Scholar] [CrossRef]
- Fu, Y.; Luo, J.; Jia, Z.Q.; Zhen, W.; Zhou, K.Q.; Gilbert, E.; Liu, D.M. Baicalein Protects against Type 2 Diabetes via Promoting Islet beta-Cell Function in Obese Diabetic Mice. Int. J. Endocrinol. 2014, 2014, 846742. [Google Scholar] [CrossRef] [PubMed]
- Xiong, J.; Wang, K.Z.; Yuan, C.X.; Xing, R.; Ni, J.B.; Hu, G.Y.; Chen, F.L.; Wang, X.P. Luteolin protects mice from severe acute pancreatitis by exerting HO-1-mediated anti-inflammatory and antioxidant effects. Int. J. Mol. Med. 2017, 39, 113–125. [Google Scholar] [CrossRef]
- Domitrovic, R.; Cvijanovic, O.; Pugel, E.P.; Zagorac, G.B.; Mahmutefendic, H.; Skoda, M. Luteolin ameliorates cisplatin-induced nephrotoxicity in mice through inhibition of platinum accumulation, inflammation and apoptosis in the kidney. Toxicology 2013, 310, 115–123. [Google Scholar] [CrossRef]
- Lu, X.Y.; Li, Y.H.; Xiao, X.W.; Li, X.B. [Inhibitory effects of luteolin on human gastric carcinoma xenografts in nude mice and its mechanism]. Zhonghua Yi Xue Za Zhi 2013, 93, 142–146. [Google Scholar] [PubMed]
- Yoon, S.P.; Maeng, Y.H.; Hong, R.; Lee, B.R.; Kim, C.G.; Kim, H.L.; Chung, J.H.; Shin, B.C. Protective effects of epigallocatechin gallate (EGCG) on streptozotocin-induced diabetic nephropathy in mice. Acta Histochem. 2014, 116, 1210–1215. [Google Scholar] [CrossRef] [PubMed]
- Qin, N.; Chen, Y.; Jin, M.N.; Zhang, C.; Qiao, W.; Yue, X.L.; Duan, H.Q.; Niu, W.Y. Anti-obesity and anti-diabetic effects of flavonoid derivative (Fla-CN) via microRNA in high fat diet induced obesity mice. Eur. J. Pharm. Sci. 2016, 82, 52–63. [Google Scholar] [CrossRef]
- Jiang, H.; Yamashita, Y.; Nakamura, A.; Croft, K.; Ashida, H. Quercetin and its metabolite isorhamnetin promote glucose uptake through different signalling pathways in myotubes. Sci. Rep. 2019, 9, 2690. [Google Scholar] [CrossRef]
- Hua, F.Z.; Ying, J.; Zhang, J.; Wang, X.F.; Hu, Y.H.; Liang, Y.P.; Liu, Q.; Xu, G.H. Naringenin pre-treatment inhibits neuroapoptosis and ameliorates cognitive impairment in rats exposed to isoflurane anesthesia by regulating the PI3/Akt/PTEN signalling pathway and suppressing NF-κB-mediated inflammation. Int. J. Mol. Med. 2016, 38, 1271–1280. [Google Scholar] [CrossRef]
- Rahman, M.M.; Shohag, S.; Islam, M.R.; Akhter, S.; Mim, S.A.; Sharma, R.; Rauf, A. An Insight into COVID-19 and Traditional Herbs: Bangladesh Perspective. Med. Chem. 2022, 19, 361–383. [Google Scholar] [CrossRef]
- Rauf, A.; Abu-Izneid, T.; Khalil, A.A.; Hafeez, N.; Olatunde, A.; Rahman, M.; Semwal, P.; Al-Awthan, Y.S.; Bahattab, O.S.; Khan, I.N.; et al. Nanoparticles in clinical trials of COVID-19: An update. Int. J. Surg. 2022, 104, 106818. [Google Scholar] [CrossRef] [PubMed]






| Flavonoids | Basic Structure | Example | ||
|---|---|---|---|---|
| Flavones |  |  |  |  |
| Flavonols |  | 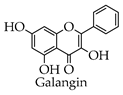 |  | 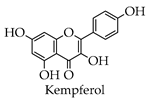 |
| Isoflavones |  | 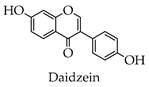 | 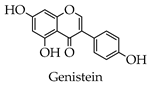 | 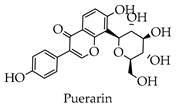 |
| Chalcones |  | 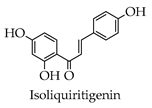 | 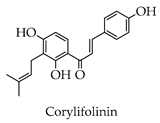 | 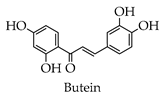 |
| Flavanes |  |  |  | 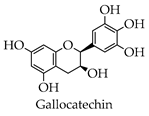 |
| Anthocyanins |  | 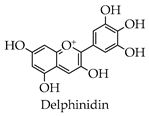 | 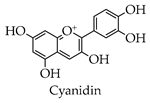 | |
| Compound | In Vitro Models | Conc. | Effects | Mechanism of Action | References |
|---|---|---|---|---|---|
| Baicalin | HepG2 cells | 16 μM | Pneumonia | Inhibits NLRP3 inflammatory vesicles | [128] |
| Rat IEC-6 cells | 10.0 μg/mL | Inflammatory bowel disease | Inhibits IL-6 and TNF-α inflammatory factor levels | [129] | |
| KOPN-8, RCH-ACV, SEM, RS4-11, NALM-6 | 10 mg/mL | Acute B-lymphoblastic leukemia | Inhibits the glycogen synthase kinase 3β and induces cell cycle arrest by upregulating p27Kip1 | [130] | |
| MCF-7 and MDA-MB-231 cells | 30 μM | Breast cancer | Inhibits breast cancer cell proliferation and induces G1/S arrest in cells | [131] | |
| Vero, BHK-21, and HEK 293T cells | 100 μM | Chikungunya virus | — | [132] | |
| Baicalein and baicalin | Vero CCL-81 cells | 20 μM | SARS-CoV-2 | Inhibits SARS-CoV-2 RNA-dependent RNA polymerase activity | [105] |
| Baicalein | Vero E6 cell | >2.0 μM | COVID-19 | Inhibits virus replication in vivo and reduces serum levels of IL-1β and TNF-α | [133] |
| Vero cell lines | 50 μM | SARS-CoV-2 | Inhibits SARS-CoV-2 replication and its 3C-like protease | [105] | |
| HCT116 cells | 50 μM | Colorectal cancer | Induces apoptosis in human colon cancer cells | [134] | |
| Silymarin | Vero cells | 749.70 µg/mL | Dengue virus | Binds to the surface protein of the virus to prevent entry into the cell | [70] |
| Luteolin | ARPE-19 cells | 50 μM | Age-related macular degeneration | Decreases levels of IL− 8 and IL− 6 | [135] |
| MDCK cells and Vero cells | From 3.75 to 240 μM | Influenza A virus | Inhibits the expression of β-COP protein | [136] | |
| Enzymatic inhibition assay | 4.6 μM | COVID-19 | Inhibits SARS-CoV-2 RNA-dependent RNA polymerase activity | [25] | |
| EGCG | Peripheral blood lymphocytes | 50 μM | HIV | — | [137] |
| live SARS-CoV-2 strain | 1 μg/mL | SARS-CoV-2 | Inhibits Nsp15 activity | [111] | |
| E. coli | 7.58 μg/ mL | SARS-CoV-2 | Inhibits the activity of 3CLpro | [112] | |
| Formononetin | Vero cells | 14.91 μmol/L | Enterovirus 71 | Inhibits EV71-induced COX-2 expression and PGE2 production via MAPKs pathway | [68] |
| Biochanin A | A549 cells | 5 μM | H5N1 influenza A viruses | Interferes with AKT, ERK 1/2, and NFκB activation to inhibit viral replication | [65] |
| Quercetin | T-REx™-293 cell line | 10 μg/mL | HCV | Inhibits NS3 protease, thereby inhibiting viral replication | [138] |
| Naringenin | Huh-7.5 cells | 25 μM | HCV | Reduces production of intracellular viral proteins | [139] |
| Compound | In Vivo Models | Conc. | Effects | Mechanism of Action | References |
|---|---|---|---|---|---|
| Baicalin | Male C57BL/6 mice | 21 mg/kg | Arthritis | Antagonism of Th-17 cells | [140] |
| Female BALB/C nude mice | 200 mg/kg | Breast cancer | Inhibits breast cancer cell proliferation and induces G1/S arrest in cells | [131] | |
| Six-week-old male C57BL/6J mice | 21 mg/kg | Diabetes | Activates AKT/AS160/GLUT4 pathway | [141] | |
| Baicalein | Male SD rats | 200 mg/kg | COVID-19 | Inhibits virus replication in vivo and reduces serum levels of IL-1β and TNF-α | [133] |
| Male ICR mice | 1, 5, and 10 mg/kg | Colorectal cancer | Induction of apoptosis in human colon cancer cells | [134] | |
| Female C57BL/6 mice | 0.8 mg/mouse nine times | Bladder cancer | Reduces expression of cyclin D1 by inhibiting new protein synthesis and promoting proteasomal degradation and reduces expression of cyclin B1 by inhibiting new protein synthesis. | [142] | |
| Male C57BL/6 mice | 0.5 mg/kg | Type 2 diabetes | Improves the viability and insulin secretion of fine beta cells and human pancreatic islets | [143] | |
| Luteolin | Male ICR mice | 100 mg/kg | Acute pancreatitis | Suppresses the activation of the NF-κB pathway | [144] |
| Male BALB/cN mice | 5mg/kg | Nephrotoxicity | Reduces Pt accumulation in the kidney to improve oxidative stress and inflammation | [145] | |
| BALB/c nude mice | 40 mg/kg | Gastric carcinoma | Downregulates VEGF-A and MMP-9 and decreases the immune response | [146] | |
| EGCG | Male C57BL/6 mice | 10 mg/kg | SARS-CoV-2 | Inhibits virus replication | [114] |
| Male ICR mice | 100 mg/kg | Diabetic nephropathy | Inhibits increased OPN expression, reduces serum creatinine, and causes proteinuria and normalized morphological changes in STZ-induced diabetic nephropathy | [147] | |
| Oroxylin A | Female BALB/c nude mice | 200 mg/kg | Lung cancer | Inhibits the activation of ERK signaling and inhibits snail protein content and EMT | [93] |
| Male DBA/1 mice | 10 mg/kg | Rheumatoid arthritis | Reduces serum levels of anti-CII Abs, IL-1β, IL-6, TNFα, and IL-17 | [61] | |
| Tiliroside | Male C57BL/6 mice | 5 mg/kg, 15 mg/kg, 300 mg/kg Dose-dependent manner | Type 2 diabetes | Regulates miR-27 expression and inhibits glycoisomerization | [148] |
| Biochanin A | Male C57BL/6 mice | 12.5, 25, and 50 mg/kg | Acute lung injury | Inhibits TLR4/NF-κB signaling pathway activation and increases PPAR-γ expression in the lungs | [126] |
| Isorhamnetin | Male ICR mice | 1 nM | Diabetes | Activates JAK/STAT pathway to increase glucose uptake by muscle cells | [149] |
| Quercetin | Male ICR mice | 0.1 nM and 1 nM | Diabetes | Activates CaMKKβ/AMPK signaling pathway and activates IRS3/PI10K/Akt signaling | [149] |
| Naringenin | Pregnant Sprague–Dawley rats | 25, 50, or 100 mg/kg | Neuroapoptosis | Regulates PI3/Akt/PTEN signaling pathway and inhibits NF-κB-mediated inflammation | [150] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, J.-Y.; Ma, Y.-X.; Liu, Y.; Peng, X.-J.; Chen, X.-Z. A Comprehensive Review of Natural Flavonoids with Anti-SARS-CoV-2 Activity. Molecules 2023, 28, 2735. https://doi.org/10.3390/molecules28062735
Yang J-Y, Ma Y-X, Liu Y, Peng X-J, Chen X-Z. A Comprehensive Review of Natural Flavonoids with Anti-SARS-CoV-2 Activity. Molecules. 2023; 28(6):2735. https://doi.org/10.3390/molecules28062735
Chicago/Turabian StyleYang, Jun-Yu, Yi-Xuan Ma, Yan Liu, Xiang-Jun Peng, and Xiang-Zhao Chen. 2023. "A Comprehensive Review of Natural Flavonoids with Anti-SARS-CoV-2 Activity" Molecules 28, no. 6: 2735. https://doi.org/10.3390/molecules28062735
APA StyleYang, J.-Y., Ma, Y.-X., Liu, Y., Peng, X.-J., & Chen, X.-Z. (2023). A Comprehensive Review of Natural Flavonoids with Anti-SARS-CoV-2 Activity. Molecules, 28(6), 2735. https://doi.org/10.3390/molecules28062735






