Abstract
Cardiovascular diseases are the leading cause of death worldwide, and as rates continue to increase, discovering mechanisms and therapeutic targets become increasingly important. An underlying cause of most cardiovascular diseases is believed to be excess reactive oxygen or nitrogen species. Glutathione, the most abundant cellular antioxidant, plays an important role in the body’s reaction to oxidative stress by forming reversible disulfide bridges with a variety of proteins, termed glutathionylation (GSylation). GSylation can alter the activity, function, and structure of proteins, making it a major regulator of cellular processes. Glutathione-protein mixed disulfide bonds are regulated by glutaredoxins (Glrxs), thioltransferase members of the thioredoxin family. Glrxs reduce GSylated proteins and make them available for another redox signaling cycle. Glrxs and GSylation play an important role in cardiovascular diseases, such as myocardial ischemia and reperfusion, cardiac hypertrophy, peripheral arterial disease, and atherosclerosis. This review primarily concerns the role of GSylation and Glrxs, particularly glutaredoxin-1 (Glrx), in cardiovascular diseases and the potential of Glrx as therapeutic agents.
1. Introduction
Over the past several decades, cardiovascular diseases (CVD) have been on the rise due to the heightened global prevalence of obesity and metabolic diseases [1,2]. Cardiovascular diseases account for the leading causes of death in the United States today and thus are a vital area of study [3,4]. As cardiovascular diseases are such a widespread issue, a profusion of research is being devoted to discovering the underlying causes and mechanisms to formulate potential treatments for many of these cardiovascular diseases. Unbiased omics approaches such as genetics, transcriptomics, metabolomics, and proteomics provide a deeper understanding of disease-associated pathways. CVDs are often associated with a perturbed redox environment [5,6,7], therefore studying the proteins involved in oxidant defense, repair, and redox signaling is such a vital aspect in the search for potential treatment of human diseases in the growing epidemic.
Glutathione (GSH) is an abundant small tripeptide functioning as a cellular antioxidant and redox buffer. The reversible addition of glutathione to protein cysteines forming a mixed-disulfide is referred to as glutathionylation (GSylation). GSylation is a physiological process that participates in redox signaling and protects protein cysteine thiols from irreversible oxidation during oxidative stress. Glutaredoxin-1 (Glrx) is an essential thioltransferase whose primary role is to remove protein GSylation [6]. While GSylation occurs transiently in physiology, a rise in GSylation is associated with various pathologies, perturbing normal redox signaling and cell function. Oxidative stress and inactivation of Glrx, in part, may contribute to the pathological protein GSylation.
Glrx plays an important role in the activity of an abundance of proteins and cellular processes by regulating the presence of these disulfide bonds, specifically through the reduction of GSH-protein disulfide bonds [8]. Glrx maintains the cellular redox homeostasis by regulating the GSylation of many vital proteins involved in signal transduction, such as phosphatases, kinases, and transcription factors. The roles of GSylation and Glrx depend on target molecules in the pathological condition. Glrx and GSylation have been implicated in a wide range of diseases, such as Parkinson’s [9,10,11], retinal degenerative disorders [12,13,14], non-alcoholic fatty liver disease [15,16,17], lung disease [18,19], and CVDs. Studies have shown that overexpressing Glrx may be an effective treatment for attenuating cardiac dysfunction in diabetic mice by maintaining redox homeostasis [20] as well as preventing cell death in rat cardiomyocytes under RNS stress [21].
In contrast, inhibition of Glrx is also vital for the revascularization of limbs following ischemia [22,23,24]. Research implicates Glrx controls fine tuning of redox signaling and may be a potential therapeutic target in a wide range of pathologies in which oxidative stress is involved. This review will focus on the GSylation and Glrx functions and targets in various types of CVD and discuss clinical applications.
2. Glutathion(GS)ylation
Glutathione (GSH), the tripeptide γ-L-glutamyl-L-cysteinyl-glycine, is one of the most abundant thiol redox-active molecules in the cell. Under normal physiological conditions, intracellular GSH concentrations range from 1 mM in most cell types to 10 mM in hepatocytes [8]. The concerted synthesis by glutathione synthetase and γ-glutamyl cysteine ligase provides the cell with GSH [25,26]. GSH is a vital cellular redox buffer and plays an essential role in combating oxidative stress, removing xenobiotics and toxins, synthesizing a variety of cellular signaling molecules [27,28], and regulating transcription factors. Various antioxidant enzymes, including glutathione peroxidases, glutaredoxins, and peroxiredoxins, use GSH as a thiol reductant to restore their enzymatic activities.
The sulfhydryl group (-SH) of protein cysteines can exist in a protonated (R-SH; thiol) or deprotonated state (R-S−; thiolate). The thiolate, as compared with the thiol, is chemically highly reactive and prone to oxidation. Various enzymes, including GAPDH and caspases use cysteine thiolates for biochemical catalysis in their active sites. Surrounding amino acids with basic or polar side chains such as histidine or serine, respectively, can stabilize the thiolate and markedly increase its chemical reactivity and sensitivity to oxidation. Exposure of the thiolate at the protein surface further renders it a likely target of redox modifications and regulation.
These reactive cysteine thiolates can exhibit a reactivity resembling that of a thiol-peroxidase and thus react with oxidants such as hydrogen peroxide. However, recent experiments suggest that hydrogen peroxide may not react directly; and peroxymonocarbonate is a reactive intermediate to oxidize cysteine of proteins [29]. The oxidation of the thiolate transiently produces sulfenic acid (R-SOH) that reacts with GSH leading to GSylation [30,31,32]. GSH acts as a thiol reductant and forms a mixed disulfide bond with the cysteine of the target protein, the first reduction step to prevent further irreversible protein thiol oxidation to sulfinic (-SO2H) and sulfonic acid (-SO3H). In a parallel NO-dependent pathway, these cysteines can be first nitros(yl)ated, and then GSylated [32,33,34].
GSH primarily functions as a redox buffer to maintain a reductive cellular environment for biochemical catalysis, a substrate for phase II detoxification reactions, and a reductant for cellular redox signaling and antioxidant defense. Cells experience oxidative stress when reactive oxygen species (ROS) such as hydrogen peroxide (H2O2) and superoxide, or reactive nitrogen species (RNS) including nitric oxide (NO), are generated in excess and overwhelm the cellular antioxidant system. Altered redox homeostasis, common to most CVDs, perturbs redox and nitric oxide signaling [35,36,37]. NO fluxes in the nanomolar range control vascular cell growth, migration, and adhesion, as well as vascular tone [38,39]. In contrast, higher NO concentrations generated by immune cells, such as macrophages, have cytotoxic and inflammatory effects [40].
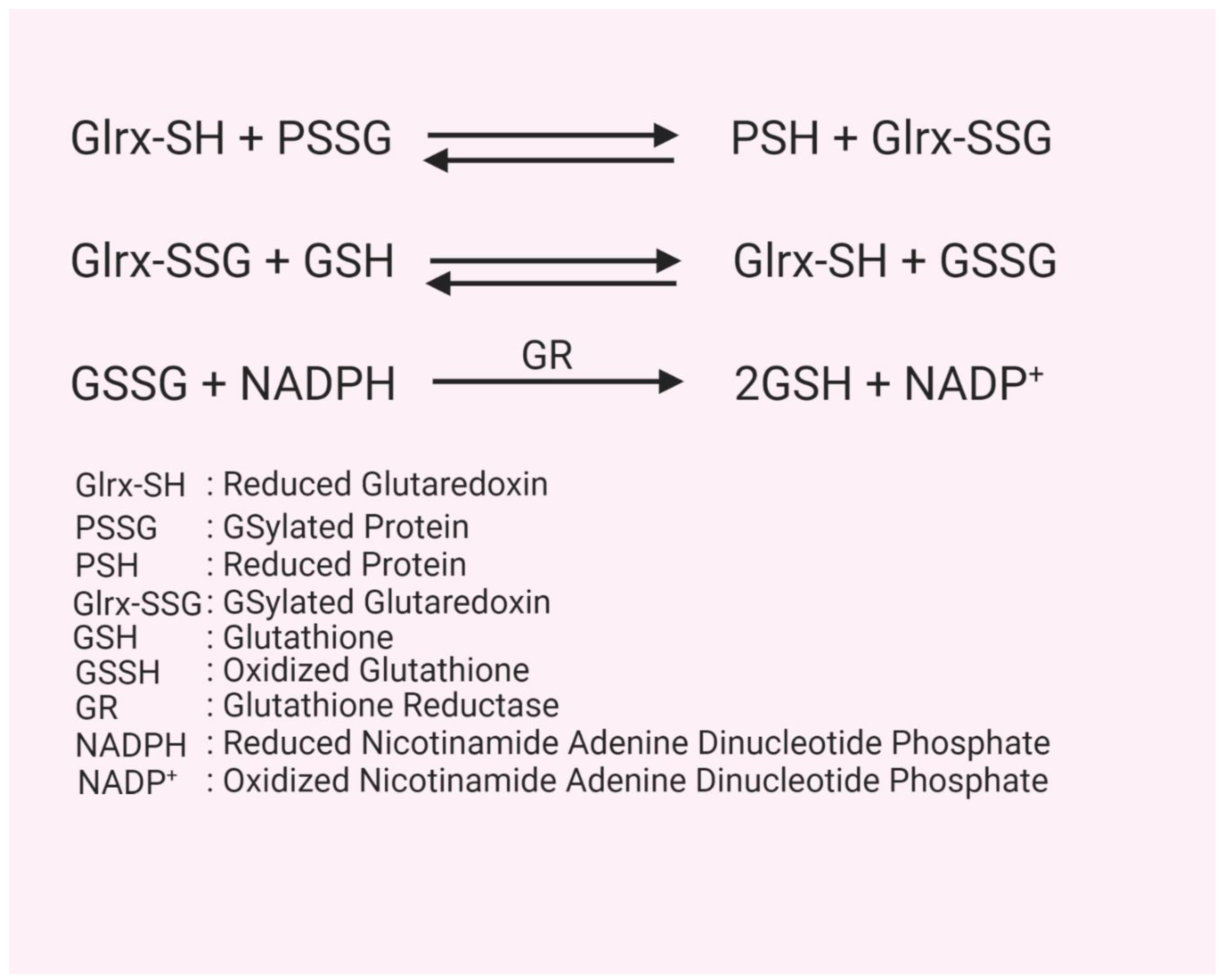
GSH plays a vital role in antioxidant defense. For instance, the conversion of H2O2 to water is catalyzed by members of the glutathione peroxidase family [41]. In this reaction, the enzyme’s selenocysteine reacts with H2O2 to produce selenenic acid and water. In two reduction steps using GSH, the selenenic acid is converted back to selenocysteine, releasing oxidized glutathione (GSSG). Glutathione reductase, under the consumption of NADPH, reduces GSSG back to two GSH molecules [8]. Protein-bound GSH (PSSG) formation can significantly alter the structure, function, and activity of many proteins, including those involved in cell proliferation, cell death, and metabolism [8]. Protein-GSH mixed disulfide bonds are reduced by glutaredoxin (Glrx). The resulting GSylated Glrx (Glrx-SSG) is then reduced by GSH, forming GSSG and the reduced active Glrx [6] (Figure 1). The reductive cellular environment and GSH can also remove protein GSylation spontaneously without the enzymatic catalysis, but it proceeds at a markedly slower rate. Thus, Glrx deficient mice are not lethal, but their tissues have a significantly higher protein GSylation level under oxidative stress [42].
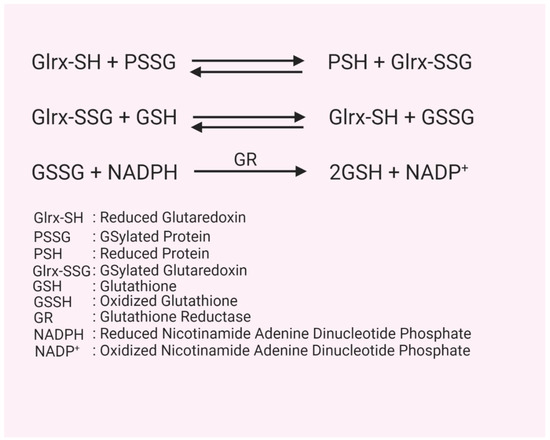
Figure 1.
Glutaredoxin reaction. Figure represents steps of protein deGSylation by glutaredoxin-1 (Glrx) and regeneration of Glrx by glutathione (GSH).
GSH is more abundant than oxidized GSSG under standard physiological conditions in the cell. In healthy organisms, a GSH:GSSG ratio of 100:1 is typical. This ratio can drop to below 10:1 under oxidative stress, therefore a low ratio of GSH to GSSG is widely considered a hallmark of oxidative stress and associated with various CVDs [43,44,45]. Since Glrx needs GSH as a cofactor, the low GSH environment may decrease Glrx activity, further increasing protein GSylation.
The transient nature and low abundance complicate the detection of physiological protein GSylation [46]. There are various methods to detect protein GSylation, each with its advantages and limitations. 35S-radiolabeling GSH (35S-GSH) is a highly sensitive and convenient method to detect GSylated proteins that requires prior inhibition of protein synthesis, followed by introducing radiolabeled 35S-cysteine into cells. Glutathione synthesis occurs independently from protein synthesis, thus, radiolabeled cysteine is mainly incorporated into glutathione. GSylated proteins can be isolated, separated on non-reducing gels, and detected by autoradiography or phosphorimaging. Loss of the radioactive signal after chemical or enzymatic reduction further confirms protein GSylation [47]. A similar method can be applied to detect GSylation using stable isotopes combined with mass spectrometry and proteomics [48].
Chemical or isotope labeled glutathione is an alternative method and can be introduced into cells as a cell-permeable ester. There is no need to inhibit protein synthesis, which can adversely affect cell physiology. In this method free thiols are blocked irreversibly by an alkylating agent. The modified thiols are then reduced by Glrx and labelled with biotin [49]. The biotinylated thiols undergo affinity purification with streptavidin and are analyzed by different proteomic approaches.
Antibody-based methods such as Western blot or immunoprecipitation allow direct detection of protein GSylation. However, commercial antibodies often lack sensitivity, produce high backgrounds, and work for select proteins only. Several other methods are also being used to detect GSylation via liquid chromatography-coupled mass spectrometry, (LC-MS)-based top-down proteomics [50], and ‘clickable’ GSH approach to detect GSylation [51]. As new technologies advance, overcoming these limitations may be possible in the near future.
3. Glutaredoxin Structure, Function, and Mechanism
Glutaredoxins (Glrxs) belong to the thioredoxin (Trx) protein family and catalyze a variety of processes including GSH-dependent redox reactions, the assembly of iron-sulfur (Fe-S) clusters, and redox signaling [52]. Glrxs contain a thioredoxin fold as an active site motif that is either Cys-X-X-Ser for the monothiol or Cys-X-X-Cys for the dithiol protein members. The thioredoxin fold is typically found in oxidoreductases and consists of a four-banded β-pleated sheet in between three alpha helices [53]. Glrxs have a cysteine in the N-terminal position of the active site, which is notably involved in the reduction of GSylated proteins (PSSGs).
There are four known members of the glutaredoxin family in mammals: glutaredoxin-1 (Glrx), glutaredoxin-2 (Glrx2), glutaredoxin-3 (Glrx3, also known as PICOT), and glutaredoxin-5 (Glrx5). These Glrxs differ in their functions, localization within the cell, substrate specificity, and amino acid sequence [54] (Table 1). Glrx and Glrx2 are dithiol, with their active site containing two cysteine residues for both Glrx (Cys-Pro-Tyr-Cys) and Glrx2 (Cys-Ser-Tyr-Cys), whereas Glrx3 [55] and Glrx5 [56] are monothiol, with only a single active site cysteine (Cys-Gly-Phe-Ser) [57]. Despite the difference in active sites, both types of Glrxs are able to bind GSH as a substrate and have varying degrees of oxidoreductase activity [52]. Glrx can perform both monothiol and dithiol reactions. In the dithiol reaction, Glrx launches a nucleophilic attack with its N-terminal active site cysteine onto a PSSG, forming a mixed disulfide. The available C-terminal active site cysteine of Glrx then attacks the mixed disulfide, forming oxidized glutaredoxin (Glrx-SSG) and releasing the reduced protein and a GSH molecule. Glrx-SSG is then reduced by two GSH molecules to reform active Glrx as well as GSSG. In the monothiol reaction, Glrx attacks the PSSG with its N-terminal active site cysteine resulting in the reduced protein and Glrx-SSG, which is then reduced by GSH to form Glrx and GSSG [6].

Table 1.
Characteristics of human glutaredoxins. Glrx, glutaredoxin-1; Glrx2, glutaredoxin-2; Glrx3, glutaredoxin-3; Glrx5, glutaredoxin-5; C, cysteines; P, proline; F, phenylalanine; Y, tyrosine; S, serine; Da, daltons; PICOT, PKC-interacting cousin of thioredoxin.
While it is only the primary function of Glrx, all four human Glrxs are capable of GSH-dependent oxidoreductase activity; they are able to reduce mixed disulfide bonds as noted earlier [52]. Glrx3 and Glrx5 notably reduce PSSGs at a much slower rate. Glrx2, Glrx3, and Glrx5 primarily function in iron-sulfur cluster assembly (2Fe-2S) and maintenance of iron homeostasis [64,65,66]. While not the focus of this review, the importance of these Glrxs and iron-sulfur clusters in many cellular processes such as DNA replication, DNA repair, transcription, and respiration should be noted [67,68]. Isoforms of Glrxs are described in detail elsewhere [69].
Glrx and Glrx3 are primarily contained in the cytoplasm, but Glrx may be present in the nucleus of some cell types as well as the mitochondrial intermembrane space [70], while Glrx2 and Glrx5 reside in the mitochondria. Glrx is considered as a main mammalian enzyme for de-GSylation and the multiple isoforms in the same location may ensure that redox regulation is tightly controlled. Glrx controls a wide variety of signaling pathways and cellular processes due to its role in regulating GSylation [8] in pathophysiological settings, including immune, reproductive, pulmonary, nervous, cancer, and cardiovascular diseases [52]. Glrx target proteins differ among organisms; they are vital components of important signaling pathways (Table 2).

Table 2.
Target proteins of glutaredoxin-1. GAPDH, glyceraldehyde 3-phosphate dehydrogenase; PTP1B, protein tyrosine phosphatase 1B; SERCA, sarco/endoplasmic reticulum Ca2+-ATPase.
4. Cardiovascular Disease
Protein GSylation has been implicated in CVD due to its importance in maintaining cardiovascular homeostasis. As the most abundant antioxidant in cells, GSH controls the regulation of many key biological processes and signaling pathways involved in CVD. Changes in protein GSylation levels and GSH:GSSG ratio are strongly correlated with the progression of CVDs, such as ischemia and reperfusion (IR), peripheral arterial disease, cardiac hypertrophy, and atherosclerosis.
4.1. Myocardial Ischemia and Reperfusion
Ischemia is known to increase protein GSylation levels, which stay elevated until the end of reperfusion [82]. Studies have focused on increasing Glrx in order to attenuate the heightened levels of GSylation during IR. Adenoviral Glrx gene therapy in type I diabetic mice protected hearts from IR injury, including decreased apoptosis of cardiomyocytes, reduced myocardial infarction size, and improved ventricular recovery [20]. Glrx controls apoptosis through modifications of proteins important in cell death pathways, such as activating Akt [79], NF-κB [24,72,83], and inhibiting Fas [84]. Akt activation results in the phosphorylation and deactivation of both FoxO and Ask-1, vital proteins involved in pro-apoptotic signaling pathways [20,79,85,86]. By inhibiting myocardial apoptotic signals, Glrx overexpression is able to attenuate infarction area and ventricular dysfunction in diabetic and non-diabetic mice [20,87]. GSylation of G-actin during IR decreased its polymerization rate and tropomyosin binding affinity, indicating that GSylation contributes to the decreased cardiac contractility associated with IR in rats [77,88].
GAPDH is one notable protein GSylated in high levels during ischemia and reperfusion (IR) [82]. A decrease in functional GAPDH due to GSylation increases apoptosis and inhibits glycolysis. We have shown oxidative or metabolic stress induces GAPDH GSylation in primary human aortic endothelial cells (HAEC). Gsylated-GAPDH is then translocated to the nucleus, where it interacts with histone deacetylating enzyme Sirtuin 1 (SirT1) and transfers GSylation to SirT1. This process, called trans-GSylation, inactivates SirT1 and results in the activation of apoptotic signaling by acetylation of the proapoptotic protein p53. Our results show that Glrx significantly de-GSylates GAPDH and protects HAEC’s from apoptosis by preventing the interaction of GAPDH with SirT1 [89]. This finding suggests that Glrx can also be utilized in favored redox signaling nodes like peroxiredoxin [90]. It is very likely that all peroxidatic cysteine enzymes act as signaling nodes and partner with very specific proteins in highly localized cellular subcompartments. Interestingly, GAPDH is GSylated in a cardiac rat IR model [82], implicating it as a possible signaling pathway leading to apoptosis in IR. The mechanism by which Glrx prevents GAPDH-SirT1 interaction through the regulation of GAPDH could have important implications in IR as well as other CVDs.
In contrast to other Glrx studies, Glrx KO mice with induced IR were shown to have similar vulnerability to acute oxidative damage as the control mice [42]. This indicates that cytosolic protein GSylation may not be as significant a cause of tissue injury in CVD as previously believed [42] or that other compensatory enzymes are upregulated to prevent progressive damage. Further, animal model research should be conducted to make more decisive conclusions on the ameliorating effects of Glrx on CVDs.
Hypoxia is a responsible factor for myocardial complications such as coronary heart disease. ROS generated during hypoxia/ischemia have adverse effects on metabolism, causing irreversible modifications of proteins, disrupt the redox state of the cells, and result in decline in cardiomyocytes contractility. Na,K ATPase maintains cardiomyocytes contractility by maintaining intracellular calcium levels. Irreversible modification of Na,K ATPase under hypoxic condition leads to cell death. Petrushanko et al. showed that acute hypoxia induces GSylation of Na,K-ATPase, inhibiting its activity and allowing the cell to avoid depletion of ATP before switching to anaerobic glycolysis. Thiol-containing compounds, including various GSH derivatives, significantly extend normal functioning of isolated rat cardiomyocytes under hypoxic conditions. Nitrosoglutathione (GSNO), which is known to induce GAPDH GSylation [33], was shown to promote faster recovery of isolated rat heart contractility by GSylation of Na,K ATPase following ischemia-reperfusion [91,92].
One prominent target of GSylation is nitric oxide synthase (NOS). When NOS is GSylated, it undergoes a reversible process called uncoupling in which its enzymatic activity converts from NO production to superoxide production, reacting with NO to generate more potent oxidants, such as peroxynitrite (ONOO−) [80]. Thus, NOS uncoupling increases oxidative stress conditions and is associated with decreased vascular endothelial cell function or caused endothelial dysfunction, which leads to a variety of CVDs, including IR and atherosclerosis [93,94]. Studies have found that Glrx reverses NOS uncoupling via de-GSylation in vitro. It was separately concluded the inhibition of Glrx increases NOS uncoupling, and Glrx overexpression attenuates NOS uncoupling, implicating Glrx as an important enzyme in the regulation of NOS [95]. These results indicate that Glrx could improve cardiovascular conditions aggravated by NOS uncoupling.
In contrast, GSylation of sarco/endoplasmic reticulum Ca2+ ATPase (SERCA) Cys674 by an acute oxidant stimulates the protein, resulting in decreased intracellular Ca2+ levels and vasorelaxation [81]. NO-induced endothelial cell migration and Ca2+ uptake depend on Cys674, and Glrx overexpression inhibits the process [96] and manifests anti-angiogenic features as mentioned later. However, irreversible oxidation of Cys674 in association with chronic oxidative stress caused degradation of SERCA protein in diabetic pig aorta [97]. These differences in functional effects likely reflect the individual pKa of the protein’s cysteine residue and, by extension, quantity and concentration of redox that is available to the protein.
4.2. Cardiac Hypertrophy
Cardiovascular hypertrophy is commonly associated with many CVDs, typically occurring in early phases. Cardiac hypertrophy is characterized by an increase in cardiomyocyte size in order to increase the function of the cardiac pump while decreasing the tension on the ventricular walls. Increased functioning capacity of the cardiac pump may be initially beneficial; however, it greatly increases the risk of heart failure, sudden death, and other heart conditions in the long term [98,99].
While many factors contribute to the onset of cardiac hypertrophy, of particular interest is the Raf/MEK/ERK pathway [100]. Stimulation of this pathway is believed to occur through mechanical stress and G-protein coupled receptors but was also shown to be dependent on GSylation of Ras in studies on rat myocytes in vitro [58]. GSylated Ras increased ERK activity and the synthesis of proteins that drive cardiac hypertrophy. The same study presented evidence that adenoviral overexpression of Glrx attenuated cardiac hypertrophy through reduction of Ras-SSG, thus preventing increased downstream protein synthesis.
Our lab demonstrated that Glrx KO mice fed a high fat high sucrose diet (HFHS) develop cardiometabolic dysfunction, leading to left ventricular hypertrophy and fibrosis, which contribute to diastolic dysfunction. Glrx deficiency likely causes impaired the metabolic flexibility (Osaki et al., in prep.).
Notably, the role of Glrx on cardiac hypertrophy depends on the pathological model. Angiotensin II-induced cardiovascular hypertrophy was attenuated in Glrx KO mice in association with lower oxidants generation in aortas [101], speculating NADPH oxidase activation, which is essential to angiotensin II signaling, might be impaired.
In addition to Glrx, Glrx2 and Glrx3 have also been shown to play a role in cardiac hypertrophy. Deletion of Glrx2 in mice hearts results in cardiac hypertrophy and fibrosis as well as hypertension [61], while Glrx3 KO in mice results in cardiac hypertrophy and heart failure [63]. Glrx3 KO mice were found to have significant left ventricular hypertrophy compared to their WT counterparts at 12 months of age. This is due to increased production of ROS in cardiomyocytes as well as Ca2+ dysregulation after Glrx3 KO [61]. In another study, Glrx3 overexpression in transgenic mice was found to inhibit cardiac hypertrophy. Glrx3 was postulated to disrupt interactions between muscle LIM protein (MLP) and calcineurin, which inhibits calcineurin-NFAT signaling, an important signaling pathway that promotes cardiomyocyte growth [102]. These studies exemplify that several Glrxs play roles in attenuating cardiac hypertrophy and will likely be dependent on protein interactions and sub-cellular localization.
4.3. Peripheral Arterial Disease
Glrx has been implicated in peripheral arterial disease and impaired vascularization in the limbs. In contrast to beneficial roles of increased Glrx in post-ischemic cardiac revascularization [87], Glrx overexpression inhibits angiogenesis in mouse hindlimb ischemia [24], while Glrx deletion in mice improves limb revascularization following ischemia [23]. Glrx inhibits angiogenesis through control of several target proteins, including tyrosine phosphatases, Rac1, HIF1-α, and NF-κB [22]. Glrx-induced Rac1 activation leads to inhibition of endothelial permeability [59] which may suppress endothelial cell migration. HIF-1α, a key angiogenic transcriptional factor, was stabilized by GSylation, further implicating the anti-angiogenic role of Glrx in hind limb ischemia [23]. The overexpression of Glrx is protective in the setting of cardiac ischemia but deleterious for ischemic limb, although both cases are associated with NF-κB activation. There are other cases showing the redox signaling in response to ischemia differs between the heart and muscles [22]. The main reason for this is probably that inhibiting apoptosis in acute ischemia is essential to myocardial survival, whereas angiogenesis potential is more important to ischemic limb recovery.
4.4. Atherosclerosis
Atherosclerosis can occur at large, medium, and small vessels leading to organ dysfunction due to ischemia, thrombotic phenomena, and tissue infarction [103]. Hyperlipidemia is an important risk factor for developing atherosclerosis [104,105]. Glrx KO has been shown to cause hyperlipidemia. Our group reported that Glrx KO mice develop hyperlipidemia, non-alcoholic fatty liver disease [17], and a cardiometabolic phenotype leading to diastolic dysfunction when fed a high fat diet (Osaki, et al. in prep).
Vascular permeability is postulated to be involved in giving rise to atherosclerosis and has been linked to a low GSH:GSSG ratio. It should be noted that GSylation and subsequent inactivation of Rac1 has been proved to play a role in vascular endothelial cell permeability. Glrx overexpression in high fat fed mice was shown to attenuate vascular permeability through deGSylation of endothelial cell proteins, particularly Rac1 [59].
One of the mechanisms behind atherosclerosis is damage to blood vessel wall endothelial cells, which are vital to upholding the integrity of the vascular wall as well as maintaining homeostasis [106,107]. This damage is often due to oxidative stress, which can induce apoptosis in endothelial cells. One of the most prominent apoptotic signaling proteins is Bim, a Bcl2 family protein that is most notably regulated by the transcription factor FoxO1, which is regulated by Akt through degradation after phosphorylation [108]. Furthermore, JNK (c-Jun N-terminal kinase), an important enzyme in stress response, has been shown to activate Bim through phosphorylation, promoting apoptotic signaling [109,110].
Endothelial cells, however, have protective mechanisms to combat oxidative stress in order to prevent apoptosis. Studies have shown that steady laminar blood flow reduces oxidative stress by inducing a reducing environment inside endothelial cells [111]. Laminar flow has also been shown to upregulate Glrx activity, which plays an important role in Akt activation [60]. Increased Glrx levels result in the prevention of apoptosis in endothelial cells by lowering Bim expression via Akt-FoxO1 signaling as well as by inhibiting JNK activation of Bim [89,112]. Additionally, as mentioned previously, Glrx may inhibit apoptosis signaling via NF-κB activation and Fas inhibition. This, along with new research indicating protein GSylation may be a major contributor to atherosclerosis, suggests Glrx may be useful as a therapeutic target in treating atherosclerosis [50].
4.5. Lipid and Glucose Metabolism
Glrx controls lipid metabolism as we show that Glrx KO mice develop fatty liver, hyperlipidemia, and obesity [17], which are risk factors for CVDs. A significant target molecule is sirtuin-1 (SirT1), an NAD+-dependent histone deacetylase, which is inactivated by GSylation [15]. The expression of lipid metabolism genes was upregulated in the Glrx KO livers, whereas adenoviral Glrx replenishment restored SirT1 activity, suppressed lipid metabolism genes and liver steatosis [17]. In humans, protein GSylation was increased, correlating with steatohepatitis, in pediatric patients with NAFLD [113]. Additionally, livers from patients diagnosed with hepatic steatosis preliminarily showed lower Glrx protein and increased GSylated protein expression [17].
Protein GSylation may stimulate adipogenesis by stabilizing the adipogenic transcription factor, CCAAT enhancer-binding protein (C/EBP) β in adipocytes. GSylation of C/EBP β inhibits its interaction with an E3 ubiquitin ligase, thus, inhibits its degradation and activates adipogenesis [114]. In a similar mechanism, GSylation stabilizes HIF-1α, and Glrx can inhibit its activation [23]. HIF-1α activates a variety of downstream genes relating to metabolism. HIF-1 induces glucose transporters and promotes glucose uptake, but also upregulates glycolytic enzymes and enhances anaerobic glycolysis, reducing mitochondrial metabolism. HIF-1 enhances lipogenesis by inducing genes involved fatty acid uptake and synthesis [115]. In mice, HIF-1α upregulation in adipocytes promotes obesity, glucose intolerance, inflammation, and fibrosis, while its deletion shows the opposite effects [116]. HIF-1α-dependent PPARγ activation causes cardiac steatosis and hypertrophy [117]. Taken together, Glrx-induced reversal of GSylation is indicative of a beneficial role in controlling lipid and glucose metabolism. In addition, Glrx stimulates insulin exocytosis in pancreatic β-cells [118].
GSylation of some molecules may not necessarily be harmful to the body. Oxidants activate 5′-adenosine monophosphate-activated protein kinase (AMPK) via GSylation [119,120], which could improve metabolic homeostasis. GSylation inhibits tumor suppressor p53 [121], which may inhibit cell death and protect hearts from ER stress [122]. However, diet-induced diabetes in Glrx KO mice enhanced pathological phenotype in the liver and the heart. We showed that inhibition of SirT1 by GSylation increased acetylated-p53, which can activate p53 and promote cell death [17]. There may be a sort of hierarchy in vivo that oxidants control signaling by GSylation.
The role of Glrx2 on metabolism is more complicated. Glrx2 KO mice worsened high-fat diet-induced insulin resistance and weight gain [123] and developed cardiac hypertrophy and hypertension with impaired mitochondrial ATP production [61]. However, heterozygous Glrx2+/− mice have attenuated high-fat diet-induced weight gain and hyperlipidemia [124]. These results likely are a result of the different mouse background used. In addition, neither of these studies used reconstitution of Glrx2 to confirm that this was the sole etiology of the phenomena.
5. Summary and Translational Application
Several clinical studies have investigated the correlation between GSH levels and a variety of CVDs. Decreased levels of GSH have been observed after myocardial infarction and stroke [125], type II diabetes [126], as well as various heart transplant surgeries [127]. Moreover, some studies observed that CVD is correlated with low ratios of GSH:GSSG, including in patients with hypertension [128], type II diabetes, or coronary heart disease [129]. A study involving 134 CVD patients and 435 healthy control subjects revealed that blood plasma GSH levels were significantly lower in the CVD patients. The relationship between low plasma GSH levels and increased risk for CVD was observed for a variety of CVD types [125]. Similar results were detected in patients with coronary heart disease in a study on 425 coronary heart disease patients and 225 healthy control subjects [129]. Another study observed that in comparison to healthy control individuals, patients with type II diabetes mellitus have a significant two-fold decrease in the GSH levels of both red blood cells and blood plasma, as well as a three-fold decrease in the GSH levels of monocytes [126]. Since Glrx uses GSH (as well as GSSG reductase) as a co-factor, lower GSH:GSSG may limit Glrx activity, resulting in effects similar to Glrx deficiency. For this reason, therapeutic Glrx administration may need concomitant GSH supply.
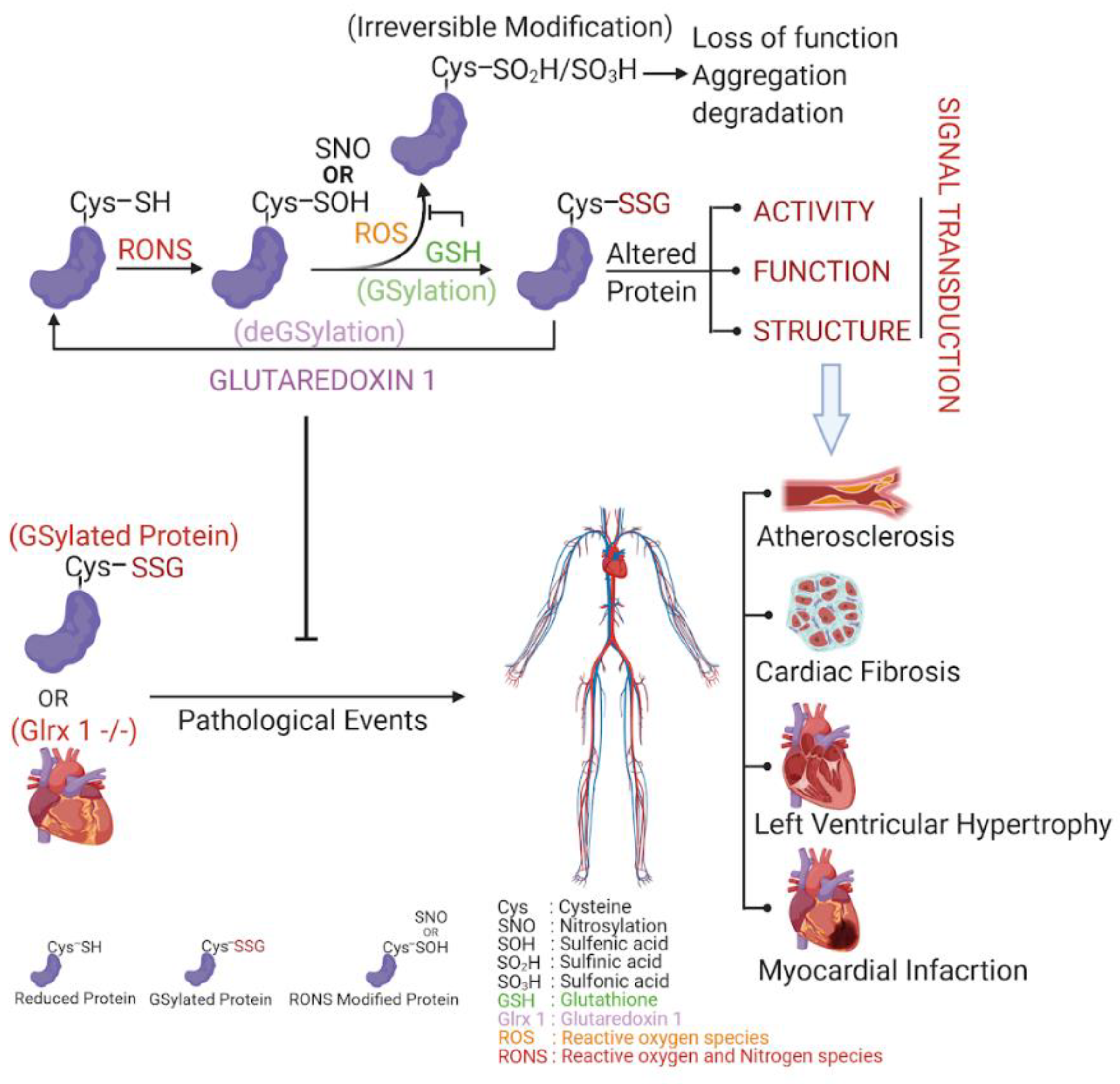
While not many studies have researched Glrxs in the human heart, one study has shown that low levels of Glrx2 appear to be correlated with myocardial infarction, left ventricular hypertrophy, as well as fibrosis [62]. Although there have been fewer studies in humans of Glrx than GSH, one notable study examined the localization of Glrx within human coronary arteries. It was discovered that in nonatherosclerotic coronary arteries, Glrx was expressed in smooth muscle cells, fibroblasts, and endothelial cells, whereas macrophages were observed to have highly expressed Glrx in atherosclerotic lesions. The same study concluded that the generation of ROS within cultured human coronary artery smooth muscle cells was correlated with increased Glrx expression, implicating that Glrx could play a role in atherosclerosis due to its antioxidant effect [130]. Clinical studies have also shown that basal plasma Glrx level is significantly lower in pre-cardiac surgery patients than in healthy control patients [131]. Decreased plasma Glrx in CVD patients could be due to the long-term increased level of oxidative stress associated with the pathology; however, the mechanism of decreased plasma Glrx in CVD patients is to be determined (Figure 2).
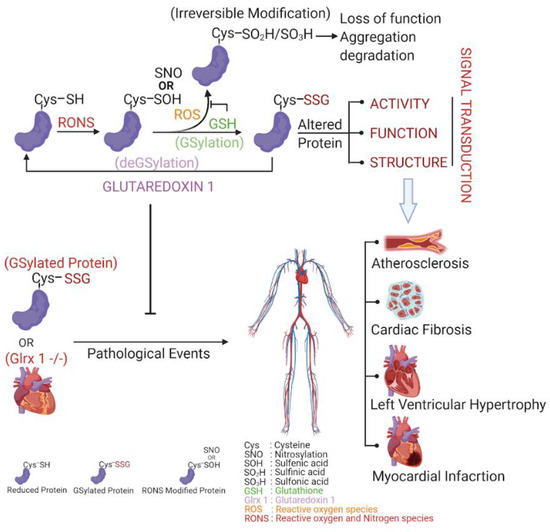
Figure 2.
GSylation, deGSylation and its pathological events. Protein cysteines are readily oxidized by RONS as reversible S-OH or S-NO. While these modifications are unstable/short lived, they are prone to irreversible modifications like HSO2/HSO3. The cell’s reducing environment tries to protect these cysteines from irreversible modifications. GSH, being one of the most abundant reductants of cells, protects protein cysteines by making GSH adducts through a process termed GSylation. While GSylation can alter the function, structure, and activities of proteins which affects signal transduction, Glrx 1 can reduce proteins by specifically removing GSH adducts called deGSylation. Hence, GSH and Glrx 1 maintains GSylation and deGSylation homeostasis in cells. Accumulation of GSylated proteins due to altered cell signaling or Glrx 1 insufficiency could induce pathological events like atherosclerosis, cardiac fibrosis, left ventricular hypertrophy, and myocardial infarction, etc.
In summary, Glrx protects cardiomyocytes and endothelial cells from acute oxidative stress-induced apoptosis, and also may prevent cardiometabolic dysfunction, suggesting its beneficial effects and potential therapeutic use for CVDs. While there have not been clinical trials testing Glrx as a therapeutic agent in CVD, advances in biological technologies such as gene therapy [132] and gene editing (e.g., CRISPR) [133], as well clinical Glrx administration as therapy for lung fibrosis [18], indicate potential going forward [134]. However, Glrx controls the fine balance of redox homeostasis and likely regulates different signaling pathways depending on the pathology. Further studies are required before applying conclusions from mice to humans. As displayed in this review, an ever-growing body of work implicates Glrx as a promising avenue for further research in the field of cardiovascular biology.
Author Contributions
Conception and design: S.H.M.R., M.B., R.M., M.M.B. Writing: M.B., S.H.M.R., M.M.B., R.M. Editing and expert comments R.M., M.M.B., S.H.M.R., M.B., D.R.P., N.M.H., Y.T., I.L. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by NIH grants R01 D K103750, R01 HL133013, R03 AG051857 and NIH CTSI award 1UL1TR001430, and the American Heart Association “Grant in Aid” 16GRNT27660006. The article contents are solely the responsibility of the authors and do not necessarily represent the official views of the awarding offices.
Conflicts of Interest
The authors declare that they have no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Abbreviations
| GSylation | glutathionylation |
| GSH | glutathione |
| CVD | cardiovascular disease |
| Glrx | glutaredoxin |
References
- Agha, M.; Agha, R. The rising prevalence of obesity. Int. J. Surg. Oncol. 2017, 2, e17. [Google Scholar]
- Sturm, R.; Hattori, A. Morbid obesity rates continue to rise rapidly in the United States. Int. J. Obes. 2013, 37, 889–891. [Google Scholar] [CrossRef] [PubMed]
- Pagidipati, N.J.; Gaziano, T.A. Estimating Deaths from Cardiovascular Disease: A Review of Global Methodologies of Mortality Measurement. Circulation 2013, 127, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Csányi, G.F., Jr. Oxidative Stress in Cardiovascular Disease. Int. J. Mol. Sci. 2014, 15, 6002–6008. [Google Scholar] [PubMed]
- Elahi, M.M.; Kong, Y.X.; Matata, B.M. Oxidative Stress as a Mediator of Cardiovascular Disease. Oxidative Med. Cell. Longev. 2009, 2, 259–269. [Google Scholar] [CrossRef]
- Mashamaite, L.N.; Rohwer, J.M.; Pillay, C.S. The glutaredoxin mono- and di-thiol mechanisms for deglutathionylation are functionally equivalent: Implications for redox systems biology. Biosci. Rep. 2015, 35, e00173. [Google Scholar] [CrossRef]
- Madamanchi, N.R.; Vendrov, A.; Runge, M.S. Oxidative Stress and Vascular Disease. Arterioscler. Thromb. Vasc. Biol. 2005, 25, 29–38. [Google Scholar] [CrossRef]
- Forman, H.J.; Zhang, H.; Rinna, A. Glutathione: Overview of its protective roles, measurement, and biosynthesis. Mol. Asp. Med. 2009, 30, 1–12. [Google Scholar]
- Miller, O.G.; Behring, J.B.; Siedlak, S.L.; Jiang, S.; Matsui, R.; Bachschmid, M.M.; Zhu, X.; Mieyal, J.J. Upregulation of Glutaredoxin-1 Activates Microglia and Promotes Neurodegeneration: Implications for Parkinson’s Disease. Antioxid. Redox Signal. 2016, 25, 967–982. [Google Scholar] [CrossRef]
- Kenchappa, R.S.; Diwakar, L.; Annepu, J.; Ravindranath, V. Estrogen and neuroprotection: Higher constitutive expression of glutaredoxin in female mice offers protection against MPTP-mediated neurodegeneration. FASEB J. 2004, 18, 1102–1104. [Google Scholar] [CrossRef]
- Durgadoss, L.; Nidadavolu, P.; Valli, R.K.; Saeed, U.; Mishra, M.; Seth, P.; Ravindranath, V. Redox modification of Akt mediated by the dopaminergic neurotoxin MPTP, in mouse midbrain, leads to down-regulation of pAkt. FASEB J. 2012, 26, 1473–1483. [Google Scholar] [CrossRef] [PubMed]
- Lou, M.F. Redox regulation in the lens. Prog. Retin. Eye Res. 2003, 22, 657–682. [Google Scholar] [CrossRef]
- Liu, X.; Jann, J.; Xavier, C.; Wu, H. Glutaredoxin 1 (Grx1) Protects Human Retinal Pigment Epithelial Cells From Oxidative Damage by Preventing AKT Glutathionylation. Investig. Ophthalmol. Vis. Sci. 2015, 56, 2821–2832. [Google Scholar] [CrossRef] [PubMed]
- Shelton, M.D.; Kern, T.S.; Mieyal, J.J. Glutaredoxin regulates nuclear factor kappa-B and intercellular adhesion molecule in Müller cells: Model of diabetic retinopathy. J. Biol. Chem. 2007, 282, 12467–12474. [Google Scholar] [CrossRef]
- Shao, D.; Fry, J.L.; Han, J.; Hou, X.; Pimentel, D.R.; Matsui, R.; Cohen, R.A.; Bachschmid, M.M. A redox-resistant sirtuin-1 mutant protects against hepatic metabolic and oxidant stress. J. Biol. Chem. 2014, 289, 7293–7306. [Google Scholar] [CrossRef]
- Zee, R.S.; Yoo, C.B.; Pimentel, D.R.; Perlman, D.H.; Burgoyne, J.R.; Hou, X.; McComb, M.E.; Costello, C.E.; Cohen, R.A.; Bachschmid, M.M. Redox regulation of sirtuin-1 by S-glutathiolation. Antioxid. Redox Signal. 2010, 13, 1023–1032. [Google Scholar] [CrossRef]
- Shao, D.; Han, J.; Hou, X.; Fry, J.; Behring, J.B.; Seta, F.; Long, M.T.; Roy, H.K.; Cohen, R.A.; Matsui, R.; et al. Glutaredoxin-1 Deficiency Causes Fatty Liver and Dyslipidemia by Inhibiting Sirtuin-1. Antioxid. Redox Signal. 2017, 27, 313–327. [Google Scholar] [CrossRef]
- Anathy, V.; Lahue, K.G.; Chapman, D.G.; Chia, S.B.; Casey, D.T.; Aboushousha, R.; van der Velden, J.L.J.; Elko, E.; Hoffman, S.M.; McMillan, D.H.; et al. Reducing protein oxidation reverses lung fibrosis. Nat. Med. 2018, 24, 1128–1135. [Google Scholar] [CrossRef]
- Anathy, V.; Aesif, S.W.; Hoffman, S.M.; Bement, J.L.; Guala, A.S.; Lahue, K.G.; Leclair, L.W.; Suratt, B.T.; Cool, C.D.; Wargo, M.J.; et al. Glutaredoxin-1 attenuates S-glutathionylation of the death receptor fas and decreases resolution of Pseudomonas aeruginosa pneumonia. Am. J. Respir. Crit. Care Med. 2014, 189, 463–474. [Google Scholar] [CrossRef]
- Lekli, I.; Mukherjee, S.; Ray, D.; Gurusamy, N.; Kim, Y.H.; Tosaki, A.; Engelman, R.M.; Ho, Y.-S.; Das, D.K. Functional recovery of diabetic mouse hearts by glutaredoxin-1 gene therapy: Role of Akt-FoxO-signaling network. Gene Ther. 2010, 17, 478–485. [Google Scholar] [CrossRef]
- Inadomi, C.; Murata, H.; Ihara, Y.; Goto, S.; Urata, Y.; Yodoi, J.; Kondo, T.; Sumikawa, K. Overexpression of glutaredoxin protects cardiomyocytes against nitric oxide-induced apoptosis with suppressing the S-nitrosylation of proteins and nuclear translocation of GAPDH. Biochem. Biophys. Res. Commun. 2012, 425, 656–661. [Google Scholar] [CrossRef] [PubMed]
- Matsui, R.; Watanabe, Y.; Murdoch, C.E. Redox regulation of ischemic limb neovascularization—What we have learned from animal studies. Redox Biol. 2017, 12, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Murdoch, C.E.; Sano, S.; Ido, Y.; Bachschmid, M.M.; Cohen, R.A.; Matsui, R. Glutathione adducts induced by ischemia and deletion of glutaredoxin-1 stabilize HIF-1α and improve limb revascularization. Proc. Natl. Acad. Sci. USA 2016, 113, 6011–6016. [Google Scholar] [CrossRef] [PubMed]
- Murdoch, C.E.; Shuler, M.; Haeussler, D.J.F.; Kikuchi, R.; Bearelly, P.; Han, J.; Watanabe, Y.; Fuster, J.J.; Walsh, K.; Ho, Y.-S.; et al. Glutaredoxin-1 up-regulation induces soluble vascular endothelial growth factor receptor 1, attenuating post-ischemia limb revascularization. J. Biol. Chem. 2014, 289, 8633–8644. [Google Scholar] [CrossRef]
- Meister, A. Glutathione metabolism and its selective modification. J. Biol. Chem. 1988, 263, 17205–17208. [Google Scholar]
- Lu, S.C. Regulation of glutathione synthesis. Mol. Asp. Med. 2009, 30, 42–59. [Google Scholar] [CrossRef]
- Halliwell, B.; Gutteridge, J.M.C. Free Radicals in Biology and Medicine; Oxford University Press: Oxford, UK, 2015. [Google Scholar]
- Meister, A. Biosynthesis and functions of glutathione, an essential biofactor. J. Nutr. Sci. Vitaminol. 1992, 38, 1–6. [Google Scholar] [CrossRef]
- Dagnell, M.; Cheng, Q.; Rizvi, S.H.M.; Pace, P.E.; Boivin, B.; Winterbourn, C.C.; Arnér, E.S.J. Bicarbonate is essential for protein-tyrosine phosphatase 1B (PTP1B) oxidation and cellular signaling through EGF-triggered phosphorylation cascades. J. Biol. Chem. 2019, 294, 12330–12338. [Google Scholar] [CrossRef]
- Schuppe-Koistinen, I.; Moldéus, P.; Bergman, T.; Cotgreave, I.A. S-thiolation of human endothelial cell glyceraldehyde-3-phosphate dehydrogenase after hydrogen peroxide treatment. Eur. J. Biochem. 1994, 221, 1033–1037. [Google Scholar] [CrossRef]
- Niture, S.K.; Velu, C.S.; Bailey, N.I.; Srivenugopal, K.S. S-thiolation mimicry: Quantitative and kinetic analysis of redox status of protein cysteines by glutathione-affinity chromatography. Arch. Biochem. Biophys. 2005, 444, 174–184. [Google Scholar] [CrossRef]
- Coles, S.J.; Easton, P.; Sharrod, H.; Hutson, S.M.; Hancock, J.; Patel, V.B.; Conway, M.E. S-Nitrosoglutathione inactivation of the mitochondrial and cytosolic BCAT proteins: S-nitrosation and S-thiolation. Biochemistry 2009, 48, 645–656. [Google Scholar] [CrossRef] [PubMed]
- Mohr, S.; Hallak, H.; de Boitte, A.; Lapetina, E.G.; Brüne, B. Nitric oxide-induced S-glutathionylation and inactivation of glyceraldehyde-3-phosphate dehydrogenase. J. Biol. Chem. 1999, 274, 9427–9430. [Google Scholar] [CrossRef] [PubMed]
- Giustarini, D.; Milzani, A.; Aldini, G.; Carini, M.; Rossi, R.; Dalle-Donne, I. S-nitrosation versus S-glutathionylation of protein sulfhydryl groups by S-nitrosoglutathione. Antioxid. Redox Signal. 2005, 7, 930–939. [Google Scholar] [CrossRef] [PubMed]
- Sies, H. Oxidative stress: Oxidants and antioxidants. Exp. Physiol. 1997, 82, 291–295. [Google Scholar] [CrossRef]
- Valko, M.; Leibfritz, D.; Moncol, J.; Cronin, M.T.D.; Mazur, M.; Telser, J. Free radicals and antioxidants in normal physiological functions and human disease. Int. J. Biochem. Cell Biol. 2007, 39, 44–84. [Google Scholar] [CrossRef]
- Di Meo, S.; Reed, T.T.; Venditti, P.; Victor, V.M. Role of ROS and RNS Sources in Physiological and Pathological Conditions. Oxid. Med. Cell. Longev. 2016, 2016. [Google Scholar] [CrossRef]
- Tousoulis, D.; Kampoli, A.-M.; Papageorgiou, C.T.N.; Stefanadis, C. The Role of Nitric Oxide on Endothelial Function. Curr. Vasc. Pharmacol. 2012, 10, 4–18. [Google Scholar] [CrossRef]
- Donald, M.; Lloyd-Jones, M.D.; Kenneth, D.; Bloch, M.D. The vascular biology of nitric oxide and its role in atherogenesis. Annu. Rev. Med. 1996, 47, 365–375. [Google Scholar]
- Sharma, J.N.; Al-Omran, A.; Parvathy, S.S. Role of nitric oxide in inflammatory diseases. Inflammopharmacology 2007, 15, 252–259. [Google Scholar] [CrossRef]
- Li, S.; Yan, T.; Yang, J.Q.; Oberley, T.D.; Oberley, L.W. The role of cellular glutathione peroxidase redox regulation in the suppression of tumor cell growth by manganese superoxide dismutase. Cancer Res. 2000, 60, 3927–3939. [Google Scholar]
- Ho, Y.-S.; Xiong, Y.; Ho, D.S.; Gao, J.; Chua, B.H.L.; Pai, H.; Mieyal, J.J. Targeted disruption of the glutaredoxin 1 gene does not sensitize adult mice to tissue injury induced by ischemia/reperfusion and hyperoxia. Free Radic. Biol. Med. 2007, 43, 1299–1312. [Google Scholar] [CrossRef]
- Schafer, F.Q.; Buettner, G.R. Redox environment of the cell as viewed through the redox state of the glutathione disulfide/glutathione couple. Free Radic. Biol. Med. 2001, 30, 1191–1212. [Google Scholar] [CrossRef]
- Rebrin, I.; Sohal, R.S. Comparison of thiol redox state of mitochondria and homogenates of various tissues between two strains of mice with different longevities. Exp. Gerontol. 2004, 39, 1513–1519. [Google Scholar] [CrossRef]
- Zitka, O.; Skalickova, S.; Gumulec, J.; Masarik, M.; Adam, V.; Hubalek, J.; Trnkova, L.; Kruseova, J.; Eckschlager, T.; Kizek, R. Redox status expressed as GSH:GSSG ratio as a marker for oxidative stress in paediatric tumour patients. Oncol. Lett. 2012, 4, 1247–1253. [Google Scholar] [CrossRef]
- Dalle-Donne, I.; Rossi, R.; Giustarini, D.; Colombo, R.; Milzani, A. S-glutathionylation in protein redox regulation. Free Radic. Biol. Med. 2007, 43, 883–898. [Google Scholar] [CrossRef]
- Ravichandran, V.; Seres, T.; Moriguchi, T.; Thomas, J.A.; Johnston, R.B., Jr. S-thiolation of glyceraldehyde-3-phosphate dehydrogenase induced by the phagocytosis-associated respiratory burst in blood monocytes. J. Biol. Chem. 1994, 269, 25010–25015. [Google Scholar] [PubMed]
- Fratelli, M.; Demol, H.; Puype, M.; Casagrande, S.; Eberini, I.; Salmona, M.; Bonetto, V.; Mengozzi, M.; Duffieux, F.; Miclet, E.; et al. Identification by redox proteomics of glutathionylated proteins in oxidatively stressed human T lymphocytes. Proc. Natl. Acad. Sci. USA 2002, 99, 3505–3510. [Google Scholar] [CrossRef] [PubMed]
- Xiong, Y.; Uys, J.D.; Tew, K.D.; Townsend, D.M. S-glutathionylation: From molecular mechanisms to health outcomes. Antioxid. Redox Signal. 2011, 15, 233–270. [Google Scholar] [CrossRef] [PubMed]
- Pastore, A.; Piemonte, F. Protein glutathionylation in cardiovascular diseases. Int. J. Mol. Sci. 2013, 14, 20845–20876. [Google Scholar] [CrossRef] [PubMed]
- VanHecke, G.C.; Abeywardana, M.Y.; Ahn, Y.-H. Proteomic Identification of Protein Glutathionylation in Cardiomyocytes. J. Proteome Res. 2019, 18, 1806–1818. [Google Scholar] [CrossRef] [PubMed]
- Lillig, C.H.; Berndt, C.; Holmgren, A. Glutaredoxin systems. Biochim. Biophys. Acta 2008, 1780, 1304–1317. [Google Scholar] [CrossRef] [PubMed]
- Eklund, H.; Cambillau, C.; Sjöberg, B.M.; Holmgren, A.; Jörnvall, H.; Höög, J.O.; Brändén, C.I. Conformational and functional similarities between glutaredoxin and thioredoxins. EMBO J. 1984, 3, 1443–1449. [Google Scholar] [CrossRef] [PubMed]
- Mieyal, J.J.; Gallogly, M.M.; Qanungo, S.; Sabens, E.A.; Shelton, M.D. Molecular mechanisms and clinical implications of reversible protein S-glutathionylation. Antioxid. Redox Signal. 2008, 10, 1941–1988. [Google Scholar] [CrossRef] [PubMed]
- Cheng, N.-H.; Zhang, W.; Chen, W.-Q.; Jin, J.; Cui, X.; Butte, N.F.; Chan, L.; Hirschi, K.D. A mammalian monothiol glutaredoxin, Grx3, is critical for cell cycle progression during embryogenesis. FEBS J. 2011, 278, 2525–2539. [Google Scholar] [CrossRef]
- Sagemark, J.; Elgán, T.H.; Bürglin, T.R.; Johansson, C.; Holmgren, A.; Berndt, K.D. Redox properties and evolution of human glutaredoxins. Proteins Struct. Funct. Bioinform. 2007, 68, 879–892. [Google Scholar] [CrossRef] [PubMed]
- Herrero, E.; de la Torre-Ruiz, M.A. Monothiol glutaredoxins: A common domain for multiple functions. Cell. Mol. Life Sci. 2007, 64, 1518–1530. [Google Scholar] [CrossRef]
- Pimentel, D.R.; Adachi, T.; Ido, Y.; Heibeck, T.; Jiang, B.; Lee, Y.; Melendez, J.A.; Cohen, R.A.; Colucci, W.S. Strain-stimulated hypertrophy in cardiac myocytes is mediated by reactive oxygen species-dependent Ras S-glutathiolation. J. Mol. Cell. Cardiol. 2006, 41, 613–622. [Google Scholar] [CrossRef]
- Han, J.; Weisbrod, R.M.; Shao, D.; Watanabe, Y.; Yin, X.; Bachschmid, M.M.; Seta, F.; Janssen-Heininger, Y.M.W.; Matsui, R.; Zang, M.; et al. The redox mechanism for vascular barrier dysfunction associated with metabolic disorders: Glutathionylation of Rac1 in endothelial cells. Redox Biol. 2016, 9, 306–319. [Google Scholar] [CrossRef]
- Wang, J.; Pan, S.; Berk, B.C. Glutaredoxin Mediates Akt and eNOS Activation by Flow in a Glutathione Reductase-Dependent Manner. Arterioscler. Thromb. Vasc. Biol. 2007, 27, 1283–1288. [Google Scholar] [CrossRef]
- Mailloux, R.J.; Xuan, J.Y.; McBride, S.; Maharsy, W.; Thorn, S.; Holterman, C.E.; Kennedy, C.R.J.; Rippstein, P.; deKemp, R.; da Silva, J.; et al. Glutaredoxin-2 is required to control oxidative phosphorylation in cardiac muscle by mediating deglutathionylation reactions. J. Biol. Chem. 2014, 289, 14812–14828. [Google Scholar] [CrossRef]
- Kanaan, G.N.; Ichim, B.; Gharibeh, L.; Maharsy, W.; Patten, D.A.; Xuan, J.Y.; Reunov, A.; Marshall, P.; Veinot, J.; Menzies, K.; et al. Glutaredoxin-2 controls cardiac mitochondrial dynamics and energetics in mice, and protects against human cardiac pathologies. Redox Biol. 2018, 14, 509–521. [Google Scholar] [CrossRef] [PubMed]
- Donelson, J.; Wang, Q.; Monroe, T.O.; Jiang, X.; Zhou, J.; Yu, H.; Mo, Q.; Sun, Q.; Marini, J.C.; Wang, X.; et al. Cardiac-specific ablation of glutaredoxin 3 leads to cardiac hypertrophy and heart failure. Physiol. Rep. 2019, 7, e14071. [Google Scholar] [CrossRef] [PubMed]
- Frey, A.G.; Palenchar, D.J.; Wildemann, J.D.; Philpott, C.C. A Glutaredoxin·BolA Complex Serves as an Iron-Sulfur Cluster Chaperone for the Cytosolic Cluster Assembly Machinery. J. Biol. Chem. 2016, 291, 22344–22356. [Google Scholar] [CrossRef] [PubMed]
- Johansson, C.; Roos, A.K.; Montano, S.J.; Sengupta, R.; Filippakopoulos, P.; Guo, K.; von Delft, F.; Holmgren, A.; Oppermann, U.; Kavanagh, K.L. The crystal structure of human GLRX5: Iron-sulfur cluster co-ordination, tetrameric assembly and monomer activity. Biochem. J. 2011, 433, 303–311. [Google Scholar] [CrossRef]
- Haunhorst, P.; Berndt, C.; Eitner, S.; Godoy, J.R.; Lillig, C.H. Characterization of the human monothiol glutaredoxin 3 (PICOT) as iron–sulfur protein. Biochem. Biophys. Res. Commun. 2010, 394, 372–376. [Google Scholar] [CrossRef]
- Ye, H.; Rouault, T.A. Human Iron−Sulfur Cluster Assembly, Cellular Iron Homeostasis, and Disease. Biochemistry 2010, 49, 4945–4956. [Google Scholar] [CrossRef]
- Rouault, T.A. Biogenesis of iron-sulfur clusters in mammalian cells: New insights and relevance to human disease. Dis. Model. Mech. 2012, 5, 155–164. [Google Scholar] [CrossRef]
- Matsui, R.; Ferran, B.; Oh, A.; Croteau, D.; Shao, D.; Han, J.; Pimentel, D.R.; Bachschmid, M.M. Redox Regulation via Glutaredoxin-1 and Protein S-Glutathionylation. Antioxid. Redox Signal. 2020, 32, 677–700. [Google Scholar] [CrossRef]
- Pai, H.V.; Starke, D.W.; Lesnefsky, E.J.; Hoppel, C.L.; Mieyal, J.J. What is the functional significance of the unique location of glutaredoxin 1 (GRx1) in the intermembrane space of mitochondria? Antioxid. Redox Signal. 2007, 9, 2027–2033. [Google Scholar] [CrossRef]
- Lind, C.; Gerdes, R.; Schuppe-Koistinen, I.; Cotgreave, I.A. Studies on the mechanism of oxidative modification of human glyceraldehyde-3-phosphate dehydrogenase by glutathione: Catalysis by glutaredoxin. Biochem. Biophys. Res. Commun. 1998, 247, 481–486. [Google Scholar] [CrossRef]
- Pineda-Molina, E.; Klatt, P.; Vázquez, J.; Marina, A.; García de Lacoba, M.; Pérez-Sala, D.; Lamas, S. Glutathionylation of the p50 subunit of NF-kappaB: A mechanism for redox-induced inhibition of DNA binding. Biochemistry 2001, 40, 14134–14142. [Google Scholar] [CrossRef] [PubMed]
- Reynaert, N.L.; van der Vliet, A.; Guala, A.S.; McGovern, T.; Hristova, M.; Pantano, C.; Heintz, N.H.; Heim, J.; Ho, Y.-S.; Matthews, D.E.; et al. Dynamic redox control of NF-kappaB through glutaredoxin-regulated S-glutathionylation of inhibitory kappaB kinase beta. Proc. Natl. Acad. Sci. USA 2006, 103, 13086–13091. [Google Scholar] [CrossRef]
- Barrett, W.C.; DeGnore, J.P.; König, S.; Fales, H.M.; Keng, Y.F.; Zhang, Z.Y.; Yim, M.B.; Chock, P.B. Regulation of PTP1B via glutathionylation of the active site cysteine 215. Biochemistry 1999, 38, 6699–6705. [Google Scholar] [CrossRef] [PubMed]
- Klatt, P.; Molina, E.P.; Lacoba, M.G.; Alicia Padilla, C.; Martínez-Galisteo, E.; Barcena, J.; Lamas, S. Redox regulation of c-Jun DNA binding by reversible S-glutathiolation. FASEB J. 1999, 13, 1481–1490. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.; Jones, A.D.; Cross, C.E.; Wong, P.S.; Van Der Vliet, A. Inactivation of creatine kinase by S-glutathionylation of the active-site cysteine residue. Biochem. J. 2000, 347 Pt 3, 821–827. [Google Scholar] [CrossRef]
- Wang, J.; Boja, E.S.; Tan, W.; Tekle, E.; Fales, H.M.; English, S.; Mieyal, J.J.; Chock, P.B. Reversible glutathionylation regulates actin polymerization in A431 cells. J. Biol. Chem. 2001, 276, 47763–47766. [Google Scholar] [CrossRef]
- Davis, D.A.; Newcomb, F.M.; Starke, D.W.; Ott, D.E.; Mieyal, J.J.; Yarchoan, R. Thioltransferase (glutaredoxin) is detected within HIV-1 and can regulate the activity of glutathionylated HIV-1 protease in vitro. J. Biol. Chem. 1997, 272, 25935–25940. [Google Scholar] [CrossRef] [PubMed]
- Murata, H.; Ihara, Y.; Nakamura, H.; Yodoi, J.; Sumikawa, K.; Kondo, T. Glutaredoxin exerts an antiapoptotic effect by regulating the redox state of Akt. J. Biol. Chem. 2003, 278, 50226–50233. [Google Scholar] [CrossRef]
- Chen, C.-A.; Wang, T.-Y.; Varadharaj, S.; Reyes, L.A.; Hemann, C.; Talukder, M.A.H.; Chen, Y.-R.; Druhan, L.J.; Zweier, J.L. S-glutathionylation uncouples eNOS and regulates its cellular and vascular function. Nature 2010, 468, 1115–1118. [Google Scholar] [CrossRef]
- Adachi, T.; Weisbrod, R.M.; Pimentel, D.R.; Ying, J.; Sharov, V.S.; Schöneich, C.; Cohen, R.A. S-Glutathiolation by peroxynitrite activates SERCA during arterial relaxation by nitric oxide. Nat. Med. 2004, 10, 1200–1207. [Google Scholar] [CrossRef]
- Eaton, P.; Wright, N.; Hearse, D.J.; Shattock, M.J. Glyceraldehyde phosphate dehydrogenase oxidation during cardiac ischemia and reperfusion. J. Mol. Cell. Cardiol. 2002, 34, 1549–1560. [Google Scholar] [CrossRef]
- Gallogly, M.M.; Starke, D.W.; Mieyal, J.J. Mechanistic and kinetic details of catalysis of thiol-disulfide exchange by glutaredoxins and potential mechanisms of regulation. Antioxid. Redox Signal. 2009, 11, 1059–1081. [Google Scholar] [CrossRef] [PubMed]
- Anathy, V.; Aesif, S.W.; Guala, A.S.; Havermans, M.; Reynaert, N.L.; Ho, Y.-S.; Budd, R.C.; Janssen-Heininger, Y.M.W. Redox amplification of apoptosis by caspase-dependent cleavage of glutaredoxin 1 and S-glutathionylation of Fas. J. Cell Biol. 2009, 184, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Song, J.J.; Rhee, J.G.; Suntharalingam, M.; Walsh, S.A.; Spitz, D.R.; Lee, Y.J. Role of glutaredoxin in metabolic oxidative stress. Glutaredoxin as a sensor of oxidative stress mediated by H2O2. J. Biol. Chem. 2002, 277, 46566–46575. [Google Scholar] [CrossRef]
- Song, J.J.; Lee, Y.J. Differential role of glutaredoxin and thioredoxin in metabolic oxidative stress-induced activation of apoptosis signal-regulating kinase 1. Biochem. J. 2003, 373, 845–853. [Google Scholar] [CrossRef] [PubMed]
- Adluri, R.S.; Thirunavukkarasu, M.; Zhan, L.; Dunna, N.R.; Akita, Y.; Selvaraju, V.; Otani, H.; Sanchez, J.A.; Ho, Y.-S.; Maulik, N. Glutaredoxin-1 overexpression enhances neovascularization and diminishes ventricular remodeling in chronic myocardial infarction. PLoS ONE 2012, 7, e34790. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.C.; Ogut, O. Decline of contractility during ischemia-reperfusion injury: Actin glutathionylation and its effect on allosteric interaction with tropomyosin. Am. J. Physiol. Cell Physiol. 2006, 290, C719–C727. [Google Scholar] [CrossRef]
- Rizvi, S.; Shao, D.; Pimentel, D.; Matsui, R.; Bachschmid, M. S-glutathionylation of Glyceraldehyde 3-Phosphate Dehydrogenase Regulates Sirtuin-1 Function through Trans-glutathionylation: Implication of Glutaredoxin-1. Free Radic. Biol. Med. 2019, 145, S37. [Google Scholar]
- Travasso, R.D.M.; Sampaio Dos Aidos, F.; Bayani, A.; Abranches, P.; Salvador, A. Localized redox relays as a privileged mode of cytoplasmic hydrogen peroxide signaling. Redox Biol. 2017, 12, 233–245. [Google Scholar] [CrossRef]
- Petrushanko, I.Y.; Yakushev, S.; Mitkevich, V.A.; Kamanina, Y.V.; Ziganshin, R.H.; Meng, X.; Anashkina, A.A.; Makhro, A.; Lopina, O.D.; Gassmann, M.; et al. S-Glutathionylation of the Na,K-ATPase Catalytic α Subunit Is a Determinant of the Enzyme Redox Sensitivity. J. Biol. Chem. 2012, 287, 32195–32205. [Google Scholar] [CrossRef] [PubMed]
- Poluektov, Y.M.; Petrushanko, I.Y.; Undrovinas, N.A.; Lakunina, V.A.; Khapchaev, A.Y.; Kapelko, V.I.; Abramov, A.A.; Lakomkin, V.L.; Novikov, M.S.; Shirinsky, V.P.; et al. Glutathione-related substances maintain cardiomyocyte contractile function in hypoxic conditions. Sci. Rep. 2019, 9, 4872. [Google Scholar] [CrossRef]
- Zweier, J.L.; Chen, C.-A.; Druhan, L.J. S-glutathionylation reshapes our understanding of endothelial nitric oxide synthase uncoupling and nitric oxide/reactive oxygen species-mediated signaling. Antioxid. Redox Signal. 2011, 14, 1769–1775. [Google Scholar] [CrossRef] [PubMed]
- Rochette, L.; Lorin, J.; Zeller, M.; Guilland, J.-C.; Lorgis, L.; Cottin, Y.; Vergely, C. Nitric oxide synthase inhibition and oxidative stress in cardiovascular diseases: Possible therapeutic targets? Pharmacol. Ther. 2013, 140, 239–257. [Google Scholar] [CrossRef]
- Chen, C.-A.; De Pascali, F.; Basye, A.; Hemann, C.; Zweier, J.L. Redox modulation of endothelial nitric oxide synthase by glutaredoxin-1 through reversible oxidative post-translational modification. Biochemistry 2013, 52, 6712–6723. [Google Scholar] [CrossRef]
- Evangelista, A.M.; Thompson, M.D.; Weisbrod, R.M.; Pimental, D.R.; Tong, X.; Bolotina, V.M.; Cohen, R.A. Redox regulation of SERCA2 is required for vascular endothelial growth factor-induced signaling and endothelial cell migration. Antioxid. Redox Signal. 2012, 17, 1099–1108. [Google Scholar] [CrossRef] [PubMed]
- Ying, J.; Sharov, V.; Xu, S.; Jiang, B.; Gerrity, R.; Schöneich, C.; Cohen, R.A. Cysteine-674 oxidation and degradation of sarcoplasmic reticulum Ca(2+) ATPase in diabetic pig aorta. Free Radic. Biol. Med. 2008, 45, 756–762. [Google Scholar] [CrossRef]
- Berenji, K.; Drazner, M.H.; Rothermel, B.A.; Hill, J.A. Does load-induced ventricular hypertrophy progress to systolic heart failure? Am. J. Physiol. Heart Circ. Physiol. 2005, 289, H8–H16. [Google Scholar] [CrossRef]
- Haider, A.W.; Larson, M.G.; Benjamin, E.J.; Levy, D. Increased left ventricular mass and hypertrophy are associated with increased risk for sudden death. J. Am. Coll. Cardiol. 1998, 32, 1454–1459. [Google Scholar] [CrossRef]
- Heineke, J.; Molkentin, J.D. Regulation of cardiac hypertrophy by intracellular signalling pathways. Nat. Rev. Mol. Cell Biol. 2006, 7, 589–600. [Google Scholar] [CrossRef]
- Bachschmid, M.M.; Xu, S.; Maitland-Toolan, K.A.; Ho, Y.-S.; Cohen, R.A.; Matsui, R. Attenuated cardiovascular hypertrophy and oxidant generation in response to angiotensin II infusion in glutaredoxin-1 knockout mice. Free Radic. Biol. Med. 2010, 49, 1221–1229. [Google Scholar] [CrossRef][Green Version]
- Jeong, D.; Kim, J.M.; Cha, H.; Oh, J.G.; Park, J.; Yun, S.-H.; Ju, E.-S.; Jeon, E.-S.; Hajjar, R.J.; Park, W.J. PICOT Attenuates Cardiac Hypertrophy by Disrupting Calcineurin–NFAT Signaling. Circ. Res. 2008, 102, 711–719. [Google Scholar] [PubMed]
- Lusis, A.J. Atherosclerosis. Nature 2000, 407, 233–241. [Google Scholar] [PubMed]
- Ross, R.; Harker, L. Hyperlipidemia and atherosclerosis. Science 1976, 193, 1094–1100. [Google Scholar] [PubMed]
- Wouters, K.; Shiri-Sverdlov, R.; van Gorp, P.J.; van Bilsen, M.; Hofker, M.H. Understanding hyperlipidemia and atherosclerosis: Lessons from genetically modified apoe and ldlr mice. Clin. Chem. Lab. Med. 2005, 43, 470–479. [Google Scholar]
- Griendling, K.K.; FitzGerald, G.A. Oxidative stress and cardiovascular injury: Part II: Animal and human studies. Circulation 2003, 108, 2034–2040. [Google Scholar]
- Fukai, T.; Galis, Z.S.; Meng, X.P.; Parthasarathy, S.; Harrison, D.G. Vascular expression of extracellular superoxide dismutase in atherosclerosis. J. Clin. Investig. 1998, 101, 2101–2111. [Google Scholar]
- Shukla, S.; Rizvi, F.; Raisuddin, S.; Kakkar, P. FoxO proteins’ nuclear retention and BH3-only protein Bim induction evoke mitochondrial dysfunction-mediated apoptosis in berberine-treated HepG2 cells. Free Radic. Biol. Med. 2014, 76, 185–199. [Google Scholar]
- Lei, K.; Davis, R.J. JNK phosphorylation of Bim-related members of the Bcl2 family induces Bax-dependent apoptosis. Proc. Natl. Acad. Sci. USA 2003, 100, 2432–2437. [Google Scholar]
- Corazza, N.; Jakob, S.; Schaer, C.; Frese, S.; Keogh, A.; Stroka, D.; Kassahn, D.; Torgler, R.; Mueller, C.; Schneider, P.; et al. TRAIL receptor-mediated JNK activation and Bim phosphorylation critically regulate Fas-mediated liver damage and lethality. J. Clin. Investig. 2006, 116, 2493–2499. [Google Scholar]
- Nigro, P.; Abe, J.-I.; Berk, B.C. Flow shear stress and atherosclerosis: A matter of site specificity. Antioxid. Redox Signal. 2011, 15, 1405–1414. [Google Scholar]
- Li, Y.; Ren, M.; Wang, X.; Cui, X.; Zhao, H.; Zhao, C.; Zhou, J.; Guo, Y.; Hu, Y.; Yan, C.; et al. Glutaredoxin 1 mediates the protective effect of steady laminar flow on endothelial cells against oxidative stress-induced apoptosis via inhibiting Bim. Sci. Rep. 2017, 7, 15539. [Google Scholar] [CrossRef] [PubMed]
- Piemonte, F.; Petrini, S.; Gaeta, L.M.; Tozzi, G.; Bertini, E.; Devito, R.; Boldrini, R.; Marcellini, M.; Ciacco, E.; Nobili, V. Protein glutathionylation increases in the liver of patients with non-alcoholic fatty liver disease. J. Gastroenterol. Hepatol. 2008, 23, e457–e464. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, Y.; Watanabe, K.; Fujioka, D.; Nakamura, K.; Nakamura, T.; Uematsu, M.; Bachschmid, M.M.; Matsui, R.; Kugiyama, K. Protein S-glutathionylation stimulate adipogenesis by stabilizing C/EBPβ in 3T3L1 cells. FASEB J. 2020, 34, 5827–5837. [Google Scholar] [CrossRef] [PubMed]
- Mylonis, I.; Simos, G.; Paraskeva, E. Hypoxia-Inducible Factors and the Regulation of Lipid Metabolism. Cells 2019, 8, 214. [Google Scholar] [CrossRef] [PubMed]
- Ban, J.-J.; Ruthenborg, R.J.; Cho, K.W.; Kim, J.-W. Regulation of obesity and insulin resistance by hypoxia-inducible factors. Hypoxia (Auckl.) 2014, 2, 171–183. [Google Scholar]
- Krishnan, J.; Suter, M.; Windak, R.; Krebs, T.; Felley, A.; Montessuit, C.; Tokarska-Schlattner, M.; Aasum, E.; Bogdanova, A.; Perriard, E.; et al. Activation of a HIF1alpha-PPARgamma axis underlies the integration of glycolytic and lipid anabolic pathways in pathologic cardiac hypertrophy. Cell Metab. 2009, 9, 512–524. [Google Scholar] [CrossRef]
- Reinbothe, T.M.; Ivarsson, R.; Li, D.-Q.; Niazi, O.; Jing, X.; Zhang, E.; Stenson, L.; Bryborn, U.; Renström, E. Glutaredoxin-1 mediates NADPH-dependent stimulation of calcium-dependent insulin secretion. Mol. Endocrinol. 2009, 23, 893–900. [Google Scholar] [CrossRef]
- Zmijewski, J.W.; Banerjee, S.; Bae, H.; Friggeri, A.; Lazarowski, E.R.; Abraham, E. Exposure to hydrogen peroxide induces oxidation and activation of AMP-activated protein kinase. J. Biol. Chem. 2010, 285, 33154–33164. [Google Scholar] [CrossRef]
- Klaus, A.; Zorman, S.; Berthier, A.; Polge, C.; Ramirez, S.; Michelland, S.; Sève, M.; Vertommen, D.; Rider, M.; Lentze, N.; et al. Glutathione S-transferases interact with AMP-activated protein kinase: Evidence for S-glutathionylation and activation in vitro. PLoS ONE 2013, 8, e62497. [Google Scholar] [CrossRef]
- Velu, C.S.; Niture, S.K.; Doneanu, C.E.; Pattabiraman, N.; Srivenugopal, K.S. Human p53 is inhibited by glutathionylation of cysteines present in the proximal DNA-binding domain during oxidative stress. Biochemistry 2007, 46, 7765–7780. [Google Scholar] [CrossRef]
- Chen, Q.; Thompson, J.; Hu, Y.; Das, A.; Lesnefsky, E.J. Cardiac Specific Knockout of p53 Decreases ER Stress-Induced Mitochondrial Damage. Front. Cardiovasc. Med. 2019, 6, 10. [Google Scholar] [CrossRef]
- Wohua, Z.; Weiming, X. Glutaredoxin 2 (GRX2) deficiency exacerbates high fat diet (HFD)-induced insulin resistance, inflammation and mitochondrial dysfunction in brain injury: A mechanism involving GSK-3β. Biomed. Pharmacother. 2019, 118, 108940. [Google Scholar] [CrossRef]
- Young, A.; Gardiner, D.; Kuksal, N.; Gill, R.; O’Brien, M.; Mailloux, R.J. Deletion of the Glutaredoxin-2 Gene Protects Mice from Diet-Induced Weight Gain, Which Correlates with Increased Mitochondrial Respiration and Proton Leaks in Skeletal Muscle. Antioxid. Redox Signal. 2019, 31, 1272–1288. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, H.; Kiyohara, Y.; Kato, I.; Kitazono, T.; Tanizaki, Y.; Kubo, M.; Ueno, H.; Ibayashi, S.; Fujishima, M.; Iida, M. Relationship Between Plasma Glutathione Levels and Cardiovascular Disease in a Defined Population. Stroke 2004, 35, 2072–2077. [Google Scholar] [CrossRef] [PubMed]
- Lagman, M.; Ly, J.; Saing, T.; Kaur Singh, M.; Vera Tudela, E.; Morris, D.; Chi, P.-T.; Ochoa, C.; Sathananthan, A.; Venketaraman, V. Investigating the causes for decreased levels of glutathione in individuals with type II diabetes. PLoS ONE 2015, 10, e0118436. [Google Scholar] [CrossRef] [PubMed]
- Damy, T.; Kirsch, M.; Khouzami, L.; Caramelle, P.; Le Corvoisier, P.; Roudot-Thoraval, F.; Dubois-Randé, J.-L.; Hittinger, L.; Pavoine, C.; Pecker, F. Glutathione deficiency in cardiac patients is related to the functional status and structural cardiac abnormalities. PLoS ONE 2009, 4, e4871. [Google Scholar] [CrossRef]
- Redón, J.; Oliva, M.R.; Tormos, C.; Giner, V.; Chaves, J.; Iradi, A.; Sáez, G.T. Antioxidant activities and oxidative stress byproducts in human hypertension. Hypertension 2003, 41, 1096–1101. [Google Scholar] [CrossRef]
- Shahid, S.U.; Shabana; Humphries, S. The SNP rs10911021 is associated with oxidative stress in coronary heart disease patients from Pakistan. Lipids Health Dis. 2018, 17, 6. [Google Scholar] [CrossRef]
- Okuda, M.; Inoue, N.; Azumi, H.; Seno, T.; Sumi, Y.; Hirata, K.I.; Kawashima, S.; Hayashi, Y.; Itoh, H.; Yodoi, J.; et al. Expression of glutaredoxin in human coronary arteries: Its potential role in antioxidant protection against atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2001, 21, 1483–1487. [Google Scholar] [CrossRef]
- Nakamura, H.; Vaage, J.; Valen, G.; Padilla, C.A.; Björnstedt, M.; Holmgren, A. Measurements of plasma glutaredoxin and thioredoxin in healthy volunteers and during open-heart surgery. Free Radic. Biol. Med. 1998, 24, 1176–1186. [Google Scholar] [CrossRef]
- Kimura, T.; Ferran, B.; Tsukahara, Y.; Shang, Q.; Desai, S.; Fedoce, A.; Pimentel, D.R.; Luptak, I.; Adachi, T.; Ido, Y.; et al. Production of adeno-associated virus vectors for in vitro and in vivo applications. Sci. Rep. 2019, 9, 13601. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Rodríguez, D.R.; Ramírez-Solís, R.; Garza-Elizondo, M.A.; Garza-Rodríguez, M.D.L.; Barrera-Saldaña, H.A. Genome editing: A perspective on the application of CRISPR/Cas9 to study human diseases (Review). Int. J. Mol. Med. 2019, 43, 1559–1574. [Google Scholar] [PubMed]
- Ahsan, M.K.; Lekli, I.; Ray, D.; Yodoi, J.; Das, D.K. Redox regulation of cell survival by the thioredoxin superfamily: An implication of redox gene therapy in the heart. Antioxid. Redox Signal. 2009, 11, 2741–2758. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).