Ibogaine Induces Cardiotoxic Necrosis in Rats—The Role of Redox Processes
Abstract
:1. Introduction
2. Results
2.1. Histopathological Analysis
2.2. Presence of Glycogen and Color Intensity of Periodic Acid-Schiff (PAS) Staining
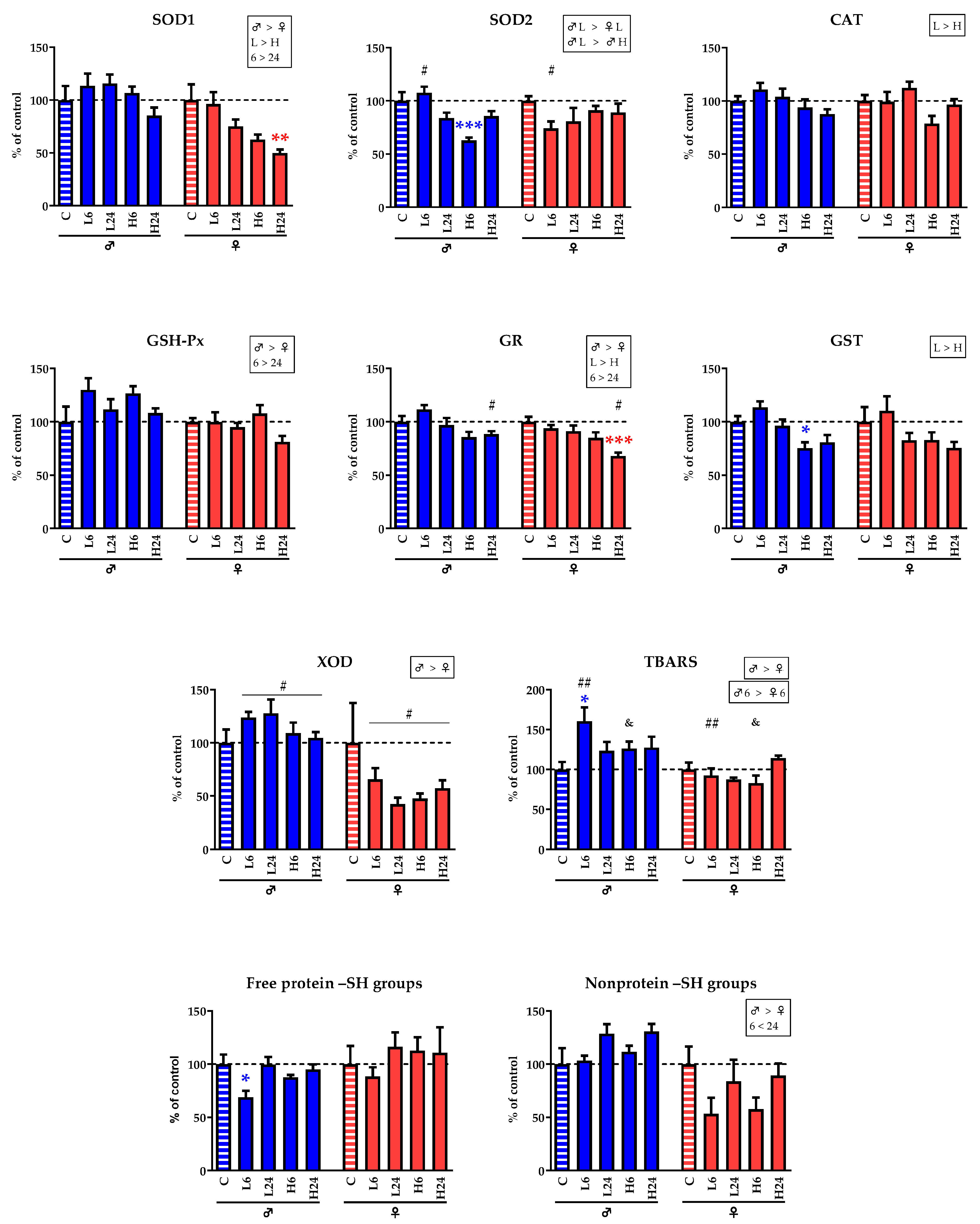
2.3. Enzyme Activities and Concentration of TBARS and –SH Groups
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Experimental Design
4.3. Tissue Preparation
4.4. Histological Analysis
4.5. Measurement of the Activities of Antioxidant Enzymes, Glutathione S-Transferases (GST) and Xanthine Oxidase (XOD)
4.6. Measurement of Concentration of TBARS, Non-Protein –SH Groups and Free Protein –SH Groups
4.7. Measurement of Protein Concentration
4.8. Data Analysis and Statistical Procedures
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Ibogaine | Noribogaine | ||||||
|---|---|---|---|---|---|---|---|
| No. Detected/Total No. | Mean | SEM | No. Detected/Total No. | Mean | SEM | ||
| ♂C | 0/6 | n.a. | n.a. | 0/6 | n.a. | n.a. | |
| ♂L6 | 2/6 | 0.0009 | 0.0002 | 6/6 | 0.0060 § | 0.0022 | |
| ♂L24 | 0/6 | n.a | n.a. | 0/6 | n.a. | n.a. | |
| ♂H6 | 5/6 | 0.0022 # | 0.0023 | 6/6 | 0.0705 & | 0.0072 | |
| ♂H24 | 2/6 | 0.0009 | 0.0002 | 6/6 | 0.0057 | 0.0032 | |
| ♀C | 0/6 | n.a. | n.a. | 0/6 | n.a. | n.a. | |
| ♀L6 | 1/6 | 0.0026 | n.a. | 6/6 | 0.0128 § | 0.0009 | |
| ♀L24 | 0/6 | n.a. | n.a. | 1/6 | 0.0112 | n.a. | |
| ♀H6 | 6/6 | 0.0076 # | 0.0010 | 6/6 | 0.1602 & | 0.0047 | |
| ♀H24 | 1/6 | 0.0008 | n.a. | 6/6 | 0.0086 | 0.0020 | |
| (a) | ||||||||||||||
| Water [mL/h/kg b.w.] | Food [g/h/kg b.w.] | Blood Glucose [mmol/L] | ||||||||||||
| Mean | SEM | Mean | SEM | Mean | Mean | |||||||||
| ♂C | 4.37 | 0.35 | 2.83 | 0.21 | 6.50 | 0.26 | ||||||||
| ♂L6 | 4.77 | 0.36 | 3.15 | 0.19 | 6.05 | 0.31 | ||||||||
| ♂L24 | 4.56 | 0.29 | 3.07 | 0.21 | 5.75 | 0.27 | ||||||||
| ♂H6 | 4.91 | 0.41 | 3.13 | 0.16 | 5.75 | 0.27 | ||||||||
| ♂H24 | 4.50 | 0.37 | 3.01 | 0.13 | 6.14 | 0.54 | ||||||||
| ♀C | 3.88 | 0.30 | 2.30 | 0.47 | 6.83 | 0.42 | ||||||||
| ♀L6 | 4.95 | 0.46 | 1.28 a | 0.48 | 5.65 a | 0.18 | ||||||||
| ♀L24 | 5.55 | 0.53 | 2.73 b | 0.20 | 6.41 | 0.38 | ||||||||
| ♀H6 | 4.09 | 0.69 | 0.76 a | 0.38 | 7.10 b | 0.39 | ||||||||
| ♀24 | 4.34 | 0.65 | 2.47 b | 0.32 | 6.84 | 0.32 | ||||||||
| (b) | ||||||||||||||
| Food [g/h/kg b.w.] | Food [g/h/kg b.w.] | |||||||||||||
| Mean | SEM | Mean | Mean | |||||||||||
| ♂L6—18 h | 3.67 | 0.13 | ♂H6—18 h | 3.78 | 0.25 | |||||||||
| ♂L6—6 h | 1.60 | 0.80 | ♂H6—6 h | 1.06 | 0.22 | |||||||||
| ♂L6—24h | 3.15 | 0.20 | ♂H6—24h | 3.13 | 0.16 | |||||||||
References
- Popik, P.; Layer, R.; Skolnick, P. 100 years of ibogaine: Neurochemical and pharmacological actions of a putative antiaddictive drug. Pharmacol. Rev. 1995, 47, 235–253. [Google Scholar] [PubMed]
- Alper, K. Ibogaine: A review. Alkaloids Chem. Biol. 2001, 56, 1–38. [Google Scholar] [PubMed]
- Litjens, R.P.; Brunt, T.M. How toxic is ibogaine? Clin. Toxicol. 2016, 54, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Alper, K.; Lotsof, H.; Kaplan, C. The ibogaine medical subculture. J. Ethnopharmacol. 2008, 115, 9–24. [Google Scholar] [CrossRef] [PubMed]
- Sheppard, S. A preliminary investigation of ibogaine: Case reports and recommendations for further study. J. Subst. Abuse Treat. 1994, 11, 379–385. [Google Scholar] [CrossRef] [PubMed]
- Koenig, X.; Hilber, K. The anti-addiction drug ibogaine and the heart: A delicate relation. Molecules 2015, 20, 2208–2228. [Google Scholar] [CrossRef] [PubMed]
- Aćimović, T.; Atanasijević, T.; Denić, K.; Lukić, V.; Popović, V.; Bogdanović, M. Death due to consumption of ibogaine: Case report. Forensic Sci. Med. Pathol. 2021, 17, 126–129. [Google Scholar] [CrossRef] [PubMed]
- Maas, U.; Strubelt, S. Fatalities after taking ibogaine in addiction treatment could be related to sudden cardiac death caused by autonomic dysfunction. Med. Hypotheses 2006, 67, 960–964. [Google Scholar] [CrossRef] [PubMed]
- Jeffcoat, R.; Cook, C.; Hill, J.; Coleman, D.; Pollack, G. Disposition of [3H] ibogaine in the rat. In NIDA Research Monograph Series; Harris, L.-S., Ed.; National Institute on Drug Abuse: Rockville, MD, USA, 1994; Volume 141, p. 309. Available online: https://archives.drugabuse.gov/sites/default/files/monograph141.pdf (accessed on 19 March 2023).
- Tatalović, N.; Vidonja Uzelac, T.; Mijović, M.; Koželj, G.; Nikolić-Kokić, A.; Oreščanin Dušić, Z.; Bresjanac, M.; Blagojević, D. Ibogaine Has Sex-Specific Plasma Bioavailability, Histopathological and Redox/Antioxidant Effects in Rat Liver and Kidneys: A Study on Females. Life 2022, 12, 16. [Google Scholar] [CrossRef] [PubMed]
- Pearl, S.M.; Hough, L.B.; Boyd, D.L.; Glick, S.D. Sex Differences in Ibogaine Antagonism of Morphine-induced Locomotor Activity and in Ibogaine Brain Levels and Metabolism. Pharmacol. Biochem. Behav. 1997, 57, 809–815. [Google Scholar] [CrossRef]
- Biosca-Brull, J.; Ona, G.; Alarcón-Franco, L.; Colomina, M.T. A transcriptomic analysis in mice following a single dose of ibogaine identifies new potential therapeutic targets. Transl. Psychiatry 2024, 14, 41. [Google Scholar] [CrossRef]
- Villalba, S.; González, B.; Junge, S.; Bernardi, A.; González, J.; Fagúndez, C.; Torterolo, P.; Carrera, I.; Urbano, F.J.; Bisagno, V. 5-HT2A Receptor Knockout Mice Show Sex-Dependent Differences following Acute Noribogaine Administration. Int. J. Mol. Sci. 2024, 25, 687. [Google Scholar] [CrossRef]
- Vidonja Uzelac, T.; Tatalović, N.; Mijović, M.; Koželj, G.; Nikolić-Kokić, A.; Oreščanin-Dušić, Z.; Bresjanac, M.; Blagojević, D. Effects of ibogaine per os application on redox homeostasis in rat liver and erythrocytes. Arch. Biol. Sci. 2019, 71, 133–144. [Google Scholar] [CrossRef]
- Vidonja Uzelac, T.; Tatalović, N.; Mijović, M.; Nikolić-Kokić, A.; Oreščanin-Dušić, Z.; Bresjanac, M.; Blagojević, D. Effects of ibogaine per os treatment on redox homeostasis in rat kidney. Arch. Biol. Sci. 2019, 71, 245–252. [Google Scholar] [CrossRef]
- Glick, S.; Maisonneuve, I.; Kitchen, B.; Fleck, M. Antagonism of alpha 3 beta 4 nicotinic receptors as a strategy to reduce opioid and stimulant self-administration. Eur. J. Pharmacol. 2002, 438, 99–105. [Google Scholar] [CrossRef]
- Leal, M.; Michelin, K.; Souza, D.; Elisabetsky, E. Ibogaine attenuation of morphine withdrawal in mice: Role of glutamate N-methyl-D-aspartate receptors. Prog. Neuropsychopharmacol. Biol. Psychiatry 2003, 27, 781–785. [Google Scholar] [CrossRef] [PubMed]
- Paškulin, R.; Jamnik, P.; Živin, M.; Raspor, P.; Štrukelj, B. Ibogaine affects brain energy metabolism. Eur. J. Pharmacol. 2006, 552, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Paškulin, R.; Jamnik, P.; Obermajer, N.; Slavić, M.; Štrukelj, B. Induction of energy metabolism related enzymes in yeast Saccharomyces cerevisiae exposed to ibogaine is adaptation to acute decrease in ATP energy pool. Eur. J. Pharmacol. 2010, 627, 131–135. [Google Scholar] [CrossRef]
- Paškulin, R.; Jamnik, P.; Danevčić, T.; Koželj, G.; Krašovec, R.; Krstić-Milošević, D.; Blagojević, D.; Štrukelj, B. Metabolic plasticity and the energy economizing effect of ibogaine, the principal alkaloid of Tabernanthe iboga. J. Ethnopharmacol. 2012, 143, 319–324. [Google Scholar] [CrossRef]
- Nikolić-Kokić, A.; Oreščanin-Dušić, Z.; Spasojević, I.; Slavić, M.; Mijušković, A.; Paškulin, R.; Miljević, Č.; Spasić, M.; Blagojević, D. Ex vivo effects of ibogaine on the activity of antioxidative enzymes in human erythrocytes. J. Ethnopharmacol. 2015, 164, 64–70. [Google Scholar] [CrossRef]
- Oreščanin-Dušić, Z.; Tatalović, N.; Vidonja-Uzelac, T.; Nestorov, J.; Nikolić-Kokić, A.; Mijušković, A.; Spasić, M.; Paškulin, R.; Bresjanac, M.; Blagojević, D. The Effects of Ibogaine on Uterine Smooth Muscle Contractions: Relation to the Activity of Antioxidant Enzymes. Oxidative Med. Cell. Longev. 2018, 2018, 5969486. [Google Scholar] [CrossRef] [PubMed]
- Tatalović, N.; Vidonja Uzelac, T.; Oreščanin Dušić, Z.; Nikolić-Kokić, A.; Bresjanac, M.; Blagojević, D. Ibogaine-Mediated ROS/Antioxidant Elevation in Isolated Rat Uterus Is _-adrenergic Receptors and KATP Channels Mediated. Antioxidants 2021, 10, 1792. [Google Scholar] [CrossRef] [PubMed]
- Vukašinović, E.; Purać, J.; Kojić, D.; Čelić, T.; Pihler, I.; Blagojević, D. Ex Vivo Effect of Ibogaine on the Transcriptional Level of Antioxidant Defense Related Genes in Honey Bee (Apis mellifera, L.) Midgut. Braz. Arch. Biol. Technol. 2021, 64, e21200773. [Google Scholar] [CrossRef]
- Reichelt, M.E.; Mellor, K.M.; Curl, C.L.; Stapleton, D.; Delbridge, L.M.D. Myocardial glycophagy—A specific glycogen handling response to metabolic stress is accentuated in the female heart. J. Mol. Cell Cardiol. 2013, 65, 67–75. [Google Scholar] [CrossRef] [PubMed]
- D’Oria, R.; Schipani, R.; Leonardini, A.; Natalicchio, A.; Perrini, S.; Cignarelli, A.; Laviola, L.; Giorgino, F. The Role of Oxidative Stress in Cardiac Disease: From Physiological Response to Injury Factor. Oxid. Med. Cell Longev. 2020, 2020, 5732956. [Google Scholar] [CrossRef] [PubMed]
- Burgoyne, J.R.; Mongue-Din, H.; Eaton, P.; Shah, A.M. Redox signaling in cardiac physiology and pathology. Circ. Res. 2012, 111, 1091–1106. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.M.; Gal, A. Cardiovascular System and Lymphatic Vessels. In Pathologic Basis of Veterinary Disease; Elsevier: St. Louis, MI, USA, 2017; pp. 561–616.e1. [Google Scholar] [CrossRef]
- Villena, J.; Henriquez, M.; Torres, V.; Moraga, F.; Díaz-Elizondo, J.; Arredondo, C.; Chiong, M.; Olea-Azar, C.; Stutzin, A.; Lavandero, S.; et al. Ceramide-induced formation of ROS and ATP depletion trigger necrosis in lymphoid cells. Free Radic. Biol. Med. 2008, 44, 1146–1160. [Google Scholar] [CrossRef] [PubMed]
- Troyano, A.; Sancho, P.; Fernández, C.; de Blas, E.; Bernardi, P.; Aller, P. The selection between apoptosis and necrosis is differentially regulated in hydrogen peroxide-treated and glutathione-depleted human promonocytic cells. Cell Death Differ. 2003, 10, 889–898. [Google Scholar] [CrossRef] [PubMed]
- Atlante, A.; Bobba, A.; Calissano, P.; Passarella, S.; Marra, E. The apoptosis/necrosis transition in cerebellar granule cells depends on the mutual relationship of the antioxidant and the proteolytic systems which regulate ROS production and cytochrome c release en route to death. J. Neurochem. 2003, 84, 960–971. [Google Scholar] [CrossRef]
- Gursahani, H.; Achampong, H.; Hadley, R.W. Diazoxide-induced activation of mitochondrial KATP channels protects against necrosis and apoptosis in cardiac myocytes, hippocampal neurons, and HepG2 cells. FASEB J. 2001, 15, pA568. [Google Scholar]
- Das, A.; Lohmann, S.M.; Kukreja, R. Overexpression of cyclic GMP-dependent protein kinases attenuates necrosis and apoptosis following ischemia/reoxygenation in adult rat cardiomyocytes via generation of ROS and opening of the mitochondrial KATP channel. Circ. Res. 2005, 97, E36–E37. [Google Scholar]
- Noma, A. ATP-regulated K+ channels in cardiac muscle. Nature 1983, 305, 147–148. [Google Scholar] [CrossRef]
- Cao, N.; Wang, J.J.; Wu, J.M.; Xu, W.L.; Wang, R.; Chen, X.D.; Feng, Y.N.; Cong, W.W.; Zhang, Y.Y.; Xiao, H.; et al. Glibenclamide alleviates β adrenergic receptor activation-induced cardiac inflammation. Acta Pharmacol. Sin. 2022, 43, 1243–1250. [Google Scholar] [CrossRef]
- Lau, R.P.; Fishbein, M.C. Chapter 12-Toxins and the heart. In Cardiovascular Pathology, 5th ed.; Buja, M.L., Butany, J., Eds.; Academic Press: Cambridge, MA, USA, 2022. [Google Scholar]
- Schlatmann, T.J.; Becker, A.E. Pathogenesis of dissecting aneurysm of aorta. Comparative histopathologic study of significance of medial changes. Am. J. Cardiol. 1977, 39, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Mash, D.; Kovera, C.; Pablo, J.; Tyndale, R.; Ervin, F.; Williams, I.; Singleton, E.; Mayor, M. Ibogaine: Complex pharmacokinetics, concerns for safety, and preliminary efficacy measures. Ann. N. Y. Acad. Sci. 2000, 914, 394–401. [Google Scholar] [CrossRef]
- Mash, D.; Kovera, C.; Buck, B.; Norenberg, M.; Shapshak, P.; Hearn, W.; Sanchez-Ramos, J. Medication development of ibogaine as a pharmacotherapy for drug dependence. Ann. N. Y. Acad. Sci. 1998, 844, 274–292. [Google Scholar] [CrossRef] [PubMed]
- Navaratnam, V. Heart Muscle: Ultrastructural Studies; Cambridge University Press: New York, NY, USA, 1987. [Google Scholar]
- Schneider, C.A.; Taegtmeyer, H. Fasting in vivo delays myocardial cell damage after brief periods of ischemia in the isolated working rat heart. Circ. Res. 1991, 68, 1045–1050. [Google Scholar] [CrossRef] [PubMed]
- Schneider, C.A.; Nguyêñ, V.T.B.; Taegtmeyer, H. Feeding and fasting determine postischemic glucose utilization in isolated working rat hearts. Am. J. Physiol. 1991, 260, H542–H548. [Google Scholar] [CrossRef] [PubMed]
- Depre, C.; Vanoverschelde, J.L.; Taegtmeyer, H. Glucose for the heart. Circulation 1999, 99, 578–588. [Google Scholar] [CrossRef]
- Milutinović, A.; Zorc-Pleskovič, R. Glycogen accumulation in cardiomyocytes and cardiotoxic effects after 3NPA treatment. Bosn. J. Basic Med. Sci. 2012, 12, 15–19. [Google Scholar] [CrossRef]
- Ahmad, F.; Arad, M.; Musi, N.; He, H.; Wolf, C.; Branco, D.; Perez-Atayde, A.R.; Stapleton, D.; Bali, D.; Xing, Y.; et al. Increased alpha2 subunit-associated AMPK activity and PRKAG2 cardiomyopathy. Circulation 2005, 112, 3140–3148. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.Y.; Ross, A.K.; Li, J.S.; Dearmey, S.M.; Mackey, J.F.; Worden, M.; Corzo, D.; Morgan, C.; Kishnani, P.S. Cardiac arrhythmias following anesthesia induction in infantile-onset Pompe disease: A case series. Paediatr. Anaesth. 2007, 17, 738–748. [Google Scholar] [CrossRef] [PubMed]
- Puthanveetil, P.; Wang, F.; Kewalramani, G.; Kim, M.S.; Hosseini-Beheshti, E.; Ng, N.; Lau, W.; Pulinilkunnil, T.; Allard, M.; Abrahani, A.; et al. Cardiac glycogen accumulation after dexamethasone is regulated by AMPK. Am. J. Physiol. Heart Circ. Physiol. 2008, 295, H1753–H1762. [Google Scholar] [CrossRef]
- Porta, J.; Vahedi-Faridi, A.; Borgstahl, G.E. Structural analysis of peroxide-soaked MnSOD crystals reveals side-on binding of peroxide to active-site manganese. J. Mol. Biol. 2010, 399, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Silverman, D.N.; Nick, H.S. Catalytic pathway of manganese superoxide dismutase by direct observation of superoxide. Methods Enzymol. 2002, 349, 61–74. [Google Scholar] [PubMed]
- Marcondes, F.K.; Bianchi, F.I.; Tanno, A.P. Determination of the estrous cycle phases of rats: Some helpful considerations. Braz. J. Biol. 2002, 62, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Luna, L.G. Manual of Histologic Staining Methods of the Armed Forces Institute of Pathology, 3rd ed.; McGraw-Hill: New York, NY, USA, 1968. [Google Scholar]
- Misra, H.; Fridovich, I. The role of superoxide anion in the autoxidation of epinephrine and a simple assay for superoxide dismutase. J. Biol. Chem. 1972, 247, 3170–3175. [Google Scholar] [CrossRef] [PubMed]
- Beutler, E. Red Cell Metabolism: A Manual of Biochemical Methods, 3rd ed.; Grune and Stratton: New York, NY, USA, 1982. [Google Scholar]
- Paglia, D.; Valentine, W. Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. J. Lab. Clin. Med. 1967, 70, 74–77. [Google Scholar]
- Glatzle, D.; Vuilleumier, J.; Weber, F.; Decker, K. Glutathione reductase test with whole blood, a convenient procedure for the assessment of the riboflavin status in humans. Experientia 1974, 30, 665–668. [Google Scholar] [CrossRef]
- Habig, N.; Pabst, M.; Jakoby, N. GST: 1st enzymatic step in mercapturic acid formation. J. Biol. Chem. 1974, 249, 7130–7139. [Google Scholar] [CrossRef]
- Terada, L.; Leff, J.; Repine, J. Measurement of xanthine oxidase in biological tissues. Methods Enzymol. 1990, 186, 651–656. [Google Scholar] [PubMed]
- Rehncrona, S.; Smith, D.; Akesson, B.; Westerberg, E.; Siesjo, B. Peroxidative changes in brain cortical fatty acids and phospholipids, as characterized during Fe2+- and ascorbic acid-stimulated lipid peroxidation in vitro. J. Neurochem. 1980, 34, 1630–1638. [Google Scholar] [CrossRef] [PubMed]
- Ellman, G. Tissue sulfhydryl groups. Arch. Biochem. Biophys. 1959, 82, 70–77. [Google Scholar] [CrossRef]
- Lowry, O.; Rosebrough, N.; Farr, A.; Randall, R. Protein measurement with folin phenol reagent. J. Biol. Chem. 1951, 193, 265–275. [Google Scholar] [CrossRef] [PubMed]
- Hinkle, E.; Wiersma, W.; Jurs, G. Applied Statistics for Behavioral Sciences, 5th ed.; Houghton Mifflin Company: Boston, MA, USA, 2002. [Google Scholar]

| (a) H&E | |||||||||||||||||||||
| Myocardial Necrosis | Myocardial Mononuclear Cell Infiltrate | Perivascular Inflammatory Infiltrate | Amount of Adipose Tissue | Pericarditis | |||||||||||||||||
| Absent | Focal | Difuse Moderate | Difuse Extensive | Decreased | Normal | Increased | |||||||||||||||
| ♂C | 6/6 | 0/6 | 0/6 | 0/6 | 0/6 | 0/6 | 0/6 | 6/6 | 0/6 | 0/6 | |||||||||||
| ♂L6 | 0/6 | 6/6 | 0/6 | 0/6 | 0/6 | 6/6 | 0/6 | 6/6 | 0/6 | 0/6 | |||||||||||
| ♂L24 | 1/6 | 5/6 | 0/6 | 0/6 | 0/6 | 6/6 | 0/6 | 6/6 | 0/6 | 0/6 | |||||||||||
| ♂H6 | 0/5 | 0/5 | 5/5 | 0/5 | 0/5 | 0/5 | 0/5 | 5/5 | 0/5 | 0/5 | |||||||||||
| ♂H24 | 0/6 | 0/6 | 3/6 | 3/6 | 0/6 | 1/6 | 0/6 | 6/6 | 0/6 | 0/6 | |||||||||||
| ♀C | 6/6 | 0/6 | 0/6 | 0/6 | 0/6 | 0/6 | 0/6 | 6/6 | 0/6 | 0/6 | |||||||||||
| ♀L6 | 3/4 | 1/4 | 0/4 | 0/4 | 0/4 | 0/4 | 0/4 | 4/4 | 0/4 | 0/4 | |||||||||||
| ♀L24 | 0/4 | 4/4 | 0/4 | 0/4 | 0/4 | 2/4 | 0/4 | 4/4 | 0/4 | 3/4 | |||||||||||
| ♀H6 | 0/6 | 0/6 | 0/6 | 6/6 | 0/6 | 5/6 | 0/6 | 6/6 | 0/6 | 0/6 | |||||||||||
| ♀H24 | 0/6 | 0/6 | 6/6 | 0/6 | 0/6 | 6/6 | 0/6 | 6/6 | 0/6 | 0/6 | |||||||||||
| (b) PAS | |||||||||||||||||||||
| % of Glycogen Positive Cells | Intensity of PAS Staining | ||||||||||||||||||||
| <33.3% | 33.3–66.6% | >66.6% | + | ++ | +++ | ||||||||||||||||
| ♂C | 5/5 | 0/5 | 0/5 | 5/5 | 0/5 | 0/5 | |||||||||||||||
| ♂L6 | 0/4 | 4/4 | 0/4 | 4/4 | 0/4 | 0/4 | |||||||||||||||
| ♂L24 | 2/4 | 2/4 | 0/4 | 4/4 | 0/4 | 0/4 | |||||||||||||||
| ♂H6 | 5/5 | 0/5 | 0/5 | 5/5 | 0/5 | 0/5 | |||||||||||||||
| ♂H24 | 6/6 | 0/6 | 0/6 | 6/6 | 0/6 | 0/6 | |||||||||||||||
| ♀C | 0/6 | 3/6 | 3/6 | 5/6 | 1/6 | 0/6 | |||||||||||||||
| ♀L6 | 0/2 | 1/2 | 1/2 | 2/2 | 0/2 | 0/2 | |||||||||||||||
| ♀L24 | 2/4 | 2/4 | 0/4 | 4/4 | 0/4 | 0/4 | |||||||||||||||
| ♀H6 | 4/5 | 1/5 | 0/5 | 5/5 | 0/5 | 0/5 | |||||||||||||||
| ♀H24 | 0/6 | 6/6 | 0/6 | 6/6 | 0/6 | 0/6 | |||||||||||||||
| ♂C | ♂L6 | ♂L24 | ♂H6 | ♂H24 | ♀C | ♀L6 | ♀L24 | ♀H6 | ♀H24 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SOD1 | mean SEM n | 6.354 0.844 6 | 7.210 0.735 6 | 7.348 0.542 6 | 6.776 0.393 6 | 5.412 0.492 6 | 9.107 1.360 6 | 8.766 1.020 6 | 6.838 0.589 6 | 5.702 0.423 6 | 4.540 ** 0.301 6 | ||
| SOD2 | mean SEM n | 3.414 0.280 6 | 3.676 0.197 6 | 2.860 0.174 6 | 2.142 *** 0.098 6 | 2.924 0.162 6 | 3.169 0.141 6 | 2.347 0.211 6 | 2.566 0.406 6 | 2.890 0.126 6 | 2.824 0.260 6 | ||
| CAT | mean SEM n | 12.10 0.543 6 | 13.38 0.768 6 | 12.53 0.925 6 | 11.36 0.928 6 | 10.58 0.563 6 | 13.53 0.749 6 | 13.42 1.244 6 | 15.16 0.805 6 | 10.65 0.965 6 | 13.05 0.729 6 | ||
| GSH-Px | mean SEM n | 35.23 5.038 6 | 45.71 3.902 6 | 39.34 3.321 6 | 44.56 2.392 6 | 38.16 1.532 6 | 35.38 1.275 6 | 35.51 3.305 6 | 33.84 1.370 6 | 38.41 2.737 6 | 28.87 1.995 6 | ||
| GR | mean SEM n | 25.38 1.428 6 | 28.84 1.052 6 | 25.03 1.753 6 | 22.11 1.296 6 | 22.86 0.704 6 | 20.68 0.987 6 | 19.41 0.659 6 | 18.84 1.114 6 | 17.56 1.080 6 | 14.02 *** 0.674 6 | ||
| GST | mean SEM n | 98.06 5.343 6 | 111.3 5.416 6 | 94.46 5.714 6 | 73.76 * 5.481 6 | 79.10 6.815 6 | 85.58 11.81 6 | 94.43 11.57 6 | 70.80 5.836 6 | 71.01 6.126 6 | 64.59 4.845 6 | ||
| XOD | mean SEM n | 0.0433 0.0054 6 | 0.0536 0.0022 6 | 0.0552 0.0057 6 | 0.0472 0.0042 6 | 0.0452 0.0024 6 | 0.0485 0.0182 6 | 0.0319 0.0051 6 | 0.0205 0.0030 6 | 0.0231 0.0022 6 | 0.0278 0.0036 6 | ||
| TBARS | mean SEM n | 23.22 2.130 6 | 37.24 * 4.065 6 | 28.62 2.569 6 | 29.28 2.027 6 | 29.60 3.156 6 | 55.30 4.741 6 | 51.10 4.901 6 | 48.26 1.278 6 | 45.72 5.307 6 | 63.14 1.723 6 | ||
| Free protein –SH groups | mean SEM n | 200.7 18.29 6 | 138.0 * 12.37 5 | 200.0 14.06 5 | 176.0 4.256 5 | 190.5 9.886 6 | 81.01 13.81 6 | 71.65 6.962 6 | 94.09 11.05 6 | 91.32 10.18 6 | 89.66 19.39 6 | ||
| Nonprotein –SH groups | mean SEM n | 2.209 0.816 6 | 2.282 0.223 5 | 2.839 0.445 5 | 2.463 0.289 5 | 2.884 0.395 6 | 6.883 2.790 6 | 3.376 2.512 6 | 5.764 3.423 6 | 3.963 1.844 6 | 6.145 1.923 6 |
| (a) One-Way ANOVA (♂C, ♂L6, ♂L24, ♂H6, ♂H24) | ||||||||||
| SOD1 | SOD2 | CAT | GSH-Px | GR | GST | XOD | TBARS | Free protein –SH groups | Nonprotein –SH groups | |
| n.s. | F = 9.44 p < 0.001 | n.s. | n.s. | F = 4.22 p < 0.01 | F = 6.84 p < 0.001 | n.s. | F = 3.00 p < 0.05 | F = 3.79 p < 0.05 | n.s. | |
| (b) One-Way ANOVA (♀C, ♀L6, ♀L24, ♀H6, ♀H24) | ||||||||||
| SOD1 | SOD2 | CAT | GSH-Px | GR | GST | XOD | TBARS | Free protein –SH groups | Nonprotein –SH groups | |
| F = 5.46 p < 0.01 | n.s. | F = 3.12 p < 0.05 | n.s. | F = 7.56 p < 0.001 | n.s. | n.s. | F = 2.95 p < 0.05 | n.s. | n.s. | |
| Three-Way ANOVA (♂L6, ♂L24, ♂H6, ♂H24, ♀L6, ♀L24, ♀H6, ♀H24) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SOD1 | SOD2 | CAT | GSH-Px | GR | GST | XOD | TBARS | Free protein –SH groups | Nonprotein –SH groups | |
| Factor: sex | ♂ > ♀ F = 42.26 p < 0.001 | n.s. | n.s. | ♂ > ♀ F = 18.32 p < 0.001 | ♂ > ♀ F = 10.66 p < 0.001 | n.s. | ♂ > ♀ F = 118.8 p < 0.001 | ♂ > ♀ F = 31.41 p < 0.001 | n.s. | ♂ > ♀ F = 24.03 p < 0.001 |
| Factor: dose | L > H F = 20.32 p < 0.001 | n.s. | L > H F = 11.37 p < 0.01 | n.s. | L > H F = 23.25 p < 0.001 | L > H F = 17.44 p < 0.001 | n.s. | n.s. | n.s. | n.s. |
| Factor: time | 6 > 24 F = 6.49 p < 0.05 | n.s. | n.s. | 6 > 24 F = 9.02 p < 0.01 | 6 > 24 F = 5.66 p < 0.05 | n.s. | n.s. | n.s. | n.s. | 6 < 24 F = 6.47 p < 0.05 |
| Interaction S × D | n.s. | F = 14.47 p < 0.001 | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. | n.s. |
| Interaction S × T | n.s. | n.s. | F = 5.19 p < 0.05 | n.s. | n.s. | n.s. | n.s. | F = 5.43 p < 0.05 | n.s. | n.s. |
| Interaction D × T | n.s. | F = 4.08 p < 0.05 | n.s. | n.s. | n.s. | n.s. | n.s. | F = 6.73 p < 0.05 | F = 4.33 p < 0.05 | n.s. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vidonja Uzelac, T.; Tatalović, N.; Mijović, M.; Miler, M.; Grahovac, T.; Oreščanin Dušić, Z.; Nikolić-Kokić, A.; Blagojević, D. Ibogaine Induces Cardiotoxic Necrosis in Rats—The Role of Redox Processes. Int. J. Mol. Sci. 2024, 25, 6527. https://doi.org/10.3390/ijms25126527
Vidonja Uzelac T, Tatalović N, Mijović M, Miler M, Grahovac T, Oreščanin Dušić Z, Nikolić-Kokić A, Blagojević D. Ibogaine Induces Cardiotoxic Necrosis in Rats—The Role of Redox Processes. International Journal of Molecular Sciences. 2024; 25(12):6527. https://doi.org/10.3390/ijms25126527
Chicago/Turabian StyleVidonja Uzelac, Teodora, Nikola Tatalović, Milica Mijović, Marko Miler, Tanja Grahovac, Zorana Oreščanin Dušić, Aleksandra Nikolić-Kokić, and Duško Blagojević. 2024. "Ibogaine Induces Cardiotoxic Necrosis in Rats—The Role of Redox Processes" International Journal of Molecular Sciences 25, no. 12: 6527. https://doi.org/10.3390/ijms25126527







